Volume 29 Number 1
The process of standardising practice: developing a gynaecology trial of void guideline
Chloe Adams, Katie Foxcroft, Karen Baker, Melissa Wright and Belinda Baker
Licensed under CC BY 4.0
Keywords trial of void, gynaecology, voiding trial, postoperative voiding dysfunction, continence
For referencing Adams C et al. The process of standardising practice: developing a gynaecology trial of void guideline. Australian and New Zealand Continence Journal 2023; 29(1):5-9.
DOI
https://doi.org/10.33235/anzcj.29.1.5-9
Submitted 30 March 2022
Accepted 16 January 2023
Abstract
This study presents the introduction of a comprehensive trial of void (TOV) guideline in the gynaecology department of a large tertiary hospital in Queensland, Australia. The aim was to standardise care and increase both nursing and medical staff compliance and satisfaction of processes in the department while improving quality of care. This was measured by a two-phased (pre- and post-implementation) survey of gynaecology department staff. The survey evaluated knowledge, confidence, compliance and satisfaction when comparing the previous TOV local protocol to a new standardised guideline introduced during the study. As follow-up, an audit of medical records was also conducted to reflect clinical practice. The TOV guideline was adopted following consultation and benchmarking with other Australian tertiary hospitals and implemented with a 3-month education program. Pre-implementation survey responses (n=51) from medical and nursing staff with wide range of gynaecology experience (35% 0–2 years, 65% >3 years) were compared with post-implementation survey responses (n=45). Staff knowledge of TOV process increased from the pre-implementation survey (71%) to post-implementation (84%). The overall improvement in satisfaction of the new guideline increased from 37% to 82%. Compliance in using the new guideline was 80% compared to 73% for the previous local protocol. Over a 4-month period for both audits, the pre-implementation audit (n=48) resulted in 33% compliance compared to the post-implementation audit (n=36), 86% compliance. The study determined that the introduction of a standardised TOV guideline improved knowledge, compliance and satisfaction when performing a TOV within the gynaecology department.
Introduction
Women undergoing gynaecological surgery, especially surgical interventions to address the cause of urinary incontinence or pelvic organ prolapse, are at risk of developing postoperative voiding dysfunction. Assessment of normal bladder function prior to hospital discharge is an important step to identify this postoperative complication. Normal bladder function is defined as both successful storage and emptying; both aspects have potential to be affected by gynaecological surgery1,2.
Trial of void (TOV) is defined as the assessment of voiding function and should be commenced immediately post-removal of an indwelling urinary catheter (IDC)1. TOV is not routinely performed following all types of gynaecological procedures, for example, a laparoscopic hysterectomy, as the complication of urinary retention for this common procedure ranges from 7–14%3. The current gold standard for assessing voiding function is by measuring micturition (urination) as well as the post-void residual (PVR), which is defined as the volume of urine left in the bladder at the completion of micturition1,4. This can be assessed by a bedside ultrasound (bladder scanner) or re-catheterisation, (intermittent catheter/Nelaton) to drain and measure the PVR volume.
Hakvoort and colleagues claimed “As abnormal PVR is a complication that necessitates additional treatment, the absence of consensus implies that part of the patients receive either undertreatment or overtreatment”5. As such, when a TOV is deemed unsuccessful within our gynaecology department, the patient requires their bladder to be emptied via an intermittent catheter or clean intermittent self-catheterisation (CISC), education to be commenced, and the treating team to be notified for further management6. If clinically appropriate and practical for the patient, CISC is the preferred intervention rather than insertion of an IDC for postoperative voiding difficulties following gynaecological surgery7.
Prior to this study, an out-of-date TOV local protocol was used by medical and nursing staff within the gynaecology department. Anecdotally, junior nursing and medical staff within the organisation had expressed confusion around the process of a TOV. This was due to varying individual approaches by medical treating teams which created confusion among staff in regards to which patients required a TOV and the correct TOV procedure.
A review of the literature revealed variable physician definition and practices on the process of a TOV in the field of gynaecology and the management of PVR and urinary retention1,5,8,9. A study completed in Western Australia by Bosco and colleagues9 explored research priorities for nurses working in the gynaecology setting which identified the highest ranking priority for research was the postoperative management of TOV10. Similarly, to mitigate clinical variation, Buchko and Robinson9 developed and implemented an algorithm which included standard definitions and a consistent protocol for TOV to minimise variation among practitioners.
The purpose of this study was to promote standardised care through the introduction of a clear and comprehensive TOV guideline. The aim was to increase medical and nursing staff compliance to the guideline and best practice, improve satisfaction of the TOV process, and increase quality of care within the unit.
Methods
Ethics
Ethics approval was granted for this study by The Royal Brisbane and Women’s Hospital Human Research Ethics Committee (HREC) for review, approval number LNR/2019/QRBW/5863, in accordance with the National Statement on Ethical Conduct in Human Research11.
Introducing a new guideline
A benchmarking review of local guidelines from five hospitals in Australia was undertaken. From this review a draft guideline was developed and circulated for critical, expert review, including stakeholders such as gynaecologists and specialised nursing staff to ensure best and evidence-based practice was implemented12. Benchmarking was chosen to guide the standardisation of care as it is well supported in the literature to evolve practice and assess current performance against best practice13. The biggest difference between the study site hospital and other facilities that were benchmarked was the type of protocol implemented. All of the benchmarked hospitals had gynaecology TOV protocols or guidelines in place, rather than a local work instruction6,14–18. Key stakeholders such as medical officers, the continence advisory service and senior nursing staff, including the safety and quality unit, were consulted by the distribution of the standardised TOV guideline for review and comment, prior to approval and publishing.
Education program
The rollout of a new guideline required gynaecology service-wide notification and education that was completed via an education bundle. Email dissemination of the TOV guideline was distributed to all current in-patient gynaecology staff (medical and nursing). Out of the 40 current active in-patient gynaecology nursing staff, 34 acknowledged that they had reviewed the guideline and received in-service education. These in-service sessions were presented by research nurses allocated as ward clinical champions. In addition to training, they provided support and were an educational resource for all gynaecology staff surrounding TOV practice. The in-service PowerPoint slides were also printed and placed within the nurses’ station as a reference tool for all staff.
The guideline was discussed at various leadership meetings within the organisation including the Gynaecology Management Advisory Group meeting, which captures both medical and nursing leaders within gynaecology. Research nurses presented at a routine registrar training session capturing junior and senior registrars. The new guideline contained a TOV flowsheet which was printed and placed in every patient bedside chart to allow for easy reference for all clinicians12.
Survey
To assess staff knowledge, confidence, compliance and satisfaction of the TOV process within gynaecology, a two-phase web-based survey of standardised practice was conducted. The survey excluded all students working in gynaecology as well as enrolled and assistant nurses and staff not actively working in the in-patient department within gynaecology. All eligible in-patient ward gynaecology medical and nursing staff within the department were invited to participate in the voluntary pre- and post-implementation surveys. At the time of the study, approximately 40 registered nurses and 55 doctors were actively rostered in the gynaecology in-patient department, with staff in each discipline having varied levels of experience in gynaecology. Participants were informed, and consent was implied by the submission of the completed survey.
The surveys were conducted over a 3-week period in February and December 2020. The collection of the surveys was completed by nurses from the research team, inviting participation from eligible medical and nursing staff in gynaecology using an iPad and multiple email disseminations. All participant privacy and confidentially was maintained throughout the quality improvement activity and all results were de-identified. A mixed method approach was utilised throughout the survey, giving the participants the ability to respond to questions by free-text and Likert scales, prompting elicit opinions, ideas, issues or questions of relevance to the TOV process within the department. In both the pre-implementation and post-implementation surveys, answers were mandatory and skip logic was used to keep the questions relevant to the selected profession. The post-implementation survey started with the question “Did you complete the pre-education survey?” to capture audience data and assess changes in practice and knowledge post the standardisation of care.
Audit
A retrospective audit of patient medical records identified those patients who required a TOV prior to discharge. Each audit included all patients booked for surgical procedures requiring a TOV over a 4-month period (pre-TOV standardisation 2 September 2019 to 3 January 2020 and post-TOV standardisation 1 January to 1 May 2021). All data were collected on a secure Excel spreadsheet and analysed by research nurses, capturing appropriate patient medical records using ORMIS ICD-10 codes to isolate specific gynaecology and urogynaecology surgical procedures that would routinely require a TOV. The same ORMIS ICD-10 codes were used for both pre- and post-implementation audits to ensure the same patient group was identified. In order to assess compliance of TOV processes, both audits were conducted by comparing the “Bladder chart for trial of void” documentation (voided versus PVR volumes and interventions/comments) against the current protocol and guideline at the time of the audit. Additionally, further medical records such as progress notes were reviewed to determine whether any deviation from the protocol parameters had occurred such as deviations in time of removal or acceptable residual volumes.
Results
Survey
The web-based survey host Citizen Space managed all survey data and analysis. In both surveys, broad gynaecology experience was captured, with staff with less than 1 year's experience to staff with over 8 years’ experience completing both surveys (pre-implementation survey 35% 0–2 years, 65% >3 years, and post-implementation survey 40% 0–2 years, 60% >3 years). The pre-implementation survey completion rates resulted in 41% (n=21) medical professionals and 59% (n=30) nursing professionals; the post-implementation survey completion rates resulted in 31% (n=14) medical professionals and 69% (n=31) nursing.
Staff knowledge of the current TOV process increased from 71% pre-implementation survey to 84% post-implementation survey (Figure 1). Staff reported 80% compliance of use of the new guideline compared to 73% use of the initial work instruction. The overall improvement in satisfaction of the new guideline increased from 37% to 82%. The 5-point Likert survey question “I am satisfied with the current TOV for gynaecology” included a compulsory free-text component.
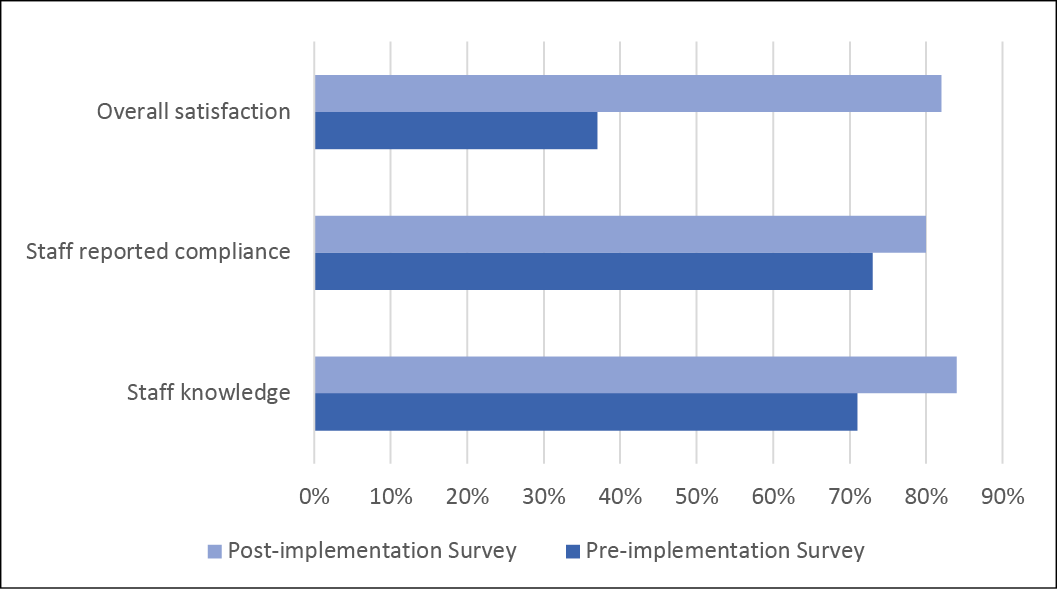
Figure 1. Gynaecology department pre- and post-implementation survey results
The pre-implementation survey evoked reoccurring answers such as “confusing, inconsistent, sometimes confusion between doctors and nurses, amounts changing weekly between consultants, no consistency across teams, different consultants request different TOV, outdated, difficult to follow, not everyone is on the same page and not clear”. In contrast, the post-implementation survey was found to have considerable differences in the reoccurring answers such as “easy to follow, easy to understand, clear and concise, clear guide, policy is clear, clearly documented, straight forward, clear instructions”.
Survey results show that satisfaction was increased (odds ratio (OR)=7.79, 95% confidence interval (CI)=3.01–20.18), as well as knowledge of the TOV process (OR=2.26, 95% CI=0.83–6.19). The overall pre- and post-implementation survey results showed significant change in practice and staff awareness of TOV within the department (Z=4.51, p<0.1) (Table 1).
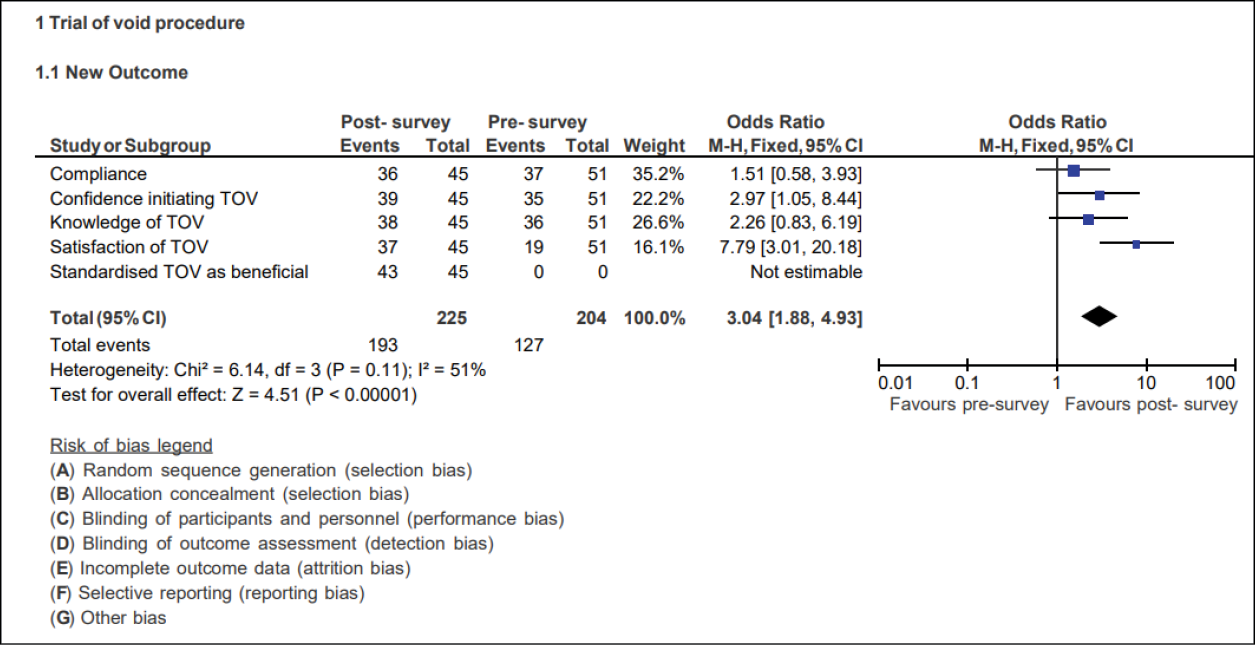
Table 1. Further analysis of pre- and post-implementation survey results
Audit
The number of patient medical records audited varied between both the pre- and post-implementation audit (n=48, n=36, respectively). Although the time period of auditing remained the same between the two, 4 months, the post-implementation audit resulted in a smaller patient group due to a decreased cohort of TOV patients. The pre-standardisation of care audit reflected a high number of 'other' results. This was due to inconsistencies in the time of removal of the IDC post-procedure due to the original work instruction not being utilised correctly (Figure 2). These patient TOVs were classified as 'other' in both audits to highlight the varying TOV practices of treating teams within the gynaecology department. Three additional classifications of 'other' included unrelated patient complications, lost documentation and partial follows. Overall compliance of the TOV procedure in gynaecology at the time of audit improved from 33% to 86%.
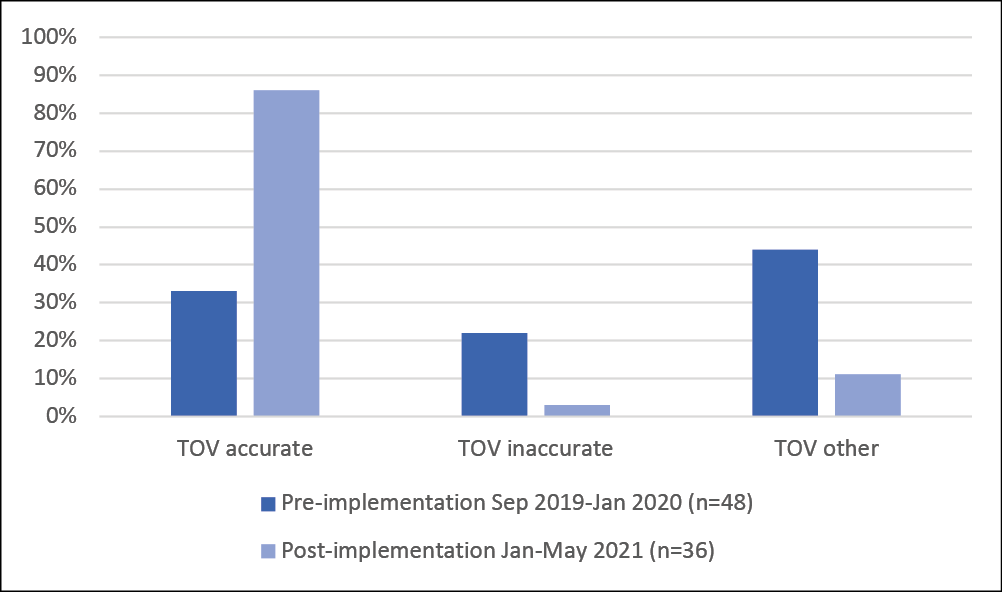
Figure 2. Retrospective patient chart TOV results pre- and post-implementation audits
Discussion
The study team determined that, following the introduction of a standardised TOV guideline, the medical and nursing staff satisfaction of the TOV process significantly increased in the gynaecology unit. It is important to note that, overall, both surveys represented lower completion rates by medical professionals than nursing, even with a higher number of staff in their cohort. However, the results remain relevant to both cohorts working in a gynaecology in-patient setting. While the timeframes of the pre- and post-implementation audit remained identical, it is believed the cancellation of surgical procedures at the tertiary hospital during the COVID-19 pandemic contributed to this decrease in surgical cases, resulting in a decreased number of post-implementation audited patients19.
There remains a lack of current cohesive literature surrounding TOV practice within gynaecology, with varied reported practices. Although compliance of the current guideline has improved, there is risk of both medical and nursing staff being unable to justify their practice. Without clear contemporary evidence and, although regarded important, recommendations may not always be implemented in routine practice if perceived not to be feasible8. This is shown in the study by Bosco and colleagues10; although clinical guidelines existed in their organisation, the management of TOV remained the number one research priority for nurses working in gynaecology.
Conclusion
This study aimed to determine if the introduction of a standardised procedure on TOV in gynaecological patients improves staff compliance and satisfaction. The major findings in our study have revealed that, within the gynaecology department, compliance, satisfaction and awareness has dramatically improved since the introduction of standardised TOV practice. Although there remains a current need for further contemporary TOV literature, this study has highlighted the importance of standardised care within a surgical unit to prevent confusion and dissatisfaction of TOV practice.
Acknowledgement
Our appreciation to Emma Dowling and Catherine Nicholas for your contribution and comments. We would also like to thank all survey participants and key stakeholders.
Conflict of interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
Author(s)
Chloe Adams*
Registered Nurse, Gynaecology Department, Women’s and Newborn Services, Royal Brisbane and Women's Hospital, QLD, Australia
Email chloe.adams@health.qld.gov.au
Katie Foxcroft
Clinical Research Manager & Adjunct Fellow, UQ Centre for Clinical Research, Perinatal Research Centre and Women’s and Newborn Services, Royal Brisbane and Women's Hospital, QLD, Australia
Karen Baker
Staff Specialist, Women’s and Newborn Services, Royal Brisbane and Women's Hospital, QLD, Australia
Melissa Wright
Continence Nurse Advisor CNC, Women’s and Newborn Services, Royal Brisbane and Women's Hospital, QLD, Australia
Belinda Baker
Clinical Nurse, Gynaecology Department, Women’s and Newborn Services, Royal Brisbane and Women's Hospital, QLD, Australia
References
- Geller EJ. Prevention and management of postoperative urinary retention after urogynecologic surgery. Int J Womens Health 2014;6:829–38.
- Elbiss HM, Moran PA, Hammad FT. Teaching patients clean intermittent self-catheterisation prior to anti-incontinence or prolapse surgery: is it necessary in women with obstructive voiding dysfunction? Int Urol Nephrol 2012;44:739–43.
- Wang R, Won S, Haviland MJ, et al. Voiding trial outcome following pelvic floor repair without incontinence procedures. Int Urogynecol J 2016;27(8):1215–20.
- Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 2010;21(1):5–26.
- Hakvoort RA, Burger MP, Emanuel MH, et al. A nationwide survey to measure practice variation of catheterisation management in patients undergoing vaginal prolapse surgery. Int Urogynecol J Pelvic Floor Dysfunct 2009;20(7):813–8.
- The Royal Brisbane Women’s Hospital. Work instruction – trial of void. Brisbane: Gynaecology Local Operating Procedure; 2014.
- Aslam N, Moran PA. Catheter use in gynaecological practice. Obstetric Gynaecol 2014;16(3):161–8.
- Meekins AR, Siddiqui NY, Amundsen CL, et al. Improving postoperative efficiency: an algorithm for expedited void trials after urogynecologic surgery. South Med J 2017;110(12):785–90.
- Buchko BL, Robinson LE. An evidence-based approach to decrease early post-operative urinary retention following urogynecologic surgery. Urologic Nurs 2012;32(5):260–73.
- Bosco AM, Williams N, Graham JM, et al. Developing research priorities for nurses working in the gynaecology setting in Western Australia. Collegian 2018;25(1):73–80.
- National Health and Medical Research Council. The National Statement on Ethical Conduct in Human Research; 2018. Available from: https://www.nhmrc.gov.au/about-us/publications/national-statement-ethical-conduct-human-research-2007-updated-2018
- Grimshaw JM, Russell IT. Achieving health gain through clinical guidelines II: ensuring guidelines change medical practice. Quality Health Care 1994;3(1):45–52.
- Mahmood T, Mukhopadhyay S. Professional development skills for obstetricians and gynaecologists. Cambridge: Cambridge University Press; 2018.
- The Royal Hospital for Women. Trial of void bladder scanning regimen. Sydney: Local Operating Theatre; 2014.
- The Royal Women’s Hospital. Bladder management: trial of void following TVT – Day Surgery Unit. Melbourne: Procedure; 2019.
- King Edward Memorial Hospital Obstetrics and Gynaecology. Clinical practice guideline – bladder management. Western Australia: KEMH Clinical Guidelines; 2019.
- Mater. Trial of void post-gynaecological surgery. Melbourne: Procedure; 2018.
- Gold Coast Hospital and Health Service. Gold Coast: Trial of void guideline. 2018.
- Rimmer MP, Al Wattar BH. Provision of obstetrics and gynaecology services during the COVID-19 pandemic: a survey of junior doctors in the UK National Health Service. BJOG 2020;127(9):1123–8.