Volume 28 Supplement
Abstracts Podium presentations 30th National Conference on Incontinence (NCOI 2022) 11-14 May 2022, at the Melbourne Convention & Exhibition Centre, Melbourne, Victoria
DOI https://doi.org/10.33235/anzcj.28.suppl.s4
The impact of educational interventions for patients living with indwelling urinary catheters: A scoping review1
Alex J1, Salamonson Y2, Ramjan L2, Montayre J2, Fitzsimons J1 & Ferguson C1 3,
- Integrated and Community Health, Western Sydney Local Health District, Mount Druitt, New South Wales, Australia,
- Western Sydney University, School of Nursing and Midwifery, Penrith, New South Wales, Australia,
- Western Sydney Nursing and Midwifery Research Centre, Blacktown, New South Wales, Australia
Introduction: Many patients start to live with a long-term indwelling urinary catheter (IDC) unexpectedly and often find difficulty adjusting their psycho-social life with an IDC insitu2. Patients are often not supported with information and resources to care for and manage their catheter and are forced to rely on the internet or other resources. Complications associated with a long-term IDC contribute to avoidable, costly hospital presentations and increasing healthcare-associated burden3. To minimise catheter-associated complications and improve patients’ quality of life, it is essential to enhance catheter self-management by increasing patient and caregiver knowledge and self-efficacy. This study aims to explore the impact of educational interventions for patients living with an indwelling urinary catheter in situ.
Materials & methods: A systematic scoping review was undertaken in accordance with PRISMA guidelines and guided by Cochrane methodology, quality appraisal using Centre for Evidence-Based Medicine (CEBM) Joanna Briggs Institute (JBI), GRADE criteria and Quality Improvement Minimum Quality Criteria Set Version 1.0 (QI-MQCS V 1.0) tools. Studies (n = 446) published between 2000 and 2020 were retrieved from CINAHL, Cochrane Library, Scopus and Medline.
Results: A total of 15 primary research studies were included in the narrative thematic synthesis, nine were from the USA, two from Australia, two from the United Kingdom, one from Italy and one from Turkey. These 15 studies were published between 2003 and 2019 and accounted for 19918 patients with an age range 15 to 99 years. Study design varied; there were 11 quantitative and four qualitative studies. Studies were of low-moderate quality. A total of four themes were identified; (i) information needs of patients living with long-term catheters; (ii) core learning content and educational approaches; (iii) feasibility and effectiveness of educational interventions to reduce complications and improve quality of life; and (iv) common outcome measures.
While it is recognised that fear and anxiety were commonly experienced among patients living with indwelling urinary catheters, there is a scarcity of information provided to patients and their caregivers4. Despite the heterogeneity in educational interventions, all studies included in this review reported the specific approach undertaken was effective in minimising catheter-associated complications and improving the quality of life of patients living with a long-term IDC in situ. A care bundle approach, that partners clinicians with the patient and caregiver, was found to be more effective in promoting IDC self-management.
Nurses are well positioned to provide opportunistic and structured, planned education related to IDC self-management in both acute hospital and community settings. Future educational intervention approaches need to focus on addressing the educational needs of clinicians, patients, and caregivers.
Conclusion: The dissemination of information and the delivery of urinary catheter education to patients is inadequate. Core components of educational interventions should address fluid intake, bowel management, hygiene and self-monitoring/management, including adverse events. There is a need for future robust trials of educational and self-management interventions to improve the quality of life of patients who have a long-term IDC and who live in the community.
References
- Alex J, Salmonson Y, Ramjam LM, et al. The impact of educational interventions for patients living with indwelling urinary catheters: A scoping review. Contemporary Nurse 2020; 56(4): 309-330.
- De Jaeger M. Exploring urinary catheters: the perspectives of patients and nurses. British Journal of Nursing 2011; 20(7): 400-408.
- Prinjha S, Chapple A, Feneley R, et al. Exploring the information needs of people living with a long-term indwelling urinary catheter: A qualitative study. Journal of Advanced Nursing, 2016. 72(6):1335-1346.
- Sweeney A, Harrington A & Button D, Suprapubic catheters—a shared understanding, from the other side looking in. Journal of Wound Ostomy & Continence Nursing, 2007; 34(4): 418-424.
Development and psychometric testing of a knowledge tool for incontinence-associated dermatitis for clinicians: The Barakat-Johnson Incontinence-Associated Dermatitis Knowledge Tool (Know-IAD)
Barakat-Johnson M1,2,3, Beeckman D4,5, Campbell J6,7, Dunk AM8, Lai M1,2, Stephenson J9 & Coyer F7,9,10
- Sydney Local Health District, Sydney, New South Wales, Australia
- University of Sydney, Sydney, New South Wales, Australia
- Queensland University of Technology, Brisbane, Queensland, Australia
- Ghent University, Ghent, Belgium
- Örebro University, Örebro, Sweden
- Griffith University, Brisbane, Queensland, Australia
- Royal Brisbane and Women’s Hospital, Brisbane, Queensland , Australia,
- Canberra Hospital, Canberra , ACT, Australia
- University of Huddersfield, Huddersfield, England
- Queensland University of Technology, Brisbane , Queensland Australia
Introduction: The purpose of this study is to describe the development and evaluation of the psychometric properties of a tool used to assess clinician knowledge of incontinence-associated dermatitis (IAD).
Materials & methods: The instrument was developed in three phases: Phase 1 involved item development, Phase 2 evaluated content validity of the instrument by surveying clinicians and lay stakeholders within a single state of Australia and Phase 3 used a pilot multi-site cross-sectional survey design to determine composite reliability and evaluate scores of the knowledge tool.
In Phase 1, the instrument was developed by five persons with clinical and research subject expertise. In Phase 2, content validity was evaluated by a group of 13 clinicians (nurses, physicians, occupational therapists, dietitians, and physiotherapists) working in an acute care health service and two consumer representatives. In Phase 3, clinicians, working across five health services and on wards with patients who were diagnosed with IAD, participated in pilot-testing the instrument.
During Phase 1, a group of local and international experts developed a preliminary tool based on an international consensus document, our prior research evaluating IAD knowledge, and consensus among an expert panel of clinicians and researchers. Phase 2 used a survey design to determine content validity of the knowledge tool. Specifically, we calculated item- and scale-level content validity ratios and content validity indices for all questions within the draft instrument. Phase 3 comprised pilot-testing of the knowledge tool using a cross-sectional survey. Analysis involved confirmatory factor analysis to confirm the hypothesised model structure of the knowledge tool, as measured by model goodness-of-fit. Composite reliability testing was undertaken to determine the extent of internal consistency between constituent items of each construct.
Results: Phase 1 developed the Barakat-Johnson Incontinence-Associated Dermatitis Knowledge tool (Know-IAD)1, comprising 19 items and divided into three domains of IAD-related knowledge: 1) Aetiology and Risk, 2) Classification and Diagnosis, and 3) Prevention and Management. In Phase 2, 18 of the 19 items demonstrated high scale content validity ratios scores on relevance (0.75) and clarity (0.82); and high scale-content validity indices scores on relevance (0.87) and clarity (0.91). In Phase 3, 204 respondents completed the survey and the Know-IAD tool. The final 18-item Know-IAD tool demonstrated construct validity by model goodness-of-fit, as measured by the root mean square error of approximation (RMSEA), which was excellent for the Aetiology and Risk domain (RMSEA=0.02) and Prevention and Management domains (RMSEA=0.02); and good in the Classification and Diagnosis domain (RMSEA=0.04). Composite reliability (CR) was good in the Aetiology and Risk domain (CR=0.76) and Prevention and Management domains (CR=0.75) and adequate in the Classification and Diagnosis domain (CR=0.64). Respondents had good understanding of aetiology and risk (72% correct responses); fairly good understanding of prevention and management of IAD (64% correct responses) and moderate understanding of classification and diagnosis (40% correct responses).
Conclusion: The Know-IAD demonstrated good psychometric properties and provides preliminary evidence that it can be applied to evaluate clinician knowledge of IAD.
References
- Barakat-Johnson M, Beeckman D, Campbell J, et al. The development and psychometric testing of a knowledge tool on incontinence-associated dermatitis for clinicians (KnowIAD). Journal of Wound Ostomy and Continence Nursing 2022; 49(1):70-77
Clinician knowledge of incontinence-associated dermatitis: A multisite survey of healthcare professionals in acute and sub-acute settings
Barakat-Johnson M1,2,3, Stephenson J4, Lai M1,2 Coyer F3,4,5
- Sydney Local Health District, Sydney, New South Wales, Australia,
- University of Sydney, Sydney, New South Wales, Australia,
- Queensland University of Technology, Brisbane, Queensland, Australia,
- University of Huddersfield, Huddersfield, England,
- Royal Brisbane and Women’s Hospital, Brisbane , Queensland, Australia
Introduction: Clinician knowledge of the prevention and management of incontinence-associated dermatitis (IAD) plays an important role in the clinical care and health outcomes of patients with incontinence. The objective of this study is to examine clinician knowledge of IAD using the Barakat-Johnson Incontinence-Associated Dermatitis Knowledge Tool (Know-IAD)1. This study2 is part of Phase One of a multicentre, multimethod translational research study aimed at implementing the evidence-based guidelines3 to prevent and manage IAD in one state in Australia4.
Materials & methods: A cross-sectional multicentre survey was conducted from November 2019 to January 2020. The Know-IAD, an 18-item validated instrument that measures knowledge of IAD in the domains: aetiology and risk, classification and diagnosis, and prevention and management, was administered to a cross-section of eligible clinicians working across six hospitals across five health services. Participants were nurses (registered nurses and enrolled nurses), doctors, allied health professionals (occupational therapists, dietitians, physiotherapists) and students (nursing and allied health).
Participants anonymously completed hard copy surveys and consent was implied upon receipt of a completed survey. Descriptive and exploratory analyses were conducted to quantify the clinicians’ knowledge about the aetiology and risk, classification and diagnosis, and prevention and management of IAD. A mean knowledge score of 70% was considered to be satisfactory. The study was approved by the local health district hospital research ethics committee (approval number: HERCC/EXCOR\19-05; X19-0121 & 2019/ETH08742).
Results: A total of 428 respondents completed the survey. The results demonstrate that, overall, the clinicians in this study had low knowledge of IAD classification and diagnosis and prevention and management (mean correct responses: 45% on classification and diagnosis; 57% on prevention and management). 67 respondents (16%) achieved >70% correct responses for the classification and diagnosis domain, and; 84 respondents (20%) achieved >70% correct responses for the prevention and management domain. Respondents had good knowledge in the aetiology and risk domain (mean correct responses: 78%) where 348 respondents (84%) obtained a score of >70% correct responses. Overall, 129 respondents (31%) achieved >70% correct responses for the entire set of items. The clinicians’ knowledge of IAD was found to be below the minimum acceptable level of 70%.
Conclusions: Clinicians in this study had low knowledge and recognition of IAD, particularly in the areas of classification and diagnosis, as well as prevention and management, compared with the knowledge of how IAD is caused and the risk factors. Further, this study has identified knowledge gaps for further education which, in turn, will lead to quality-of-life improvements among patients.
References
- Barakat-Johnson M, Beeckman D, Campbell J, et al. The development and psychometric testing of a knowledge tool on incontinence-associated dermatitis for clinicians (KnowIAD). Journal of Wound Ostomy and Continence Nursing, 2022; 49(1): 70-77.
- Barakat-Johnson M, Stephenson J, Basjarahil S, et al. Clinician Knowledge of Incontinence-Associated Dermatitis: A Multisite Survey of Healthcare Professionals in Acute and Subacute Settings. Journal of Wound Ostomy and Continence Nursing. 2022 Mar-Apr 01;49(2):159-167.
- Beeckman D, Campbell J, Campbell K, et al. Proceedings from the Global IAD Expert Panel. Incontinence-associated dermatitis: moving prevention forward. Wounds International. 2015.
- Barakat-Johnson M, Basjarahil S, Campbell J, et al. Implementing best available evidence into practice for incontinence-associated dermatitis in Australia: A multisite multimethod study protocol. Journal of Tissue Viability. 2021;30(1): 67-77.
Australian children’s data retrieved with an innovative eHealth bedwetting solution
Pop V1, Yoneyama M2, Imazawa K2, Ann Hu A3, Chen T3, Christine Cheng C4, Summerville M5,
Meyer S5, Tutelaers M1, van Zanten J1, Swinckels P1 & Alex Hu A4
- LifeSense Group, Eindhoven, The Netherlands,
- LifeSense Group Japan, Tokyo, Japan,
- Institute of Occupational Health and Safety (IOHS), Taipei, Taiwan,
- Megabona International, Taipei, Taiwan,
- BioLIfe, Sydney, New South Wales, Australia
Introduction: This study is based on data from 117 children from Australia, aged between six and 12 years with bedwetting issues. Persistent bedwetting (functional nocturnal enuresis) becomes a problem once a child has reached six years of age and continues to wet the bed at least twice a week over three consecutive months. This common problem affects 12% of all six to 12-year-olds and can be both frustrating and embarrassing to children and parents1.
One solution to tackle functional nocturnal enuresis is a bedwetting alarm. This product helps train the child’s brain to recognise the body signals when the bladder is full and stay dry at night2. Based on this concept we developed an innovative non-invasive eHealth bedwetting alarm (called Oopsie Heroes Plus), including a tiny bedwetting sensor and simple mobile device application.
The aim of this study is to demonstrate the effectiveness of using the bedwetting alarm system to record accurate data about bedwetting, provide a better understanding of the bedwetting issues and eventually cure children from bedwetting sooner.
Materials & methods: Data relating to Australian children, aged six to 12 years, was collected via a mobile phone application. Consent has been requested from all users during the app installation. The children’s parents noted the child’s age and gender in the mobile phone application.
The sensor was attached to the underwear of the child (user) using a double-sided adhesive sticker. In case of a bedwetting event, the bedwetting sensor detected urine in the underwear and emitted a pulsating frequency sound which the application on the mobile device detected. As a result of a bedwetting event, the mobile emitted within less than five seconds an interval alarm sound that woke up the child. The mobile alarm sound could be for example a pre-recorded parents voice which has been proven to be the fastest and most effective way to wake a child up during his night-time sleep3. Data was automatically uploaded to our database and stored anonymously.
Results: The average age of the 117 users was 8 years and 3 months . The division in gender was 67% boys (n=78) and 33% girls (n=39). See figure 1.
The Australian data indicates that the average age at which users try a bedwetting alarm is approximately 8 years old. The gender division of (67% boys, 33% girls) correlates with research indicating a 2/3 vs. 1/3 division between boys and girls1.
Based on collected user data, we see that after using the bedwetting device and app children’s bedwetting frequency events decreased. From this we conclude that children using a bedwetting alarm can learn to control their bladder at night. This is in keeping with the current research 2.
Conclusion:
The bedwetting alarm demonstrates it is an effective system to:
- Discreetly collect bedwetting event data
- Provide an overview of events to parents/carers
- Help children wake up on time after a bedwetting event takes place.
This system can especially be of value to healthcare professionals and parents interested in understanding a child’s bedwetting pattern.
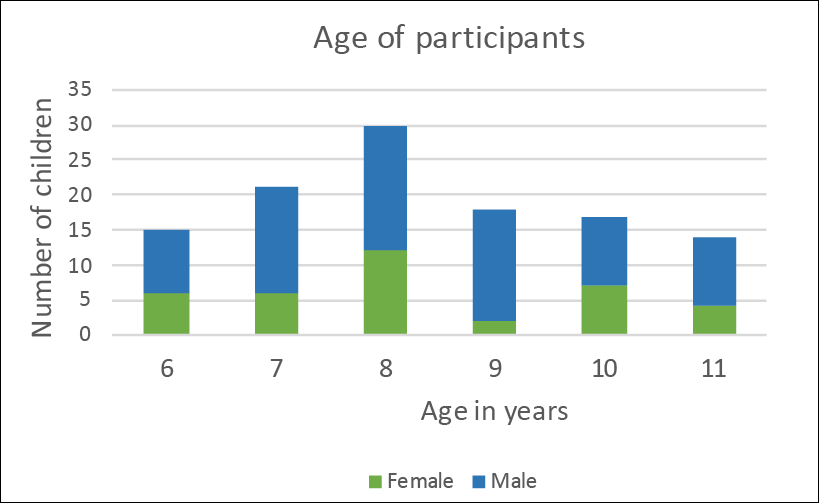
Figure 1: Number and age of participants
References
- Doleys D M. Behavioral treatments for nocturnal enuresis in children: a review of the recent literature. Psychological Bulletin 1977; 84(1): 30-54.
- Baker H. Practical solutions to help parents deal with childhood bedwetting. Professional nurse 2001;17(2): 133-136.
- Smith G A, Chounthirath T, & Splaingard M. Effectiveness of a Voice Smoke Alarm Using the Child’s Name for Sleeping Children: A Randomized Trial. The Journal of Pediatrics 2019.
Age-dependent effect of atosiban, an oxytocin receptor antagonist, on bladder contraction: Implications for the treatment of overactive bladder
Badshah M1, Ibrahim JP6, Ngie Su NN2, Loveland KL1, Fietz D5, Middendorff R4, Whittaker MR3 & Exintaris B2
- Department of Molecular and Translational Sciences, Monash University, Clayton, Victoria, Australia,
- Drug Discovery Biology, Monash Institute of Pharmaceutical Sciences, Melbourne, Victoria, Australia,
- Drug Delivery Disposition and Dynamics, Monash Institute of Pharmaceutical Sciences, Melbourne, Victoria, Australia,
- Institute of Anatomy and Cell Biology, Justus-Liebig-University, Giessen, Germany,
- Institute of Veterinary Anatomy, Histology and Embryology, Justus-Liebig-University, Giessen, Germany
- School of Biomedical Sciences, University of Queensland, Brisbane, Queensland, Australia
Introduction: Overactive bladder (OAB) is an age-related disorder characterised by disruptive lower urinary tract symptoms (LUTS) that include changes in frequency, urgency, nocturia, and urge incontinence. Though occurring at any age, symptoms increase with age, resulting in the gradual deterioration of the patient’s quality of life.
The development of LUTS may be linked to overexpression of oxytocin receptors (OXTRs) within bladder detrusor muscle, resulting in increased baseline myogenic tone.
Thus, it is hypothesized that targeting OXTRs within the bladder using oxytocin antagonists such as atosiban may attenuate myogenic tone within the bladder, thereby providing a new therapeutic avenue for the treatment of OAB.
Materials & methods: Contractility studies were conducted on bladder tissue from young (7-8 weeks) and older (7-9-months) Sprague-Dawley male rats (n=5, each group) via tension gauge organ bath with cumulative dose-response curves to oxytocin (10-11 to 10-6 M) generated pre-and post-incubation with atosiban (1 uM & 10-5M).
Results: In this study, oxytocin (1uM) significantly increased contractility in both age group male rats, while atosiban (10-5M) substantially inhibited oxytocin (1 uM) -induced contractility (p<0.001). Interestingly, lower concentrations of atosiban (1uM) were also capable of significant inhibition (p<0.05) of oxytocin-induced contractility in young but not older rats.
Conclusion: These findings suggest young rat bladder is more sensitive to inhibition of oxytocin-induced contractility via the antagonist atosiban than aged rats, indicating age-related differences in drug efficacy and may reflect differences in tissue physiology. Further studies are underway to understand the role of OXTRs within the bladder to improve our understanding of OAB and LUTS, and to explore future therapeutic opportunities.
The effect of 12 weeks of estriol cream on stress urinary incontinence post menopause: a prospective multi-national observational study
Te West N1, Harris K2, Jefferey S3, de Nie I4, Parkin K1, Roovers J-P4 & Moore KH1
- Department of Urogynaecology, St George Hospital, School of Women’s and Children’s Health, University of New South Wales, Sydney, New South Wales, Australia,
- The George Institute for Global Health, University of New South Wales, Sydney, New South Wales, Australia,
- Department of Obstetrics and Gynaecology, Groote Schuur Hospital, Cape Town, South Africa,
- Department of Obstetrics and Gynaecology, Academic Medical Center, Amsterdam, The Netherlands
Introduction: Stress urinary incontinence (SUI) is a debilitating condition affecting up to 35% of women. A decline in oestrogen at menopause is thought to contribute to urinary incontinence, with 70% of women relating the onset to their last menses 1. Theoretically, vaginal oestrogen should have a treatment effect in women with SUI, as oestrogen receptors are found in the bladder, urethra, vagina and pelvic floor muscles 1. Topical oestrogens increase urethral resistance by thickening the superficial layer of the urethral epithelium and increasing the periurethral vascularity. Because the vascular network accounts for one third of the urethral pressure, the estriol thus raises the urethral closure pressure and creates a more efficient mucosal seal.
Vaginal oestrogen cream changes urethral cytology by increasing intermediate and superficial epithelial cells and decreasing transitional cells (known as a positive maturation index). A positive maturation index has been shown to correspond to improvement in SUI symptoms. Unfortunately, the quantitative evidence for the benefit of vaginal oestrogen cream in women with stress incontinence is very limited.
The latest Cochrane review published in 2012 on vaginal oestrogen therapy concluded that such treatment may improve or cure incontinence2. However, sample sizes were small and there were marked differences in types, dosages, duration and routes of administration of the oestrogen therapy. It is recommended that future research should include standardised, validated, reproducible and simple outcome measures including quality-of-life tests.
A more recent pragmatic pilot study using estriol cream for six weeks showed significant benefit for the SUI domain of the Urogenital Distress Inventory-6 (UDI-6) 3. However, the most recent United States Food and Drug Administration (FaDA) report4 indicated that 12 weeks of estriol cream was needed for treatment of vaginal atrophy. Therefore, the aim of this prospective multinational observational study was to provide quantitative measures of urinary incontinence in women after 12 weeks of vaginal estriol cream as monotherapy.
Material & methods: Postmenopausal women with symptoms of either pure SUI or stress predominant mixed urinary incontinence were instructed to apply a constant dose of estriol cream vaginally (with written instructions). Baseline and post treatment outcome measures were obtained.
Main outcome measures: The stress domain of the UDI-6 was the primary subjective outcome measure and the vaginal pH was the primary objective outcome. Other subjective outcomes included the International Consultation on Incontinence Questionnaire Urinary Incontinence Short Form (ICIQ-SF), Incontinence Impact Questionnaire-7 (IIQ-7), Most Bothersome Symptom (MBS) approach and Patient’s Global Impression of Improvement (PGI-I). The secondary objective outcome used was the erect cough stress test. Patient compliance was also recorded. The study was approved by the local health district research ethics committees.
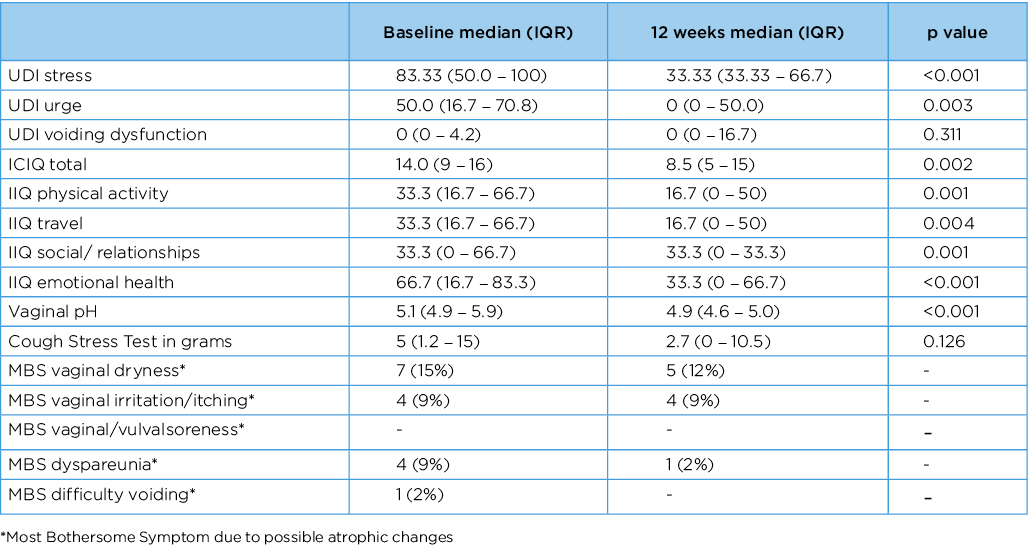
Results: There were 46 postmenopausal participants, median age 62.1 (IQR 56.2–65.4). At 12 weeks the stress domain of UDI-6 significantly improved from 83.3 (IQR 50–100) to 33.3 (33.3–66.6, P=0.001) and the vaginal pH from 5.1 (4.9–5.9) to 4.9 (4.6–5.0, p=0.005). The pad test at 12-week follow-up measured <1g in 18/43 patients (42%) and dry rate for the ICIQ-SF was 14/43 (33%). See Table 1 for results of primary and secondary outcome measures.
Conclusion: Twelve weeks of vaginal estriol cream significantly reduced symptoms of stress urinary incontinence in post-menopausal women.
Table 1. Results of primary and secondary outcome measures.
References
- Robinson D & Cardozo L. Estrogens and the Lower Urinary Tract. Neurourol Urodyn. 2011;30(5):754-757.
- Cody JD, Jacobs ML, Richardson K, et al. Oestrogen therapy for urinary incontinence in post-menopausal women. Cochrane Database Syst Rev. 2012 Issue 10. Art. No.: CD001405.
- Weber MA, Lim V, Oryszczyn J, et al. The Effect of Vaginal Oestriol Cream on Subjective and Objective Symptoms of Stress Urinary Incontinence and Vaginal Atrophy: An International Multi-Centre Pilot Study. Gynecologic and obstetric investigation 2017;82 (1):15-21.
- US Department of Health and Human Services FaDA, Center for Drug Evaluation and Research (CDER): . Guidance for Industry: Estrogen and Estrogen/Progestin Drug Products to Treat Vasomotor Symptoms and Vulvar and Vaginal Atrophy Symptoms Recommendations for Clinical Evaluation. 2003: Rockville, MD
Sacral neuromodulation in Australian patients with neurogenic lower urinary tract dysfunction
Pham C1,2, Parkin C2,3, Yang Y4, Delaney D1,2,4 & Chung A 1,2,3,4
- Northern Beaches Hospital, Frenchs Forest, New South Wales, Australia,
- North Shore Urology Research Group, St Leonards, New South Wales, Australia,
- Royal North Shore Hospital, St Leonards, New South Wales, Australia,
- North Shore Private Hospital, St Leonards, New South Wales, Australia
Objective: The understanding of the utility of sacral neuromodulation (SNM) for neurogenic lower urinary tract dysfunction (NLUTD) is limited, with only small series in the literature and to our knowledge, no published Australian data. The aim of this study was to evaluate the clinical outcomes of SNM for treatment of NLUTD in Australian patients.
Materials & methods: A retrospective analysis of patients who received a permanent SNM implant between December 2014 and March 2021 was conducted. Patients completed a urodynamic test pre-operatively. They completed a 3-day bladder diary, uroflowmetry and post-void residual (PVR) measurement pre-operatively and at 6-monthly intervals post-operatively following SNM insertion. Urinary function, patient reported outcome measures and adverse events were assessed. This study was approved by the local human research ethics committee.
Results: A total of 36 patients received a permanent SNM implant. The mean follow-up duration was 25±20 months, with the majority (89%, n=32) of patients reporting a >50% improvement on bladder diary evaluation. There was a significant increase in void volume (p<0.001), decrease in PVR (p<0.001), decrease in voiding frequency (p<0.001), decrease in incontinence episodes (p=0.002) and decrease in pad number (p<0.001). There was no significant difference in peak flow (p=0.21). There was no significant difference in SNM efficacy between patients with progressive or non-progressive neurological conditions.
Conclusion: SNM is a safe and effective therapy for NLUTD in the context of both progressive and non-progressive neurological conditions. It should be offered more readily to patients with NLUTD given it is a minimally invasive treatment option with potential to make clinically meaningful improvement to quality of life.
The safety of surgical mesh - What is YouTube teaching our patients?
Parkin C1,2, Pham C1,3 & Chung A1,2,3
- North Shore Urology Research Group, St Leonards, New South Wales, Australia,
- Royal North Shore Hospital, St Leonards, New South Wales, Australia,
- Northern Beaches Hospital, Frenchs Forest, New South Wales, Australia
Introduction: Due to the complications associated with transvaginal mesh for pelvic organ prolapse repair, many patients are worried about consenting to urological procedures which also involve mesh, such as for stress urinary incontinence. This study assesses the quality and content available to patients on YouTube when searching for information about the safety of mesh in surgery.
Materials & methods: Two independent reviewers, both medical practitioners, searched the social media platform You Tube in June 2021 using the search term ‘is surgical mesh safe’ and evaluated the first 50 videos listed. Information related to views, video producer, quality of content, understandability and actionability was assessed. The videos were assessed using the validated Patient Education Materials Assessment Tool (PEMAT) and DISCERN instrument criteria 1,2. PEMAT is a tool used to assess the understandability and actionability of audio-visual content. The DISCERN criteria was used to assess the quality of health information through the sourcing, bias and reliability of information. Statistical computing used R software3 for statistical analysis, including univariate analysis of PEMAT and DISCERN scores.
Results: Only 60% of videos were produced by a recognised medical institution. Despite the median PEMAT understandability score being 77%, there was limited actionability of content reflected by a PEMAT score of 23%. The overall quality of information provided was poor and failed to adequately address the safety of surgical mesh. There was no association with the numbered listing on YouTube or number of views with higher PEMAT or DISCERN scores.
Conclusion: YouTube is one of the most readily accessible mediums for health information. It is shown to be a poor source of information on the safety, utility and efficacy of surgical mesh. The quality of information was significantly biased. Concerningly, there was no association between the quality of content and the number of views. Medical practitioners need to be aware of this as patients may have preconceptions on the use of mesh.
References
- Shoemaker SJ, Wolf MS & Brach C. The Patient Education Materials Assessment Tool (PEMAT) and User’s Guide. Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services: Rockville, MD, 2013 (updated 2020) Available at https://www.ahrq.gov/health-literacy/patient-education/pemat.html Accessed 3 June 2021
- DISCERN Online. Quality criteria for consumer health information. The British Library and the NHS Executive Research & Development Programme 1997 Available at: http://www.discern.org.uk/discern_instrument.php Accessed 3 June 2021
- R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing. 2020 Vienna, Austria. Available at: www.R-project.org/ Accessed March 2022.
Incontinence-related outcome measures after radical prostatectomy
Pham C1, Patel M1,2 & Mungovan S3,4
- Specialty of Surgery, Faculty of Medicine and Health, University of Sydney, Camperdown, New South Wales, Australia
- Westmead Private Hospital, Westmead, New South Wales, Australia
- Westmead Private Physiotherapy Services, Westmead, New South Wales, Australia
- The Clinical Research Institute, Westmead, New South Wales, Australia
Introduction: The objective was to evaluate the correlation between three- and six-week postoperative 24-hour pad weight, daily pad number and the International Consultation on Incontinence Questionnaires for Male Lower Urinary Tract (ICIQ-MLUTS), ICIQ-Short Form (ICIQ-SF) and UCLA Prostate Cancer Index (UCLA-PCI) in patients undergoing robotic-assisted radical prostatectomy (RARP).
Materials & methods: This prospective study included patients undergoing RARP between February and November 2019. Patients completed a 24-hour pad test, assessing pad weight and number, and three validated patient reported outcome measures (PROMs); the ICIQ-MLUTS, ICIQ-SF and UCLA-PCI, pre-operatively and at three and six weeks post-operatively. This study was approved by the local human research ethics committee.
Results: A total of 47 patients were included in the study. There was a strong correlation between 24-hour pad weight and the ICIQ-SF at three weeks (r=0.71, p<.001) and six weeks (r=0.68, p<.001). There was a strong correlation between 24-hour pad weight and ICIQ-MLUTS incontinence (r=0.80, p<.01) and incontinence QoL burden (r=0.79, p<.01) at six weeks. There was a moderate correlation between the 24-hour pad weight and UCLA-PCI urinary function (r=0.58, p<.001) and urinary QoL burden (r=0.66, p<.001) at six weeks. The ICIQ-MLUTS voiding, frequency and nocturia domains and the UCLA-PCI bowel and sexual function domains did not significantly correlate with 24-hour pad weight.
Conclusion: PROMs are a reliable substitute for the 24-hour pad weight test for post-prostatectomy incontinence (PPI) assessments in the early post-RARP period. The ICIQ-SF and UCLA-PCI urinary function and QoL scores correlate with 24-hour pad weight. However, the ICIQ-MLUTS incontinence and QoL scores provide the strongest correlation with PPI.
NITE-SS, a nocturnal bladder symptom score for older adults
Bower W F1, Goonan R1, Wagg A2, Ervin C1 & Whishaw DM1
- Melbourne Health, Melbourne, Victoria, Australia,
- University of Alberta, Edmonton, Canada
Introduction: Nocturia commonly occurs alongside other symptoms of bladder dysfunction at night, such as urinary urgency, urgency incontinence and enuresis 1. A symptom-specific score for bladder dysfunction at night has recently been developed 2. The aim of this study was to test the nocturnal bladder symptom score (NITE-SS) that captures clinically relevant domains and to generate a robust short form. Quantification of nocturnal bladder dysfunction will enable future evaluation of the impact of individualised treatment.
Materials & methods: The NITE-SS measure was developed from a subjective patient-orientated perspective and refined following patient feedback2. In this study, factor analysis was performed on the original measure with the aim of reducing the number of variables. Endorsement frequency was obtained for all items and sub-scales using counts; items with a high floor effect (i.e. >70% of responses ‘never’ or its equivalent) or >20% missing data were noted. Principal component analysis was used to extract the maximum variance explained by the first factors and then by subsequent factors. We report factor loading, eigenvalues and factor scores from a sample of 150 NITE-SS completed by individuals older than 70 years who were either inpatients at our hospital or attending outpatient clinics. Analyses are presented to justify the final NITE-SS. The study was approved by the institutional ethics committee (QA2021045).
Results: Of the 151 NITE-SS data sets, 98 were completed by inpatients and 53 by community-dwelling older adults attending a hospital continence clinic. Females comprised 68% of the responders. The data set contained no missing values. Nocturia of at least twice per night, frequent urinary urgency, incontinence while asleep and incontinence en route to the bathroom at night were reported by 70.8%, 47%, 20.6% and 19.8% of participants respectively. Five items showed a floor effect. All correlation coefficients were <0.8 indicating no multi-collinearity. Kaiser-Meyer-Olkin = 0.83; Bartlett’s test of sphericity was significant. Four factors returned an eigenvalue >1.0 explaining a cumulative variance of 59%. Specific items related to symptom description were retained. The decision tree for removing redundant items considered weighting in multiple components, inter-relationship, likelihood of change post-intervention and low endorsement frequency. Finally, three factors were identified: sleep, incontinence and personal bother attributable to LUTS at night. The final metric (Figure 1*) contained 13 items each scored as 0 for lowest level of attribute through to 4 for most negative.
Conclusion: The new metric, NITE-SS, has been successfully subjected to principal component analysis and is now ready for reliability and sensitivity testing in an older age cohort.
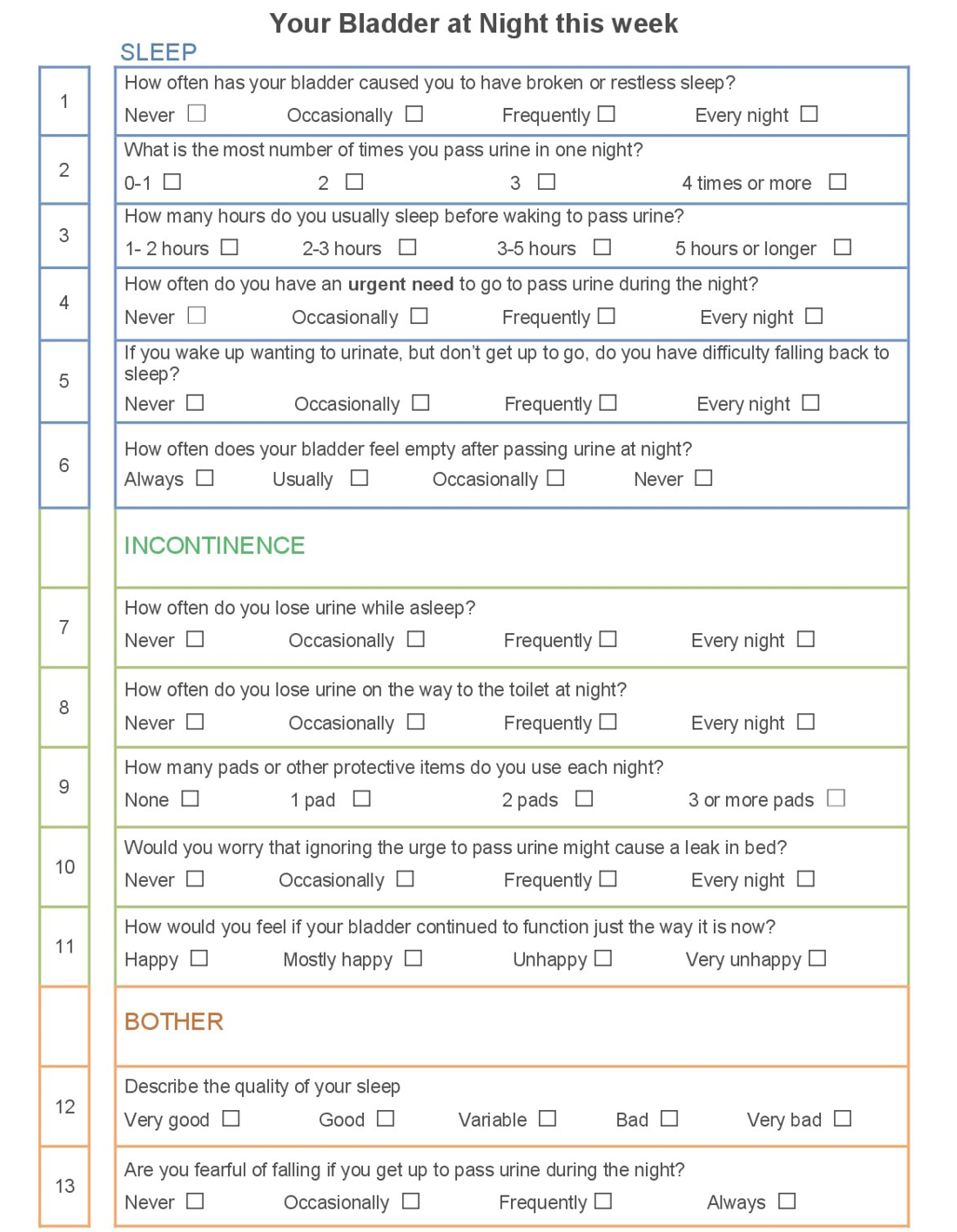
Figure 1: Final three factor version of NITE-SS
References
- Nguyen HX, Penukonda S, Stephen S, et al. Wake-up call: 4 out of 5 older hospitalised patients have nocturnal lower urinary tract symptoms. Australasian Journal on Ageing. 2021; 40(4): 457-460
- Bower WF, Ervin CF, Whishaw DM, et al. Initial development of a patient-centred symptom score for bladder dysfunction at night in older hospitalised patients. Australian and New Zealand Continence Journal 2021; 27(3):71-76
The time to complete bowel care for people with a recent spinal cord injury. Is it worth the time, resources and cost? A non-inferiority, crossover, randomised controlled trial comparing two methods of enema administration
Kelly L1,2, Harvey L1, Glinsky J1,3, Garratt G4 & Nier L1,2
- University of Sydney, St Leonards, New South Wales, Australia,
- Royal North Shore Hospital, St Leonards, New South Wales, Australia,
- Northern Sydney Local Health District, St Leonards, New South Wales, Australia,
- Royal Rehab, Ryde, New South Wales, Australia
Introduction: Effective bowel functioning is one of the most important areas of management for a person living with spinal cord injury (SCI) 1. Despite this, there is a lack of consensus among nurses working in the speciality of SCI as to which is the optimal bowel care routine. Some people who had sustained a recent SCI used daily micro enemas (low enema), while others used micro enemas in a 10mL syringe with a nelaton catheter attached (high enema). There was no obvious evidence to support the high enema routine only that some nurses felt that high enemas were better because they were quicker than low enemas.
Therefore, the objective of the randomised controlled trial was to determine whether low enemas are as quick, if not quicker than high enemas in the time that it takes to complete bowel care in people with a recent SCI.
Materials & methods: Twenty people admitted to hospital with recent SCI were randomly assigned to two treatment sequences; four weeks of low enemas followed by four weeks of high enemas, or vice versa. Each treatment sequence was eight weeks with a crossover at the end of week four. The primary outcome was time to complete bowel care. Secondary outcomes reflected faecal incontinence, quality-of-life, perception of treatment effectiveness and participant reported time to complete bowel care. The primary and secondary outcomes were measured by blinded assessors in week four and week eight. A non-inferiority margin of 10 minutes for time to complete bowel care was set a priori. Ethics approval was provided by the Northern Sydney Local Health District Human Research Committee. The trial was prospectively registered at the Australian New Zealand Clinical Trial Registry (www.anzctr.org.au; ACTRN12618000221257 with a Universal Trial Number: U1111-1194-6282).
Results: The mean between group difference (95% CI) for the time to complete bowel care was -0.5 minutes (-2.8 to 1.8), where a negative value favours the high enema. Results were similar for all secondary outcomes (see Figure 1.).
Conclusions: Low enemas are as effective, if not more effective than as high enemas and therefore should be the optimal bowel care routine for people with a recent SCI.
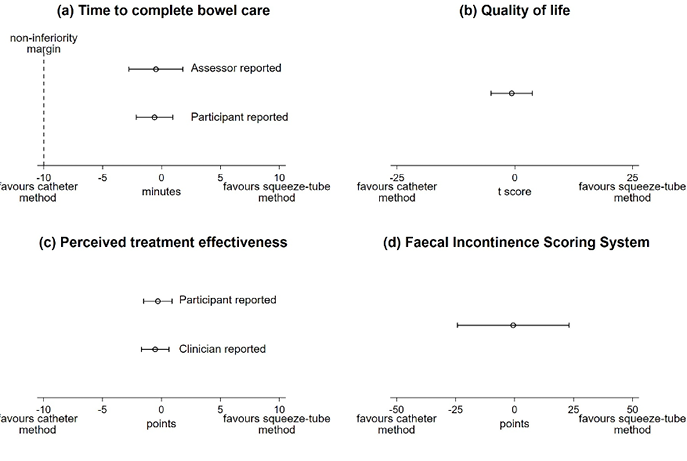
Figure 1. Primary and Secondary Outcome Measures Mean between group differences with (95% CI)
Reference
- Anderson KD. Targeting recovery: Priorities of the spinal cord-injured population. J Neurotrauma 2004; 21(10): 1371-83.
Development of an acute spinal cord injury neurogenic bladder and bowel pathway
Levy C1, Gaikward S2, Whishaw DM3 & Bower WF1, 3, 4
- Department of Physiotherapy, Royal Melbourne Hospital, Melbourne, Victoria, Australia,
- Department of Nursing, Royal Melbourne Hospital, Melbourne, Victoria, Australia
- Continence Service, Sub-Acute Community Services, Royal Melbourne Hospital, Melbourne, Victoria, Australia
- Department of Aged Care, Faculty of Medicine, Dentistry and Health Sciences, University of Melbourne, Melbourne, Victoria, Australia
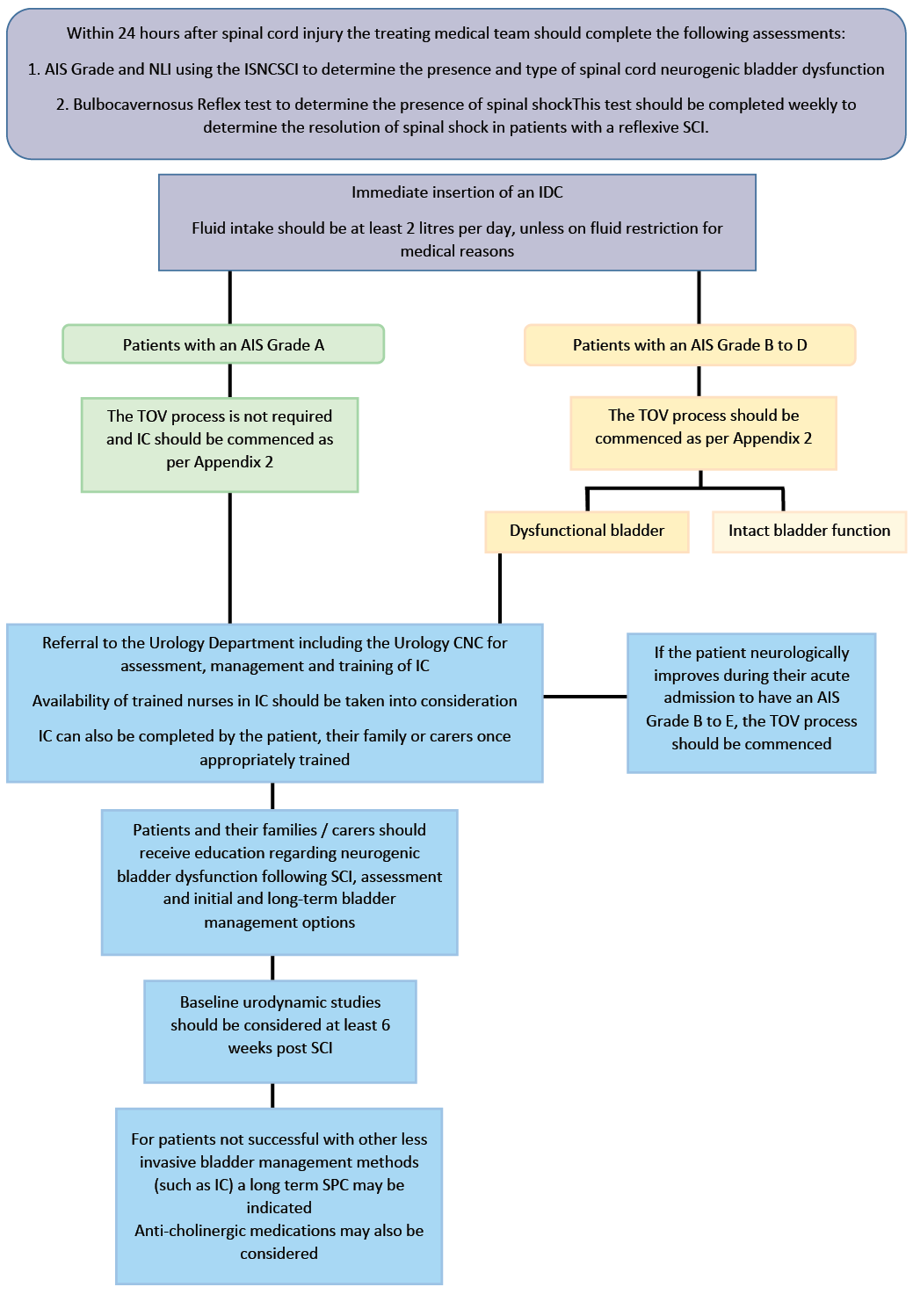
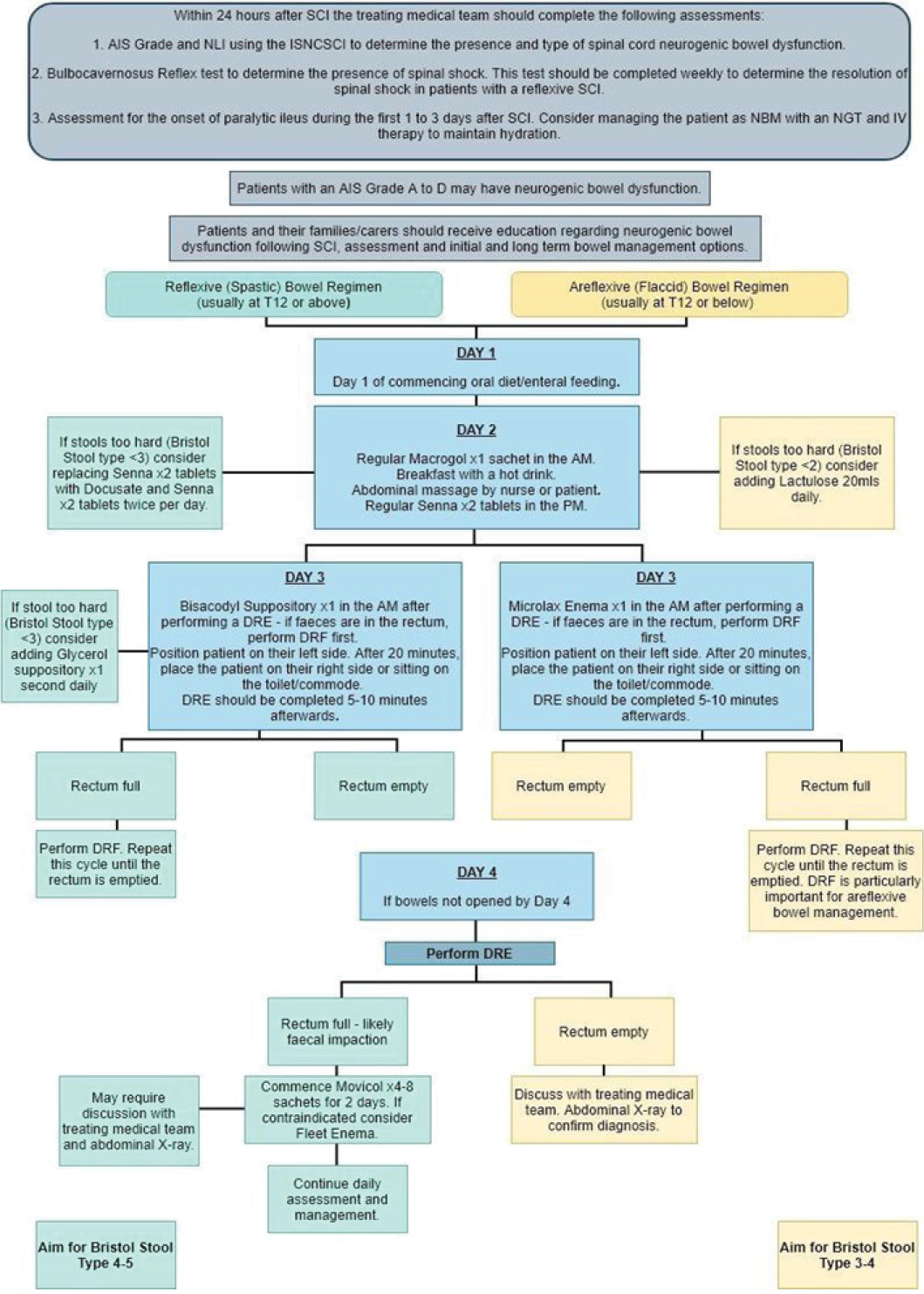
Introduction: The aims of this project were twofold. Firstly, to determine optimal assessment and management of patients with acute neurogenic bladder and/or bowel dysfunction immediately following spinal cord injury (SCI), based on research and best clinical practice. Secondly, to translate these findings into a policy that all clinical staff involved in the care of SCI patients could access and implement in practice.
Materials & methods: A literature review was performed for papers from the last decade that described management of bladder and bowel dysfunction after acute SCI. Evidence underlying optimal management was reviewed by two of the authors, summarised and presented to the multidisciplinary team caring for patients with SCI within our organisation. An optimal clinical pathway suitable to the ward culture of our institution and informed by this relevant literature was formulated and reviewed by key stakeholders within the institution.
Results: Eleven papers were included in the literature review. Two clinical guidelines were also retrieved and reviewed1.2. Key findings related to assessment, management and the benefits of adhering to a protocol of clinical practice were summarised. Fidelity with evidence identified was evaluated and practice gaps recognised.
Timely and appropriate assessment, management and treatment of patients with spinal cord neurogenic bladder and / or bowel dysfunction during acute care was pivotal in optimising bladder and bowel function and mitigating risk of preventable harm prior to discharge to specialised rehabilitation. Acute SCI bladder (Figure 1a) and bowel (Figure 1b) management pathways were subsequently developed to provide clear guidance to clinical staff within our organisation. Anticipated barriers to the translation of this pathway into clinical process of care within our organisation’s unique culture and environment were identified.
Conclusion: To meet an evidence-practice gap in acute hospital bladder and bowel care, the available evidence was reviewed and summarised. Using this evidence, a clinical management pathway for both bladder and bowel was developed to help optimise care provided to SCI patients. The future direction for this research is the implementation process of the management pathways. A formal implementation process will now be rolled out, whereby clinical staff will have access to education about the underlying rationale for change and given opportunity to be part of an iterative process to embed best practice into usual care for SCI patients within this organisation.
References
- Hogan M, Mullane J. (2019). Management of spinal neurogenic bladder & bowel. University College London Hospitals NHS Foundation Trust.
- Byrne C, Clements R, Mahony A. (2018). VSCS - Neurogenic bladder management. Austin Health: Melbourne
The phosphodiesterase inhibitors tadalafil (Cialis®) and sildenafil (Viagra®) enhance vasodilation of the bladder vasculature.
Nilsson D, Chess-Williams R & Sellers D
Centre for Urology Research, Bond University, Gold Coast, Queensland, Australia
Introduction: Research suggests that reduced blood flow to the bladder may be involved in the pathology of lower urinary tract symptoms 1. Ageing, obesity and atherosclerosis are involved in these reductions in perfusion. Tadalafil and sildenafil are clinically used phosphodiesterase-5 (PDE5) inhibitors, which are used to treat erectile dysfunction, but have been demonstrated to improve lower urinary tract symptoms and blood flow in animal models 2. It is yet to be determined whether these drugs may be acting directly on the bladder vasculature to potentiate relaxation. Thus, the study aim was to determine whether these clinically used inhibitors can potentiate nitric oxide-mediated relaxations of the porcine model of the superior vesical artery.
Materials & methods: Superior vesical artery branches from pigs (6-months-old) were obtained from a local abattoir. Sections (~4mm length, ~1mm internal diameter) were isolated and mounted between two horizontal stirrups in 30mL organ baths containing oxygenated physiological salt solution at 37˚C. Electrical field stimulations (EFS) were obtained at 80V (~90mA) at 20Hz, 10sec trains with a 1ms pulse width. EFS-mediated responses were abolished with tetrodotoxin (10-6M). EFS-mediated responses were obtained in absence and presence of L-NNA (NOS inhibitor), L-NPA (nNOS inhibitor), guanethidine (sympatholytic), αβmATP (desensitise purinergic), tadalafil and sildenafil (PDE5 inhibitors). Experiments were completed using intact and endothelium-denuded vessels.
Results: Stimulation of the nerves by EFS caused a distinct initial contraction and a slower relaxation of the porcine superior vesical arteries (Fig. 1A). Following the addition of αβmATP and guanethidine in denuded vessels, relaxation responses were significantly (p<0.01 vs control, n=7) enhanced from -0.07g±0.04 to -0.37g±0.06 (Fig. 1B). The selective neuronal nitric oxide synthase (nNOS) inhibitor L-NPA significantly (p<0.01 vs Guanethidine, n=7) reduced relaxation responses by ~80% (Fig. 1B), suggesting a dominant role of nNOS within the vessel. The clinically used PDE5 inhibitor tadalafil and sildenafil significantly (p<0.01 vs Guanethidine, n=6) enhanced relaxations by 28% and 52%, respectively (Fig. 1D).
Conclusion: Nitric oxide plays a predominant and important role in the vascular tone of the porcine superior vesical artery, generated by endothelial and neuronal nitric oxide synthase. Both clinically used phosphodiesterase-5 inhibitors potentiated nitric oxide-mediated relaxation demonstrating the isoenzyme phosphodiesterase-5 is present within the tissue. Due to the predominance of nitric oxide within the superior vesical artery, the phosphodiesterase-5 inhibitors, tadalafil and sildenafil, could exert their action on the bladder vasculature and have the potential as therapeutics for ischaemic-related bladder dysfunctions.
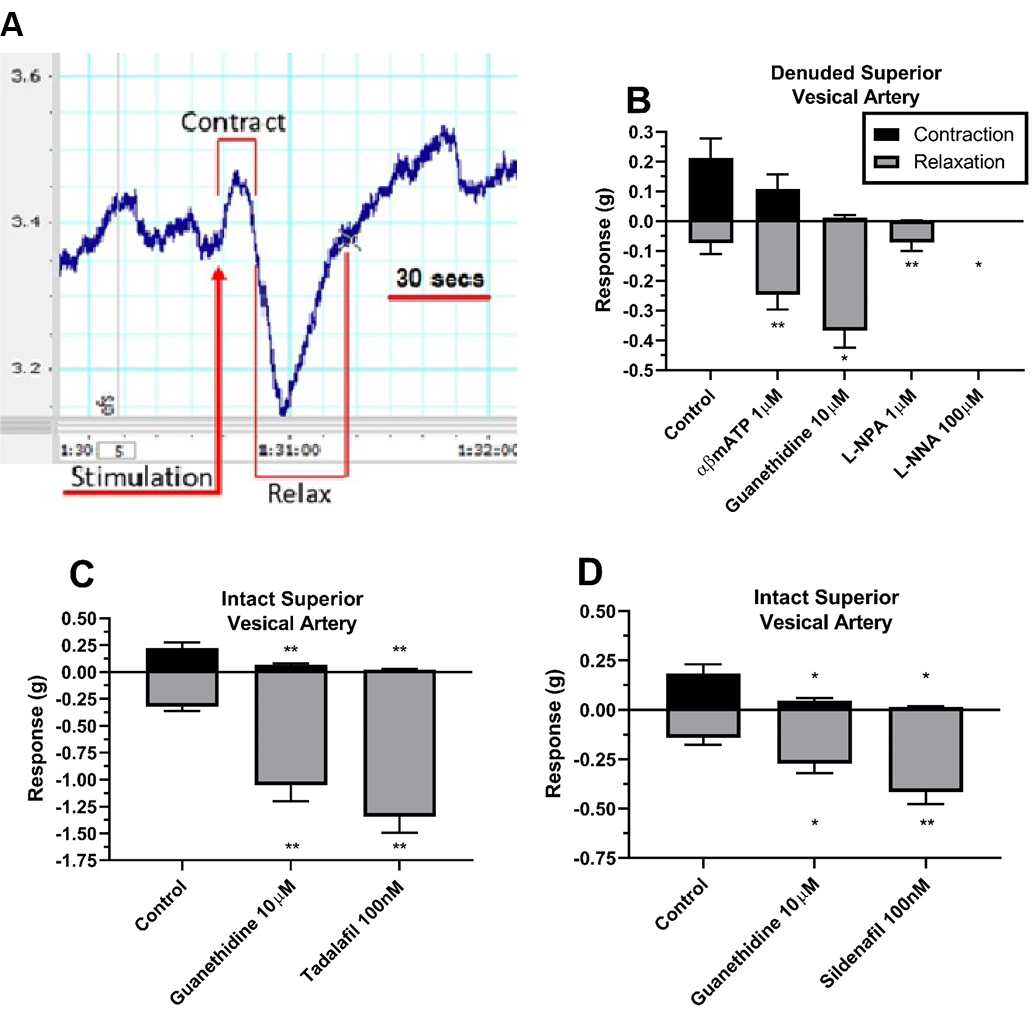
Figure 1. A) Representative trace of EFS-mediated contraction and relaxation on porcine superior vesical artery (SVA). B) Isolation and abolishment of EFS-mediated nitric oxide relaxation on denuded SVA (n=7). Potentiation of EFS-mediated relaxations by PDE5 inhibitors tadalafil (C) and sildenafil (D) on intact SVA (n=6). Data is mean ±SEM. *p<0.05, **p<0.01.
References
- Andersson KE, Boedtkjer DB & Forman A. The link between vascular dysfunction, bladder ischemia, and aging bladder dysfunction. Ther Adv Urol. 2017;9(1):11-27.
- Nomiya M, Burmeister DM, Sawada N, et al. Prophylactic effect of tadalafil on bladder function in a rat model of chronic bladder ischemia. J Urol. 2013;189(2):754-61.
CO2 Surgical laser for treatment of stress urinary incontinence in women: A randomised controlled trial
Alexander J1, Karjalainen P1, Ow LL1, Kulkarni M1, Lee J1, Leitch A1, Ryan G1 & Rosamilia A1,3
- Monash Health, Bentleigh East, Victoria, Australia
- University of New South Wates Sydney, Randwick, New South Wales, Australia
- Monash University, Clayton, Victoria, Australia
Introduction: Stress Urinary incontinence (SUI) is a common condition that can be treated conservatively and/or surgically. Given the risks of surgery, there would be benefits for patients in the development of effective non-surgical treatment options. Some studies have suggested laser therapy may improve or cure SUI 1,2 ; however, there is a lack of sham-controlled randomised controlled trials (RCT) to judge treatment efficacy.
The objective of this study was to compare the effects of CO2 vaginal laser versus sham for the treatment of stress urinary incontinence (SUI).
Materials & methods: Study Design was a multi-centre, participant-blinded, sham-controlled parallel group (1:1) superiority RCT. It was performed in outpatient clinics in two hospitals. We included women aged 18 to 80 years with objective and subjective SUI. Participants had undertaken or declined supervised pelvic floor muscle training.
The intervention was performed using a CO2 fractionated vaginal laser. Participants underwent three treatments, four weeks apart, with increasing energy and density settings. Sham was performed using an identical technique with a deactivated pedal.
The primary outcome was the subjective SUI rate (proportion with leak with cough, sneeze, or laughter) at three months after completion of treatment. Secondary outcomes included objective SUI, change in the disease specific patient reported outcomes (PRO), and generic quality of life (HRQOL) as well as adverse effects. Categorical outcomes were compared using the chi-squared test and continuous outcomes using analysis of covariance adjusting for the baseline score. Approval for the trial was obtained from the local human research ethics committee (HREC/16/MonH/387) and registered in The Australian New Zealand Clinical Trials registry (ACTRN12617000099325).
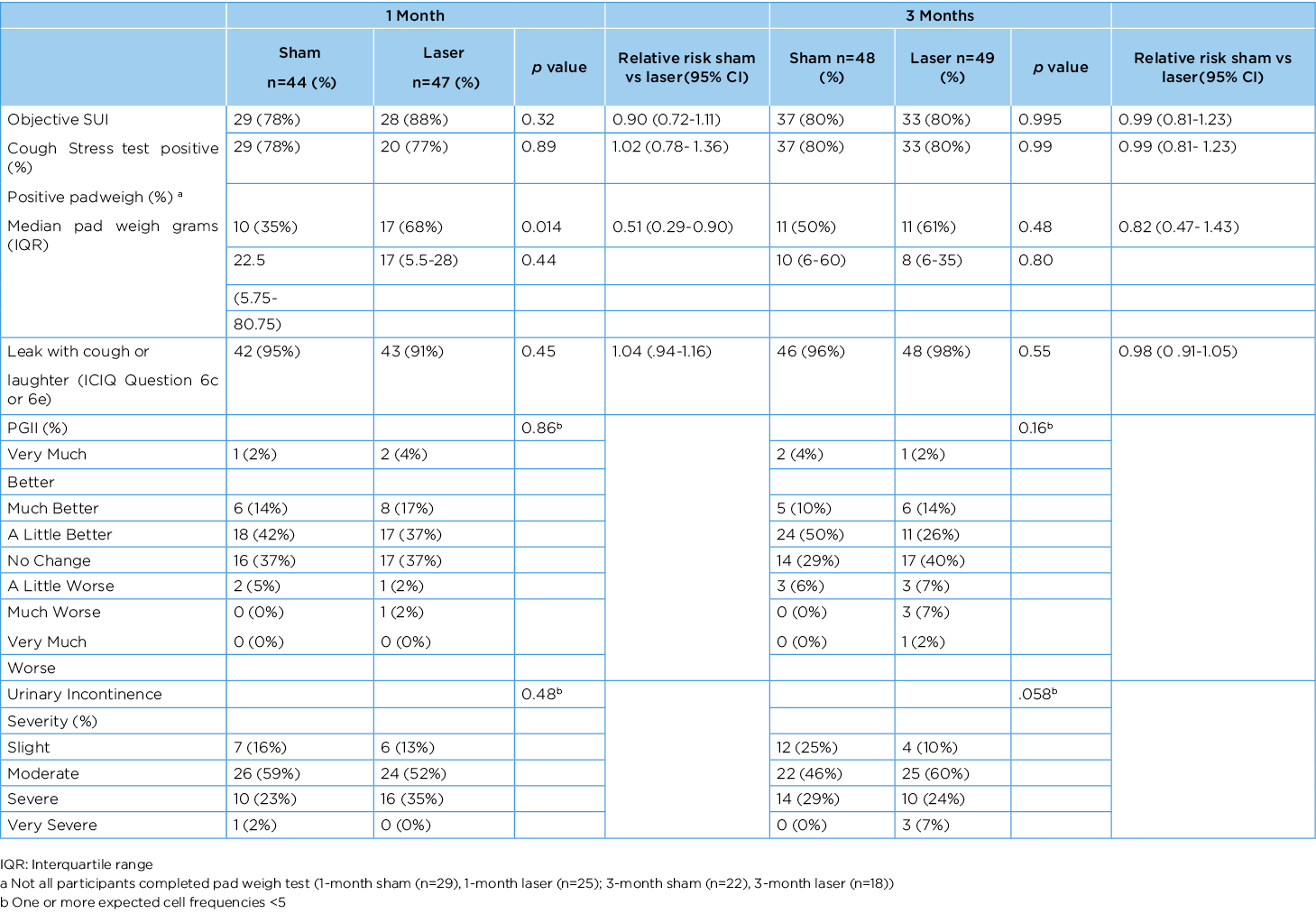
Results: 52 participants received laser and 49 sham treatment. One participant in each group withdrew from the study before the endpoint and two participants in the laser group did not participate in the follow-up visits. Participant mean age was 53 years (34-79), mean body mass index (BMI) was 26.1 (18.1-49.6) and 90% were vaginally parous. At three months, there was no difference between participants in subjective SUI (46 (96%) vs 48 (98%), (RR 0.98 (95% CI, .91-1.05) p=0.55) or objective SUI (37 (80%) vs 33 (80%), (RR 0.99 (95% CI, .81-1.23 p=0.995) (table 1). The PRO and HRQOL were also comparable between the groups. Vaginal bleeding occurred in three participants after laser and one participant after sham. Pain during treatment did not differ between laser and sham.
Conclusion: We were unable to show an improvement in SUI after CO2 vaginal laser therapy compared to sham treatment.
Table 1 Categorical outcomes after CO2 Laser Treatment at 1 and 3 months
References
- Blaganje M, Šc´epanovic´ D, Žgur L, et al. Non-ablative Er:YAG laser therapy effect on stress urinary incontinence related to quality of life and sexual function: A randomized controlled trial. Eur J Obstet Gynecol Reprod Biol. 2018;224:153-158.
- Franic´ D & Fistonic´ I, Laser Therapy in the Treatment of Female Urinary Incontinence and Genitourinary Syndrome of Menopause: An Update. BioMed Research International 2019; Article ID 1576359.
Mini or retropubic sling in women with intrinsic sphincter deficiency at 6 months: an RCT (Mini RISD)
Ow LL1,2, Murray C2, AlexanderJ1,3, J Lee3, Leitch A1, Dwyer P2 & Rosamilia A1
- Monash Health, Moorabbin, Victoria, Australia
- Mercy Hospital for Women, Heidelberg, Victoria, Australia
- University of NSW, Sydney, New South Wales, Australia
Introduction: Intrinsic sphincter deficiency (ISD) is associated with a higher risk of sling failure and is difficult to treat. The retropubic (RP) sling and the ‘mini’ single incision sling (SIS) are two treatment options. Comparison of the efficacy and safety for these procedures in women diagnosed with ISD has not been determined.
The RP sling has been shown to be superior to the obturator sling for the treatment of SUI associated with ISD1 ; however, the RP sling is associated with more complications such as bleeding, bladder injury and voiding difficulty2,3. The ‘mini’ SIS provides a ‘hammock’ support and can be placed under more tension than an obturator sling. It is plausible that the SIS could be as effective as the retropubic sling but associated with fewer complications.
The objective was to assess if the SIS is as efficacious as the RP sling for women with urodynamic stress incontinence (USI) and ISD and to compare clinical outcomes.
Materials & methods: This was a muti-centre randomised controlled trial involving women diagnosed with SUI/ISD. Demographic data of eligible women and Pelvic Organ Prolapse Quantification System (POP–Q) examination was collected. Randomisation to SIS or RP occurred in equal probability. Concomitant prolapse operation was performed as required. Post-operative interview and examination were performed at six weeks and six months. Examination included uroflow, cough stress test and POPQ assessment. Standardised questionnaires were performed at six months.
Primary outcome was to assess the objective cure rate (negative clinical cough stress test) of the SIS against the RP sling at six months post- surgery. Secondary outcomes included immediate and short term post-operative complications and patient reported outcomes.
Categorical Outcomes were compared using the chi-squared test and continuous outcomes using the independent samples t-test for normally distributed data. .
Results: 112 women were randomised and completed six month follow up. Of those 54 women were randomised to SIS and 58 women to RP sling. Results were analysed by an intention to treat (ITT) analysis. No women crossed groups. We did not achieve our sample size of 132 due to a combination of factors including withdrawal of approval of the SIS from the local regulatory body, Covid-19 restrictions on recruitment/surgery and women’s reluctance to have mesh.
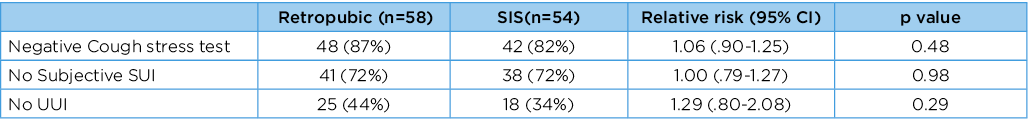
Average age of participants was 66 years and body mass index (BMI) 27kg/m2. Table 1 shows results at six months. There was no difference in post-operative complications between the two groups; however, for one participant the SIS was removed for groin pain. At six months, women who had no symptoms of SUI (72% RP group versus 72% SIS) and who had a negative cough stress test (87% RP versus 82% SIS) were similar, and 78% in the RP group and 76% in the SIS group reported improvement as “very much better or much better” (RR 1.06 (95% CI 0.68-1.66), p=0.79).
Two women had repeat surgery at six months. One in the RP group (1.7%) and one in the SIS group (1.9%). At two years, four women in the RP group (6.9%) had repeat surgery and six women in the SIS group (11.1%).
Conclusion: After six months, we are unable to show a difference in subjective or objective cure between groups. With time, more women had repeat surgery.
Table 1. Categorical Outcomes (chi-squared)
References
- Ford AA & Ogah JA. Retropubic or transobturator mid-urethral slings for intrinsic sphincter deficiency-related stress urinary incontinence in women: a systematic review and meta-analysis. IUJ. 2017;27(1):19-28.
- Novara G, Artibani W, Barber MD, et al. Updated systematic review and meta-analysis of the comparative data on colposuspensions, pubovaginal slings, and midurethral tapes in the surgical treatment of female stress urinary incontinence. Eur Urol. 2010;58(2):218-38.
- Ford AA, Rogerson L, Cody JD, Ogah J. Mid-urethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev. 2015;(7):CD006375.
Resident expectations and preferences for continence care in Australian residential aged care homes
Ostaszkiewicz J, Cecil J, Kosowicz L, Garratt S, Wise E & Dow B
National Ageing Research Institute, Parkville, Victoria, Australia
Introduction: Prior research suggests incontinence has negative effects on the quality of life of older people living in residential aged care homes 1. Urinary incontinence increases an older person’s risk of falling 2 and developing incontinence-associated dermatitis 3. Despite these impacts, there is limited evidence about the lived experience of people with continence care needs in Australian residential aged care homes.
The aim of this project was to explore aged care residents’ expectations and preferences for continence care in Australian residential aged care homes.
Materials & methods: 13 older people, purposively recruited from two regional and one metropolitan residential aged care home in Victoria, were interviewed using an unstructured open-ended approach. Interview recordings were thematically analysed by two independent researchers. A deductive coding framework was used to make cross comparisons with the propositional concepts in a draft best practice model of continence care. The study was approved by Austin Health Human Ethics Committee (HREC/63029/Austin-2020). The project was carried out according to the National Statement on Ethical Conduct in Human Research4.
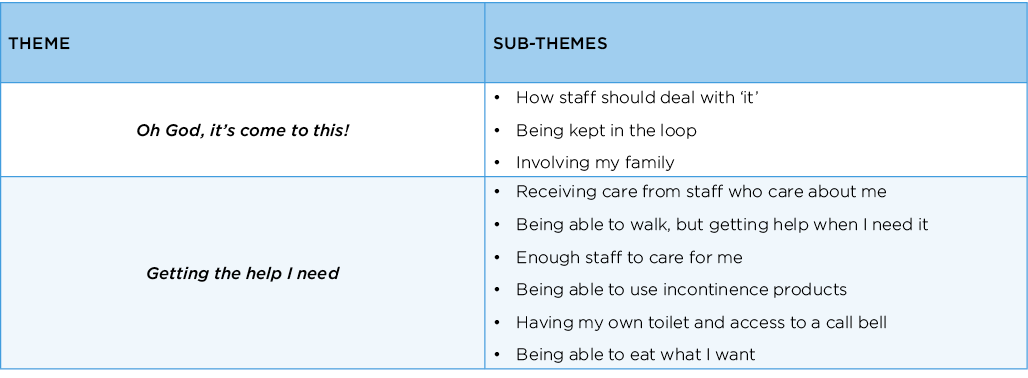
Results: Two core themes emerged: (i) ‘Oh God, it’s come to this’ and (ii) Getting the help I need. (See Box 1). “Oh God, it’s come to this” expresses the sense of dismay some residents felt from the experience of incontinence and their reliance on staff for help. Residents indicated they wanted to be ‘kept-in-the-loop’ about decisions regarding their continence care. Some expressed gratitude that their families were aware of their needs and advocated for them.
All residents emphasised the importance of receiving timely and responsive assistance to maintain optimal bladder and/or bowel control. A key concern was a perceived lack of staff to meet their individual needs, particularly during the night. Residents were not confident that staff could respond promptly to their requests for assistance, and this caused both anxiety and distress. Inadequate staffing was considered to be a major obstacle to receiving prompt practical assistance. Residents also indicated they wanted care from staff who were kind and responsive, who knew them as an individual and understood their needs. They also emphasised the importance of incontinence products, a call bell, a private bathroom, food and fluid of their own choosing, and the ability to walk independently or with a mobility aid.
Conclusion: The findings validate several witness statements submitted to the Australian Royal Commission into Aged Care Quality and Safety in relation to continence management in some residential aged care homes. This evidence was used to design a new approach to continence care that could align with broader consumer and community expectations and preferences.
Box 1
References
- Xu D & Kane RL. Effect of urinary incontinence on older nursing home residents’ self-reported quality of life. J Am Geriatr Soc. 2013;61(9):1473-81.
- Damian J, Pastor-Barriuso R, Valderrama-Gama E, et al. Factors associated with falls among older adults living in institutions. BMC Geriatr. 2013;13:Article 6.
- VanDamme N, Van den Bussche K, De Meyer D, et al. Independent risk factors for the development of skin erosion due to incontinence (incontinence-associated dermatitis category 2) in nursing home residents: results from a multivariate binary regression analysis. Int Wound J. 2017; 14(5):801–810
- National Health and Medical Research Council. The National Statement on Ethical Conduct in Human Research.; 2007 [cited 2022 March 20] Available from: http://www.nhmrc.gov.au/_files_nhmrc/publications/attachments/e72.pdf.
Staff and carer perspectives of quality continence care in Australian residential aged care homes
Ostaszkiewicz J, Cecil J, Kosowicz L, Garratt S, Wise E & Dow B
National Ageing Research Institute, Parkville, Victoria, Australia
Introduction: Quality care can only meet the needs of a population if that care is consistent with consumers’ values and preferences. Moreover, approaches to consumer involvement in research and health policy vary and consumer involvement has not been widespread. Few studies have sought to elicit the views of residential aged care consumers about what constitutes quality continence care.
The aim of this project was to consult with residential aged care consumers to establish their expectations and preferences about continence care.
Materials & methods: A mixed methods approach was used to consult with two consumer groups: (i) informal carers/family members of residents (current or past) and (ii) residential aged care staff members with expertise in managing or supervising continence care. They were consulted via: (i) an anonymous Australian-wide online survey, (ii) qualitative interviews and (iii) co-design workshops.
The online survey invited participants to rank several factors in terms of their importance to continence care in residential aged care homes. These factors included personal factors, staff qualities, information for residents and families, information for staff and resources. Descriptive statistics were used for demographic and ranked preferences. Likert-scale results were expressed as diverging stacked bar graphs. Statistically significant differences (p<0.05) between Likert-scale data subsets were determined by a Kruskal-Wallis H test.
At the completion of the survey, participants were invited to participate in an in-depth qualitative interview and/or co-design workshop. Participants were invited to describe their expectations about quality continence care in Australian residential aged care homes.
Two researchers independently used an inductive thematic analysis approach to analyse the qualitative data. The study was approved by Austin Health Human Ethics Committee (HREC/63029/Austin-2020). The project was carried out according to the National Statement on Ethical Conduct in Human Research1.
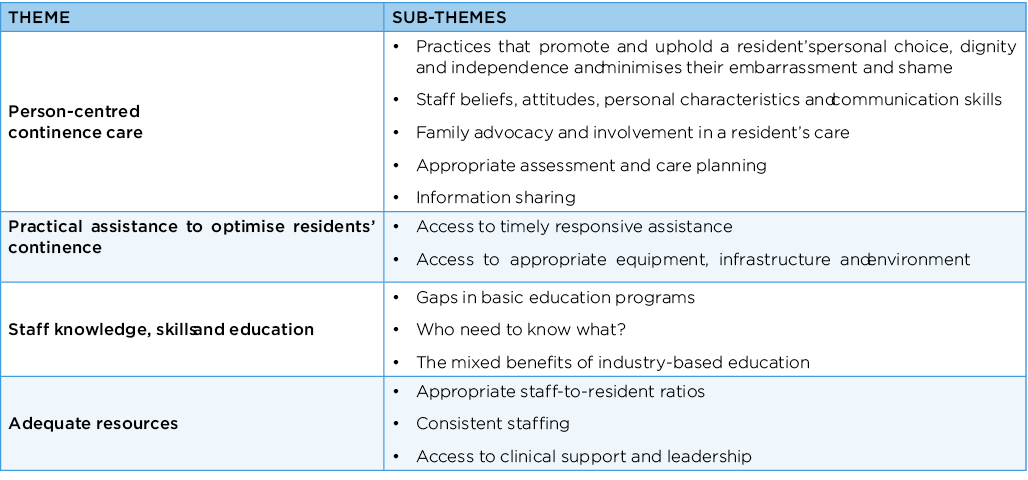
Results: The quantitative Likert-scale responses revealed that all factors were equally ‘very important’ to participants. Qualitative findings revealed (i) a person-centred approach to continence care was important, as was (ii) practical assistance to optimise residents’ continence; (iii) care from staff who were knowledgeable, skilled and educated; and (iv) access to adequate resources. These four themes and their sub-themes are further described in Box 1.
Conclusion: This project established an evidence-base about the expectations and preferences of family carers and residential aged care staff regarding quality continence care in Australian residential aged care homes. This evidence was used to design a best practice model of continence care for Australia’s residential aged care sector. The model contributes to broader efforts to improve the quality of continence care in Australia’s residential aged care homes.
References
- National Health and Medical Research Council. The National Statement on Ethical Conduct in Human Research.; 2007 [cited 2022 March 20] Available from: http://www.nhmrc.gov.au/_files_nhmrc/publications/attachments/e72.pdf.