Volume 30 Number 2
Effect of diabetes on mechanisms controlling bladder function
Mr Aidan Mckeon, Dr Donna Sellers, Dr Catherine McDermott, Professor Russ Chess-Williams
Licensed under CC BY 4.0
DOI 10.33235/anzcj.30.2.37
Objective: A majority of patients with diabetes are afflicted with some form of lower urinary tract symptoms (up to 95% in some populations1), a phenomenon commonly referred to as diabetic bladder dysfunction (DBD). The symptoms experienced by individuals vary widely from overactive bladder symptoms such as increased urge and frequency, or underactive bladder symptoms such as hesitancy and increased residual volume or mixed symptoms. This complicates research and the mechanisms by which diabetes induces bladder dysfunction are still not well understood. Additionally, poor glycaemic control is believed to exacerbate symptoms, although the details have been difficult to elucidate from clinical studies. Thus, we aimed to use in vitro and in vivo studies to investigate the mechanisms involved in diabetic bladder dysfunction in diabetic mice.
Methods: Diabetes was induced in adult female mice by treating with streptozotocin (50mg/kg i.p. daily for 5 days), which affects the pancreas and produces a type 1 diabetes model. Bladder function was examined by measuring voiding patterns and behaviour during the 16-day treatment period, isolated whole bladder preparations and cystometry in urethane-anaesthetised mice (0.9g/kg s.c. and 0.3g/kg i.p.). For whole bladder preparations (in vitro) bladders were isolated from mice and catheterised via the urethra with a 3-way catheter connected to a pressure transducer, outflow tap and infusion pump, to allow filling with saline. Neurogenic bladder contractile responses to nerve stimulation and responses to agents acting on the key neurotransmitter pathways involved in bladder function were examined. In cystometry (in vivo) experiments bladder function was examined under a continuous saline infusion.
Results: Diabetic mice had increased (P<0.05) blood glucose (19.1±1.2mmol/L, n=15) compared to controls (9.3±0.4mmol/L, n=14) and urine output was increased four-fold (P<0.02). In isolated whole bladders, neurogenic responses to nerve stimulation were significantly reduced in diabetic mice (Figure 1). At 20Hz stimulation bladder responses from diabetic mice were significantly lower (10.3±3.6mmHg, n=4)(P<0.03) than controls (23.2±1.4mmHg, n=6). Similarly, pressure responses to the primary neurotransmitter adenosine triphosphate (ATP), were reduced (P<0.04) in bladders from diabetic mice (16.9±3.6mmHg) compared to controls (23.9±0.9mmHg). In vivo, cystometry showed that the peak pressure during voiding was reduced (P=0.03) in diabetic animals (28.2±0.9mmHg, n=11) compared with controls (32.4±1.6mmHg, n=8).
Conclusion: The results suggest that diabetes results in reduced pressure development in the bladder during voiding, which is caused by depressed neurogenic contractions resulting from reduced release of the neurotransmitter ATP.
Project Funding
This research was supported by an Australian Government Research Training Program Scholarship.
Ethics Approval Number: 2017/AE000536: Stress and bladder dysfunction, and 2022/AE000224: Mechanisms of Bladder Dysfunction.
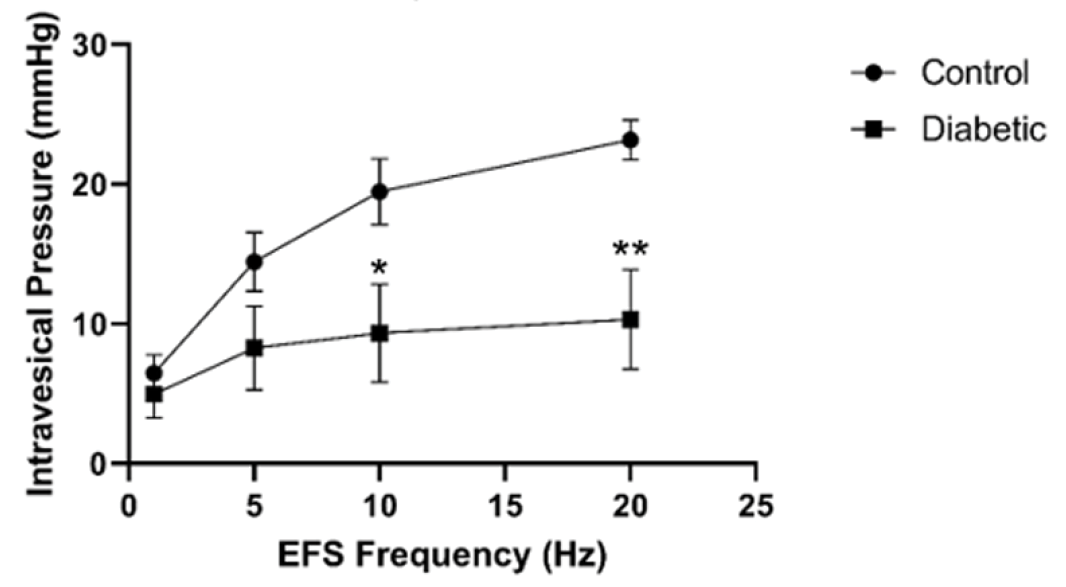
Figure 1. Pressure responses of isolasted bladders to nerve stimulation via electric field stimulation at a variety of frequencies. Data is mean ± SEM. (Control n = 6, Diabetic n = 4, * P<0.05 vs control, ** P<0.01 vs control)
Author(s)
Mr Aidan Mckeon1, Dr Donna Sellers1, Dr Catherine McDermott1, Professor Russ Chess-Williams1
1Bond University, Gold Coast, Australia
References
- Changxiao H, Zhengyong Y, Shibing Y, Caiwen W, Yingchuan H, Wei H, Hanhui W, Dong L, Peng H, Jing L, Rui Z, Jia L, Hong S. Clinical and urodynamic evaluation of women referred with diabetes mellitus. Int Urogynecol J. 2014;25(7):979-83. doi: 10.1007/s00192-014-2354-5.