Volume 28 Number 4
Telehealth continence education classes: a feasible alternative to in-person classes
Marielle Collings and Robyn Brennen
Keywords education, incontinence, telehealth, women, conservative
For referencing Collings M & Brennen R. Telehealth continence education classes: a feasible alternative to in-person classes. Australian and New Zealand Continence Journal 2022; 28(4):84-88.
DOI
https://doi.org/10.33235/anzcj.28.4.84-88
Submitted 1 August 2022
Accepted 31 October 2022
Abstract
Due to the COVID-19 pandemic, many group education sessions provided by healthcare services during 2020 were transitioned to telehealth. Research evaluating the delivery of group continence education via telehealth is limited. To investigate the feasibility of telehealth continence education, we conducted a retrospective audit of telehealth classes from July to December 2020 and in-person continence education classes from July to December 2018. We compared client attendance to classes, demographic data including age and distance lived from the clinic, feedback survey responses, and time spent by staff organising and conducting the classes. Quantitative data were analysed using descriptive statistics. Qualitative survey responses were analysed to identify key feedback. The non-attendance rate for the telehealth classes was 32% (n=13) compared to 35% (n=26) for the in-person classes. Feedback for the telehealth classes was positive, with 73% of survey respondents agreeing or strongly agreeing that it was easy to join the session. All respondents agreed or strongly agreed that the telehealth classes were interesting compared to 94% of respondents for the in-person classes. Lack of access to, or familiarity with, technology were limiting factors for telehealth class attendance. Telehealth therefore appears to be a feasible modality for the delivery of continence education classes, with comparable attendance rates to in-person classes. However, access to technology may be a barrier to attendance for some clients and telehealth classes may be more time consuming for clinicians.
Introduction
In the context of the COVID-19 pandemic and public health directives, many in-person services offered by Australian public healthcare providers were suspended1. Healthcare services rapidly adopted the use of telehealth to provide care during this period2. Telehealth can be described as the “…delivery of clinical health services using information and communication technologies to bridge the geographic separation of the clinician and consumer”3. The results of a survey of Australian allied health practitioners demonstrates the limited utilisation of telehealth prior to the pandemic – only 18% of surveyed allied health clinicians had previously used telehealth4.
At a specialist, multidisciplinary community continence service in Melbourne, Australia, physiotherapist-led group classes are provided as part of a standard model of care. Group continence education classes provide clients with information about self-management strategies while they are awaiting their first appointments and thus reduce waiting times for clients to access such information5. These classes were transitioned to telehealth in response to the pandemic. Previous case reports have suggested that telehealth may be an effective tool for the management of women experiencing incontinence6; however, research evaluating the delivery of group continence education classes via telehealth is lacking. Our aim was to compare the feasibility of telehealth continence education classes to in-person continence education classes. Secondary outcomes included client satisfaction with telehealth classes, attendance to both in-person and telehealth classes, and the comparable time taken to conduct both classes.
Methods
Participants
A retrospective audit of data from continence education classes was conducted. Data from telehealth classes which ran from July to December 2020 and in-person classes which ran from July to December 2018 were analysed. All clients triaged to the classes during these time periods were included in the analysis. Clients were triaged to the group education classes at the point of referral if they were female and English-speaking. Clients were excluded from the in-person education classes if they had co-morbidities or circumstances which would prevent them from attending an in-person class at the clinic (such as a mobility limitation) or implementing the self-management techniques provided in the classes, such as a cognitive impairment. The inability to attend an in-person class at the clinic was not an exclusion criterion for the telehealth classes. Clients who were triaged to the classes in the 2020 period were contacted by telephone to ensure they had the ability to attend a telehealth session. Figures 1 & 2 outline the processes from point of referral for the in-person and telehealth classes respectively.
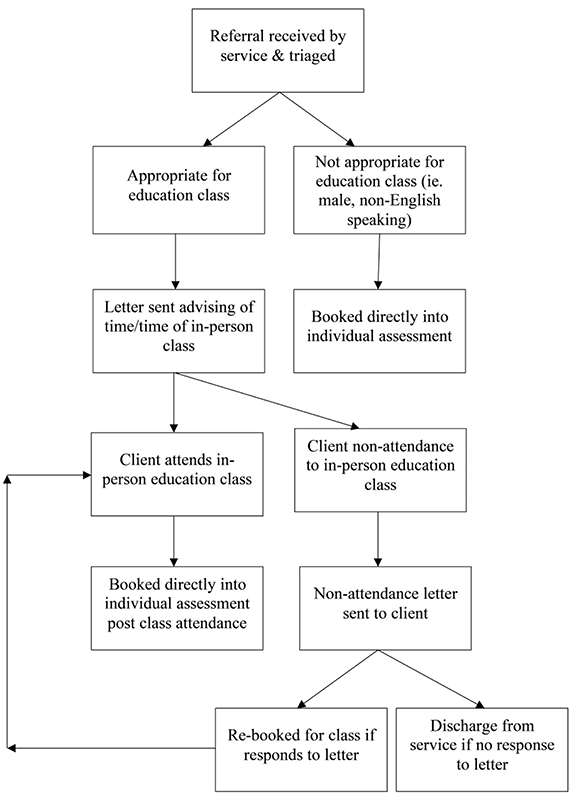
Figure 1. Flow chart outlining the processes for the in-person classes from point
of referral to class attendance or non-attendance
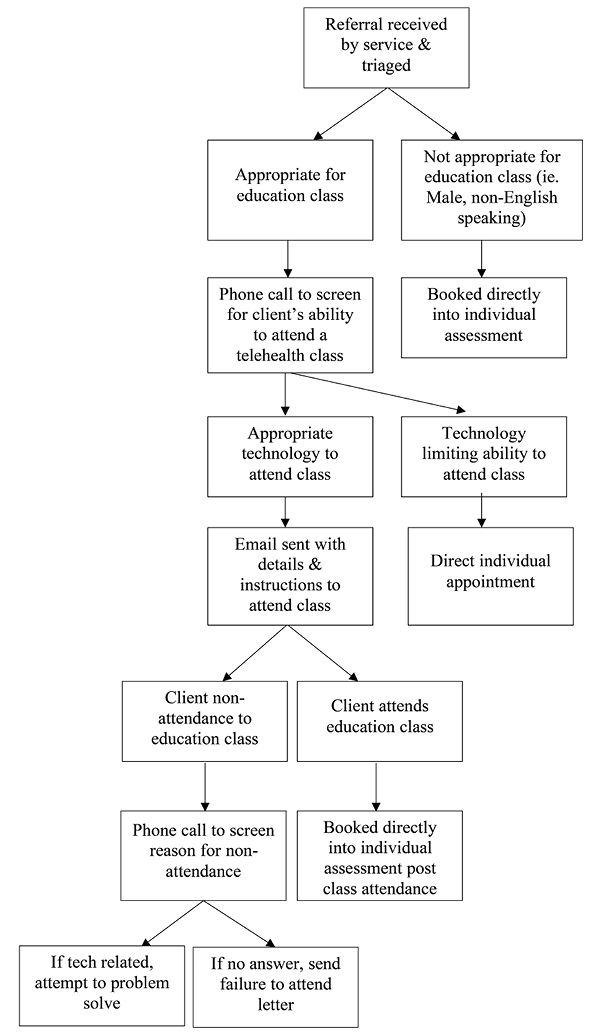
Figure 2. Flow chart outlining the processes for the telehealth classes from point of
referral to class attendance or non-attendance
Data collection
Demographic data on clients allocated to group education sessions was obtained from patient records. This included client age and residential address. Residential addresses were then used to calculate the straight-line distance clients reside from clinics, using 'how far is it?' distance calculator software. Class participants routinely provided feedback on the classes via a five-point Likert scale, with the option to provide long form additional feedback at the end of the survey. This survey was implemented within the service from December 2018. Due to missing data, in-person class feedback surveys were analysed for this study from December 2018 to February 2019. Telehealth class survey responses from July to December 2020 classes were analysed. Attendance to telehealth classes and telehealth feedback survey responses were extracted from telehealth software. Attendance records to in-person classes were accessed from clinic scheduling software.
To run the classes, staff were required to contact and allocate clients to classes, complete clinical questionnaires with clients, set up the telehealth software, conduct the classes, attend to the required documentation after the class, and book initial assessment appointments for the clients. The total time taken by staff to complete the above tasks for classes was retrospectively estimated, with comparisons to scheduled diaries and clinic data were used to support these estimations.
Data analysis
All quantitative data were analysed using descriptive statistics. Additional long form comments from telehealth class survey responses were analysed. The primary investigator identified key feedback from the responses which were then cross checked by the co-investigator.
Ethics
This audit was approved by the Monash Health Research Office as a quality project, consistent with the NHMRC Ethical Considerations in Quality Assurance & Evaluation Activities (2014) guideline. HREC Reference Number: QA/73114/MonH-2021-250478(v1).
Results
In the 2020 referral period, the service received 427 referrals; 46 clients (11%) met the inclusion criteria to attend the telehealth class. Nine clients triaged to the telehealth class in the referral period were not allocated to the class due to limitations with technology. In the equivalent baseline period, the service received 579 referrals; 75 clients (13%) were eligible for the in-person classes (Table 1).
Participant demographics
The median age of clients who attended telehealth classes was slightly younger, at 58 years of age compared to 69 years for the in-person classes. The median age of clients who failed to attend was 61 years for the telehealth classes and 63 years for the in-person classes (Table 2). The median distance clients lived from the clinic was higher in the telehealth attendees (8km) than the in-person attendees (6km). The median distance for clients who failed to attend the classes was similar in each group (8km). The non-attendance rate for the telehealth classes was 32% (n=13) compared to 35% (n=26) for the in-person classes.
Participant feedback
Eight clients completed the feedback survey for the telehealth classes, with six of these clients including additional long form comments. A total of 17 clients completed the feedback survey for the in-person class, including one client who only partially completed the survey. A total of 73% of survey respondents agreed or strongly agreed that it was easy to join the telehealth session. All respondents agreed or strongly agreed that the telehealth classes were interesting compared to 94% of respondents for the in-person classes.
The additional feedback was analysed to identify key feedback – difficulty with technology, quality of presentation and appreciation of class.
Key feedback 1: Difficulty with technology
Participants reported having issues using the technology, evidenced by quotes such as “I struggled to login” and “I’m not really savvy… with all things electronic”. Participants also seemed to struggle with the quality of audio-visual components of the class, for example, “… I managed to lose visual but had audio”.
Key feedback 2: Quality of presentation
Feedback regarding the quality of the presenter was mixed – “wonderful approach delivering information and addressing participants” and “the presenter talks a little bit too fast”.
Key feedback 3: Appreciation of class
Despite the above feedback, participants reported that they valued the telehealth format, for example “I would like to see more of this kind of training sessions [sic] from now on”. They were also grateful for the content of the sessions, “think [sic] incontinence clinic” and “your support is greatly appreciated”.
Staff time
Eleven telehealth classes were conducted during July to December 2020 and an estimated total of 55 staff hours (approximately 5 hours per class) were dedicated to organising and running the classes during this time. Nine in-person classes were conducted during the 2018 period and an estimated 27 staff hours (approximately 3 hours per class) were dedicated to organising and running the classes.
Discussion
This study evaluated the feasibility of telehealth group education classes for women experiencing incontinence. In this audit, the percentage of referrals triaged to classes was comparable across the two time periods. A total of 20% of clients triaged to the telehealth class were unable to attend due to limitations with technology. This is consistent with previous research which has identified acceptance of technology and the technological ability of patients as major barriers to telehealth4,7,8. There may also be a correlation between the ages of clients who have the capability to attend a continence telehealth education class as the median age of attendees to the in-person class was higher. Banbury et al identified that older clients may have difficulties logging into telehealth group sessions or overcoming technical difficulties during sessions due to limited technological skills7.
It was hypothesised by the investigators that there would be a higher rate of non-attendance to the telehealth classes compared to in-person classes due to the additional barrier of technology. However, in this review, clients were screened for their technological capabilities prior to being booked into the telehealth class. This may account for the comparable non-attendance rates across in-person and online classes in this study, as clients who may have failed to attend due to technology were not allocated to this class.
However, while technology may be a barrier to attendance, telehealth may be more convenient for some clients, such as those who live remotely, have work commitments, are required to look after children, have mobility limitations or are immunocompromised4,7. This was reflected in the feedback from a participant in the telehealth class who identified that telehealth sessions were particularly helpful for clients with mobility problems or who are immunocompromised. In our study, attendees to telehealth classes lived slightly further away from the clinics compared to attendees to in-person classes; however, the potential distance would have been limited by the specific catchment area from which our clients are accepted. Previous studies indicate that telehealth services may reduce the tyranny of distance4,7 and future studies should investigate the provision of telehealth classes to clients living regionally and remotely.
Feedback for the content of the two classes was positive and a large portion of survey respondents reported that it was easy to join the telehealth session. This feedback is consistent with findings in the Australia-wide survey by Filbay and colleagues who found that 85% of clients who received group allied health sessions via telehealth were somewhat or very satisfied with the services they received and 81% of clients found the technology somewhat or very easy to use4.
Despite only being allocated to telehealth classes if participants self-reported the ability to attend, 27% of survey respondents disagreed that it was easy to join the telehealth session and issues with technology was a key theme which emerged from thematic analysis of survey comments. Filbay and colleagues found that 18% of clients who attended group allied health telehealth sessions reported technical or internet issues4. Joining the telehealth class and issues with the audio-visual components of the session were the elements participants reported struggling with the most. However, the individual reasons participants may have identified these issues were not explored further in this study. It is possible participants were impeded by the quality of their internet connection, the usability of the telehealth software, or the participants'4 overall technological literacy. Filbay and colleagues reported internet troubles to be a more common concern during individual consultations than clients finding telehealth technology hard to use; more than 75% of clients in their study who utilised telehealth reported confidence using technology. Despite this, other clients appeared to value the format of the telehealth class which is consistent with findings of Filbay and colleagues who reported that a large portion of clients found group allied health telehealth sessions to be effective and convenient4.
Based on the analysis of staff diaries during the two time periods, telehealth classes may require a larger time commitment from staff compared to the in-person classes. This is likely due to the additional tasks associated with running the telehealth classes, such as telephone screening clients to determine their technology ability and setting up telehealth software. In their scoping review, Snoswell and colleagues concluded that telehealth models of care do not always reduce healthcare costs, particularly in the short- to medium-term3. They also found conflicting evidence regarding the efficiency of substituting in-person services with telehealth services and identified that an increased administrative workload associated with telehealth may offset any clinical efficiencies gained3. This may be relevant to the model of care utilised in this study. However, the overall benefits of improved attendance rate to initial appointment demonstrated in our previous work5 may outweigh the cost of increased administrative workload. Further evaluation and refinement of the telehealth class model of care utilised in this study are warranted due to the increased financial and time commitments associated with telehealth classes.
Possible strategies to reduce the workload on clinicians could be to phase out telephone screening of clients or to delegate administrative tasks to allied health assistants or reception staff. Recorded classes may also be a possibility; however, client attendance and engagement in the recording would need to be monitored in-order to maintain high attendance rates to first appointment.
Conclusion
Based on the findings of this audit, telehealth appears to be a feasible modality for the delivery of continence education classes. However, access to technology and digital literacy may be a barrier to attendance for some clients, and telehealth classes may be more time consuming for clinicians.
Conflict of interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
Author(s)
Marielle Collings*
Monash Health Community Continence Service, Cheltenham, VIC, Australia
Monash Health Physiotherapy Department, Dandenong Hospital, Dandenong, VIC 3175, Australia
Email marielle.collings@monashhealth.org
Robyn Brennen
Monash Health Community Continence Service, Cheltenham, VIC, Australia
Monash University, Department of Physiotherapy, School of Primary and Allied Health Care, Frankston, VIC, Australia
The University of Melbourne, Department of Physiotherapy, Parkville, VIC, Australia
*Corresponding author
References
Department of Health. COVID-19 telehealth items guide. Canberra: Department of Health; July 2020 [cited 2021 Jan 31]. Available from: https://www.health.gov.au/resources/publications/coronavirus-covid-19-telehealth-items-guide
Taylor A, Caffrey LJ, Gesesew HA, et al. How Australian health care services adapted to telehealth during the COVID-19 pandemic: a survey of telehealth professionals. Front Public Hlth 2021;9. Available from: https://www.frontiersin.org/articles/10.3389/fpubh.2021.648009/full#B1
Snoswell CL, Taylor ML, Comans TA, et al. Determining if telehealth can reduce health system costs: scoping review. J Med Internet Res 2020;22(10):e17298. doi: 10.2196/17298
Filbay S, Hinman R, Lawford B, et al. Telehealth by allied health practitioners during the COVID-19 pandemic: an Australian wide survey of clinicians and clients. Melbourne: University of Melbourne; April 2021 [cited 2021 Sep 29]. Available from: https://healthsciences.unimelb.edu.au/__data/assets/pdf_file/0009/3775923/Telehealth-by-allied-health-practitioners-during-the-COVID-19-pandemic-Report-April-2021.pdf
Brennen R, Combe S, Funnell L, et al. The acceptability and impact of introductory group continence education session at a multidisciplinary continence service. ePoster presented at ICS 2020 Online; 2020 Nov 19–22; Online Meeting. Available from: https://www.ics.org/2020/abstract/127
Conlan L, Thompson J, Fary R. An exploration of the efficacy of telehealth in the assessment and management of stress urinary incontinence among women in rural locations. Aust NZ Cont J 2016;22(3):58–64.
Banbury A, Parkinson L, Nancarrow S, et al. Delivering patient education by group videoconferencing into the home: lessons learnt from the Telehealth Literacy Project. J Telemed Telecare 2016 Oct 30;22(8):483–488.
Parker S, Prince A, Thomas L, et al. Electronic, mobile and telehealth tools for vulnerable patients with chronic disease: a systematic review and realist synthesis. BMJ Open 2018 Aug 29;8(8):e019192. Available from: https://bmjopen.bmj.com/content/8/8/e019192.info