Volume 29 Number 2
Abstracts – Podium Presentations Joint 31st National Conference on Incontinence (NCOI) and the 4th Functional Urology Symposium (FUS) (NCOIFUS23) 14-17 June 2023 Adelaide Convention Centre, Adelaide SA
Licensed under CC BY 4.0
DOI https://doi.org/10.33235/anzcj.29.2.22-47
Experience of Playing Sport/Exercising for Women with Pelvic Floor Symptoms: A Qualitative Study
Dakic J1,2, Hay-Smith J 3, Kuan-Yin L4, Cook J 5, Frawley H2,6,7
1Monash University,Melbourne
2The University of Melbourne, Melbourne
3University of Otago, Wellington
4National Cheng Kung University, Taiwan
5La Trobe University, Melbourne
6The Royal Women’s Hospital, Parkville, Victoria
7Mercy Hospital for Women, Heidelberg, Victoria
Introduction & Objectives: Compared with men, women participate in organised sport at a lower rate, and encounter unique barriers to participation.1 One in three women across all sports experience pelvic floor (PF) symptoms such as urinary incontinence during training/competition.2 Despite this, there is sparse qualitative research on the experience of women who play sport/exercise with PF symptoms. Through in-depth semi-structured interviews, we explored the experiences of symptomatic women within sports/exercise settings and the impact of PF symptoms on sports/exercise participation.
Methods: A qualitative descriptive design was used. Random women from an existing database were invited to participate in a semi-structured interview via online platform (Zoom). Interviews were audio recorded and transcribed verbatim. Data were analysed using inductive qualitative content analysis, managed via NVivo software. Patterns of women’s experiences within the data were identified, leading to development of a coding scheme that was then applied to all data. Codes were merged or linked to form themes representing the latent meaning of the content and agreed on in discussion by the research team. Quotations were selected to illustrate themes. Information power guided the decision to cease recruitment. Included participants (n=23) were 18-65-year-old women (average age 46.2 years), residing in Australia who had experienced a breadth of PF symptoms (96% urinary incontinence, 35% pelvic organ prolapse and 48% anal incontinence) whilst exercising (in the past or currently). Women needed a conversational level of English to participate.
Results: Participants played a variety of sports and levels of participation (78% recreational). We identified four main themes: (i) I can’t exercise the way I would like to, (ii) it affects my emotional and social well-being, (iii) where I exercise affects my experience and (iv) there is so much planning to be able to exercise. Women reported wide-ranging impact on their ability to participate in their preferred type, intensity and frequency of exercise. Women perceived judgement from others, anger, fear of symptoms becoming known and isolation from teams/group exercise settings as a consequence of symptoms. Meticulous and restrictive coping strategies were needed to limit symptom provocation during exercise, including limiting fluid intake and careful consideration of clothing/containment options (Table 1). The culture of the sporting environment influenced whether women continued or ceased exercising - positive role models (other members or support staff), education and re-design of uniform to allow covert containment of leakage were strategies identified to promote a positive culture.
Table 1: Coping strategies for exercising with pelvic floor symptoms
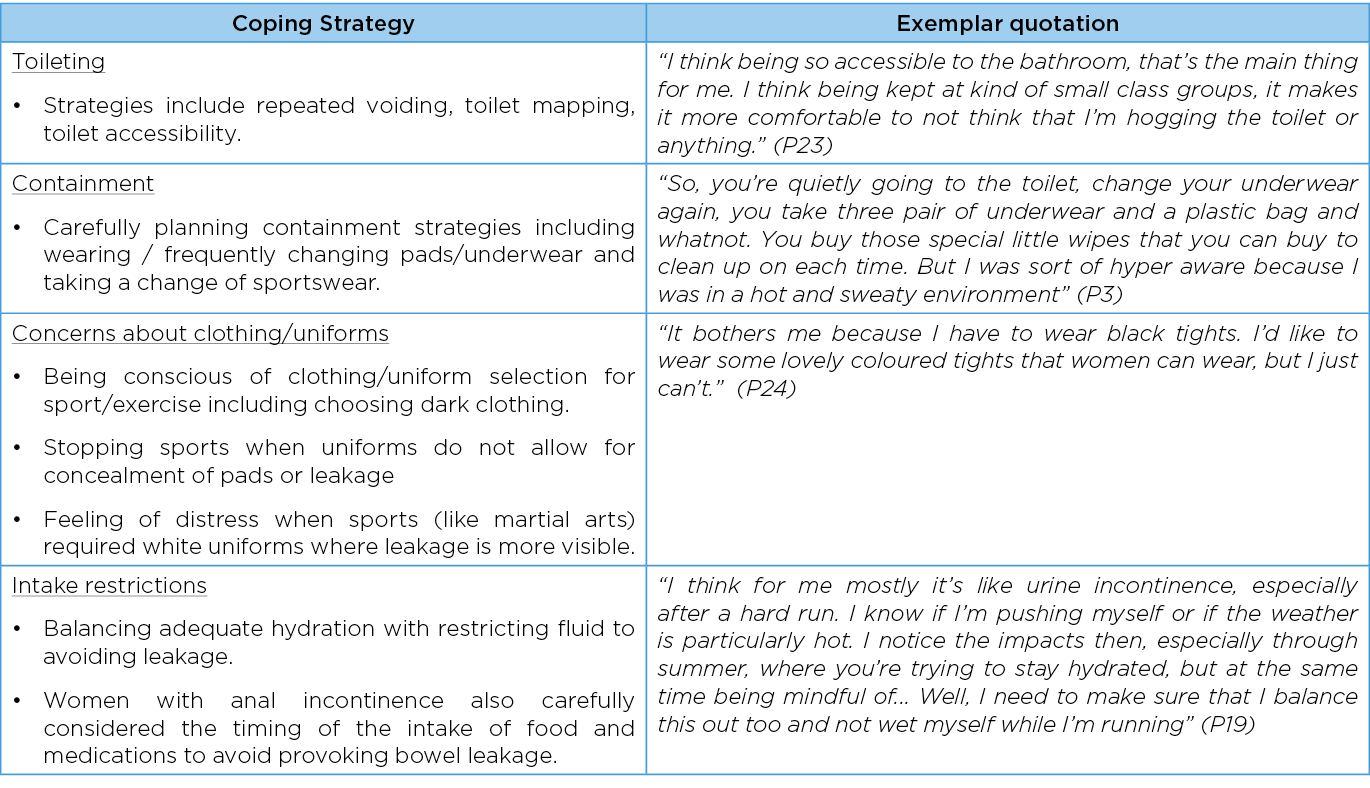
Conclusions: Experiencing PF symptoms during sport/exercise caused considerable limitation to participation. Generation of negative emotions and painstaking coping strategies to avoid symptoms, limited the social and mental health benefits typically associated with sport/exercise in symptomatic women. In order to promote women’s participation in sport, co-designed strategies for (i) screening and management of PF symptoms and (ii) promotion of a supportive and inclusive culture within sports/exercise settings are needed.
Disclosures
Ethics approval number: Ref - 2021-22466-21024-3, 24th August 2021
Conflict of Interest
We have no actual or potential declarations to make.
Funding
This research was supported by funding from the Australian Bladder Foundation Grant managed by the Continence Foundation of Australia.
References
- Women in Sport., 2022, Available from: https://www.clearinghouseforsport.gov.au/kb/women-in-sport
- Teixeira et al., 2018, Int Urogynecol J, 29(12):1717-25.
Early Experience of Transabdominal and Novel Transvaginal Robot-Assisted Laparoscopic Removal of Transvaginal Mesh
Harley F1,3, Fong E2, Yao H1,3,4, O’Connell H3,4,
1Eastern Health, Box Hill, Victoria
2Urology Institute, Auckland
3University of Melbourne, Melbourne
4Monash University, Melbourne
Introduction & Objectives Pelvic mesh removal after transvaginal mesh placement has until recently been a technically difficult procedure with varying results. It typically involved transvaginal, open pelvic, laparoscopic, or a combination of approaches. It has become a necessary procedure of recent times due to the now recognized complications. Rates of refractory pain for Mid Urethral Slings Systems (MUSS) are reported at 2% for retropubic and 5.3% for transobturator1, and the rates of erosion are 2.3% and 2.7%, respectively1. Despite the relatively low rates of significant complications1, mesh necessitating removal is still a significant issue due to the large number of devices placed. It is estimated that in 2009, 89.1% of SUI procedures were MUSS2. Until recently robotic assisted pelvic mesh removal has been described in only a small number of cases. This study aims at determining the feasibility and safety of using robot-assisted laparoscopic surgery in the removal of pelvic mesh via the transabdominal and novel transvaginal approach.
Methods A prospective multi-site case series study was performed on women who underwent transabdominal or transvaginal robot-assisted removal of pelvic mesh. Women were offered participation in this study with pelvic mesh and a clinical indication for mesh removal if they were older than the age of 18. Alternative surgical options, including conventional open removal of mesh, were discussed, and offered to patients. The primary outcome of this study is the rate of successful removal of mesh and the 30-day complication rates. Ethics approval was obtained for this study and was registered with the Australia and New Zealand clinical trials registry.
Results Thirty patients were involved in this study. Median age was 62. Median operative and console time was 240 and 148 minutes, respectively. Concomitant reconstructive procedures were performed in 40% of patients. Complete or near-complete mesh removal was achieved in 83.3% of patients. For the remaining patients, partial removal of mesh was performed as per pre- preoperative counselling. Three Clavien-Dindo grade 3b complications resulted from mesh removal: concomitant ureteric and bladder injury, omental bleed, and groin wound infection.
Conclusions This small case series presents the early experience of robotic-assisted removal of transvaginal mesh with a transvaginal or transabdominal approach and demonstrates the feasibility with removal of both retropubic and transobturator mid-urethral synthetic sling as well as transvaginal prolapse meshes with transobturator and sacrospinous mesh arms. Further studies are required to expand understanding on the learning curve, operating times, complication rates, and functional outcome of this operation.
References
- Blaivas JG, Purohit RS, Benedon MS, et al. Safety considerations for synthetic sling surgery. Nat Rev Urol. 2015 Sep;12(9):481-509. PubMed PMID: 26282209. Epub 2015/08/19.
- Jonsson Funk M, Levin PJ, Wu JM. Trends in the surgical management of stress urinary incontinence. Obstet Gynecol. 2012 Apr;119(4):845-51. PubMed PMID: 22433349. Pubmed Central PMCID: PMC3310349. Epub 2012/03/22.
How to prevent urinary tract infections: what is online video content teaching our patients?
Zhuo, KY1,2,3,4,5, Alvarado, M2,3, Nassour A2,3, Chung, A1,2,3,4,5
1Royal North Shore Hospital, St Leonards, NSW
2North Shore Urology Research Group, St Leonards, NSW
3Northern Beaches Hospital, Frenchs Forest, NSW
4Macquarie Hospital, Macquarie Park, NSW
5North Shore Private Hospital, St Leonards, NSW
Disclosures:
Ethics: Not required
Project funding: Nil funding
Conflicts of interest: One of the authors is a proctor for Medtronic (sacral neuromodulation) and Boston Scientific (artificial urinary sphincter, penile prosthesis).
The other authors do not have any conflicts of interest to declare.
Introduction: Urinary tract infections (UTIs), are a leading cause of health related morbidity in the community. As a result, many patients will often seek unverified sources of information for methods to prevent urinary tract infections. This study aims to assess the quality of health education for the prevention of urinary tract infections on the global online video sharing platform, YouTube.
Materials and Methods: Three medical practitioners independently reviewed and evaluated the first 50 videos listed in February 2023, when using the search terms “How to prevent UTIs” on YouTube, the online video sharing platform.
Information regarding the number of video views, creator, as well as video content quality, understandability and actionability were recorded. Each video was assessed according to the DISCERN criteria and Patient Education Materials Assessment Tool (PEMAT)1,2. The DISCERN criteria are a commonly used method of assessing the reliability and quality of information provided by audio-visual content related to consumer health information, whilst the PEMAT is a tool developed to assess both the understandability and actionability of audio-visual content. Statistical analysis was performed using IBM SPSS Statistics V28. P-values <0.05 were considered statistically significant.
Results: Forty-Seven videos were analysed (3 non-English videos excluded). Only 16/47 (34%)of the videos were produced by a recognised medical institution. 43/47 (91%) of videos were addressed at patients, whilst 4/47 (9%) were targeted at clinicians. The median number of views per video was 24,110 (range: 88–5552204).
The overall quality of evidence-based material regarding UTI prevention was poor to moderate, manifested by a mean (range) DISCERN criteria score of 3.1 (1–5). Despite the average PEMAT understandability score being 63% (range: 22–100%), there was limited actionability of content reflected by a mean PEMAT score of 68% (range: 0–100%). Content produced by recognised medical institutions was not associated with higher PEMAT (understandability/actionability: p=0.36/p=0.20) scores but was found to have higher DISCERN criteria (p=0.03) scores. The number of video views was not associated with higher PEMAT (understandability/actionability: p=0.55/p=0.57) or DISCERN criteria (p=0.34) scores.
Conclusion: YouTube is one of the most accessible mediums for health education. Video information from medical institutions were more factual than that of non-medical institutions and media influencers. However, there was no difference in the quality of delivery between medical and non-medical institutions that may not always convey evidence-based information. Medical practitioners must be aware that patients may present with inaccurate preconceptions regarding prevention methods for their urinary tract infections and should be prepared to address these during counselling with patients.
References
- Charnock D, et al., DISCERN: an instrument for judging the quality of written consumer health information on treatment choices., 1999, J Epidemiol Community Health, 53(2),105-11.
- Agency for Healthcare Research and Quality, PEMAT Tool for Audiovisual Materials (PEMAT- A/V), 2013, Webpage, Available from: https://www.ahrq.gov/health-literacy/patient-education/pemat- av.html.
Evaluating the content validity of the 3PSQ in People with Persistent Pelvic Pain: A mixed method cross-sectional study.
Thompson J1, Hart S, Anderson T, Ruland A, Melville C, D’Arcy M, Pontifex A, Savin C, Tinetti A, Chalmers KJ
1Body Logic – Pelvic Health Clinic, Perth
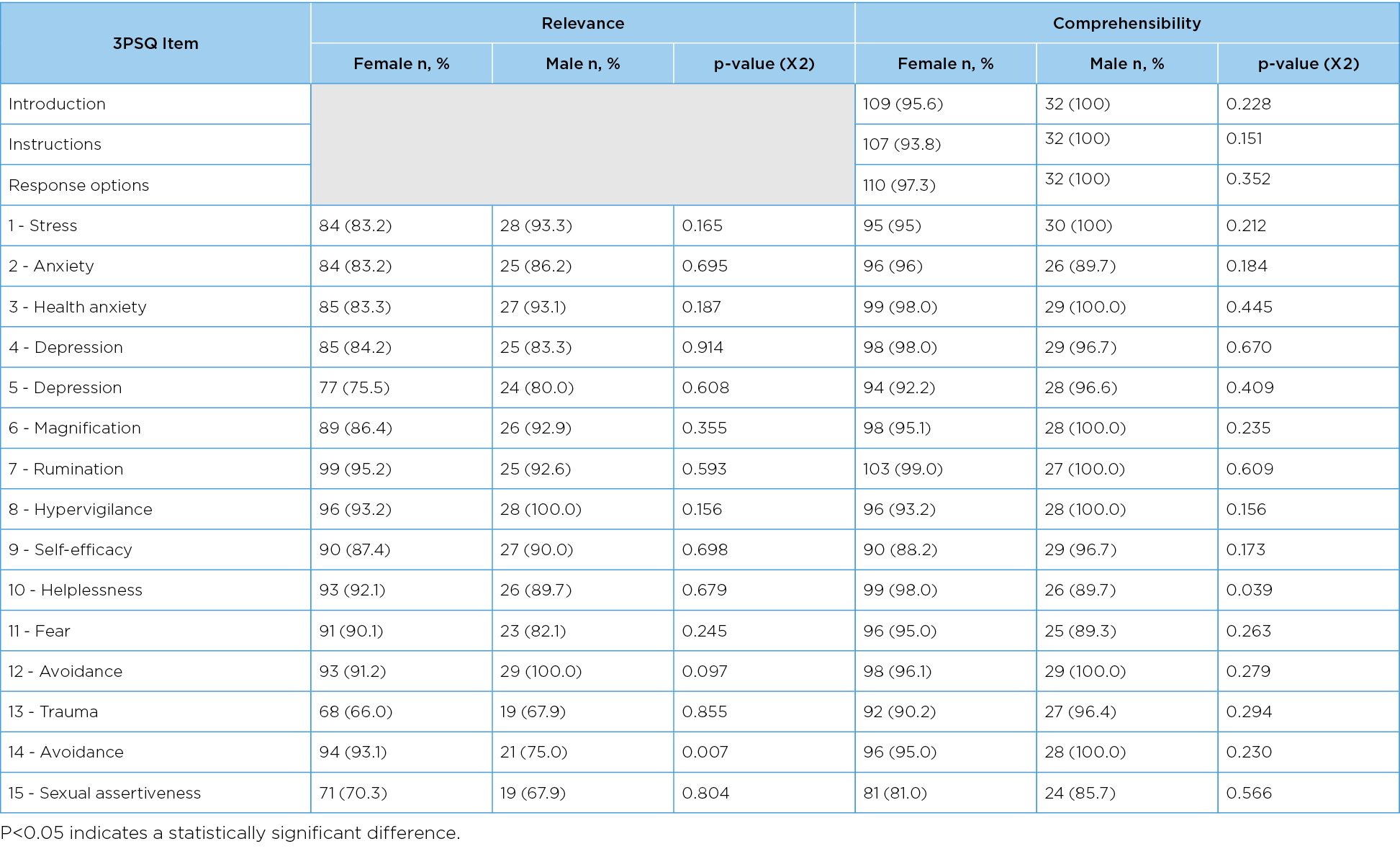
Introduction & Objectives: Early identification of psychological factors in people with persistent pelvic pain (PPP) is recommended by the European Association of Urology (EAU)1. The psychometric properties of the newly developed Pelvic Pain Psychological Screening Questionnaire (3PSQ) need to be established.
The aim of this study was to evaluate the content validity (relevance, comprehensibility and comprehensiveness) of the 3PSQ.
Methods: Participants with PPP completed the 3PSQ via an online survey and answered questions regarding the relevance and comprehensibility of each item, and the comprehensiveness of the overall questionnaire. Participants were recruited via social media platforms, health professional networks and word of mouth. Inclusion criteria: over 18 years of age, current pelvic pain lasting six months or longer with or without a diagnosis of pelvic pain. Exclusion criteria: currently pregnant, pregnancy or pelvic surgery in the previous six months. Quantitative data regarding dichotomous content validity answers and demographics were analysed using descriptive statistics. Qualitative data regarding the relevance, comprehensibility and comprehensiveness of the 3PSQ were analysed using content analysis. An expert panel reviewed the results prior to recommending changes to the 3PSQ.
Results: A total of 146 people (114 female and 32 male) with PPP participated. All males and at least 93.8% of females agreed the introduction, instructions and response options were comprehensible. More than 80% of participants agreed 12 out of 15 items of the 3PSQ were relevant. Comprehensiveness of the 3PSQ yielded an agreement percentage of 42% for females and 31.3% for males. The lower agreement for comprehensiveness may have been because many participants misinterpreted the purpose of the 3PSQ. Analysis of the qualitative data revealed many participants suggested comprehensiveness could be improved by capturing the impact of their pain on other aspects of their life such as work and relationships or not feeling heard by medical professionals. These other life impacts are outside the scope of the 3PSQ. Only one psychological construct (suicidal ideation) was identified as missing. Based on expert panel review of the quantitative and qualitative data, wording changes to the 3PSQ were implemented to make the questions clearer. The panel concluded suicidal ideation was an inappropriate construct to include in a self-reported questionnaire, and would be better asked in a sensitive, in-person manner.
Clinically, the 3PSQ would not be administered in isolation; rather in conjunction with an extensive subjective history and the use of other PROMs that capture the symptoms and impacts of PPP such as the Australian Pelvic Floor Questionnaire2 or Pelvic Pain Impact Questionnaire3.
Conclusion: The 3PSQ has been validated by people with PPP as being relevant, easily understood and including all psychological factors pertinent to this population. This study has demonstrated a high agreement score for relevance, comprehensibility and a moderate score for comprehensiveness. The 3PSQ will provide health professionals with a one-page questionnaire that screens for a comprehensive set of psychological factors relevant to PPP, aligning with the EAU guidelines.
Disclosure
Ethics approval number HRE2022-0374.
This project had no funding to declare.
Conflict of interest: I have no actual or potential declarations to make.
Table 1. Quantitative Relevance and Comprehensibility Data
References
- Engeler DB, A.P.; Berghmans, B; Birch, J; Borovicka, J; Cottrell, A.M.; Dinis-Oliveira, P; Elneil, S; Hughes, J; Messelink, E.J.; Pinto, R.A.; van Poelgeest, M.L.; Tidman, V; de C Williams, A.C. . EAU Guidelines on Chronic Pelvic Pain. EAU Guidelines Office; 2022.
- Baessler K, O’Neill SM, Maher CF, Battistutta D. Australian pelvic floor questionnaire: a validated interviewer-administered pelvic floor questionnaire for routine clinic and research. International Urogynecology Journal. 2009;20(2):149-158.
- Chalmers KJ, Catley MJ, Evans SF, Moseley GL. Clinical assessment of the impact of pelvic pain on women. Pain. 2017;158(3):498-504.
Australian health care practitioners providing pessaries for women with pelvic organ prolapse: a survey of practice
Neumann P1,2, McEvoy K 1, Wright O1, Griffin R1, Moger H1, McGinnity K1, Sciacca R1, Thompson J1, Das R 1,2, Nurkic I1
1Curtin University, Perth
2University of South Australia, Adelaide
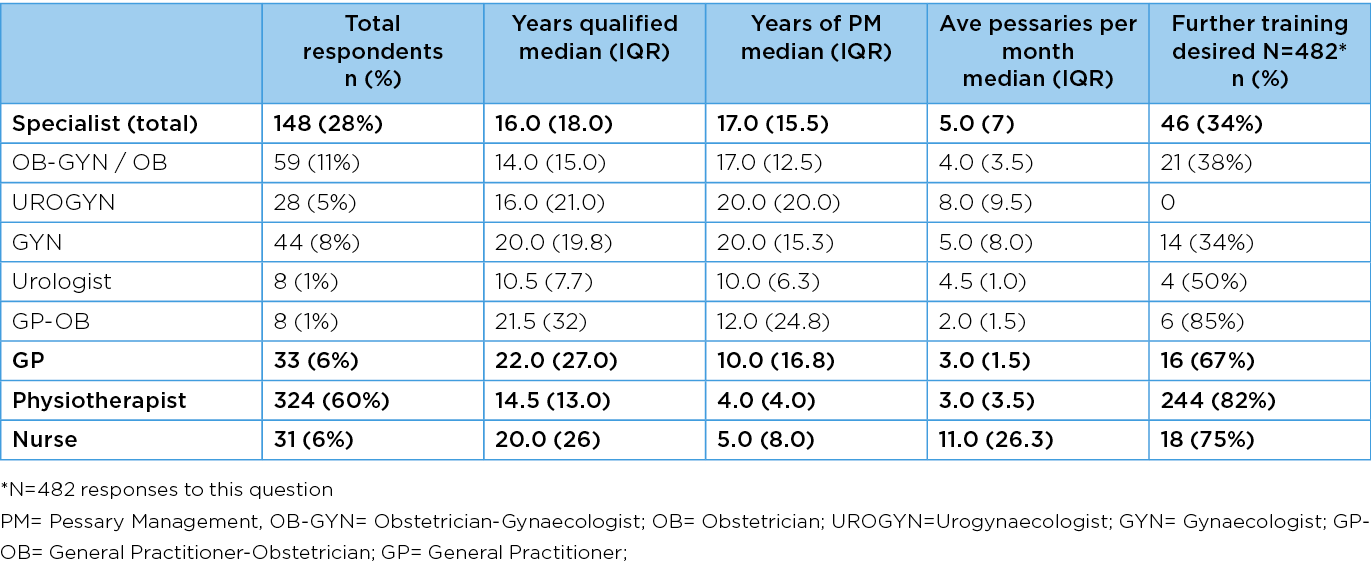
Introduction & Objectives Vaginal pessaries are an effective treatment for pelvic organ prolapse (POP) and an alternative to surgery1. Traditionally, pessary management (PM) has been provided by medical professionals, particularly gynaecologists, and nurses, but recent international studies have identified physiotherapists as providers of pessary care2. It is unknown which health care practitioners (HCPs) provide PM for POP in Australia or the distribution of services. We aimed to describe professional characteristics of HCPs providing PM services in Australia and where those services are being delivered.
Methods Using a cross-sectional study design, a self-reported electronic survey was developed using the Qualtrics XM (Provo, UT) platform, and distributed to Australian HCPs providing PM for POP, between 26 June and 31 August 2022, with reminder emails sent 14 days after the initial distribution.
Ethical approval was obtained from (Curtin University HREC). Target respondents were medical specialists (urogynaecologists, obstetrician-gynaecologists, gynaecologists, general practitioner-obstetricians, urologists), general practitioners, nurses and physiotherapists who manage pessaries. Recruitment included purposive and snowball sampling, targeting known HCPs and health care facilities providing PM for prolapse and via professional organisations.
Data were exported to Excel in csv format for cleaning before importation into Jamovi 2.3 for statistical analysis. Missing data were accounted for and results from partially completed surveys were included. Calculations relating to percentages were adjusted to reflect the individual question response rate.
Responses were analysed using descriptive statistics and key variables were reported using frequencies (numbers and percentages), including HCP professional profile, geographical location of PM services, clinical settings, aspects of PM and training
Results Of the 536 respondents, there were 324 (60%) physiotherapists, 148 (28%) specialists, 33 (6%) General Practitioners and 31 (6%) nurses. Most (n=332, 64%) worked within metropolitan regions, 140 (27%) in rural, 108 (21%) in regional and 10 (2%) in remote areas. Most (n=418, 85%) worked privately, 153 (46%) worked publicly, and 85 (17%) in both. Ring pessaries were most commonly used, followed by cube and Gellhorn. HCPs reported variable training in PM, including 11 (2%) with no training and most (336, 69%) reported workplaces with no mandatory competency standard. 324 (67%) wanted further training. Women in rural and remote areas travelled long distances to access services.
Conclusions Doctors, nurses and physiotherapists provided PM in Australia, predominantly (91%) in metropolitan and regional centres. HCPs had variable training and experience in PM, with rural and remote HCPs particularly wanting further training. This study highlights the need for accessible PM services, standardised and competency-based training for HCPs, and governance structures to support safe care.
Disclosures
Ethics approval number: Curtin University HREC number HRE2022-0325.
Project Funding: Curtin University contributed $100 towards promoting our study within the Australian Physiotherapy Association. This did not affect the survey’s design, execution or analysis.
COI: The authors have no actual or potential declarations to make.
References
- Bugge C, Adams EJ, Gopinath D, Stewart F, Dembinsky M, Sobiesuo P, Kearney R (2020) Pessaries (mechanical devices) for managing pelvic organ prolapse in women. Cochrane Database Syst Rev (11).
- Brown CA, Pradhan A, Pandeva I (2021) Current trends in pessary management of vaginal prolapse: a multidisciplinary survey of UK practice. Int Urogynecol J 32 (4):1015-1022.
Table 1 Demographics of HCP respondents by professional group (N= 536)
The feasibility of pelvic floor muscle training delivered via telehealth to treat urinary and/or faecal incontinence after gynaecological cancer surgery: a single cohort feasibility study
Brennen R1, Soh S2, Denehy L1,3, Lin K4, Frawley H1,5,6
1University of Melbourne, Melbourne
2Monash University, Melbourne
3Peter McCallum Cancer Centre, Melbourne
4National Chen Kun University, Taiwan
5Royal Woman’s Hospital, Melbourne
6Mercy Hospital for Women, Melbourne
Introduction and objectives: Treatment for gynaecological cancer may impact pelvic floor function, with studies finding high rates of urinary incontinence (UI), faecal incontinence (FI) and pelvic floor muscle dysfunction after treatment. However, few studies of pelvic floor muscle training (PFMT) for UI or FI have been conducted and no studies to date have investigated PFMT delivered via telehealth without any in-person assessments to manage UI and/or FI in this population. Therefore, our study aimed to assess the feasibility of recruiting to and delivering such an intervention, and clinical outcomes before and after the intervention.
Methods: In this pre-post single cohort clinical trial, women who had UI or FI after surgery for gynaecological cancer underwent a 12-week physiotherapist-supervised PFMT program delivered via telehealth and supplemented with an intra-vaginal pressure biofeedback device. The intervention involved seven videoconference sessions, with real-time feedback from the biofeedback device, and a daily home exercise program supported by an associated application which participants downloaded to their mobile device. Feasibility outcomes were the proportion of eligible patients recruited to the study, attendance at the videoconference sessions, and adherence to the home exercise program. Participant satisfaction and acceptability was rated on a 7-point numerical rating scale (from 1 = very dissatisfied/very unacceptable to 7 = very satisfied/very acceptable).
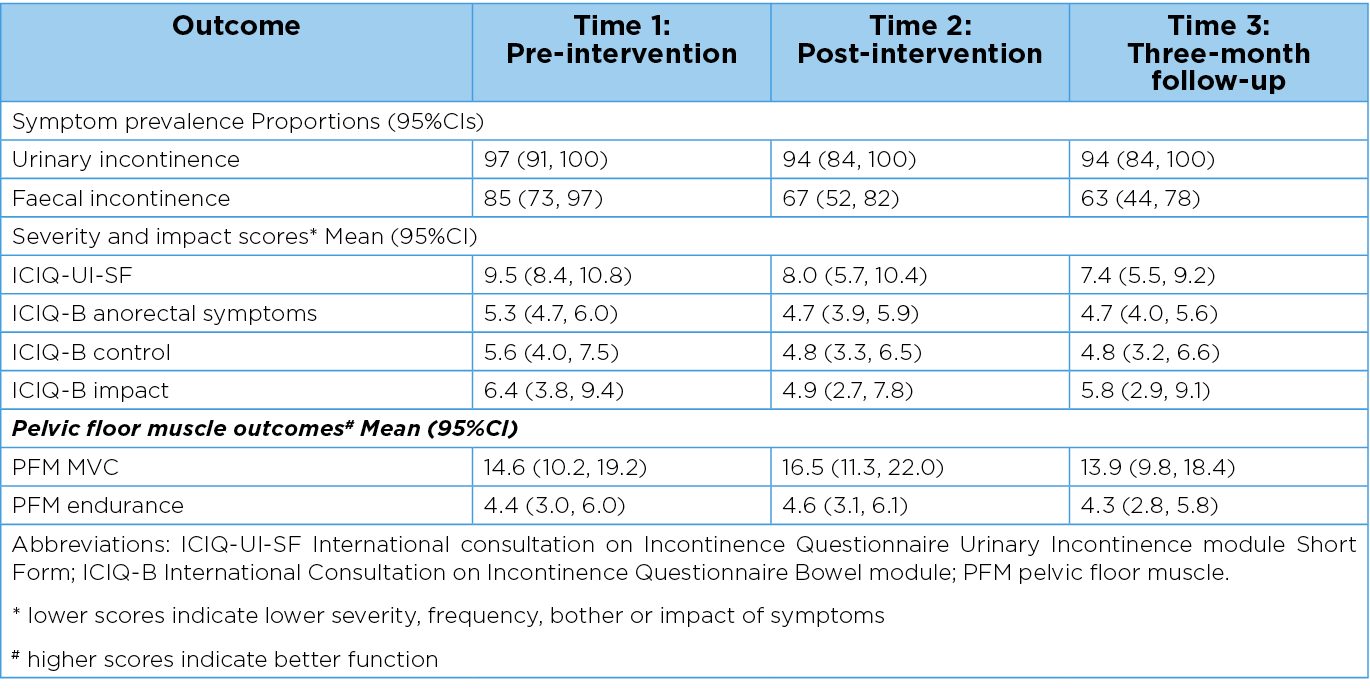
Clinical outcomes were assessed at baseline, immediately post intervention and at three-months follow-up using the International Consultation on Incontinence UI module Short Form (ICIQ-UI SF), the International Consultation on Incontinence Bowel module (ICIQ-B) and the intravaginal biofeedback device. Means and 95% confidence intervals for all time points were analysed using bootstrapping methods.
Results
Feasibility outcomes
A total of 63 women were eligible, of which 39 (62%) consented to the study. Baseline outcome measures were not completed by three participants who were not enrolled in the trial. Of the 36 participants who enrolled in the trial, 32 (89%) received the intervention. The majority (n=30, 94%) demonstrated high engagement, attending at least six of the seven videoconference sessions. Adherence was moderate, with 24 participants (75%) completing five-to-seven PFMT sessions per week during the 12-week intervention period. At the three-month follow-up, 25 (78%) participants reported doing regular PFMT, with 16 (50%) reporting a frequency of at least three PFMT sessions a week. Most participants (n=24, 77%) rated the videoconference sessions as very acceptable and 14 (44%) rated the intravaginal sensor as very acceptable.
Clinical outcomes
All clinical outcome measures improved immediately post-intervention (Table 1), however the magnitudes of these improvements were small. At three-months follow-up, improvements were sustained for prevalence, ICIQ-UI SF and ICIQ-B domains but not PFM outcomes.
Conclusions: This study showed that PFMT delivered via telehealth may be feasible and acceptable to treat UI and/or FI after gynaecological cancer treatment. The study was not powered for the clinical outcome measures and did not have a control group, therefore large randomised controlled trials would be needed to investigate clinical effectiveness.
Funding: This study was supported by a Physiotherapy Research Foundation Seeding Grant. The principal investigator is supported by an Australian Government Research Training Program Scholarship.
Table 1: Clinical outcomes
The natural history of pelvic floor disorders before and after hysterectomy for gynaecological cancer
Brennen R1, Lin K2, Denhy L1,3, Soh S4, Frawley H1,5,6
1University of Melbourne, Melbourne
2National Cheng Kun University, Taiwan
3Peter McCallun Cancer Centre, Melbourne
4Monash University, Melbourne
5Mercy Hospital for Women, Melbourne
6Royal Women’s Hospital, Melbourne
Introduction and objectives: Treatments for gynaecological cancer may contribute to symptoms of pelvic floor disorders including urinary incontinence, faecal incontinence and dyspareunia. These disorders are associated with lower physical activity (PA) levels and health-related quality-of-life (HRQoL) in the general population. There are currently no prospective studies assessing the prevalence and severity of pelvic floor disorders, PA and HRQoL prior to and following hysterectomy for gynaecological cancer. The aim of this study was to investigate the prevalence and severity of pelvic floor disorders, levels of PA and HRQoL in females before and after hysterectomy for gynaecological cancer.
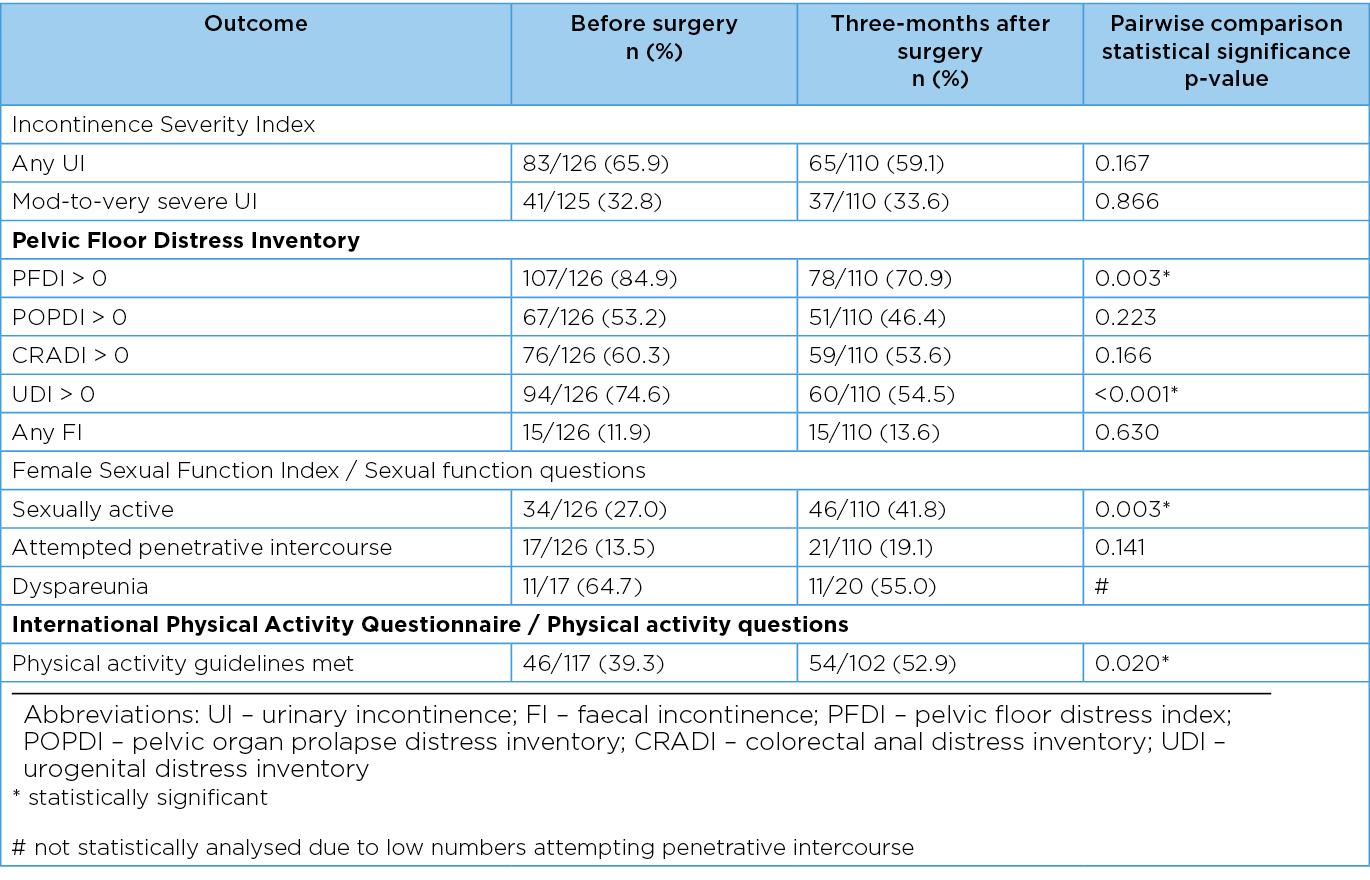
Methods: This longitudinal study included adult females undergoing hysterectomy for endometrial, ovarian, cervical or uterine cancer. Symptoms of pelvic floor disorders, PA levels and HRQoL were assessed pre-surgery, six-weeks and three-months after surgery using: the Incontinence Severity Index, the Pelvic Floor Distress Inventory-Short Form (PFDI-20), the PFDI-20 subdomains of the Urogenital Distress Inventory (UDI-6), the Colorectal-Anal Distress Inventory (CRADI-6) and the Pelvic Organ Prolapse Distress Inventory (POPDI-8), the Female Sexual Function Index, the International Physical Activity Questionnaire and the European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire. Change over time in each outcome was analysed using generalised estimating equations or linear mixed models.
Results: Of 277 eligible patients, 126 consented to participate. The majority of participants had stage 1 cancer (62%) and the most common cancer was endometrial cancer (69%). The prevalence of urinary incontinence was 66% before and 59% three-months after surgery, while the prevalence of faecal incontinence was 12% before and 14% three month after surgery, these differences were not statistically significant (Table 1). However, the prevalence of pelvic floor symptoms on the PFDI-20 and urogenital symptoms UDI-6 subdomain decreased significantly (Table 1). The incidence of urinary incontinence three-months after surgery was 10%, and 8% of participants developed new faecal incontinence. At three-months after surgery, 42% of participants reported sexual activity in the preceding four weeks compared to 27% before surgery (p=0.003). The prevalence of dyspareunia was high in those who had attempted penetrative intercourse both before (n=11/17) and three-months after surgery (n=11/20). Only 39% of the participants met PA guidelines before surgery, and this increased significantly to 53% at three-months post-surgery (p=0.020). Scores on the global health status/QoL domain of the EORTC-QLQ C30 did not significantly change from before surgery (mean 64.8/100, 95%CI 61.2, 68.4) to three-months (mean 69.4/100, 95%CI 65.6, 73.2) after surgery (mean difference 4.6, 95%CI -0.6, 9.8).
Conclusions: Patients with gynaecological cancer experienced high rates of pelvic floor disorders before and after hysterectomy. New cases of urinary and faecal incontinence developed between pre-surgery and three-months post-surgery. Physical activity levels increased significantly, and HRQoL did not significantly change between pre-surgery and three-months post-surgery. These findings suggest that clinicians working with gynaecology-oncology patients undergoing hysterectomy may need to consider screening and providing treatment options for pelvic floor disorders. Further prospective studies are required to identify subgroups of patients most at risk of pelvic floor disorders, and clinical trials assessing feasibility and effectiveness of treatments are warranted.
Funding: This project was supported by an Australian Physiotherapy Association Physiotherapy Research Foundation Project Grant. The principal investigator was supported by an Australian Government Research Training Program Scholarship.
Table 1: Prevalence of pelvic floor disorders and physical activity levels before and after surgery
Are muscarinic agonists and acetylcholinesterase inhibitors effective for the treatment of underactive bladder?
Moro C1, Veer V1, Phelps C1
Centre for Urology Research, Faculty of Health Sciences and Medicine, Bond University, Queensland
Introduction & Objectives: There are a range of mechanisms and systems underlying urinary bladder contractions, with interactions between nerves, endogenously released chemicals and receptors all playing a part in the overall function1,2. However, when contraction is inhibited, such as with underactive bladder, it can be challenging to work out which mechanisms may be at fault. Nonetheless, it is feasible that parasympathomimetics (muscarinic agonists and acetylcholinesterase inhibitors) might be beneficial for enhancing contractions of the urinary bladder, which is of particular interest in the pharmaceutical treatment of underactive bladder. This study systematically reviewed and meta-analysed the current literature to assess the effectiveness of muscarinic agonists and acetylcholinesterase inhibitors for the treatment of underactive bladder.
Methods: An a priori protocol was registered in PROSPERO, and database searches were undertaken within Embase, PubMed and CENTRAL. The study included both randomised and non-randomised controlled trials that incorporated patients with underactive bladder. Articles that compared any parasympathomimetic medication to a placebo, no treatment, or other pharmaceuticals were included. Risk ratios, mean differences and odds ratios were calculated from the extracted data.
Results: 3024 participants were included across twelve trials. There were significant differences between selected comparators and parasympathomimetics (favouring parasympathomimetics) in the number of patients with urinary retention, although no overall difference was identified to mean postvoid volume. There was a significant difference at up to 1-week post-intervention, favouring parasympathomimetics, but no difference at 1-month post-intervention. There were no differences identified in adverse events.
Conclusions: The literature is not clear as hypothesised regarding whether the prescription of parasympathomimetics is evidence-based for the treatment of underactive bladder3. The overall evidence is of low quality, and studies tended to end without long-term follow-ups. However, there are some observed benefits, with no major identified risk factors from parasympathomimetic prescriptions. Although it is not entirely possible to draw clear evidence-based conclusions from the current literature, this study has identified a clear need for well-controlled clinical trials to be conducted in the future.
References
- Phelps C, Chess-Williams R, Moro C. The dependence of urinary bladder responses on extracellular calcium varies between muscarinic, histamine, 5-HT (serotonin), neurokinin, prostaglandin, and angiotensin receptor activation. Front Physiol. 2022;13; doi: https://doi.org/10.3389/fphys.2022.841181
- Phelps C, Chess-Williams R, Moro C. The role of intracellular calcium and Rho kinase pathways in G protein-coupled receptor-mediated contractions of urinary bladder urothelium and lamina propria. Am J Physiol Cell Physiol. doi: https://doi.org/10.1152/ajpcell.00441.2022
- Moro C, Phelps C, Veer V, Clark J, Glasziou P, Tikkinen KAO, et al. The effectiveness of parasympathomimetics for treating underactive bladder: A systematic review and meta-analysis. Neurourol Urodyn. 2021;41(1):127-39; doi: https://doi.org/10.1002/nau.24839
An Australasian primary care clinical practice pathway for uncomplicated recurrent urinary tract infections in women
Snider R1,2, Dowling C1,2, Sengupta S1,2
1Eastern Health Clinical School, Monash University, Melbourne
2Department of Urology, Eastern Health, Melbourne
Introduction & Objective Recurrent urinary tract infections (rUTIs) are a common reason for referral to specialist Urology clinics. Specialty international guidelines provide insight into prophylaxis options but lack conclusive stepwise direction for primary care resulting in unnecessary escalation to specialists, despite a wide variety of prescribed and over the counter treatments available. We aim to develop a clinical practice pathway (CPP) that improves primary care of women with uncomplicated rUTIs by educating general practitioners.
Methods The CPP was developed by integrating a literature review of different prophylactic agents used in women with uncomplicated rUTIs with an audit of local specialist practice through a 2 round Delphi Study. The literature search strategy was developed in consultation with an information specialist and conducted on the platforms of Embase, Medline Ovid and Cochrane Trials Registry. The Delphi study was registered with the local ethics board and Australasian specialists with a known subspecialty clinical practice in the subject area were identified and invited to participate in the anonymous study after completion of informed consent. Questions were posed utilizing open ended and Likert scale responses. Consensus opinion was predefined ≥ 60% of respondents rating >4 and or <2 respectively for each statement and or question. The second survey incorporated feedback from the pooled panel responses, incorporation of structed questions based on the open-ended responses in survey 1 and a refined Likert Scale. The CPP was then circulated for review by the Delphi panel.
Results On review of the literature pertaining to prophylaxis strategies in adult women with uncomplicated rUTIs, there is limited high quality evidence with recent studies finding promising results for agents such as D-mannose, methenamine hippurate and immunotherapy. Although traditionally regarded as mainstay prevention, the evidence on antibiotic prophylaxis is also limited. The evidence is inconclusive regarding cranberry products and probiotics.
The Delphi panel included 24 participants with consensus opinions including:
- Increasing daily fluids; optimization of constipation/faecal incontinence; avoid vaginal douching and practice of post coital voiding
- Correction of pelvic organ prolapse and urinary incontinence and managing raised PVR
- Use of methenamine Hippurate, D-mannose and topical oestrogen
- Infrequent use of cranberry, immunotherapy or intravesical therapy
Consensus was not reached on the use of probiotics and antibiotic prophylaxis.
The CPP which covers the domains of assessment, management and referral, will be presented in algorithm format at the meeting.
Conclusion The clinical practice pathway synthesises the findings from the literature review, supported by the Delphi responses. The next stage of this project is a pilot study of the pathway in primary care.
Benefits of Co-Design with Consumers to Develop a No-Language Resource on Incontinence
Zerafa N
Continence Foundation of Australia, Surrey Hills, Victoria
Introduction and Objectives: With 56% of people with incontinence not seeking help1, and 47% with incorrect perceptions of incontinence1, there is a real need for key messages to reach and connect with as many people as possible. This is further compounded for culturally and linguistically diverse communities, where language barriers prevent people from accessing and understanding health information.
To address this gap, we aimed to create an inclusive resource to reach a diverse and broad population, independent of written or spoken language.
A co-design process was embarked on to engage a cross-section of consumers to share their wisdom and experience to design the resource. Co-design is a collaborative process involving community members to contribute to the formulation and solution of the problem.
The aims of this co-design process were to:
- Develop a resource easily understood by diverse audiences
- Clearly communicate two key messages - the symptoms of incontinence and where to get help
- Identify the preferred format to ensure maximum accessibility
Methods: The process commenced by asking co-design participants how we could overcome the language barrier.
Twenty people took part in two workshops to generate ideas and build early-stage content prototypes. A small number of participants from these workshops continued providing feedback in the prototype development.
These prototypes were refined and tested with another 29 people. The co-design participants had no prior contact with our organisation and represented people with and without lived experience of incontinence.
The final prototypes were further designed and developed into a series of videos, with a small sample of consumers testing the videos for a final check of message integrity.
Results: Three prototypes were developed and converted into animated videos, showcasing three types of incontinence: urgency, stress and frequency.
The final concept of animated videos drew on the rich range of ideas that resulted from the engaged and dynamic discussions by co-design participants. We learned that it was important to consider:
- Inclusion
- Story telling
- Transparency
- Empowerment
- Dignity.
Throughout the co-design process, participants from a diverse range of demographic backgrounds, self-reported2 high levels of:
Positivity in working with the organisation
Safety in contributing and sharing
Satisfaction in sharing thoughts and ideas.
Conclusion: The co-design process generated many ideas and enthusiasm from all participants that would not have been imagined otherwise. Using codesign facilitated learning and built capacity for broadening consumer involvement in the organisation’s core activities.
It enabled us to incorporate the strengths and richness of consumers’ lived experience with or without incontinence, reinforcing our vision for an Australian community free of the stigma and restrictions of all aspects of incontinence across the lifespan.
References
- Continence Foundation of Australia. Annual Report: The National Consumer Continence Survey 2022. [Internet] 2022 [updated 2022 Nov 17; cited 2022 Feb 27]; Available from: https://www.continence.org.au/sites/default/files/2022-11/Annual%20Report%202022_Singles.pdf
- Continence Foundation of Australia. Survey Monkey – Workshops 1 & 2 Survey Feedback. September 2022
Suprapubic catheter usage – a simple procedure, but is it so?
Losco G1,2, Thompson N2
1Te Whatu Ora - Waitaha Canterbury, Christchurch
2University of Otago, Christchurch
Introduction & Objectives: Suprapubic catheter (SPC) insertion is a common urological procedure, often considered to be safe and straightforward. However, our experience suggests this procedure may be associated with significant comorbidity, serious adverse events, and a higher length of stay than expected. There is a lack of published data surrounding the safety of this procedure, and potential risk factors for complications both short and long term are unclear. This study aimed to understand current rates of SPC insertion, demographics, indications, complications, and length of stay.
Methods: A retrospective review of all patients having undergone SPC insertion at Canterbury DHB since the inception of the SPC synoptic operation note in 2017 was undertaken. Data was collected on demographics, indication, procedural details, in-hospital complications, length of stay and long-term complications. Patient groups were identified to determine if there were any predictive factors placing individuals at an increased risk of complications.
Results: Data was analysed on 210 SPC insertions performed using the Add-a-Cath trocar technique (30% female); the mean age at insertion was 64.2 (range: 8-98). Overall, there were two intraoperative bowel perforations, and 47.7% of SPC insertions were associated with at least one complication following discharge requiring reattendance to hospital. The mean length of stay for those who presented to hospital with complications was 3.1 days. Infective factors were the most common cause, accounting for 43.3% of presentations. The highest rate of complications arose within patients aged 30-39 (83.3%) and 50-59 (58.1%). Inability to manage intermittent catheterisation as the indication was associated with the highest rate of complications (70%), followed by not tolerating urethral catheterisation (64.5%) and urinary retention (55%). Overall complications were similar in patients whose bladder was filled via cystoscope (50.4%) versus urethral catheter (44.7%). Eight patients (4%) required surgical reinsertion of their SPC.
Seven patients underwent open cut-down SPC insertion (42.9% female); of these, there was one intraoperative bowel perforation and 57.1% experienced at least one complication following discharge. The average number of visits relating to SPC complications following discharge was eight. The most common complications included bladder spasms (35.9%), catheter leakage (25.6%) and UTI (12.8%).
Conclusions: While SPC insertions are commonly perceived to be well tolerated by patients and a simple solution to catheter-related issues, our study highlights a higher than previously understood rate of complications following discharge. This data will facilitate informed decision making between clinician and patient, recognising potential risk factors that increase an individual’s likelihood of experiencing adverse events leading to improved resource allocation.
A novel method to assess female voiding. Is transpubic sonography a reliable assessment of functional voiding in asymptomatic females?
Dellar B1, Hodges P, Stafford R, Chung E
1University of Queensland, Brisbane
Introduction & Objectives Most diagnostic tests for voiding function are static in nature and urodynamic test is invasive. This study applied concurrent uroflowmetry and an innovative ultrasound imaging method to evaluate voiding parameters. There were two aims. 1) Establish a new technique to image functional voiding in asymptomatic women. 2) Assess inter- and intra-tester, and test-retest reliability of transpubic voiding sonography measures
Methods Following ethics approval (2021/HE000137), 32 healthy women with no history of lower urinary tract conditions consented to participate and were scanned separately by 2 sonographers (BD and RT) over 2 days (Day 1-s1; Day 2- s2). Sonographers were blinded to each other’s measurements. Normative measurements of the bladder neck displacement and urethral movement during void and pelvic floor muscle activation were obtained. A curve array (1-5 MHz) ultrasound transducer was placed in a longitudinal plane transpubic through the long axis of the fibrocartilaginous symphysis joint (SP) to measure these variables and electronic recording of the duration of void was recorded. The recorded ultrasound video was replayed and still images taken at start, max void and end void were printed and measurable data obtained and compared. Contraction of the pelvic floor muscles and the impact of straining were also assessed.
Results All participants completed the study and there was no reported adverse event. The mean age was 35 (standard deviation 9.4) years old while the BMI was 24 (4.7) kg/m2. The mean and stand deviation (SD) of the pubourethral angle at full max and end void ranged between 120 (SD 16.2) to 125 (SD 15.8) degrees. This increased to 140 (SD 18.5) degrees with straining and 94 (SD 15.9) degrees at contraction of the pelvic floor muscles. The mean and standard deviation (SD) of the fixed landmark, Symphysis pubis length were 38.2mm and 3.9. The mean (SD) values of the bladder neck diameter and urethral diameter during voiding were 8.3mm (SD 3) and 5.2mm (SD 2.0) respectively.
Bland-Altman analysis of pubourethral angle at full bladder was compared. Between s1BD and s2BD (intra tester), there was a bias of 2.3 degrees (s2BD higher); between s1BD and s2RT (inter-tester) there was a bias of 3 degrees (s2RT higher); and between BD and s2RT (test-retest) there was a bias of 3.5 degrees (s2RT higher). The differences between all measurements had an approximately normal distribution. The intraclass correlation coefficients were 0.68, 0.60 and 0.93 and indicating ‘good to excellent’ levels of agreement between respective measures.
Conclusions This study showed that transpubic voiding sonography is consistent and reproducible diagnostic test with good intra and inter tester measure reliability, and could be utilized to provide an alternative, non-invasive real-time method of female functional voiding assessment.
The development of a perineal specific body perception questionnaire, based on the Fremantle Back Awareness Questionnaire, to measure body perception in individuals with persistent perineal pain.
Jones C1, Kelly M1, Thompson J1, Martin R1, Petrou A1, Vandyken C2, Bond J3, Wand BM4, Ng L1
1Curtin Univerity, Perth, WA
2McMaster University, Hamilton, Canada
3Brunel University, London, UK
4The University of Notre Dame Australia, Fremantle, WA
Introduction & Objectives Persistent pelvic pain affects up to one in four women and up to one in seven men worldwide.1 Pelvic pain includes the perineum plus genitals and can contribute to lower urinary tract and bowel issues, sexual dysfunction, pelvic floor muscle disorders and gynecological dysfunction. Studies in this population have repeatedly demonstrated changes in somatosensory integration, and significant morphological changes in the brain.2 It is well established that altered body perception in the presence of persistent pain can indicate dysfunction in the central processing of noxious information. Therefore, changes in body perception is a useful clinical finding which can inform effective treatment. The Fremantle back awareness questionnaire (FreBAQ)3 was developed to enhance the assessment of body perception changes in the chronic low back pain population. Currently no assessment tool exists for identifying these changes in body perception in people with persistent perineal pain.
The primary aim of this study was to develop a body perception questionnaire specific to persistent perineal pain, using a modified electronic Delphi technique. The secondary aim was to assess face validity of the new questionnaire, with a pilot cross-sectional cohort study.
Methods A focus group created a draft of the proposed questionnaire based on the pre-existing FreBAQ.
A panel of 14 healthcare practitioners with a special interest in pain, completed three Delphi rounds of moderated teleconference discussions followed by anonymous voting, via electronic survey, to refine the wording of each questionnaire item. A pilot sample of 17 participants with persistent perineal pain tested the face validity of the new Fremantle Perineal Awareness Questionnaire (FrePAQ).
Results All panel participants completed all three rounds of the Delphi study. Informed discussion by the international panel of experts, created and refined wording for the new assessment tool. After three rounds, consensus was achieved on a nine-item questionnaire specific to persistent perineal pain. Pilot study participants with perineal pain judged the FrePAQ to be expedient, easy to understand and relevant to their pain experience.
Conclusions The FrePAQ is a novel assessment tool developed to identify changes in body perception in people with persistent perineal pain. This will enable therapists to better target treatment aimed at normalising body perception and potentially improve clinical outcomes.
References
- Engeler D, Baranowski A, Berghmans B, et al. EAU Guidelines on Chronic Pelvic Pain (2022) EAU Guidelines Office, Arnhem, The Netherlands. accessed: https://uroweb.org/guidelines/chronic-pelvic-pain
- Bhatt R, Gupta A, Rapkin A, et al. Altered gray matter volume in sensorimotor and thalamic regions associated with pain in localized provoked vulvodynia: a voxel-based morphometry study. Pain. 2019;160(7):1529-1540. dx.doi:10.1097/j.pain.0000000000001532.
- Wand B, James M, Abbaszadeh S, et al. Assessing self-perception in patients with chronic low back pain: development of a back-specific body-perception questionnaire. J Back Musculoskelet Rehabil. 2014;27(4):463-473. doi:10.3233/BMR-140467.
Clinical practice trends in pelvic floor procedures: survey results from the Australasian Pelvic Floor Procedure Registry
Ahern S1, Kartik A1, Jayasinghe RT1, Honardoost MA1, Daly O1,2
1School of Public Health and Preventive Medicine, Monash University, Melbourne, Victoria, Australia
2Western Health, Centre for Digital Transformation of Health, Melbourne University, Victoria, Australia
Introduction and objectives: The Australasian Pelvic Floor Procedure Registry (APFPR) was established in 2019 following an Australian Senate Inquiry, to monitor the safety and quality of Stress Urinary Incontinence (SUI) and Pelvic Organ Prolapse (POP) procedures involving mesh or other prostheses1,2. While the registry’s establishment and national rollout was significantly impacted by the COVID pandemic in 2020-22, as of February 2023 there are 32 sites that had governance approval, with 18 public and private sites actively participating across seven jurisdictions. Following clinical feedback that highlighted changing clinical practice, the APFPR Steering Committee in 2022 undertook a bi-national clinician survey to better understand related environmental factors and to reassess the scope of the registry.
Methods: A clinician survey was developed regarding previous and current surgical practice for PFDs; and key factors associated with any changing practice. Demographic information included clinician years of practice, jurisdiction, hospital setting, and public vs private practice. The survey was distributed via the APFPR to contributing clinicians, as well as to USANZ and UGSA membership via mailing lists and at craft group meetings.
Results: The survey returned 79 responses across the three craft groups, estimated to be an approximately 15% response rate. All jurisdictions were represented except the NT, with 80% from metropolitan areas and 71% from a mixed public/private setting. Respondents comprised those with < 5 years of specialty practice (17%) to those with > 30 years (15%).
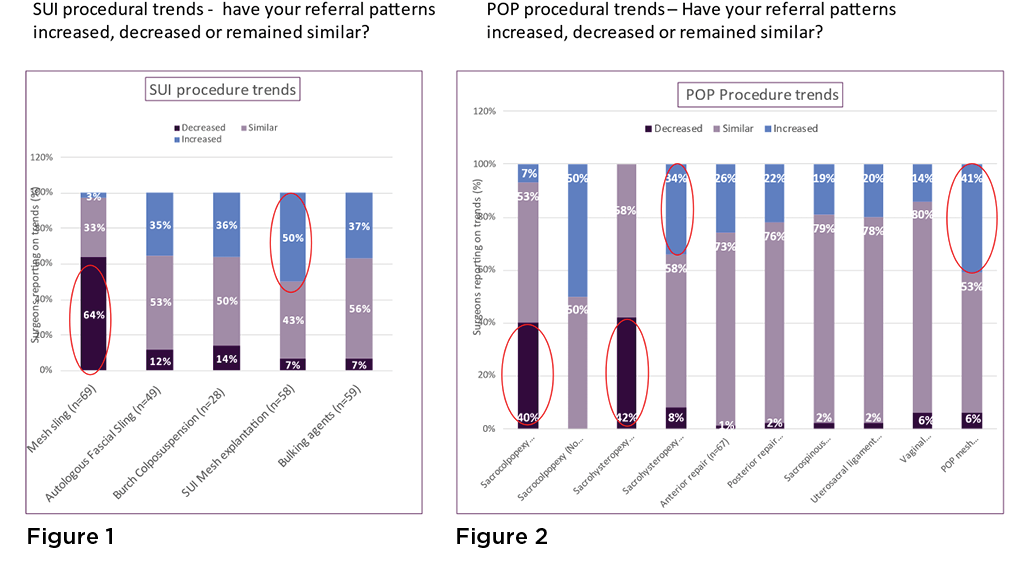
Regarding SUI (Figure 1), approximately two thirds of respondents had noted a reduction in mesh sling procedures, and 50% had noted an increase in mesh explantation following SUI procedures. Reasons identified for this was patient preference (83%), litigation concerns (59%) and COVID restrictions (39%). Clinician responses included undertaking other procedures (54%), changing to non-operative management (17%), referral to others (15%) and upskilling (2%).
Regarding POP (Figure 2), approximately 40% of respondents had noted a reduction in sacrocolpopexy and sacrohysteropexy procedures with mesh, with 50% and 34% noting an increase in these procedures without mesh respectively. Over 40% noted an increase in mesh explantation following POP procedures. Reasons identified for these changes were mesh availability (81%), patient preference (62%), litigation concerns (38%) and COVID restrictions (29%). Clinician responses included undertaking other procedures (71%), upskilling (14%), referral to others (10%), and changing to non-operative management (5%).
Seventy-five percent of respondents recommended adding non-mesh SUI including autologous fascial slings procedures to the APFPR. No change was recommended for POP procedures.
Conclusion: The APFPR survey identified a significant change in surgical practice for PFPs over the last 5 years due to a range of external factors. Surgeons are undertaking more mesh explantations, and many are upskilling, especially for management of POP. The APFPR will update the procedures that it captures to effectively monitor relevant patient outcomes into the future.
References
- Ahern S et al. 2022 Report No 1, pages 36
- Daly, J.O. et al. 2019 Aust N Z J Obstet Gynaecol. 59 (4): p. 473-476.
Key pain science education concepts for persistent pelvic pain: an e-Delphi study of expert clinicians
Mardon A1, Leake HB1, Wilson MW1, Karran E1, Parker R2, Malani R3, Moseley L1, Chalmers J1,4
1IIMPACT in Health, University Of South Australia, Adelaide
2Department of Anaesthesia and Perioperative Medicine, University of Cape Town, Cape Town, South Africa
3MGM School of Physiotherapy, Aurangabad, A constituent unit of MGMIHS, Maharashtra, India
4Western Sydney University, Campbelltown, NSW
Introduction: Persistent pelvic pain (PPP) affects approximately one in five females and has significant impact on one’s physical, psychological, and social wellbeing. Patient education is a critical component of persistent pain management. Pain science education (PSE) is one type of patient education, that aims to better people’s understanding of the ‘what’, ‘why’, and ‘how’ of pain.1 PSE has been shown to be effective at reducing pain and disability in musculoskeletal pain conditions.2 Investigations into the role of PSE in PPP management remains in its infancy, which may be in part be due to the lack of targeted curricular for this population. The aim of this study was to gain expert consensus on the key PSE concepts for females with PPP.
Methods: A three-round electronic Delphi (e-Delphi) process sought the opinions of a multi-disciplinary panel comprising of 20 international expert clinicians. Panel members rated concepts derived from open-ended responses using a six-point Likert scale (not at all important - very important). Consensus was considered reached for items with an IQR <1.0. Panel members responses were considered stable when no statistically significant change (p ≥ .05) was detected between the rounds using the nonparametric Wilcoxon matched pairs signed rank test.
Results: The e-Delphi response rate was over 75%. The panel raised 125 key PSE concepts for females with PPP, of which 89 (71.2%) reached consensus and 124 (99.2%) reached stability. Thirteen themes were developed to represent overarching PSE concepts for PPP, including: ‘the experience of pain’; ‘there are different types of pain’; ‘the brain and the nervous system are involved in pain’; ‘pain is protective’; ‘PPP involves changes to the brain and nervous system’; ‘PPP doesn’t always equate to tissue pathology’; ‘PPP can change and improve’; ‘many factors influence PPP’; ‘PPP can be influenced by biological factors’; ‘PPP can be influenced by the pelvic floor’; ‘PPP can be influenced by psychosocial factors’; ‘PPP can be managed in many ways’; and ‘PSE can help reduce PPP’. Seventeen PSE concepts were also generated for specific PPP conditions (e.g., endometriosis) and seven concepts for specific life stages related to PPP (e.g., adolescence).
Conclusion: This study provides the first list of key PSE concepts tailored for females with PPP, as developed by an international panel of expert clinicians. These concepts can be considered when developing and implementing PSE curricular for females with PPP.
Disclosure
This project has ethics approval from the University of South Australia Human Research Ethics Committee (no. 204706).
Presenter and author are supported by the Research Training Program Stipend as a postgraduate student at the University of South Australia. Other authors are supported by a Leadership Investigator grant from the National Health & Medical Research Council of Australia ((NHMRC) ID 1178444). Author is supported by a grant awarded from The Hospital Research Fund (Grant Number PG105576).
I have a competing financial relationship/s affiliation/s that could be perceived as having a bearing on my presentation. I have listed all current competing interests or affiliations below:
Presenter has been reimbursed travel costs related to presentation of research on pain at scientific conferences/symposia. Author has led a research program developing, testing and implementing pain science education programs. Professional and scientific bodies have reimbursed him for travel costs related to presentation of research on pain education at scientific conferences/symposia. He has received speaker fees for lectures on pain and rehabilitation. He receives book royalties from NOIgroup publications, Dancing Giraffe Press & OPTP, for books on pain education. He has received support from: Institutes of Health, California; AIA Australia; Reality Health’ Connect Health UK; Kaiser Permanente. Author has received speaker fees for talks on pain. Author has received speaker fees for lectures on physiotherapy and pain. Professional bodies have reimbursed her for travel costs related to presentation of research on physiotherapy and pain at scientific congresses.
References
- Moseley GL, Butler DS. Fifteen Years of Explaining Pain: The Past, Present, and Future. J Pain. 2015 Sep;16(9):807–13.
- Watson JA, Ryan CG, Cooper L, Ellington D, Whittle R, Lavender M, et al. Pain Neuroscience Education for Adults With Chronic Musculoskeletal Pain: A Mixed-Methods Systematic Review and Meta-Analysis. J Pain. 2019 Oct;20(10):1140.e1-1140.e22.
What pain science concepts are important to females with persistent pelvic pain? A reflexive thematic analysis
Mardon A1, Chalmers J1,2, Heathcote L3, Freedman L4, Malani R5, Parker R6, Neumann P1,
Moseley L1, Leake H1
1IIMPACT in Health, University of South Australia, Adelaide
2Western Sydney University, Campbelltown, NSW
3Health Psychology Section, Institute of Psychiatry Psychology and Neuroscience, King’s College London, London
4EndoActive, Sydney
5MGM School of Physiotherapy, Aurangabad, A constituent unit of MGMIHS, Aurangabad, India
6Department of Anaesthesia and Perioperative Medicine, University of Cape Town, Cape Town, South Africa
Introduction: Pain science education (PSE) aims to provide people with an understanding of ‘how pain works’ and the biopsychosocial model of pain; it has been demonstrated to reduce pain and disability in musculoskeletal pain conditions. Preliminary evidence suggests PSE may be effective for females with PPP,1–3 however the content has yet to be optimised for this population. Therefore, the aim of this study was to identify PSE concepts that females with PPP consider important and why.
Methods: Twenty individual, semi-structured interviews were conducted with adult females who self-identified as having ‘improved’ PPP and had engaged with PSE. Most participants had been diagnosed with endometriosis (n=16). Data were analysed using reflexive thematic analysis.
Results: Four themes were generated capturing PSE concepts considered important by people with ‘improved’ PPP: (i) “A sensitised nervous system leads to over-protective pain” validated their PPP as being real; (ii) “Pain doesn’t have to mean the body is damaged (although sometimes it does)” provided reassurance that PPP does not mean their condition is worsening; (iii) “How I think, feel, and ‘see’ my pain can make it worse” enabled participants to find optimal ways to manage their pain; (iv) “I can change my pain… slowly” provided hope that PPP can improve and empowerment to pursue improvement as a viable goal (Figure 1).
Conclusion: This study generated four PSE learning concepts that are important to females whose PPP has improved and may provide a framework for optimizing PSE for females with PPP.
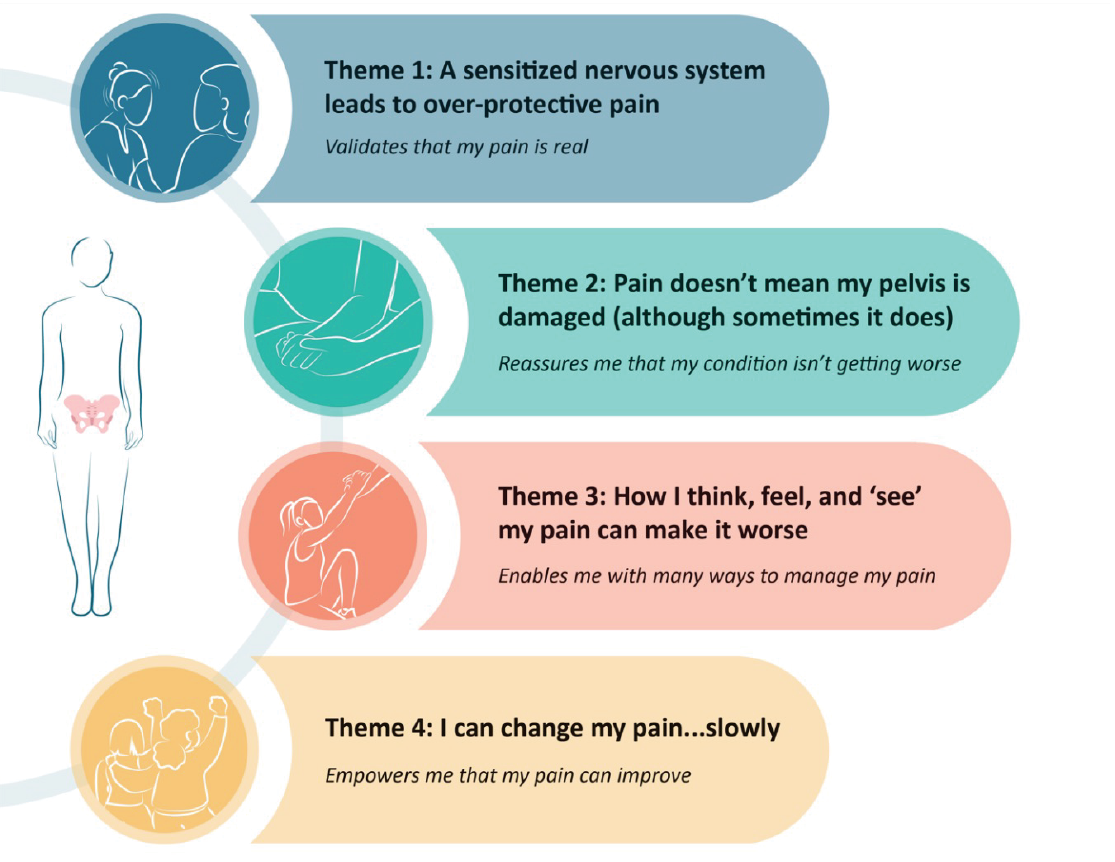
Figure 1: Important pain science education concepts for females with persistent pelvic pain
Disclosure
This project has ethics approval from the University of South Australia Human Research Ethics Committee (no. 203392).
Presenter is supported by the Research Training Program Stipend as a postgraduate student at the University of South Australia. Other authors are supported by a Leadership Investigator grant from the National Health & Medical Research Council of Australia ((NHMRC) ID 1178444). Other author is supported by a grant awarded from The Hospital Research Fund (Grant Number PG105576).
I have a competing financial relationship/s affiliation/s that could be perceived as having a bearing on my presentation. I have listed all current competing interests or affiliations below:
Presenter has been reimbursed travel costs related to presentation of research on pain at scientific conferences/symposia. Author has led a research program developing, testing and implementing pain science education programs. Professional and scientific bodies have reimbursed him for travel costs related to presentation of research on pain education at scientific conferences/symposia. He has received speaker fees for lectures on pain and rehabilitation. He receives book royalties from NOIgroup publications, Dancing Giraffe Press & OPTP, for books on pain education. He has received support from: Institutes of Health, California; AIA Australia; Reality Health’ Connect Health UK; Kaiser Permanente. Author has received speaker fees for talks on pain. Author has received speaker fees for lectures on physiotherapy and pain. Professional bodies have reimbursed her for travel costs related to presentation of research on physiotherapy and pain at scientific congresses.
References
- Locke L, Neumann P, Thompson J, Briffa K. Management of pelvic floor muscle pain with pelvic floor physiotherapy incorporating neuroscience-based pain education: A prospective case-series report. The Australian and New Zealand Continence Journal [Internet]. [cited 2022 Apr 21];25(2):30–8. Available from: https://search.informit.org/doi/10.3316/informit.460538222434258
- James A, Thompson J, Neumann P, Briffa K. Change in pain knowledge after a neuroscience education seminar for women with chronic pelvic pain. The Australian and New Zealand Continence Journal [Internet]. [cited 2022 Apr 21];25(2):39–44. Available from: https://search.informit.org/doi/10.3316/informit.460594121348032
- Beaumont T, Phillips K, Hull ML, Green R. Does group physiotherapy improve pain scores and reduce the impact of pelvic pain for women referred with persistent pelvic pain? A clinical trial. Journal of Endometriosis and Pelvic Pain Disorders [Internet]. 2022 Dec 1 [cited 2023 Feb 15];14(4):169–77. Available from: https://doi.org/10.1177/22840265221141527
Functional outcomes 12 months post full mesh removal – a retrospective analysis of a single centre
Emerson A1, Couchman MAP1
1Central Adelaide Local Health Network, RAH, Adelaide
Introduction and Objective The Federal Senate Standing Committee on Community Affairs released 13 recommendations for consideration in a concerted response to health-related adverse outcomes with the use of transvaginal mesh1. Medical professional colleges and specialist societies require members to monitor, record and report on the outcomes of mesh-related procedures as per recommendation 10. An inter-disciplinary team was formed in South Australia, to offer mesh-injured consumers interdisciplinary management. Full mesh removal was offered from 2022. In counselling about full mesh removal, post-operative outcomes regarding continence (urinary) and chronic pelvic pain were key areas of concern for consumers. Currently, there are minimal data available regarding the impact of full mesh removal on the rates of urinary incontinence and the impact on chronic pelvic pain levels in Australian women. We retrospectively analysed patient-reported outcomes to better inform consumers and future decision making, predominantly regarding urinary incontinence and pelvic pain.
Methods A total of 15 patients underwent full mesh removal surgery throughout 2022. Each consumer completed two surveys in the waiting bay prior to their surgery. Post-operative surveys were distributed at 6 months and 12 months via post (with a reply-paid envelope) or email. The two surveys used were the ‘International Consultation on Incontinence Questionnaire – Urinary Incontinence, Short Form’ (ICIQ-UI SF) & the ‘Pelvic Pain Impact Questionnaire’ (PPIQ). The questionnaires were de-identified for analysis.
Results Surgeries were performed periodically throughout 2022 and a total of 15 surveys were completed pre-operatively. At the time of analysis, 13 participants were 6 month’s post-operative and 5 had returned completed surveys whilst 6 participants were 12 months post-operative and 1 survey had been returned.
The average age of the group was 58.5 years, with the average time from implantation to removal being 11.5 years. 88% of the implants removed were tension-free vaginal tapes (retropubic and/or obturator).
Pre-operative ICIQ-UI SF results demonstrated the mean result of 9.2/21, indicating a moderate quality of life impact relating to urinary incontinence at the time of mesh removal. At 6 months post-operatively, the ICIQ-UI SF mean result was 12.4/21 with an increase to 21/21 at 12 months.
Pre-operative PPIQ results demonstrated a mean result of 15.7/32, indicating a moderate degree of chronic pelvic pain impacted quality of life. At 6 months post-operatively, the PPIQ mean result had decreased to 13/32 and at 12 months, the mean score was 7/32.
Conclusion The results demonstrate that the removal of a mesh implant can result in the return of, or an increase in the severity of, urinary incontinence, whilst it can have a positive impact on the severity of chronic pelvic pain experienced. The sample size in this cohort is small, with a decreasing number responding to the post-operative questionnaires; therefore, it is difficult to ascertain statistical significance. However, this is a real-world report of the key quality of life factors following full mesh removal in South Australia and allows for accurate counselling of patients undertaking mesh removal. Further surveys will be undertaken on an annual basis until 5 years post removal surgery.
References
- Commonwealth of Australia. (2018). Number of women in Australia who have had transvaginal mesh implants and related matters (ISBN 978-1-76010-701-7). Retrieved from https://www.aph.gov.au/Parliamentary_Business/Committees/Senate/Community_Affairs/MeshImplants/Report
Testing the convergent validity of the Pelvic Pain Psychological Screening Questionnaire (3PSQ): An observational, cross-sectional study
Dwyer S1, Yassin N1, Barwood A1, Yammouni L1, Thompson J1 Chalmers J2
1School of Physiotherapy and Exercise Sciences, Curtin University, Perth
2IMPACT in Health, University of South Australia, Adelaide
Introduction & Objectives Persistent pelvic pain (PPP) is a complex condition, with pain resolution occurring in only 20-25% of those seeking treatment1, thus it is a significant and continuing global health problem. Screening for psychological factors, as part of a thorough biopsychosocial assessment, provides an individualised, patient-centred approach to care, which has been shown to enhance treatment outcomes2. However, comprehensive screening for all potential psychological elements of PPP involves administering multiple lengthy questionnaires, the majority of which are not directly targeting people with PPP, nor have they been validated in this specific population.
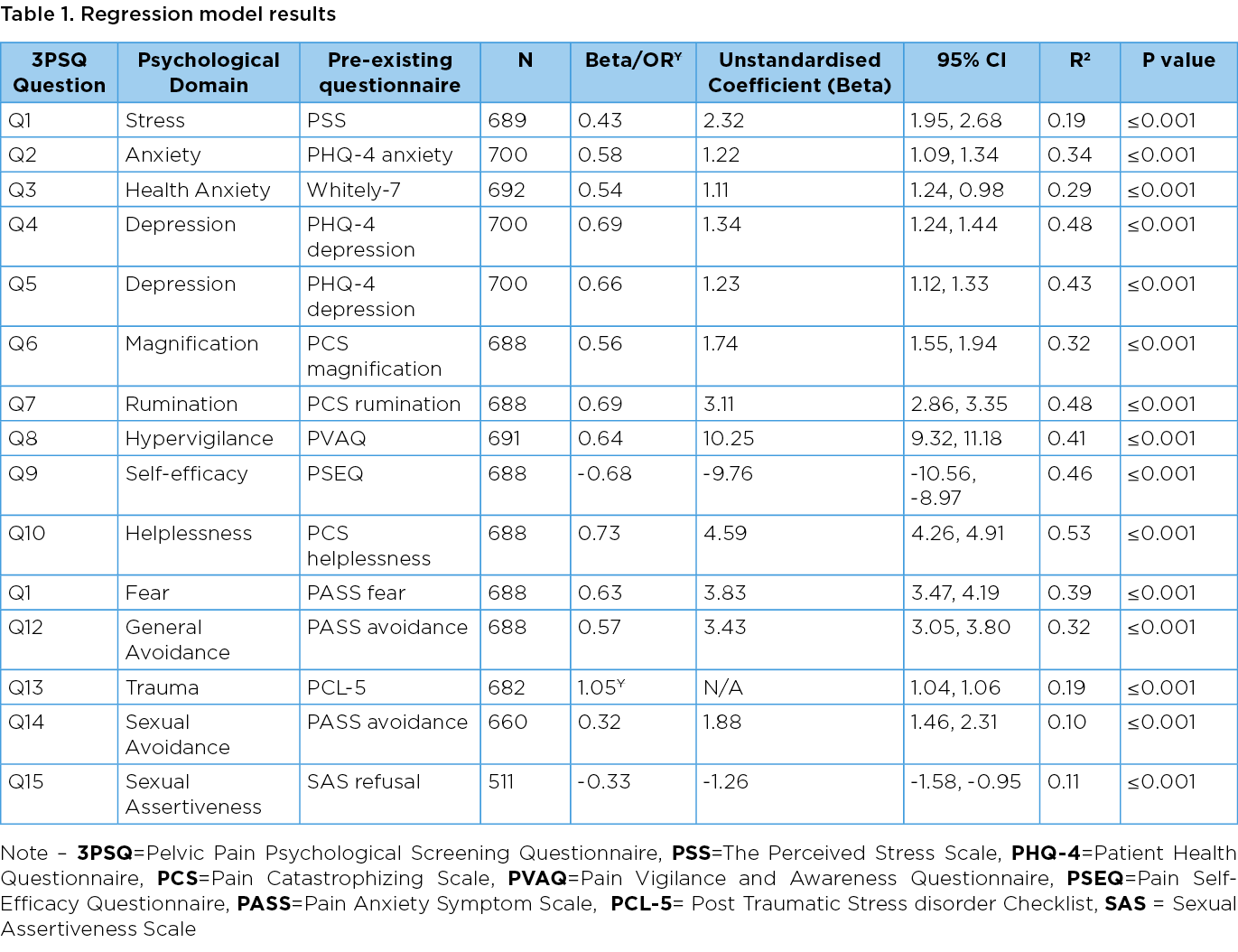
The Pelvic Pain Psychological Screening Questionnaire (3PSQ) was developed to screen 13 psychological factors known to affect treatment outcomes in patients with PPP: stress, anxiety, depression, health anxiety, magnification, rumination, helplessness, hypervigilance, self-efficacy, fear, avoidance, trauma, and sexual assertiveness. Each 3PSQ question was derived from 9 original validated questionnaires. The aim of this observational cross-sectional study was to establish the convergent validity of the 3PSQ.
Methods An online survey consisting of the 3PSQ and all 9 original validated questionnaires was distributed through social media platforms and specialist clinics.
Participants from around the world with self-reported pelvic pain, with or without a formal diagnosis, were invited to participate in the study. Participants over the age of 18 years, who identified as any gender were deemed eligible. Participants who were pregnant, or had experienced childbirth or pelvic surgery in the preceding 6 months, were excluded from the study.
Responses were compared using linear or logistic regression models and summarised with standardised beta (β) coefficients and Odd Ratios (OR), respectively; a strong relationship was hypothesised. A target sample size of 485 people was required to detect a small effect size, with 80% power, in a linear regression model (R2=0.02).
Results 789 participants (93% female, 6% male and 1% gender variant or non-binary) with a mean age of 39 (13.3 SD) and range of 18-76 years were included in the analysis.
All fourteen linear regression models were in the hypothesised direction and reached the target coefficient of >0.30 (standardised β 0.322-0.725). The logistic regression model confirmed the hypothesised positive relationship between the binary 3PSQ question and comparative questionnaire (OR 1.049). All results were statistically significant, see Table 1 for all results.
Conclusions The 3PSQ is the first tool designed to specifically screen for the presence of 13 psychological factors in the pelvic pain population, and this study has established the convergent validity for each of the 15 screening questions. Clinicians can now use the tool with confidence, knowing that each question validly screens for the intended psychological factor, within a pelvic pain population.
Disclosures
University Human Research Ethics Committee, Curtin University (Approval number: HRE2020-0356 and HRE2020-0302)
The researchers of this study received a $100 donation from Curtin University, with researchers contributing a further $100. A total of $200 was allocated to the cost of an optional prize draw, one of four $50 vouchers, which participants could enter at the end of the survey as a token of appreciation for their time.
References
- Weijenborg PTM. Women in pain: the course and diagnostics of chronic pelvic pain. [doctoral thesis]. Leiden, Netherlands: Leiden University; 2009.
- Engeler D, Baranowski AP, Berghmans B, et al. EAU Guidelines on Chronic Pelvic Pain: European Association of Urology; 2019.