Volume 28 Number 4
Abstracts UroGynaecological Society of Australasia Annual Scientific Meeting, Sydney 21-24 September 2022
DOI https://doi.org/10.33235/anzcj.28.4.89-94
For full abstract program contact UGSA www.ugsa.com.au
Subjective outcomes of pain following Tension Free Vaginal Tape Surgery – a 10 year follow up survey
Smith H & Short J
Christchurch Women’s Hospital, Christchurch, New Zealand
Introduction: Stress urinary incontinence (SUI) is a common condition, affecting 10-20% of adult women1. Mid-urethral slings (MUS) are a widely studied and effective surgical procedure for the treatment of SUI. The self-reported subjective cure rate following MUS is 83.3% within 12 months, and 86.9% at 1-5 years2. There is limited data regarding long term efficacy; however, the cure rate appears to remain high2.
In recent times, MUS procedures have been placed under scrutiny, in association with enquiries into adverse outcomes associated with mesh implants for pelvic organ prolapse. Complications, that may necessitate removal of the prosthesis include mesh erosion, which is reported in 2.09% of cases2, and pain. There is limited data regarding the persistence of long-term pain; however, the rate is likely low, affecting 1% or fewer women more than six months after surgery3.
The aim of this study was to assess subjective long-term rates of pain for women who have undergone a MUS procedure for management of stress urinary incontinence.
Materials & method: All women who underwent a MUS procedure, performed by a gynaecologist, at a tertiary centre in New Zealand in 2009-2010 were identified through a clinical records search. A de-identified survey with covering letter was posted to participants’ most recent home address, with a return addressed postage paid envelope included. Participants were requested to return the survey within 28 days.
The survey consisted of 10 questions. Three questions were from the ICS Incontinence Questionnaire-Urinary Incontinence Short Form validated questionnaire to assess current symptoms. Four questions assessed pre- and post-operative symptoms including pain, one reviewed additional post-operative treatments and two assessed overall satisfaction regarding the procedure. The survey took approximately 10 minutes to complete.
The primary outcome measure was development of new reported pain following the MUS procedure. The secondary outcome measure was overall satisfaction with the procedure.
Results: From the records search, 150 participants were identified; 15 were excluded do to 11 deceased and 4 had no documented postal address. A total of 135 surveys were distributed, with a response rate of 50.4% (n=68).
Seven (10.3%) respondents reported development of pain following their MUS procedure. Six respondents were followed up and offered a clinical assessment of the nature of their symptoms, and of those one was uncontactable. Four women reported pain symptoms unrelated to the MUS procedure due to; e.g. lichen sclerosis, vaginal atrophy, levator myalgia and short episodes of self-limiting pelvic pain. Two respondents reported new onset of pain experienced, a complication necessitating mesh removal. Both had a history of two MUS procedures prior to symptom onset. The uncontactable patient indicated in her survey response that no further treatment was needed following the procedure. The revised rate of long-term pain secondary to MUS procedure was 2/68 (2.9%)
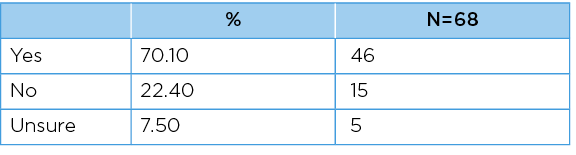
Of the respondents, 49 (73.1%) reported the MUS procedure was successful in improving symptoms of stress urinary incontinence, and 46 (70.1%) that they would recommend the MUS procedure to a friend.
Table 1: Respondents opinions regarding whether the MUS procedure was successful
in improving symptoms of stress urinary incontinence.
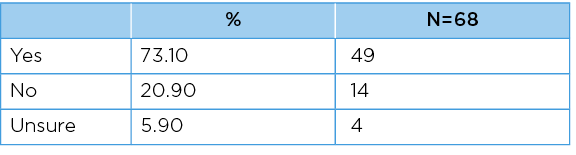
Table 2: Respondents opinion regarding whether they would recommend
a MUS procedure to a friend.
This survey of long-term outcomes for women who underwent a MUS procedure shows a 2.9% rate of chronic pain likely caused by the sling procedure itself. The women reporting persistent pain following MUS procedure both underwent two MUS procedures. This indicates that a repeat procedure may be a risk factor for the development of chronic pain and this should be taken into account when assessing patients with recurrent stress urinary incontinence after an MUS procedure. This survey suggests that the rate of persistent pain following a single MUS is low.
The initial rate of long-term pain reported by survey respondents was 10.3%. On further review, the majority (4/7) were found to have alternative causes for pain, not related to the MUS procedure. This highlights a difficulty with surveys of patient-reported outcome measures in accurately gathering information and reminds us to be cautious when interpreting results.
The rate of long-term satisfaction with the MUS procedure is high, with >70% of respondent’s replying positively to the survey questions assessing this.
Conclusions: This study was a cross-sectional survey with a 10-year follow up. The strength of this study is the ability to assess long-term subjective outcomes in this group of women. Weaknesses include recall and non-response bias. In addition, there is loss to follow up, with a 50.4% response rate, and a small number of women being uncontactable to include in this research. This loss to follow up, as well as the previously mentioned risk of bias that is inherent in survey research, supports the establishment of a prospective registry to record and follow up outcomes of MUS procedures.
References
- International Urogynecological Association. Stress Urinary Incontinence. https://www.yourpelvicfloor.org/conditions/stress-urinary-incontinence/ Accessed October 2021.
- Ford AA, Rogerson L, Cody JD, et al. Mid-urethral sling operations for stress urinary incontinence in women. Cochrane Database of Systematic Reviews 2017, Issue 7: Art. No.: CD006375.
- Medicines and Healthcare Products Regulatory Agency. A summary of the evidence on the benefits and risks of vaginal mesh implants. 28 October 2014. URL https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/402162/Summary
_of_the_evidence_on_the_benefits_and_risks_of_vaginal_mesh_implants.pdf
Outcomes from the first 100 pelvic mesh removal surgeries at the Queensland Pelvic Mesh Service
Hasted T, Krause H, Mowat A, Dr Yu Hwee Tan Y, Wong V, Frazer M & Goh J
Queensland Pelvic Mesh Service, Varsity Lakes Day Hospital, Varsity Lakes, Gold Coast, QLD, Australia
Introduction: Pelvic mesh (PM) was an approved surgical treatment for stress urinary incontinence (SUI) and pelvic organ prolapse (POP) in women. However, it has been associated with numerous complications leaving some women debilitated, out of work and suffering from poor quality of life1,2. Documented post-operative adverse events or complications include (but are not limited to) mesh erosion, bleeding, infection, pain, organ perforation, dyspareunia, recurrent prolapse and vaginal scarring3-6. Internationally, this has triggered a number of lawsuits and government-initiated inquiries. At the conclusion of the national senate inquiry, it was recommended that specialist multidisciplinary units for the assessment and management of PM related complications be established7. In response, a state-wide multidisciplinary service was established at our tertiary institution in 2019 to provide clinical assessments, medical treatments, surgical intervention, chronic pain management, psychological care, physiotherapy and social work support. Units similar to ours are being established around the world but to date little has been published from these units with respect to what implants are being removed and why, surgical approaches, complications, success rates and the patient experience.
Objectives: Our prospective study aimed to:
1) Record and better understand the experience of women with PM related complications
2) Assess outcomes following management
Materials & methods: Our mixed methods study employed validated questionnaires aimed to assess severity of patient symptoms, quality of life and impression of improvement. Patients were invited to complete questionnaires at baseline, during and post treatment. We have collected data related to the first 100 patients who underwent partial or complete mesh excision surgery in our service. Each patient’s symptoms, demographics and comorbidities were recorded in standardised interviews. Findings from examinations and cystoscopies were recorded.
Our surgical technique for removing various types of mesh have been documented. We used the Clavien-Dindo classification to record surgical complications. Histological and microscopy results from surgical specimens were collected. Standardised phone interviews were undertaken between 6-24 months post-operatively.
Results: Patient satisfaction and impression of improvement is being analysed and compared between patients who have had different:
– implants
– main symptoms (e.g., dyspareunia, groin pain, pelvic pain, recurrent urinary tract infections, voiding dysfunction, bleeding, autoimmune conditions)
– examination findings (e.g., mesh erosion, tenderness at mesh sites, pelvic floor tenderness, interstitial cystitis).
Follow-up phone interviews and analysis will be completed by December 2021. Provisional results suggest most patients are happy they have had surgery, but satisfaction and degree of symptom improvement varies depending on presenting symptoms and their perceived severity, examination findings, baseline continence and post-operative continence. Serious surgical complications are rare. Histological and microscopy results vary.
Conclusions: Our study captures the experiences, perceptions and symptoms of women on entry to our unit, during their care and post-operatively.
The findings from this study will be useful to other clinicians in patient selection for surgery and may inform how they counsel women around what they might expect after mesh removal.
References
- Besser L, Schwarzman P, Mastrolia SA, et al. Comparative analysis of early adverse events of pelvic organ prolapse repair with or without transvaginal mesh using Clavien-Dindo classification. International Journal of Gynecology & Obstetrics. 2018; 142(1): 108-13.
- Mazloomdoost D, Pauls RN, Kleeman SD, et al. Outcomes and Characteristics of Patients Undergoing Surgical Management for Mesh Related Complications. Female Pelvic Medicine & Reconstructive Surgery. 2018;24(1):32-8.
- Cundiff GW, Quinlan DJ, van Rensburg JA, et al. Foundation for an evidence-informed algorithm for treating pelvic floor mesh complications: a review. BJOG: An International Journal of Obstetrics & Gynaecology. 2018;125(8):1026-37.
- Hammett J, Peters A, Trowbridge E, et al. Short-term surgical outcomes and characteristics of patients with mesh complications from pelvic organ prolapse and stress urinary incontinence surgery. International Urogynecology Journal. 2014;25(4):465-70.
- Barski D, Otto T & Gerullis H. Systematic review and classification of complications after anterior, posterior, apical, and total vaginal mesh implantation for prolapse repair. Surgical Technology International. 2014;24:217-24.
- Abed H, Rahn DD, Lowenstein L, et al. Incidence and management of graft erosion, wound granulation, and dyspareunia following vaginal prolapse repair with graft materials: a systematic review. International Urogynecology Journal. 2011;22(7):789-98.
- Commonwealth of Australia. Number of women in Australia who have had transvaginal mesh implants and related matters. Canberra, ACT: Senate Community Affairs Committee Secretariat; 2018.
Australian health care professionals’ beliefs and attitudes towards the management of chronic pelvic pain: a cross-sectional survey.
Chan E1, Hart M2, Vardy J3, Dallin R4, Wise E5, Karantanis E6 & Beales D5.
1. Department of Physiotherapy, St George Hospital, Kogarah, NSW, Australia
2. Department of Physiotherapy, King Edward Memorial Hospital, Perth, WA, Australia
3. Department of Physiotherapy, Eastern Health, Melbourne, VIC, Australia
4. Body Sense Physiotherapy, Joondalup, WA, Australia
5. Curtin School of Allied Health, Curtin University, Perth, WA, Australia
6. The University of New South Wales, Sydney, NSW, Australia
Department of Obstetrics and Gynaecology, St George Hospital, Kogarah, NSW, Australia
Introduction: The objective was to comparatively document the current beliefs and practice behaviours of health care professionals; physiotherapists, gynaecologists, and general practitioners (GPs) in the management of chronic pelvic pain (CPP) in Australian women.
Materials & method: A cross-sectional online survey study of health care professionals (HCPs). A 19-question survey focused on beliefs and practice behaviours in the management of CPP was distributed nationally in Australia between June-July 2021.
Results: In total, 446/538 responses were included for statistical analysis, including 75 gynaecologists/urogynaecologists, 184 GPs and 187 physiotherapists. Most of the respondents were female (88.1%) with male (11.7%) and other (0.2%). All three professions rated patient’s beliefs (89.8%), nervous system sensitisation (85.7%), stress/anxiety/depression (91.9%), fear avoidance (83.3%), history of sexual/emotional/physical abuse (94.1%) and pelvic floor muscle overactivity (85.0%) as very or extremely important factors in the development of CPP. Most gynaecologists/urogynaecologists (71.0%) and GPs (70.2%) always referred for pelvic ultrasound when assessing CPP. Physiotherapists assessed goal setting (88.8%) and screened for patients’ beliefs (80.9%) more often than gynaecologists/urogynaecologists (30.4%, 39.1%) and GPs (46.5%, 29%).
Conclusion: All three groups of HCPs demonstrated a good understanding of pain mechanisms and incorporated a biopsychosocial approach to assessment and management of women with CPP. The responses from all three groups of HCPs aligned with guideline recommended care.
Outcomes after different number of injection sites and concentrations of intravesical Onabotulinum Toxin A
Young N1, McGauran M1,2, Alexander J3, Murray C4, Carswell F & Schierlitz L4.
1. Department of Obstetrics & Gynaecology, Mercy Hospital for Women, Melbourne, Victoria, Australia
2. Department of Obstetrics & Gynaecology, University of Melbourne, Victoria, Australia
3. Department of Urogynaecology, Royal North Shore Hospital, NSW, Australia
4. Department of Urogynaecology, Mercy Hospital for Women, Melbourne, Victoria, Australia
Introduction: Overactive bladder, with or without urge urinary incontinence, affects 17% of women worldwide, and has a detrimental impact on overall quality of life and health-related consequences1,2. Onabotulinum Toxin A (Botox®) is approved for the treatment of refractory overactive bladder and is safe and effective. There is limited data on the optimal dilution and number of injection sites of Botox. It has been previously demonstrated in studies of Botox® injection sites other than the bladder, that lower concentration and larger volume increases diffusion of Botox® 3.
The aim of this research was to examine local practice regarding the technical aspects of the procedure including dose, dilution and number of injections administered and the impact of variations in administration protocols on efficacy and complications.
Materials & methods: This is a single centre retrospective cohort study which examined the use of Botox® for refractory idiopathic overactive bladder (OAB) and interstitial cystitis (IC). A database was formed including all patients who received intravesical Botox® treatment in both outpatient and inpatient settings at the Mercy Hospital for Women, Heidelberg, between 2016 and 2021. Medical records were reviewed to collect patient demographics, medication use, urinary symptoms, and the technical aspects of Botox® procedures. The primary outcome of the study was time-to-return of symptoms. The secondary outcome was the presence of voiding dysfunction.
Results: 280 episodes of Botox administration across 133 patients were analysed. 100 units of Botox® was administered in all patients. From the available data, this was diluted in 10mL of saline in 112 patients (43.9%), 20mL in 100 patients (39.2%) and 30mL in 43 patients (16.9%). Botox® was administered across 10 injections sites in 77 patients (29.4%), 20 injections in 143 (54.6%) and 30 injections in 42 (16%). Days to symptom recurrence were recorded, with an overall mean time to symptom recurrence of 194.52 days (SD 148.76). There was a trend towards increasing days to symptom recurrence with increased number of injections, with a median time of 126.5 days (IQR 153.75) for 10 injections, 159 days (IQR 193.5) for 20 injections, and 284 days (IQR 133) for 30 injections. Increased volume of dilution also showed a similar trend, with 141.5 days (IQR 147.5) for 10mL, 165 days (IQR 165.5) for 20mL, and 260 days (IQR 124.75) for 30mL dilution. There was a statistically significant correlation between number of injections and days to recurrence (beta co-efficient 0.412, p<0.001) and volume of dilution and days to recurrence (beta co-efficient 0.318, p<0.001). Clean intermittent self-catheterisation for voiding dysfunction was required in 42 patients (15.8%). Urinary tract infections occurred in 25 patients (9.4%).
Conclusions: A trend towards increased time to return of symptoms associated with increased number of injections and increased dilution of Botox® was observed. The authors believe this trend would be worth exploring through a prospective study design to better understand how outcomes may be optimised in women being treated with intravesical Botox® for OAB and IC.
References
- Stewart WF, Van Rooyen JB, Cundiff GW, et al. Prevalence and burden of overactive bladder in the United States. World Journal of Urology. 2003; 20(6): 327-336
- Wagner TH, Hu T, Bentkover J, et al. Health related consequences of overactive bladder. American Journal of Managed Care. 2002; 8(19 Suppl): 5598-607.
- Hsu TSJ, Dover JS & Arndt KA. Effect of volume and concentration on the diffusion of Botulinum Toxin A. JAMA Dermatology; 2004; 14(11): 1351-1354
Mode of delivery following OASI: a 7-year retrospective review and follow up cohort survey
Young R, Bates L & King J
Westmead Hospital, Sydney, NSW, Australia
Introduction: The object of this study1 was to describe mode of delivery outcomes for women following obstetric anal sphincter injury (OASI); to review the grades of tear, endoanal ultrasound (EAUS) findings, and subsequent delivery outcomes; and long-term symptoms on follow up.
Materials & method: This study was conducted in two parts. The first stage involved a retrospective review of all cases of OASI at a tertiary hospital in Australia over a 7-year period (2013 – 2019) where the patient underwent a subsequent delivery in this unit. Notes were reviewed to classify the severity of the index tear; results of follow up endo-anal ultrasound; St Marks score at the time of ultrasound; the management plan made during subsequent pregnancies; and factors that may have influenced mode of delivery (e.g., labour prior to booked caesarean section, caesarean section due to foetal distress, SGA or breech). Following this, we undertook a retrospective cohort survey, inviting the 247 women who experienced OASI to complete a survey. This was done via post, telephone, or online, as per patient preference.
Results: Of 27,284 vaginal births, 828 women experienced OASI (3.03%), of which 86.6% had been nulliparous. Of these, 247 (29.8%) had at least one documented subsequent birth by January 2021 at the unit and 29 (3.5%) had two to four subsequent deliveries. As part of follow up on the index OASI, 81% had an EAUS at our institution by a single operator, of which the majority were normal (92.5%, 185/200). Those with a residual defect at EAUS were more likely to have a caesarean for all subsequent deliveries (53%) than if EAUS was normal (23.8%). A persistent defect was more likely following 3C/4th degree tears (24%) than after 3A/B tears (5.2%). Of those with a subsequent vaginal delivery (68% of deliveries), there was a recurrent OASI rate of 5.4% (9 patients) and 5 had both a caesarean and vaginal delivery.
There were 90 discrete responses (36.4% response rate) to the follow up survey. Only 88 responses were able to be linked with information from the patient notes, as two participants did not enter their unique participant identification code in their online response. Of the 88 respondents, 68% had vaginal births for all subsequent deliveries. Follow up EAUS was performed in 87.5%; none demonstrated a persistent defect. Only 34% recalled being counselled on future deliveries at the time of OASI; 63% recalled counselling during their subsequent pregnancy. Vaginal delivery was the preferred mode of delivery in 77.8%. The majority had high levels of satisfaction with the mode of delivery that occurred (75.6% scoring 8 or greater on a Likert scale of 0-10 and only 4.4% scoring 4 or less). Satisfaction was slightly higher in the caesarean section group than vaginal delivery group (82% scoring 8-10 vs 71.7%). Participants were asked to comment on reasons for their levels of satisfaction. Responses indicated that this corresponded more with the communication that was received and how supported or listened to women felt, rather than the mode of delivery itself.
Faecal or flatus incontinence was reported in 17.8% after the index delivery; 12% have had these symptoms since. Of those who had only vaginal births 10% reported symptoms after the index delivery; 15% since. Of those who had only caesarean sections since OASI, 29.6% reported faecal or flatus incontinence prior to their last delivery but only 7.4% since. Our results may be impacted by the low numbers followed up. A St Mark’s incontinence score was performed. There was no statistically significant difference between scores for those having had vaginal deliveries vs caesarean sections when compared with a two-tailed T-test (p = 0.59). One participant in the follow up cohort had a recurrent OASI (3A followed by 3C tear) and reported being asymptomatic with a St Mark’s incontinence score of 1. Of those surveyed 7 participants had sustained a 3C/4th degree tear – of these only one had a subsequent vaginal delivery. None reported faecal/flatus incontinence symptoms.
Conclusions: In our Unit, most women who sustain OASI will go on to have a subsequent vaginal delivery in future pregnancies. Overall, this was their preferred mode, however, those who were surveyed that underwent caesarean section also had high satisfaction rates. The majority remain asymptomatic at long term follow up. There were no statistically significant differences in incontinence scores between women who had vaginal deliveries vs those having caesarean sections only for subsequent births. The rate of recurrent OASI of 5.4% was comparable to that in the existing literature.
Reference
- Young R, Bates L, The S, et al. Mode of delivery following obstetric anal sphincter injury: a 7-year retrospective review and follow-up cohort survey. Int Urogynecol J. 2022; https://doi.org/10.1007/s00192-022-05294-3