Volume 28 Number 2
Pelvic floor muscle training to prevent stress urinary incontinence during pregnancy: a review
Alannah Turner
Keywords pregnancy, prevention, urinary incontinence, pelvic floor muscle training
For referencing Turner A. Pelvic floor muscle training to prevent stress urinary incontinence during pregnancy: a review. Australian and New Zealand Continence Journal 2022; 28(2):29-33
DOI
https://doi.org/10.33235/anzcj.28.2.29-33
Submitted 27 November 2021
Accepted 19 May 2022
Abstract
The purpose of this review was to explore the current evidence for pelvic floor muscle training alone, or in combination with exercise, in the prevention of stress urinary incontinence during pregnancy. The aim of this review was to determine evidence-based recommendations for clinical practice. Electronic databases were searched in July 2021 for studies published from 2014 to 2021. Randomised controlled trials, cohort studies, reviews and systematic reviews were included if they assessed the effect of pelvic floor muscle training on preventing stress urinary incontinence or unspecified urinary incontinence in pregnant women. Thirteen papers – one meta-analysis, four systematic reviews, four reviews, and four randomised controlled trials – were included in this review. Despite results generally demonstrating a trend towards pelvic floor muscle training having a protective effect in this population, it remains unclear whether the effects are enough to be clinically meaningful. Greater effects were observed in studies where women were appropriately supervised and had sufficient training dosage to elicit pelvic floor muscle strength adaptations. Further research demonstrating consistency in dosage, how pelvic floor muscle strength is assessed and measured, and monitoring program adherence, is required.
Introduction
Urinary incontinence (UI) is the “complaint of involuntary loss of urine”1, with stress urinary incontinence Stress urinary incontinence being the most common type of UI reported during pregnancy2,3. SUI is the “complaint of involuntary loss of urine on effort or physical exertion (e.g. sporting activities), or on sneezing or coughing”1. During pregnancy, the mean SUI prevalence is 41%, ranging in the research from 19–75%2,4, and the rates increase with maternal age.
The mechanisms for developing SUI during pregnancy may include incompetence of the urethral sphincter and weakness of the pelvic floor muscles (PFM)4. Maternal weight gain may weaken the PFM by increasing intra-abdominal pressure, impairing blood flow, and altering neural innervation. Foetal weight may also cause weakness of the PFM by chronically stressing the muscles. There are known collagen and hormonal changes in pregnancy that will also impact the efficacy of the PFM, create urethral and ligamentous hypermobility, and impair urethral closing pressure5.
Pelvic floor muscle training (PFMT) is often advocated by health professionals as a measure to prevent SUI during pregnancy, although the research on its effectiveness is equivocal. For the purpose of this review, PFMT involves voluntary contraction of the PFM for one or more sets5. Usual care in preventing pregnancy-related UI involves education around lifestyle management, such as cessation of smoking, maintaining healthy weight, preventing constipation, and the introduction of PFMT and appropriate exercise participation for their training level6.
Bø and colleagues7(p121) proposed that the primary goal of PFMT was to improve the "…automatic co-contraction of the PFM to counteract any increase in abdominal pressure or ground reaction force". Increasing the hypertrophy of the PFM may help to elevate the pelvic floor and bladder resting positions and provide additional support to the pelvic organs. The PFM helps to maintain continence by providing closure support to the external urethral sphincter and the levator hiatus5,8. Given the mechanical and hormonal changes associated with pregnancy and the impact these have on the continence mechanisms, the aim of PFMT during pregnancy is to mitigate these effects where possible.
The purpose of this review was to explore the recent evidence for PFMT alone, or in combination with exercise, in the prevention of SUI during pregnancy, and to make recommendations on best-practice.
Literature search strategy
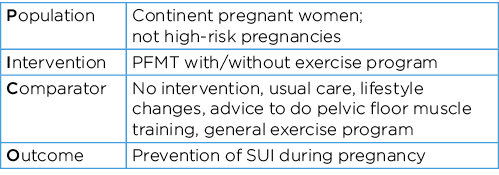
The participants, interventions, comparisons and outcomes (PICO) framework9 was used to guide the literature search strategy (Box 1).
Box 1. PICO framework
The search terms Pregnant OR pregnancy OR antenatal OR nulliparous OR multiparous (AND) “stress urinary incontinence” OR “urinary incontinence” OR “urinary leakage” (AND) “pelvic floor muscle training” OR “pelvic floor exercises” OR “Kegel exercises” OR “pelvic floor rehabilitation” were used to search five databases – Web of Science, Cochrane Library, CINAHL, Embase, PubMed. Articles were included if they were in the English language, published between the years 2014–2021, included pregnant women who were continent only, included a PFMT intervention to target the prevention of SUI or UI (if not distinguished from urge UI), and if the study design was a controlled clinical trial, cohort study, or a systematic review with or without meta-analysis. Articles were excluded if they were specific to urge UI rather than SUI, if they included participants with high-risk pregnancies, or if they included women who reported UI at baseline. A hand search of the available reference lists of included articles was also conducted.
The initial articles were selected by reviewing the abstracts and determining whether the contents were relevant to the proposed research question, were from a peer-reviewed journal source, and whether the study established a cause and effect relationship of PFMT in preventing SUI during pregnancy. Further analysis was done to determine the methodological quality of the papers, and then to group research papers based on the study design and whether the research focused on PFMT alone or in combination with exercise.
Results
Of the 433 documents identified in the search, 16 full text articles were assessed for eligibility and, following further assessment, three studies were excluded, leaving 13 studies to be included in the review3,5,8,10–19 –one meta-analysis12, four systematic reviews8,10,13,17, four reviews5,11,14,15, and four randomised controlled trials (RCTs)3,16,18,19. The search strategy according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)20 is shown in Figure 1.
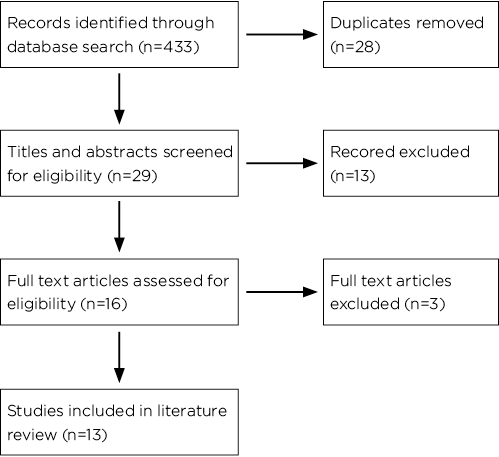
Figure 1. Search strategy PRISMA flowchart
Evidence for PFMT alone in the prevention of SUI during pregnancy
In a systematic review of 22 trials involving 8,485 women, Boyle and colleagues10 report that there was insufficient evidence on the effect of PFMT in prevention of SUI (RR 0.44, 95% CI 0.14–1.33), and positive effects were only observed in early postpartum. They conclude there was a greater effect on UI in more heavily supervised programs and those with effective dosing. Schreiner and collegues8 collated the results from 11 trials involving a total of 2,529 pregnant women and found mixed results of PFMT in the prevention of SUI during pregnancy, but demonstrated a positive effect, particularly in the larger more robust study designs. In a review paper of 10 trials involving 1,350 pregnant women, Soave and colleagues5 conclude that, despite the data showing that patients who were randomised to PFMT experienced 62% fewer symptoms of UI in late pregnancy, the studies were deemed to be of "low" quality and thus the authors contend that results should be interpreted with caution.
In a more recent review, Woodley and colleagues11 collated the results of six moderate-quality trials involving 624 women with an intervention of antenatal PFMT alone (compared to usual care) and report a 62% reduction in risk of developing UI in later pregnancy (95% CI 0.20–0.72). A meta-analysis by Lu and colleagues12, of 15 studies involving 1,615 women, reports a relative risk reduction of 29% (95% CI 0.622–0.816) in the PFMT intervention group compared to usual care and report statistically significant improvements in PFM strength as weighted mean difference (WMD: 8.448) and less urine leakage (WMD: –1.699) in the intervention group compared to usual care control. An earlier systematic review by Mørkved and Bø13 focused on three clinical trials involving 654 continent pregnant women and found statistically significant effects of PFMT in prevention of UI in pregnancy, despite heterogeneity of dosage, length of intervention, and follow-up.
Positive statistical trends in the prevention of UI during pregnancy using PFMT compared to controls are reported by Khorasani and colleagues14 who reviewed nine RCTs and Romeikienė and Bartkevičienė15 who reviewed 22 articles. However, both reviews only briefly mentioned the effects, with no reference to confidence intervals or risk reduction, and amalgamated pre- and post-partum results.
Two recent RCTs report positive effects of PFMT in the prevention of UI during pregnancy. A study of 60 continent pregnant women by Kahyaoglu Sut and Kaplan16 compared a control group of usual care to an intervention group consisting of 6 weeks of self-directed PFMT (3 times per day, 10 repetitions of 10-second holds) with fortnightly follow-up. The intervention group showed no change to UI symptoms and quality of life (QoL), while the control group showed a worsening of UI and QoL at 36–38 weeks. The authors, therefore, contend that PFMT during pregnancy had a protective effect against developing UI16. An RCT that involved 70 continent primigravid women3 compared an antenatal care control group (n=35) to a midwife-supervised PFMT program (n=35). The PFMT group was held for 6 weeks and included verbal instructions, three 45-minute training sessions plus daily self-directed PFMT. They found 9/35 women in the intervention group developed SUI at 38 weeks compared to 16/35 women in the control group (27% compared to 53%, OR 3.05, 95% CI 1.07–8.70).
Evidence for PFMT and exercise in the prevention of SUI during pregnancy
Three of the included studies observed the effect of PFMT and exercise together in the prevention of UI during pregnancy17–19. One systematic review by Davenport and colleagues17 concludes that PFMT alone saw a 37% reduction in prenatal and postnatal UI, compared to a 50% reduction if PFMT was done with aerobic exercise. Pelaez, and colleagues18 conducted an RCT comparing a control group receiving usual antenatal care with information about PFMT and an intervention group in which, over 22 weeks, participants did three sessions of 55–60 minutes of exercise each week run by exercise science graduates; each session included 10 minutes of PFMT. Those in the intervention group who reported never experiencing UI during their pregnancy were around 95%, compared to 61% in the control group (p<0.001). Szumilewicz and colleagues19 report an RCT involving 260 women that compared a group of continent pregnant women who were given an intervention of a 6-week high- and low-load exercise three times per week and PFMT, with a control group of continent pregnant women receiving usual care. While UI symptoms were only the secondary outcome measure assessed using a validated outcome measure (short form Incontinence Impact Questionnaire (IIQ-7)), results demonstrated statistically significant improvements in the intervention group for electromyography activity in the 3-second PFM lift (p<0.014), but no differences in the prevalence of UI after the 6-week intervention.
Limitations
A difficulty in assessing the literature is that many studies do not differentiate SUI and overactive bladder symptoms and report UI only, making it difficult to determine the effect of PFMT on the prevention of SUI alone. Clinically, this effect may not be significant for many pregnant women who just want to avoid UI altogether, but for research purposes, it is important to distinguish, particularly if one is more responsive to change with PFMT.
Only two studies reviewed report PFM strength measures12,19, and correct technique, if measured at all, was often deemed acceptable if participants could simply stop the flow of urine3. Without measuring PFM strength, the hypertrophy effect cannot be validated as the reason for the prevention of UI. Not assessing for correct technique may dilute results by including participants who might be adhering to the treatment protocol, but ineffectively training their PFM. This is perhaps a reasonable explanation as to why previous reviews5,8,10 did not assert the effectiveness of PFMT in the prevention of pregnancy-related SUI.
Among the studies reviewed there was also a large discrepancy in terms of dosage, and initiation of exercise intervention, making it difficult to determine the minimum clinically important difference to elicit a protective effect of PFMT. It could be concluded that, if the intervention group was under-prescribed PFMT in the study protocol, the reason for a lack of positive trend could simply be due to insufficient dosage.
There was ambiguity and a lack of consistency in measuring UI or SUI among the studies, with some studies using validated outcome measures11,19, some relying on self-reporting3,4,15,17, and some reporting a combination of outcome measures12,13.
Few studies measured and reported on adherence to PFMT in both the control and the intervention groups. Mørkved and Bø13 critically observed that if participants in the intervention group were not adhering to the program, we simply cannot determine the effect of PFMT. Furthermore, many of the papers reviewed report that studies discouraged control groups from doing PFMT10,18, but there was variability in measuring and reporting adherence13,17. Whilst not specifically stated in the research, there is the potential for diluting the effectiveness of PFMT observed in the intervention group if the control group is unknowingly participating in some form of PFMT also (especially given that usual care often includes advice on PFMT).
The last limitation, with potentially the largest implication for clinical practice, is the likelihood of PFMT in preventing SUI in pregnancy, presented in the research as odds ratio (OR: 0.44–0.63) and relative risk reduction (RRR: 0.38–0.712). It is difficult for a health professional or a private paying client to justify a preventative intervention that affords only a moderate protective effect, particularly when research supports frequently supervised sessions having a greater effect10 (with more frequent sessions incurring greater individual cost).
The review highlighted the need for research studies that have adequate dosage to achieve a training effect, measures PFM strength at baseline and post-intervention, uses consistent and validated outcome measures, and monitors adherence to PFMT programs. Perhaps then will the research show even greater relative risk reduction to be clinically justifiable to women, particularly in the private practice setting.
Recommendations for PFMT in pregnancy in the prevention of SUI
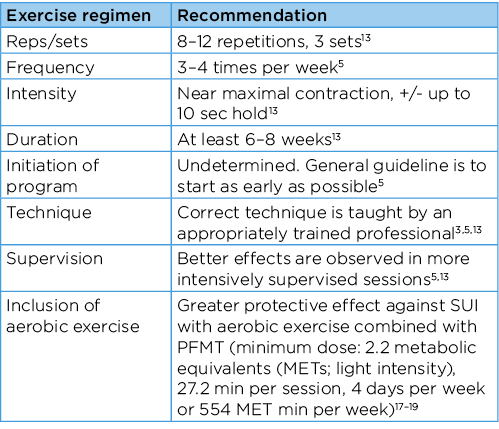
At present, there is no consensus in the literature or published protocol concerning the correct dose of PFMT in pregnancy, nor a minimum dose required for training effect5. The heterogeneity in dosage reported in the studies included in this review creates a challenge to determine effective training dosage. Based on the evidence in this review, Table 1 presents this author’s recommendations for a training protocol to prevent SUI during pregnancy. Previous research has shown that up to 30% of women are unable to voluntarily contract their PFM7, thus it is recommended that women should be taught the correct PFM contraction11 before commencing PFMT. The literature reviews that exist on PFMT in the prevention of SUI during pregnancy emphasise that under-dosing PFMT may result in inadequate training effect, and therefore no preventative effect on SUI5,13. Table 1 outlines training recommendations, provides a basis upon which to build a PFMT prevention program in the pregnant population, and presents an opportunity for further research.
Table 1. Recommendations for PFMT in pregnancy in the prevention of SUI
Implications for future research and current practice
SUI is a common complaint in late pregnancy due to various mechanical and hormonal changes, and PFMT is often advocated as a preventative measure. The research presented in this literature review demonstrated that while PFMT may prevent SUI during pregnancy, the strength of the effect remains equivocal. The protective effect of PFMT is strengthened when women are closely supervised and have sufficient training dosage to elicit PFM strength adaptations. Further research on PFMT interventions is needed to confirm the sufficient dosage to achieve a training effect, the PFM strength measured at baseline and post-intervention, and that monitoring adherence to PFMT programs would substantiate recommendation. There remains a significant opportunity for the multidisciplinary team to work collaboratively and in agreement with pregnant women who would like to be proactive in preventing SUI; any discussion must include PFMT wherever possible.
Author(s)
Alannah Turner
Department of Physiotherapy, School of Health Sciences,
The University of Melbourne, VIC, Australia
Conflict of interest
The author declares no conflicts of interest.
Funding
The author received no funding for this study.
References
- Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J: Incl Pelvic Floor Dysfunct 2010;21(1):4–20.
- Davidson MJ, Kruger JA. Prevalence of urinary incontinence during pregnancy: a narrative review. ANZ Continence J 2018;24(4):112–7.
- Sangsawang B, Sangsawang N. Is a 6-week supervised pelvic floor muscle exercise program effective in preventing stress urinary incontinence in late pregnancy in primigravid women? A randomized controlled trial. Eur J Obstet Gynecol 2016;197(1):103–10.
- Sangsawang B, Sangsawang N. Stress urinary incontinence in pregnant women: a review of prevalence, pathophysiology, and treatment. Int Urogynecol J 2013;24(6):901–12.
- Soave I, Scarani S, Mallozzi M, et al. Pelvic floor muscle training for prevention and treatment of urinary incontinence during pregnancy and after childbirth and its effect on urinary system and supportive structures assessed by objective measurement techniques. Arch Gynecol Obstet 2019;299(3):609–23.
- Abrams P, Cardozo L, Wagg A, Wein, A. Primary prevention, continence promotion, models of care and education (Chapter 21). Incontinence. 6th edition. ICI-ICS. International Continence Society: Bristol UK; 2017.
- Bø K,, Mørkved S. Pelvic floor and exercise science (Chapter 6). In Bø K, Berghmans B, Mørkved S, et al, editors. Evidence-based physical therapy for the pelvic floor: bridging science and clinical practice. 2nd edition. Churchill Livingstone/Elsevier: London; 2015.
- Schreiner L, Crivelatti I, de Oliveira JM, et al. Systematic review of pelvic floor interventions during pregnancy. Int J Gynecol Obstet 2018;143(1):10–18.
- Kloda LA, Boruff JT, Cavalcante AS. A comparison of patient, intervention, comparison, outcome (PICO) to a new, alternative clinical question framework for search skills, search results, and self-efficacy: a randomized controlled trial. J Med Libr Assoc 2020;108(2):185–94.
- Boyle R, Hay-Smith EJ, Cody JD, et al. Pelvic floor muscle training for prevention and treatment of urinary and fecal incontinence in antenatal and postnatal women: a short version Cochrane review. Neurourol Urodynam 2014;33(3):269–76.
- Woodley SJ, Lawrenson P, Boyle R, Cody JD, et al. Pelvic floor muscle training for preventing and treating urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Systemat Rev 2020, Issue 5. Art. No.: CD007471.
- Lu J, Zhang H, Liu L, Jin W, et al. Meta-analysis of perinatal pelvic floor muscle training on urinary incontinence. West J Nurs Res 2020;43(6):597–605.
- Mørkved S, Bø K. Effect of pelvic floor muscle training during pregnancy and after childbirth on prevention and treatment of urinary incontinence: a systematic review. Br J Sports Med 2014;48(4):299–310.
- Khorasani F, Ghaderi F, Ahadi P, et al. Physiotherapy and pelvic floor muscle exercises for the prevention and treatment of pregnancy-related pelvic floor dysfunctions: a systematic review and meta-analysis. Int J Women’s Health Reprod. Sci 2020;8(2):125-32.
- Romeikienė KE, Bartkevičienė D. Pelvic-floor dysfunction prevention in prepartum and postpartum periods. Medicina (Kaunas) 2021;57(4).
- Kahyaoglu Sut H, Balkanli Kaplan P. Effect of pelvic floor muscle exercise on pelvic floor muscle activity and voiding functions during pregnancy and the postpartum period. Neurourol Urodynam 2016;35(3):417–22.
- Davenport MH, Nagpal TS, Mottola MF, et al. Prenatal exercise (including but not limited to pelvic floor muscle training) and urinary incontinence during and following pregnancy: a systematic review and meta-analysis. Br J Sports Med 2018;52(21):1397–404.
- Pelaez M, Gonzalez-Cerron S, Montejo R, et al. Pelvic floor muscle training included in a pregnancy exercise program is effective in primary prevention of urinary incontinence: a randomized controlled trial. Neurourol Urodynam 2014;33(1):67–71.
- Szumilewicz A, Kuchta A, Kranich M, et al. Prenatal high-low impact exercise program supported by pelvic floor muscle education and training decreases the life impact of postnatal urinary incontinence: a quasiexperimental trial. Medicine 2020;99(6):e18874.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol 2021;134:178–89.