Volume 28 Number 3
The design and feasibility pilot of a model to guide continence care in Australian residential aged care homes
Joan Ostaszkiewicz, Leona Kosowicz, Jessica Cecil, Erica Wise, Stephanie Garratt and Briony Dow
Keywords incontinence, model of care, evidence-based practice, residential aged care, mixed methods
For referencing Ostaszkiewicz J et al. The design and feasibility pilot of a model to guide continence care in Australian residential aged care homes. Australian and New Zealand Continence Journal 2022; 28(3):40-49.
DOI
https://doi.org/10.33235/anzcj.28.3.40-49
Submitted 1 April 2022
Accepted 20 July 2022
Abstract
To co-design and pilot test a best practice model of continence care and knowledge translation resources for Australian residential aged care, a mixed methods study was undertaken. The study had four stages: (1) a scoping review of literature; (2) a survey, interviews and co-design workshops with residential aged care stakeholders; (3) the co-design of a draft model and knowledge translation resources; and (4) a pilot trial of an education program and qualitative interviews with residents. The pilot trial involved a convenience sample of 22 staff (registered and enrolled nurses and personal care assistants) from two Australian residential aged care homes. Staff completed one pre- and two post-education surveys, and 13 aged care residents were interviewed about their views about continence care. Pilot test data revealed post-education improvements in staff knowledge for eight of the ten questions, and 100% agreement on the feasibility, appropriateness and acceptability of the model and education program. Of the 22 participants, 63% rated the education as ‘very helpful’ in applying the model to practice and 37% rated it as ‘somewhat helpful’. There was no statistically significant difference between the results of any of the three assessment surveys. A content analysis of resident interviews validated the importance of evidence-based, safe, clinically-informed, person-centred continence care that optimises a resident's functional abilities and responds to their individual needs, choices and dignity. The Continence Foundation of Australia has used these findings to design Continence SMART Care (CSC), which represents best practice continence care, meets the Aged Care Quality Standards, and aligns with current reform strategies for the aged care sector. Further research is required to determine the impact on practice and resident outcomes, and its relevance for use in other settings or countries.
Introduction
Urinary incontinence (UI) and faecal incontinence (FI) in residential care homes are prevalent, long-standing, and pervasive problems. They incur human, financial and social costs. Meeting the needs of frail older people with incontinence in this setting is challenging, particularly if they have multiple comorbidities1. Incontinence also increases the workload for care providers, as well as costs to the home2.
UI impacts negatively on the quality of life of aged care residents, as reported in an analysis of data from 11,621 long-term residents of aged care homes in the USA, which found those with UI scored significantly lower on dignity, autonomy, mood sense of comfort and social engagement than did those without UI3. The negative impacts of UI extend to increasing an older person’s risk of falling4,5, or of developing a urinary tract infection6,7 or incontinence-associated dermatitis8. Moreover, UI is a predictor of higher mortality in general, and particularly among frail older adults9.
Although incontinence is a potentially preventable and treatable symptom10, its management in many residential aged care homes is based on routine and is underpinned by the belief that incontinence is an intractable condition of old age1. Evidence from several countries suggests the management of incontinence in care settings, including hospital and long-term aged care, fails to meet community expectations and is not consistent with recommended guidelines11,12 nor community expectations13.
Guidelines for the management of incontinence promote prevention strategies, a comprehensive assessment to identify a person’s individual preferences and needs, including identification and treatment of potentially modifiable causes, and the implementation of a care plan that reflects the person’s preferences and needs14,15. However, research identifies a lack of assessment of incontinence in many long-term aged care settings16–18.
In addition to a lack of assessment, research points to: a lack of resident choice related to continence care19; resident and family dissatisfaction with the quality of continence care20; insufficient time to provide continence care21; low rates of toileting assistance22; a routine approach to bowel management23; the overuse and inappropriate use of aperients24; the indiscriminate use of incontinence products25; polypharmacy24; the overuse of anticholinergic medicines26,27; a lack of prevention and management strategies for incontinence-associated dermatitis28; inappropriate antibiotic use for residents with indwelling urinary catheters29; missed care30; and a lack of education for healthcare professionals about UI31.
Given the ongoing concerns about the quality of continence care in long-term care settings, the aim of the project was to co-design and pilot a best practice model of continence care that reflected the best available evidence, represented the expectations of people with the lived experience of incontinence and their families, and was fit-for-purpose for Australian residential aged care homes.
Materials and methods
Using a mixed methods approach32, the project was undertaken in four stages as described in Table 1. The project was undertaken by researchers from the National Ageing Research Institute (NARI) and was overseen by a Project Advisory Group (PAG) (with representatives from the Australian Government and the Continence Foundation of Australia (CFA). It also comprised consumer representatives and individuals from aged care advocacy groups, as well as professionals with continence and aged care subject matter expertise. The study was approved by Austin Health Human Ethics Committee, HREC Reference Number: HREC/63029/Austin-2020. It was carried out according to the National Statement on Ethical Conduct in Human Research33.
Table 1. Project activities
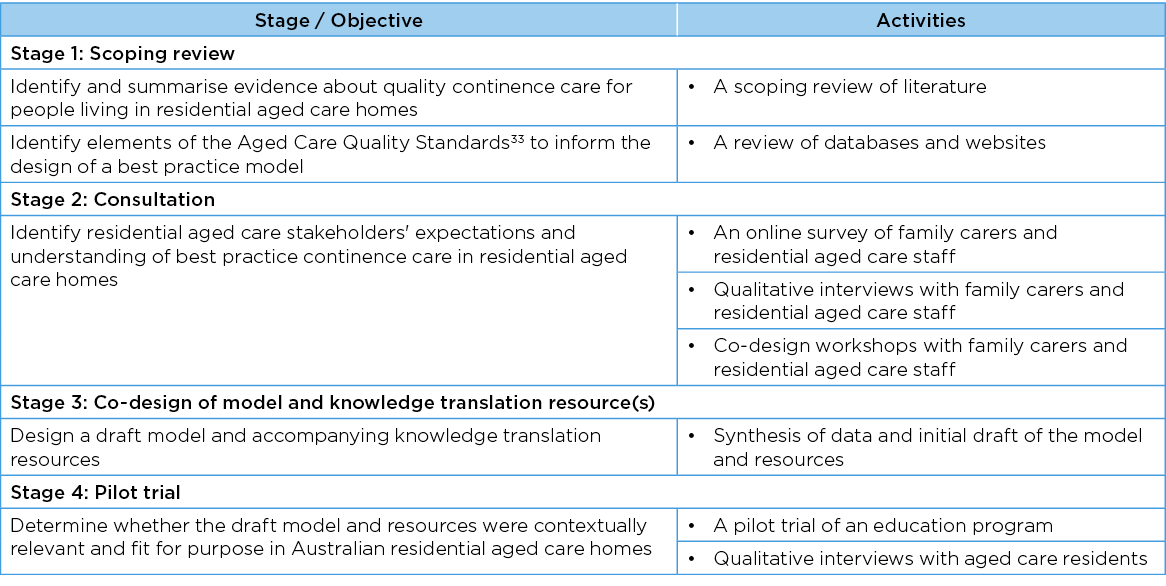
Stage 1: Scoping review
The aim of the scoping review was to identify and summarise evidence about quality continence care for people living in residential aged care homes in order to inform the model design. The literature review sought to answer questions about the prevalence, risk and impact of UI, FI and other bladder and bowel symptoms in residential aged care homes, and the effects of interventions. The methodology was developed using the Joanna Briggs Institute (JBI) Reviewers’ manual35 and reporting was in line with PRISMA-ScR guidelines36. Studies sponsored by drug companies, or the manufacturer of incontinence products were excluded. The findings of each study were extracted and tabled. Where gaps were identified, further searching was conducted using online databases to identify published literature in that area. Relevant grey literature, including continence guidelines, were also reviewed.
Stage 2: Consultation
To understand stakeholder expectations, preferences and concerns about continence care in residential aged care homes, family carers/relatives of older people requiring care in a residential aged care home or staff members currently working in a residential aged care home anywhere in Australia were recruited via Facebook, Twitter, newsletters and email databases targeting volunteer databases and peak bodies and organisations in Australia. A mixed methods research approach was employed and consisted of an online survey, qualitative interviews and co-design workshops.
Online survey
Participants completed an online anonymous survey to rank the importance of several factors to continence care in residential aged care homes. They were offered the opportunity to win one of three $40 gift cards in appreciation of their time. At the completion of the survey, participants were invited to participate in an in-depth telephone interview and/or online co-design workshop.
Qualitative interviews
Participants were interviewed by phone to elicit their opinions about what constituted ‘good’ continence care in residential aged care homes, what residents and family members and staff needed to know, and the resources required to provide good continence care. The questions were informed by findings of the literature review and in consultation with the PAG. Specifically, participants were asked:
- When thinking about continence care for people living in residential aged care, what do you think are the most important things to consider?
- When thinking about continence care for aged care residents, what do you think the most important qualities that the staff should have?
- What do you think residents and family members need to know about incontinence?
- What do you think staff need to know about incontinence in order to provide good continence care?
- What other resources (apart from staff and resident education) are needed to provide good continence care?
- What are some of the barriers to good continence care in residential aged care?
Co-designed workshops
Two online co-design workshops were held for another group of residential aged care home stakeholders. In the first workshop, participants discussed the components of a draft model of care and resources required to deliver the model. In the second workshop, they reviewed a set of propositional concepts for a draft model. The workshops were based on World Café’s seven integrated principles37.
Data analysis
Quantitative data were described using frequency and percentages for categorical data and Likert scales. A 2-tailed test of population proportion was used to determine statistically significant differences between categorical data subsets. Likert scale results were expressed as diverging stacked bar graphs where results are aligned to the centre of the neutral response. Statistically significant differences between Likert scale data subsets were determined by a Mann-Whitney U test between two independent groups and a Kruskal-Wallis H test between two or more independent groups. Differences between subgroups were only reported where they were calculated to be statistically significant (p<0.05).
Qualitative data were uploaded into NVivo 1238, a software package to facilitate the organisation of qualitative analysis. Two researchers independently used an inductive thematic analysis approach to develop a coding framework, which was then further developed collaboratively. The coding framework was independently applied by both researchers to the anonymised data. Differences in coding were discussed and mediated by a third researcher where necessary. The interviews were transcribed and analysed with survey comments and co-design workshop findings to identify the major themes.
Stage 3: Co-design of model and knowledge translation resource(s)
Findings from the scoping review, online survey, qualitative interviews and the first co-design workshop were synthesised to co-design a model and accompanying knowledge translation resources. Feedback was sought from PAG members and participants of the second co-design workshop. This information informed further iterations to the draft model and resources.
Stage 4: Pilot trial
A pilot trial of the draft model of care was conducted to determine its feasibility and application. Convenience sampling was used to recruit staff from residential aged care homes with whom the researchers had a working relationship. Nurse unit managers (NUMs) identified up to 10 registered nurses, enrolled nurses or personal care assistants experienced in providing continence care for the education program. Managers of the homes provided administrative approval for their organisation’s participation and individual staff provided informed consent. Homes were reimbursed for staff costs.
The pilot trial involved a 3-hour education program consisting of four modules of education. The program was delivered live online by two researchers using the Zoom platform. Three surveys were drafted with reference to the literature and the findings from previous stages of the research. They consisted of multiple-choice questions. The draft surveys were reviewed by the education team from the CFA and adapted accordingly. The three surveys were:
- A pre-education pilot study survey (administered 1 week prior to the education).
- An immediate post-education pilot study survey (administered within 1 week following the education).
- A follow-up post-education pilot study survey (administered 4 weeks after the education).
Free text comments were also invited. Participants were asked to indicate the appropriateness, acceptability and feasibility of the draft model and education program and to indicate areas for improvement. Quantitative data were analysed using summary statistical analysis in excel. Qualitative data transcribed from the education sessions and from the survey’s open-ended questions were subject to content analysis conducted by two researchers who each independently reviewed the data to draw out the major themes. The results of the evaluation forms, together with additional feedback from the participants and the researchers’ observations and experiences, were collated and analysed and used to adapt the model.
Validation: resident interviews
To further validate the propositional concepts in the draft model of continence care, qualitative interviews were conducted with residential aged care home residents who were assessed as cognitively able to provide informed consent and had the capacity to take part in a face-to-face interview of 30–60 minutes' duration. Residents were purposively recruited from residential age care homes that had staff participate in the trial of the draft model education program. They were recruited by the NUM of each home. Using an open-ended interview approach, participants were interviewed about their opinions about what constituted ‘good’ continence care in residential aged care homes, what they and family members and staff needed to know, and the resources required to provide good continence care. Data collection continued until saturation was reached.
Interviews were recorded, transcribed and thematically analysed using NVivo 1238. Two researchers independently reviewed the data to identify the major themes. The themes extracted by the two researchers were compared for any differences, and agreement was researched. A deductive coding framework was used to make cross comparisons with the propositional concepts in the draft model.
Results
Stage 1: Scoping review
The scoping review of literature identified 1,776 peer-reviewed publications. After removal of duplicates, 223 were included. Over 500 guidelines, frameworks and policy documents were located; 24 were eligible for inclusion. Data from each study were extracted and tabled according to whether they addressed the prevalence, risk or impact of UI, FI, dual incontinence, and other bladder/bowel symptoms, or was an evaluation of an intervention. The findings from each study were synthesised and translated into recommendations that address the following six topics:
- Caring for a resident with incontinence and other bladder and bowel symptoms (14 recommendations).
- Caring for a resident with an indwelling urinary catheter (7 recommendations).
- Caring for a resident with incontinence-associated dermatitis (5 recommendations).
- Educating the residential aged care home workforce about continence care (5 recommendations).
- Addressing organisational and policy factors that influence the quality of continence care in residential aged care (13 recommendations).
- Providing end-of-life continence care (5 recommendations).
Each recommendation was translated into an evidence statement that was then mapped to one or more of the Australian Aged Care Quality Standards33.
Stage 2: Consultation
Online survey
An online survey was completed by 177 aged care stakeholders. Most of the factors were ranked as ‘very important’, with ranking between 83–95%. A total of 90% of respondents who completed the survey also indicated that information for residents and families about incontinence options was ‘very important’, as was information about care options (85%) and treatment options (75%).
When asked to rank these factors from ‘most’ to ‘least important’, most respondents ranked ‘access to timely staff help’ as the ‘most important’ aspect, followed by ‘help to reach and use the toilet’, followed by ‘help to maintain continence’. ‘Dignity’ was also ranked highly, as was ‘a skilled and trained workforce’.
Qualitative interviews
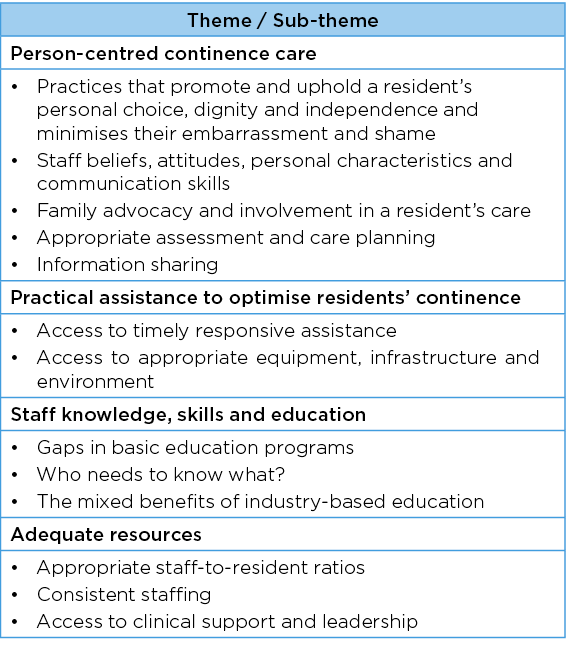
Qualitative interviews were conducted with 14 participants. Findings revealed participants valued continence care that was person-centred, practical, delivered by staff who were knowledgeable, skilled and educated, and was appropriately resourced (Table 2).
Table 2. Themes and sub-themes from qualitative interviews
Co-design workshops
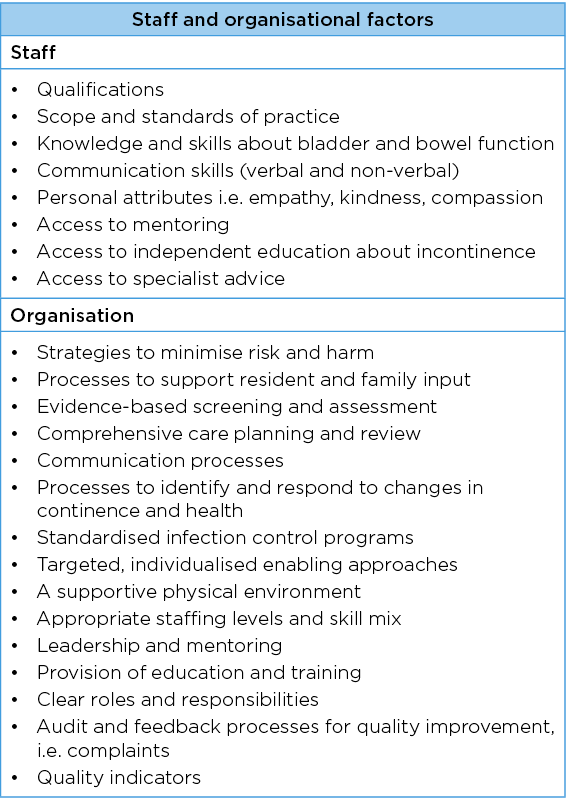
The co-design workshops were attended by 18 people – 10 participants in the first session and eight in the second. Participants represented an equal mix of individuals who worked in residential aged care homes and family carers of residential aged care home residents. The findings from all sources were synthesised by the researchers using an inductive approach. This led to the identification of several factors that stakeholders believed were important to residents and families for quality continence care (Table 3), as well as staff and organisational factors that potentially affect the quality of continence care in this setting (Table 4). All of these factors were included in the final model.
Table 3. Factors that are considered important to residents and families for quality continence care in residential aged care homes
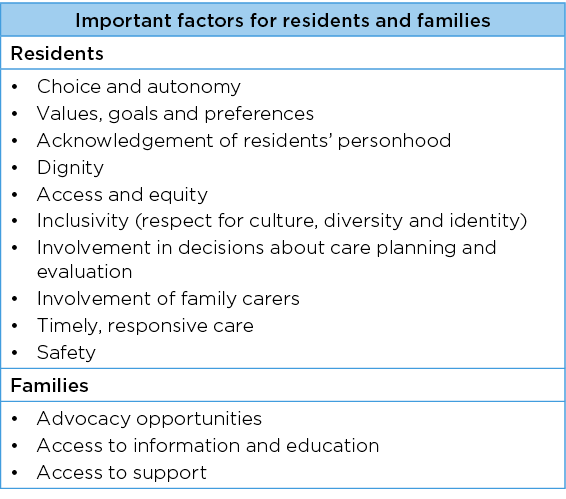
Table 4. Staff and organisational factors that potentially influence the quality of continence care in residential aged care homes
Stage 3: Co-design of model and knowledge translation resource(s)
The draft model consisted of 10 aspirational statements (Figure 1):
- Continence care is person-centred through supported shared decision-making.
- Continence care is clinically informed through an assessment process.
- Continence care is informed by the best available evidence.
- Continence care protects a resident’s dignity.
- Continence care optimises a resident’s functional abilities.
- Continence care is timely and responsive.
- Continence care is inclusive and respectful of a resident’s culture, diversity and identity.
- Continence care is safe.
- Continence care is provided by appropriately trained and skilled staff.
- Continence care is appropriately resourced (Appendix 1).
To support its use in practice, five knowledge translation resources were designed (Figure 2):
- A consumer guide to continence care in residential aged care.
- A continence care decision support tool.
- A continence care organisational audit tool.
- A continence care education resource.
- Continence care evidence statements.

Figure 1. The Best Practice Model of Continence Care in residential aged care
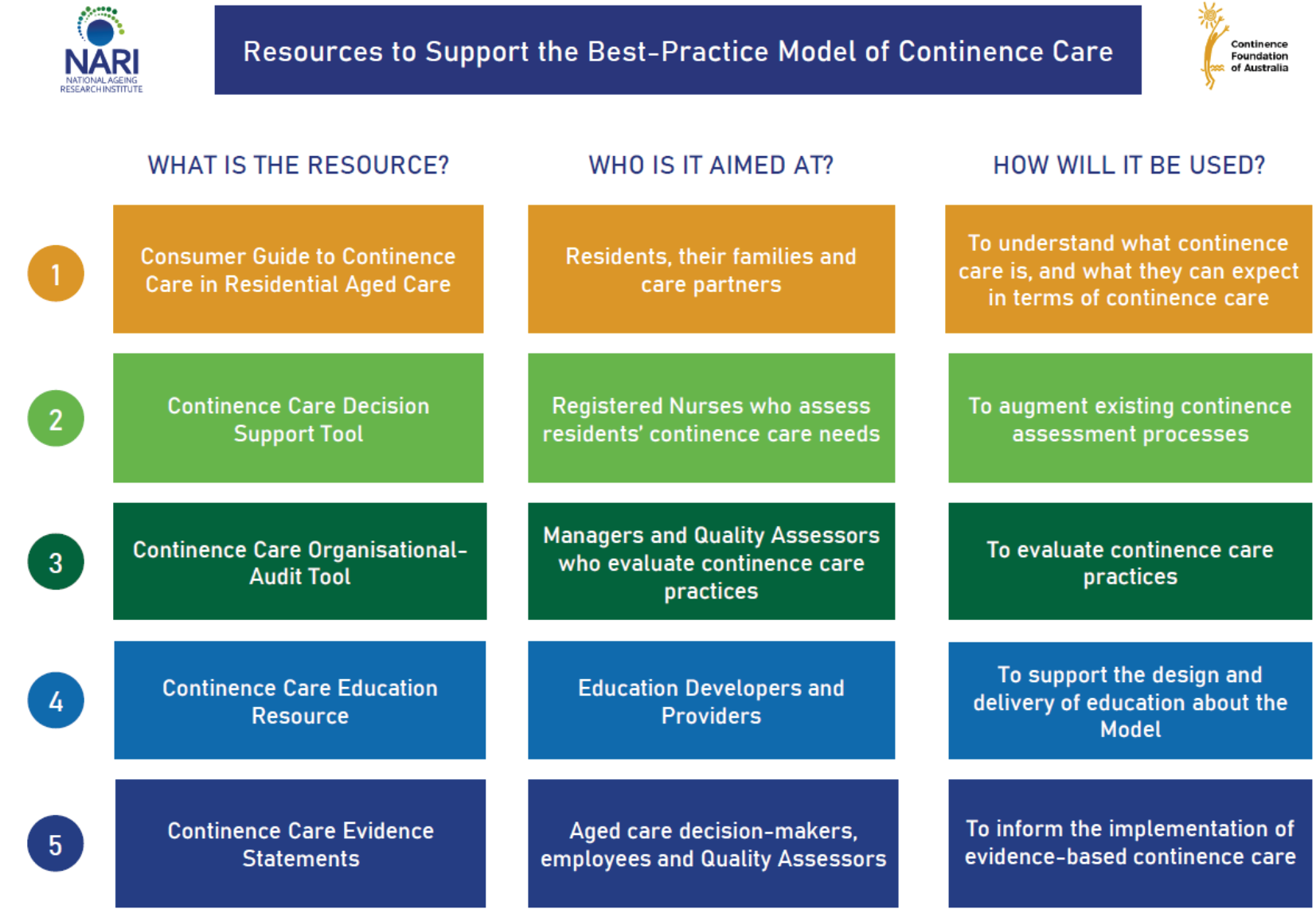
Figure 2. Knowledge translation resources to accompany the model of continence care
Stage 4: Pilot trial
The pilot trial
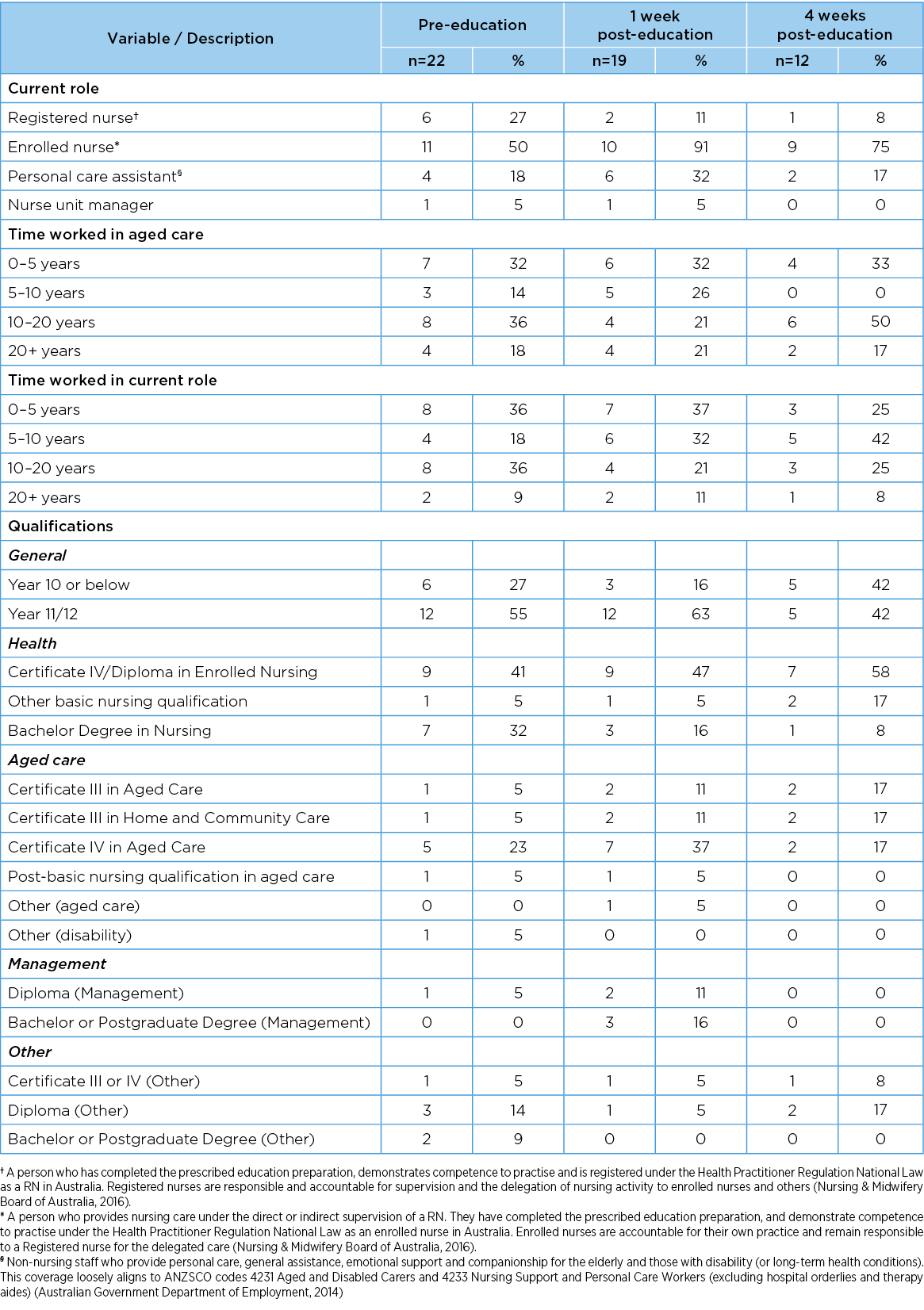
Twenty two staff members from two residential aged care homes attended the education sessions and completed the pre-education survey. Nineteen completed the post-education survey within 1 week of the education sessions. Twelve participants completed the follow-up post-education survey at 4 weeks. Participant demographic characteristics, including roles, qualifications, length of service in a residential aged care home and time in current role, are shown in Table 5.
Table 5. Demographic profiles of education program pilot participants
Knowledge of continence care
Prior to training, staff scored an average of 76%±10.6% on the survey designed to test their knowledge. Scores increased to 81%±7.2% within the week of educational training and decreased slightly to 80%±9.1% at 4 weeks post-education. There was no statistically significant difference between the results of any of the three assessment surveys.
Two of the multiple-choice questions appeared to be problematic for participants. Unlike the remaining eight questions, there was no upward trend in these two questions following the education session. These were questions about the definitions of "resident care preferences" and an "aged care consumer pathway for continence care".
Ratings of the appropriateness, acceptability and feasibility of the model and education program
Participants were asked to rate the appropriateness, acceptability and feasibility of the model and the education program in a series of nine assessment questions. All participants who responded 1 week and 4 weeks post-education strongly agreed that the model was appropriate, acceptable and feasible to implement. Eighteen of the 19 participants who responded in the first survey strongly agreed that the education program was appropriate, with the remaining participant only ‘agreeing’ and not ‘strongly agreeing’ with the statement.
Survey responses immediately post-education showed that 63% of participants rated the education program as very helpful, while 37% rated it as somewhat helpful. After 4 weeks, of the 12 respondents, 55% rated the education program as very helpful and 45% somewhat helpful. No participants at either time point felt that the education program would be not helpful at all.
Qualitative comments
A content analysis of comments about the education suggested the need for further independent contemporary information about continence care for residential aged care home staff. Comments noted the emphasis within the program on the role of empathy in the delivery of continence care and the information about how emotions impact on residents’ and staff behaviour. Participants noted that while the causes of incontinence were covered in sufficient detail in the education program, more information could and should be provided on details of continence assessment and practical strategies about how to communicate well with residents about incontinence. Participants provided several suggestions for applying the information to practice, and the model of delivery.
Qualitative interviews with aged care residents
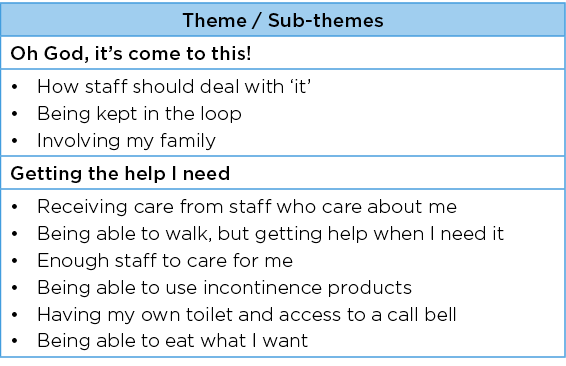
Thirteen residential aged care home residents were interviewed – nine residents living in rural residential aged care homes and four in a metropolitan residential aged care home. Two major themes emerged from the qualitative data: (i) Oh God, it’s come to this! and (ii) Getting the help I need. The themes, together with their sub-themes, are listed in Table 6.
Table 6. Themes and sub-themes from resident interviews
The pilot and validation activity confirmed the salient of the existing concepts and indicated no requirement to alter the model. The collective findings from qualitative interviews with residents, and from the data collected during the pilot trial, informed the need for minor revisions to the draft model and accompanying knowledge translation resources. In particular, the project management group revised the educational content to ensure a stronger alignment with the principles of the model.
Discussion
The aim of the project was to co-design and pilot a best practice model of continence care that reflected the best available evidence, represented the expectations of people with the lived experience of incontinence and their families, and was fit-for-purpose for Australian residential aged care homes. We were unfortunately unable to demonstrate statistically significant differences in staff knowledge between the results of the three assessment surveys. Whist the small sample size was a key factor, it could also relate to the lack of reliability and validity of the data collection instrument.
The education program about the model differed from standard educational programs about incontinence for the aged care workforce. The data collection instrument was designed by the team to align with the educational content. It needs to be further tested, as does the model and the methods to evaluate the uptake of the model. Despite this finding, we suggest the model and accompanying resources have multiple uses.
As the model describes best practice continence care, its use in practice could augment aged care providers’ efforts to meet and exceed quality standards and contribute to broader efforts to strengthen systems to ensure quality care in this setting. The model could also underpin and inform education about continence care for the residential aged care home workforce in particular and thereby augment the government's and industry’s overall strategy to build workforce knowledge and skills.
Prior research identifies major gaps in education about incontinence for aged care employees as well as for healthcare professionals31,39. The educational learning objectives and educational content designed as part of the project could partially address this gap. It primarily targets nurses and personal care assistants working with residential aged care home residents. However, the holistic nature of the model also means it may have broader applicability to other organisational settings such as in acute care or institutions for people living with a disability who have continence care needs. By establishing and articulating what characterises best practice continence care, the model could also inform the design of quality indicators to evaluate the quality of continence care in a residential aged care home context.
Despite the rigorous approach undertaken to design the model, further consultation is required to ensure it is inclusive and respectful of the diversity of residential aged care home residents, such as residents from cultural and linguistically diverse backgrounds, First Nations peoples and people who identify as Lesbian, Gay, Bisexual, Transgender and Gender Diverse, and/or Intersex, as well as residents with an ostomy or indwelling urinary catheter. Moreover, as the data are based on a small sample of staff from only two residential aged care homes and a convenience sampling approach, the findings could reflect a bias toward negative experiences and may or may not represent the quality of continence care in all residential aged care homes. Hence, a robust pre/post-study or randomised controlled trial is required to evaluate the effects of the model on residents, their families and aged care providers in different residential aged care homes and in different cultural contexts.
Conclusion
The Best Practice Model of Continence Care designed by NARI is a theoretical model that describes best practice care for a residential aged care home resident who requires support to maintain continence or manage incontinence or other bladder and bowel symptoms. The focus is on evidence-informed, safe, clinically informed, person-centred continence care that optimises a resident’s functional abilities and responds to their individual needs, choices and dignity. As such, the model promotes and supports the goal of care as well as the goal of cure. The design approach was characterised by an iterative process of collecting, synthesising and integrating evidence from multiple sources. It therefore represents the best available evidence, incorporates the expectations of people with the lived experience of incontinence and other residential aged care home stakeholders, and is fit-for-purpose.
The model could inform the development of quality standards and quality indicators for continence care in residential aged care. It also has the potential to reframe current education about continence care for the aged care workforce. To this end, the Continence Foundation of Australia has designed a comprehensive program titled Continence SMART Care (CSC), and is adopting a phased approach to its implementation.
Although a rigorous approach was used to design the Best Practice Model of Continence Care and CSC, further research is nevertheless required to determine the impact on practice and resident outcomes broadly as well as its contextual relevance for use in other settings or countries.
Acknowledgements
The researchers would like to thank the Continence Foundation of Australia for funding the study and acknowledge the members of the Project Advisory Group and study participants.
Conflict of interest
The authors declare no conflicts of interest.
Funding
This research was funded by the Continence Foundation of Australia.
Appendix
Click here to download appendix 1
Author(s)
Joan Ostaszkiewicz*
Director, Aged Care Division
National Ageing Research Institute Ltd,
Parkville, Melbourne, VIC, Australia
Email j.ostaszkiewicz@nari.edu.au
Leona Kosowicz
Research Assistant, Aged Care Division
National Ageing Research Institute Ltd
Parkville, Melbourne, VIC, Australia
Jessica Cecil
Research Fellow, Aged Care Division
National Ageing Research Institute Ltd,
Parkville, Melbourne, VIC, Australia
Erica Wise
Tailored Training Program Coordinator
HU3, La Trobe University, Bundoora, VIC, Australia
Stephanie Garratt
Research Officer
National Ageing Research Institute Ltd,
Parkville, Melbourne, VIC, Australia
Briony Dow
Director
National Ageing Research Institute Ltd,
Parkville, Melbourne, VIC, Australia
*Corresponding author
References
- Ostaszkiewicz J. Providing continence care in residential aged care facilities: a Grounded theory study [dissertation]. Melbourne, Australia: Deakin University; 2013.
- Mandl M, Halfens RJG, Lohrmann C. Incontinence care in residential aged care homes: a cross-sectional study. J Adv Nurs 2015;71(9):2142–2152.
- Xu D, Kane RL. Effect of urinary incontinence on older residential aged care home residents’ self-reported quality of life. J Am Geriatr Soc 2013;61(9):1473–81.
- Damian J, Pastor-Barriuso R, Valderrama-Gama E, et al. Factors associated with falls among older adults living in institutions. BMC Geriatr 2013;13:6.
- Foley AL, Loharuka S, Barrett JA, et al. Association between the geriatric giants of urinary incontinence and falls in older people using data from the Leicestershire MRC Incontinence Study. Age Ageing 2012;41:35–40.
- Govender Y, Gabriel I, Minassian V, et al. The current evidence on the association between the urinary microbiome and urinary incontinence in women. Front Cell Infect Microbiol 2019. doi:10.3389/fcimb.2019.00133
- Shamliyan TA, Wyman JF, Ping R, et al. Male urinary incontinence: prevalence, risk factors, and preventive interventions. Rev Urol 2009;11(3):145–165.
- Van Damme N, Van den Bussche K, De Meyer D, et al. Independent risk factors for the development of skin erosion due to incontinence (incontinence-associated dermatitis category 2) in residential aged care home residents: results from a multivariate binary regression analysis. Int Wound J 2017;14(5):801–810.
- John G, Bardini C, Combescure C, et al. Urinary incontinence as a predictor of death: a systematic review and meta-analysis. PLoS ONE 2016;11(7):e0158992.
- Abrams P, Cardozo L, Wagg A, Wein A, editors. Incontinence. 6th ed. Bristol, UK: ICI-ICS International Continence Society; 2017. ISBN:978-0956960733.
- Palmer MH, Johnson TM II. Quality of incontinence management in US nursing homes: a failing grade. J Am Geriatr Soc 2003;51(12):1810–2.
- Mid Staffordshire NHS Foundation Trust Public Inquiry. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry: executive summary; 2013. Available from: https://www.gov.uk/government/publications/report-of-the-mid-staffordshire-nhs-foundation-trust-public-inquiry
- Royal Commission into Aged Care Quality and Safety. Final report: care, dignity and respect; 2021. Available from: https://agedcare.royalcommission.gov.au/publications/final-report
- NHS England. Excellence in continence care: practical guidance for commissioners and leaders in health and social care; 2018. Available from: https://www.england.nhs.uk/publication/excellence-in-continence-care/
- Wagg AS, Kung Chen L, Johnson T II, et al. Incontinence in frail older persons. In: Abrams P, Cardozo L, Wagg A, Wein A, editors. Incontinence. 6th ed. Bristol, UK: ICI-ICS International Continence Society; 2017. p. 1309–14422017.
- Brandeis GH, Baumann MM, Hossain M, et al. The prevalence of potentially remediable urinary incontinence in frail older people: a study using the Minimum Data Set. J Am Geriatr Soc 1997;45(2):179–84.
- Harrison T, Blozis S, Manning A, et al. Quality of care to residential aged care home residents with incontinence. Geriatr Nurs 2019;40(2):166–73.
- Watson N, Brink C, Zimmer J, et al. Use of the AHCPR urinary incontinence guideline in residential aged care homes. J Am Geriatr Soc 2003;51:1779–1786.
- Simmons SF, Durkin DW, Rahman AN, et al. Resident characteristics related to the lack of morning care provision in long-term care. Gerontol 2013; 53(1):151–161.
- Francis A, McGregor J, Scott S. Case studies from the Aged Care Complaints Commissioner’s clinical unit. ANZCJ 2018;24(3):75.
- Eagar K, Westera A, Kobel C. Australian residential aged care is understaffed. Med J Aust 2020;212(11):507–508.e1.
- Jerez-Roig J, Santos MM, Souza DL, et al. Prevalence of urinary incontinence and associated factors in residential aged care home residents. Neurourol Urodyn 2016;35(1):102–7.
- Saga S, Seim A, Mørkved S, et al. Bowel problem management among residential aged care home residents: a mixed methods study. BMC Nurs 2014;25;13(1):35.
- Cusack S, Day MR, Wills T, et al. Older people and laxative use: comparison between community and long-term care settings. Br J Nurs 2012;11;21(12):711–4, 716–7.
- Omli R, Skotnes LH, Romild U, et al. Pad per day usage, urinary incontinence and urinary tract infections in residential aged care home residents. Age Ageing 2010;39(5):549–54.
- Niznik J, Zhao X, Jiang T, et al. Anticholinergic prescribing in Medicare. Part D: beneficiaries residing in residential aged care homes: results from a retrospective cross-sectional analysis of Medicare data. Drugs Aging 201;34(12):925–939.
- Zarowitz BJ, Allen C, O’Shea T, et al. Challenges in the pharmacological management of residential aged care home residents with overactive bladder or urinary incontinence. J Am Geriatr Soc 2015;63(11):2298–307.
- Bliss DZ, Gurvich OV, Mathiason MA, et al. Prevention of incontinence-associated skin damage in residential aged care homes. West J Nurs Res 2017;39(5):643–659.
- Armbruster CE, Prenovost K, Mobley HL, et al. How often do clinically diagnosed catheter-associated urinary tract infections in residential aged care homes meet standardized criteria? J Am Geriatr Soc 2017;65(2):395–401.
- Ludlow K, Churruca K, Mumford V, et al. Unfinished care in residential aged care facilities: an integrative review. Gerontol 2021;3;61(3):e61–e74.
- McClurg D, Cheater FM, Eustice S, et al. A multi-professional UK wide survey of undergraduate continence education. Neurourol Urodyn 2013;32(3):224–9.
- Tashakkori A, Teddlie C. Handbook of mixed methods in social & behavioral research. Thousand Oaks, CA: Sage; 2003.
- Australian Government Aged Care Quality and Safety Commission. Aged care quality standards; 2019. Available from: https://www.agedcarequality.gov.au/providers/standards
- National Health and Medical Research Council. National statement on ethical conduct in human research; 2018. Available from: https://www.nhmrc.gov.au/about-us/publications/national-statement-ethical-conduct-human-research-2007-updated-2018
- The Joanna Briggs Institute (JBI). Reviewers’ manual. The University of Adelaide, SA: The Joanna Briggs Institute; 2015.
- Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMAScR): checklist and Explanation. Ann Intern Med 2018;169:467–473.
- Fouché C, Light G. An invitation to dialogue: ‘The World Café’ in social work research. Qual Soc Work 2011;10(1):28–48.
- QSR International Pty Ltd. NVivo (Version 12); 2018. Available from: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home
- Ostaszkiewicz J, Tomlinson E, Hunter K. The effects of education about urinary incontinence on nurses’ and nursing assistants’ knowledge, attitudes, continence care practices and patient outcomes. J WOCN 2020;47(4):365–380.