Volume 30 Number 2
Characteristics of Participants 3-Months After Pelvic Fracture: Midpoint of an Intervention Trial
Ms Carly McConnell, Ms Alisha da Silva, Mr David Priddle, A/Prof Wendy Bower
Licensed under CC BY 4.0
DOI 10.33235/anzcj.30.2.20
Introduction: Fracture to any part of the pelvis can impact pelvic floor function. Our prior small pilot observational study revealed that women can have significant enduring symptoms of bladder, bowel and sexual impairment at least one-year post injury and that men also suffer changes in urogenital function.1 This abstract presents interim findings of the observational component to a large implementation study screening for pelvic floor dysfunction (PFD) in pelvic trauma patients at 6 and 12 months with nested randomisation to physiotherapy care when PFD is identified.
Objectives: To determine the prevalence and severity of pelvic floor dysfunction 3-months post pelvic fracture.
Methods: Acute adult inpatients post pelvic fracture were recruited from two tertiary trauma hospitals. Standardised metrics of urogenital function were completed at baseline (recall based on 4 weeks prior to injury) and repeated again 3-months post injury. The instruments used were the Australian Pelvic Floor Questionnaire (APFQ)2 and simplified International Index of Erectile Function (IIEF-5, males only).3 Measures were completed electronically using a secure web application (REDCap). De-identified data was imported to SPSS software Version 28 for descriptive analysis. PFD was defined as an increase from baseline in any APFQ domain score of 1 or an IIEF-5 total score of 21 or less.
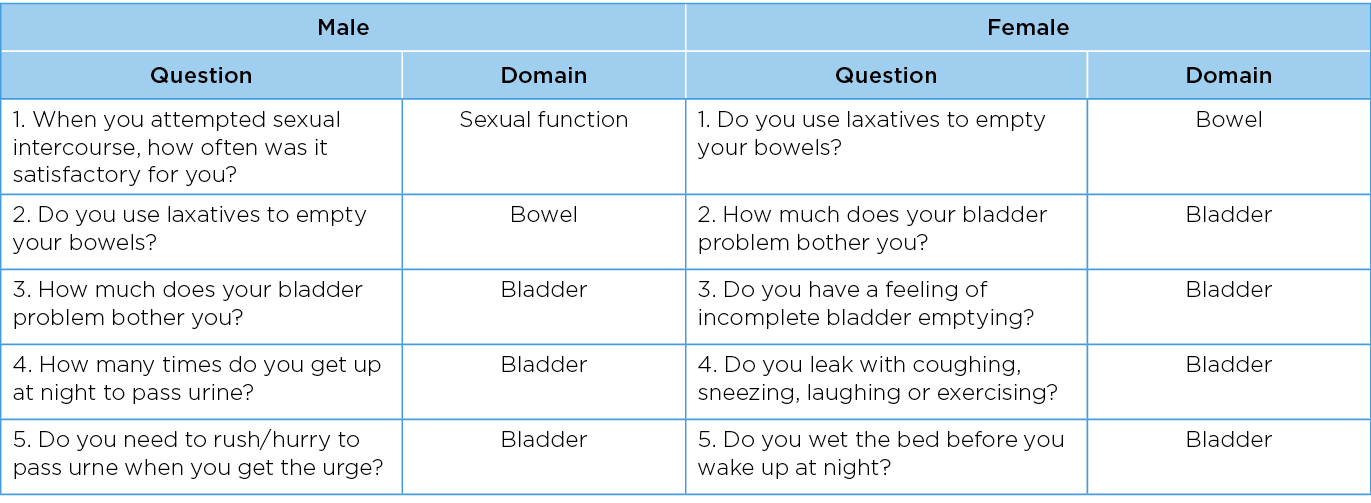
Results: A total of 546 patients have been screened up to November 2023; isolated acetabular injury excluded 23.5% of potential participants. Two hundred and thirty-seven participants have been recruited, with significantly more males (n=150) than females (n=87). A total of 65% of participants were identified as having PFD at 3 months; 62% in males and 71% in females. Table 1 describes the top five questionnaire items on which score were worse at 3-month follow up compared to pre-injury. A requirement for aperients and bladder-related bother was prioritised by both sexes.
Conclusion: Three months after traumatic insult to the pelvic girdle, nearly 2/3 of patients were found to have a PFD. These participants have subsequently been randomised into the nested controlled trial to determine the uptake of referral to specialised continence or urology services. Reassessment at 12 months will identify both the natural history of PFD with usual orthopaedic care, and uptake and patient status after referral for pelvic physiotherapy.
Project Funding
Value-based Healthcare Innovation Grant Program, Transport Accident Commission.
Ethics Approval Number: 2021.034, RMH66244.
Table 1. The top 5 items in the APQF and IIEF-5 with the largest change signifying worsening in pelvic floor function from baseline to 3-month assesssments stratified by sex.
Author(s)
Ms Carly McConnell1, Ms Alisha da Silva1, Mr David Priddle1, A/Prof Wendy Bower1,2
1Department of Allied Health, The Royal Melbourne Hospital, Parkville, Australia
2Faculty of Medicine, Dentistry and Health Sciences, The University of Melbourne, Parkville, Australia
References
- McConnell CL, Hawkins SM, Granger CL, Bower WF. Pelvic floor dysfunction one year post-pelvic trauma: An observational pilot study. The Australian and New Zealand Continence Journal [Internet]. 2020;26(4):98–102. Available from: https://search.informit.org/doi/10.3316/informit.560666123785690
- Baessler K, O’Neill SM, Maher CF, Battistutta D. Australian pelvic floor questionnaire: a validated interviewer-administered pelvic floor questionnaire for routine clinic and research. Int Urogynecol J [Internet]. 2009;20(2):149–58. Available from: https://doi.org/10.1007/s00192-008-0742-4
- Rosen R, Cappelleri J, Lipsky J, Pen Ä B. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction [Internet]. Available from: http://www.stockton-press.co.uk/ijir