Volume 30 Number 2
9 Percutaneous Tibial Nerve Stimulation for Overactive Bladder Syndrome: a single-arm trial
Dr Hnin Yee Kyaw, Professor Hannah Krause, Professor Judith Goh
Licensed under CC BY 4.0
DOI 10.33235/anzcj.30.2.32
Objective: Overactive bladder (OAB) is estimated to affect 11.8% of women worldwide causing diminished quality of life, feelings of guilt, apathy, reduced self-esteem and depressive symptoms.1,2 Lifestyle modifications and muscarinic receptor antagonist remain the mainstay of treatment, but are limited by their efficacy and adverse effects. Access to third-line therapies of intravesical botox or sacral neuromodulation is limited by its invasive nature. Percutaneous tibial nerve stimulation (PTNS) has emerged as a non-invasive treatment option for OAB.
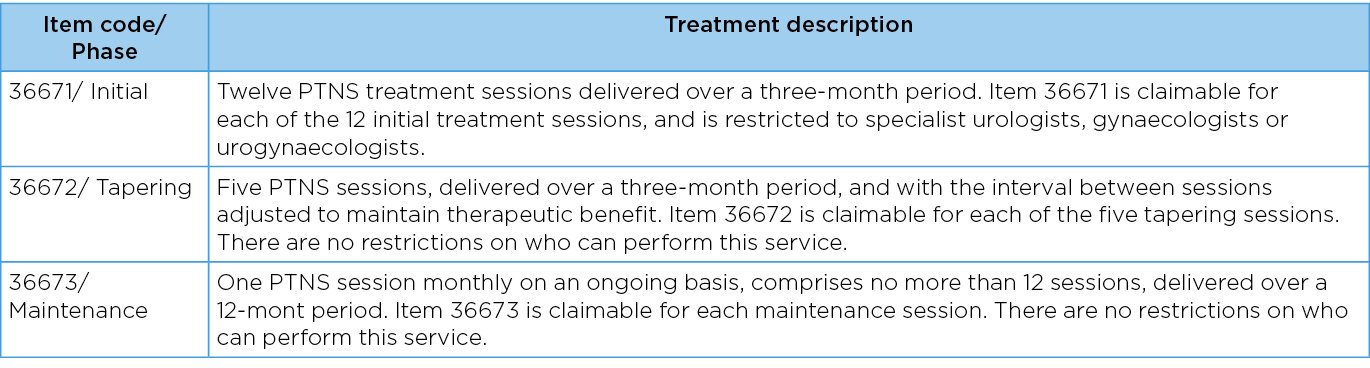
The objective of this study is to establish PTNS administered based on the Medicare Benefit Schedule treatment regime as a safe and effective treatment for OAB.3
Methods: A single-arm trial involving 84 women with a diagnosis of OAB requiring third-line treatment was offered PTNS administered by urogynaecologists. The primary treatment outcome was patient reported visual analogue score (VAS) improvement of at least 50%. Secondary outcome measures were Urinary Distress Inventory Short Form (UDI-6) score and 2-day bladder diary. Patients also provided feedback on adverse effects encountered. Inclusion criteria for participants with OAB consisted of the ability to provide informed consent, willingness to complete UDI-6 questionnaire and bladder diary, as well as other MBS criteria such as failure of conservative management including anti-cholinergic agents, not suitable for botulinum type A therapy, and not suitable for sacral nerve stimulation. Patients were excluded if there were contraindications to PTNS treatment, were unable or unwilling to participate with treatment protocol, or had no diagnosis of OAB.
Results: Eighty-four women between the ages of 25 – 101 years (mean: 72.6 years, median: 75 years) participated in the study. Only one participant had no documented urodynamic study as she was 98 years old at the time of entry into the study. Fifty-eight participants (69%) had detrusor overactivity diagnosed on a previous urodynamic study, a further 6 participants (7%) had bladder oversensitivity, and 4 participants had voiding dysfunction. Thirty-nine participants had undergone a hysterectomy. Twenty-one participants had previously received continence surgery, with the most common procedure being insertion of mesh mid-urethral sling (n=14). Some participants had previously received more than one type of continence surgery. Other types of continence surgeries were colposuspension (n=5) and urethral bulking injections (n=4). Drop out rate from initial treatment regime was 6%. The results showed successful initial treatment protocol of 77.2% based on VAS, and a statistically significant improvement in mean UDI-6 score of 20.13 (P<0.01, SD 12.52). Continued success following tapering protocol of 60.8% with a mean maintenance treatment duration of 21.2 months. 26 women who qualified for maintenance treatment regime discontinued treatment for various reasons after a mean maintenance treatment duration of 14.2 months. No adverse effects were reported.
Conclusions: This trial agrees with previously published literature on the effectiveness and safety of PTNS as a treatment modality for OAB. Following the treatment regime as described by the Medicare Benefit Schedule showed showed 77% initial treatment success, and 60% long term success in improving symptoms by at least 50%. Further RCTs to evaluate the optimal treatment protocol are warranted to establish a standardised regime.
Table 1. MBS items listed for PTNS therapy.
Author(s)
Dr Hnin Yee Kyaw1, Professor Hannah Krause1,2, Professor Judith Goh1,2
1Gold Coast University Hospital, Southport, Australia, 2Greenslopes Private Hospital, Greenslopes, Australia
References
- Simonelli C, Tripodi F, Vizzari V, Rossi R. Psycho-relational aspects of urinary incontinence in female sexuality. Urologia Journal. 2008;75(1):14-19. doi:10.1177/039156030807500103
- Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, Coyne K, Kelleher C, Hampel C, Artibani W, Abrams P. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. European urology. 2006;50(6):1306-15. doi.org/10.1016/j.eururo.2006.09.019.
- New MBS items for Percutaneous Tibial Nerve Stimulation (PTNS) for the treatment of idiopathic overactive bladder (2018) http://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/content/factsheet-PTNS. Accessed 15 Janaury 2022.