Volume 25 Number 1
The utilisation of a negative pressure wound therapy clinical decision tree in an acute care setting tissue viability service
Katie Leek, Julie M Murdoch, Catherine H McCarthy
Keywords negative pressure wound therapy, critical care, acute care, complex wounds
For referencing Leek K, Murdoch JM & McCarthy CH. The utilisation of a negative pressure wound therapy clinical decision tree in an acute care setting tissue viability service. Journal of Wound Management 2024;25(1):2-10.
DOI
10.35279/jowm2024.25.01.03
Submitted 13 June 2023
Accepted 1 November 2023
Abstract
The aim of this case series and service evaluation was to demonstrate the beneficial clinical and economic outcomes of the utilisation of a negative pressure wound therapy (NPWT) clinical decision tree within routine practice. A total of 16 retrospective anonymised complex wound case studies were referred to the tissue viability nursing (TVN) service. Patients received NPWT as inpatients, as per routine practice. Data was reported as an aggregated cohort, with further stratification by wound type. Descriptive statistics were utilised. The most prevalent wound type was dehisced surgical wounds (n=10; 62.5%) located on the abdomen (n=9; 56.25%). Risk of contamination (43.75%) and exudate management (43.75%) were the most common rationales for choosing traditional NPWT (tNPWT). Seven patients (43.75%) were discharged from hospital still requiring NPWT, with five (71.4%) having wound criteria suitable for single use NPWT (sNPWT). Using tNPWT and sNPWT alongside a clinical decision tree can assist in optimising NPWT delivery to patients within an acute care setting.
Key messages
- A service evaluation and case series of complex and challenging wounds managed by a nurse-led tissue viability nursing (TVN) service in a large trauma hospital using traditional negative pressure wound therapy (tNPWT) and single use NPWT (sNPWT).
- The aim of this case series and service evaluation was to demonstrate the beneficial clinical and economic outcomes of the utilisation of a NPWT clinical decision tree within routine practice in an acute care setting.
- The most prevalent wound type was dehisced surgical wounds (n=10; 62.5%) located on the abdomen (n=9; 56.25%). Risk of contamination (43.75%) and exudate management (43.75%) were the most common rationales for choosing tNPWT. Seven patients (43.75%) were discharged from hospital still requiring NPWT, with five (71.4%) having wound criteria suitable for sNPWT.
Introduction
The cost of wound care within the UK is rising, with current estimates showing the overall cost to the National Health Service (NHS), annually, to be £8.3billion1. In addition, the number of patients requiring wound management is expected to increase due to an ageing population and increased prevalence of multiple underlying conditions2. Although it is widely acknowledged that the majority of wound care is managed within the community setting1,3, the impact of the COVID‑19 pandemic has seen a rise in hospital admissions for patients with open wounds4. Therefore, already stretched healthcare providers are receiving growing pressure to manage wounds efficiently across community services, while acute services are under pressure to reduce length of stay and release much needed bed availability, resulting in a higher proportion of wounds being managed in the community setting. Three main drivers that can determine how efficient wound care can be achieved have been identified – the time it takes to heal a wound, the frequency of dressing changes, and the incidence of complications2,5.
The appropriate use of advanced wound therapies can improve patient outcomes and the duration of treatment, and cut healthcare costs related to wound management6,7. Negative pressure wound therapy (NPWT) is one of the most effective and widely used interventions for problematic wounds8 and is indicated for a plethora of wound types9, with an established and understood mode of action10. Two systems of delivery now exist and can be categorised by traditional NPWT (tNPWT) and single use NPWT (sNPWT). tNPWT is commonly utilised to manage large, heavily exuding wounds and is delivered using an appropriate filler (foam or gauze) shaped to the wound bed and secured with a film drape to form a sealed system. tNPWT then delivers sub-atmospheric pressure between –50 and –175mmHg9, through a non-disposable pump with an attached disposable canister to collect and manage high volumes of exudate. sNPWT became available around 10 years ago to manage low-to-moderate exudate volume and shallower wounds11. Some sNPWT devices use a dressing for fluid management and as a wound interface which allow wider coverage of the peri-wound area12. These devices deliver sub-atmospheric pressure to the wound bed through an integrated dressing, single patient use portable pump and can exist with or without a canister. Dressing changes with each device depend on patient need, clinician assessment and should follow the recommended instructions for use (IFU) by the manufacturer.
Both modes of delivery of NPWT provide similar clinical benefits to a wound, but allow clinicians flexibility in terms of choice based on wound and patient factors8,13. Furthermore, a step-across approach of tNPWT to sNPWT (or vice versa) can be taken, i.e., tNPWT may be suitable for a larger heavily exuding wound until the overall volume and level of exudate reduces; the wound may then be transitioned to sNPWT8. However, most healthcare professionals determine which system to use on a case-by-case basis, which can lead to inconsistency and variation of when to use NPWT, which system to employ and, where appropriate, when to transition between the two14.
In response to these challenges, in 2020 an International Consensus Panel of eight experts in wound care and NPWT from Canada, Spain, the United States and the United Kingdom convened to address how and when to use NPWT, and when to transition between tNPWT and sNPWT. Ten statements (Figure 1) were agreed upon by the expert panel in the following categories: therapeutic goals; wound related factors; patient satisfaction and quality of life; care-setting related factors; economic-related factors and NPWT system related factors. In addition to these statements, the panel developed a NPWT clinical decision tree to guide the selection between tNPWT and sNPWT; the tool also guides the clinician to which filler may be appropriate according to the wound’s characteristics (Figure 1).
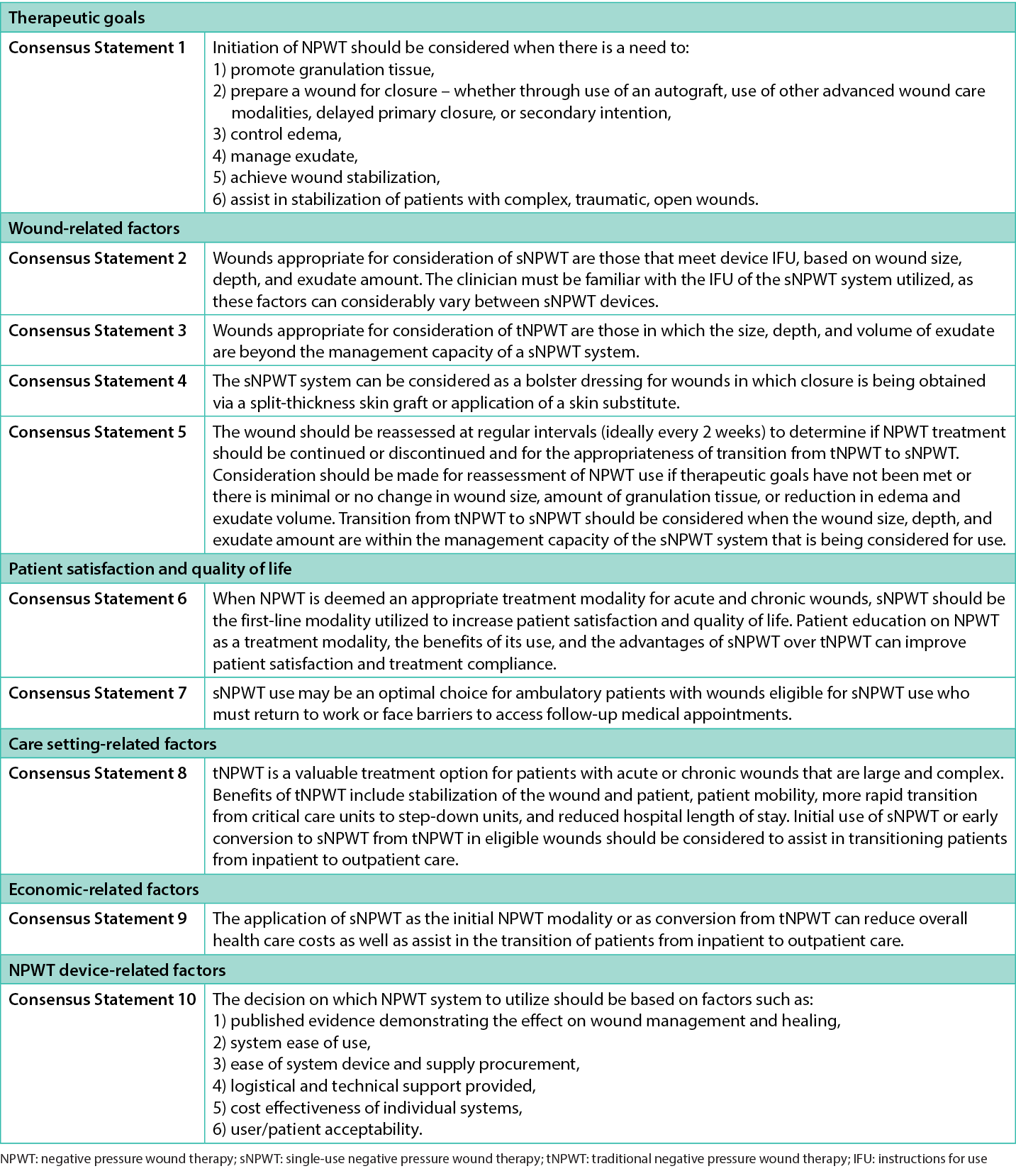
Figure 1. NPWT consensus statements by category14
The Royal Stoke University Hospital is one of the largest teaching and research hospitals in the UK, offering a full range of general acute hospital services as well as holding major trauma centre status. NPWT has been a well-established wound management option initiated and led predominately by the tissue viability nursing (TVN) team who serve the majority of inpatient services and surgical specialties. The team were early adopters of the NPWT clinical decision tree (Figure 2) supporting their clinical practice and guiding them to which NPWT system could be used at the most appropriate time to improve clinical and patient outcomes. The NPWT devices used by TVN team are RENASYS™ TOUCH tNPWT and PICO™ sNPWT devices (Smith and Nephew, Hull, UK). One key objective of the TVN team is to initiate NPWT within the inpatient environment and regularly discharge patients into the community to continue therapy to maximise healing between hospital to home. The aim of this service evaluation is to demonstrate the potential beneficial clinical and economic outcomes the adoption of the NPWT clinical decision tree could offer within routine wound care practice.
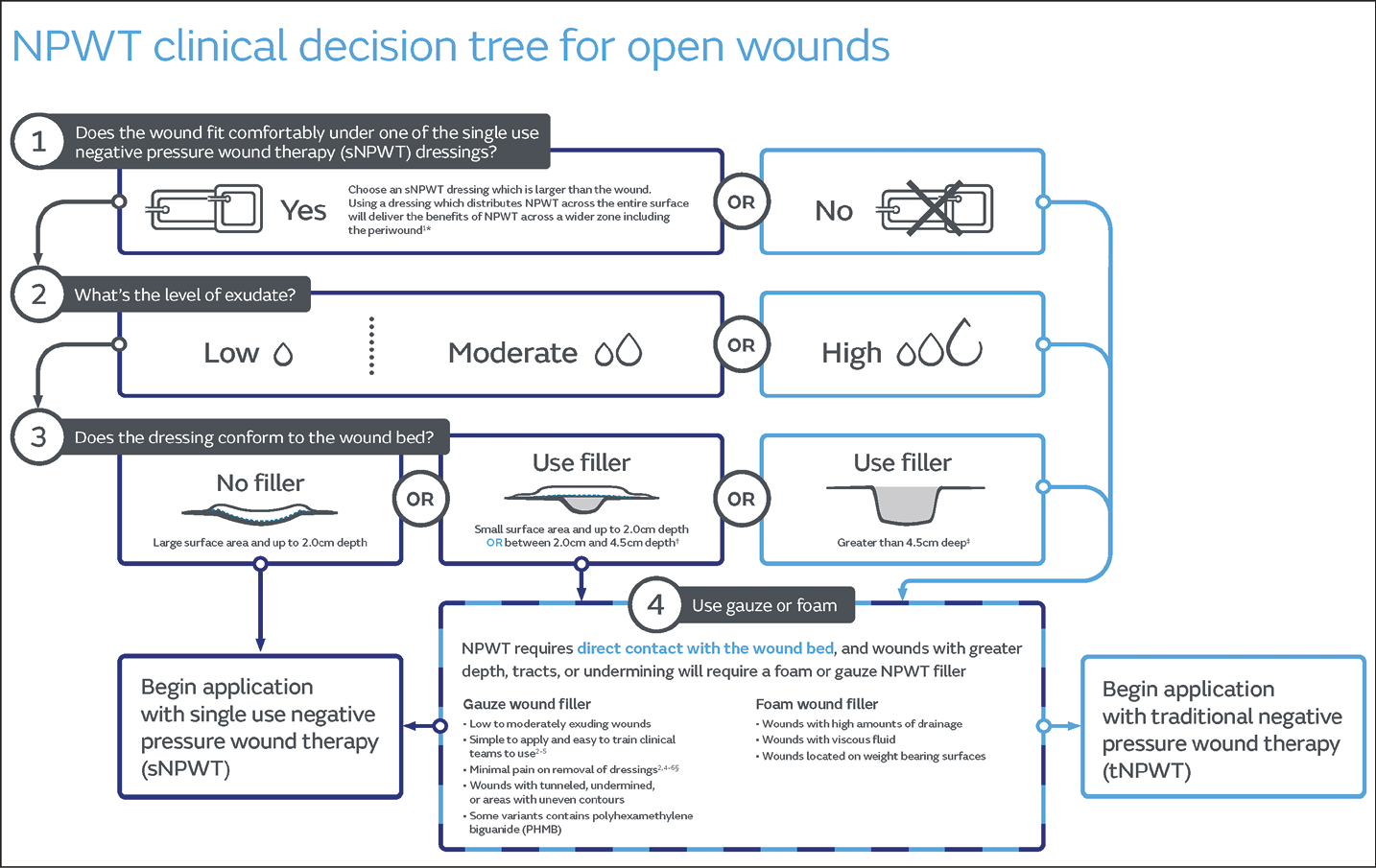
Figure 2. NPWT clinical decision making tree for the management of open wounds14
Methods
This service evaluation included a review of retrospective anonymised cases of patients referred to the TVN service at The Royal Stoke University Hospital from a variety of inpatient services. Ethics committee approval was not required as this project was classified as a service evaluation, as per guidance from the UK Health Research Authority15. All the cases received were patients referred for review and/or assessment for wound management from January 2021 until January 2022. Patients were included in the review if they had been initiated on NPWT and required continuous follow up by the TVN team for wound management due to complexity of the wound or multiple co-morbidities. Patients receiving NPWT during the same time period as part of standard care who were not seen by the TVN team were not included in this service evaluation. As part of routine standard of care all patients received NPWT (tNPWT or sNPWT) as an inpatient. The cases were then reviewed alongside the NPWT clinical decision making tree (Figure 2).
De-identified, routine data was extracted retrospectively from the patients’ medical records and recorded on anonymised case study templates. Clinicians were asked to document wound characteristics and NPWT product utilisation until discontinuation of NPWT or discharge from the TVN service. Standard wound photography was captured to record wound progression until discharge from the TVN service, with patient consent for photographic images recorded in the patient medical records. The data from the case study templates were aggregated and transcribed into an Excel (Microsoft Office 365) spreadsheet file. A two-step quality control of data entry was performed. The results were reported as an aggregated data set using descriptive statistics.
Results
A total of 16 anonymised case study template forms were received from the TVN service; all were included in this analysis. Clinical judgement was used to determine the most appropriate type of NPWT at TVN service presentation to meet the needs of the patient and the wound. Each case was then reviewed alongside the NPWT clinical decision tree (Figure 2). The use of NPWT was employed in two ways, using tNPWT and sNPWT. NPWT was applied until no longer clinically required, either continued to discontinuation of therapy and ‘stepped down’ to conservative dressings and discharged from the TVN service, or the patient was discharged from hospital to continue NPWT in the community. Of the 16 patients included in this service evaluation, two patients died whilst receiving NPWT. Neither of the deaths were related to their wound nor the tNPWT provided.
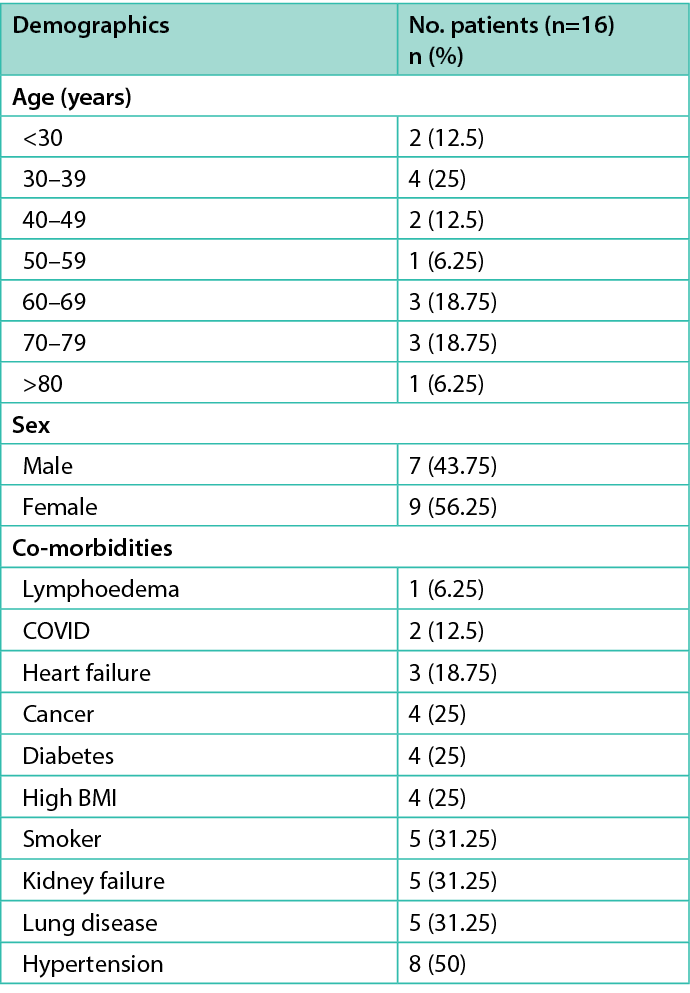
Table 1 summarises the patient demographics, whereby there was a representation of open wounds across a range of age categories, the highest percentage of patients (n=4; 25%) being between 30–39 years of age. In terms of patient gender, there were more female patients (n=9; 56.25%). There was a wide range of co-morbidities within the cohort, with eight (50%) patients diagnosed with hypertension. Kidney failure (n=5; 31.25%), lung disease (n=5; 31.25%) and current smoker (n=5; 31.25%) were the next prevalent conditions, all of which are common comorbidities that can affect wound healing.
Table 1. Patient demographics (n=16)
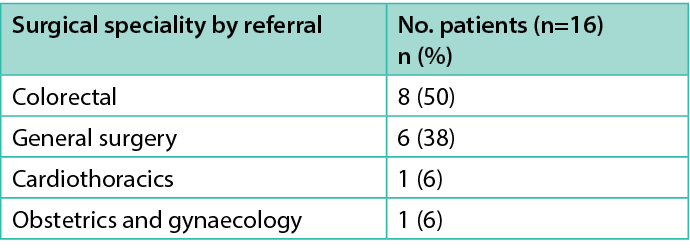
Wound type, location and duration information are shown in Table 2. Wound duration for chronic wounds was defined as a wound that has failed to heal progressively in a timely manner16 and acute wounds as being present for less than 4 weeks. The most prevalent wound types reported were dehisced surgical wounds (n=10; 62.5%), followed by abscess (n=4; 25%) and haematoma (n=2; 12.5%). All these wounds had required surgical intervention, such as the opening of a closed surgical incision, incision and drainage, or surgical debridement resulting in an open wound with or without a cavity. The anatomical location of the wounds treated by the TVN team were mostly located on the abdomen (n=9; 56.25%). The TVN team assess and review patients based on a referral system to the service from a wide range of surgical specialities within the hospital. Table 3 summarises the source of referral by surgical speciality, with the highest number of referrals for TVN from colorectal surgery (n=8; 50%), followed by general surgery (n=6; 38%), cardiothoracics (n=1; 6%) and obstetrics and gynaecology (n=1; 6%).
Table 2. Wound type and location (n=16)
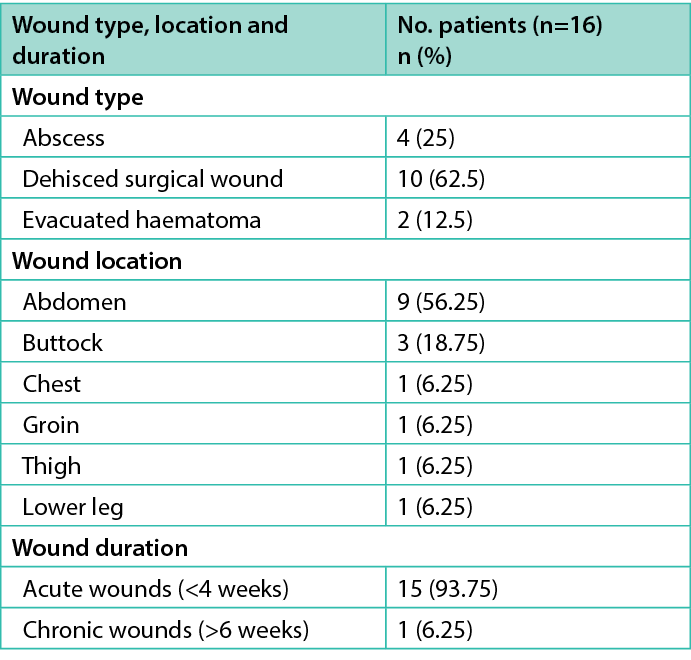
Table 3. Source of referral to TVN service by surgical speciality
All patients referred into the TVN service had received previous management of their wounds as an inpatient prior to referral. Table 4 shows the wound dressing types prior to TVN assessment, the subsequent NPWT device chosen for use and the type of filler used in conjunction with NPWT. Figure 3 summarises the rationale when choosing the most appropriate NPWT device. Most patients (n=11; 68.75%) received conservative dressings prior to the first TVN visit, with the remaining patients receiving sNPWT (n=5; 31.25%). Patients were assessed for NPWT and received the most appropriate device to manage their wound at presentation to the TVN team. A total of 15 (93.75%) patients received tNPWT, one (6.25%) received tNPWT with step-across to sNPWT, and no patients received only sNPWT. As expected, a wound filler was used for all patients receiving tNPWT, with foam being the most used (n=9; 56.25%), followed by combination of fillers, foam and gauze (n=4; 25%), and gauze alone (n=3; 18.75%). The patient who received sNPWT did not require a filler due to shallow wound depth.
Table 4. Wound management device utilisation
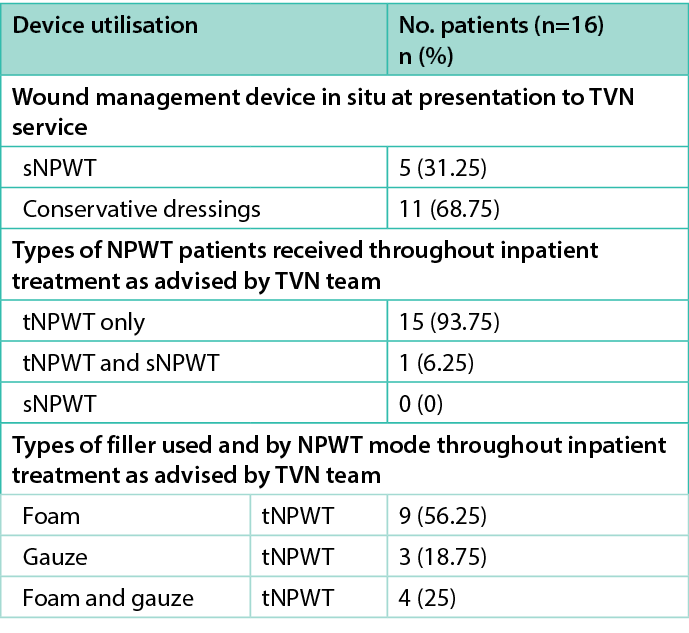
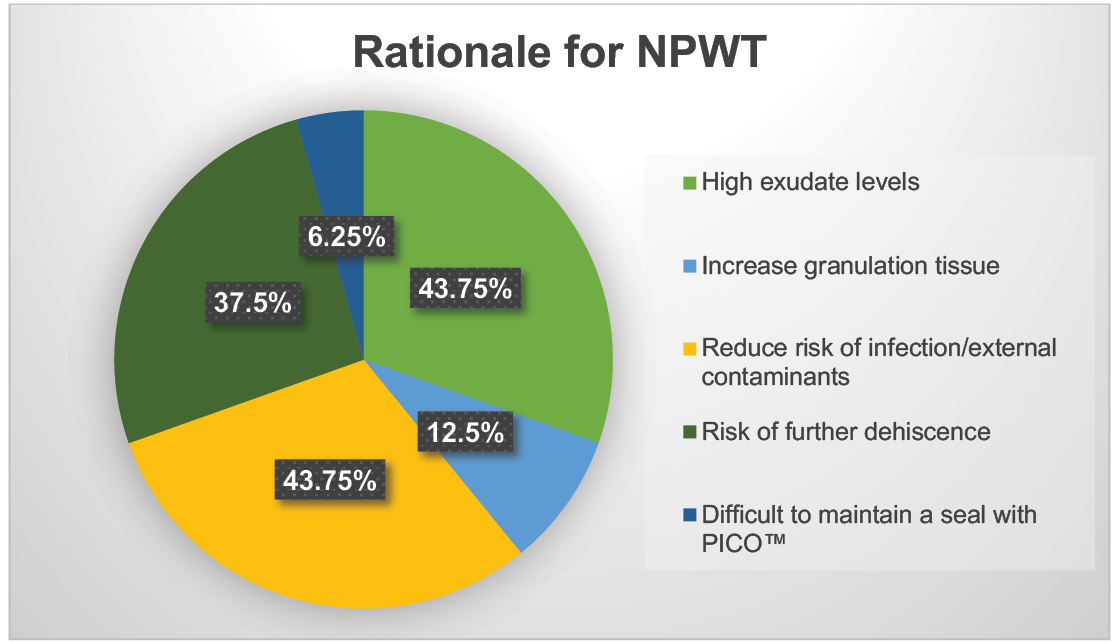
Figure 3. TVN service rationale for use of inpatient NPWT (n=16)
Table 5 details the aggregated wound type area and volume at presentation to the TVN service and at the end of TVN management. In addition, the mean average percentage change in wound area and volume is reported. It can be clearly demonstrated that the evacuated haematoma (n=2) and abscess (n=4) wounds both responded to NPWT delivery through the area (–18.01%; –97.62%) and volume (–60.87%; –93.99%) reductions, respectively. There was a large proportional increase in both wound area (228.95%) and volume (759%) for the 10 dehisced surgical wounds.
Table 5. Mean percentage change in wound dimensions per wound type at start and end of TVN service treatment period
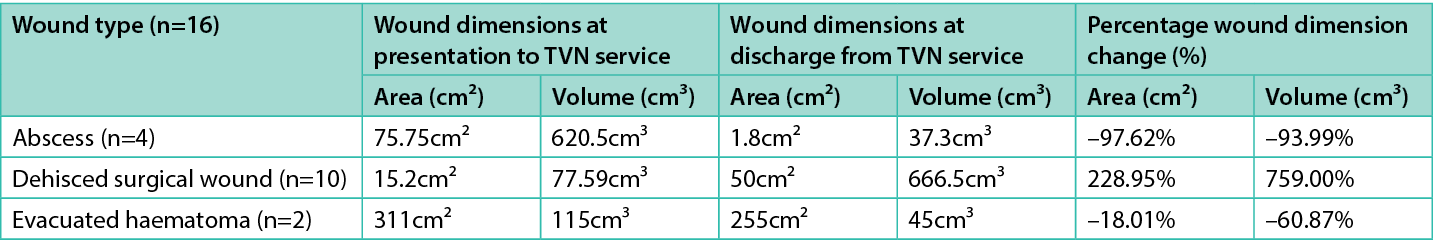
This was not unexpected as three patients presented with large dehisced abdominal wounds which, despite NPWT, continued to dehisce as their general medical condition deteriorated during treatment. The TVN shared the following quote “all products used appropriately but patients’ poor health contributed to deterioration”. A photographic series of one of these dehisced surgical wounds, from initial closed incision to full dehiscence, can be seen in Figure 4, demonstrating how the wound increased in size due to poor post-surgical recovery; tNPWT was utilised appropriately to manage the high volumes of exuding fluid and reduce the risk of further external contamination.
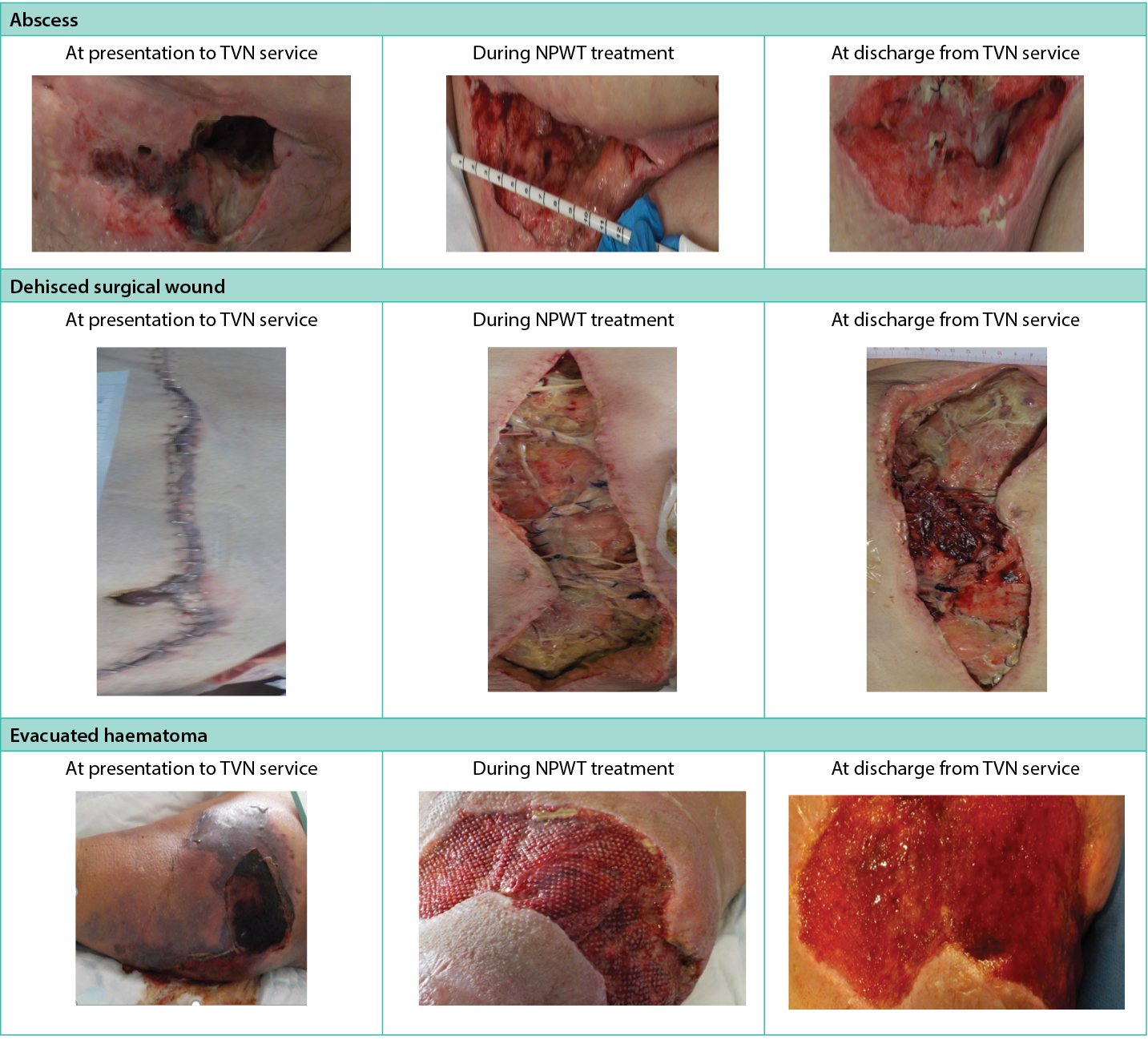
Figure 4. Wound photography during NPWT use by wound type
Surgical wound dehiscence can be defined as the rupturing or splitting apart of the margins of a closed incision12. Abdominal wound dehiscence is the most widely reported dehiscence17, and is a significant post-operative complication. Dehiscence usually occurs 5–8 days post-surgery and can range from partial to full wound breakdown18. The reasons can be technical, such as sutures breaking, inadequate splinting or patient-related factors such as wound infection and obesity17. Larger, dehisced wounds may require longer term use of NPWT, particularly when there has been significant tissue loss and wounds may be left open to heal by secondary intention19. NPWT is widely used to manage these wounds, providing stability to the wound edges by reducing lateral tension and eliminating dead space; this is important in preventing the accumulation of fluid which may increase the risk of infection.
Patients spent a mean of 6.3 days in hospital prior to seeing a TVN for assessment of their wound and commencing NPWT. Across all wound types, patients were seen on average three times by a member of the TVN team for review and treatment/application of NPWT (Table 6). In total, 156 days of NPWT were delivered across the 16-patient cohort, with the mean number of days of NPWT provided as 6.5, compared to the maximum number of days for one patient requiring 27. This longer period of tNPWT was necessary to manage the symptoms of the largest and most complex dehisced abdominal wound. Overall, the reported patient cohort spent 259 days in hospital; however, it is important to note that length of stay cannot all be attributed to their wound management. The aim of the TVN team is to provide specialist support and advice for patients with complex wounds and these complexities often arise from the patients’ condition at the time of their inpatient stay. Patients are often complex or at high risk of wound healing complications due to co-morbidities, and/or they are inpatients due to being acutely unwell which has caused their wound to become a challenge in terms of symptoms. Figure 5 describes inpatient discharge status by category.
Table 6. Patient hospitalisation (days) during TVN service wound management
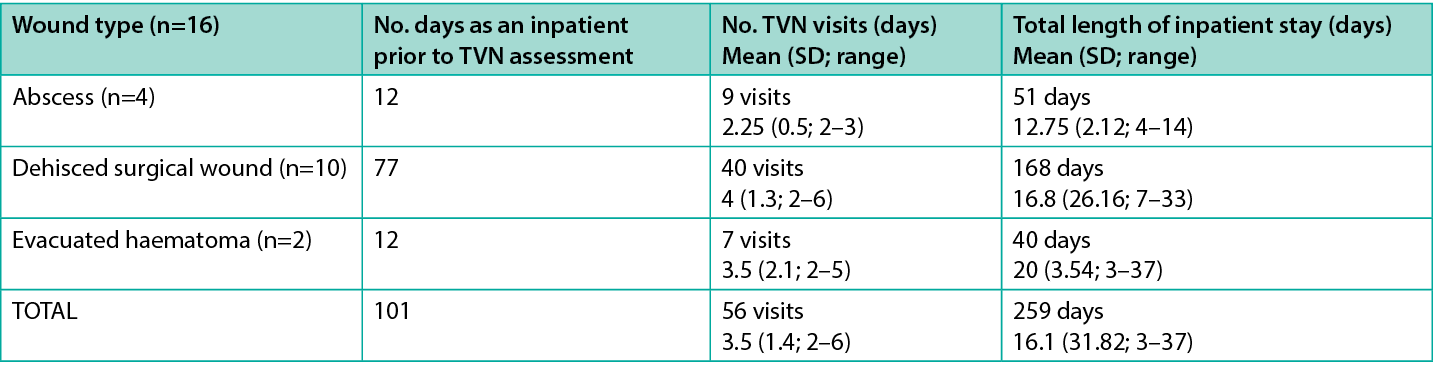
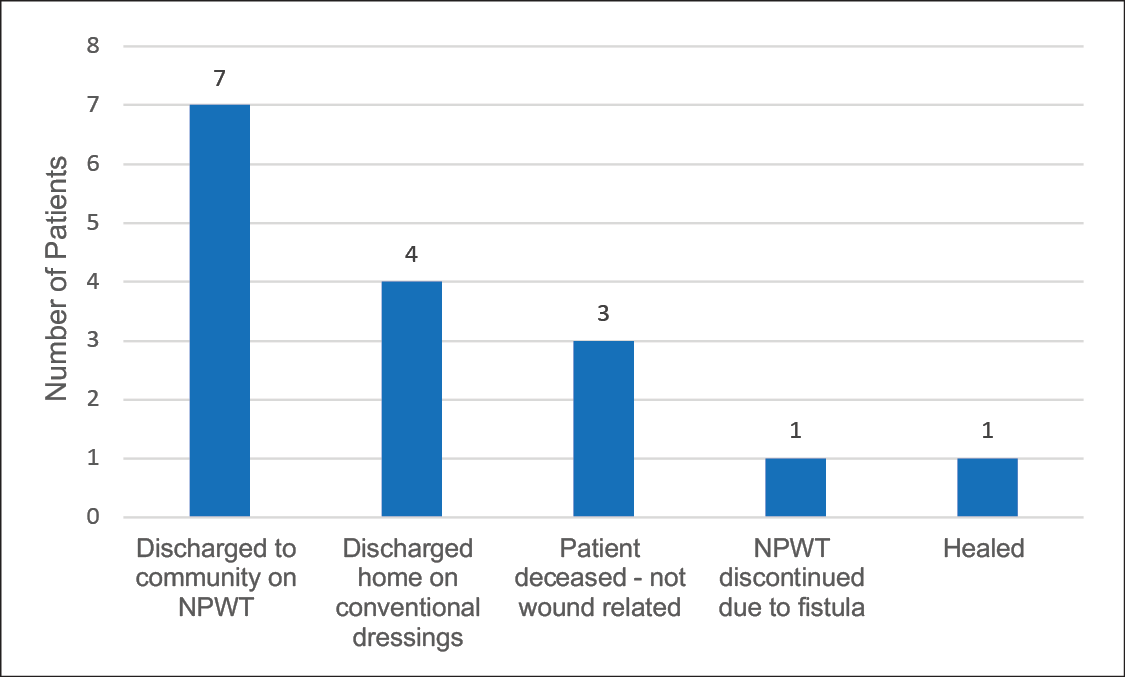
Figure 5. Clinical outcomes at discharge from TVN service (n=16)
Table 7 specifically highlights the aggregated cohort and wound types by the number of days of NPWT prior to TVN service involvement and during TVN-managed NPWT, including by modality (tNPWT or sNPWT). It is important to state that sNPWT could only be initiated if the wound met the criteria within the sNPWT device instructions around wound size, depth and exudate level as aligned to the clinical decision tree in Figure 2. Due to the complexity of all the wounds in the cohort, all commenced NPWT using the traditional system with a canister, which is designed to manage large complex wounds due to higher fluid handling capability. However, during treatment, and by consulting the NPWT clinical decision tree (Figure 2), exudate levels decreased to a level in one dehisced surgical wound which allowed the patient to step-across from tNPWT to sNPWT.
Table 7. Duration and type of NPWT received as an inpatient by wound type
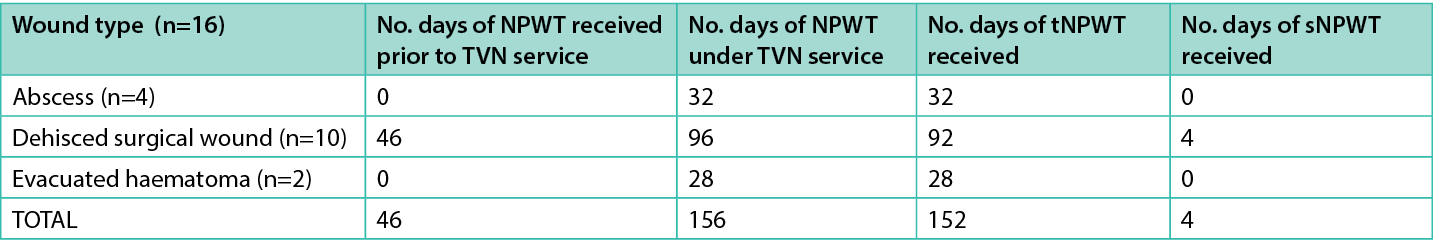
It is routine practice at the hospital that only a small proportion of patients are discharged from an acute TVN service with tNPWT still in situ; these patients are usually brought back to the outpatient care setting for dressing changes and specialist review. This is due to the challenge of logistics in device management and funding and availability of tNPWT therapy by separate organisations. However, not all community-based NHS Trusts have the same clinical decision making process in place and access to the same NPWT systems. Regular discharge from this acute NHS Trust to local community services is usually on conventional dressings with the recommendation they continue NPWT. A referral is made to the community TVN team to assess and initiate NPWT once the patient is home; however, this may lead to delay in continuation of therapy. Table 8 demonstrates where seven patients (43.75%) were discharged from hospital still requiring NPWT; zero patients were discharged from hospital with a tNPWT or sNPWT system in situ.
Table 8. NPWT usage by wound type at discharge TVN service
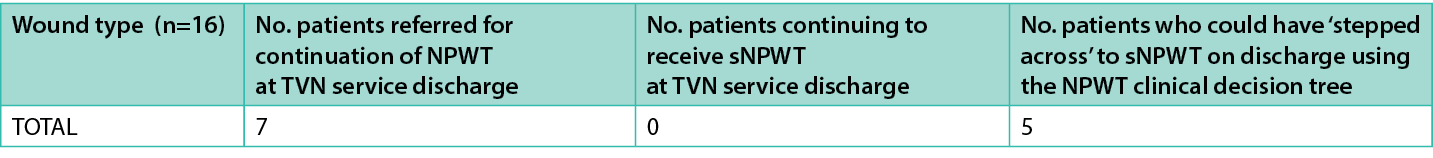
Using the NPWT clinical decision tree (Figure 2) and assessing each wound by size, depth and exudate level, it is suggested that five of the seven wounds (71.4%) discharged for continuation of NPWT could have received a sNPWT system where therapy and wound healing may have continued. This is demonstrated in Figure 6.
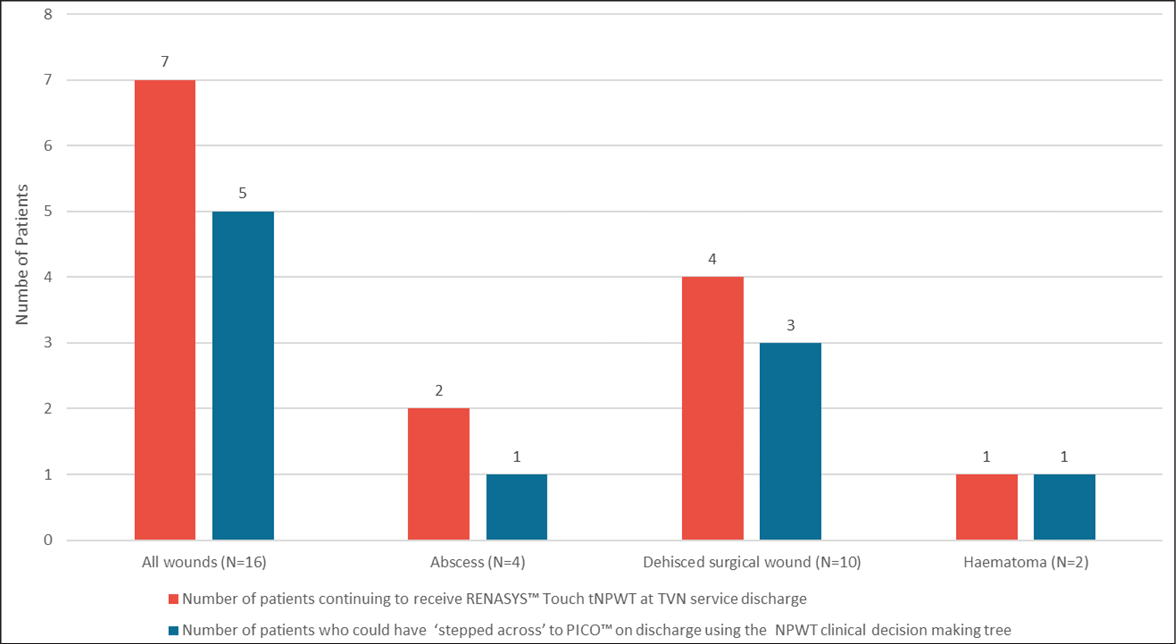
Figure 6. Number of patients continuing NPWT therapy at discharge and those who could be stepped across to sNPWT
Discussion
NPWT has become widely used in the management of complex wounds for both inpatient and outpatient care20 and has been described as an effective treatment for wounds of multiple aetiologies6,21. NPWT was initially introduced in hospital care for acute, traumatic and or post-surgical wounds22. The development of tNPWT and sNPWT devices has allowed clinicians flexibility and choice in the delivery of NPWT for treating open wounds depending on the specific need of the wound and the patient.
The focus of initiating NPWT within an inpatient care environment is often centred around ‘short term goals’ which include: evaluation of dressing solution; management of wound exudate; control of wound odour; regulation of patient pain levels; and prevention of infection10. This may allow safe and efficient management of the symptoms of a wound, therefore enabling and allowing additional supportive care and treatment to be given by other healthcare professionals. This is reflected in the complexity in the co-morbidities of the patients and their adjunctive health needs as seen by the TVN service at The Royal Stoke University Hospital.
Initiation and coordination of NPWT is often conducted by a TVN service which supports both medical and ward-based nurses in the application and management of NPWT. The TVN service also coordinates discharge to the community if continued NPWT is required; this may support the ‘longer term goals’ of NPWT, including reduction in wound exudate volume, intended wound closure through secondary suture or secondary intention healing, production of healthy granulation tissue, and reduction in wound area10. These longer term goals are often set once the patient is past the acute period of treatment and within an outpatient or home care setting.
Early initiation of NPWT can reduce the length of inpatient days in acute, intensive and long-term acute care settings23. Furthermore, NPWT may mean more wounds can be treated using fewer resources and at the same time, providing a better quality of care24; for example, NPWT can lead to fewer dressing changes, less exposure to external contaminants and less disruption to the healing process25. This is especially relevant when nursing patients with high risk of developing infection due to a deteriorating general health condition and/or co-morbidities. Initiating NPWT earlier may also facilitate speedier discharge, thus freeing up hospital beds24 and resulting in overall reduction of wound care costs14.
The average daily cost of a surgical bed at The Royal Stoke University Hospital is £350. Considering the number of inpatient days (259) across the reported cohort of 16 patients, this equates to £90,650 with an average length of stay costing £5,635 per patient. It is likely that the largest cohort of patients using the maximum hospital resources are those with dehisced surgical wounds (n=10); the highest number of inpatient days for this wound type was 138, resulting in a bed day cost of £48,300. These patients received 46 days collectively of NPWT prior to TVN service being involved, which equates to £16,100 bed day cost. It could be considered that, if these patients were referred sooner, some costs may have been saved as the patient could potentially have been discharged earlier, resulting in availability of surgical beds, increasing capacity and throughput of patients.
The NHS long term plan 2022–23 priorities and operational planning guidance26 was released to address the most urgent priorities to be addressed post-pandemic. One of the main areas of focus was to “deliver significantly more elective care to tackle the backlog”. Discharging patients home from surgical beds on appropriate therapy to continue care in the community is one way of releasing much needed bed capacity. To support this potential saving of cost and resource, five of the seven patients discharged to the community to continue NPWT could potentially have ‘stepped across’ to sNPWT from tNPWT. Stepping across patients to sNPWT prior to going home not only potentially reduces the risk of a more complicated discharge process, but the ‘switch’ to sNPWT may also release tNPWT pumps for other patients requiring NPWT therapy who, due to their wound size, depth and exudate level, are not able to receive sNPWT. Furthermore, for patients receiving NPWT, a smaller, more portable device such as sNPWT may improve their wound healing experience and quality of life24 as some patients can find the tNPWT pump and attachments difficult to move around with at home27. Statement 6 of the international consensus document14 recommends that, when appropriate, “sNPWT should be the first line modality utilized to increase patient satisfaction and quality of life”.
The implementation of the NPWT clinical decision tree at The Royal Stoke University Hospital continues to be reviewed by the TVN service and is subject to an ongoing service evaluation, whereby further data will be published on its continued utilisation within an acute NHS Trust.
Conclusion
The use of appropriate NPWT, using different modalities, has been illustrated within this service evaluation. Through the utilisation of international consensus statement guidance and a clinical decision tree, NPWT can be chosen and utilised based on key wound criteria, enabling both clinical, patient and health economic outcomes to be improved.
Implications for Clinical Practice
NPWT can be used not only to accelerate healing but also to appropriately manage the symptoms of complex and challenging wounds in the acute care setting. The use of a decision making tree for NPWT can support healthcare professionals in guiding the most appropriate mode of delivery to maximise clinical and economic outcomes. Stepping across to sNPWT, where appropriate, can support patient discharge from the acute setting.
Further research
There is a need to extend this evaluation over a longer period of time to review the continued clinical and economic outcomes.
Conflict of Interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
Author(s)
Katie Leek1 MSc, RGN, Julie M Murdoch2 PhD, Catherine H McCarthy*2 BSc (Hons), PGDip, DN, RN
1Tissue Viability and Continence Service Lead, The Royal Stoke University Hospital, Stoke on Trent, Staffordshire, UK
2Global Clinical Strategy – Advanced Wound Management, Global Clinical and Medical Affairs, Smith and Nephew, Watford, UK
*Corresponding author email Catherine.mccarthy@smith-nephew.com
References
- Guest JF, Fuller GW, Vowden P. Cohort study evaluating the burden of wounds to the UK’s National Health Service in 2017/2018: update from 2012/2013. BMJ Open 2020;10(12):e045253. doi:10.1136/bmjopen-2020-045253
- Lindholm C, Searle R. Wound management for the 21st century: combining effectiveness and efficiency. Int Wound J 2016;13 Suppl 2(Suppl 2):5–15. doi:10.1111/iwj.12623
- Drew P, Posnett J, Rusling L. The cost of wound care for a local population in England. Int Wound J 2007;4(2):149–55. doi:10.1111/j.1742-481X.2007.00337.x
- Atkin L, Geri C, Horch R, Lazaro Martinez JL. Clinician expectations in wound care during the COVID‑19 pandemic: March 2020 to January 2021. Wound Int 2021;12(2).
- Dowsett C, Bielby A, Searle R. Reconciling increasing wound care demands with available resources. J Wound Care 2014;23(11):552, 554, 556–8 passim. doi:10.12968/jowc.2014.23.11.552
- Hampton J. Providing cost-effective treatment of hard-to-heal wounds in the community through use of NPWT. Br J Community Nurs 2015;Suppl Community Wound Care:S14, S16–20. doi:10.12968/bjcn.2015.20.Sup6.S14
- Anthony H. Efficiency and cost effectiveness of negative pressure wound therapy. Nurs Stand 2015;30(8):64–70. doi:10.7748/ns.30.8.64.s50
- Brownhill VR, Huddleston E, Bell A, et al. Pre-clinical assessment of single-use negative pressure wound therapy during in vivo porcine wound healing. Adv Wound Care 2021;10(7):345–356. doi:10.1089/wound.2020.1218
- Borys S, Hohendorff J, Frankfurter C, Kiec-Wilk B, Malecki MT. Negative pressure wound therapy use in diabetic foot syndrome-from mechanisms of action to clinical practice. Eur J Clin Invest 2019;49(4):e13067. doi:10.1111/eci.13067
- Apelqvist J, Willy C, Fagerdahl AM, et al. EWMA document: negative pressure wound therapy. J Wound Care 2017;26(Sup3):S1-s154. doi:10.12968/jowc.2017.26.Sup3.S1
- Malmsjö M, Huddleston E, Martin R. Biological effects of a disposable, canisterless negative pressure wound therapy system. Eplasty 2014;14:e15.
- World Union of Wound Healing Societies. Consensus document: surgical wound dehiscence: improving prevention and outcomes. Wounds International; 2018.
- Rossato M, Ryrie M, Robinson M, Searle R, Murdoch J. Use of NPWT as part of a hospital and home wound management service. J Community Nurs 2021;35(4):50–57.
- Hurd T, Kirsner RS, Sancho-Insenser JJ, et al. International consensus panel recommendations for the optimization of traditional and single-use negative pressure wound therapy in the treatment of acute and chronic wounds. Wounds 2021;33(suppl 2):S1-s11.
- Health Research Authority. Defining research. http://www.hra-decisiontools.org.uk/research/docs/definingresearchtable_oct2017-1.pdf
- Frykberg RG, Banks J. Challenges in the treatment of chronic wounds. Adv Wound Care 2015;4(9):560–582. doi:10.1089/wound.2015.0635
- Sandy-Hodgetts K, Carville K, Leslie GD. Determining risk factors for surgical wound dehiscence: a literature review. Int Wound J 2015;12(3):265–75. doi:10.1111/iwj.12088
- Rosen R, Manna, B. Wound dehiscence. Stat Pearls: Treasure Island; 2023.
- Dumville JC, Land L, Evans D, Peinemann F. Negative pressure wound therapy for treating leg ulcers. Cochrane Database Syst Rev 2015;2015(7):CD011354. doi:10.1002/14651858.CD011354.pub2
- Bobkiewicz A, Banasiewicz T, Ledwosinski W, Drews M. Medical terminology associated with negative pressure wound therapy (NPWT): understanding and misunderstanding in the field of NPWT. Neg Pressure Wound Ther 2014;1(2):69–73.
- Apelqvist J, Armstrong DG, Lavery LA, Boulton AJ. Resource utilization and economic costs of care based on a randomized trial of vacuum-assisted closure therapy in the treatment of diabetic foot wounds. Am J Surg 2008;195(6):782–8. doi:10.1016/j.amjsurg.2007.06.023
- Moffatt CJ, Mapplebeck L, Murray S, Morgan PA. The experience of patients with complex wounds and the use of NPWT in a home-care setting. J Wound Care 2011;20(11):512, 514, 516, passim. doi:10.12968/jowc.2011.20.11.512
- Baharestani MM, Houliston-Otto DB, Barnes S. Early versus late initiation of negative pressure wound therapy: examining the impact on home care length of stay. Ostomy Wound Manage 2008;54(11):48–53.
- Dowsett C, Davis L, Henderson V, Searle R. The economic benefits of negative pressure wound therapy in community-based wound care in the NHS. Int Wound J 2012;9(5):544–52. doi:10.1111/j.1742-481X.2011.00913.x
- Payne WG, Posnett J, Alvarez O, et al. A prospective, randomized clinical trial to assess the cost-effectiveness of a modern foam dressing versus a traditional saline gauze dressing in the treatment of stage II pressure ulcers. Ostomy Wound Manage 2009;55(2):50–5.
- NHS England. NHS long term plan 2022–23 priorities and operational planning guidance. NHS England; 2022.
- Janssen AH, Mommers EH, Notter J, de Vries Reilingh TS, Wegdam JA. Negative pressure wound therapy versus standard wound care on quality of life: a systematic review. J Wound Care 2016;25(3):154, 156–9. doi:10.12968/jowc.2016.25.3.154
