Volume 25 Number 1
Benefits of inelastic and short-stretch bandages in leg ulcer: a narrative review
Maria F Morales-Labarca, Claudia N Ramirez Castro
Keywords compression bandage, wound healing, Leg ulcer, inelastic bandages, short-stretch bandages
For referencing Morales-Labarca MF & Ramirez Castro CN. Benefits of inelastic and short-stretch bandages in leg ulcer: a narrative review. Journal of Wound Management 2024;25(1):22-30.
DOI
10.35279/jowm2024.25.01.06
Submitted 20 October 2023
Accepted 8 November 2023
Abstract
Compression therapy (CT) in venous leg ulcer (VLU) treatment has been further investigated, obtaining such favourable results – by improving chronic venous hypertension and enhancing other positive effects in its pathophysiology – that it is currently the cornerstone of its treatment. However, leg ulcers (LU) of non-venous aetiology can also benefit from CT. To date, current contraindications for CT are minimal. Despite these benefits, only 50 - 60% of these patients receive CT as part of their treatment, resulting in lower healing rates than expected.
Inelastic bandages (IB) and short-stretch bandage (SSB) have multiple benefits in LU and VLU treatment as they provide low resting pressures and high working pressures >60mmHg in standing and walking, improving venous haemodynamics. The aim of this narrative review was to describe the benefits of IB and SSB in the treatment of LU non venous etiology.
We conducted a non-systematic review of literature guided by the Scale for the Quality Assessment of Narrative Articles (SANRA), regarding the benefits of IB and short-stretch bandage (SSB) CT systems in LU non venous etiology. IB are safety systems which can be useful in multiple LU aetiology, including chronic venous hypertension, diabetes, peripheral arterial disease (PAD) and inflammatory diseases, reducing pain, time for wound healing, oedema, exudate, inflammatory process, and sanitary costs. IB and SSB have benefits that other elastic materials are often unable to achieve and, when their knowledge and training are well established, they have been shown to improve LU patient care.
Key messages
- Compression therapy (CT) is the cornerstone treatment in people with Venous Leg Ulcer (VLU) or any type of leg ulcer (LU), leading to wound healing. However, only around half of the patients are beneficiaries for this kind of treatment.
- Inelastic bandages (IB) are safety systems which can be useful in multiple LU aetiologies (for example diabetes, peripheral arterial disease (PAD) and inflammatory diseases), and healthcare professionals should aim to incorporate these in their treatment.
- IB and short-stretch bandages (SSB) reduces healing time, pain, oedema, exudate and inflammatory process, improving patient quality of life (QOL)
Introduction
Compression therapy (CT) is a fundamental pillar in the treatment of leg ulcers (LU) and has been practised for over 300 years1,2. Because venous leg ulcers (VLU) are the most prevalent chronic LU3–6, affecting 1–2% of the population, increasing with age3–6, CT has been extensively studied in this type of wound, obtaining such favourable results that it is currently the cornerstone of its treatment together with the early surgical resolution of venous reflux7–13. Relative frequencies of other aetiologies (including arterial, mixed and other types) are between 5–30% of chronic lower limb wounds9. However, LU of non-venous aetiology can also benefit from CT, by acting on inflammation process and gravity on legs14,15. To date, current contraindications for CT are minimal16–18. Despite these benefits, only 50 - 60% of these patients receive CT as part of their treatment19, resulting in lower healing rates than expected13,20–24.
When there is no arterial involvement, the necessary level of CT to treat LU and VLU should be high compression, that is 40mmHg7,12,13,21,25–29, and when an appropriate vascular assessment has been done. Current expert consensus indicate if there are no distal peripheral pulses, an Ankle Brachial Pressure Index (ABPI) should be performed so all patients with LU and palpable pulses can receive this compression level24. It is important to consider that patients with diabetes or end-stage chronic kidney disease could have an inaccurate ABPI result due medial calcification24. Some stiff bandages as inelastic bandages (IB), short-stretch bandage (SSB) and multicomponent SSB (MSSB) can provide low resting pressures and high working pressures >60mmHg in standing and walking21,30, improving venous haemodynamics, when compared with elastic bandages and elastic compression stockings31,32. In fact, the stiffer the compression product, the greater the effectiveness in peak pressure on calf pump while walking8. To achieve these pressure ranges in an elastic bandage, they would also have to be applied at rest, which would be intolerable for patients and could increase the risk of some side effects related to the high level of rest pressure30. However, while O’Meara et al state that multicomponent systems containing an elastic bandage appear to be more effective than those composed mainly of IB materials, and two-component bandage systems appear to perform as well as four-layer bandages (4LB)10.
It was therefore considered necessary to carry out an investigation of the evidence to make a better therapeutic understanding of IB and SSB. Considering the conflicting evidence between different types of dressing materials, an investigation of the current evidence is necessary to achieve a better therapeutic understanding of BI and SSB.The aim of this narrative review was to describe the benefits of IB and SSB in the treatment of LU non venous etiology.
Methods
A non-systematic review of literature was carried out which was guided by the Scale for the Quality Assessment of Narrative Articles (SANRA)33. A search was carried out in five scientific databases – Pubmed, Web of Science, CINAHL, SciELO and Cuiden. The Boolean operators AND and OR were used, with the following keywords: inelastic bandages, short-stretch bandages, leg ulcer, wound healing. Filters used were English, Spanish and Portuguese languages, and publication years 2013–2023, all study design and international consensus document by scientific associations were included, except grey literature. A final result of 30 articles was obtained for complete reading plus nine consensus and manually selected articles which were independently analysed by two researchers where the inclusion criteria were studies that address treatments with IB and SSB in people with any type of LU (Figure 1).
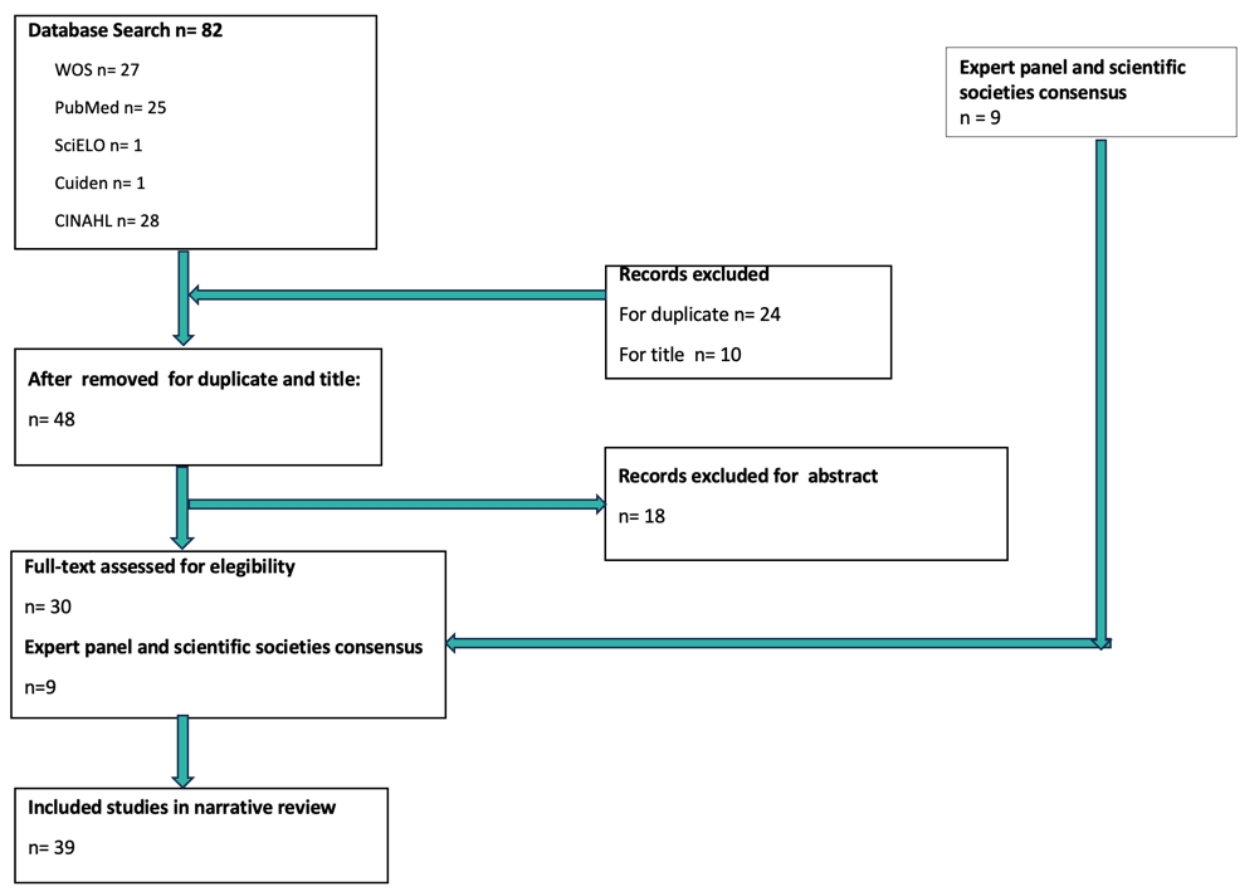
Figure 1. Flow diagram for the review process
Results
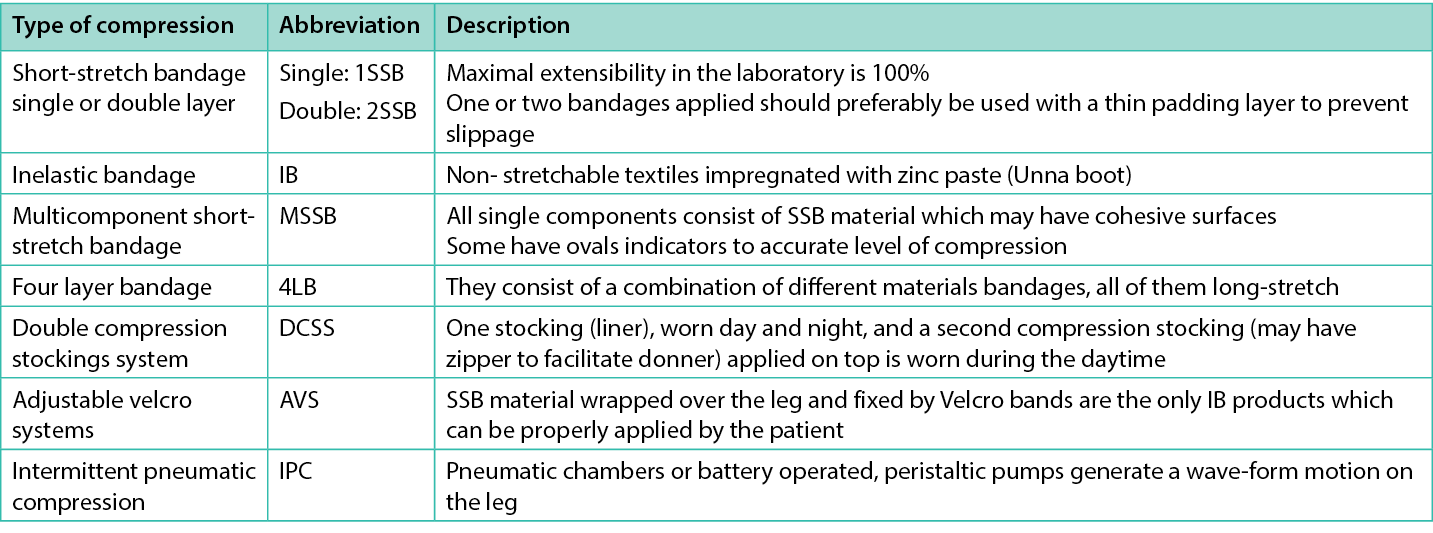
Analysis of articles and consensus led to describing eight dimensions to consider regarding the clinical decision of the use of IB and SSB in the treatment of people with any type of LU. The different CT systems appearing in the research are described in Table 1.
Table 1. Compression Therapy systems that appeared in the literature review (adapted from Partsch21)
Faster healing time
A Cochrane Systematic Review that evaluated the effectiveness of using bandages or compression stockings compared with not using them in the treatment of VLU determined that using CT doubles the probability of healing, compared with not using it, with a moderate level of evidence11. Subsequently, evidence supports the use of all forms of CT in comparison to no CT for treating LU24,34. In fact, in a RCT comparing the use of SSB with not using CT, the rates of complete healing at 3 months was 71% versus 25% respectively34. In addition, 21% of people who did not use CT experienced an increase in the size of their LU within 3 months34.
Dolibog et al, in a clinical randomised pilot study (70 participants), compared three types of CT in persons with superficial deep venous reflux alone or combined with the segmental variety – intermittent pneumatic compression (IPC), stockings and SSB. The results showed that 2SSB improved the area of the wound at 15 weeks (p=0.01), but it was not better than the other CT systems. The authors conclude it could be related to the fact that it is not a multilayer system with 40–50mmHg35. The same authors in another study mentioned that MSSB are more effective in achieving wound healing, probably because they maintain pressure and rigidity, than those that use only one type of material; they are also cost-effective by reducing healing time36 (Figure 2). In addition, according with Zarchi and Jemec, this may be related to the greater accuracy that MSSB can provide, compared to other types of bandages; they showed in their study that more nurses achieve the level of compression expected when using this kind of system37 (Figure 3). Similar conclusions about multicomponent systems being superior to single component systems were mentioned by Mauck et al on a systematic review and meta-analysis38. In fact, results from a scoping survey of registered nurses showed that the most used type of CT was MSSB39.
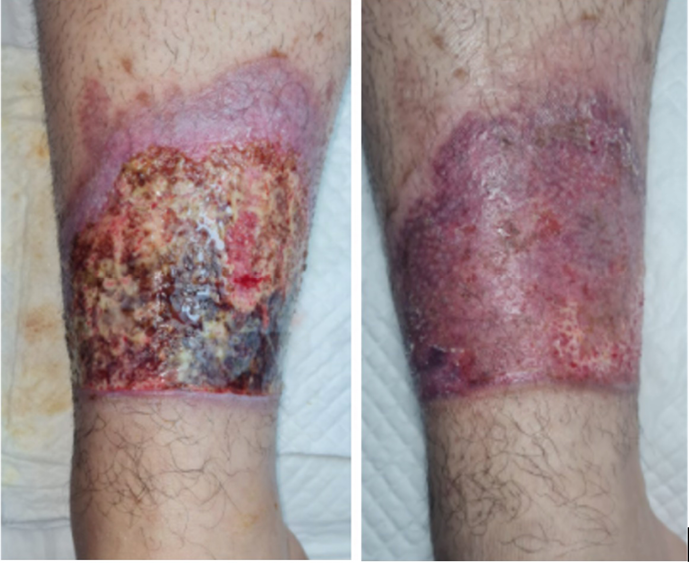
Figure 2. LU burn treated with multicomponent SSB which healed within 4 weeks

Figure 3. Multicomponent SSB with indicators
In a meta-analysis that included seven studies and analysed 1446 ulcers to compare healing times between 4LB and 2SSB, it was determined that healing time is similar for both systems, with no statistically significant differences between them – 73.6±14.64 days for ulcers treated with 4LB and 83.8±24.89 days for 2SSB. The authors highlighted the relevance of training of healthcare providers to achieve those levels of compression, and that selection must based on evidence, patient tolerability and preferences40. In fact, Stücker et al showed in their narrative review a MSSB clinical evaluation that revealed no significantly different healing rates within 2 months of treatment compared to 4LB41. However, Nelson and Harrison showed in a meta-analysis result that in a comparison between 4LB and 2SSB, there was no superior benefit in favour of 4LB (hazard for healing with 2SSB over 4LB 0.88, 95% CI 0.76–1.02). The authors concluded that when a new product is compared in a clinical context where greater skills with the old product has already been generated, learning curves may bias its use42.
LU healing rates are connected to ankle range of motion and bulk. 4LB can impair the dorsiflexion and consequently diminish the contraction of a calf pump to improve venous return and lymphatic drainage43. Brambilla and colleagues conducted a study with 63 participants to determine an holistic treatment involving CT and moist wound healing. The cover of the wounds were resolved with bacterial binding dressing, three-layer silicone foam, periwound skin protectant, 1SSB and IB double compression stockings system (DCSS) where oedema was controlled. In 85% of cases, a reduction in size or complete wound healing was achieved within 12 weeks. Wounds that had not healed in that timeframe had reduced in size, ranging from 43.8–92.4%44.
In a RCT by Mosti and colleagues comparing other type of IB devices with SSB, they found there was no statistical significance difference in healing rate between adjustable velcro systems (AVS) and MSSB45 when it is properly applied through training healthcare professionals. Paranhos et al conducted a systematic review and meta-analysis including eight studies and 643 patients to evaluate the efficacy of IB, showing that IB had best results for wounds with areas more than 10cm2, and elastic bandages with areas below 10cm2. In their conclusions, a moderate degree of evidence showed there was no difference using IB regarding the healing rates of VLU; nevertheless, they claim that IB is a low cost alternative to reduce venous hypertension and oedema in reduced public health resources, which boosts the treatment of VLU. Also, they mentioned its effectiveness depends on correct application technique, healthcare professional involvement, cooperation and patient compliance46.
A mixed-treatment comparison (MTC) meta-analysis of high-CT treatments for VLU showed that among MSSB, SSB, IB, 4LB and DCSS, MSSB was the most effective47. Considering that data came from two small RCTs; is crucial aiding the interpretation of these findings based in the quality of the evidence.
Reduction of oedema and exudate
CT is capable of controlling oedema and exudate, by reducing capillary filtration, moving fluid from compressed tissues to non-compressed tissues, and improving lymphatic drainage. Additionally, it increases venous blood flow and reduces venous pressure and pooling11,48. According to Atkin et al, CT should be used to control wound moisture when there is oedema since it improves tissue oxygenation and promotes an adequate environment for cell and keratinocyte migration, in addition to the consequent reduction in exudate, by reducing interstitial oedema22. This allows a shorter distance between tissue, capillaries and lymphatic vessels, improving supply of oxygen, nutrients, antibiotics and other cellular products that enhance tissue conditions and even treat infections such as lower limb cellulitis49.
Ritchie mentioned IB as first choice for patients with a large amount of reducible oedema and exudate, on both mobile and immobile patients and unusually shaped limbs, before changing to another type of CT like DCSS or AVS in VLU43. This change of CT type was made in an holistic treatment of VLU in the initial oedematous phase44. Despite any venous aetiology, hydrostatic pressure in the upright position can produce oedema and leads to a LU50. - According to Bjork and Ehmann oedema classification, watery oedema decrease easily with multilayer bandages. Putty tissue and woody tissue oedema (whose have more fibrotic damage), reduces better with rigid materials, since it improves lymphatic drainage8. According to Partsch and Mosti, SSB are capable of quickly reducing oedema in lower limbs, so it is important to reapply frequently or installing them with a 50mmHg in the initial oedematous phase. This is related to the fact that 20% of the loss of compression level is caused by the rapid reduction of oedema51 (Figure 4). Although benefits among different CT are clear, clinical judge and patient preferences must consider in the election when is a large, oedematous or awkwardly shaped legs47.
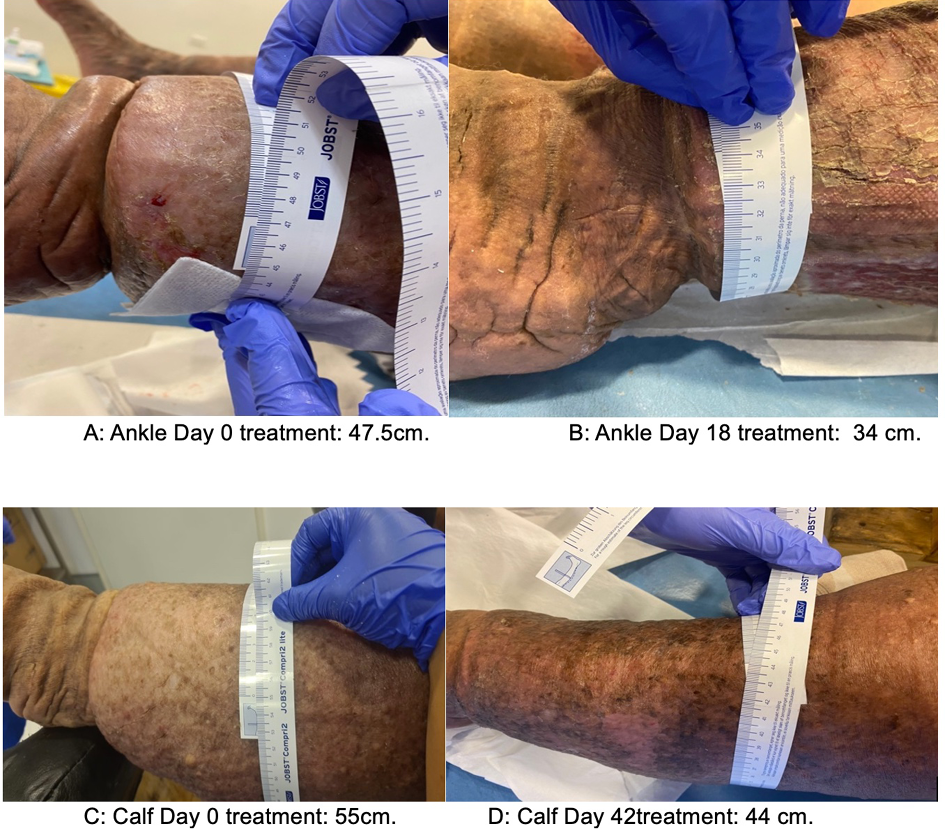
Figure 4. Oedema reduction with IB systems and changes three times a week initially and then twice weekly
Use in PAD and improvement of capillary flow
It is possible to use stiff CT systems in patients with mixed ulcer (MU) and arterial ulcers (AU), when ABPI is between 0.5–0.8, avoiding <0.524,50,52,53. Supporting this statement, an Expert Consensus of Vascular Nurses recommends application just with SSB <40mmHg of compression in ABPI 0.6–0.852. Isoherranen et al reported on a systematic review methodology document, a study that showed the promotion of healing through 20–30mmHg CT in MU and AU, resulting in similar healing rates with VLU, 60% (n=24) and 65% (n=20), respectively. The authors concluded that if there are no contraindications, CT should be incorporated in the treatment from the patient’s first visit24.
According to a mathematical model to compare 3LB with 2SSB in wound healing rates, one of the variables that they include was improving oxygen flow through the capillary perfusion that both bandages could produce. Although this was not the main result, this study mentioned that more external pressure on the veins could increase oxygen transport over the wound edge54. Sanchez and Partsch conducted a case report on a 72-year-old woman with a 3-month history of LU, accompanied by continuous pain, signs of inflammation, and oedema. ABPI was measured at 0.42, and the diagnosis indicated chronic ischemia of grade IV, deemed non-revascularizable. As part of the treatment plan, the patient initiated pharmacological therapy to alleviate pain and manage underlying conditions. Additionally, her leg was wrapped with a first fixation layer and a 1SSB, with precise daily supervision by medical professionals applying 50mmHg pressure. After 4 months, the LU exhibited complete healing. The authors concluded that CT reduced oedema and inflammation while accelerating capillary flow, leading to an increase in shear stress. This, in turn, triggered the release of anti-inflammatory mediators from endothelial cells50. Also, emphasised the importance of such interventions being administered by trained healthcare providers.
Decrease in inflammatory process
Ritchie, in her CT literature review, mentioned that patients with LU and a diagnosis of diabetes, rheumatoid arthritis/vasculitis and presentation of atypical distribution of ulcers were situations that needed to be referred for specialist assessment, but not as a contraindication for CT43. In fact, Haesler, in her evidence summary, mentioned a best practice recommendation that vasculitis may have a higher risk for individuals, but may be still indicated34. According to Isoherranen et al, once advanced or critical PAD has been ruled out, CT should be used in all patients with LU and oedema, even if the cause is not venous. Pyoderma gangrenosum or vasculitic ulcers are inflammatory disease and very painful ulcers, and CT can reduce tissue deposits of immunological complexes, so it is recommended to start with low compression levels of 20mmHg to achieve 30mmHg increase gradually based on tolerance55 (Figure 5). These low compression levels at rest can be achieved with IB or SSB. CT has been used safely in LU with inflammatory aetiology, reducing the use of corticosteroids, reducing inflammation, odour, pain and oedema, without major complications56. In addition, it is able to aid the debridement of devitalised tissue due to the control of underlying inflammation (Figure 6), allowing it to pass from this stage to the next one; this was shown within an evaluation of a MSSB system in 19 patients who showed improvement in type of tissue in 63% of patients within 4 weeks57.
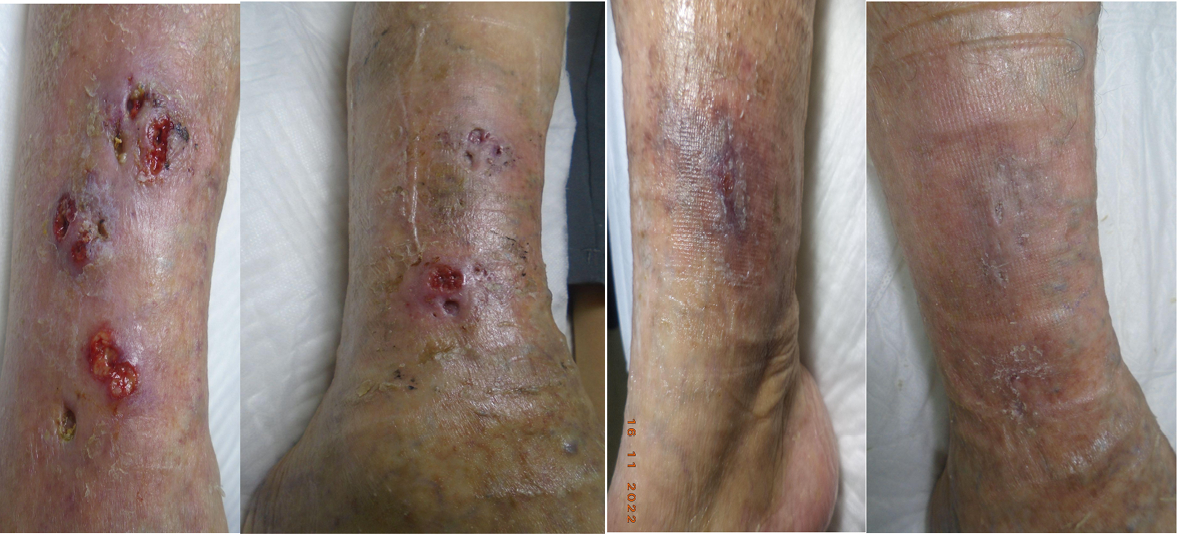
Figure 5. Pyoderma gangrenosum treated with i) just with dressing wound, ii) since starting with a SSB, iii) reduction of 50% of wound area at 4 weeks of treatment and iv) healed within 4 months

Figure 6. 2SSB allows secondary debridement in mixed VLU
Cost-effectiveness
Albuquerque et al presented a systematic literature review, to compare the effectiveness of SSB with other types of treatments, among other objectives. One of the included RCTs demonstrate there is no significant difference between 4LB and 2SSB. Another RCT included a small sample of 45 participants, finding 2SSB more expensive than 3LB48. Sodré et al conducted a cost-effectiveness study that considered 12 RCT of LU comparing multilayer bandages with IB (Unna boot) and 2SSB. The results determined that multilayer bandages are the most cost-effective option (including 4LB and MCSS) in terms of costs and healing times, followed by the IB and then 2SSB. Treatment with IB was found to have the lowest cost, while the 2SSB had the highest cost, considering additional factors such as padding layer and bandage washing, which increased total costs58, but still maintained its effectiveness. Considering the frequency of changing bandages as part of the effectiveness and costs, Partsch and Mosti described the concept pressure time integral (PTI) as distribution of the pressure dose over time. PTI for SSB is more stated when the change of bandages is every 2–3 days. To maintain this PTI through 7 days, SSB and MSSB should be wrapped with an initial pressure greater than 50mmHg51, then change the bandage when it is loose, or based on healing needs52.
Combination with other types of bandages
Partsch described a useful and old procedure to treat large ulcers and heavily congestive legs, the Fischer technique, developed in 1910 by a pupil of Unna, Heinrich Fischer. This historical practice is an alternative among stiffness materials and mixes two IB, where an IB (zinc oxide paste bandage) is used plus a 100% cotton SSB to deliver compression >50mmHg at rest and greater compression during calf contraction59 (Figure 7). It is indicated to treat LU and lymphoedema when ankle pressure is >60mHg, but it must be applied with an appropriate padding in this area to protect the Achilles tendon from the high pressure.

Figure 7. Modified Fischer technique for the treatment of LU and lymphoedema.
A: Wound dressing. B: Synthetic pad bandage. C: Zinc paste Unna boot D: SSB 100% cotton. D: Cohesive bandage for slipping prevention
Pain reduction
Pain is one of the most important issues related with compromised quality of life (QOL)48. According to the expert consensus of Ousey et al, CT has beneficial effects in addition to the healing of wounds/ulcers, such as improving lymph drainage, reducing oedema and pain60. A study by Mosti et al. included 180 participants with VLU and mixed LU to compare treatment with foam esclerotherapy and 1SSB applying in supine position >60mmHg in first group and 40mmHg in second group. The pain associated with a LU was able to be decreased with IB materials (p≤0.001) in 4 weeks in people with VLU without arterial involvement, and 8–12 weeks in a person with MU (ABPI 0.5–0.8)61. According to Albuquerque et al, in a systematic review of the benefits of IB materials in VLU treatment, a randomised control trial (RCT) showed that 4LB and 1SSB both improve QOL but, to reduce pain, 1SSB are more likely to have better results in QOL48. Paranhos et al, in a systematic review and meta-analysis, demonstrated all VLU treated with CT improved pain, although with no statistically significant difference among groups including 4LB, elastic bandage and IB46.
As part of LU treatment, pain must be part of assessment and interventions and a plan for analgesia should be included through all processes according to patient feedback43. In addition, raising legs, avoiding prolonged periods of sitting and standing, and daily walking should be incorporated into the patient’s routine.
Better adherence to treatment and QOL
The QOL of people with LU can be impaired by wound status, pain, oedema, job loss (including leisure and social activities), depression, co morbidities and overall treatment costs44,48. Brambilla and colleagues mentioned patients may have better QOL if their treatment includes compression bandages that are capable of reducing wound exudate and oedema. Based on a systematic review by Shi et al that included four studies and 859 participants, it was found that the use of CT versus not using compression reduces pain and may improve disease-specific QOL in 12 weeks to 12 months11.
A recent meta-review compared different types of CT, including elastic, IB materials and number of layers, and their results showed that it was not possible to conclude which CT systems represent the most effective for healing VLU. What they do highlight is the importance of correct application and patient compliance to maximise the probability of wound closure, because it is known that CT leads LU to wound healing62. Nevertheless, IB and SSB are more comfortable and tolerable for patients because IB materials lose pressure immediately after installing them, without losing their effectiveness, and are tolerable during night wear49. This comfort and tolerance to the bandages may generate greater adherence to the treatment of CT.
In this context, the more rigid the CT system, the lower the dose of compression that can be indicated and specially delivered by IB, thereby enhancing patient comfort8. However, AVS can contribute to patient QOL, related to skin care and easily donning, improving their self-autonomy63,64, but not all clinical contexts and patients can afford this type of device. In this context, IB and SSB still remain a good option for patients, although CT should be discussed with patients to consider their choices to improve concordance with the treatment plan43. According to a systematic review that explored evidence for multicomponent systems in the treatment of VLU, it was reported that MSSB, combining a first layer pad and SSB cohesive second layer, are more comfortable and tolerable than other systems. MSSB were capable of improving the ability to carry out daily activities and wear usual footwear, and showed a better aesthetic aspect65. A study that determined a holistic treatment strategy with 2SSB, DCSS and moist wound healing in VLU reported a positive impact in patient QOL. After this treatment, there was a shift from high to low impairment during the period study and from low to no impairment in tasks such as lifting objects, walking, standing and household and gardening chores44.
Limitations of review
It is acknowledged that most of articles included in this narrative review focused on VLU, necessitating the inclusion of expert consensus guidelines of LU from other etiologies. Furthermore, if the review were to be conducted again, it would be advisable to utilize an alternative database to broaden the scope of results related to the treatment of lLU.
Conclusion
IB and SSB have different benefits to patients with LU, specially in initial phase of LU. MSSB can achieve healing rates faster than other types of CT. In people with PAD, it is possible to use stiff CT systems, with modified compression, avoiding ABPI <0.5. If there are no contraindications, CT should be incorporated in the treatment plan from the patient’s first visit. LU and a diagnosis of diabetes, rheumatoid arthritis/vasculitis, pyoderma gangrenosum and presentation of atypical distribution can be benefit with CT with similar level of compression as people with PAD. Additionally, in large ulcer and heavily congestive legs, a combination of different types of IB and SSB can be recommended.
It is emphasised that health professionals should be appropriately trained to perform the application adequately in both special cases and the general population with LU to achieve the expected level of compression. When clinicians select a type of IC and SSB, costs should be considered as MSSB are more cost-effective than other types of elastic and IB materials.
In terms of QOL, pain stands out as one of the most significant concerns. It can be alleviated through CT, with superior outcomes observed when using 1SSB within a specific timeframe. It is essential to incorporate a plan for analgesia. Additionally, patients find IB, SSB, and MSSB more comfortable and tolerable. As the rigidity of the CT increases, a lower dose of compression can be recommended and administered through IB materials, thereby enhancing patient QOL. Finally, an holistic approach that includes wound bed preparation and considers the benefits of SSB can enhance QOL and improve wound healing in LU.
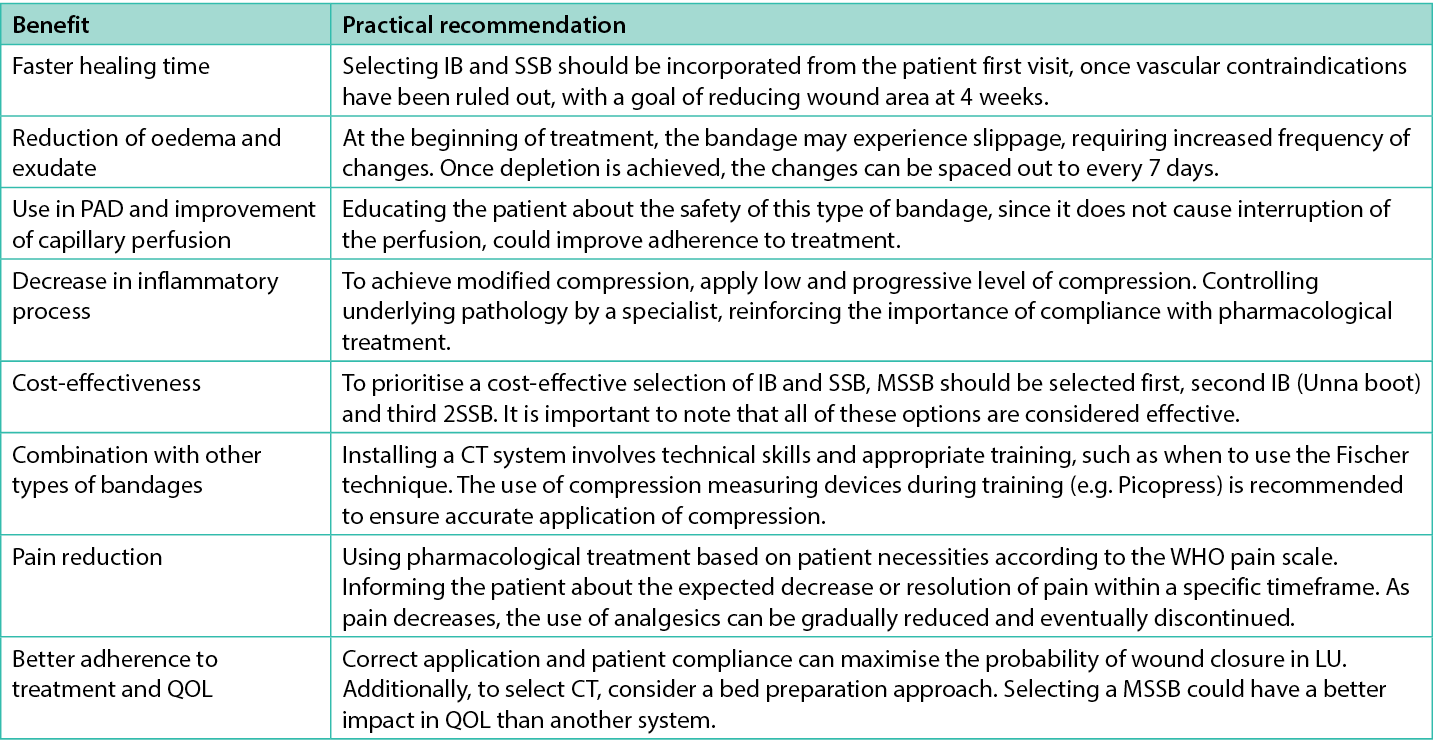
Table 2. Benefits of IB and SSB and practical recommendations
Implication for clinical practice
- IB and SSB are capable of giving benefit to LU, regardless of their aetiology.
- MSSB can improve wound healing cost effectiveness, pain and QOL in people with LU.
- Patients with inflammatory diseases, including PAD, can heal their LU with modified compression through IB and SSB.
- Healthcare professionals must be trained to achieve expected levels of compression to treat LU of different aetiologies.
Further research
We believe that additional research is necessary concerning the effectiveness of a MSSB with visual indicators. This research can aid healthcare professionals in enhancing the application of this type of CT for the treatment of LU without venous etiology. This recommendation stems from the observation that most of the research in this field has been conducted with 4LB in the context of VLU.
Acknowledgments
We would like to thank PhD Jessica Salvo Arias and PhD(c) Francisca Villagran Silva for the technical support, and Giselle Avila Gonzalez, Tamara Castro Pérez, and Cristian Valdivia for facilitate pictures of some of the clinical cases.
Ethical Considerations
All of the images included in this article have informed consent of each patient.
Conflict of Interest
The authors declare that one of them works for a laboratory that markets compression therapy products (Maria Fernanda Morales-Labarca), however, there are no conflicts of interest on the part of Claudia Ramirez Castro, who did not receive any funding during the writing of this scientific text
Funding
The authors received no funding for this study.
Author(s)
Maria F Morales-Labarca1 MTeach(HEd), Claudia N Ramirez Castro*2 MHlthInstMgmt
1Wound Care Clinical Specialist and Compression Therapy, Essity Health & Medical, Chile.
2Clinical Training Coordinator and Networking, Medical Management Department, Coaniquem Chile.
*Corresponding author email cramirez@coaniquem.org
References
- Chi YW, Raffetto JD. Venous leg ulceration pathophysiology and evidence based treatment. Vasc Med (UK) 2015;20(2):168–81.
- Meyer O. The ambulatory treatment of leg ulcers with pressure bandages. Ind Med Surg 1949;18(4):161.
- Álvarez Fernández LJ, Lozano F, Marinello-Roura J, Masegosa- Medina JA. Encuesta epidemiológica sobre la insuficiencia venosa crónica en España: estudio DETECT-IVC 2006. [An epidemiological survey on chronic venous insufficiency in Spain: the DETECT-IVC 2006 study]. Angiologia 2008;60(1):27–36.
- Ruckley C V. Socioeconomic impact of chronic venous insufficiency and leg ulcers. Angiol 1997;48(1):67–9.
- De Maeseneer MG, Kakkos SK, Aherne T, Baekgaard N, Black S, Blomgren L, et al. Editor’s choice – European Society for Vascular Surgery (ESVS) 2022 clinical practice guidelines on the management of chronic venous disease of the lower limbs. Eur J Vasc Endovasc Surg 2022;63(2):184–267.
- Etufugh CN, Phillips TJ. Venous ulcers. Clin Dermatol 2007;25(1):121–30.
- Zahra S, Arundel C, Jones K, Davill T, Roberts G, Dumville J. VenUS 6: a randomised controlled trial of compression therapies for the treatment of venous leg ulcers: study design and update. J Wound Manage 2022;23(1):13–7.
- Bjork R, Ehmann S. S.T.R.I.D.E. professional guide to compression garment selection for the lower extremity. J Wound Care 2019;28(August):1–44.
- Harding K et al. Simplifying venous leg ulcer management. Recommendations from an expert working group. Wounds International; 2015.
- O’Meara S, Cullum N, Nelson EA, Dumville JC. Compression for venous leg ulcers. Cochrane Database System Rev 2012;2012(11).
- Shi C, Dumville JC, Cullum N, Connaughton E, Norman G. Compression bandages or stockings versus no compression for treating venous leg ulcers (review). Cochrane Database System Rev 2021;2021(7):CD013397.
- Marinel.lo J, Verdú J. Conferencia Nacional de Consenso sobre Úlceras de la Extremidad Inferior (C.O.N.U.E.I.). [National Consensus Conference on Ulcers of the Lower Extremity (C.O.N.U.E.I.) Document from consensus. C.O.N.U.E.I.]; 2018. p. 119
- Wounds UK. Best practice statement: holistic management of venous leg ulceration (2nd edition). Wounds UK; 2022.
- Partsch H, Mortimer P. Compression for leg wounds. Br J Dermatol 2015;173(2):359–69.
- Conde Montero E, Serra Perrucho N, de la Cueva Dobao P. Theory and practice of compression therapy for treating and preventing venous ulcers. Actas Dermosifiliogr 2020;111(10):829–34.
- Mosti G, Iabichella ML, Partsch H. Compression therapy in mixed ulcers increases venous output and arterial perfusion. J Vasc Surg 2012;55(1):122–8.
- Andriessen A, Apelqvist J, Mosti G, Partsch H, Gonska C, Abel M. Compression therapy for venous leg ulcers: risk factors for adverse events and complications, contraindications – a review of present guidelines. J Eur Acad Dermatol Venereol 2017;31(9):1562–8.
- Rabe E, Partsch H, Morrison N, Meissner MH, Mosti G, Lattimer CR, et al. Risks and contraindications of medical compression treatment – a critical reappraisal. An international consensus statement. Phlebol 2020;35(7):447–60.
- Wounds International. Consenso internacional. La importancia de un tratamiento eficiente de heridas. [International consensus. Making the case for cost-effective wound management]. Wounds international 2013.
- Milic DJ, Zivic SS, Bogdanovic DC, Karanovic ND, Golubovic ZV. Risk factors related to the failure of venous leg ulcers to heal with compression treatment. J Vasc Surg 2009;49(5):1242–7.
- Partsch H. Compression for the management of venous leg ulcers: which material do we have? Phlebol 2014;29(S1):140–5.
- Atkin L, Bućko Z, Montero EC, Cutting K, Moffatt C, Probst A, et al. Implementing TIMERS: the race against hard-to-heal wounds. J Wound Care 2019;23(3):S1–52.
- Sibbald RG, Elliott JA, Persaud-Jaimangal R, Goodman L, Armstrong DG, Harley C, et al. Wound bed preparation 2021. Adv Skin Wound Care 2021;34(4):183–95.
- Isoherranen K, Montero EC, Atkin L, M C, Annette H, JD I, et al. Lower leg ulcer diagnosis and principles of treatment. Including recommendations for comprehensive assessment and referral pathways. J Wound Manage 2023;24(1).
- Nelson EA, Ruckley C V., Barbenel JC. Improvements in bandaging technique following training. J Wound Care 1995;4(4):181–4.
- Vowden P, Vowden K. Doppler assessment and ABPI: interpretation in the management of leg ulceration. World Wide Wounds; 2001.
- European Wound Management Association (EWMA). Understanding compression therapy. Position document. EWMA; 2002.
- Moffatt C. Variability of pressure provided by sustained compression. Int Wound J 2008;5(2):259–65.
- World Union of Wound Healing Societies. Compresión en las úlceras venosas de las extremidades inferiores. Documento de consenso. World Union of Wound Healing Societies; 2008.
- Partsch H. Inelastic compression by bandages: effective, but requiring education. Wounds Int 2017;8(7):6–9.
- de Abreu AM, de Oliveira BGRB. A study of the Unna boot compared with the elastic bandage in venous ulcers: a randomized clinical trial. Rev Lat Am Enfermagem 2015;23(4):571–7.
- Franks P, Barker J, Laeuchli S, Mosti G. Management of patients with venous leg ulcers: challenges and current best practice. J Wound Care; 2016.
- Baethge C, Goldbeck-Wood S, Mertens S. SANRA: una escala para la evaluación de la calidad de los artículos de revisión narrativa. [SANRA: a scale for the quality assessment of narrative review articles]. Res Integr Peer Rev 2019;4(1):2–8.
- Haesler E. Evidence summary: venous leg ulcers: compression with short stretch (inelastic) bandages. Wound Pract Res 2019;27:134–6.
- Dolibog P, Franek A, Taradaj J, Polak A, Dolibog P, Blaszczak E, et al. A randomized, controlled clinical pilot study comparing three types of compression therapy to treat venous leg ulcers in patients with superficial and/or segmental deep venous reflux. Ostomy Wound Manage 2013;59(8):22–30.
- Dolibog P, Franek A, Taradaj J, Dolibog P, Blaszczak E, Polak A, et al. A comparative clinical study on five types of compression therapy in patients with venous leg ulcers. Int J Med Sci 2014;11(1):34–43.
- Zarchi K, Jemec GBE. Delivery of compression therapy for venous leg ulcers. JAMA Dermatol 2014;150(7):730–6.
- Mauck KF, Asi N, Elraiyah TA, Undavalli C, Nabhan M, Altayar O, et al. Comparative systematic review and meta-analysis of compression modalities for the promotion of venous ulcer healing and reducing ulcer recurrence. J Vasc Surg 2014;60(2):71S-U103.
- Oates A, Adderley U. Survey of registered nurses’ selection of compression systems for the treatment of venous leg ulcers in the UK. J Tissue Viabil 2019;28(2):115–9.
- De Carvalho MR, Peixoto BU, Silveira IA, de Oliveria B. A Meta-analysis to compare four-layer to short-stretch compression bandaging for venous leg ulcer healing. Ostomy Wound Manage 2018;64(5):30–7.
- Stücker M, Link K, Reich-Schupke S, Altmeyer P, Doerler M. Compression and venous ulcers. Phlebol 2013 Mar;28 Suppl 1:68–72.
- Nelson EA, Harrison MB. Different context, different results: venous ulcer healing and the use of two high-compression technologies. J Clin Nurs 2014;23(5–6):768–73.
- Ritchie G. Understanding compression: part 4 – bandaging and skin care. J Comm Nurs 2018;32(5):22–30.
- Brambilla R, Aloisi D, Weingard I, Fioruzzi M, Heisterkamp T, Janthur E, et al. VERUM – a European approach for successful venous leg ulcer healing: implementation of a comprehensive therapy concept (VERUM13) in daily practice. EWMA J 2013 Oct;13(2):19–23.
- Mosti G, Mancini S, Bruni S, Serantoni S, Gazzabin L, Bucalossi M, et al. Adjustable compression wrap devices are cheaper and more effective than inelastic bandages for venous leg ulcer healing. A multicentric Italian randomized clinical experience. Phlebol 2020;35(2):124–33.
- Paranhos T, Paiva CSB, Cardoso FCI, Apolinario PP, Rodrigues RCM, Oliveira HC, et al. Systematic review and meta-analysis of the efficacy of Unna boot in the treatment of venous leg ulcers. Wound Repair Regen 2021;29(3):443–51.
- Ashby RL, Gabe R, Ali S, Saramago P, Chuang LH, Adderley U, et al. VenUS IV (venous leg ulcer study IV) – compression hosiery compared with compression bandaging in the treatment of venous leg ulcers: a randomised controlled trial, mixed-treatment comparison and decision-analytic model. Health Technol Assess 2014;18(57):V–293.
- Albuquerque G, Ferreira RJO, Costa P, Nunes R, Cunha M. Effectiveness of short-stretch compressive therapy beyond healing of varicose ulcers: systematic review. Revista Rol De Enfermeria 2018;41(11–12):73–8.
- Lantis JC, Barrett C, Couch KS, Ehmann S, Greenstein E, Ostler M, et al. A dual compression system: preliminary clinical insights from the US. J Wound Care 2020;29(9):S29–37.
- Sanchez C, Partsch H. Healing of an arterial leg ulcer by compression bandaging: a case report. J Wound Care 2017 Feb;26(Sup2):S18–22.
- Partsch H, Mosti G. Pressure-time integral of elastic versus inelastic bandages: practical implications. EWMA J 2013;13(2):15–7.
- Asociación española de enfermería vascular y heridas. Guía de práctica clínica: consenso sobre úlceras vasculares y pie diabético. [Spanish Association of Vascular and Wound Nursing. Guide of Clinical practice: consensus on vascular ulcers and diabetic foot.] Guía de Práctica Clínica. (3rd edition) 2017;1–140.
- Vowden P, Kerr A, Mosti G. Demystifying mild, moderate and high compression systems – when and how to intrroduce “lighter” compression. Wounds International; 2020.
- Flegg JA, Kasza J, Darby I, Weller CD. Healing of venous ulcers using compression therapy: predictions of a mathematical model. J Theor Biol 2015;379:1–9.
- Isoherranen K, Jordan O’Brien J, Barker J, et al. Atypical wounds. Best clinical practice and challenges. J Wound Care 2019;177–86.
- Croitoru D, Naderi-Azad S, Sachdeva M, Piguet V, Alavi A. A wound care specialist’s approach to pyoderma gangrenosum. Adv Wound Care (New Rochelle) 2020;9(12):686–94.
- Carr C, Shadwell J, Regan P, Hammett S. An evaluation of short-stretch compression systems for chronic lower-limb leg ulcers. Br J Community Nurs 2015 Mar;Suppl Wound:S38, S40-7.
- Sodré SLS, Nogueira G de A, Abreu AM de, Marta CB, Peregrino AA de F, Silva RCL da. Análisis costo-efectividad del tratamiento con terapia compresiva en la cicatrización de úlceras venosas. [Cost-effectiveness analysis of the treatment with compressive therapy in the healing of venous ulcers]. Rev Lat Am Enfermagem 2023;31:e3839.
- Partsch H. Applying Unna boot bandages with high pressure: Fischer bandages. Clinical practice. Wounds Int 2019;10(3).
- Ousey K, Atkin L, Conway B. Compression therapy for pharmacy teams. Wounds UK; 2021.
- Mosti G, Cavezzi A, Massimetti G, Partsch H. Recalcitrant venous leg ulcers may heal by outpatient treatment of venous disease even in the presence of concomitant arterial occlusive disease. Eur J Vasc Endovasc Surg 2016 Sep;52(3):385–91.
- Patton D, Avsar P, Sayeh A, Budri A, O’Connor T, Walsh S, et al. A meta-review of the impact of compression therapy on venous leg ulcer healing. Int Wound J 2023;20(2):430–47.
- Lee N. An evaluation on the use of adjustable compression wrapping devices as an alternative to compression bandaging in lower leg wounds. Wounds Int 2018;9(4):12–9.
- Stather P, Petty C, Langthorne H, Rayner E, Zhang J, Hayden K, et al. A randomised controlled clinical trial comparing the effectiveness of bandaging compared to the JuxtaCuresTM device in the management of people with venous ulceration: feasibility study. Phlebol 2021 Aug;36(7):505–14.
- Welsh L. What is the existing evidence supporting the efficacy of compression bandage systems containing both elastic and inelastic components (mixed-component systems)? A systematic review. J Clin Nurs 2017;26(9–10):1189–203.
