Volume 25 Number 1
Holistic Management of Wound-Related Pain An overview of the evidence and recommendations for clinical practice
Samantha Holloway, Kirsti Ahmajärvi, Nicoletta Frescos, Sue Jenkins, Alisha Oropallo,
Simona Slezáková, Andrea Pokorná
For referencing Holloway S, Ahmajärvi K, Frescos N, Jenkins S, Oropallo A, Slezáková S, Pokorná A. Holistic Management of Wound-Related Pain. J Wound Management, 2024;25(1 Sup1). S1-S84.
DOI 10.35279/jowm2024.25.01.sup01
Abstract
Background Pain is a significant factor associated with wounds. Its presence can impact on every aspect of an individual, affecting their overall quality of life (QoL) including ability to function, as well as their social and psychological well-being. Holistic approaches that can help to address wound-related pain are vital to improve patient outcomes.
Aim We aimed to review the evidence for the holistic management of wound-related pain in individuals with chronic wounds in order to provide recommendations for healthcare professionals in clinical practice.
Method The L OVE platform was used for the search as wound and burn are in the same search category. L OVE collects systematic reviews retrieved from the systematic reviews database Epistemonikos and allocates them to specific L OVEs and questions. We conducted our search for reviews related to wounds and burns in November 2022. Retrieved titles and abstracts were exported into Rayyan. The search was organised within Rayyan according to the focus for each chapter to retrieve evidence on pain assessment, physical therapies, patient education, psychological approaches, and complementary and alternative approaches. A systematic approach was used by senior experts in wound and pain management for double-blind screening and application of inclusion criteria (chronic wounds and pain) to agree on articles for review. Sources related to acute wounds (including burn injuries) were excluded. The L OVE search was supplemented by narrative reviews of literature identified from the individual systematic reviews and handsearching of relevant sources.
Results Thirty-eight systematic reviews and 27 additional articles were identified providing a total of 65 individual pieces of evidence. The number of reviews and articles included: pain assessment (n=25); physical therapies (n=8); patient education (n=12); psychological approaches (n=2); complementary and alternative approaches (n=18). The literature related to pain assessment highlighted that assessment of wound-related pain is complex and multidimensional. Healthcare providers must determine the most suitable assessment tool for their patients and in doing so consider an individual’s ability to respond to the assessment, as there is no one assessment tool to measure pain, as ‘one size does not fit all’.
In terms of physical therapies, physical exercise is important, although the majority of evidence relates to individuals with venous leg ulcers (VLUs). In relation to management, clinicians need to recognize procedural-related pain, particularly in relation to debridement procedures. There may be a role for topical impregnated dressings and topical anaesthetics in this case. Equally it is important to manage moisture to prevent maceration and reduce the risk of pain from periwound skin irritation (dermatitis). For individuals with malignant fungating wounds (MFW) a combination of therapies to manage symptoms is recommended.
Specific research related to patient education and wound-related pain is lacking, however areas that should be considered include aetiology of the wound and causes of pain, non-pharmacological and pharmacological methods for pain relief, methods for assessing pain relief, as well as impact of pain on QoL. Psychological approaches need to consider the factors associated with pain (attention, cognitions, emotions and emotion regulation and overt behaviour) in order to determine the most appropriate treatment strategy. Evidence to make recommendations for wound-related pain is sparse; however, there may be a role for social models of care and motivation enhancement programmes for individuals with leg ulcers. Additionally, aromatherapy and music therapy may also be helpful. Evidence for other chronic wounds is lacking. There is some evidence to support the role of honey for the management of wound-related pain, specifically the research indicates that the analgesic action may be related to its anti-inflammatory properties. Evidence for traditional Chinese medicine (TCM), plants, low-dose topical steroids and low level-laser therapy was very weak.
Conclusion The experience of wound-related pain is complex and needs to take into consideration the psychological and social factors that can impact on an individual’s QoL to ensure a holistic approach. Equally the assessment of wound-related pain is complex and multidimensional. Healthcare providers must determine the most suitable assessment tool for their patients and in doing so consider an individual’s ability to respond to the assessment. Management of wound-related pain may require both non-pharmacological and pharmacological approaches and can include dressings and devices. A holistic strategy should also incorporate both education (patient and healthcare professional) and psychological approaches to improve patient outcomes.
Our review has identified a lack of scientific resources on wound-related pain management to make clear recommendations for effective strategies. What is needed are further prospective studies of patients with wound-related pain and different types of non-healing wounds. Such research should be cognisant that a phenomenon as complex as pain must also be examined comprehensively. The phenomenon of pain has a high degree of subjective perception and individuals have different coping strategies, and healthcare professionals need to be mindful of this. The main determinants of wound-related pain management cannot solely be based on the wound symptomatology and the process of care (healing), but also need to consider the individuality of the patient and their current needs.
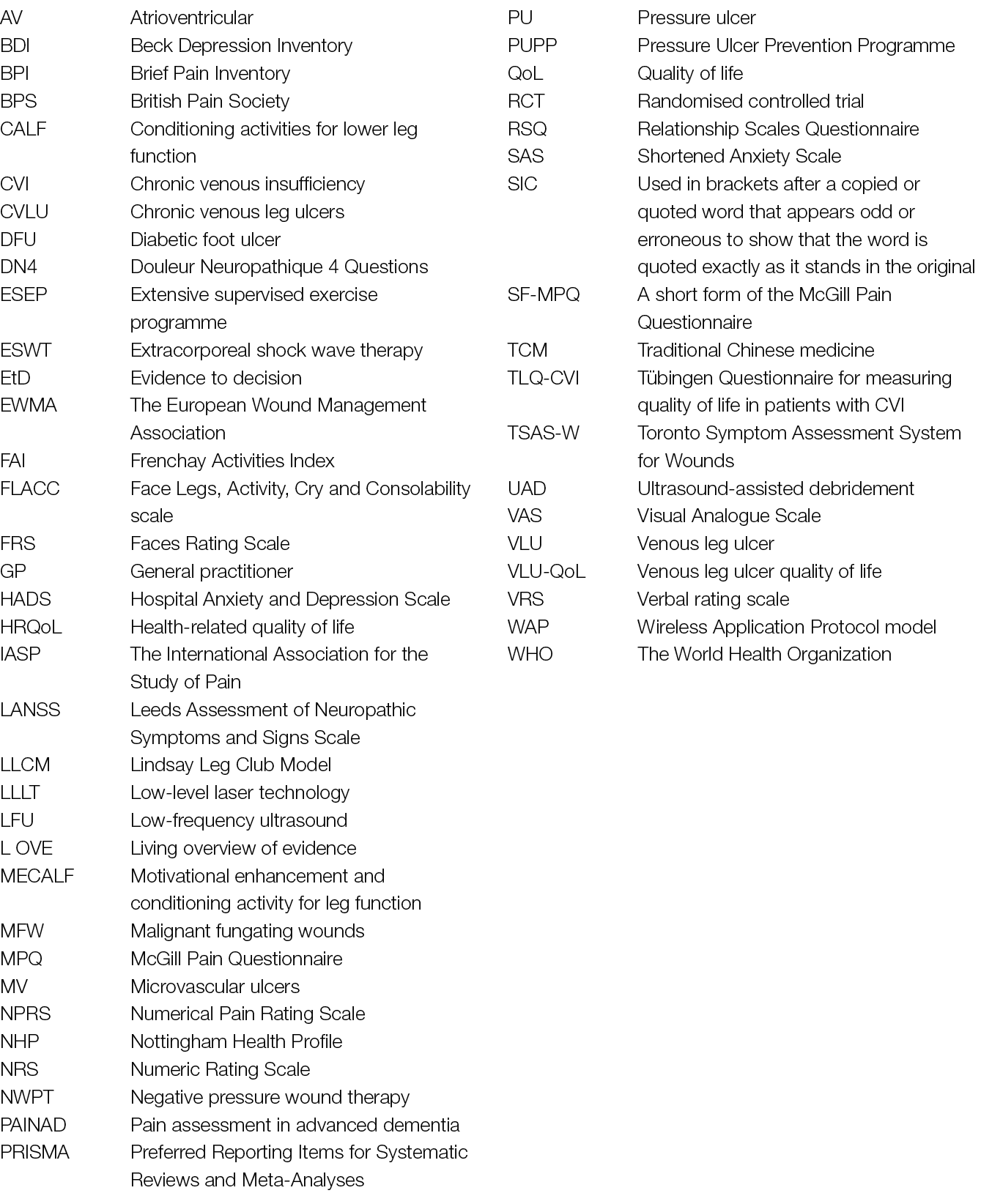
Abbreviations
1. Introduction
Pain is a multidimensional phenomenon that is predisposed by biological, psychological and social factors which influence how pain is experienced and how it should be managed.1 Additionally, individuals learn the concept of pain through life experiences.2,3 Pain, particularly chronic/ persistent pain can also have adverse effects on function and on social and psychological well-being, therefore effective pain management is vital. In a study by Gardner et al.4 the authors reported that wound care procedures cause moderate to severe pain in up to 74% of patients and almost half (36%) of the patients with open wounds experienced severe pain. In combination with chronic wounds pain can also have a significant impact on the quality of life (QoL) of individuals.5 In fact, pain has been reported as one of the most difficult aspects for individuals with wounds to deal with, as it can impair activity, sociality and sleep.6
A detailed description of the search strategy methodology for each chapter is provided as appendices to this document. We searched the L OVE platform, which collects systematic reviews retrieved from the systematic reviews database Epistemonikos7 and allocates them to specific L OVEs and questions.8 The chapters are organised according to the L OVE filters applied. The Chapter 2 examines the multidimensional nature of pain, beginning with acute (nociceptive) pain, and aspects of chronic pain as it relates to individuals with wounds. Chapter 3 explores the evidence related to pain assessment to establish which assessment tools are being used in research and clinical practice. Chapter 4 considers the range of physical therapies available for the management of wound-related pain and offers some guidance for healthcare professionals. In this chapter ‘physical therapy’ does not relate purely to the professional practice of a ‘physical therapist’, instead the term has been applied in the wider context and according to the L OVE filters. Hence the role of interventions to manage anticipatory and procedural pain as well as inflammation are discussed. Chapter 5 examines evidence related to patient education, including determinants of non-adherence, tailored treatment regimes, the role of social models of care, motivation enhancement programmes and the importance of listening to individuals. Chapter 6 reviews the role of psychological approaches to the management of wound-related pain, building on evidence from Chapter 2. The final chapter presents an overview of the evidence related to complementary and alternative therapies, according to the L OVE database categorisation. In this chapter the role of honey is reviewed, as well as traditional Chine medicine, plant therapies, low level laser therapy and interventions for MFWs.
Each chapter provides a summary of recommendations based on the evidence, as well as the author group’s clinical experience and expertise to guide implementation into clinical practice. The document concludes with a discussion of the challenges healthcare professionals and individuals face and where we see the current gaps in the evidence base.
Our approach to developing this document has been to frame the subject matter within a biopsychosocial framework to support a holistic approach to the assessment and management of wound-related pain. We recognise that the prevention of pain is also important, therefore we have tried to identify strategies that should help to minimise pain. We have discussed the role of non-pharmacological and topical pharmacological techniques, however the use of first line analgesics to manage pain are outside the scope of the document which is intended for healthcare professionals who are not pain specialists.
| Detailed information about pain assessment tools and summary tables of the evidence included can be found online in a separate Appendices document. |
2. The multidimensional nature of pain
2.1 Definition of pain
The International Association for the Study of Pain (IASP) defines pain as:
An unpleasant sensory and emotional experience associated with or resembling that associated with, actual or potential tissue damage.9
This definition is used widely and is applicable to wound-related pain as it refers to actual or potential tissue damage, such as may be present with an impending pressure ulcer/pressure injury (PU)*. The inclusion of the sensory and emotional aspects of pain ensures that the multidimensional aspects are fundamental to effective pain management.
Additionally the IASP categorises pain as acute and chronic.10 Box 1 shows the current definition of acute pain and Box 2 shows the definition of chronic pain.
Box 1: Definition of acute pain
| Acute pain happens suddenly, starts out sharp or intense and serves as a warning sign of disease or threat to the body. It is caused by injury, surgery, illness, trauma, or painful medical procedures and generally lasts from a few minutes to less than 6 months. Acute pain usually disappears whenever the underlying cause is treated or healed.10 |
Box 2: Definition of chronic pain
| The IASP definition of chronic pain is pain that persists for 3 months or more and that it can, ‘persist despite successful management of the condition that initially caused it, or because the underlying medical condition cannot be treated successfully’.10 |
The World Union of Wound Healing Societies11 categorised wound pain in five categories (Table 1).
Table 1: World Union of Wound Healing Societies categories of wound pain, adapted from World Union of Wound Healing Societies (2004)11
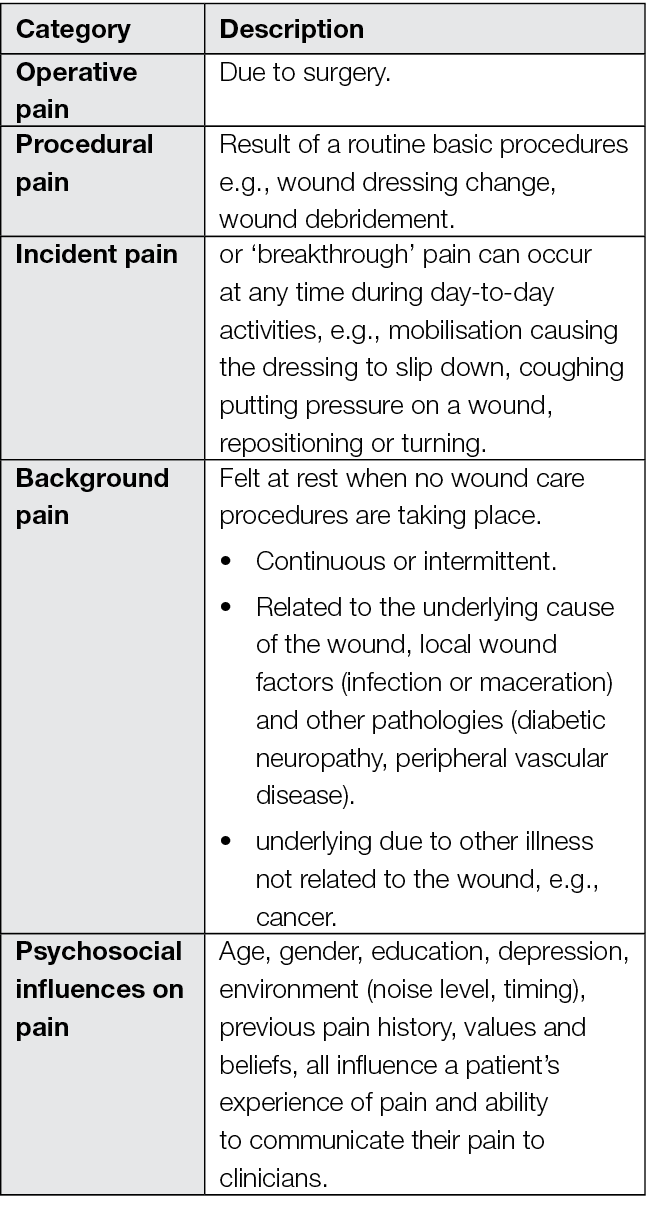
These categories can help to guide the healthcare professional on what may cause wound-related pain and therefore the selection of appropriate pain management strategies. To manage pain effectively, the healthcare professional requires an understanding of pain, based on the biopsychosocial model, as this can help to explain how and why an individual feels pain and where analgesic strategies work.
2.2 An introduction to the physiology of pain
Mechanisms associated with the experience of pain include nociceptive (tissue damage), inflammatory, neuropathic (nerve-related)12 and ischaemic pain (which may be involved in incisional pain).10,13 Pain is a complex process, and to help understand it fully, it is important to firstly consider the nociceptive process (acute pain).
2.2.1 Acute pain
There are four physiological stages in nociception, which may give rise to the experience of pain: transduction, transmission, perception and modulation. They occur as a result of the transfer of stimuli from the site of injury in the periphery, via the central nervous system (spinal cord), through to the brain.14 The process is summarised in Table 2.15,16
Table 2: The anatomy and physiology of pain, adapted from Osterweis et al (1987) and Yam et al (2018)15, 16
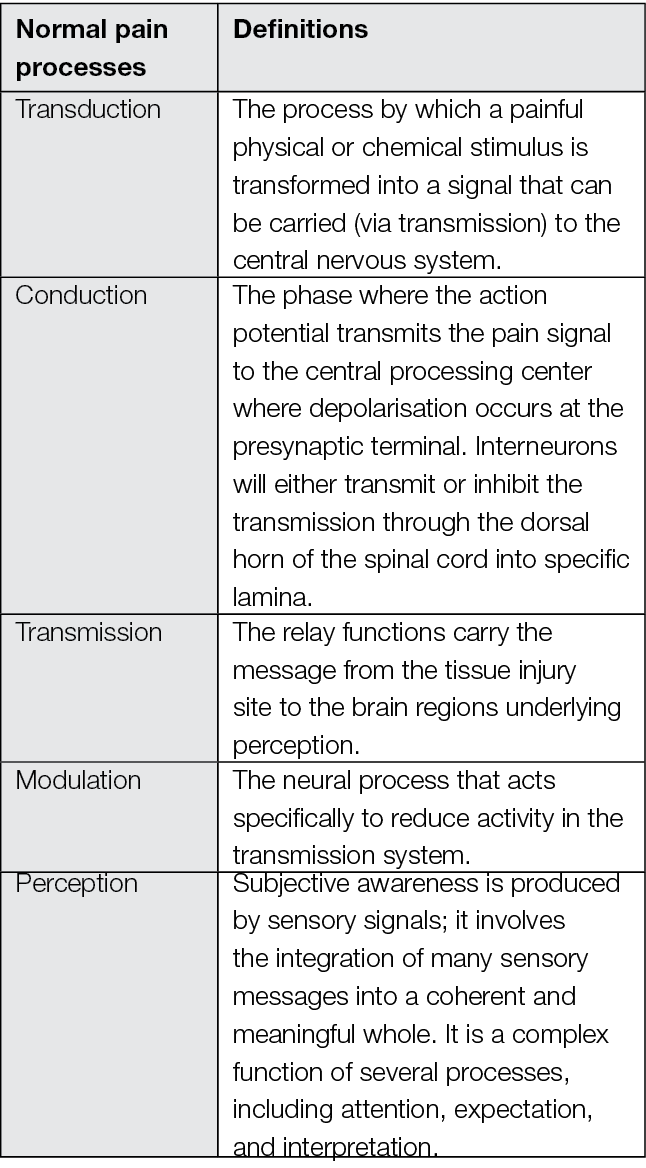
2.2.2 Transduction
Swift and Middleton14 summarised the physiology of pain. During transduction, following the peripheral stimulus, e.g., from tissue damage, wound management procedures or infection, the stimulus is changed into a nerve impulse (Figure 1). Nociceptors on the surface of the nerve endings respond to noxious stimuli and interact between the stimulus and the receptors. This triggers chemical changes through chemical mediators, including bradykinin, creating an action potential (electrical signal).16 Action potentials travel from the periphery to the dorsal horn in the ‘conduction’ phase. The larger the stimulus, e.g., tissue damage, size of the wound, the higher the frequency of action potentials, which may result in the individual experiencing more severe pain. The relationship between nociception and pain is non-linear and both are impacted by psychosocial factors.
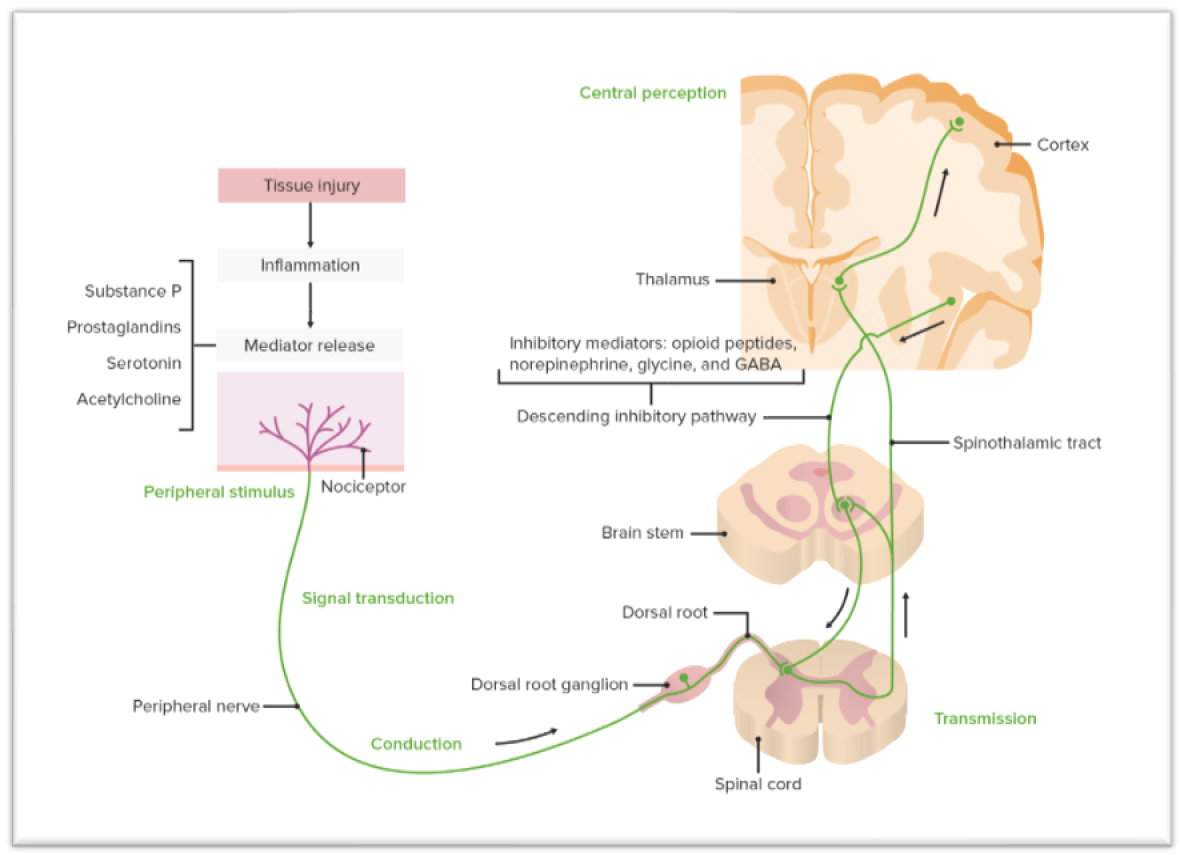
Figure 1: The basic route of nociception, transduction and transmission upon noxious stimuli in ascending and descending order. Lecturi Medical Education Resource (2022),17 permission to use granted.
Injury and inflammation lead to a cascade of activating factors from blood, local, migrating inflammatory cells and injured cells. They activate C fibres through receptors found on the afferent terminal that sensitise these terminals.18 Chemical mediators involved in the inflammatory process including substance P, prostaglandins and serotonin, are also involved in angiogenesis, vasodilation, cell growth and cell proliferation that occurs in wound healing.
Inflammation occurs as damage to the tissue releases inflammatory mediators causing arteriole dilation, and the area becomes discoloured/erythematous and hot. Contraction of the endothelium of capillaries and venioles occurs with subsequent fluid and cell transmission into the local area causing swelling and pain.19
2.2.3 Transmission
There are three responses in the transmission phase, when the impulse travels to the brain (note that the impulses can travel up to and down from the brain), due to antidromic reflex or local neural peptide formation.20
The impulses travel from:
- Nociceptors to the spinal cord
- Spinal cord to the brain.
- Brain stem to other parts of the brain.
During the first response, impulse conduction occurs through the cycling of sodium and potassium channels between extracellular and intracellular fluid. This involves the A-delta and C fibres. The A-delta fibres are mildly myelinated, therefore they transmit impulses more quickly and produce the ‘first pain’ (sharp sensation) felt following injury. C fibres transmit more slowly and produce the ‘second pain’ (dull, burning sensation).
When the nociceptive impulse reaches the spinal cord, it crosses a synapse through the release of the neurotransmitters by diffusion, which activates a secondary neuron. Each neuron has a cell body in the dorsal root ganglion. It is a long process, an axon divides and sends one branch out to the periphery and one into the spinal cord. The primary afferent nociceptors have axons that are relatively thin and conduct impulses slowly. To release enough neurotransmitters to transmit the signal onto the next phase, sufficient activation of nociceptors is required with facilitation and inhibition occurring within descending pathways.
2.2.4 Modulation
Modulation occurs through ascending and descending mechanisms. Ascending mechanisms, described by the Gate Control Theory of pain, are activated by touch or pressure. An example is knocking your hand and rubbing that area to reduce the pain felt. A-delta and C fibres trigger the secondary neurones. They then compete to transmit the secondary neurone, but if there is more activation of A-delta fibres (e.g., during rubbing), there is an alternative stimulus provided, creating descending inhibition, reducing the pain experience. During the descending mechanisms, from the brain down to the spinal cord, the descending nerve fibres release chemical mediators, endogenous opioids, gamma-aminobutyric acid (GABA), noradrenalin, neurotensin and serotonin. These inhibit the release of neurotransmitters, making it difficult for the secondary neuron to create a new action potential (the next phase).14
2.2.5 Perception
The individual experiences (feels) pain as a salient experience during the perception phase while recognising, defining, and responding to pain. This phase involves three areas of the brain, the cortex (location and motor response), the limbic system (emotional response) and the reticular system (arousal response). Distraction and relaxation techniques work in this phase to reduce the experience of pain.
Pain perception includes several psychological processes that provide feedback to influence pain perception. They are:
- Attentional orienting to the painful sensation and its source,
- Cognitive appraisal of the meaning of the sensation,
- Emotional, psychophysiological, and behavioural reactions.21
2.3 Chronic (persistent) pain
The definition of chronic pain was presented previously. The IASP further define chronic pain into two groups of chronic pain syndromes.22
Chronic primary pain or chronic secondary pain23: Chronic primary pain includes conditions such as fibromyalgia or non-specific low-back pain; Chronic secondary pain is secondary to another disease, surgery, or injury. Chronic pain in chronic wounds, may therefore be a type of chronic secondary pain. Chronic wounds may also have chronic secondary neuropathic pain.24 Chronic pain often becomes the sole or predominant clinical problem in some individuals. Numerous physiological changes occur in the neuraxis as a result of chronic, persistent pain. These include neuropathic pain, wind up, sensitisation and neuroplasticity which are elaborated on in the following sections.
2.3.1 Neuropathic pain
Non-healing wounds result in an abnormal nociceptive pathway which can result in neuropathic pain and changes in sensation with peripheral and central changes due to nerve injury or peripheral neuropathy. The IASP define neuropathic pain as:
Pain initiated or caused by a primary lesion or dysfunction of the nervous system.25,22
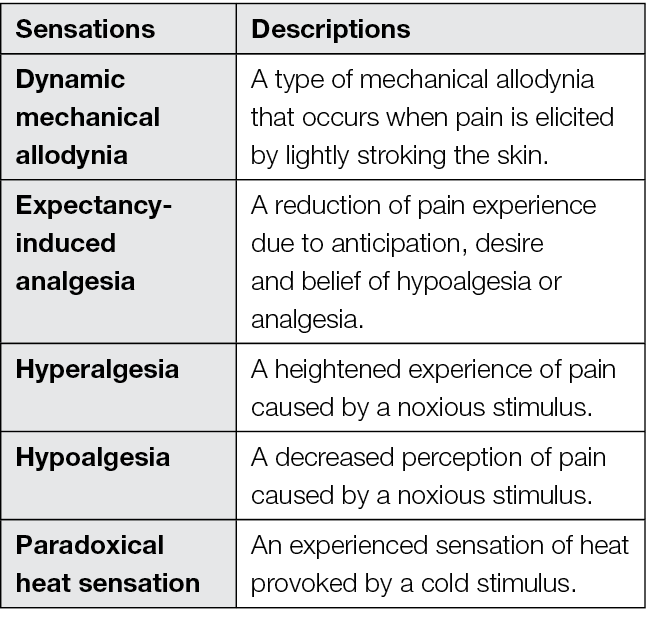
Neuropathic pain can be caused by damage anywhere along the neuraxis: peripheral nervous system, spinal or supraspinal nervous system. It can also be caused by tissue and nerve injury, as well as by conditions such as diabetic neuropathy. It is characterised by the sensations described in Table 3. These painful sensations affect the individual’s sensory system, their well-being, mood, focus and thinking. It is important to note that classic measures to reduce acute pain (nociceptive pain) are not effective for neuropathic pain as the neural pain transduction and transmission pathways are different.
Table 3: Peripheral and central changes due to nerve injury or peripheral neuropathy, adapted from Colloca et al (2017)26
Additionally, proprioceptors are sensory receptors that transduce itchy sensations and position sense, for example, of joints.
2.3.2 Wind up
Based on the Melzack and Wall theory of pain27 the process of wind up was identified. Wind-up occurs when the pain signal into the central nervous system becomes stronger and longer lasting. This physiologic process involves activation of receptors normally dormant on post-synaptic nerve endings. Wind-up occurs anywhere in the spinal cord or brain (transmission, modulation and perception). When pain is persistent there is activation of receptors that are normally dormant on post-synaptic nerve endings. This is why pain starting in a small area progresses to a larger area, such as an injury to the finger that results in pain in the entire hand.28
2.3.3 Sensitisation
As a result of prolonged high-frequency signalling into the dorsal horn, there is more stimulation of the transmitter glutamate (short-acting), substance P and Calcitonin Gene-related Peptide (CGRP), with consequent amplification of nociceptive information from the periphery into the central nervous system. When this state is achieved, neurones become sensitised. As a result, nociceptors become more efficient by three predominant mechanisms.29
- An increase baseline voltage across the cell membrane of the neurone
- Production of more ion channels
- Ion channels stay open longer
These processes contribute to a clinical phenomenon called central sensitisation.
During sensitisation, pain amplifies further due to the release of serotonin. In low quantities, serotonin can increase nociceptive signalling. In high quantities, there is an inhibitory effect. The brainstem can amplify nociception through high-frequency or prolonged nociceptive signalling.14
2.3.4 Neuroplasticity
Neuroplasticity is the ability of the brain and nervous system to adapt and change. Chronic pain can persist after damaged tissue(s) heals and can be due to nerve damage or a result of neuroplasticity secondary to the damage to tissues or neurons. The mechanisms involved in neuroplasticity occur throughout the neuraxis including the somatosensory circuit of the spinal dorsal horn, thalamus, and cortex associated with chronic pain.30 Neuroplasticity in relation to pain is unhelpful as it can exacerbate persistent pain. Neuroplasticity can also become maladaptive; such as in persistent pain where protective systems become more efficient at doing their job, even when it is not required.
2.4 Pain and the wound healing physiological response
The normal physiology of wound healing occurs as a result of sequential overlapping phases to enable tissue reconstitution.31 Pain is often experienced during the inflammatory phase, when damaged cells, pathogens, and bacteria are removed from the wound area. Swelling, heat, pain and erythema occur because of the white blood cells, growth factors, nutrients and enzymes, and it is associated with the peripheral phase of nociception. There is an increase in local biological mediators impacting nociception, either due to damage or from the inflammatory response itself.32 The build-up of fluid leads to swelling and the swollen tissues push against sensitive nerve endings. These and other chemical changes affect how nerves behave, which can contribute to pain.
In addition, there are intrinsic and extrinsic factors that affect wound healing for example, hypoxia, bacterial colonisation, ischaemia, reperfusion injury, altered cellular response, and collagen synthesis defects. Many of these will also stimulate the peripheral response in nociception and therefore need to be addressed as part of the assessment and management of pain.
2.5 Chronic wounds and chronic pain: what are the similarities?
Chronic, persistent wounds are characterised by full-thickness tissue loss in the form of arterial ulcers, diabetic foot ulcers (DFUs), venous ulcers, pressure injuries/ulcers, or infected open surgical wounds or from trauma. Chronicity in wounds is defined by the wound healing process itself and the subsequent non-response to treatment.27,33,34 They are described as a wound that does not heal within 4 weeks or, does not heal within an acceptable time of receiving standard care.35 Ferreira et al36 proposed a number of features of a chronic wound and argued that it should include at least one of the following:
- Persistent for more than three months
- Compromised vascularity or necrosis
- Presence of infection
- Associated comorbidities which impair the healing potential
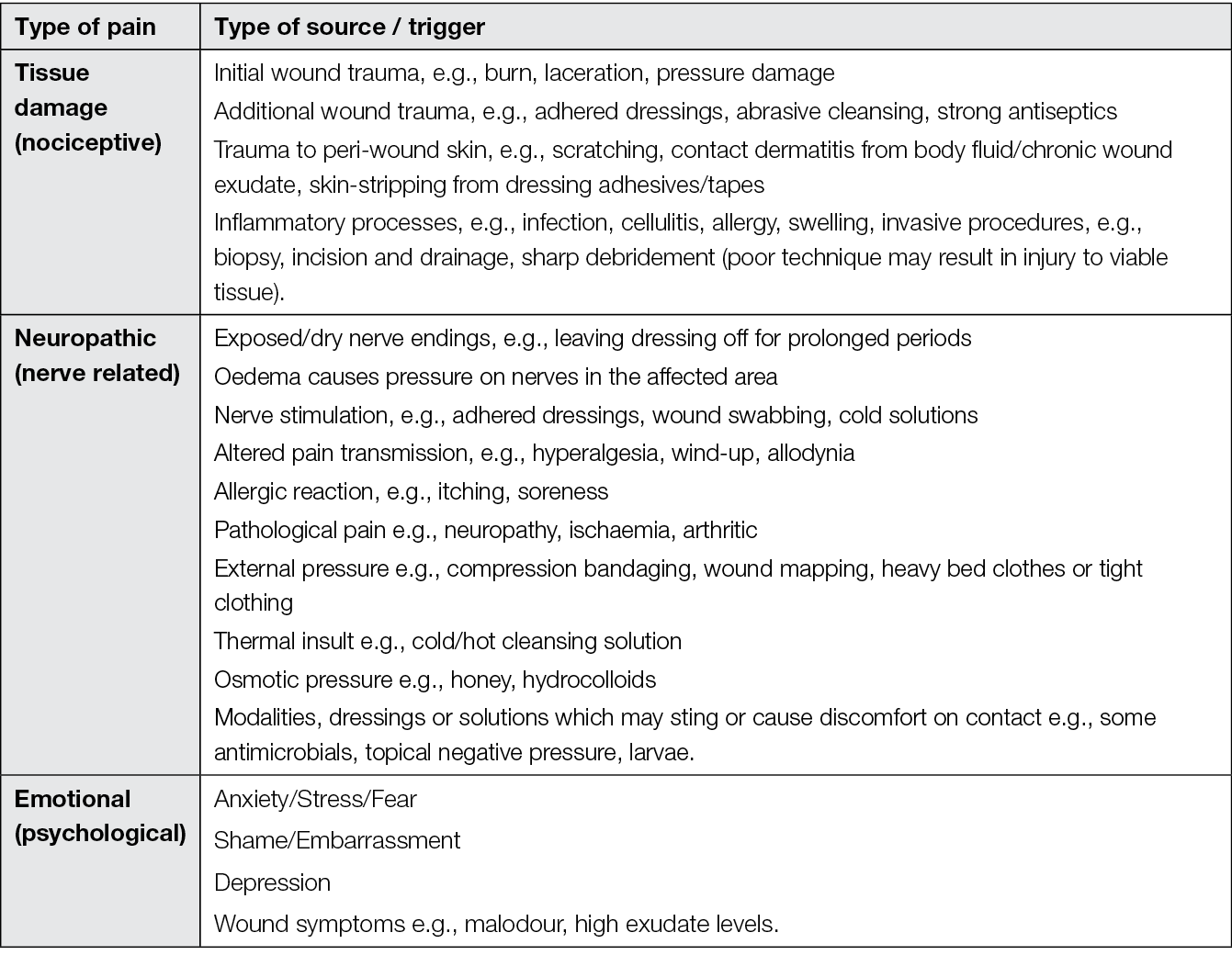
The definition of chronic pain includes the feature of being present for more than three months; however, it does not include the notion of persistent pain which is more evident in the literature related to wounds. Therefore, it is important to approach wound care with the understanding that all wounds have the potential to be painful. The sources and triggers for wound-related pain (acute and chronic), are summarised in Table 4.
Table 4: Pain sources and triggers, adapted from Vuolo (2009)37
2.6 Psychosocial factors associated with pain
Many psychosocial factors contribute to the pain experience, including emotional (psychological) factors.37 In individuals with chronic wounds and pain the clinician needs to be aware of these, as they will affect an individual’s experience of chronic pain. Table 5 summarises the factors and potential consequences.
Table 5: Psychological factors in pain and their processes, adapted from Linton and Shaw (2011)2
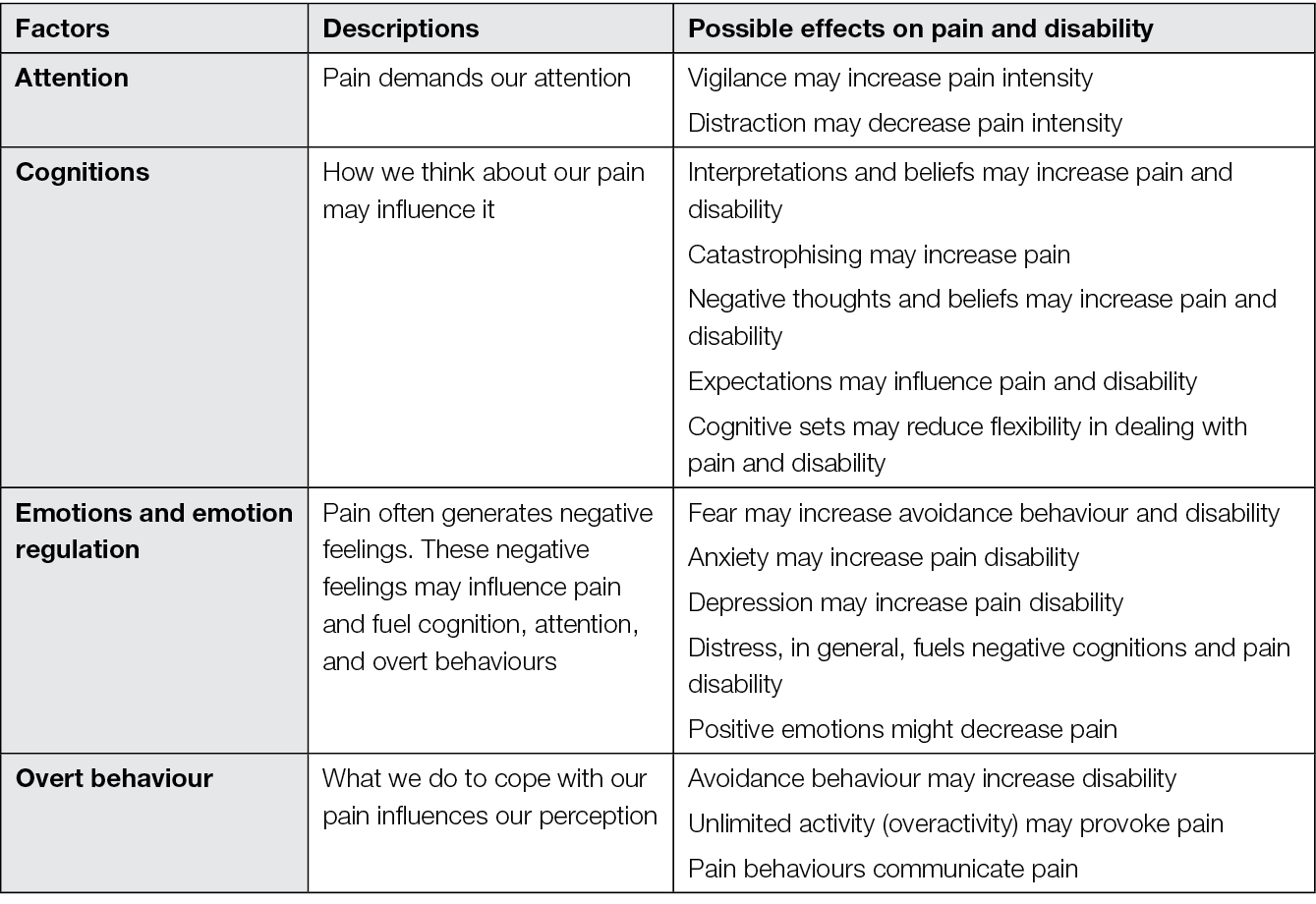
Pain perception is modulated by cognitive and emotional variables such as predictability, controllability, attentional focus, or fear of pain. The psychological factors that modulate the perception of pain include:
- Expectancy
- Perceived controllability
- Fear and anxiety
- Appraisal processes
- Perceived self-efficacy (an individual’s confidence in their ability to control or manage various aspects of health conditions associated with pain, such as pain and disability), and
- Contingencies of reinforcement.38,39
Increased stress levels, cortisol levels, and the thought of pain can affect wound healing. Heightened anxiety lowers an individual’s pain threshold and tolerance and may result in increased vigilance of somatic signals. This has the potential to impact neural sensitisation. The vicious cycle of pain, stress/anxiety and worsening of pain can delay wound healing.6,40
2.7 Psychological factors that influence the experience of wound pain
Psychological factors that influence the experience of wound-related pain include the wound (non-healing, exudate, odour), fear and anxiety (non-healing, pain during wound care, background pain), poor sleep, traumatic experiences (previous/historical) and depression (a long-term condition or may be linked to the wound / persistent pain).6,40,41 In addition, individuals with chronic wounds often have comorbidities which can influence wound healing and their experience of pain. A multidisciplinary approach to managing individuals is essential to provide appropriate person-centred care. The biopsychosocial Integrated Wound Pain Model provides a useful framework to help understand the complexities of wound-related pain (Figure 2).42
INTEGRATED WOUND PAIN MODEL
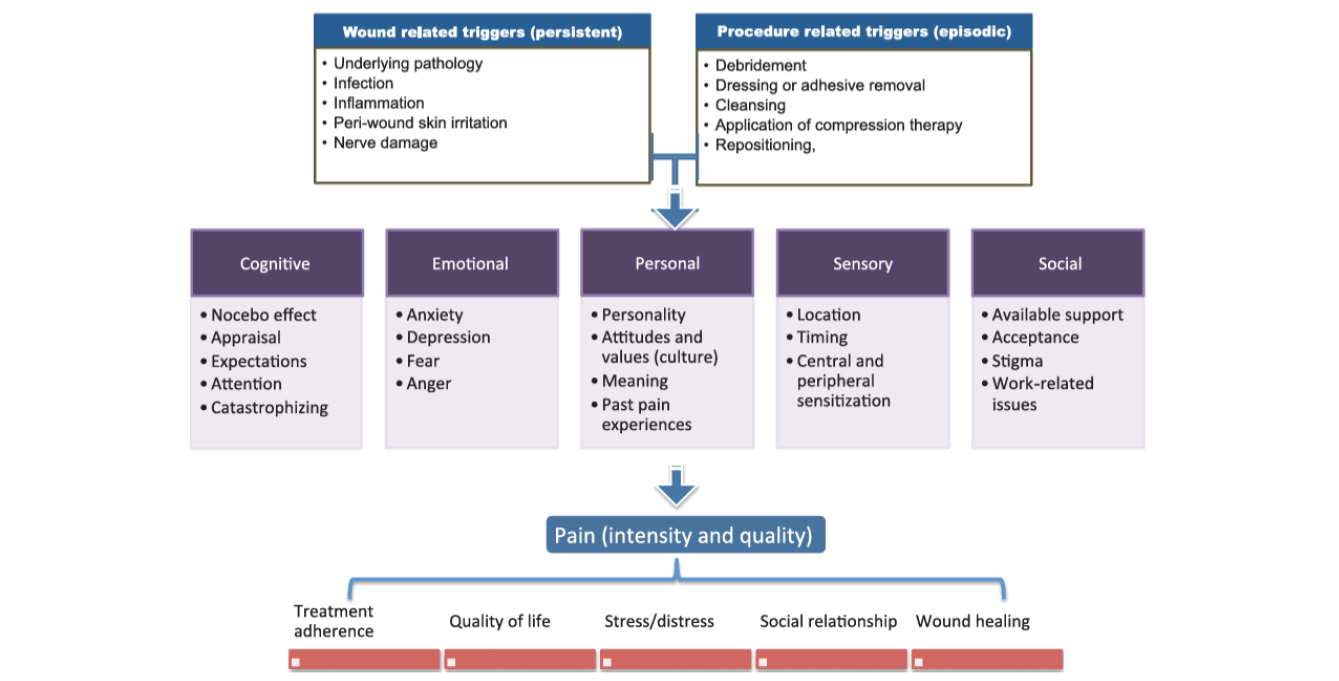
Figure 2: Integrated Wound Pain Model. Woo (2012),42 permission to use granted
2.8 Social factors that influence the experience of wound pain
Table 6 summarises the biopsychosocial factors associated with chronic pain. Social factors that influence the experience of wound-related pain include levels of education, social deprivation, isolation, poor/reduced mobility and culture.41,43
Table 6: Biopsychosocial factors associated with the development of chronic pain, Mills et al (2019) 44, pe274
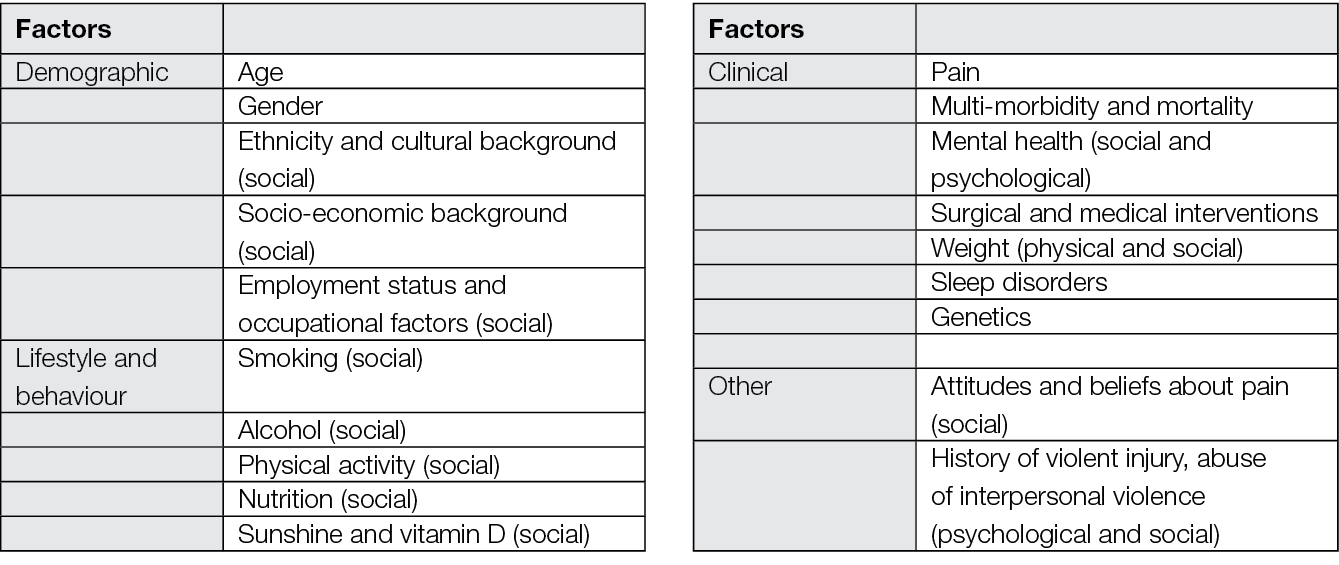
These factors should be taken into consideration in assessing individuals with wound-related pain. More recently perceptions of injustice45, the influence of significant other46,47 and their beliefs are also important psychosocial factors from the chronic pain research.
In considering the impact that wound-related pain can have on the individual, it has been established that understanding the pain experience and how it should be managed is not just about pharmacological and non-pharmacological strategies. The experience of pain is subjective and complex and involves psychological and social factors that can impact on an individual’s QoL. Figure 3 illustrates the consequence of these factors.48
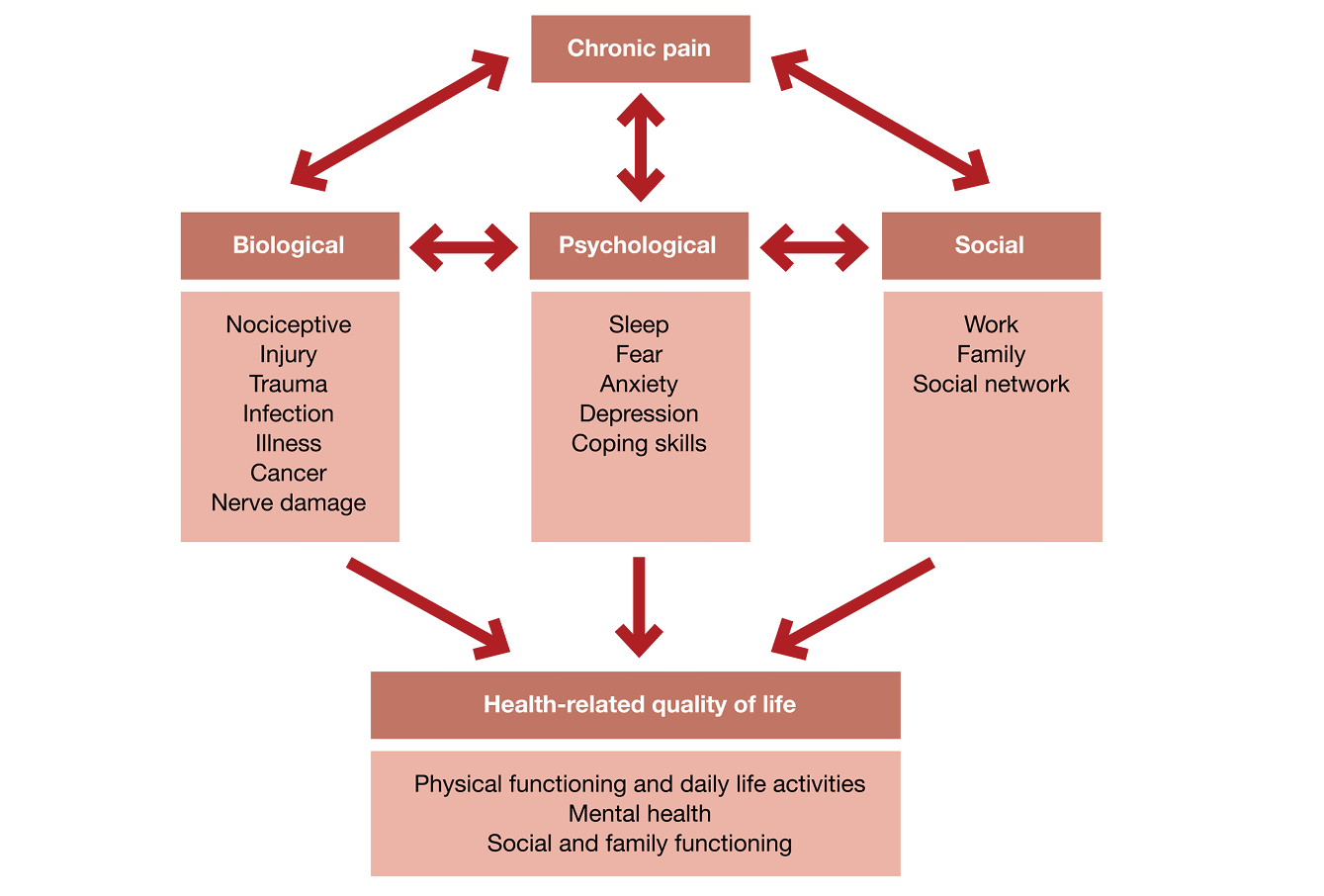
Figure 3: Biopsychosocial model of pain and consequences on the quality of life, adapted from Duenas et al (2016),48 p457
In relation to wound-related pain, management needs to be person-centred and should empower the individual to take control of their condition49 with support from the wider multi-disciplinary team.
2.9 Wound-related pain and person-centred care
The European Wound Management Association (EWMA) published a document in 2020 examining the importance of person-centred care emphasising the need to include individuals as partners in their care and treatment. Of equal importance is ensuring that the needs of the individual are at the core of the decision-making process.50
2.10 Key points regarding the nature of wound-related pain
- Wound care procedures have been shown to cause moderate to severe pain in 74% of individuals with open wounds.
- Pain impacts on activity, sociality, and sleep.
- The experience of pain can be related to tissue damage, nerve-related and ischaemic pain.
- The presence of a non-healing wound can give rise to neuropathic pain due to maladaptive plasticity via complex neuro-immune-endocrine interactions.
- Pain is a normal sign in the inflammatory phase of wound healing, so all wounds have the potential to be painful. In combination with other intrinsic and extrinsic factors pain can be exacerbated. Therefore, there is a need to address these as part of the assessment and management of an individual with a wound.
- Psycho-social factors contribute to the pain experience, particularly emotional (psychological) factors which can also act as modulating factors.
- The experience of wound-related pain is complex and needs to take into consideration the psychological and social factors that can impact on an individual’s QoL.
The next chapter will examine the topic of assessment of wound-related pain.
3. Wound-related pain assessment
3.1 Introduction
This chapter reviews evidence related to assessment tools for pain, specifically wound-related pain, and chronic wounds. For the review we supplemented the search for systematic reviews with an update of a previous scoping review undertaken for pain assessment in individuals with chronic lower leg wounds51 to present a narrative review of the evidence. The updated review sought to identify evidence for all chronic wounds of any aetiology. The search strategy and results identified using the L OVE platform are presented first, followed by the narrative review. A summary of recommendations from the evidence, clinical experience and expertise is provided at the end of the chapter to facilitate implementation into clinical practice.
3.2 Method
3.2.1 Search method
The search strategy aimed to find systematic reviews related to the wound pain assessment. We searched L OVE platform, which collects systematic reviews retrieved from the systematic reviews database Epistemonikos7 and allocates them to specific L OVEs and questions.8 We conducted a search in L OVE for wounds and burns on 4 November 2022, and retrieved relevant systematic reviews using this combination of keywords: Pain AND (assess* OR Measure* OR evaluat* OR apprais* OR tool* OR scale* OR questionnaire* OR test* OR chart* ORsurvey* OR diary OR diaries OR report* OR self-report* OR intensity OR severit* OR instrument* OR NRS OR VAS OR VRS OR SF-MPQ OR MPQ OR WBFPS OR FPS) There were no language, publication year or publication status restrictions.
We screened the reference lists of all eligible systematic reviews and hand-searched websites of relevant organisations/institutions and other sources.
3.2.2 Inclusion criteria
Systematic reviews of pain and chronic wounds which discussed an assessment of wound-related pain.
3.2.3 Exclusion criteria
Acute wounds, burns (burn injuries)
3.2.4 Selection of studies
Retrieved titles and abstracts were exported into Rayyan52 by an information specialist Simona Slezáková. The title and abstracts were screened in duplicate and independently by two authors, Nicoletta Frescos and Kirsti Ahmajärvi. The blind mode within Rayyan was kept on until both authors had completed the first screening. Subsequently, the blind mode was turned off to allow the authors to view each other’s decisions. The authors then met to resolve the disagreements and agree which results would move to the second stage of a full-text review of selected articles. Full-text screening was conducted similarly to the title and abstract screening. Following the full-text screening a list of studies for inclusion/exclusion was created. The original search yielded 285 results. Following the title and abstract screening 261 were excluded, the main reason for exclusion being the wrong outcome or population. This generated 24 articles for full text review. Of these, 19 full texts were excluded as they did not have the relevant outcome, population, the detail of assessment tools used in the studies or were not written in English. Five reviews met the inclusion criteria and were included in the analysis. The screening and assessment process is described in detail in the flow diagram (Figure 4).
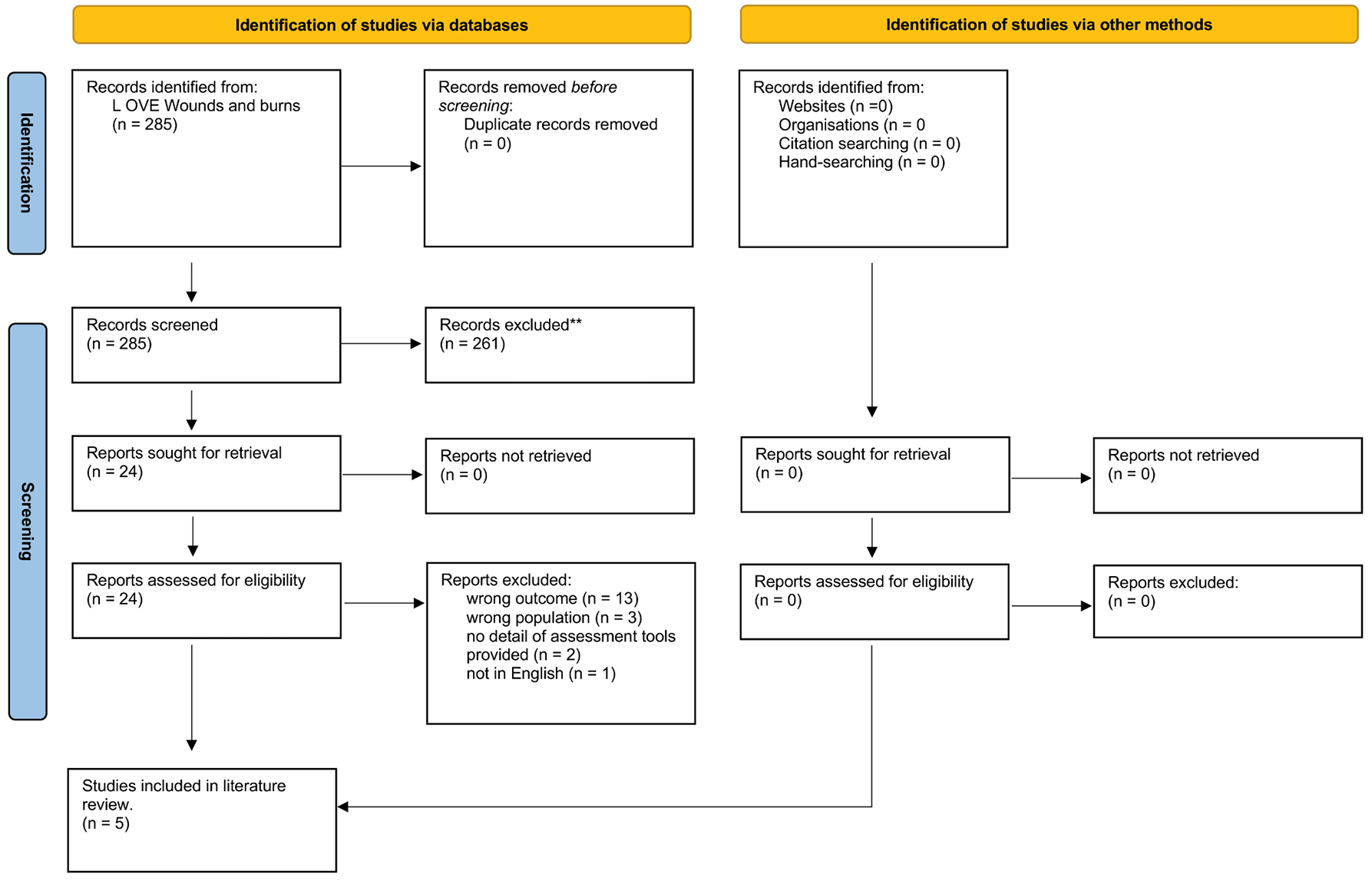
Figure 4: Flow diagram of the screening and the assessment process for wound related pain (modified PRISMA 2020 flow diagram)
3.2.5 Data extraction
Relevant data were extracted from the included reviews by Nicoletta Frescos and reviewed by Kirsti Ahmajärvi.
3.3 Results
3.3.1 Characteristics of the systematic reviews
The five systematic reviews identified a total of 144 studies. The number of studies included in each review ranged from 13 to 70 and the date range for the database search was from 1980–2022 across all the reviews. The studies included in the reviews were conducted predominantly in the United Kingdom, Sweden, Germany, United States with fewer in Portugal, Spain, Poland, Switzerland, Canada, France, Australia, New Zealand, China, Brazil India, Netherlands, Italy, France and Denmark. One study53 did not provide information related to geographical location.
Three of the reviews53,54,55 focused on wound related pain in patients with chronic leg ulcers (venous, arterial and mixed wounds), one review investigated MFWs56 and one investigated skin diseases which were predominately studies related to chronic ulcers (PUs, venous leg ulcers (VLUs) and arterial ulcers).57
In their literature search on PUs/injuries and the treatment of pain, malodour and exudate, De Laat et al.53 said the McGill Pain Questionnaire (MPQ), the Visual Analogue Scale (VAS) and the Faces Rating Scale (FRS) (Appendix 1) were useful tools in the assessment of pain in patients with PUs. The authors stated that although the MPQ has not been tested specifically in patients with PU, it provides a description of the qualities of pain and measurement of pain intensity. De Laat and colleagues noted that the MPQ was difficult for some patients to complete in particular for patients who were acutely ill. They suggested that the VAS was an easy and suitable tool to measure pain associated with PUs, as was the FRS which is known to be useful for patients with speech problems and cognitive impairment. In summary, De Laat and colleagues concluded that the MPQ, the VAS and the FRS are useful instruments to assess PU-related pain.53
The VAS consists of a horizontal line of 10cm long, with ‘no pain’ at one end and ‘worst imaginable (or possible) pain’ at the other end (Figure 5a). Individuals are asked to mark the position on the line that best reflects the intensity of their pain.53,58 Subsequent iterations of the tool include numbers where 0 is no pain and 10 is the worst possible pain (Figure 5b).
Figure 5a: Traditional Visual Analogue Scale (VAS), de Latt et al (2005)53
Figure 5b: Adapted Visual Analogue Scale (VAS), adapted from European Pain Federation59
Note: A mark is placed on the line at the point that represents the level of pain observed. This is measured in millimeters from the left anchor “no pain” to generate a pain score. The word “distress” can replace “pain” to create a distress scale.
Herber et al.54 undertook a systematic review to examine the impact of leg ulceration on patients’ QoL. Twenty-four studies including quantitative, qualitative, and mixed methods were analysed. Pain was described in 11 quantitative and qualitative studies. Thirteen quantitative studies used various QoL and pain assessment instruments to analyse the impact of venous or arterial leg ulcers. The Herber and colleagues stated that overall the studies used validated assessment tools and the frequency of tools used were: Short-form McGill Pain Questionnaire (SF-MPQ) (n=4 studies), Nottingham Health Profile (NHP) (n=3 studies), Hospital Anxiety & Depression Scale (n=2 studies), Health Locus of Control (n=2 studies) (Appendix 1), Short-Form Health Survey (SF-36)60 (n=2 studies), Life Satisfaction Index (n=2 studies), and the Numerical Pain Rating Scale (NPRS) (n=1 study) (Figure 6). One study from Germany used the Tübinger Questionnaire for measuring QoL in patients with chronic venous insufficiency (TLQ-CVI) and another study used the modified version of the Skindex, which is a generic instrument to measure of the effects of skin disease on QoL. It has been used as a basis for more specific tools to measure QoL in particular populations, such as the venous leg ulcer quality of life (VLU-QoL).61
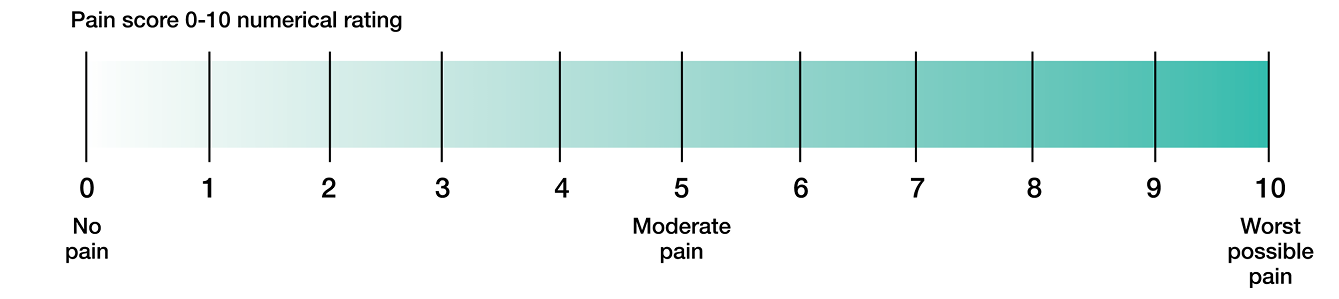
Figure 6: Numerical Pain Rating Scale, adapted from Physiopedia Pain (2023)62
There are various iterations of the Numeric Rating Scale (NRS) and verbal rating scale (VRS), including combinations of both i.e. Numerical Verbal Scale (NVS) or Verbal Numerical Rating Scale (VNRS) or Numeric Pain Scale (NPS). The most commonly used scale in research is the NPRS. In clinical practice the verbal scales are more widely used.
As reflected in the various QoL tools outlined in this study, pain is a multidimensional experience. QoL questionnaires can be classified into generic (e.g., SF-36), disease (e.g., VLU-QoL) and domain specific (e.g., MPQ). Wound related pain encompasses numerous domains including physiological, sensory affective and behavioural and accurate pain assessment can influenced by a variety of factors such as stress, anxiety and coping skills.63 The choice of tool is dependent on what outcome measures are sought, as specific questionnaires do not necessarily capture the full impact of wound related pain on QoL but can be supplemented with an additional, relevant generic tool which can result in a more detailed understanding of the impact.
A more recent systematic review by Purcell et al.55 examined the effectiveness of topical analgesics and topical local anaesthetics for reducing pain in chronic leg ulcers. The review included 23 studies the majority of which were in Europe (n=20). With regards to the assessment tools used to measure pain, these included the NRS (n=5), VAS (n=15), VRS (n=3), and numeric box scale (n=3). For the studies using topical anaesthetic agents the VAS was the predominant pain assessment tool used. The possible reason why the VAS was commonly used in these trials could be due to the ease of administration and scoring and its conceptual simplicity, which can be an advantage in terms of time efficiency for data collection. Furthermore, the VAS is the most studied and commonly used tool in clinical studies and is considered to be the gold standard for pain intensity measurements.64
Gutierrez et al57 conducted a systematic review on the use of topical opioids for various skin diseases, including chronic ulcers, burns, oral lichen planus, post photodynamic therapy and split-thickness skin grafts. The review analysed common formulations of either topical morphine and diamorphine in combination with a hydrogel. Of the 14 studies reviewed, 9 studies focused on chronic wounds, (PUs (n=4), venous and/or arterial ulcers (n=3), or ulcers of various aetiologies (n=2) including traumatic, malignant, cellulitis, and necrotic angiodermatitis). The pain assessment tool used for PUs were VAS (n=2), NRS (n=1) and VRS (none, mild moderate, severe and overwhelming) (n=1). For venous and/or arterial ulcers two studies used VAS and one used NRS. One study on traumatic wounds, malignant wounds and cellulitis used the NRS for their measurement of pain, the other referred to the use of a Numeric Pain Scale (NPS). On further review the NRS and the NPS were one and the same.
The use of three different unidimensional pain assessment tools were identified in these studies, which highlights a lack of consensus in the type of pain assessment tools used and questions the homogeneity and generalisability of pain outcome measures across different wound aetiologies.
Da Costa Ferreira et al.56 conducted a scoping review to synthesise the literature on topical therapies for wound pain management in individuals with MFWs. Of the 70 studies reviewed, the authors found that for the majority of the studies, pain was not assessed using a validated tool. In fact, less than one-third (31.4%) of the studies assessed wound related pain using standardised assessment tools. The tools most commonly used in 22 studies were the VAS, the Numerical Verbal Scale and the multidimensional MPQ. One study assessed pain by categories (no pain, weak, moderate and severe).
3.4 Summary of the evidence from the systematic reviews
Based on the findings of the five systematic reviews evaluated there is evidence related to the assessment of pain in individuals with chronic wounds including, PUs, leg ulcers and MFWs (Appendix 2). In some studies pain was assessed using a form of rating scale i.e., VAS, NRS, McGill, FRS in other studies pain and discomfort was assessed as part of a wider consideration of QoL. Given the multidimensional nature of pain, it is perhaps justified to use more comprehensive measures that incorporate QoL and reflect a biopsychosocial approach to pain. However, we also recognise that there are circumstances where clinicians want to be able to assess wound-related pain specifically, therefore, as part of this chapter we also undertook a wider review of the existing evidence with a view to developing recommendations for clinical practice.
3.5 Narrative/thematic review of assessment of wound-related pain
3.5.1 Search strategy
We conducted a further literature search for validated pain assessment tools to assess and/or measure wound related pain. The search strategy aimed to find relevant and high-quality literature related to the topic of validated pain assessment tools to assess or measure wound related pain. The following databases were searched on the 23 December 2022 in collaboration with a research librarian. Medline (Ovid Platform 1946 onwards), Embase (Ovid Platform 1947 onwards), PsycINFO (Ovid Platform 1806 onwards) and CINAHL (EBSCO Platform 1937). The literature search was limited to the following study types, clinical trials, guidelines, systematic review, meta-analyses, observational studies, validation studies or randomised controlled trials (RCTs). Search results were limited to English language and human articles only. Lower limb/extremities-related articles were excluded. There were no limits or restrictions placed on publication years or publication status.
The following MeSH and keywords were searched using the appropriate Boolean operators: Pain Measurement/, “Surveys and Questionnaires”/, Nursing Assessment/, Pain/, Chronic Pain/, Nociceptive Pain/, Pain Perception/, “Wounds and Injuries”/, Wound Healing/, Ulcer/, Surveys/, exp Questionnaires/, exp Measurement/, (MH “Wounds and Injuries”), (MH “Wounds, Chronic”), (MH “Fungating Wounds”), (MH “Wounds, Penetrating”), (MH “Surgical Wound Dehiscence”), (MH “Pain”), (MH “Questionnaires”), (MH “Surveys”), (MH “McGill Pain Questionnaire”), (MH “Clinical Assessment Tools”), (MH “Pain Measurement”), (pain adj2 assessment*), (pain adj2 tool*), (pain adj2 score*), (pain adj2 questionnaire*), (pain adj2 survey*), (pain adj2 measure*), (pain adj2 scale*), (pain adj2 instrument*), (pain adj2 chart*), (pain adj2 appraisal*), (pain adj2 indicat*), (pain adj2 self report*), (pain adj2 check list*), pain*, pain assessment tool*, pain scale*, pain measure*, pain assessment*, pain rating scale*, pain questionnaire*, pain survey*, wound*, ulcer*, coloni?* wound*, contamin* wound*, infect* wound*, coloni?* ulcer*, contamin* ulcer*, infect* ulcer*, validate*, validation, validating.
For a more detailed search strategy for each database please see Appendix 3. A secondary search was conducted via Google Scholar to look for any related articles not indexed in the above databases. The librarian screened the reference lists of all eligible articles and hand-searched the websites of relevant organisations/institutions and other sources.
3.5.2 Data management
All citations were initially exported into Endnote X9 (Thomson Reuters, New York, USA) for automated removal of duplicates, and the remaining unique citations were imported into the Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia) and any further identified duplicates were removed.
3.5.3 Study selection
The Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia) was used by two independent reviewers during the study selection process to screen titles and abstracts: Nicoletta Frescos (NF) and Kirsti Ahmajärvi (KA) and any conflicts were discussed and resolved at this stage of the study selection process. NF conducted the full-text review and extracted the data using a data extraction tool developed by NF and previously tested on two articles to assess their adequacy.
3.5.4 Search results
The original search yielded 89 results, following the screen of titles and abstracts 56 were excluded, the main reason for exclusion being the wrong study outcomes, wrong populations (burns, other skin conditions) or was not related specifically to pain in chronic wounds. This generated 27 articles for full text review, eight of which were excluded as they were the wrong study design or wrong populations, and one was not in English. After searching other sources of literature one additional paper was added, thus a total of 20 articles were used for thematic review. The screening and assessment process is outlined in Figure 7.
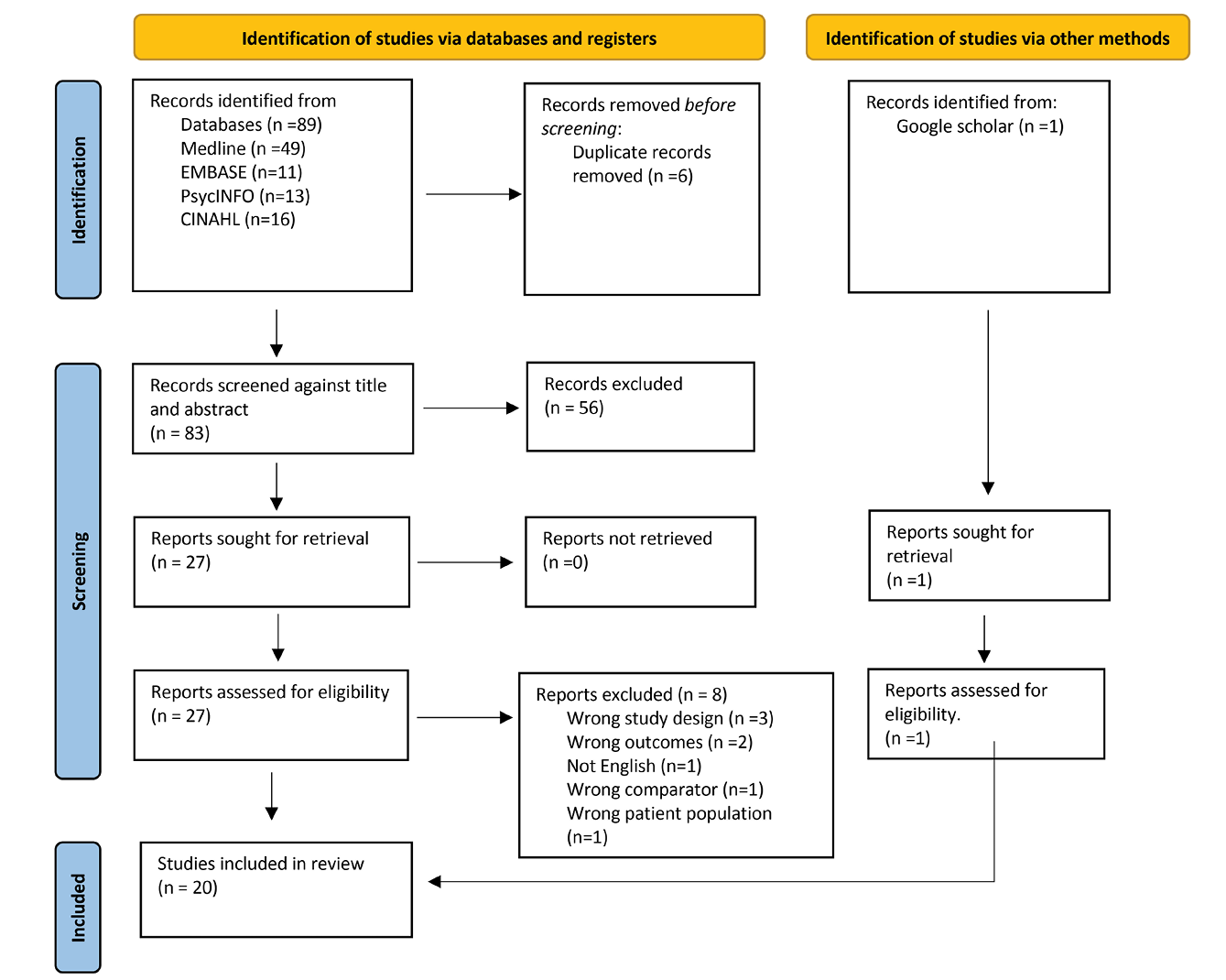
Figure 7: Flow diagram for the narrative review (modified PRISMA 2020 flow diagram)
3.5.5 Characteristics of the studies
The majority of studies were undertaken in the United Kingdom (UK), specifically England (n=6, 31.5%), followed by the Canada (n=4,21.1%). Nine studies (47.3%) were published in the last six years (2016–2022). Regarding the types of studies, 7 (35%) were cross-sectional studies, 4 (20%) non-systematic literature reviews, 2 (10%) prospective cohort studies and 7 (35%) other methodologies including, surveys, a systematic review with Rasch analysis (Appendix 4). Six studies (30%) included QoL as a component of wound-related pain assessment.
The characteristics of the studies will be described thematically-based on the study design and outcomes and will describe the assessment tools used. The review identified six categories of studies on wound-related pain assessment tools:
- Literature review of pain assessment tools for wound related pain
- Assessment of the utility of pain assessment instruments for chronic wound-related pain
- Instruments assessing QoL and psychosocial impact of wound related pain
- Models of pain assessment and frameworks
- Generic studies on assessment of wound-related pain
- Special population specific instruments.
3.6 Pain assessment tools for wound-related pain
There were five reviews undertaken that examined the literature on wound pain assessment.65,66,51,67,68 Three of these reviews65,66,51 focused on pain in chronic lower limb wounds, one focused on wound related background pain68 and the other67 reviewed pain in chronic wounds as a more general topic.
Nemeth et al65 compared the psychometric, clinical sensibility, and pain-specific properties of pain assessment tools for individuals with leg ulcer. The authors identified 54 pain assessment tools of which five met their criteria. The five tools appraised were Pain Ruler, NRS, VAS, VRS and the SF-MPQ. The Pain Ruler is a ruler that has eleven points from 0 (no pain) to 10 (excruciating pain). The patient matches the word which they feel describes their pain to the number that corresponds to their pain intensity.69 Nemeth and colleagues concluded that each tool met the psychometric, clinical sensibility, and pain-specific criteria to varying degrees. The most extensively used tool in the leg ulcer population was the VAS, which was used in eight studies, followed by the SF-MPQ, which was used in three studies, and the VRS used in two studies. Whilst these tools demonstrated reliability and validity, no evidence indicated that the five tools had been specifically evaluated psychometrically with the population of individuals with leg ulcers.
In an integrative review Newbern66 examined the experience and perceptions of pain to identify the effects on QoL in patients with chronic wounds related to lower extremity vascular disease. Newbern said one of the key drivers for this study was that the lack of validated clinical assessment tools to assess pain was a barrier to adequate assessment,66 the author also cited the findings of a study by Dickinson et al (2016) on wound pain associated with DFUs, found a difference in clinician and researcher-reported pain prevalence and that clinicians often underassess pain prevalence when they are not using a formal pain assessment tool. As part of the review, Newbern appraised the evidence related to pain assessment practices. Of the 14 studies, 11 pain instruments were reviewed. Pain specific tools (n=3) included: the Brief Pain Inventory (BPI), NRS and the SF-MPQ; tools that measured QoL (n=3): Modified EQ-5D Questionnaire, Medical Outcome Study (MOS) Pain Measures and SF-36 Health Status Questionnaire. Four tools which assessed neuropathic pain specifically: the Neuropathic Pain Scale, Neuropathic Pain Symptom Inventory and the Diabetic Peripheral Neuropathic Pain Impact Measure. Two other assessment tools in the review were included because of their relevance to the psychosocial impact of pain; the Hospital Depression and Anxiety Scale related to pain perceptions and delayed wound healing to increased depression and anxiety and the Brockopp-Warden Pain Knowledge/Bias Questionnaire which compares the provider perception of pain with the patient perception of pain. Newbern’s review was narrative rather than analytical concluding that there is a lack of validated pain and QoL assessment tools for individuals with DFUs or chronic lower extremity wounds.
The aim of the scoping review by Frescos51 was to ascertain if a validated and holistic pain assessment instrument is available for use in the primary care setting to assess wound pain in chronic lower limb wounds. From the four studies that met the inclusion criteria seven of the most commonly used generic assessment tools were identified and appraised. Only four assessment tools, the NRS, VAS, VRS and SF-MPQ were justified to be suitable for leg wounds. The review concluded that there is insufficient evidence to recommend one pain assessment tool that is suitable for all chronic lower limb wounds.
The review by Jenkins67 focuses on the biopsychosocial perspective and highlights six pain domains. As there were no validated pain assessment tools found specifically for chronic wounds the recommended pain assessment tools discussed for each domain were based on the Outcome Measures’ guidance developed by the British Pain Society (BPS), and the Faculty of Pain Medicine (FoPM) (2019). Jenkins67 noted that tools to assess wound-related pain need to address pain quantity, physical functioning, emotional functioning and a person’s global rating. Jenkins67 recommended the use of unidimensional pain tools (which include the VAS, VRS and NRS) for pain quantity or measurement.. These are used to determine the level of chronic pain and to evaluate the effectiveness of pain management specifically.
The BPI is recommended for assessment of the impact of chronic pain on physical functioning as it is a multidimensional tool and has been psychometrically and linguistically validated in many languages70. To assess the impact on emotional functioning the Becks Depression Inventory (BDI) and the Hospital Anxiety and Depression Scale (HADS) were deemed appropriate. These screening tools identify whether there is a need to refer the patient for a mental health review and management. Jenkins also discussed the Patient Global Impression of Change questionnaire to provide a long-term evaluation of the patient’s rating on the progress of their wound pain management strategy.67 As in the other literature reviews, Jenkins concluded that there was a lack of validated pain assessment tools for wound-related pain for individuals with chronic wounds.
The systematic review and meta-analysis by Leren et al.68 predominately focused on wound-related background pain in individuals with chronic VLUs (CVLUs). Background pain is defined by Leren and colleagues as, “pain that is related to the underlying cause of the wound, local wound factors and other related pathologies, such as skin irritation”, Leren and colleagues clarified that for the purposes of their review background pain was, “wound-related pain that is not caused by dressing changes or other procedures”.
In total 36 studies were included of which the majority (n=27) reported pain intensity. The common assessment tools used were NRS (n=12 studies), VAS (n=10 studies) and VRS (n=6 studies). Leren et al stated that there was variation in how the tools were applied: For example, different versions of the VRS and NRS. Furthermore, various anchor points were used, for example, zero was not always used as the lowest point, but all tools included a point that related to no pain, and for the highest point, various descriptions were used such as “unbearable pain, worst pain ever experienced, severe pain, intense pain, most pain”. This required the authors to use standard methods for converting different rating scales for the purposes of the meta-analysis.
Other tools used for pain characteristics were the SF-MPQ (n=3 studies), the neuropathic pain questionnaire DN4 (n=1 study), and the BPI for pain interference in sleep (n=1 study). Leren et al68 concluded that researchers and clinicians did not use standardised methods for assessing background pain in individuals with wounds. They argued that this was due to the lack of standardised methods for defining aetiology of wounds, as well as conceptualising, defining, and assessing core outcome measures such as pain.
3.7 Assessment of the utility of pain assessment tools for wound-related pain
Four studies assessed the utility of pain assessment tools for chronic wound-related pain.71,34,72,73
3.7.1 Leg ulcers
Noonan and Burge71 investigated the differences in pain characteristics of venous, arterial and mixed arterial/venous ulcerations, the authors used the unidimensional scales VRS and the VAS to measure pain intensity and the SF-MPQ sensory and affective dimensions to measure the quality of pain. The COOP Chart System74 was used to measure pain and general function, health and QoL. The COOP Function Charts are a brief screening tool to measure patient function status in the primary care setting. There are nine charts which measure:
- physical condition
- emotional condition
- daily work
- social activities
- pain
- change in condition
- overall condition
- social support
- QoL
For each chart there are five responses to choose from, each response is illustrated with a drawing that graphically illustrates the five points. High scores represent unfavourable scores on the measure.75
Leren et al stated that the unidimensional rating scales fail to reflect the complexity of pain, thus the SF-MPQ was also used, as it provides a better description of the complexity of pain: It includes word pain descriptors and, therefore, demonstrates the multidimensional nature of pain. Furthermore, they noted that reliable and validated pain measurement scales should not be used in isolation, meaning that the assessment of other influencing factors such as physical, psychosocial and emotional factors, should be included as these impact an individual’s perception of pain, which can in turn influence the effectiveness of interventions for the management of wound-related pain. This is a particularly interesting viewpoint as based on the evaluation of the systematic reviews that have been undertaken since this early study researchers seem to be focused on identifying the most valid and reliable pain assessment tool to use, which potentially perpetuates the notion that there is such a tool.
3.7.2 Pressure ulcers (PUs)
In their study of individuals with a spinal cord injury (SCI) and a PU, Roth et al34 investigated the associations between pain measures, (NPRS, and MPQ dimensions) and psychosocial measures and pain (pain catastrophising and mood variables). The NPRS is a reliable and valid unidimensional assessment of pain intensity that is sensitive to changes in pain experiences 76. The MPQ is a multifactorial measurement of present pain intensity and quality.51 The SF-MPQ was found to be more sensitive to pain experience than a unidimensional rating of pain intensity as measured using the NPRS. The MPQ showed a positive relationship between increasing pain experience and advanced wound stage, whereas the NPRS did not discriminate changes in the severity of pain across the stages of wound severity.
To assess the relationship between measures of pain, depression and affective distress, Roth et al used the Centre for Epidemiologic Studies Depression Scale,77,78 which consists of a 20 item scale for depressive symptoms and from the Brief Symptom Inventory, the Global Severity Index was used to measure global affective distress.79 The scale for pain catastrophising was derived from the Coping Strategies Questionnaire80 which uses a 7 point scale to assess the individuals use of various coping strategies when dealing with pain.
Roth et al34 found that the NPRS had a significant correlation with pain catastrophising (r=0.63, p<0.05), but did not relate to any of the other pain rating scales of the MPQ or measures of depression and distress which are commonly associated in individuals with chronic pain. The MPQ total and sensory scale were statistically significantly related to the Global Severity Index (r=0.62 and p<0.05, r=0.61 and p<0.05, respectively) and to the depression scale (r=0.91, p<0.001), however no association was found with the NPRS for either affective distress or depressive symptoms. Pain catastrophising was positively related to pain intensity (r=0.63, p<0.05) and more severe levels of affective distress (r=0.84, p<0.001) and more severe depressive symptoms (r=0.89, p<0.001). Roth and colleagues concluded that the results support the relative utility of the multidimensional MPQ for the assessment of chronic wound pain in individuals with SCI and PU when compared to the unidimensional NRS.
3.7.3 Chronic pain: nociceptive and neuropathic mechanisms
Nociceptive and neuropathic mechanisms often coexist in individuals with chronic pain.81 Two studies72,73 investigated assessment instruments that would be suitable in differentiating neuropathic pain symptoms to diagnose the underlying pathophysiological mechanisms of pain in different populations.
The Leeds Assessment of Neuropathic Symptoms and Signs Scale (LANSS)82 is a validated and reliable tool used to discriminate between neuropathic and nociceptive pain.83 The LANSS includes five patient-reported symptom items and two clinical sensory testing items associated with neuropathic pain. Rutherford72 used the LANSS to investigate whether it is a suitable tool as an outcome measure in people with PU related pain. The psychometric and Rasch analysis was undertaken with a sample of 709 patients with PU. The findings did not support the LANSS as a reliable and valid tool for the measurement of PU-related neuropathic pain. It was unable to detect clinical change in neuropathic pain in response to treatment and may underestimate differences in pain experienced for people with severe PU. There was low correlation between the LANSS and VAS indicating that neuropathic pain as measured by LANSS was not related to pain intensity. Rutherford et al proposed that the LANSS remains primarily a screening tool as it is not suitable for outcome measures.
The MPQ uses different descriptors that can differentiate neuropathic from nociceptive pain (Appendix 1). Kogure et al73 utilised the MPQ to categorise ischaemic pain into nociceptive /inflammatory pain or neuropathic pain. Kogure and colleagues examined the discriminant validity of the category by providing a list of distinct pain quality descriptors in the MPQ to dichotomise the types of pain. Kogure et al argued that the underlying pathophysiological mechanisms of ischaemic ulcer pain include a strong neuropathic component based on the underlying being related to peripheral vascular disease (including diabetic angiopathy) which is an inflammatory and nociceptive pain condition. Two categories of neuropathic pain characteristics were proposed: superficial pain descriptions of neuropathic quality and deep-somatic descriptions of nociceptive quality.
Using 78-word descriptors from the MPQ, Kogure et al investigated pain characteristics in 365 patients with neuropathic pain and 124 patients with nociceptive pain which included inflammatory pain. The diagnosis of was based on the history and clinical examination including some imaging. The patients who were categorised as having neuropathic often described their pain as ‘cutting’ and ‘burning’ pain, and the coefficients of these descriptors had a high numerical value in the discriminant function. Patients categorised as having nociceptive pain frequently used word descriptors of ‘squeezing’ and ‘dull’ pain, these words are not included in the other neuropathic screening tools. Kogure et al concluded that although the MPQ descriptors were not able to distinguish between different types of pain, the MPQ has the potential to differentially diagnose various pain disorders and assist in diagnosing the underlying pathophysiology. Kogure et al also argued that this can potentially be useful in guiding the selection of appropriate analgesics for the treatment of pain.73
The assessment of pain is quite complex due to the multidimensional properties and qualities of pain, measuring specific dimensions of pain can help to establish the cause of, in this instance neuropathic pain, and guide appropriate management strategies as demonstrated by Kogure’s study.73
3.8 Instruments assessing quality of life (QoL) and the psychosocial impact of wound-related pain
From Chapter 1 of this document, you will be aware that pain has many properties and qualities; it is multidimensional, as it is a combination of factors including sensation, emotion, nerve and memory. The assessment of pain should include the physical, psychological and emotional impact for assessing the biopsychosocial aspects of pain. Multidimensional pain assessment tools are usually used to assess chronic pain and measure how pain affects QoL. A number of studies have examined the links between pain and psychosocial factors using generic QoL assessment tools.40,66,84
The assessment of different dimensions of pain and its impact on QoL in people with chronic wounds was reviewed by Jenkins.67 The review examined instruments to assess physical functioning and emotional functioning.
In total eight multidimensional tools were discussed. The BPI was recommended to assess physical functioning. The BPI measures pain, physical and emotional functioning. It is designed to measure both pain intensity and the interference pain has on functional activities.85,86 The SF-BPI contains one item and uses the NRS to measure how much pain has interfered with certain aspects of life: mood, sleep, walking ability, social activity, relations with other and enjoyment of life. Several studies have shown good test-retest reliability and sensitivity to differences in pain characteristics associated with different diseases, as well its suitability for repeated evaluation of pain.87,88 The measure has also been shown to be valid and reliable across widely different cultural and linguistic backgrounds.89
Jenkins67 considered seven tools designed to measure emotional functioning, discussing two related to depression in more depth. The Beck Depression Inventory (BDI) measures characteristic attitudes and symptoms of depression and includes 21 items that ask questions about mood, self-dislike, social withdrawal and sleep disturbance. Each item has scoring from 0–3 to reflect their intensity. Higher total scores indicate more severe depressive symptoms. Similarly, the HADS also asks a series of questions to identify symptoms of anxiety and depression. The scoring is based on two subscales anxiety (HADS-A) and depression (HADS-D). It has 14 items that is rated on a scale from 0–3. A higher total score indicates higher distress. The EuroQol 5D90 was listed as a recommendation as the tool of choice for the measurement of QoL.
3.8.1 Venous leg ulcers (VLUs)
In a RCT on the cost effectiveness of community leg ulcer clinics, Walters et al91 compared four generic instruments for measuring health-related quality of life (HRQoL) in people with VLUs. The MOS 36-Item Short-Form Health Survey (SF-36); EuroQol (EQ); SF-MPQ and the Frenchay Activities Index (FAI) were completed by 233 patients on three occasions, initial assessment, 3 months and 12 months.
The SF-MPQ was used as a quantitative measure of pain. Walters et al evaluated the capacity of the instruments to differentiate between patients with healed or not healed venous ulcers at a point in time (discriminative properties) and measured any change in HRQoL in the patients over time (evaluative properties) in response to treatment. The SF-36 M was the most widely used generic HRQoL questionnaire at the time. It contains 36 questions measuring health across eight dimensions of physical functioning, role limitation because of physical health, social functioning, vitality or energy, pain, mental health, role limitation because of emotional problems and general health. The questionnaire generates a score from 0–100, where 100 indicates ‘good health’. The EQ consists of five questions on mobility, self-care, usual activities, pain and anxiety. The FAI is intended to measure the level of independence. It is a 15-item questionnaire with three domains: ability to undertake domestic chores; leisure or work; and outdoor activities. Items are recorded for frequency of the activity in the past 3 months and for the past 6 months. The scores range from 15–60. Walters et al.91 highlighted that consideration should be given to the time interval for use of the various questionnaires. For example, all the dimensions of the SF-MPQ refer to pain in the past week except for one item VAS Now which asks about the status.91 Similarly, the EQ also questions the current health status on the day of the completion of the questionnaire, whereas the SF-36 items are a combination of health status now and in the past four weeks. The FAI asks about the frequency of activities over 3 to 6 months. These time intervals make it difficult to interpret the relative evaluative properties of the instruments particularly when measuring short term changes and using instruments with long time interval reference periods.
Walters et al91 noted that as there is no specific assessment tool for evaluating the outcome of interventions in individuals with VLUs, the SF-MPQ can be used for short term follow up, and the SF-36 for longer term follow up, with or without the SF-MPQ.
3.9 Pain in older persons with chronic wounds
Woo92 explored the relationship of attachment style and pain in older persons with chronic wounds. Woo noted that according to the attachment theory:
Pain is perceived as a threat that often triggers negative emotions such as fear and anxiety. To control and regulate the impact of negative emotions, the attachment system is called into play, precipitating a sequence of events and attachment behaviours.92 (p171)
The SF-MPQ was used for the assessment of characteristics of chronic wound pain, the NRS was used to measure pain intensity and the Pain Assessment in Advanced Dementia (PAINAD)58 scale was also used. The PAINAD is an observation pain tool that assesses behavioural domains of breathing, negative vocalisations, facial expression, body language and consolability.58 The two assessment instruments that were employed to determine the psychological and behavioural determinants were the Relationship Scales Questionnaire (RSQ), and the Shortened Anxiety Scale (SAS). The RSQ helps to discriminate three attachment patterns described as: secure, avoidant (dismissing), and ambivalent. It is a relatively easy instrument to complete in particular for older adults as it has minimal risk of response fatigue.93 The SAS is a subjective measure of anxiety. It is a short form item scale that was derived from the Spielberger State-Trait Anxiety Inventory94 which has 20 items to measure the frequency of present state anxiety and trait anxiety, being how much anxiety represents personality characteristics. The SAS includes six self-reported items; frightened, worried, nervous, comfortable, pleasant, and at ease.
Subjects rate each adjective on a four-point Likert scale ranging from ‘not at all’ to ‘very much’.
Woo92 evaluated pain, anticipatory pain, anxiety and attachment patterns for wound dressing changes. The author compared the scores at baseline, dressing removal, cleansing, dressing reapplication and shortly after dressing changes. The results showed that participants who experienced higher levels of attachment anxiety represented by fearful avoidant and preoccupied attachment patterns expressed higher levels of anticipatory pain, anxiety prior to dressing change, and pain during dressing change than individuals who are secure with their relationship between attachement and pain. Additionally, participants with Avoidant attachment expressed the highest levels of anticipatory pain and anxiety. In contrast, Dismissive attachment style was characterised by the lowest anticipatory pain and anxiety scores. Woo (92) concluded that clinicians must be aware of the impact of personality, anxiety and anticipation of pain can have on patients’ pain experiences and that there is complex relationship between pain, anxiety and attachment (self-insecurity) behaviours.
3.10 Models and frameworks for pain assessment
3.10.1 Heal not hurt
Heal not hurt is a wound pain assessment and recording tool developed by Barrett95 with industry support to improve wound pain management at dressing changes. It is a two-sided document that acts as a prompt to assess pain, one side consists of four assessment tools for pain: FRS, VRS, VAS and NRS and lists key questions to prompt the basis of the assessment plan and care. The other side is a documentation sheet to record patients’ pain scores before, during and after dressing changes. The tool has not been validated and has only undergone an evaluation in its pilot stage. No evidence of citations was found in other studies, nor information on the extent of its use, however it is a simple user-friendly tool that can be used by nurses to assess and manage pain and improve documentation.
3.10.2 Toronto Symptom Assessment System for Wounds (TSAS-W)
Maida, et al96 developed the Toronto Symptom Assessment System for Wounds (TSAS-W) to measure pain and symptom distress associated with common wounds. The TSAS-W is a patient-rated symptom assessment tool using the 11-point NRS to measure the poly-symptoms burden directly related to wounds. The symptoms include: pain (during dressing and /or debridement and between dressings and / or debridement); exudate; cosmetic concerns; odour; itchiness; bleeding; mass effect (swelling or oedema around the wound, bulk or mass effect from wound and bulk or mass effect from dressings); crusting and restricted movement. This was a two-phase study with the first phase identifying the most common symptoms association with wounds and the second phase was the development of the TSAS-W. The tool was developed to address a gap in palliative wound care that includes the assessment of wound-related pain and symptom issues from the patient’s perspective. Although the TWAS-W shows promise, it has not been tested for reliability or validity, nor is there evidence of its use in the literature. The study emphasised the need for assessment tools that measure wound-related pain and symptom issues as highlighted by the lack of appropriate assessment tools in their literature review. The availability of these types of tools, instruments, or questionnaires may serve to promote improvements in clinical assessment and result in improved outcomes, especially when they are completed by the patient.
3.10.3 Wound Associated Pain model (WAP)
A prospective study of 111 participants with leg and foot ulcers was conducted by Woo and Sibbald97 to evaluate pain control and healing trajectory of chronic wounds by applying the Wound Associated Pain (WAP) Model (Figure 8). The model was developed to assist practitioners in managing the complexity of chronic wound associated pain and integrating the principles of wound pain assessment and management into principles of wound bed preparation. The WAP model consists of three components: patient centred care; wound aetiology; and local wound factors. The NRS was the pain instrument used for the study, as Woo and Sibbald stated it is a reliable and validated tool based on the study by Herr and Mobily (1993) who found the NRS to be significantly related to the Pain Thermometer (r=0.91), the vertical VAS (r=0.92) and the VRS (r=0.91) in older patients, and more reliable than the VAS in people with lower education levels (Taylor and Herr 2003).
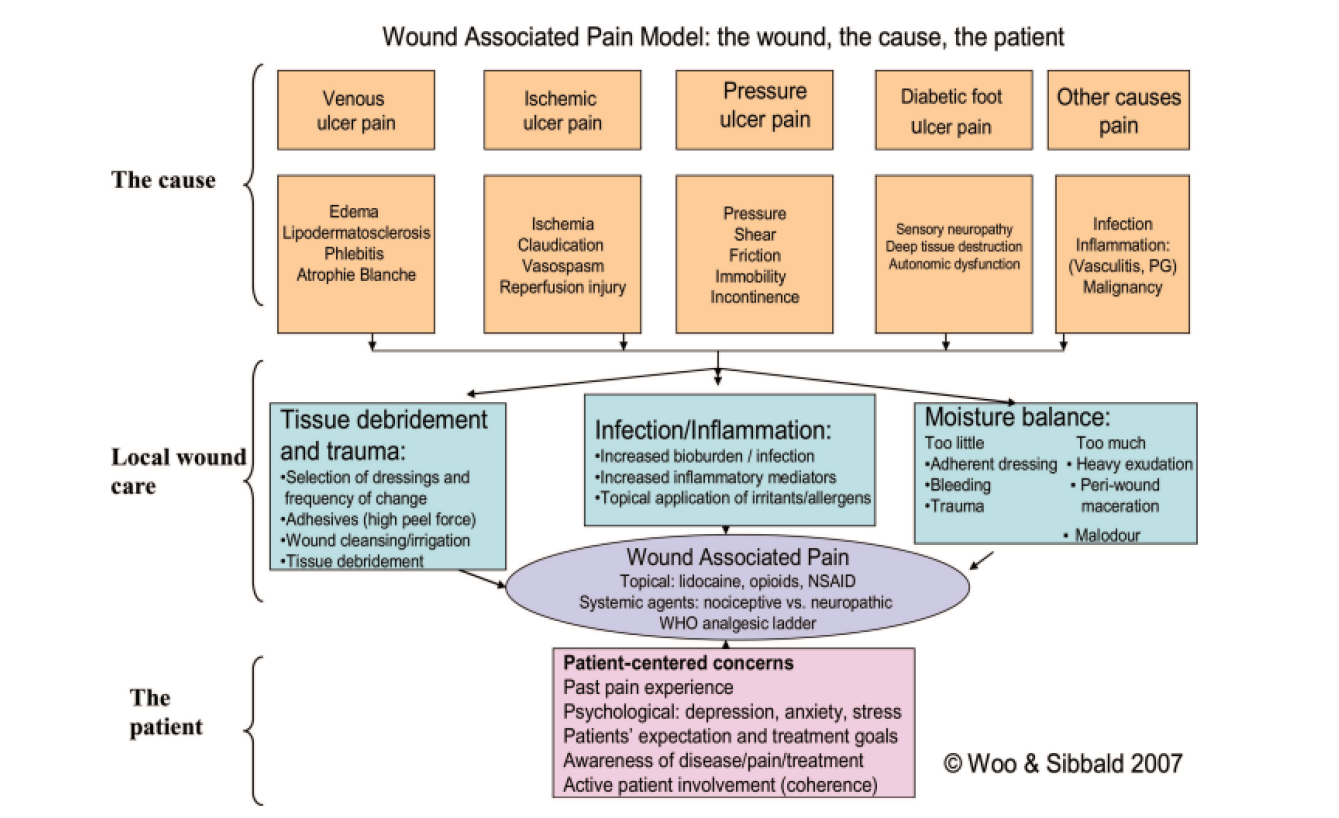
Figure 8: Wound Associated Pain Model: the wound, the cause, the patient, Woo and Sibbald (2007)97, permission to use granted
The results showed that more than 60% of participants reported wound-related pain at the beginning of the study. By applying the WAP model, significant changes were found in pain intensity (p<.001), when correcting the wound cause, addressing the patient-centred concerns and using pain reduction strategies, such as careful selection and application of wound dressings, and use of topical or systemic analgesics. Woo and Sibbald97 concluded that a comprehensive patient assessment as outlined in the WAP Model can improve wound-related pain and healing rates for chronic leg and foot ulcers.
3.11 Generic evidence on wound-related pain
In a narrative discussion regarding considerations and procedures for managing pain in patients with chronic wounds White98 discussed key elements of pain assessment. White argued that a holistic patient assessment is paramount in understanding the patients pain experience and that no single pain measuring scale suits all patients. Once the appropriate tool is chosen, based on the needs of the patient, the same tool should be used for subsequent assessments. The assessment should include: identifying the pain type whether it is nociceptive, neuropathic or mixed; the duration and severity of pain; the impact pain has on the patient; and pain relief rating in terms of assessment of post-pain treatment scores.
Frescos99 undertook a survey of 1189 wound healthcare practitioners to determine how practitioners assess wound-related pain, including the types of assessment tools used and frequency of assessment. Frescos found that 63% (n=738) of practitioners indicated that they used a validated pain assessment tool. The most common assessment tools used were the VAS (n=52) and NRS (n=328), other tools used were the VRS, FRS and the Abbey Scale which is used for patients with dementia. When comparing the use of validated tools between the professions, nurses were more likely to use the VAS, faces scale and NRS than other professions involved in wound management. However, the majority of practitioners used a combination of different assessment tools and or methods based on the patient’s cognition, language or vocabulary.
In an exploratory study Leren et al100 used a combination of three tools and a question about avoidance of physical activities because of their ulcer pain was used to assess pain fluctuation in individuals with CVLU. The characteristics of ulcer-related background pain was assessed using SF-MPQ and BPI providing scores for ulcer pain intensity, pain interference and pain qualities. Leren et al used one question from the Pain Quality Assessment Scale (PQAS) which is a validated tool for assessing various types of neuropathic and nociceptive pain. To assess how pain fluctuated during the day, the participants were asked whether their pain was intermittent, variable, or constant. This study highlights the necessity to combine several pain assessment questionnaires to measure the variety of pain characteristics for a holistic pain assessment and effective pain management.
3.12 Pain assessment tools for individuals with a cognitive impairment
According to Breuer,101 failure to report pain is common among those with communication difficulties. The author also noted that cognitive impairment in older people adds further complexity in determining and measuring pain. Assessing pain in patients with cognitive impairment or non-verbal patients is considered as a major challenge. Three different pain assessment tools that were specially designed to assess the pain in people with difficulty in verbally expressing pain were identified within five studies included: the FRS (n=3), the PAINAD scale (n=3) and the Abbey scale (n=1).
3.12.1 Faces Rating Scale (FRS)
The FRS, also known as the Wong-Baker FACES™ Pain Rating Scale, is a self-reporting pain scale used mainly for children and adults who cannot understand other scales. The FRS is a visual scale which uses cartoon faces ranging from a smiling face for ‘no pain’ to a tearful face for ‘worst pain’ (Appendix 1). Studies have shown that these scales are beneficial for patients who have learning difficulties or poor language skills.102 The Faces Pain Scale-Revised (FPS-R)103 features faces with increasingly pained expressions but no smiles or tears. The scale uses a 0–10 metric with 0 = no pain and 10 = very much pain.
A cross-sectional study by Dallam et al104 used both the VAS and FRS to determine the perceived pain intensity of PUs in hospitalised patients. The VAS pain scores were found to be inversely correlated with age and positively correlated with maximum pain intensity of FRS. The evaluation showed that although both tools could be used by cognitively impaired patients, they found it was easier to respond to the FRS than to the VAS, as did patients from culturally diverse populations where English was not their first language. Freeman et al105 also used the VAS and FRS to quantify PU pain in hospitalised elderly patients. They found high reliability between VAS and FRS for pain assessment in populations with diminished verbal and cognitive impairment and concluded that the FRS was a valid measure of assessing pain in the older person.
3.12.2 PAINAD
Woo92 and Ren et al106 endorsed the use of the PAINAD scale for individuals with dementia. This is supported in the review by Jenkins67 who also recommended the PAINAD scale as a valid and reliable tool for the assessment of pain in non-verbal older adults or individuals with cognitive impairment.
The PAINAD is used to determine the behavioural indicators of pain in cognitively impaired and non-communicative individuals.92 It is a five-item observational tool that assesses breathing, negative vocalisation, facial expression, body language, and the ability to be consoled. Each behaviour can be graded from 0 to 2 according to the severity of behaviour exhibited, thus giving a total score of 10, with mild pain having a score ranging from 1–3, moderate pain 4–6 and severe pain 7–10. Warden et al58 identified that the PAINAD score has a strong correlation with an observer-rated pain severity VAS.
Woo92 utilised the PAINAD to evaluate the behavioural indicators of pain at before, during and after dressing and found that there is increased number of pain-related behaviours during dressing changes and that facial expressions were the most observed behaviours, followed by body movement and vocalisation. Ren106 examined compliance with evidence-based criteria for individuals with DFUs, specifically in relation to assessment and management of dressing related pain. The VAS was used to assess pain and for those with cognitive impairment the Chinese-PAINAD scale was used. One of the key barriers found by Ren was the lack of standardised pain assessment tools to drive the implementation of best practice for wound pain assessment.
3.12.3 Abbey Scale
In the survey by Frescos99 on pain assessment tools for wound-related pain, the results indicated that the FRS and Abbey Scale were common tools used by healthcare practitioners in wound care to assess pain in people with dementia or who were unable to verbalise their pain. The Abbey Scale is specifically for use with patients with end or late-stage dementia who are unable to verbalise or articulate their needs. It is a one-page assessment tool which uses non-verbal observable cues which are then scored to ascertain the level of pain the person is experiencing.107 The tool is easy to use and takes one minute to administer and document the results. The tool can also be used as a measure of effectiveness for interventions. The pain scale has been found to have high inter-rater reliability.108 Although there is limited evidence in the literature to validate the clinical use of the scale, it is a commonly used in Residential Aged Care facilities for the assessment of people with cognitive impairment who cannot describe their experiences of pain coherently.109
3.12.4 Face, Legs, Activity, Cry and Consolability (FLACC) Scale
Although the search strategy for this review did not find any studies on assessment of wound-related pain in children it is worthy to note the Face Legs, Activity, Cry and Consolability (FLACC) Scale (Appendix 1). This is a commonly used behavioural observation pain scale in infants and children for the measurement of three types of pain, including procedural pain, postoperative pain and acute pain has been culturally adapted into different versions for use in different clinical settings.110 However, the FLACC scale is limited in the capacity to discriminate between pain and distress. A systematic review evaluating the reliability, validity and feasibility of the scale found that there was sufficient evidence to support its use in post operative pain assessment111 and in procedural pain measurement110 despite concerns to distinguish between pain and non-pain related distress. A study evaluating the psychometric properties112 also supported the use of the FLACC scale for measuring observational pain in infants and children but stated that further studies are still needed to provide robust evidence.
3.13 Pain assessment and clinical product evaluations
Pain assessment tools are frequently used for clinical evaluations of new wound care products. Tickle94 noted that in three different clinical evaluations of foam dressings the studies used different tools including the VAS, NRS (sic) and FRS. When we reviewed the study by Tickle we did not agree that it was an NRS scale, so we have reported it in this way to indicate that this was how the author described the scale. In a clinical evaluation King and Barrett113 used a numeric scale (0–10).114 Other forms of pain assessment include descriptive categories of pain (no pain, mild, moderate, severe and very severe pain).115 Most recently Seckam et al115 used a qualitative phrase ‘my wound hurt’ (not at all, a little, moderately quite a lot and very much). Collectively it’s apparent that there is a tendency use unidimensional pain assessment tools to measure pain intensity in relation to product evaluation approaches. This is likely to be perhaps because they are simple, quick, and easy to administer and are sensitive to treatment effects. Additionally, they may also be closely related to the procedural pain experienced.
3.14 Summary of evidence
The evidence highlights that the assessment of wound-related pain is complex and multidimensional. Healthcare providers must determine what the most suitable assessment tool is for their patients and in doing so consider an individual’s ability to respond to the assessment. Clinicians must determine what characteristics or dimensions of pain they are seeking to assess and what is the purpose of the assessment for the specific outcome measures they are seeking. Therefore, there is no one pain assessment tool that is appropriate for all individuals, and that ‘one size does not fit all’.
Based on the evidence reviewed we would recommend the use of a multidimensional tool in conjunction with a pain intensity tool. We acknowledge that we have not conducted a systematic review, therefore it was not possible to present a GRADE evidence to decision (EtD) framework116 which is a systematic and transparent approach to making well informed healthcare choices. Nevertheless, the recommendations for clinical practice and healthcare professionals are summarised on the best available evidence for clinical practice as well as from clinical experience and expertise. Table 7 summarises the most commonly used tools in clinical practice and a summary of recommendations for pain assessment for individuals with wound-related pain is shown in Table 8.
Table 7: Most commonly used tools in clinical practice
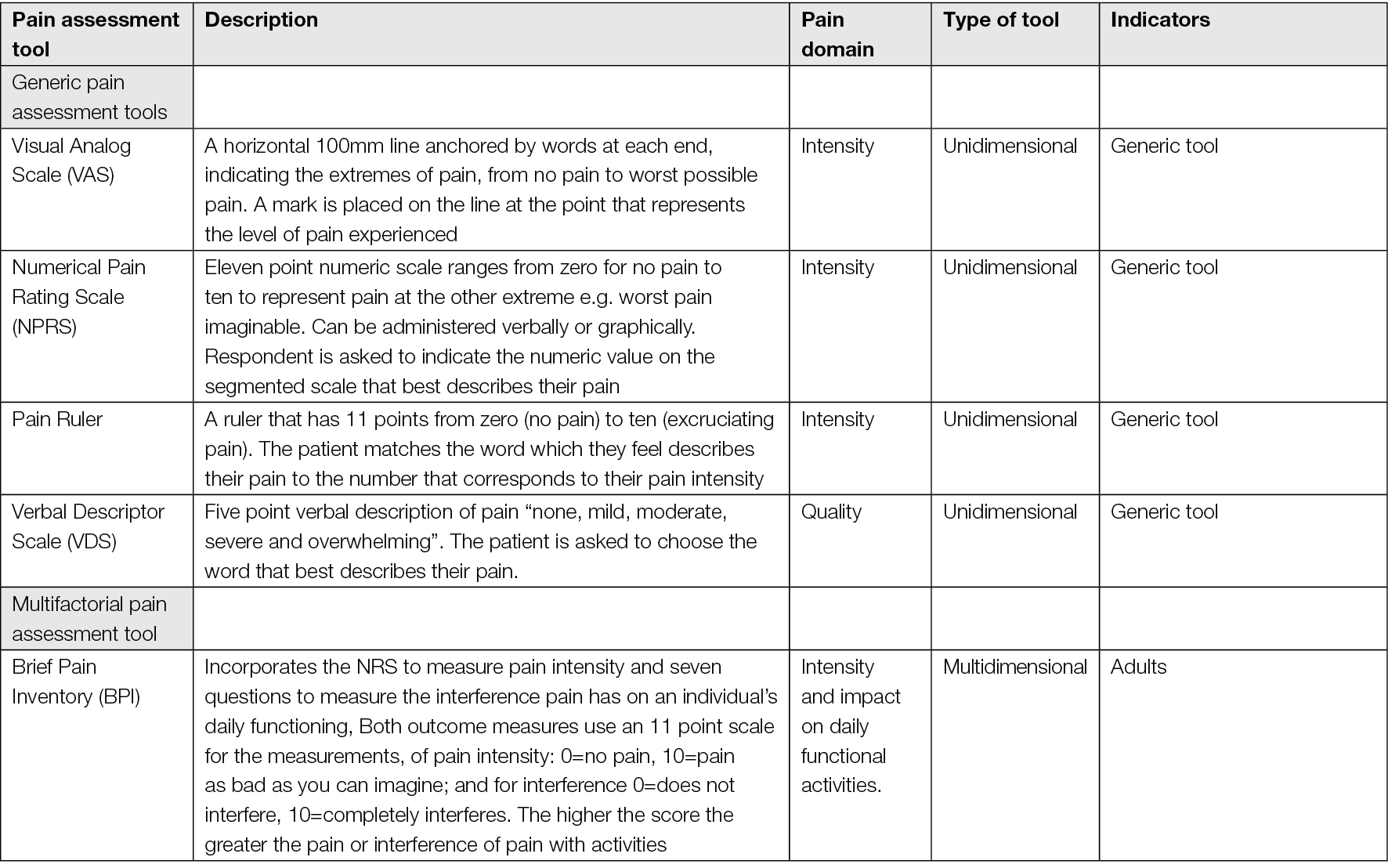
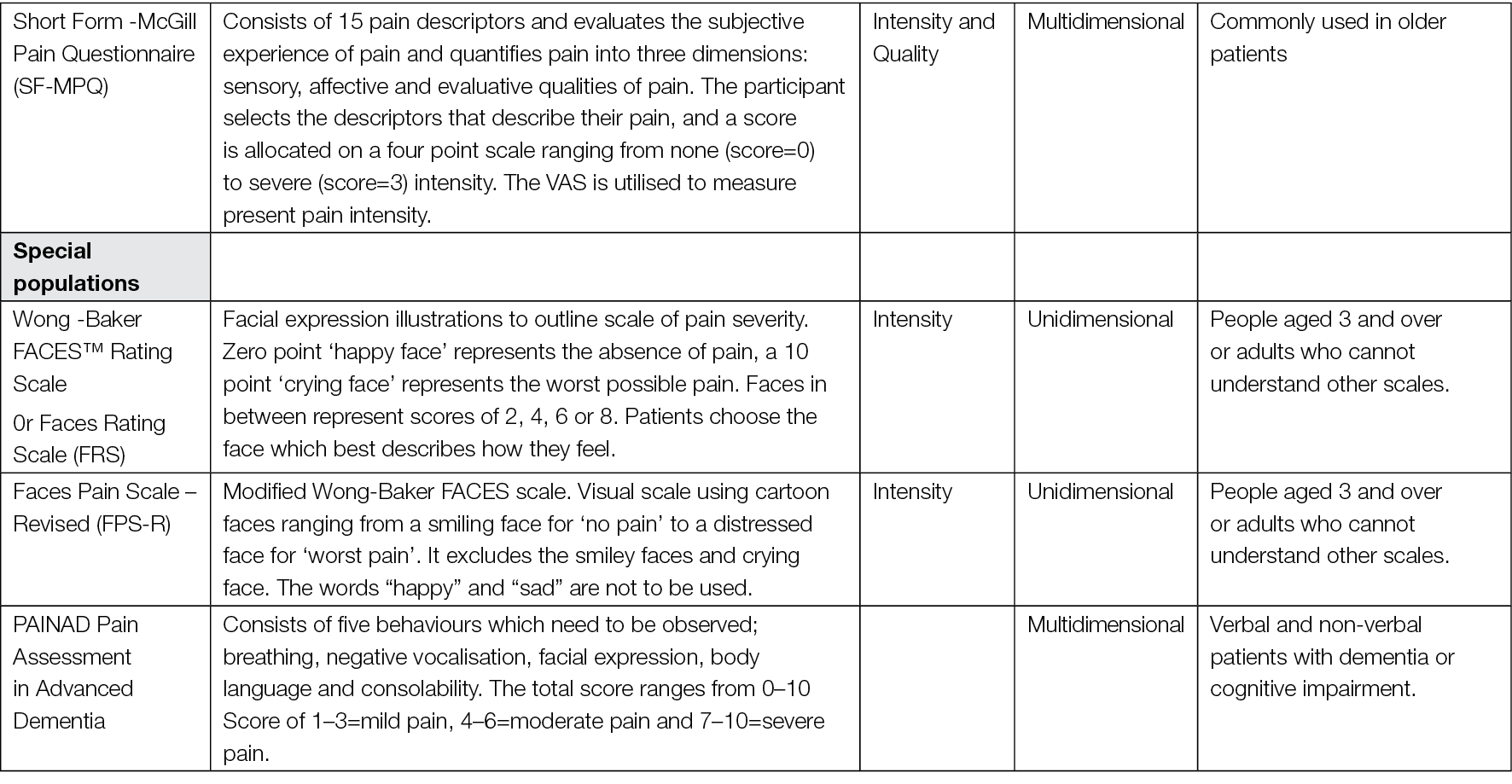
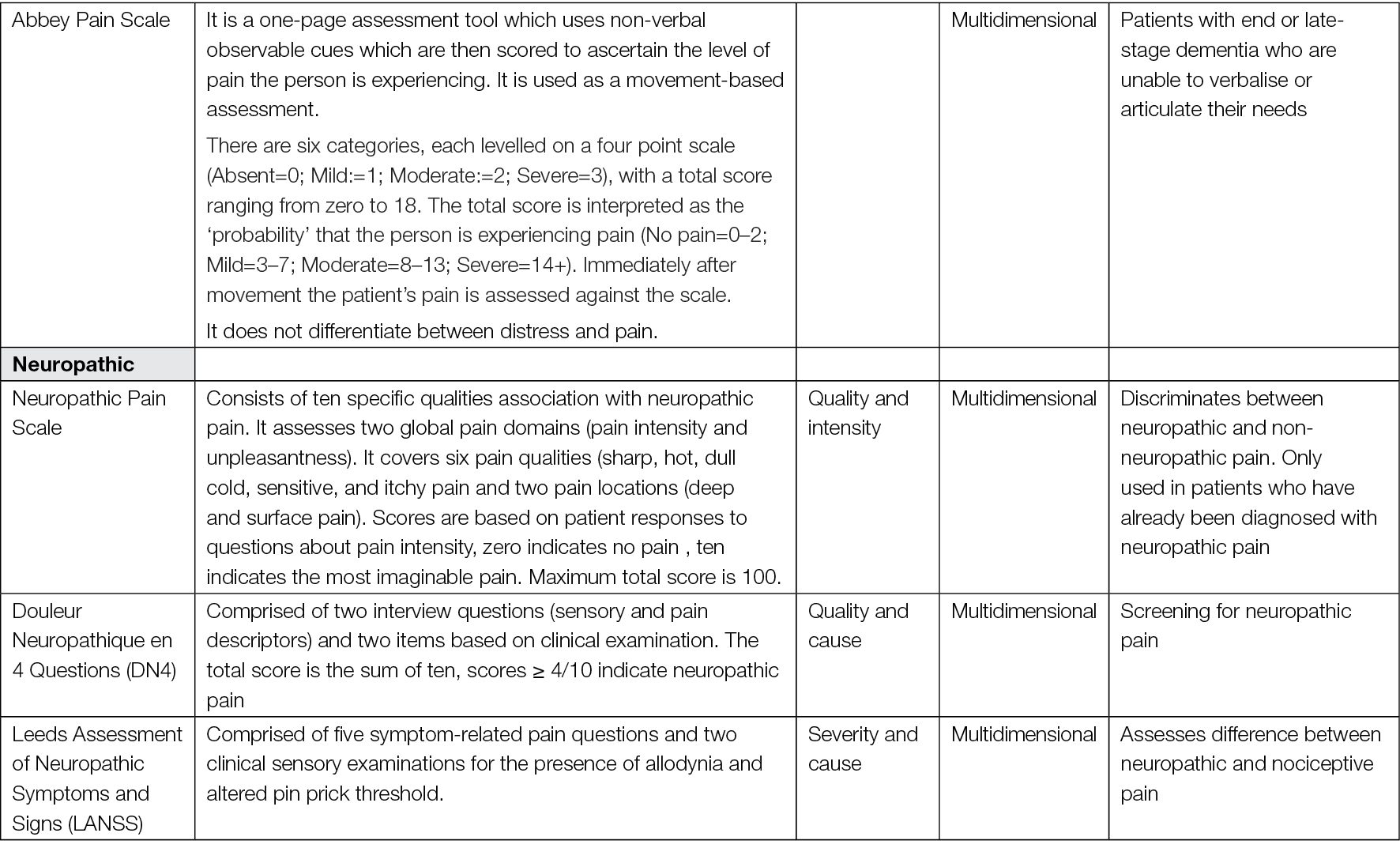
Table 8: Summary of recommendations for pain assessment for individuals with wound-related pain
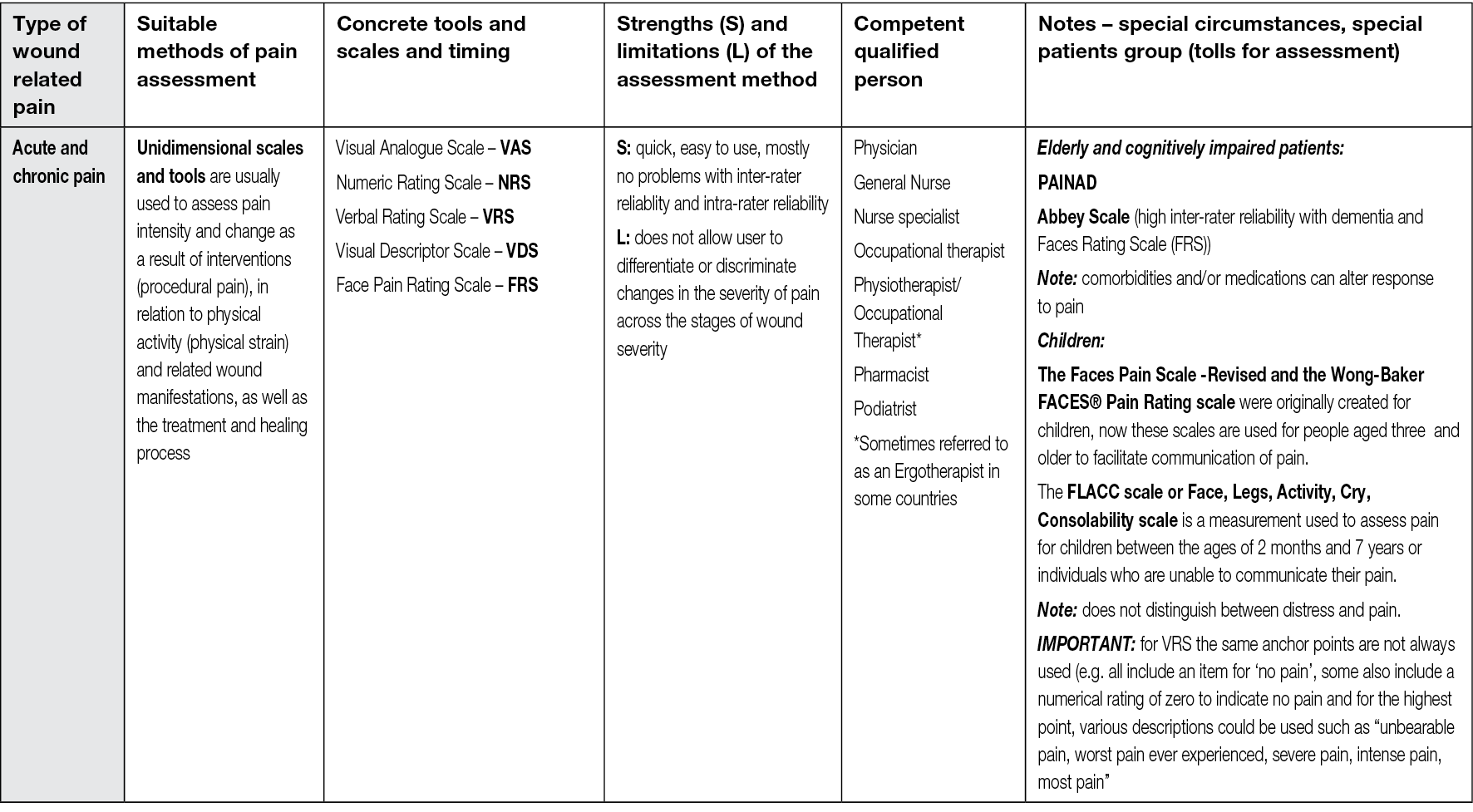

4. Physical therapies for wound-related pain management
4.1 Introduction
This chapter reviews evidence related to physical therapies for wound-related pain management and chronic wounds. It is important to note that the definition of physical therapy according to the search strategy did not limit the evidence to Physical Therapy which refers to the profession. The results are based on five articles retrieved from the L OVE platform. An additional three articles identified from the references within the reviews are also discussed. These articles examined the use of topical analgesics for management of anticipatory pain, debridement and procedural-related pain and the potential effect of negative pressure wound therapy (NPWT) in reducing inflammation and by association, pain. In keeping with the theme of ‘procedural-related’ pain, evidence associated with the use of dressings is also reviewed in this chapter. The evidence for this aspect was identified by hand-searching of the literature. A summary of recommendations from the evidence, clinical experience and expertise is provided at the end of the chapter to facilitate implementation into clinical practice.
4.2 Method
4.2.1 Search method
The search strategy aimed to find systematic reviews related to the role of Physical Therapies in the holistic management of wound-related pain. We searched the L OVE platform, which collects systematic reviews retrieved from the systematic reviews database Epistemonikos7 and allocates them to specific L OVEs and questions8. We conducted a search of L OVE for wounds and burns on 17 June 2022, and retrieved relevant systematic reviews using the filters for physical therapy and rehabilitation. There were no language, publication year or publication status restrictions.
We screened the reference lists of all eligible systematic reviews and hand-searched websites of relevant organisations/institutions and other sources.
4.2.2 Inclusion criteria
Systematic reviews of pain and chronic wounds, which discussed an intervention related to management of wound-related pain were included.
4.2.3 Exclusion criteria
Acute wounds, burns (burn injuries)
4.2.4 Selection of studies
Retrieved titles and abstracts were exported into Rayyan52 by an information specialist, Simona Slezáková. The title and abstracts were screened in duplicate and independently by two authors, Kirsti Ahmajärvi (KA) and Nicoletta Frescos (NF).The blind mode within Rayyan was kept on until both authors had completed the first screening. Subsequently, the blind mode was turned off to allow the authors to view each other’s decisions. The authors then met to resolve the disagreements and agree which results would move to the second stage of a full-text review of selected articles. Full-text screening was conducted similarly to the title and abstract screening. Following the full-text screening a list of studies for inclusion / exclusion was created. The original search yielded 185 results. Following the title and abstract screening 171 were excluded, the main reason for exclusion being the wrong outcome or population. This generated 14 articles for full text review. Nine full texts were excluded as they did not have the relevant outcome. Five reviews met the inclusion criteria and were included in the analysis (Appendix 5). Moreover, hand-searching retrieved three more articles (Appendix 6). Finally, 8 systematic reviews were included in our literature review. The screening and assessment process is described in detail in the flow diagram (Figure 9).
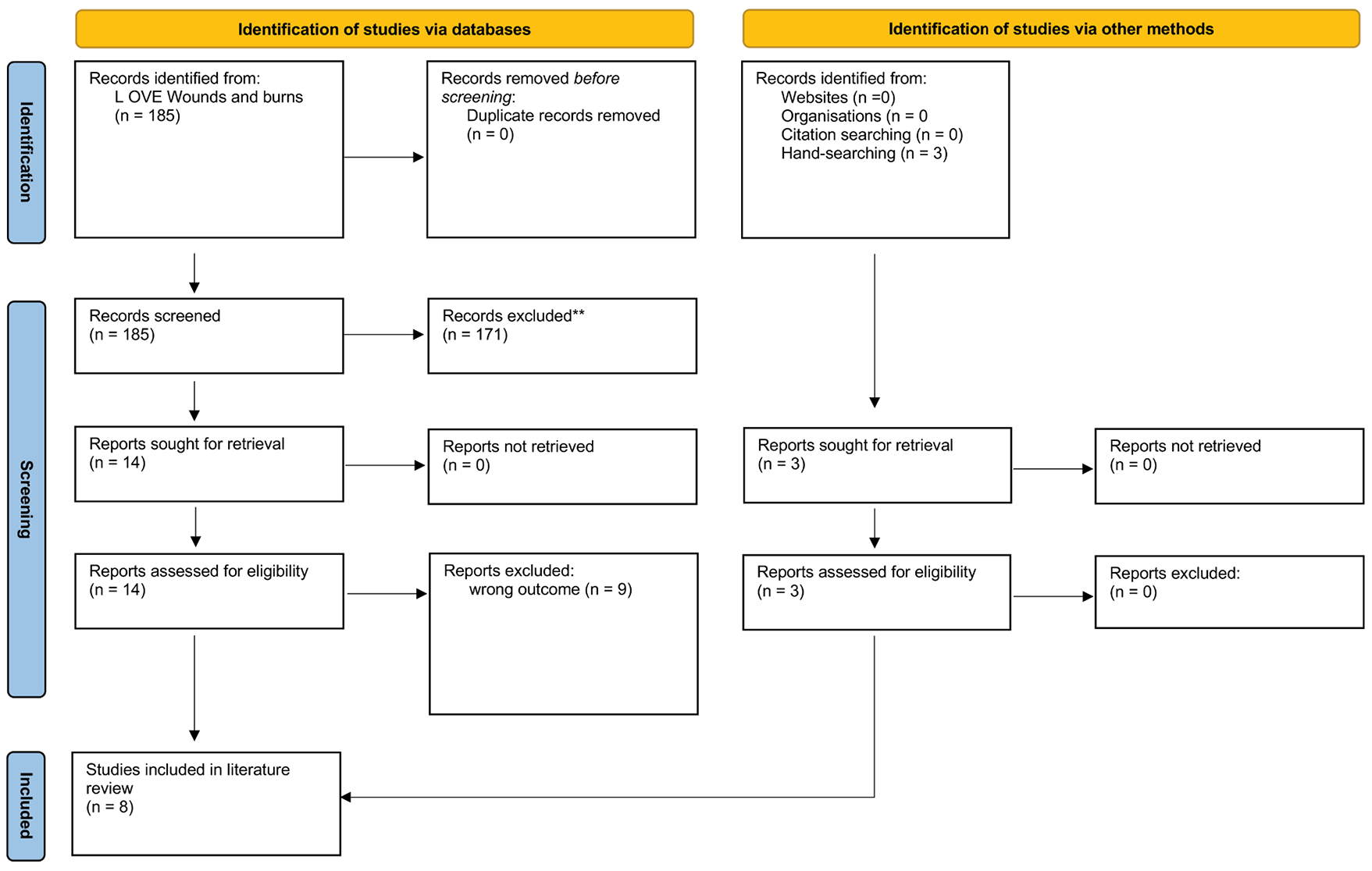
Figure 9: Flow diagram of the screening and the assessment process for physical therapies, (modified PRISMA 2020 flow diagram)
4.2.5 Data extraction
Relevant data were extracted from the included reviews by KA and NF.
4.3 Background
The World Health Organization analgesic ladder is widely used to guide the management of acute and chronic pain117 for non-specialists. This chapter does not discuss the use of drug treatments for the management of pain as this was considered to be outside the scope of this document. Our recommendation would be to consider referring the individual to a specialist when the usual non-specialist interventions have failed, or where the pain is poorly controlled, and the individual is experiencing distress.
We would also like to point out that based on the literature search methodology undertaken for this chapter the use of honey as an intervention for management of wound-related pain was not retrieved in relation to physical modalities. Instead, the evidence to support the use of honey will be examined in the Complementary and Alternative Approaches chapter, which was according to the indexing within Epistemonikos.
4.4 Results
4.4.1 Characteristics of the systematic reviews via Rayyan
Five reviews included a total of 56 studies. The date range of the include studies was 1996–2018 and the number of included articles varied in the reviews between 2–25. A total of 2492 patients were included, and the studies were conducted in the following countries: Netherlands, Ireland, Australia, Poland, United States of America, England or unspecified English-speaking countries: however not all the studies reported the geographical location. Studies included all types of the ulcers; vascular, venous, PU, DFUs etc. Exclusion criteria was acute wounds and burns, but if the study included both chronic and acute wounds it was included with the evidence on chronic wounds being examined.
4.4.2 Characteristics of the systematic reviews via hand-searching
The three additional systematic reviews retrieved by hand searching included a total of 123 articles which were published 1990–2022 and were conducted in the following countries: England, Poland, USA, Switzerland, Canada, Spain, Scotland, Australia, New Zealand, Brazil, China, Denmark, France, Sweden. Of the total number of studies which reported sample size /number of participants there were 4689 participants, with samples ranging from 1–280.
Collectively, the evidence provided data from 179 studies published between 1990–2022 with a total sample size of over 7000 patients and included at least 15 different countries.
4.5 Physical therapies
Physical therapies for management of wound-related pain include physical therapy and physical activity, careful consideration when undertaking dressing changes: such caution in the procedure itself and also using atraumatic dressings. Impregnated, medicated dressings may also be used and, of course, the use of analgesics taken before or after a procedure is also an important factor. The evidence reviewed for this chapter also indicated that there may also be a role for the use of NPWT in the management of wound-related pain. Additionally, the use of extracorporeal shock wave therapy (ESWT) is discussed as a treatment method for chronic wounds with specific reference to its use for wound debridement, as it has been reported to be less painful.
Yim et al’s118 systematic review examined the effect of physical therapy on wound healing and QoL in patients suffering from VLUs. Ten studies met the criteria for inclusion, which focused on the role of exercise on ankle joint mobility. Interventions discussed included, walking, heel-raises in standing position, tip-toe exercise, cycling, use of elastic (sic) bands (taken to mean resistance bands in this context) and use of a treadmill. Supervision by a Physical Therapist or Physical Therapy Assistant or a nurse were also considered as physical therapy according to this review.
Tools for measuring QoL included domains related to pain, for example, the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36), and the NHP. Disease specific tools were also used and included the Chronic Lower Limb Venous Insufficiency and Venous Insufficiency Epidemiologic and Economic Study Questionnaires.
Of the 10 studies included in the review only two (Davies et al 2007 and Zajkowski et al 2006) reported reduction in pain after exercise, however a key finding was that pain was the main domain affecting QoL and in turn physical exercise had a positive effect on QoL. The overall conclusion was that improvements in HRQoL were related to improvement in pain, rather than wound healing. However, it is known that the presence of pain can cause stress and anxiety which in turn can have a negative effect on wound healing (see Chapter 2: Multidimensional Nature of Pain). Therefore, the findings of the review by Yim et al118 strengthens the evidence that management of wound-related pain is important to improve patient outcomes.
Smith et al119 also investigated the effect of exercise on wound healing in patients with VLU. Smith and colleagues evaluated exercise as adjunctive or additional therapy with compression therapy. Six articles published between 2009–2017 were included. Participants were from outpatient clinics, hospitals and patients living at home. Outcomes of interest across the studies included time to heal, size and recurrence of the wound, pain, QoL, adverse events and economic aspects were also considered.
Two studies cited in the review by Smith et al119 (Meager et al (2012) and Szewczyk et al (2010)) characterised pain as a specific outcome measure. Meager et al studied the use of an exercise programme in addition to compression compared with compression therapy alone. Similarly, Szewczyk et al studied the impact of an extensive supervised exercise programme (ESEP). The studies included 32–35 participants respectively and the programmes lasted for 9–12 weeks. In the study by Meagher et al the intervention group were asked to exercise at home undertaking a minimum of 10,000 steps daily while in the Szewczyk et al study the participants were asked to walk 3km daily and additionally perform 3 times 15 sets of heel raises, foot movements or alternative foot exercises. The results from both studies showed that there was no increase in pain levels after increasing the level of daily exercise.
The 10,000 Steps programme used a VAS to assess pain and the ESEP programme used a three point pain scale where 0=no pain, 1=moderate and 2=severe pain. Smith et al119 noted that a limitation of these, and the other studies, was the lack of validated pain assessment tools with the majority of studies using self-reported measures. Overall, there was a lack of data reported to facilitate scrutiny of the results and this limits the conclusions that can be drawn.
While these studies provide evidence that pain did not increase during or after exercise, the implications for the role of physical exercise as a strategy for management of wound-related pain is less clear. Nevertheless, wound healing was a primary outcome of the studies and physical therapy has been discussed as one approach to help support healing. Equally pain was discussed as one of the major factors that can have a negative effect on an individual’s QoL. Collectively this evidence supports the idea of the multidimensional nature of pain and the need to consider the physical, social, and psychological factors that can affect the experience of pain.
4.6 Topical analgesics
Topical analgesics are commonly used when treating anticipatory pain during procedural treatments in wound care. For example, to carry out a painful dressing change or when wound debridement is required. The effectiveness of topical analgesics has also been investigated as an intervention for pain treatment.
Purcell et al55 undertook a review to examine the effectiveness of topical analgesics and local anaesthetics in the treatment of pain of patients with chronic leg ulcers. They identified a total of 406 articles of which 23 met the inclusion criteria. Many of the studies were conducted in Europe (n=20). The range of participants varied across these studies from fewer than 25 up to 835 in one study. Purcell and colleagues categorised the results into two main groups; those who had topical analgesics (n=10) and the others who had local anaesthetics (n=13).
Assessment of pain in the studies which examined the use of topical analgesics (n=10) was undertaken using a variety of methods including, numeric rating scale (NRS), VAS, visual rating scale and numeric box scale. The type of wounds included in the studies were mostly venous in origin and the intervention consisted mostly of foam dressings with ibuprofen (dose of 0.5mg/cm2). According to six studies the use of impregnated foam dressings reduced pain compared to placebo or standard care. However, five studies reported adverse events related to ibuprofen, which were mainly related to irritation of the skin, allergic reactions, bleeding, and increased pain. The use of a topical morphine gel was also investigated in three studies. Morphine gel was applied to the wound bed daily in doses of 0.5mg/cm2, 10mg and 0.5%/g though it was difficult to determine the effectiveness due to the small sample sizes.
In the studies examining the effect of local anaesthetics (specifically prilocaine and lidocaine) for management of pain related to debridement of chronic wounds the results indicated a statistically significant effect on reduction of pain. The doses used were prilocaine 2% or 5% and lidocaine 10%. However, some studies used larger doses (up to 150g lidocaine). Three of the studies investigated the toxicity levels after treatment and concluded that safe doses are 2% and 5% of lidocaine/prilocaine cream. Across the studies the average application time was 30 minutes; however, in two studies this was extended to 45 minutes or 60 minutes. Adverse events reported included irritation, burning, itching.
The results of the review by Purcell et al55 suggested that the use of a topical analgesics in the form of an impregnated ibuprofen dressing or lidocaine/prilocaine cream can reduce chronic leg ulcer pain, yet the evidence is inconsistent. Furthermore, there was a lack of sufficient data to support the use of opioid impregnated gel for topical pain management. With regards to the use of topical anaesthetics, the evidence for their use in reducing pain associated with debridement indicates that lidocaine/prilocaine gel has the strongest evidence.
Further evidence related to management of wound-related pain associated with debridement will be explored in more detail in a subsequent section.
In a recent scoping review examining the use of topical therapies in the management of pain in malignant fungating wounds (MFWs), Costa Ferreira et al6 concluded that there was a lack of evidence for the effectiveness of existing wound-related pain management strategies.
Costa Ferriera and colleagues reviewed 796 articles of which 70 studies were included for analysis. The majority of the studies were in English (88.6%) and were undertaken in the UK (n=18, 24.3%) or United States (n=16, 22.9%). Almost half of the studies (45.7%) were non-systematic reviews, one third (28.5%) were case studies and 25.8% other types of studies (controlled trials, systematic reviews, cohorts, guidelines and surveys). The sample sizes were between 1–60 patients. The population was adults over 18 years old who were from different settings, including home care, long-term care, palliative care units and hospitals.
Costa Ferreira et al identified 20 different therapies for pain management. The most commonly used interventions included wound dressings (58.6%), analgesic drugs (55.7%), topical antimicrobials (25.7%), skin barriers (15.7%), cryotherapy (5.7%) and NPWT (4.3%). Costa Ferreira et al56 grouped the therapies into two main categories: topical therapies which were applied in the wound; or in the periwound skin.
From the RCTs reviewed, positive outcomes for the management of wound-related pain were associated with the use of lidocaine/prilocaine 2.5%, morphine gel 0.2% as analgesics.
The results also showed that antimicrobials such as, metronidazole 0.8%, polyhexamethylene biguanide (PHMB) with betadine 0.1% solution, octenidine solution, honey and silver had a positive effect on reported pain. Costa Ferreira et al56 noted that a combination of topical therapies to address high levels of exudation and also to avoid adhesion of dressings to the wound bed also need to be considered as approaches to pain management.
Of the total number of articles reviewed (n=70) 26 studies reported on the use of non-adherent dressings for pain management. Of note is that all studies combined the use of dressings with other interventions for pain management, for example opioids, topical anaesthetics, and antiseptics. The use of hydrogel dressings was examined in 11/70 of the studies, with the consensus view being that these reduced pain by maintaining moisture on the wound bed. Hydrogel dressings were also combined with opioids, anaesthetics, and antiseptics in some studies. Ten studies reported the use of ‘absorbent’ dressings in combination with other products to control exudate, the view being that this strategy helped to reduce the risk of moisture-related dermatitis and consequently helped to manage pain. The use of dressings impregnated with ibuprofen as an anti-inflammatory dressing were also discussed as an option.
Like the previous review by Purcell et al,55 Costa Ferreira et al56 examined the use of topical application of opioids and topical anaesthetics to the wound bed as a strategy to manage pain. Of the 70 studies reviewed, 33 examined one or both interventions. Regarding topical anaesthetics, the use of lidocaine, prilocaine, benzocaine and tricyclic anaesthesia were mentioned but no information was provided on the formulation and dosage.
Of the studies examining the use of topical antimicrobials (n=3) the most common interventions included, metronidazole, silver sulfadiazine, nanocrystalline silver, honey, and topical antiseptics. The justification from the authors of these studies being that the main effect of using these preparations was their potential for killing micro-organisms which they said reduced the risk of wound infection. Pain was included as an outcome measure in the studies. While these studies were not examining the management of wound-related pain per se it is recognised that pain, and/or increased pain is associated with the presence of a wound infection120 (therefore clinicians need to determine whether the presence of a wound infection is the underlying cause of the wound-related pain to establish the most appropriate intervention(s).
With regards to periwound management the use of topical therapies (such as zinc oxide, silicone, dimethicone, petrolatum, acrylate, cyanoacrylate, hydrocolloid and vitamin-rich ointment [A and D]) was addressed in 11 studies. Overall, it was suggested these have a positive effect on pain, however there was a lack of information further regarding assessment of pain and no data were provided to support this claim. Whilst the focus of the current document was wound-related pain specifically, periwound damage can contribute to pain and discomfort 121 therefore strategies to address periwound pain must also be taken into consideration in the wider context of ‘wound-related pain’.
A major limitation of the studies in the review by Costa Ferreira et al56 was the variation in pain assessment tools used (Visual analogical scale, Numeric verbal scale, McGill’s questionnaire and assessment by categories). This makes it difficult to determine the impact of interventions for the management of wound-related pain. Yet pain is one of the most significant symptoms affecting QoL among people suffering from MFWs, therefore to determine the clinical effectiveness of different interventions for MFW with regards to wound-related pain specifically there is also a need for a more standardised approach to pain assessment: One cannot be viewed in isolation of the other.
4.7 Debridement
Wound-related pain is commonly associated with debridement procedures122,123 which encompass; surgical and sharp techniques as well as non-excisional methods such as, scrubbing, washing, enzymatic, hydro surgery, maggot therapy, high-pressure irrigation, and use of ultrasound. Several debridement options may be associated with what is referred to as ‘procedural-related pain’, where the wound may be painful just for the period the procedure is being undertaken, and painless afterwards. For the purposes of this document, it was felt to be important to address procedural-related pain in the wider context of wound-related pain.
Ramundo and Gray124 reviewed literature to study ultrasonic mist debridement for different aetiologies of wounds including venous, ischaemic, neuropathic, trauma origin and hard-to-heal ulcers. Ramundo and Gray identified only two studies which provided a total of 203 participants. Ramundo and Gray found no statistical difference in the wound healing between the groups treated with conventional methods and low-level ultrasonic mist therapy. Pain was treated with local anaesthetics when reported by patients, however pain was not a primary or secondary outcome of the studies.
Herberger et al125 investigated the use of ultrasound-assisted debridement (UAD) versus surgical debridement (curettage), in an RCT (n=67). Herberger and colleagues used a VAS scale to assess pain before, during and after the treatment. Pain was considered as a main outcome measure alongside patient benefit and tolerability, and wound healing. Herberger et al used a topical local anaesthetic cream (containing lidocaine and prilocaine), applied to the wound bed 60 minutes before the procedure, and recorded whether patients also required the use of additional oral analgesia. The results showed that there was no significant increase in pain in either group, however in the intervention group, which had UAD, the baseline data shows that patients had higher pain scores pre-procedure, yet they did not experience more pain than the patients receiving regular treatment post-procedure. There were also no significant differences between the groups in efficacy or tolerability of the techniques.
Chang et al126 investigated the use of low-frequency ultrasound (LFU) as a debridement method for chronic wounds and found that less pain was reported with this technique. Chang and colleagues discussed that ultrasound is a method which uses acoustic energy to remove dead tissue in the wound bed, thereby promoting wound healing. Furthermore, they discussed that the proposed mechanism of actions of ultrasound are both mechanical and thermal which can have a positive effect at a cellular level.126 Low-hertz Ultrasound (20–60kHz) has been found to reduce exudate and has a positive effect on the presence of biofilm on the wound.127 Furthermore an early study by Schoenenbach and Song,128 cited by Ramundo and Gray124 reported that ultrasound decreased the level of Pseudomonas in the wound bed of patients with burn wounds. The studies in the review by Chang and colleagues examined the use of LFU in patients with PUs, DFUs, arterial and venous ulcers, surgical and/or traumatic ulcers and burn wounds.126
Chang et al126 reviewed 25 studies providing a total of 850 participants. Studies were heterogenous in design and no meta-analyses were found. The majority of the studies evaluated the use of MIST® Therapy (n=19), which is the most often used LFU therapy. In seven studies there was a reported reduction in wound pain when using LFU. Compared with other standard debridement techniques there were no differences between the modalities with regards to removal of fibrin and necrosis, and all showed positive effects on granulation of tissue formation and QoL.
It is acknowledged that the use of UAD is not indicated for the management of wound-related pain, however the current document considers pain to be a central feature of QoL measures, therefore these reviews support the importance of considering the potential consequences of procedural-related pain when selecting the most appropriate debridement method.
4.8 Negative pressure wound therapy (NPWT)
NPWT has a number of reported effects including reduction of wound exudate and inflammation, it also enhances angiogenesis and epithelialization thereby reducing wound healing time.129 However, NPWT can be associated with pain related to the system and the dressing (foam/filler) used and whether this dressing adheres to the wound bed.130 As discussed in the chapter examining the multidimensional nature of pain this can have a significant impact on an individual’s well-being, which brings to the fore the importance of considering psychological aspects in the wider context of wound-related pain.
Upton and Andrews130 reviewed the use of NPWT examining the outcomes of pain and trauma specifically. The authors included 30 studies (n=152 participants) and found that gauze-based filling was less painful than foam as pain was associated with adherence of the foam into the wound bed. In a previous study by Upton et al131 which included 43 patients in an out-patient setting the authors identified a significant reduction in pain when using atraumatic dressings compared to conventional dressings. In a multicentre study Teot et al132 investigated 66 patients receiving 1145 days NPWT treatment combined with a non-adhesive, non-occlusive dressing. Pain was assessed during each treatment procedure and at two consecutive dressing changes, however the pain assessment tool used was not reported. Upton and Andrews discussed that if there was less trauma associated with the NPWT dressing change the procedure was less painful. The same authors reported that pain related to NPWT also reduced over time, however this was not a statistically significant finding. Furthermore, the authors discussed that because NPWT has a positive influence on the time to wound healing this is turn has a positive impact on the experience of pain.
The systematic review by Costa Ferreira et al56 examined the use of NPWT in the management of MFW. However, there were only three studies providing a total of six patients. As NPWT is contraindicated in patients with MFW and the strength of evidence for this population is low we were unable to make any recommendations based on this systematic review.
4.9 Extracorporeal shock wave therapy (ESWT)
ESWT has been used in the treatment of urinary stones however its use has also been reported in the treatment of chronic wounds.133,134 ESWT is biphasic, high-energy acoustic pulses which create transient pressure waves in three-dimensional space, and it rapidly rises pressure which is applied to tissue without causing any damage.135 The effect of the device is to produce low energy pulses which can penetrate the skin up to a 3 cm depth.
Dymarek et al136 studied the efficacy of ESWT in wound healing. The authors discussed that ESWT has an anti-inflammatory effect, enhancing tissue granulation, improving blood flow perfusion, angiogenesis and re-epithelialization. The authors also discussed that the therapy reduces necrotic tissue and time to complete wound closure. Dymarek and colleagues identified 393 articles published between 2000–2013 of which 13 studies met the criteria giving a total sample size of 919.
Overall, the results showed that ESWT was considered a safe, mostly painless non-invasive treatment method, however pain was self-reported, and no pain assessment tools or scores are mentioned. The included studies indicated that ESWT has been used as an adjunctive treatment for different aetiologies of wounds including VLUs, DFUs, arterial insufficiency ulcers, PUs, acute burns wounds, surgical wounds and post-traumatic wounds. According to the review no local anaesthesia or analgesia were needed while ESWT was being carried out. However, some adverse events were reported including pain and bleeding. The primary outcome in the studies reviewed was wound healing rather than wound-related pain specifically, however as the mechanism of action of the therapy is mostly anti-inflammatory it was considered applicable to the topic.
4.10 Procedural-related pain: role of dressings
Additional sources of evidence that were reviewed included articles provided by the companies sponsoring this document.
A total of 62 references were provided by three companies, of these 55 were available as full text. The full-text articles were reviewed by Alisha Oropallo and Samantha Holloway independently. The criteria for inclusion were that the article had to discuss wound-related pain and focused on chronic wounds (i.e., PUs, leg ulcers, DFUs or MFWs). None of the articles met the criteria for inclusion as the studies related to acute wounds, burns, orthopaedics and some were animal studies. However, 12 articles were identified as providing supporting information for a number of important aspects of the assessment and management of wound-related pain. These included reported use of specific dressings (n=9) and the use of a topical steroid (in crushed tablet form) for the management of peristomal pyoderma gangrenosum (n=1). One review and one experimental study explored the pathophysiology of pain to examine the role of toll-like receptors (TLRs) and toxic by-products of bacterial lysis. A summary of the main characteristics of these articles are included as supplementary information in Appendix 7.
In relation to this chapter which examines physical therapies for pain management, including the impact of procedural-related pain, there is evidence that highlights the impact of dressing adhesion on pain intensity137 which supports the need for choosing dressings that will minimise pain on removal138. There are also a series of articles examining the role of polymeric membrane dressings (PMD) and the effect on pain associated with antinociceptive actions, modulation of inflammation, and mechanical and thermal hyperalgesia.139 The ability to control oedema and by association, pain, has been evidenced in several published articles.140,141 Hegarty and Wong114 examined the use of a PMD in 23 patients with a radiotherapy-induced skin reaction. Patients reported positive outcomes in relation to pain, exudate control and comfort. In addition, an RCT conducted on partial thickness burns and split thickness skin grafts,142 demonstrated a statistically significant reduction in wound pain (p<0.01) and increases in patient comfort (p<0.01) when compared to the standard of care.
Several studies examined the role of foam dressings in patients with leg ulcers and PUs and reported positive outcomes with regard to no pain being experienced whilst the dressing was in situ or at dressing change/removal.143,115,113,144
The case series examining the use of crushed oral prednisolone tablet mixed with Stomahesive Protective Powder for the management of pain associated with peristomal pyoderma gangrenosum145 presents a novel use of a medication to treat a relatively rare presentation*.
*Note: Inclusion of this evidence in this chapter does not infer any recommendation as it is an off-licence use but it does highlight that in some circumstances, particularly for unusual wounds more research on other potential interventions is needed.
4.11 Summary of evidence
Evidence to support the role of physical therapies to manage wound-related pain incorporates physical exercise, as well as the importance of considering anticipatory pain where topical analgesics may be useful, and procedural-related pain (associated with wound debridement and dressings changes) where other approaches may need to be considered.
Regarding the role of physical exercise and wound-related pain the topic has been studied mostly in individuals with VLU. Furthermore, the primary outcomes of the evidence reviewed was wound healing and/or QoL rather than wound-related pain management specifically. Nevertheless, pain was considered as a secondary outcome or as an important category of the QoL measurement tools. According to the available evidence, there is only low-quality support for the use of physical exercise as an approach to the management of wound-related pain. Although an important finding was that physical therapy did not increase pain during or after exercise when patients were asked to increase their level of daily activity. Therefore, a recommendation would be to encourage individuals with VLU to exercise, particularly as venous insufficiency is associated with oedema, which in turn can cause discomfort (heaviness in the legs) and pain.
Some of the evidence reviewed highlighted the need for clinicians to consider procedural-related pain, particularly in relation to the use of debridement. Wound-related pain may occur during debridement procedures and can be treated systemically using oral analgesics, as well as the use of topical analgesics and local anaesthetics both during and after a debridement procedure or when dressing changes are painful. According to the systematic reviews of Purcell et al55 and Costa Ferreira et al56 there was a significant reduction in procedural pain (dressing changes and debridement) when using dressings with ibuprofen and with the use of prilocaine/lidocaine as local anaesthetics. Therefore, these products might have also had a positive effect in the treatment of chronic wound-related pain, however, evidence is still scarce and inconsistent.
There is a need for methodologically high-quality investigations focusing on pain management in chronic wounds and pain assessment. As part of this further research, information on the setting, clinically relevant outcomes related to pain and larger sample sizes would enhance the strength of the evidence. Based on the existing evidence, we could conclude that there is evidence to support the use of ibuprofen impregnated foam dressings and local anaesthetics in reducing wound-related pain regarding procedural pain related to debridement and dressing changes.
In relation to the management of exudate there were inferences from the evidence that maintaining moisture balance is an important consideration for dressing choice as maceration could exacerbate the experience of pain as could the presence of peri-wound dermatitis. Similarly, the evidence reviewed highlights the importance of recognising and treating wound infection promptly, as pain is both a potential sign of infection and the experience of pain can be worsened by the presence of a wound infection. However, one of the challenges of drawing any specific conclusions is that many of the studies did not include pain management as primary outcome, pain was considered as one of the symptoms in the infected wounds.
The evidence to support LFU suggests that it may be useful debridement technique. More specifically neither technique led to an increase in the reported level of pain and from the patients’ perspective the therapy was tolerable. Our recommendation is not that UAD and LFU should be considered as a treatment for pain, but in terms of procedural-related pain, and by association, wound-related pain this approach could be utilised by appropriately trained clinicians.
ESWT has been used as debridement method in several studies, one of the findings was that no additional pain treatment was required during the procedure. Additionally, the therapy has a positive effect on wound healing and has anti-inflammatory effects which the evidence suggests improves blood flow perfusion and angiogenesis ,as well as helping to reduce the presence of necrotic tissue. Indirectly it can be seen how these effects could impact on wound-related pain.
Evidence for the management of MFW wounds indicated that positive results in the treatment of pain was observed with the use of lidocaine/prilocaine 2.5% and morphine gel 0.2% as analgesics. In relation to antimicrobials and antiseptics the research showed that metronidazole 0.8%, polyhexamethylene biguanide (PHMB) with betadine 0.1% solution, octenidine solution, honey and silver have been used. Also, the use of non-adherent dressings covered with ibuprofen or dressings with opioids, had positive results in the studies of the effect in pain management locally, though further studies were required on different types of opioids. Topical therapies aimed at non-traumatic dressing changes and avoiding microtrauma if the dressing had adhered to the wound bed were discussed. Also, a combination of topical therapies used to reduce exudation and adhesion to wound bed in dressing changes were considered as pain management for this particular group of patients.
We acknowledge that we have not conducted a systematic review, therefore it was not possible to present a GRADE EtD framework116 which is a systematic and transparent approach to making well informed healthcare choices.116 Nevertheless, the recommendations are summarised from the best available evidence for clinical practice, as well as from clinical experience and expertise.
4.12 Summary of recommendations
A summary of recommendations for this topic is provided in Table 9.
Table 9: Summary of recommendations for physical therapies for individuals with wound-related wound pain
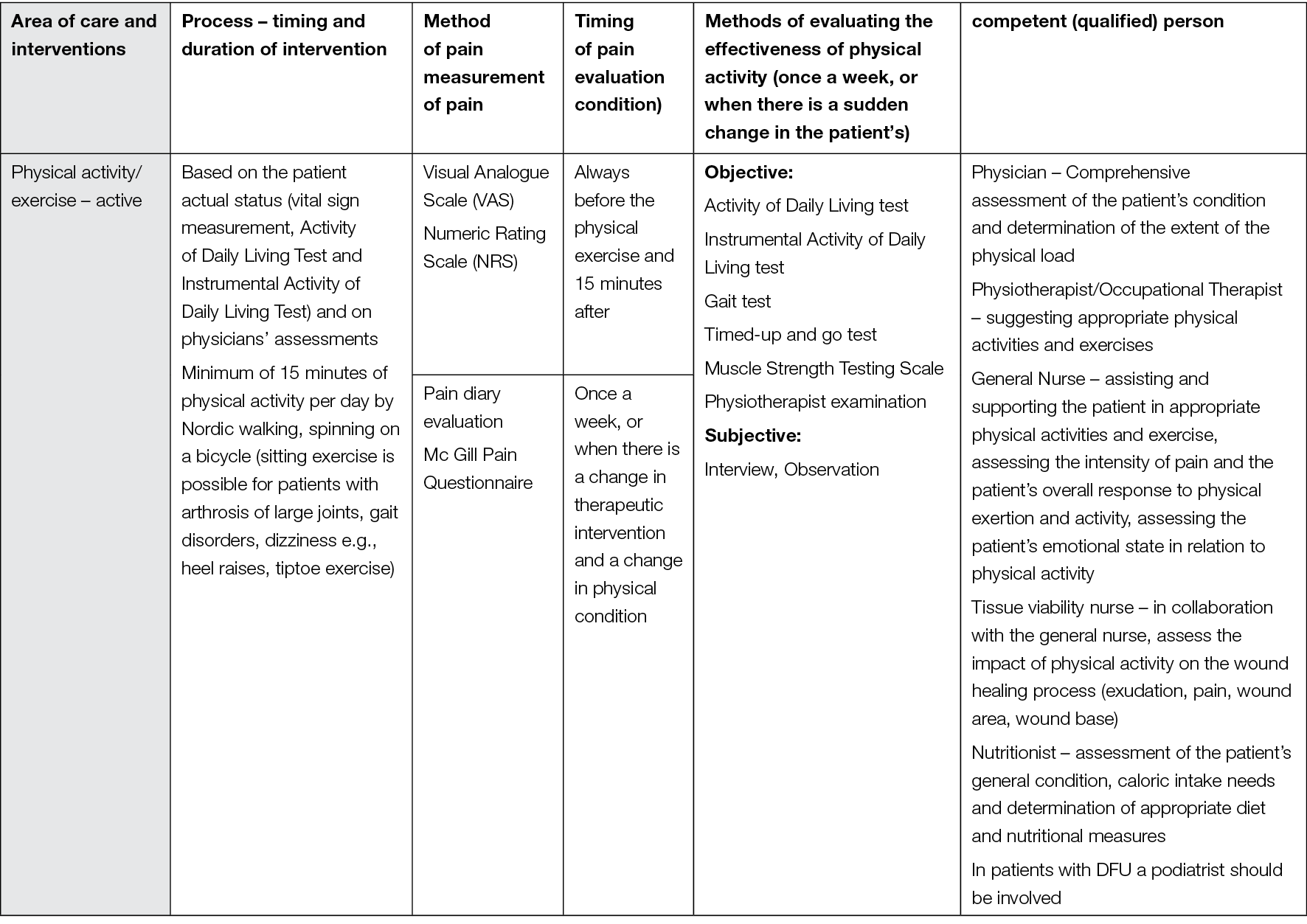

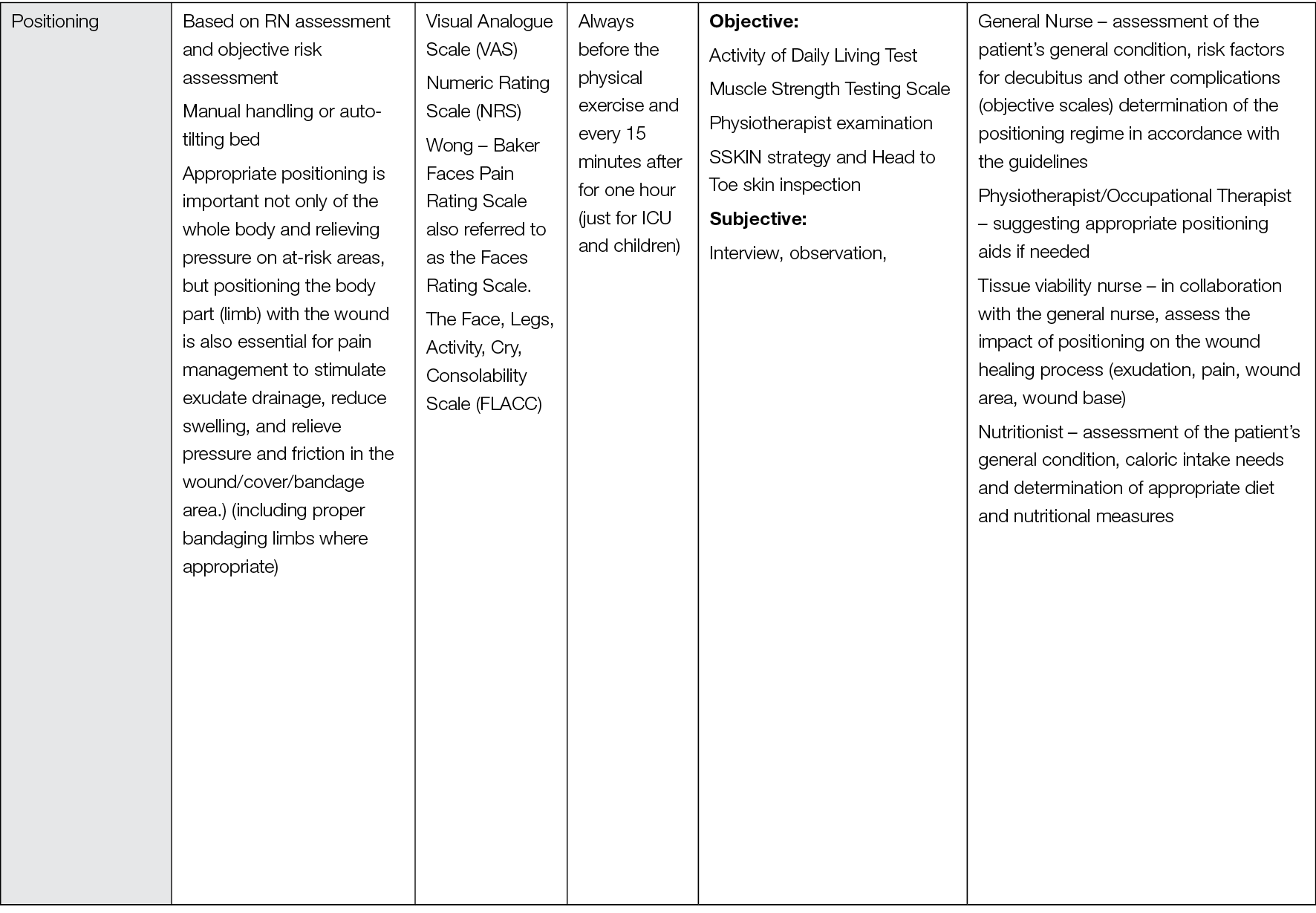
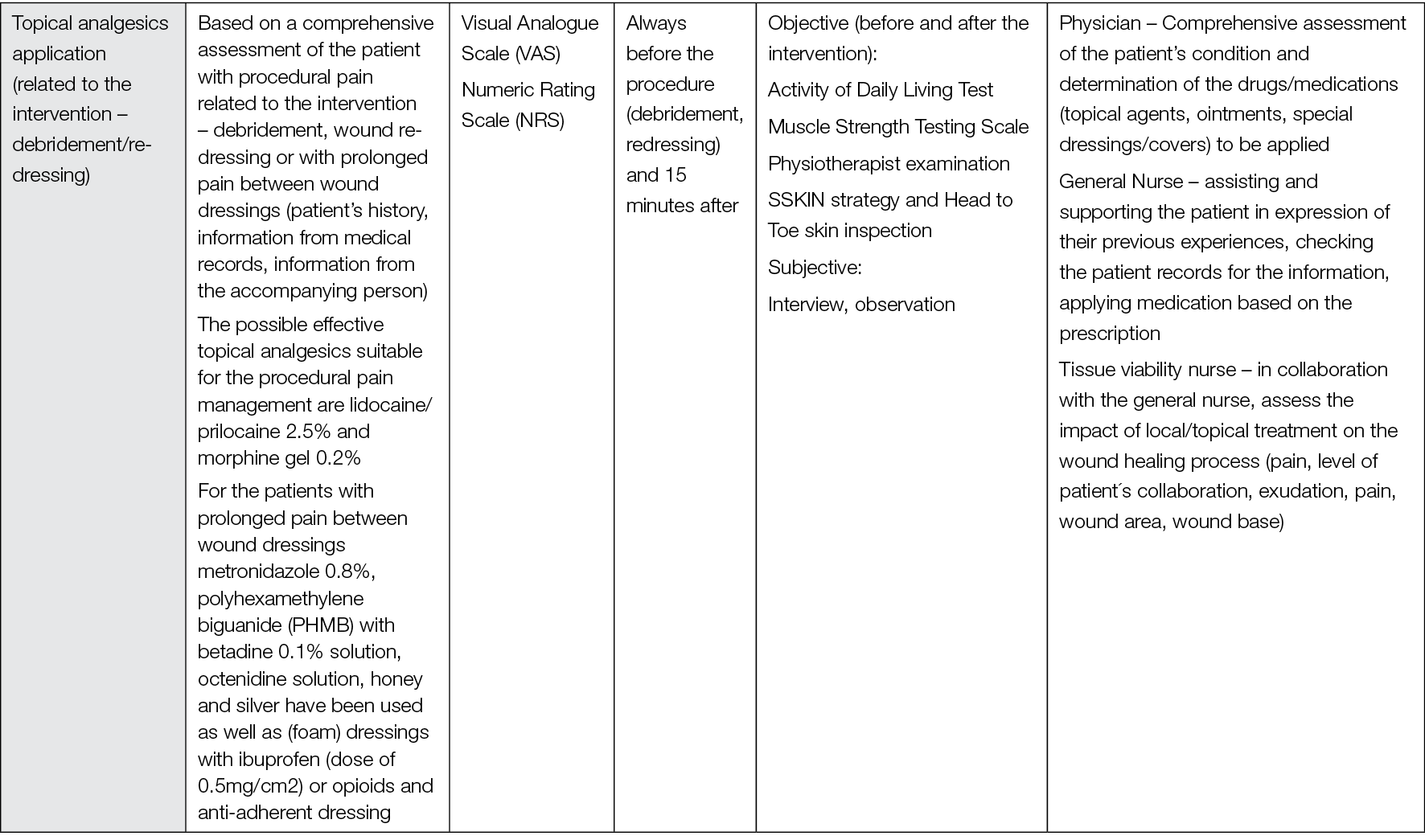
5. Role of patient education for wound-related pain
5.1 Introduction
This chapter reviews evidence related to the role of patient education for wound-related pain management and chronic wounds. The results are based on five systematic reviews, supplemented by seven individual studies identified from the reviews. A summary of recommendations from the evidence, clinical experience and expertise is provided at the end of the chapter to facilitate implementation into clinical practice.
5.2 Method
5.2.1 Search method
The search strategy aimed to find systematic reviews related to the role of patient education in the holistic management of wound related pain. We searched the L OVE platform, which collects systematic reviews retrieved from the systematic reviews database Epistemonikos7 and allocates them to specific L OVEs and questions.8 We conducted a search in L OVE Wounds and burns on 17 June 2022 and retrieved relevant systematic reviews using the filter for ‘behavioural’ interventions. There were no language, publication year or publication status restrictions.
We screened the reference lists of all eligible systematic reviews and hand searched websites of relevant organisations and institutions.
5.2.2 Inclusion criteria
Systematic reviews of pain and chronic wounds which discussed an intervention related to pain and patient education.
5.2.3 Exclusion criteria
Acute wounds, burns (burn injuries)
5.2.4 Selection of studies
Retrieved titles and abstracts were exported into Rayyan 52 by an information specialist (Simona Slezáková). The title and abstracts were screened in duplicate and independently by two authors (Andrea Pokorná, Samantha Holloway). The blind mode within Rayyan was kept on until both authors had completed the first screening. Subsequently the blind mode was turned off to allow the authors to view each other’s decisions. The authors then met to resolve the disagreements and agree which results would move to the second stage of full-text review of selected articles. Full text-screening was conducted similarly to the title and abstract screening. Following the full-text screening a list of studies for inclusion / exclusion was created.
The original search yielded 112 results. Following the title and abstract screening 96 were excluded, the main reason for exclusion being that they were acute wounds (burns, surgical). This generated 16 articles for full text review, from which we screened 15, as one full text was not available. Ten full texts were excluded as they did not have the relevant outcome or population. Of the remaining number, five articles met the inclusion criteria and were included in the analysis. From these five systematic reviews, seven individual studies were identified and included as part of the analyses (Appendices 8 and 9 respectively). The screening and the assessment process is described in detail in flow diagram (Figure 10).
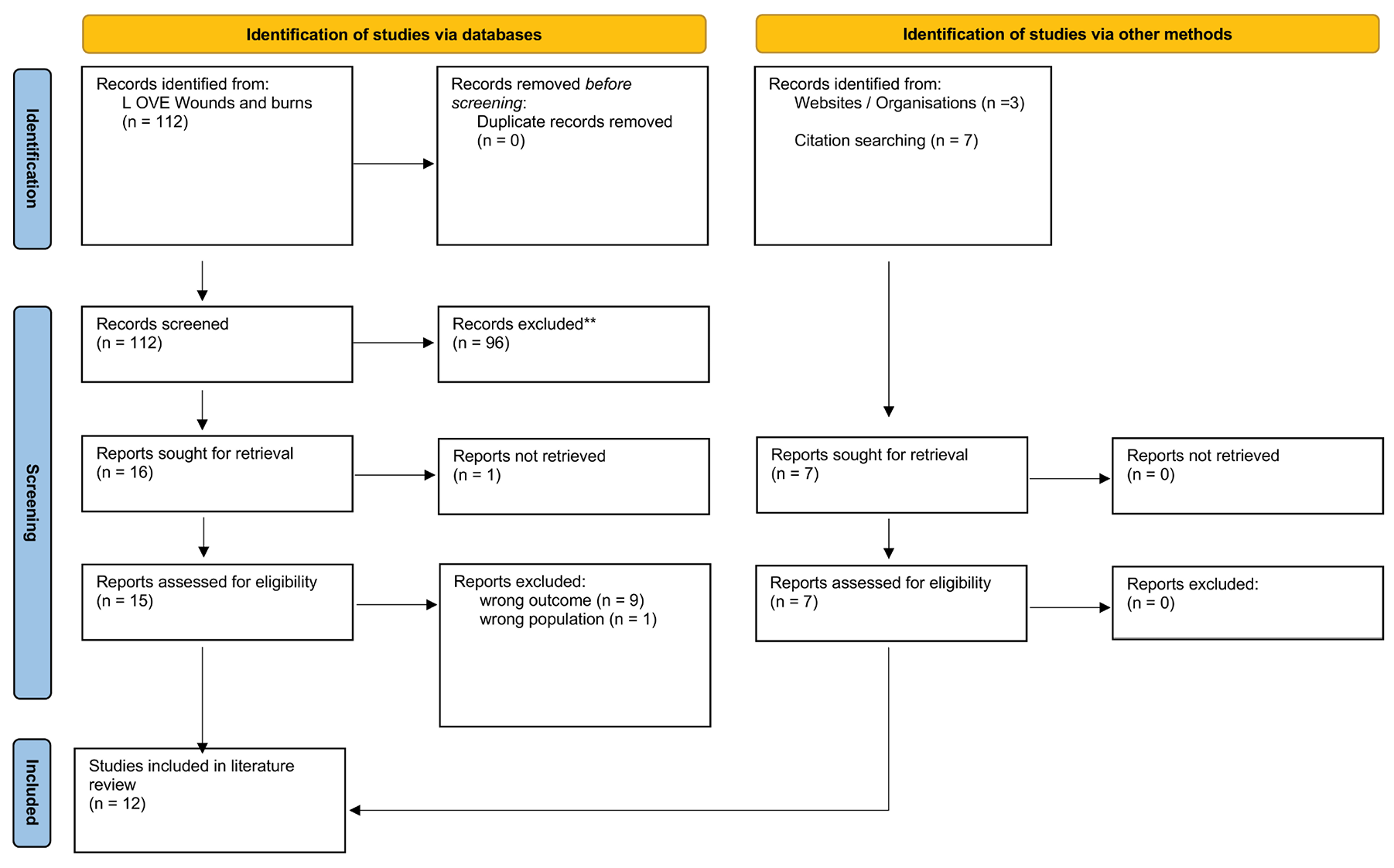
Figure 10: Flow diagram of the screening and the assessment process for role of patient education (modified PRISMA 2020 flow diagram)
5.2.5 Data extraction
Relevant data were extracted from the included reviews by Samantha Holloway.
5.3 Results
5.3.1 Characteristics of the systematic reviews
The five systematic reviews included a total of 66 studies. The number of studies included ranged from three to 31 and the date range for the database search was from 1995–2021 across all the reviews. The total sample size derived from the reviews was 10,499 patients and 144 health/social care professionals. One study146 did not provide clear information on the number of participants in the seven studies each reviewed. The studies included in the reviews were conducted predominantly in the UK, USA and Australia, with fewer in Sweden, Germany, New Zealand, Brazil, Canada, Denmark, Netherlands, Iran, Morocco, Switzerland, China, Ireland, France, India and South Korea. One study147 did not collate the information by geographical location. Three of the reviews146,147,148 focused on participants with leg ulcers (venous, chronic), one review examined all types of chronic wounds (DFU, VLU, PU)149 and one investigated PUs.150 The aims of the reviews were heterogenous, so it was not possible to pool the data across the evidence.
5.3.2 Leg ulcers
Two studies147,148 examined reasons or determinants of non-adherence to prescribed compression therapy. Van Hecke et al147 identified that pain, discomfort and a lack of valid lifestyle advice by healthcare professionals (including conflicting advice, no specific advice or impossibility of instructions) were identified as primary reasons for non-adherence. Van Hecke and colleagues concluded that a pain management programme was recommended, although no further information was provided on what such a programme might include. The BPS151 produced guidelines for pain management programmes (PMPs), this is currently undergoing a review and update. Both Van Hecke et al147 and Weller et al148 also noted that communication with the patient’s GP is required to ensure provision of analgesia. Importantly, and in relation to the use of compression therapy specifically, Van Hecke et al and Weller et al highlighted that it’s important for nurses (sic) to inform the patient that their pain levels may increase during the first few weeks of therapy, therefore it may be helpful to take regular analgesia. Provision of ‘coping instructions’ was mentioned but not elaborated on.
Weller et al148 reviewed the benefits and harms of interventions to help people adhere to compression therapy for VLU. One of the outcomes of the review included pain. Of the three studies cited, one (Edwards et al, 2009) examined the effectiveness of a community nursing intervention on QoL and wound healing in patients with chronic leg ulcers. The intervention included attendance at a weekly leg club with peer support, goal setting and social interaction plus standard care which was compared to standard care alone. Pain was also one of the secondary outcomes in the study and was assessed using the RAND instrument and SF-36 at 12 weeks and the Medical Outcomes Study Pain Measure at 24 weeks (on a 100-point continuous scale) (Box 3). The data for the 24-week follow-up showed that there may be a small decrease in pain intensity in the participants attending the Leg Club compared with the home visit care group (overall total pain score, Z=2.71, p=0.003). The Leg Club referred to in the study is based on the Lindsay Leg Club Model (LLCM)152 which is said to provide an environment where members (sic) can access education, advice and information, however Edwards et al’s (2009) study does not mention providing education or advice specifically.
The finding that a LLCM may have a positive impact on pain is supported in a review by Liberato et al146 who examined nursing interventions used for the management of pain in people with venous ulcers. Liberato and colleagues reviewed an earlier study by Edwards et al (2005) which was an RCT to determine the effectiveness of a community nursing intervention (a Leg Club) on pain and healing. Edwards et al reported significant improvements in levels of pain and ulcer healing in the intervention group receiving the ‘new model of care’. Similarly, the study undertaken in 2005 (Edwards et al. 2005) fails to mention whether specific guidance or advice was provided. More recently Gethin et al149 (undertook a review of evidence for person-centred care in chronic wound care. One of the themes that emerged was Patient Education and as part of this Gethin and colleagues149 discussed the later study by Edwards et al (2009) arguing that it supports the positive impact that the LLCM of care can have on patient education and reduction of pain.
Taken together these three reviews suggest that provision of care based on the LLCM can have a positive impact on pain, however whether this is related to the provision of patient education and advice in a Leg Club specifically is not clear and would require further exploration.
Box 3: References for evaluation instruments for QoL and pain measurement
|
SF-36 Brazier, J.E., Harper, N.M., Jones, A., O’Cathain, K.J., Thomas, T., Usherwood, T. & Westlake, L. (1992). Validating the SF-36 health questionnaire: A new outcome measure for primary care. BMJ, 305:160 Also available here: https://nexusipe.org/advancing/assessment-evaluation/short-form-sf-36-health-survey Medical Outcomes Study https://jamanetwork.com/journals/jama/article-abstract/378368 |
Gethin et al149 included a study by Kelechi et al (2014) in their systematic review. Kelechi et al reported on the effect of a nurse-directed intervention to reduce pain and improve behavioural and physical outcomes in patients with critically colonised/infected chronic leg ulcers (n=21). The intervention, Motivational enhancement and conditioning activity for leg function (MECALF) was compared to conditioning activities for lower leg function (CALF) alone. Outcomes included, pain, motivation, self-efficacy, physical activity, leg strength, and range of motion. The intervention was a six week motivational enhancement programme, including patient education, and a conditioning activity for leg function, plus two additional visits in weeks 6–8 without active motivational enhancement. The control group completed conditioning activities along with a handout at baseline and weekly visits. The results showed that overall pain was statistically significantly reduced (p=0.046) in both groups of patients with painful critically colonised/infected leg ulcers measured at week 8; two weeks after the study period. The CALF group experienced a slightly greater reduction in pain intensity than the MECALF group which suggests that exercise activities supported by written information and regular follow-up is an effective strategy with no requirement for additional motivational approaches. However, this was a small study (n=21), therefore it is difficult to generalise the findings too widely.
Gethin et al’s149 review also examined research by Tulleners et al (2019) who studied the impact of a new transdisciplinary specialist service supplemented with telehealth consultations offered to 29 patients with VLUs. Tulleners and colleagues examined patient experience and outcomes such as wound healing and QoL, including self-reported pain scores on a scale of 0–10.90 All participants received a tailored dressing plan upon completion of their appointment, with directions on dressing type, application and exercises, if appropriate. The average QoL score based on a 0–1 scale with 1 representing the ‘best health you can imagine’, increased from 0.69 to 0.84 (p<0.001) after three months; wound size decreased by 85.4%; and pain, reported using a 10-point scale, reduced from a mean of 6.35 to 4.74 (p<0.001). The inference from this study was that patient-centred care, listening to patient feedback and exploring reasons why they were unable to follow a suggested care plan is important. This finding supports the need for shared decision-making and concordance with goals of management, including consideration of pain, and in turn confirms the need for education to be part of a collaborative approach.
The notion of the importance of listening to patients was identified in a qualitative study by Green et al,153 which was included in Gethin et al’s149 systematic review. Green et al identified that during nurse-patient consultations opportunities to explore issues related to experience of living with leg ulceration were not always fully explored. Green and colleagues provided an example of a patient being unsure whether increased pain fell within the nurse’s sphere of responsibility and instead discussing the pain with a doctor in a medical consultation. Equally if the patient perceives the nurse to be busy or in a hurry, they may not wish to hold them up. In the wider context of patient education and wound pain the implications of this study are that healthcare professionals need to demonstrate a willingness to listen and engage with the individual in order to facilitate a therapeutic relationship to address any issues they may have.153 This conclusion is also reflected in the EWMA Document, Evidence for Person-Centred Care in Chronic Wound Care.50
Overall, the findings from this set of evidence are applicable to individuals with chronic leg ulcers specifically.
5.3.3 Pressure ulcers (PUs)
The systematic review by Thomas et al150 examined the effectiveness of structured patient education in individuals with PU. Thomas and colleagues studied the impact on knowledge, participation, wound healing, and QoL. Of the five studies cited in the review two reported that patient education had a positive effect on QoL: Carlson et al (2019) and Arora et al (2017). The concept of pain is reflected in both the QoL tools used by these authors (EQ-5D-5L [pain/discomfort] and SF-36 [pain]) therefore the studies were deemed relevant to this review.
Arora et al (2017) employed the use of pamphlets about PU prevention, weekly advice by telephone for 12 weeks, which included information on self-help strategies i.e. appropriate seating, bed overlays, cushions, equipment, diet, nutrition and wound dressings. In addition, they were advised about techniques to relieve pressure and when to seek further medical or nursing attention. Some participants were advised to remain on strict bed rest. Participants were also provided with continence advice. Each week, participants and the health-care professionals negotiated goals that were reviewed at the next phone call.
Carlson et al’s (2019) intervention included a Pressure Ulcer Prevention Programme (PUPP) which included six modules (Table 10). Module 5 (Happiness and Personal Well-Being) included an element related to managing pain.
Table 10: Pressure Ulcer Prevention Programme (PUPP) – modules overview (reproduced from Carlson et al. 2019) (154)
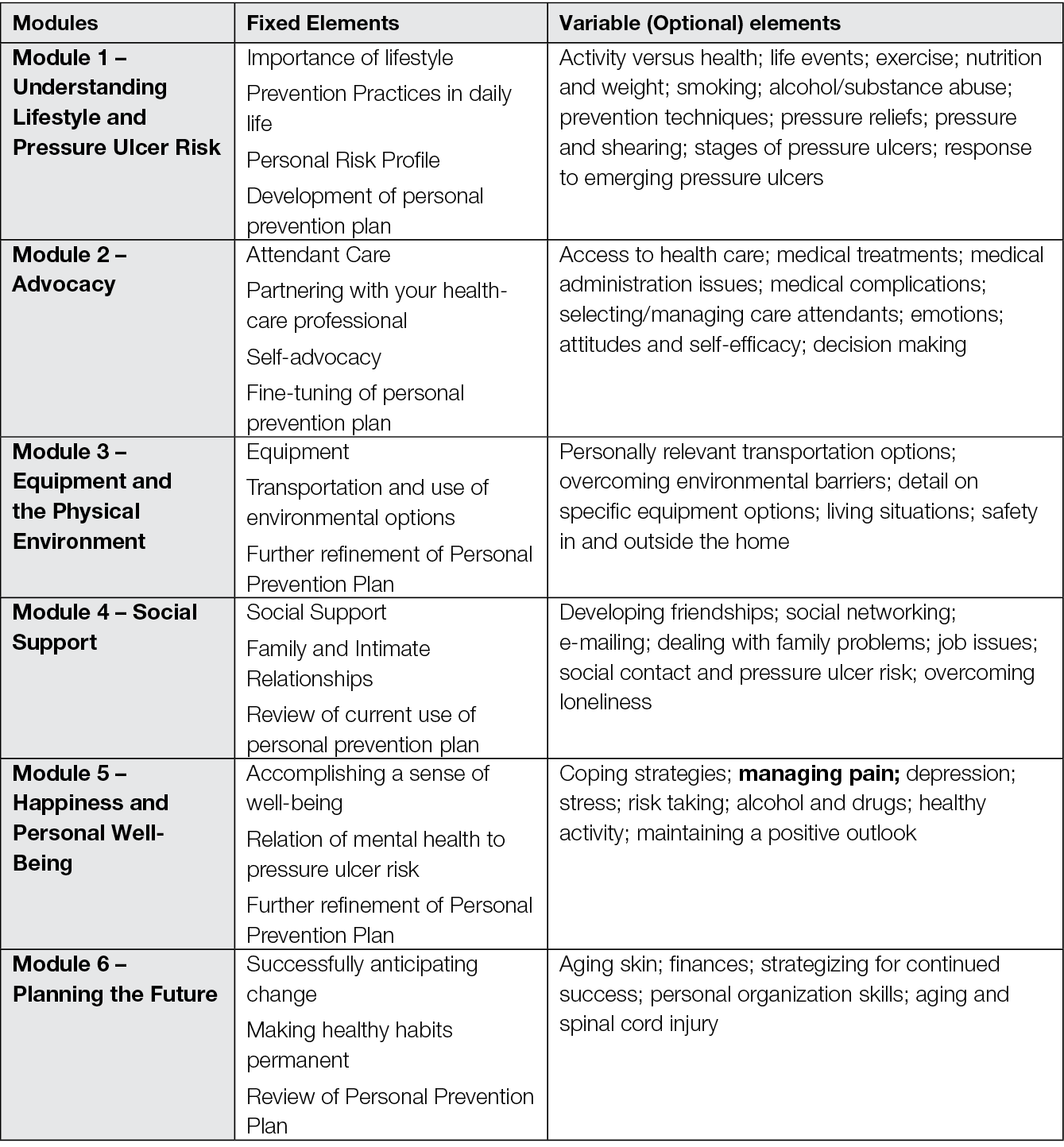
The intervention group received a structured approach to the delivery of the PUPP module content. This was supported with a combination of in-home visits and phone contact. Communication was provided in English or Spanish (based in patient preference). Occupational Therapists delivered the intervention and liaised with Registered Nurses if wound care issues arose. The PUPP included an ‘intensive phase’ (months 1–6) and a ‘tapered phase’ (months 7–12). During the intensive phase pre-planned weekly contact included individual, face-to-face home sessions (n=9) and telephone calls (n=15). The majority of the content of each module was delivered in the intensive phase. During the tapered phase, contact was twice per week and included in-person one on one home visits (n=2) and telephone calls (n=9). Contacts in the tapered phase centred on review of prevention practices, reinforcement of personalised lifestyle applications, and responses to developing risk situations. Throughout the intervention, face-to-face sessions lasted on average 1.5 hours, and phone call duration averaged 30 minutes. Carlson et al (2019) sought to determine the impact of the PUPP intervention on PU incidence specifically and showed that rates did not differ between the intervention and control group. With regards to changes in QoL and in particular the difference in pain at baseline and at 12 months there was no statistically difference in the intervention versus the control group.
Thomas et al150 deemed the two studies to be of high methodological quality and suggested that the findings support the effectiveness of structured patient education for individuals with a spinal cord injury and PI in improving QoL. However, the implications for provision of patient education related to pain and wounds is unclear.
5.4 Summary of recommendations based on the evidence
Based on a careful analysis of available resources and our current scientific and clinical experience, we have presented a summary of recommendations for wound and pain patient education in Table 11. Pain is unfortunately a common part of life for persons with non-healing wounds, yet the field of pain management is still under-researched scientifically and recommendations for patient education are lacking. It should be borne in mind that individuals with different types of wounds experience different types of pain in terms of duration, characteristic features and nature of influencing factors. In the Evidence Framework Summary presented we have attempted to identify the most important areas for education, along with listing appropriate educational tools and indicating competent professionals to implement education. Through this Evidence Framework we are focusing on empowering practitioners to drive change through engaging them equitably in the design, production, and use of evidence. At the core of the framework’s theory of change is a belief, that by prioritizing the learning and decision-making needs of practitioners, and by working collaboratively with practitioners to build timely evidence, we will see more effective programs, policies, and practices with evidence of equitable outcomes for patients, their families, and all other stakeholders. We acknowledge that we have not conducted a systematic review, therefore it was not possible to present a GRADE EtD framework,116 which is a systematic and transparent approach to making well informed healthcare choices. Nevertheless, the recommendations are summarised on the best available evidence for clinical practice, as well as clinical experience and expertise.
Table 11: Summary of recommendations for patient education
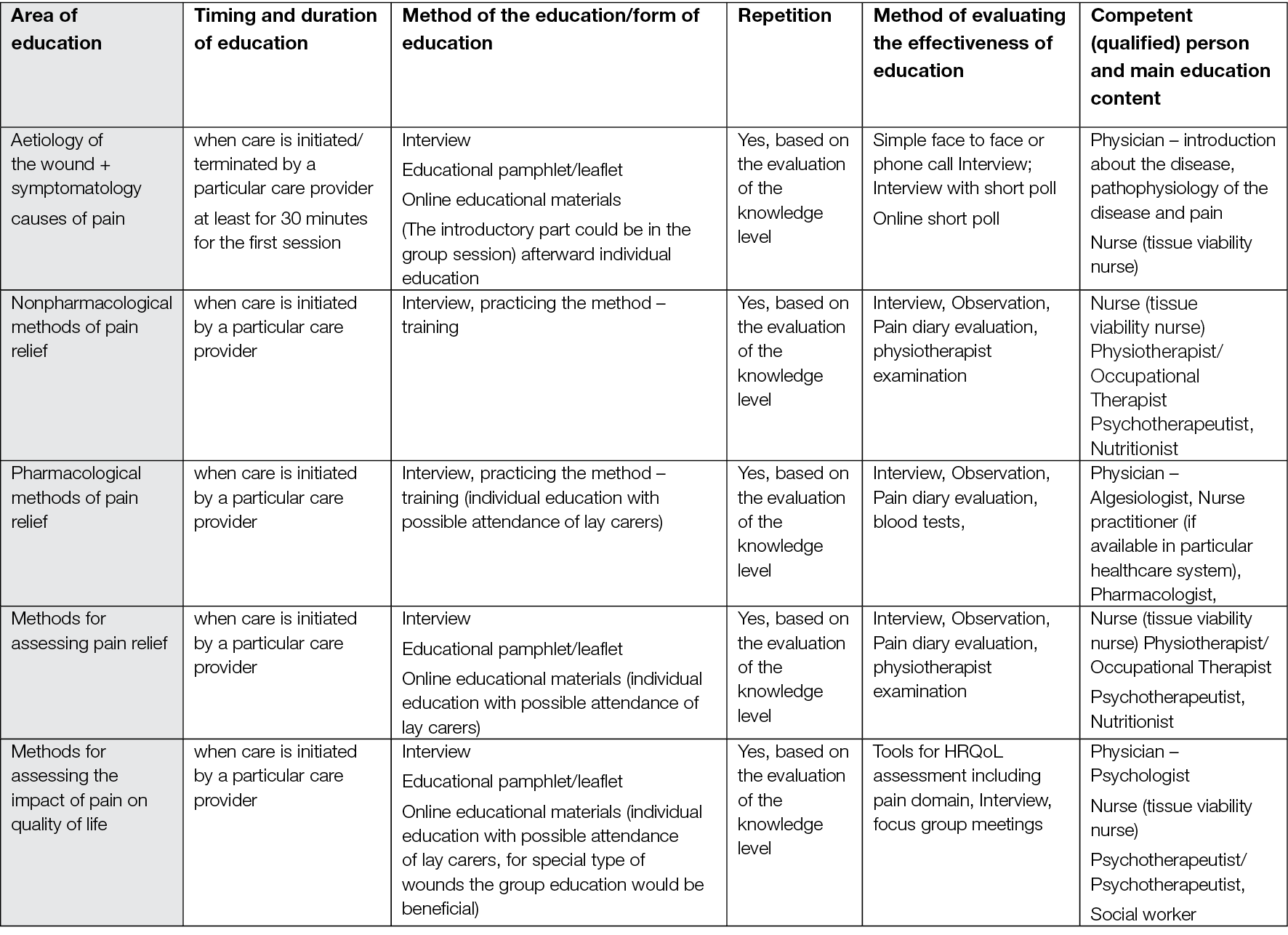
6. Role of psychological approaches for wound-related pain
6.1 Introduction
This chapter reviews evidence related to the role of psychological therapies for wound-related pain management and chronic wounds. The results are based on two systematic reviews. A summary of recommendations from the evidence, clinical experience and expertise is provided at the end of the chapter to facilitate implementation into clinical practice.
6.2 Method
6.2.1 Search method
The search strategy aimed to find systematic reviews related to the role of psychological approaches in the holistic management of wound related pain. We searched the L OVE platform, which collects systematic reviews retrieved from the systematic reviews database Epistemonikos7 and allocates them to specific L OVEs and questions.8 We conducted a search in L OVE Wounds and burns on 17 June 2022 and retrieved relevant systematic reviews using the filter for ‘behavioural’ interventions. There were no language, publication year or publication status restrictions.
We screened the reference lists of all eligible systematic reviews and hand searched websites of relevant organisations and institutions.
6.2.2 Inclusion criteria
Systematic reviews of pain and chronic wounds, which discussed an intervention related to management of wound-related pain were included.
6.2.3 Exclusion criteria
Acute wounds, burns (burn injuries).
6.2.4 Selection of studies
Retrieved titles and abstracts were exported into Rayyan52 by an information specialist (Simona Slezáková). The title and abstracts were screened in duplicate and independently by two authors (Alisha Oropallo, Andrea Pokorná). The blind mode within Rayyan was kept on until both authors had completed the first screening. Subsequently the blind mode was turned off to allow the authors to view each other’s decisions. The authors then met to resolve the disagreements and agree which results would move to the second stage of full-text review of selected articles. Full text-screening was conducted similarly to the title and abstract screening Following the full-text screening a list of studies for inclusion/exclusion was created.
The original search yielded 112 results. Following the title and abstract screening 100 were excluded, the main reasons for exclusion being wrong outcome or population. This generated 12 articles for full text review. Ten full texts were excluded as they did not have the relevant outcome or population (nine of them were focused on patients with burn injuries and one of them specifically on children with burns injuries). Two articles met the inclusion criteria and were included in the analysis (Appendix 10). The screening and the assessment process is described in detail in flow diagram (Figure 11).
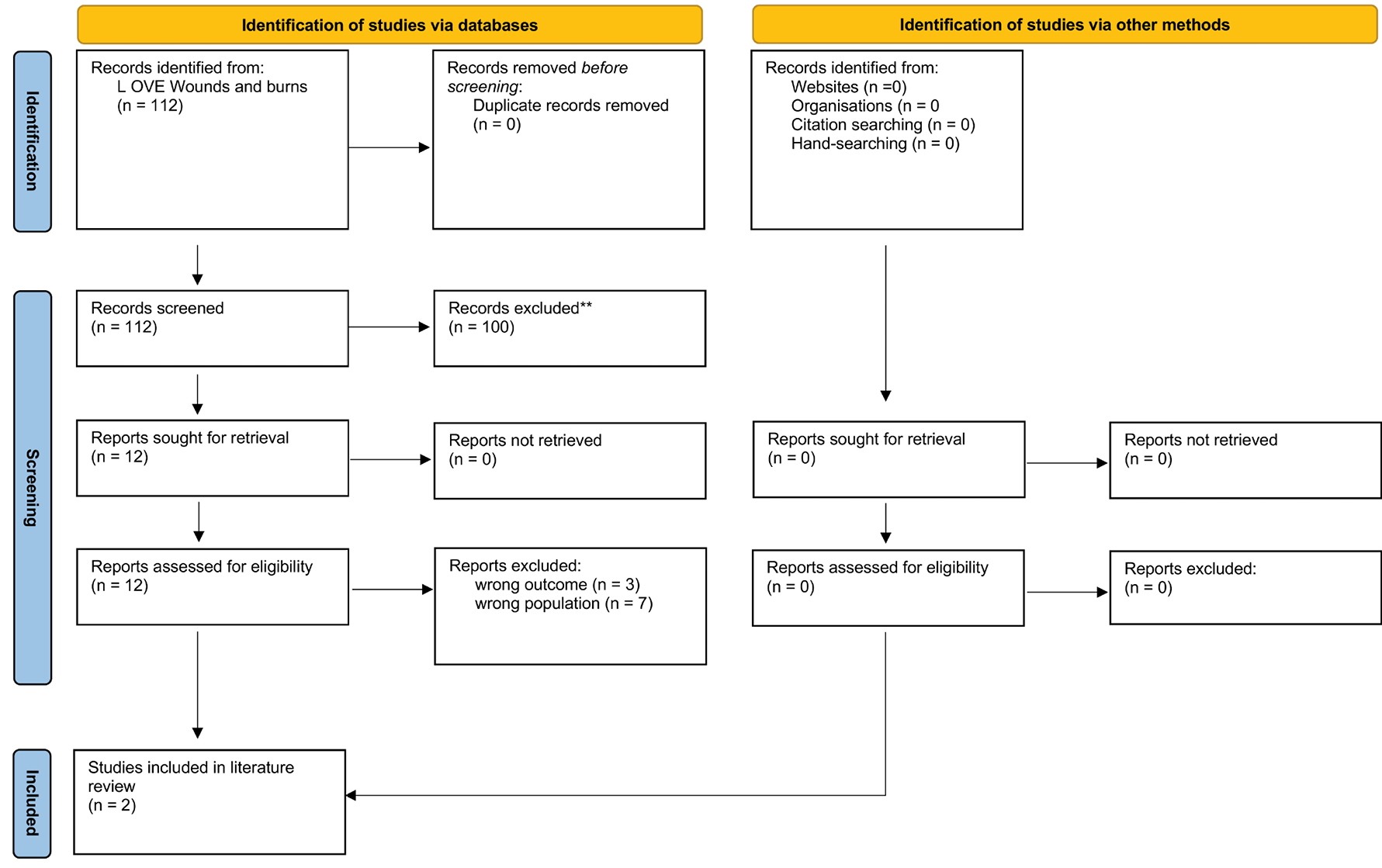
Figure 11: Flow diagram of the screening and the assessment process for psychological approaches (modified PRISMA 2020 flow diagram)
6.2.5 Data extraction
Relevant data were extracted from the included reviews by Samantha Holloway.
6.3 Results
6.3.1 Characteristics of the systematic reviews
The characteristics of the two reviews146,149 have already been discussed in Chapter 5 on patient education.
Liberato and colleagues146 reviewed nursing interventions used in the management of pain in people with VLUs.Of relevance to the psychological aspects of managing pain was the study by Kane et al155 which examined the use of aromatherapy and music therapy as strategies to manage pain during dressing changes. This study will be discussed in more detail in the next chapter which reviews complementary and alternative therapies, however, in relation to psychological aspects the results of the study point to the applicability of these therapies as potential distraction/relaxation techniques2 (Table 13). Liberato et al146 also discussed the positive impact that social models of care for individuals with chronic venous ulcers (such as Leg Clubs) can have in terms of social support. It could also be that attendance at a Leg Club impacts on the attention, cognition and emotion domains proposed by Linton and Shaw2, although further research examining these specific aspects would be needed to explore this.
Gethin et al149 also reviewed the role of Leg Clubs and cited a study by Finlayson et al (2010). The intervention included weekly Leg Club visits, peer support, goal setting and social interaction promotion. The results showed an increase in QoL including activities of daily living, morale and self-esteem. Wound healing (ulcer area reduction) and pain reduction were also reported. In relation to Linton and Shaw’s 2 work these findings speak to Leg Clubs having a positive effect on a number of factors (attention, cognition and emotion) to counteract the possible effects on pain and disability.
Gethin et al149 discussed a study by Kelechi et al (2014) (reviewed in Chapter 5) which reported on the positive outcomes of a motivational enhancement programme for individuals with infected leg ulcers. Based on these results it would appear that such a programme may help to address negative cognition (cognitive restructuring) and emotion/emotion regulation activation, thereby promoting well-being). This literature search found no evidence on psychological approaches to managing wound-related pain, such as Acceptance Commitment Therapy (ACT) or Cognitive Behavioural Therapy (CBT) that are currently used in the management of chronic pain.156 Table 12 summarises the psychological factors associated with pain, their processes and additionally treatment strategies that may be suitable for individuals living with chronic wound-related pain.
Table 12: Psychological factors in pain, their processes and management strategies2
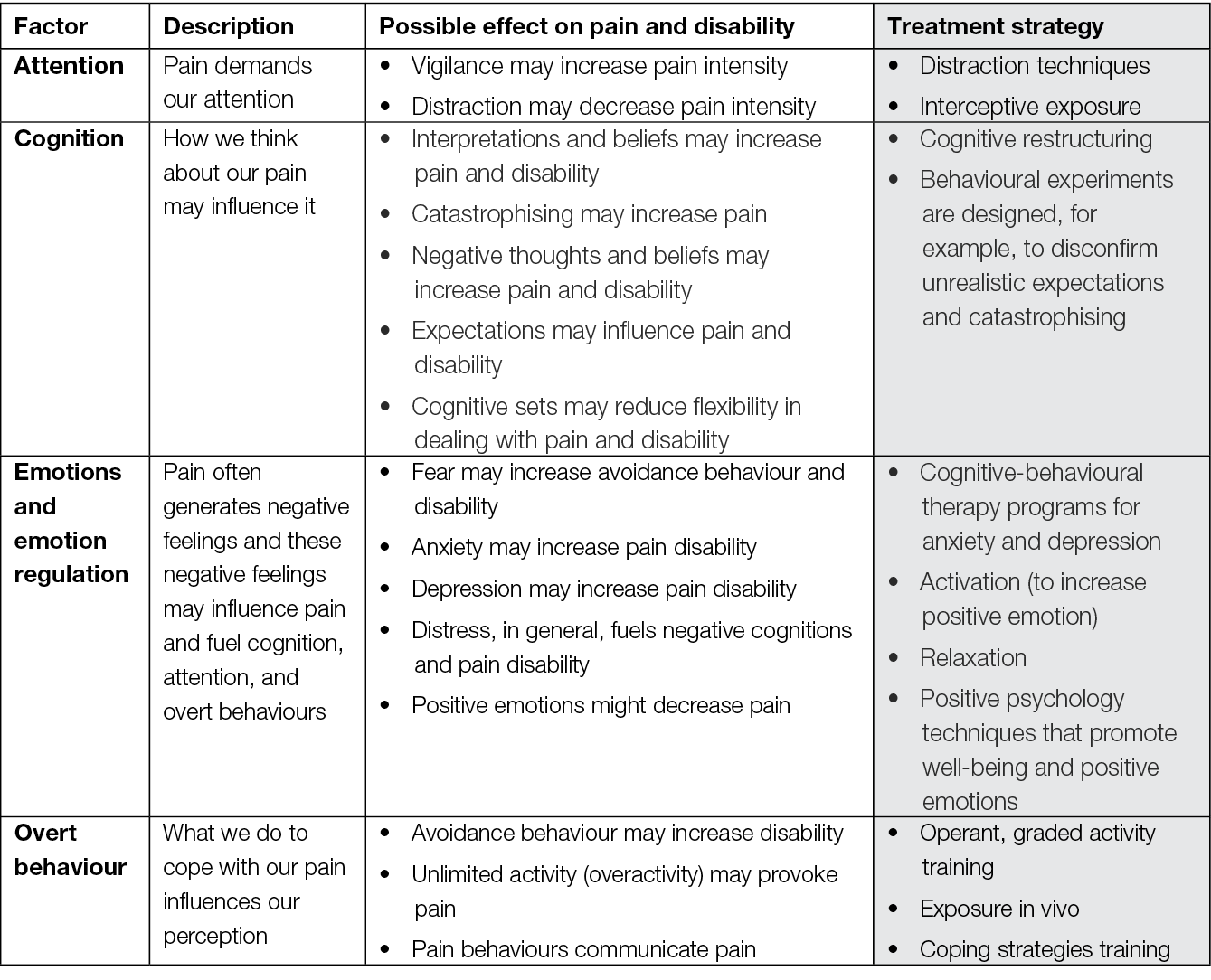
Figure 12 presents nociception, pain perception, and the biobehavioural response to pain, in the nociceptive pathway (adapted from Garland21) and where pain management strategies work.
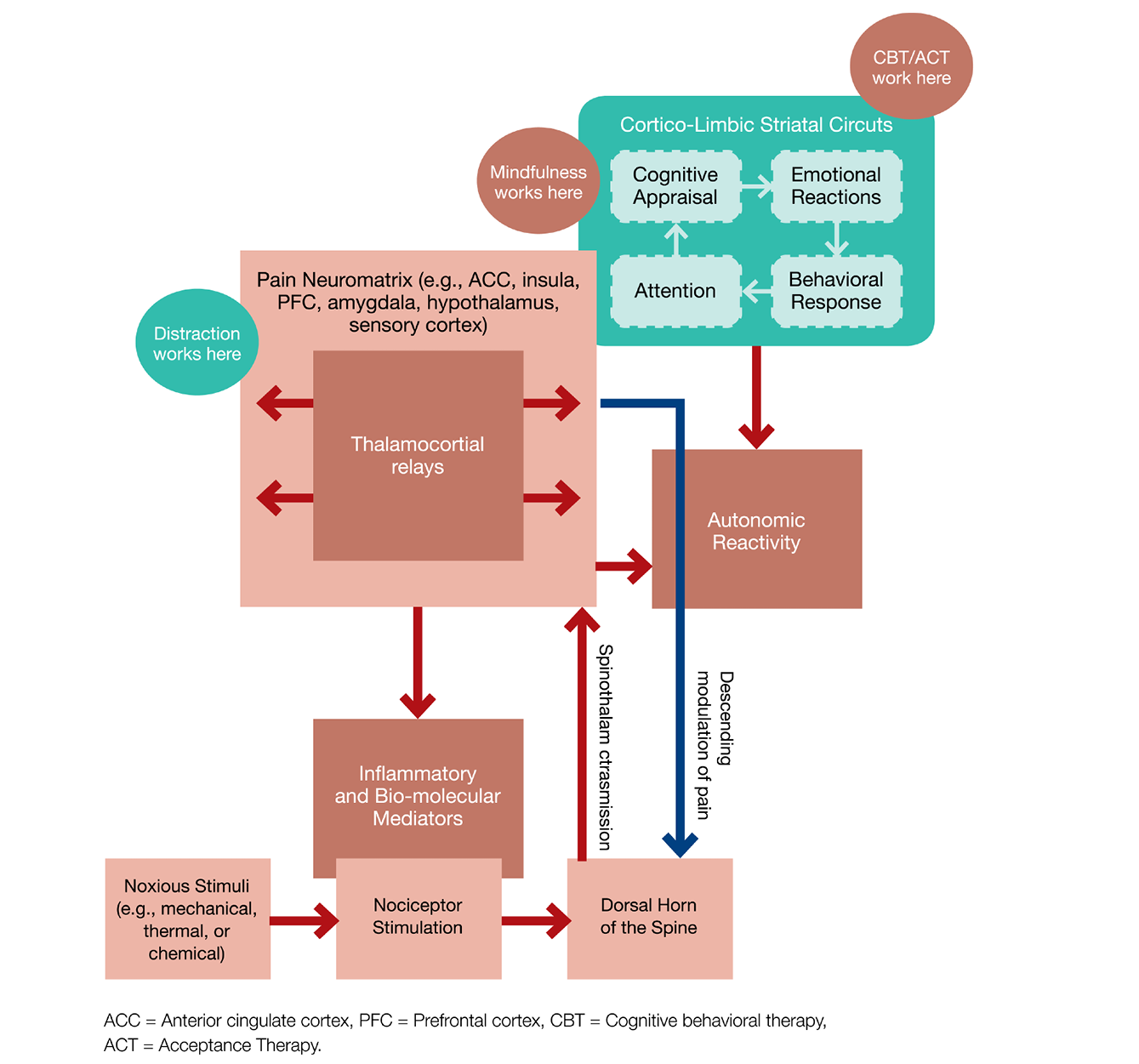
Figure 12: The nociceptive pathway, adapted from Garland (2012)21
6.4 Summary of recommendations
No specific conclusions from the limited body of evidence for psychological approaches could be elicited. However, some key themes emerged, for example the use of distraction and relaxation techniques to help with procedural-related pain was noted. The evidence also seemed to indicate a role for social models of care and specifically Leg Clubs in helping to manage pain. Based on these findings that such models have an indirect effect of reduction of pain are likely to be related to the reported increases in QoL measures. These QoL measures include enhancing ability to undertake activities of daily living and improving self-esteem. There also seemed to be evidence that strategies to enhance motivation and patient activation are important. Approaches that promote an individual’s well-being as well as helping to regulate emotions are essential.
The next chapter will examine the evidence for complementary and alternative approaches for wound-related pain.
7. Role of complementary and alternative medicine for wound-related pain
7.1 Introduction
This chapter reviews evidence related to the role of complementary and alternative therapies for wound-related pain management and chronic wounds. The search results for this theme identified reviews related to honey, traditional Chinese medicine (TCM), anthocleista, low-level laser therapy, Ficus Deltoidea Jack and interventions for MFWs. The results are based on 18 systematic reviews. A summary of recommendations from the evidence, clinical experience and expertise is provided at the end of the chapter to facilitate implementation into clinical practice.
7.2 Method
7.2.1 Search method
The search strategy aimed to find systematic reviews related to the role of complementary and alternative medicine in the holistic management of wound-related pain. We searched the L OVE platform, which collects systematic reviews retrieved from the systematic reviews database Epistemonikos7 and allocates them to specific L OVEs and questions.8 We conducted a search in L OVE for wounds and burns on 17 June 17 2022, and retrieved relevant systematic reviews using the filter for complementary and alternative medicine. There were no language, publication year or publication status restrictions.
We screened the reference lists of all eligible systematic reviews and hand-searched websites of relevant organisations and institutions.
7.2.2 Inclusion criteria
Systematic reviews of pain and chronic wounds, which discussed an intervention related to pain and complementary and alternative medicine.
7.2.3 Exclusion criteria
Acute wounds, burns (burn injuries).
7.2.4 Selection of studies
Retrieved titles and abstracts were exported into Rayyan52 by an information specialist, Simona Slezáková. The title and abstracts were screened in duplicate and independently by two authors (Kirsti Ahmajärvi, Samantha Holloway). The blind mode within Rayyan was kept on until both authors had completed the first screening. Subsequently, the blind mode was turned off to allow the authors to view each other’s decisions. The authors then met to resolve the disagreements and agree which results would move to the second stage of a full-text review of selected articles. Full-text screening was conducted similarly to the title and abstract screening. Following the full-text screening a list of studies for inclusion / exclusion was created.
The original search yielded 158 results including one duplicate. Following the title and abstract screening 125 were excluded, the main reason for exclusion being that they were acute wounds (burns, surgical). This generated 32 articles for full text review. Of these 14 full texts were excluded as they did not have the relevant outcome/population or did not meet criteria for publication type. This left 18 articles that met the criteria and were included in the analysis (Appendix 11). The screening and assessment process is described in detail in the flow diagram (Figure 13).
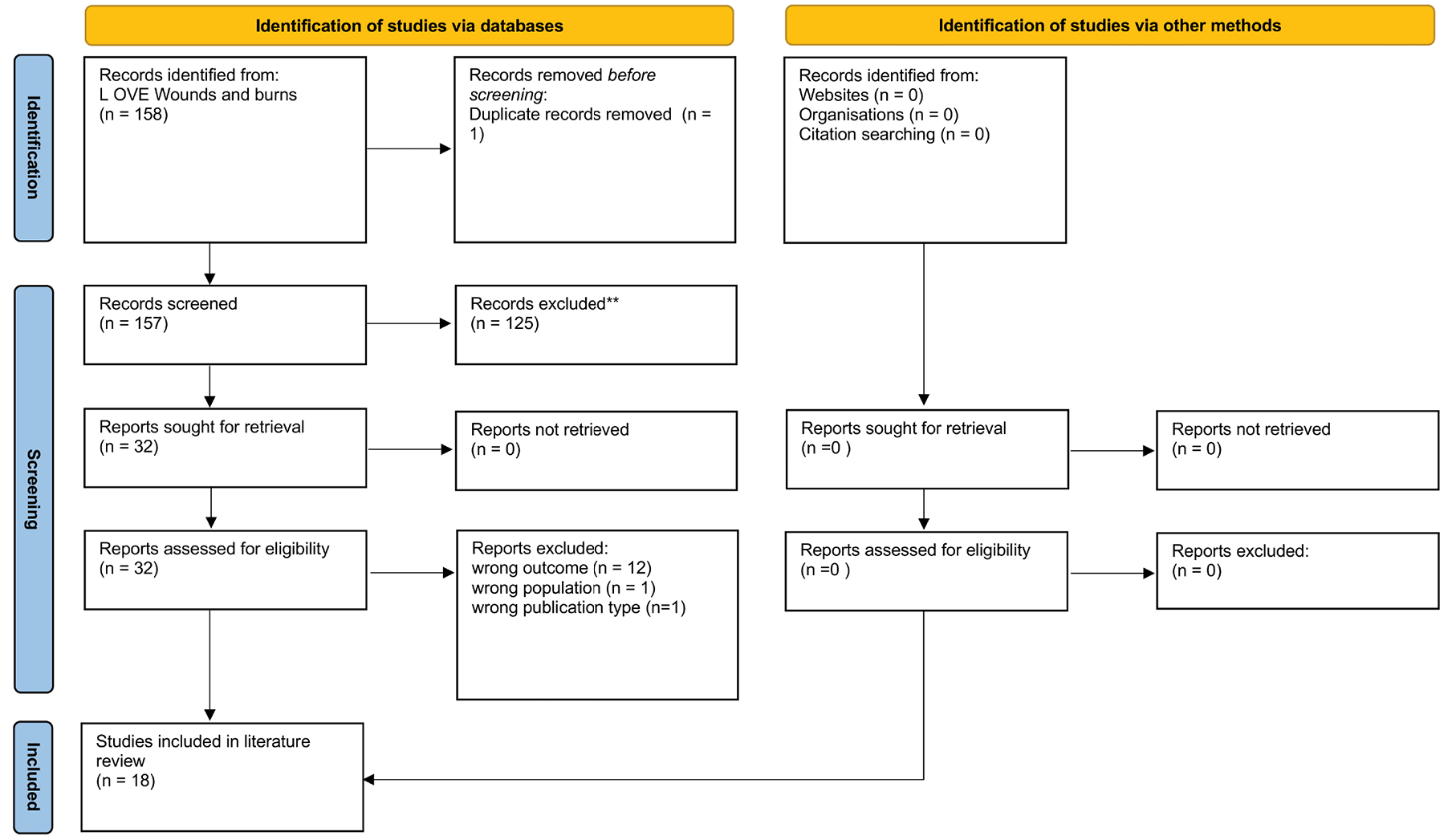
Figure 13: Flow diagram of the screening and the assessment process for complementary and alternative medicine (modified PRISMA 2020 flow diagram)
7.2.5 Data extraction
Relevant data were extracted from the included reviews by Samantha Holloway.
7.3 Results
7.3.1 Characteristics of the systematic reviews
A full-text review of 18 systematic reviews was undertaken; the topics of the reviews included honey (n=10), TCM (n=2), anthocleista (n=1), low-level laser (n=1), Ficus Deltoidea Jack (Moraceae) (n=1), interventions for MFWs (n=1) and two were generic reviews of any interventions for chronic wounds which included alleviation of pain.
Of the 18 systematic reviews, 11 provided a detailed PRISMA flow diagram to report the number of studies included. The total number of studies across these reviews was n=315, with n=133 focusing solely on the use of honey. The remaining seven reviews did not provide sufficient information to determine the number or type of studies; in fact, these were more of a narrative synthesis of the evidence rather than true SRs. Thirteen reviews provided information about the date range or indicated a specific search date. The date range for the searches across these reviews was 1966–2019 for human/clinical studies and slightly more recent for in vivo and in vitro (animal) studies (2021). Five reviews did not provide information about the date range. Only seven of the 18 reviews provided information about the sample sizes of the studies included; the total number of participants was n=3392, and of these, more than half (n=1875) related to the use of honey.
Twelve of the reviews provided information about the geographical location of the studies. For the studies examining the use of honey, most continents were represented, with no predominance in one particular country (Box 4).
Box 4: Geographical location of studies related to honey
| Africa | Netherlands | UK | Nigeria |
| Belgium | Egypt | Germany | Portugal |
| Qatar | New Zealand | Malaysia | Denmark |
| Greece | Saudi Arabia | India | Pakistan |
| Hong Kong | Indonesia | Czech Republic | China |
One review of the use of propolis focused on Polish research, and the reviews on generic interventions examined evidence from Canada, Denmark, Australia, and the UK. The review of icus Deltoidea Jack (Moraceae) focused on its use in Malaysia, and the use of TCM was based on studies in China.157
The evidence will be presented in themes related to the interventions, beginning with the use of honey.
7.4 Honey
The earliest review reporting on the use of honey was by Fox158 who reviewed evidence from individual and multiple case studies published between 1966–2002. Six studies were identified, providing a total of 66 patients with different wound types (recalcitrant surgical wounds, chronic wounds, ‘ulceration’, chronic infected wounds, leg ulceration and recalcitrant wounds and ulcers). Five of the studies examined the effect of honey on pain, with three reporting a decrease in pain. Very limited information was provided on the methodological quality of the studies; in particular, it was difficult to determine how pain was assessed. The review sets the scene for the role of honey and its potential impact on pain but is relatively limited in terms of providing strong evidence.
A subsequent review by Mwipatayi et al159 examined the evidence for the clinical effects of topical honey on chronic leg ulcers (CLU). Pain was not a primary outcome of the review; however, Mwipatayi and colleagues discussed pain as part of the theoretical framework for their review, highlighting the reported anti-inflammatory effects of honey. While the review title suggests the focus was on patients with CLU, of the total number of patients included (n=50), less than half (n=21) had chronic wounds. Mwipatayi et al discussed that all of the studies reviewed were at risk of different sources of bias (lack of blinding, poor reporting quality, and limited sample sizes). All of the studies were clinical, observational trials, and none reported on the effect of honey on wound-related pain.
Bardy et al160 provided a synthesis of the evidence related to the role of honey in cancer care. The authors cited two studies which examined pain in patients with leg ulcers: Dunford and Hanano (2004) and Oluwatosin et al (2000). The multi-centre, non-randomised study by Dunford and Hanano (2004) included 40 patients, the results showed a statistically significant reduction in pain (1.6±1.22 to 1.08±1.54, p<0.001). However, in a non-randomised, comparative study Oluwatosin et al (2000) did not find any statistically significant reduction in pain at the end of treatment (p>.05).
Dunford and Hanano’s (2004) research is the most detailed account of the assessment of pain and the effect of honey identified as part of this current review; therefore, this study was reviewed in more detail. Dunford and Hanano used the McGill Pain Questionnaire to assess pain, where zero=no pain; 1=mild pain; 2=discomfort; 3=distressing pain; 4=horrible pain; 5=excruciating pain. The results showed that 50% (n=20) of patients experienced a decrease in reported pain levels (Table 13). Eleven patients reported increased pain, eight of whom attributed the change to the honey dressing specifically. This was something the earlier review by Fox158 had not identified as a side effect. Dunford and Hanano (2004) also noted that patients whose wounds were larger at baseline reported that their pain increased or there was a sustained elevation of pain. In turn, when wound size was reduced there was a decrease in pain. None of the other studies reviewed discussed the link between wound size and reported pain levels, so it is difficult to draw any definitive conclusions about this aspect.
Table 13: Summary of pain scores and percentage wound reduction and rate of wound reduction, reproduced from Dunford and Hanano (2004)61
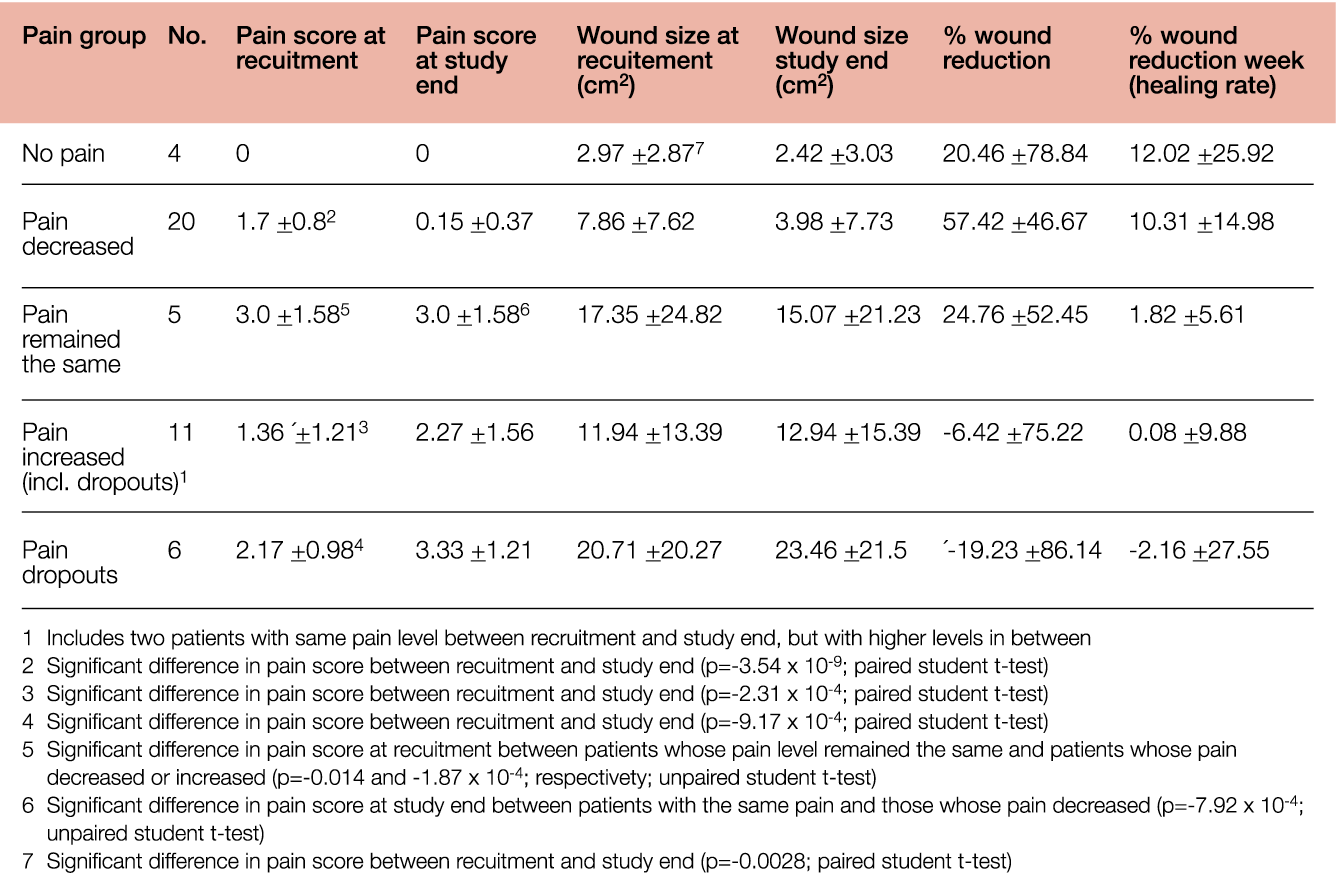
Vandamme et al162 published a review of Honey in modern wound care in the Burns journal. Of the 55 studies included, 19 related to chronic wounds (VLU, DFU, PU/PI). Examining evidence published up to July 2012, Vandamme and colleagues discussed one RCT which examined pain as a primary outcome suggesting that honey has a statistically significant effect on pain. Five studies reported measuring the parameters of wound pain with two reporting a positive effect, but this was not statistically significant (Table 14). Over half of the studies in the review did not report pain as an outcome measure.162
Table 14: Outcomes of the included studies by wound category and design, reproduced from Vandamme et al (2013)162
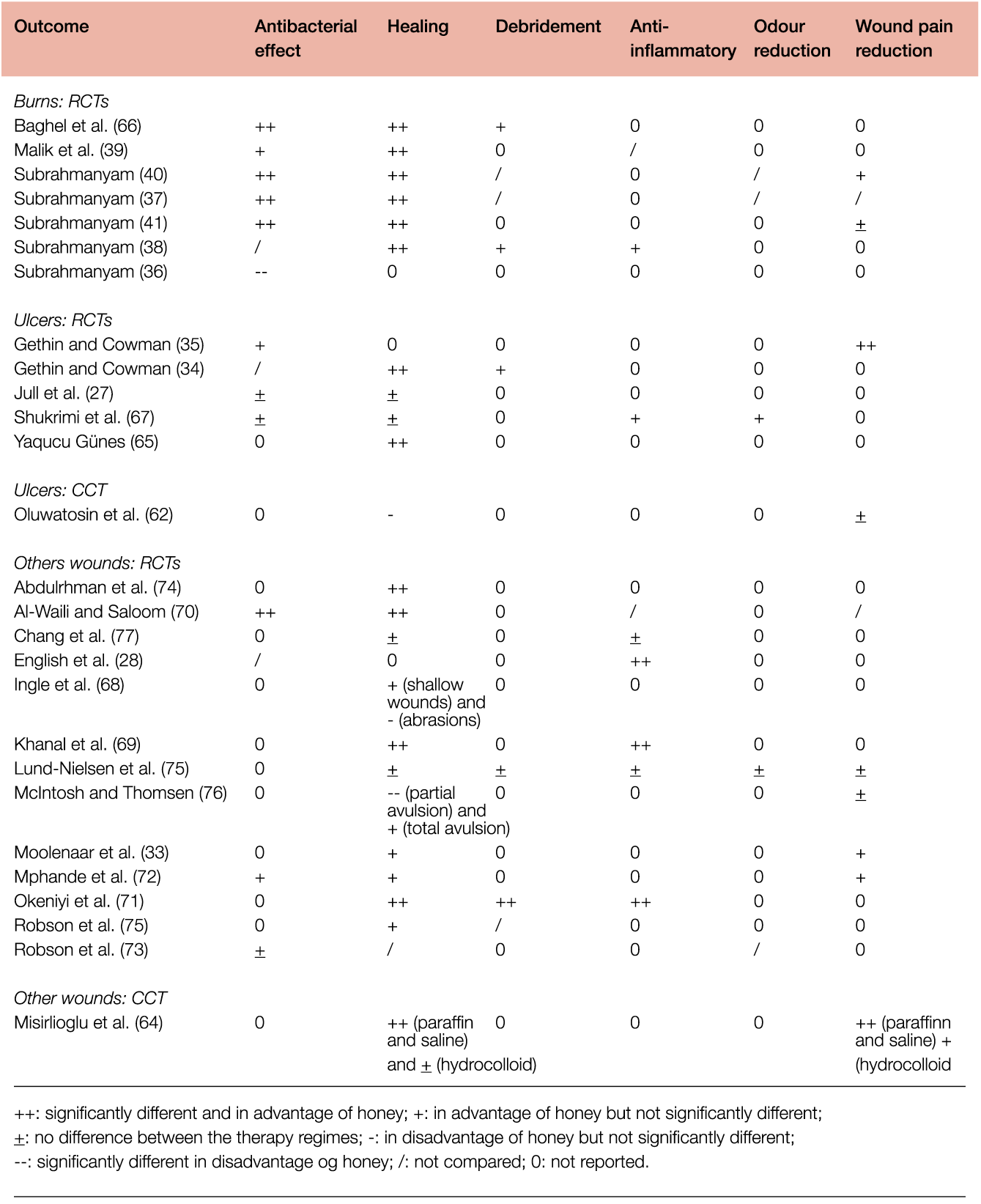
The numbers in left column refer to references in Vandamme et al.162
A review in the same year by Yaghoobi et al163 examined the evidence for the antioxidant, antibacterial and anti-inflammatory properties of honey. The review was included as it is well-known that pain is a sign of inflammation; therefore, it was relevant to the subject of wound-related pain. Yaghoobi and colleagues proposed that the anti-inflammatory action of honey leads to a reduction in oedema and exudate production.163 Citing Simon et al (2009), Yaghoobi et al discussed that the anti-inflammatory effect of honey also reduces pain caused by pressure on nerve endings and reduces the amount of prostaglandin produced in the inflammatory process (see Chapter 2: The Multidimensional Nature of Pain for more on the role of prostaglandin in inflammation).
Yaghoobi et al163 concluded that the evidence for the use of honey was stronger for burn injuries than for individuals with chronic leg ulcers with regard to pain relief. However the review included animal as well as human studies and the authors did not report the number of studies or participants separately to determine the reliability of the review. Oryan et al164 presented a narrative review of the mechanisms and therapeutic properties of honey on wound healing. Similar to the review by Yaghoobi et al163. Oryan and colleagues discussed the anti-inflammatory properties of honey and based on evidence from six studies, proposed that honey can help to reduce oedema and pain. A more recent review by Anastasiou et al165 examined the in vitro and in vivo evidence for the therapeutic properties of honey to inform its use for individuals with DFU. The review focused on animal wounds specifically, which limits the external validity to some degree; however, Oryan et al suggested that honey can reduce prostaglandin levels and thus decrease oedema, exudation and inflammation. Oryan et al also proposed that the effect was to reduce ‘topical’ pain. The implications for peripheral or nociceptive pain are not clear (165).
Yaghoobi and colleagues also proposed that honey can contribute to the painless lifting of sloughy tissue due to its debridement action (163); this view was echoed by Anastasiou et al. (165). Whilst this does not relate to the management of wound-related pain per se, it is a clinically important consideration in the wider context of holistic management of pain in relation to wound bed preparation and debridement.
In a recent review of the use of honey in the management of nonhealing wounds, Vyhlídalová et al. (166) examined data from 13 primary studies (RCTs n=8, Prospective studies n=5). The number of participants in the assessed studies ranged from 10 to 375, and all but one was related to adults. Six of the studies investigated the effect of honey on the management of DFU, two pertaining to individuals with LU and one MFW; the remaining studies included wounds of various aetiologies. Vyhlídalová and colleagues (166) did not comment on the findings related to pain in their conclusion, but examination of the individual studies (Biglari et al. 2013, Gulati 2014, and Mohamed 2015) provided evidence of a decrease in the pain levels during the study (based on a VAS scale). Biglari et al. (2013) also reported on the reduction of the need for analgesics during dressing changes.
The most recent review of honey was undertaken by Yilmaz et al167 who examined RCTs (n=30) published between 2009–2019. The studies represent findings from a range of geographical locations including Pakistan, Iran, India, Saudi Arabia, Denmark, Indonesia, Greece, China, the Czech Republic and the UK. They concluded that honey provided rapid epithelization and wound contraction in wound healing, had an anti-inflammatory and debridement effect, decreased pain, ensured infection control, shortened wound healing time and was cost-effective. Four of the studies included mentioned pain as a specific outcome, one of which related to burn injuries, and three included patients with chronic wounds. Dubashi and Sindwani (168) compared the use of honey to phenytoin in 150 patients (group A, 50 patients treated with honey; group B, 50 patients treated with phenytoin; group C, 50 patients treated with saline dressings). The underlying wound aetiology was wound infections (n=32), trophic ulcers (n=33), DFUs (n=51), venous ulcers (n=22) and pressure sores (sic) (n=12). Pain was assessed using a Visual Analog Scale (VAS) on days 5, 10, 15 and 20. Table 15 shows the pain scores at each time point.168
Table 15: Comparison of pain score at the 5th, 10th, 15th and 20th days, reproduced from Dubashi and Sindwani (2015)168
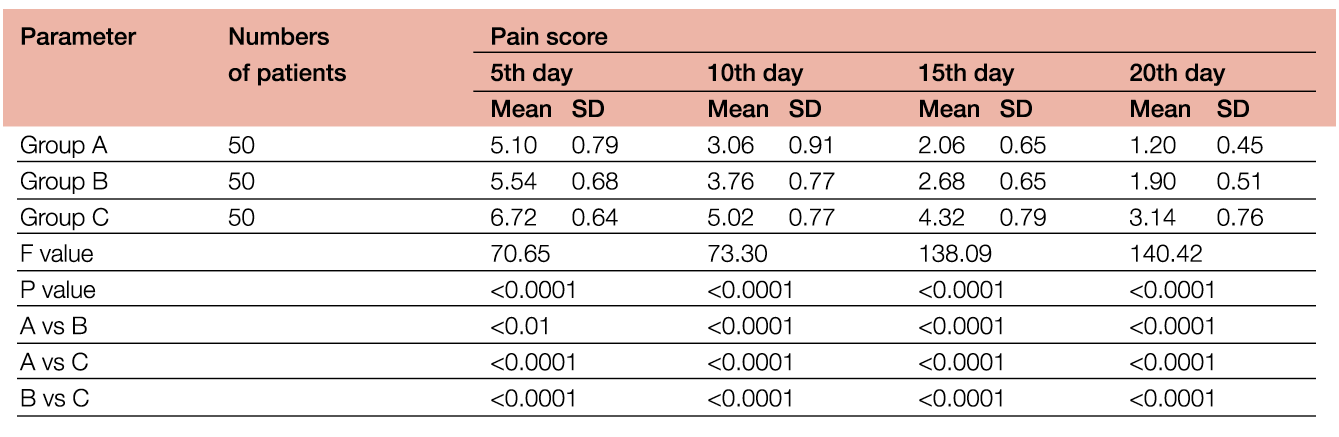
Yimaz et al proposed that the experience of pain is reduced due to the anti-inflammatory activity of honey, but this is speculative rather than based on data from their study.
Zeleníková and Vyhlídalová169 reported on the results of a prospective interventional study in elderly persons receiving home care (n=40). The intervention group was treated with honey (n=20), and the control group (n=20) had conventional dressings, with the patients being followed up for three months. The Wound Healing Continuum (WHC) guided the assessment, and a VAS was used to assess pain intensity. Wound aetiologies included PUs (n=7), lower leg ulcers (n=9) and diabetic foot syndrome (n=4). Zelenikova and Vyhlidalova reported that there was a statistically significant difference in pain intensity between the two groups (p=0.0007), with higher pain scores being indicated by controls (169). Table 16 shows the differences in pain intensity reported between the two groups at dressing change on Day 1 and Day 20. While the results for Day 20 are statistically significant (p 0.0007), Zelenikova and Vyhlidalova do not report on the pain intensity scores in the intervening 19 days to determine any variance in reported pain. This limits the conclusions that can be drawn.
Table 16: Differences in pain intensity between groups, adapted from Zeleníková and Vyhlídalová (2019)169
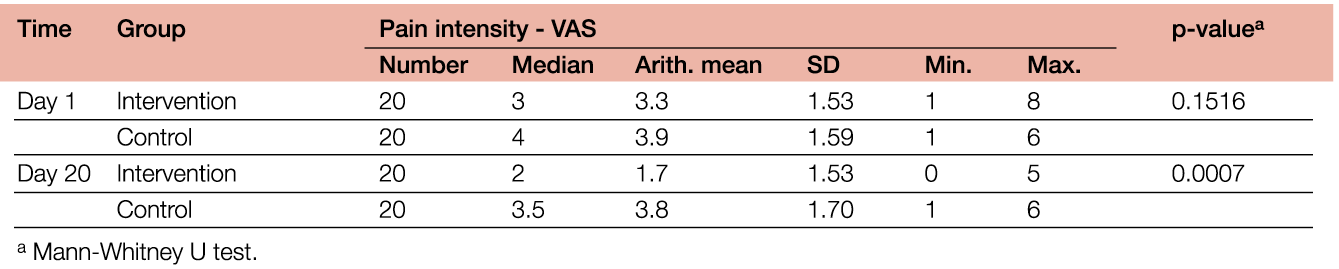
Rojczyk et al170 undertook a review of Polish research on propolis and its medical application for wound healing. While pain was mentioned as an outcome, this was in relation to a symptom of mouth ulcers. Rojczyk and colleagues discuss the anti-inflammatory properties of honey but in relation to the physiological response in wound healing rather than as a potential approach to the treatment of wound-related pain.
Overall, the evidence of the use of honey for the management of wound-related pain seems to indicate that the effects may be related to its anti-inflammatory properties.
7.5 Effects of aromatherapy and music on pain
Liberato et al146 reviewed the evidence for a range of nursing interventions for the management of pain in patients with VLUs. They undertook their search in June 2015 and identified seven studies for inclusion. Liberato and colleagues reported on a pilot study by Kane et al155 which examined the use of ‘odour therapies’ (lavender and lemon) and music therapies (relaxing and preferred music). The sample size was small (n=8), mainly male (n=5), with a mean age of 70.1 years. The SF-MPQ was used, which comprises a 10cm line (no pain to worst possible pain), and the Present Pain Inventory (PPI) was also used. It is a 6-point verbal descriptor scale, rated 0–6. Kane et al155 observed that pain increased during the dressing change procedure, and the lavender odour therapy reduced pain immediately after the procedure. For the music therapies, the study demonstrated no significant effects on pain intensity either during or after the dressing change. Kane et al suggested that the relaxing music, and not the preferred music, may have an analgesic effect (reduced pain intensity) after the dressing change; however, no statistically significant difference was shown. These results are based on one small pilot study, so making specific recommendations for either therapy is difficult.
7.6 Evidence to support therapies for malignant fungating wounds (MFWs) and pain
Tsichlakidou et al171 examined interventions to support symptom management (malodour, exudate, pain and bleeding) in individuals with MFWs. The treatments investigated included manuka honey, NPWT and foams (with and without silver). The review was limited to evidence indexed on Medline only. Tsichlakidou et al identified a range of evidence (n=9), including cross-sectional studies, ‘patient group study’, qualitative/descriptive/cross-sectional, RCTs and case studies. The review cites evidence published up to 2017. Tsichlakidou and colleagues conclusion centred around the use of oral opioids to manage pain, but a number of individual studies discussed the use of different dressings to manage wound-related pain171. This included Maund (2008), who reported on the use of an ionic sheet hydrogel dressing for pain relief. Lund-Nielsen (2011) compared the use of honey-coated bandages compared with silver-coated bandages and found no statistically significant difference in terms of wound size, cleanliness, malodour, exudation and wound pain. (Note: please also see the discussion of topical analgesics and anaesthetics in Chapter 4, Section 4.6).
7.6.1 Traditional Chinese medicine (TCM)
Two systematic reviews examined the use of TCM, specifically the genus Desmodium species, in terms of its anti-inflammatory, anti-pyretic and analgesic activity. Ma et al172 included experimental, animal and human studies; however, it’s not clear how many studies and participants were included. The article was a narrative synthesis of the available evidence with inhibition of pain discussed in relation to joint, rheumatoid, stomach, ear, lumbar and traumatic swelling. There was no discussion of the use of Desmodium species for wound-related pain.
Li et al173 evaluated the effectiveness of the external application of TCM (EA-TCM) in individuals with VLU. Li and colleagues included 16 studies with a total of 1269 participants. Across the studies, there were 660 subjects in the experimental groups and 609 in the controls. The sample sizes ranged from 51–164. The TCM interventions included ointments (n=9 studies), powders (n=3 studies), Chinese-herb external washing (n=3 studies), paste and oil (n=1 in each case). Comparison of the same interventions showed that there were significant differences in total effectiveness rates between EA-TCM and conventional therapy groups (RR=1.22, 95% confidence interval [CI]=1.16– 1.29, and P<0.00001). Compared to conventional therapy, EA-TCM combined with conventional therapy had a superior total effectiveness rate (RR=1.11, 95% CI=1.04–1.19, and P=0.003). There were no significant differences in recurrence rates during follow-up and final pain measurements between the experimental and those in the control groups (RR=0.86, 95% CI=0.31–2.39, and P=0.85; MD −0.75, 95% CI= −2.15–0.65, and P=0.29). Two of the studies reported final pain measurements: Xu (2012) and Zhang (2013). The pooled results showed that there was a difference between the intervention and control groups.
Li et al stated that due to the low methodological quality of the studies, it was difficult to draw conclusions. Based on these reviews, there appears to be a lack of strong evidence for the use of TCM for the management of wound-related pain.
7.7 Anthocleista
Anyanwu et al174 reviewed ethnobotany, phytochemistry and pharmacology of the genus Anthocleista, of which there are approximately 50 species. This plant is used as a form of traditional medicine in Africa. Anyanwu et al sought to determine its effects on various conditions, including pain. Where pain was mentioned, this related to chest and abdominal pain treatment. In relation to pain associated with wounds and inflammation, the nature of the injury was unclear; therefore, it was difficult to draw any conclusions about its effects on wound-related pain.
7.8 Non-specific reviews
Ongarora175 explored the topic of technological improvements in the management of chronic wounds, specifically to identify advances in alleviating pain, promoting healing or controlling wound infections. The author included ‘articles in scientific journals’ (n=119) which had been published after the year 2000. With regard to the management of pain, Ongarora discussed one study which used low-dose topical steroids (LDTS) in patients with chronic wounds (n=34) across three centres over a three month period (176). Pain levels were assessed using a patient-rated VAS (0–10) as ‘no response’, ‘poor response’ (<50% reduction), ‘good response’ (>50% reduction) and ‘total’ (no pain, VAS rating 0). Table 17 summarises the outcomes for the LDTS.
Table 17: Outcomes achieved with topical corticosteroid treatment (adapted from Ongarora 2022) (175)
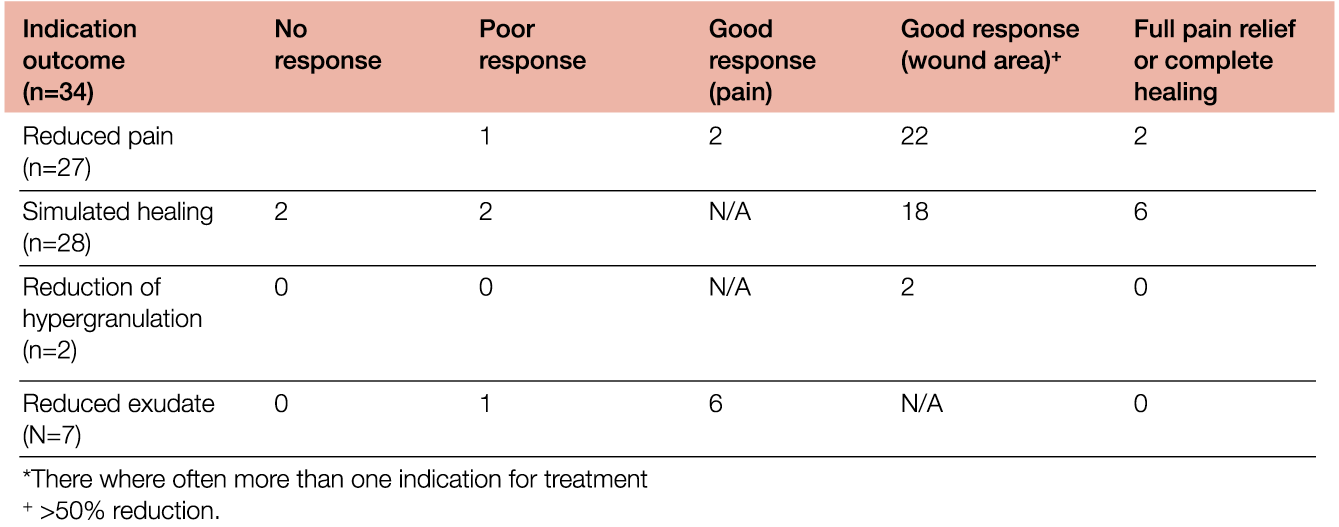
The overall conclusion was that it accelerated healing, reduced pain, and controlled the formation of hypergranulation tissue formation in 79% (n=27) patients. Ongarora proposed that LDTS suppressed inflammation, which positively influenced healing and pain relief. However, they cautioned that careful monitoring is required because of the risk of sensitisation. No other studies were found that examined the use of topical LDTS.
7.9 Low-level laser technology (LLLT)
Peplow et al177 reported on the evidence base for the use of low-level laser technology (LLLT) for pain relief and wound healing. This systematic review examined research from animal (n=16 studies) and human studies (n=15). The human studies provided a total of 41 patients from case studies and observational studies. While patients had mainly acute wounds the review was included as it discussed the use of the therapy as laser acupuncture therefore it was deemed relevant in the wider context of wound-related pain. Five studies examined the effect of LLLT on pain and inflammation where the pain was measured using a modified VAS (self-evaluation) or by more subjective measures (‘patients reporting of pain’). While many studies focused on outcomes associated with the effect of LLLT to stimulate wound healing, the studies also reported positive outcomes regarding the therapy’s ability to decrease pain and inflammation. As none of the studies examined the effect of LLLT on wound-related pain specifically, it is difficult to draw firm conclusions. However, the evidence points to a potential gap in the research regarding the use of this technology to treat wound-related pain.
7.10 Summary of recommendations
Based on a thorough review of available resources and clinical experience, it is very difficult to recommend practices of complementary and alternative medicine that have a clear positive impact on wound-related pain. The available studies that have used various alternative approaches have not always assessed pain as a primary outcome and have used different rating scales to measure pain intensity. In terms of the evidence base for complementary and alternative medicine, one aspect that could strengthen future research is to move away from using solely unidimensional tools to assess pain, such as VAS and NRS and instead use multidimensional scales and tools that facilitate the assessment of the nature of the pain and other parameters. More specifically, most of the studies did not examine wound-related pain specifically, however this is partly understandable as it is difficult to isolate the experience of pain because of its multidimensional nature.
It was not possible to present a GRADE EtD framework, which is a systematic and transparent approach to making well informed healthcare choices, due to the lack of systematic and well-designed studies addressing the influence of complementary and alternative medicine on wound-related pain. Therefore, for this chapter it was not possible to prepare a summary of recommendations for clinical practice. Therefore is a need for new studies that directly investigate the impact of complementary and alternative approaches on pain in individuals with wounds.
7.11 Key points
- There is some evidence to support the role of honey for the management of wound-related pain, specifically the research indicates that the analgesic action may be related to its anti-inflammatory properties. This helped to reduce localised oedema and exudate which in turn reduces the effects of prostaglandin and therefore the pressure on nerve endings. Some studies also reported a reduction in pain intensity. Much of the evidence for honey relates to leg ulcers and one study reported an increase in pain with the use of honey, therefore the evidence is contradictory in some respects. Also, in relation to honey, due its debridement properties, the evidence suggests that the effect on pain is in relation to quicker wound closure.
- There is limited evidence to support the use of aromatherapy and music, however these approaches may help in terms of providing a ‘distraction’ and, as they are unlikely to be harmful, it’s certainly worth discussing with individuals whether they would find these helpful.
- Evidence for TCM, Plants, LDTS and LLLT was very weak.
8. Challenges and next steps for the holistic management of wound-related pain
The experience of pain is subjective and complex; therefore, approaches need to consider and include the psychological aspects as well as the social factors that affect the individual. Hence a multidisciplinary approach, with different healthcare professionals and expertise, is needed. Yet despite advances in pain assessment and pain management over the last three decades, pain is not always managed effectively.178, 179 It has been argued that there has been a lack of referrals to pain services or cross-team working, such as between those in wound care and pain management, in caring for individuals with chronic wounds and persistent pain.180 This situation may be related to individual and healthcare-related barriers to pain and wound management.
System-related factors include the lack of clearly defined standards and pain management protocols, and limited access to pain specialists and, in some instances, appropriate analgesics due to healthcare policies and economy.181,182 In the healthcare profession, barriers to effectively managing pain may include personal attitudes, beliefs, culture, sensitivity, and knowledge and understanding.183 In individuals with pain, barriers may relate to genetics, culture, spirituality, prior experience, anxiety, attitudes and beliefs about pain and how pain management affects the experience of pain, knowledge, and understanding.184,185,186,187
Several authors have identified a gap in the education of undergraduate healthcare students throughout the western world with regards to the topic of pain education. 188,189,190,191 Furthermore, clinicians report not feeling confident about managing those with chronic pain.192 As a consequence, this can influence attitudes about pain and health outcomes of individuals with pain.193,194,191 A systematic review by Ortiz et al,195 found that nurses’ knowledge of pain was positively related to previous pain training, highlighting the need to ensure appropriate pain education provision in preparing students for clinical practice.
There is a paucity of evidence examining patients’ knowledge and understanding of wound-related pain specifically and how clinicians communicate it. This is a significant gap in the literature, given the multidimensional nature of pain and the influence of biopsychosocial factors. This could be addressed by future research exploring individuals’ knowledge and understanding of wound-related pain. Until new evidence emerges to inform patient education for wound-related pain, there are opportunities to develop patient information brochures and booklets to support knowledge and understanding. Additionally, digital forms of information can be provided via social media, videos, and software applications to encourage improved pain literacy. Importantly, patient information should be provided in a structured way which facilitates active engagement and shared-decision making as a part of patient-centred care. Sometimes people worry about overusing analgesics and, conversely, others overuse them. Therefore, it is essential to increase health literacy and financial literacy to improve pain management and keep patients in partnership in the care process. This can include increasing understanding that improper use of pain medication can lead to further complications.196
Overall, there is a lack of prospective studies focusing on the management of wound-related pain and effective treatment strategies.
Gaps in the evidence base
It is acknowledged that different approaches are used in the chronic pain settings, as part of the multidisciplinary approach to pain management. For example, Pain Neuroscience Education (PNE) is used as part of physiotherapy/manipulative approaches,197 however, there was no evidence found in this literature search for education in those with chronic wound-related pain. The evidence base for pharmochemical therapeutics that may be of benefit for individuals with wound-related pain also warrants consideration. These areas could be considered in the future for further research.
In this document, we discussed the potential role of distraction therapy to help with the management of procedural pain. Evidence from the study of individuals with complex regional pain syndrome suggests that rather than distraction strategies, approaches that foster attentional orienting to a painful sensation is more effective. It’s not known if this is also the case for individuals with wound-related pain, but it is certainly worth exploring to determine the best strategy.
We are aware that there are a number of studies examining interventions such as electrical stimulation and the role that may have in managing pain; however, our search did not identify an existing systematic review that has examined the evidence base. Such a review is needed to inform clinical practice.
One-page summary: holistic management of wound-related pain

9. Resources to support knowledge and education for the holistic management of wound-related pain
EWMA wound curricula (physicians and nurses)
- Wound Healing Curriculum (2015). (Adopted in 2018 by UEMS and approved as the official ETR for specialisation in wound healing for physicians)
- Wound Curriculum for Student Nurses – EQF level 4 (2021)
- Wound Curriculum for Nurses – EQF levels 5 – 7 (2017, 2019, 2020)
EWMA E-Learning
- Module 6: Introduction to Pain in Wound Management (2022)
EWMA projects and documents
- EWMA Document: The Impact of Patient Health and Lifestyle Factors on Wound Healing (2022)
- EWMA Document: Evidence for Person-Centred Care in Chronic Wound Care (2020)
- EWMA Video project: Living with Chronic Wounds (2018)
Resources are available for free reading and download at www.ewma.org
Author(s)
Samantha Holloway (Editor), RN, MSc, PGCert
Centre for Medical Education, School of Medicine, School of Biomedical and Life Sciences, Cardiff University, Wales, UK
Kirsti Ahmajärvi, MD
Specialist in General Medicine, Special Competence in Wound Management, Specializing Physician in Geriatrics, Helsinki University Hospital and University of Helsinki, Helsinki, Finland
Nicoletta Frescos, PhD, MPH, BAppSci(Pod), FWA
Faculty of Pain Medicine, Australian and New Zealand College of Anaesthetists and Adjunct Lecturer, La Trobe University, Victoria, Australia
Sue Jenkins, RN, MSc, PGCert
Centre for Medical Education, School of Medicine, School of Biomedical and Life Sciences, Cardiff University, Wales, UK
Alisha Oropallo, MD, MSc
Donald and Barbara Zucker School of Medicine, Hofstra University/Northwell Health, Hempstead, New York, USA
Simona Slezáková, PhD
Masaryk University, Faculty of Medicine, Dept. of Health Sciences, Institute of Biostatistic and Analyses, The Czech National Centre for Evidence-Based Healthcare and Knowledge Translation, Brno, Czech Republic
Andrea Pokorná, Prof, PhD, RN
Masaryk University, Faculty of Medicine, Dept. of Health Sciences, Institute of Biostatistic and Analyses, The Czech National Centre for Evidence-Based Healthcare and Knowledge Translation Brno, Czech Republic
Critical reviewers
Dr Stefano Coaccioli, Chief
Dept. of Internal Medicine, Rheumatology and Medical Pain Therapy, Santa Maria General Hospital, Terni, Italy
Andrew Colwill, Advanced Physiotherapy Practitioner
Velindre NHS Trust, Cardiff University, Cardiff, Wales, UK
Professor Kevin Woo, PhD RN NSWOC FAPWCA
Queen’s University, School of Nursing, Kingston, Ontario, Canada
Corresponding author:
Samantha Holloway
HollowaySL1@cardiff.ac.uk
Editorial support:
Anne Wad
EWMA Secretariat
© EWMA 2024 Copyright of published material and illustrations is the property of the European Wound Management Association. However, provided prior written consent for their reproduction, including parallel publishing (e.g., via repository), is obtained from EWMA via the Editorial Board of the Journal, and proper acknowledgement is given, such permission will normally be readily granted. Requests to produce material should state where material is to be published, and, if it is abstracted, summarised, or abbreviated, then the proposed new text should be sent to Journal of Wound Management Editor for final approval. Although EWMA has taken great care to ensure accuracy, EWMA will not be liable for any errors of omission or inaccuracies in this publication.
Published by the European Wound Management Association, Nordre Fasanvej 113, 2, 2000 Frederiksberg, Denmark
Web: www.ewma.org. Email: ewma@ewma.org
The EWMA Holistic Management of Wound-Related Pain document is supported by Convatec, Essity and PolyMem
References
- Love-Jones SJ. Pain as a Subjective, Multidimensional Experience. In: Abd-Elsayed A, editor. Pain [Internet]. Cham: Springer International Publishing; 2019 [cited 2024 Jan 5]. p. 141–4. Available from: http://link.springer.com/10.1007/978-3-319-99124-5_35
- Linton SJ, Shaw WS. Impact of Psychological Factors in the Experience of Pain. Phys Ther. 2011 May 1;91(5):700–11.
- Craig KD, MacKenzie NE. What is pain: Are cognitive and social features core components? Paediatr Neonatal Pain. 2021 Sep;3(3):106–18.
- Gardner SE, Blodgett NP, Hillis SL, Borhart E, Malloy L, Abbott L, et al. HI-TENS Reduces Moderate-to-Severe Pain Associated With Most Wound Care Procedures: A Pilot Study. Biol Res Nurs. 2014 Jul;16(3):310–9.
- Green J, Jester R, McKinley R, Pooler A. The impact of chronic venous leg ulcers: a systematic review. J Wound Care. 2014 Dec 2;23(12):601–12.
- Woo KY, Harding K, Price P, Sibbald G. Minimising wound-related pain at dressing change: evidence-informed practice. Int Wound J. 2008 May;5(2):144–57.
- Epistemonikos [Internet]. Available from: https://www.epistemonikos.cl/proyectos/love/
- i L·OVE evidence [Internet]. [cited 2023 Nov 29]. Available from: https://iloveevidence.com/
- International Association for the Study of Pain. IASP Announces Revised Definition of Pain [Internet]. International Association for the Study of Pain (IASP). 2020 [cited 2023 Sep 1]. Available from: https://www.iasp-pain.org/publications/iasp-news/iasp-announces-revised-definition-of-pain/
- International Association for the Study of Pain Acute Pain. International Association for the Study of Pain (IASP). [cited 2023 Sep 1]. Acute Pain. Available from: https://www.iasp-pain.org/resources/topics/acute-pain/
- World Union of Wound Healing Societies. Minimising pain at wound dressing-related procedures: a WUWHS consensus document [Internet]. Wounds International; Available from: https://www.woundsinternational.com/resources/details/minimising-pain-wound-dressing-related-procedures-wuwhs-consensus-document
- Arroyo-Novoa CM, Figueroa-Ramos MI, Miaskowski C, Padilla G, Stotts N, Puntillo KA. Acute Wound Pain: Gaining a Better Understanding. Adv Skin Wound Care. 2009 Aug;22(8):373–80.
- Pogatzki-Zahn EM, Zahn PK, Brennan TJ. Postoperative pain—clinical implications of basic research. Best Pract Res Clin Anaesthesiol. 2007 Mar;21(1):3–13.
- Swift A. Understanding the effect of pain and how the human body responds. Nurs Times. 2018;114(3):22–6.
- The Anatomy and Physiology of Pain. In: Pain and Disability: Clinical, Behavioral, and Public Policy Perspectives [Internet]. Washington, D.C.: National Academies Press; 1987 [cited 2023 Sep 1]. p. 991. Available from: http://www.nap.edu/catalog/991
- Yam M, Loh Y, Tan C, Khadijah Adam S, Abdul Manan N, Basir R. General Pathways of Pain Sensation and the Major Neurotransmitters Involved in Pain Regulation. Int J Mol Sci. 2018 Jul 24;19(8):2164.
- Lecturio [Internet]. [cited 2023 Sep 21]. Pain: Types and Pathways – Lecturio. Available from: https://app.lecturio.com/#/article/3862?return=__app__%2Fsearch%2Fnociception
- Xu Q, Yaksh TL. A brief comparison of the pathophysiology of inflammatory versus neuropathic pain. Curr Opin Anaesthesiol. 2011 Aug;24(4):400–7.
- Answine JF. A Basic Review of Pain Pathways and Analgesia. Anaesth News Spec Ed. 2018;139–54.
- Sorkin LS, Eddinger KA, Woller SA, Yaksh TL. Origins of antidromic activity in sensory afferent fibers and neurogenic inflammation. Semin Immunopathol. 2018 May;40(3):237–47.
- Garland EL. Pain Processing in the Human Nervous System. Prim Care Clin Off Pract. 2012 Sep;39(3):561–71.
- IASP International Association for the Study of Pain [Internet]. [cited 2023 Sep 21]. Definitions of Chronic Pain Syndomes. Available from: https://www.iasp-pain.org/advocacy/definitions-of-chronic-pain-syndromes/
- Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain. 2019 Jan;160(1):19–27.
- Revision of the International Classification of Diseases (ICD-11) [Internet]. International Association for the Study of Pain (IASP). [cited 2023 Sep 4]. Available from: https://www.iasp-pain.org/advocacy/icd-11-pain-classification/
- Scholz J, Finnerup NB, Attal N, Aziz Q, Baron R, Bennett MI, et al. The IASP classification of chronic pain for ICD-11: chronic neuropathic pain. Pain. 2019 Jan;160(1):53–9.
- Colloca L, Ludman T, Bouhassira D, Baron R, Dickenson AH, Yarnitsky D, et al. Neuropathic pain. Nat Rev Dis Primer. 2017 Feb 16;3(1):17002.
- Melzack R, Wall PD. Pain Mechanisms: A New Theory: A gate control system modulates sensory input from the skin before it evokes pain perception and response. Science. 1965 Nov 19;150(3699):971–9.
- Mendell LM. The Path to Discovery of Windup and Central Sensitization. Front Pain Res. 2022 Feb 15;3:833104.
- Woolf CJ. Central sensitization: Implications for the diagnosis and treatment of pain. Pain. 2011 Mar;152(3):S2–15.
- Hiraga S ichiro, Itokazu T, Nishibe M, Yamashita T. Neuroplasticity related to chronic pain and its modulation by microglia. Inflamm Regen. 2022 Dec;42(1):15.
- Thiruvoth F, Mohapatra D, Sivakumar D, Chittoria R, Nandhagopal V. Current concepts in the physiology of adult wound healing. Plast Aesthetic Res. 2015;2(5):250.
- Hannoodee S, Nasuruddin DN. Acute Inflammatory Response. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 [cited 2023 Sep 1]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK556083/
- Briggs M, Bennett MI, Closs SJ, Cocks K. Painful leg ulceration: a prospective, longitudinal cohort study. Wound Repair Regen. 2007 Mar;15(2):186–91.
- Roth RS, Lowery JC, Hamill JB. Assessing Persistent Pain and Its Relation to Affective Distress, Depressive Symptoms, and Pain Catastrophizing in Patients with Chronic Wounds: A Pilot Study. Am J Phys Med Rehabil. 2004 Nov;83(11):827–34.
- Moffatt CJ, Franks PJ, Hollinworth H. Understanding wound pain and trauma: an international perspective. Pain Wound Dress Chang Eur Wound Manag Assoc Position Doc. 2002;
- Ferreira MC, Tuma P, Carvalho VF, Kamamoto F. Complex wounds. Clinics. 2006;61(6):571–8.
- Vuolo JC. Wound-related pain: key sources and triggers. Br J Nurs. 2009 Aug 13;18(Sup5):S20–5.
- Turk DC, Meichenbaum D, Genest M. Pain and behavioral medicine: a cognitive-behavioral perspective. 3. pr. New York: Guilford Pr; 1983. (The Guilford clinical psychology and psychotherapy series).
- Main CJ, Spanswick CC. Pain management: an interdisciplinary approach. Edinburgh ; New York: Churchill Livingstone; 2000.
- Solowiej K, Mason V, Upton D. Psychological stress and pain in wound care, part 2: a review of pain and stress assessment tools. J Wound Care. 2010 Mar;19(3):110–5.
- Upton D, Solowiej K, Hender C, Woo KY. Stress and pain associated with dressing change in patients with chronic wounds. J Wound Care. 2012 Feb;21(2):53–61.
- Woo KY. Exploring the Effects of Pain and Stress on Wound Healing. Adv Skin Wound Care. 2012 Jan;25(1):38–44.
- Richardson C. An introduction to the biopsychosocial complexities of managing wound pain. J Wound Care. 2012 Jun;21(6):267–73.
- Mills SEE, Nicolson KP, Smith BH. Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br J Anaesth. 2019 Aug;123(2):e273–83.
- Bissell DA, Ziadni MS, Sturgeon JA. Perceived injustice in chronic pain: an examination through the lens of predictive processing. Pain Manag. 2018 Mar;8(2):129–38.
- Burns JW, Post KM, Smith DA, Porter LS, Buvanendran A, Fras AM, et al. Spouse criticism and hostility during marital interaction: effects on pain intensity and behaviors among individuals with chronic low back pain. Pain. 2018 Jan;159(1):25–32.
- Rabey M, Buldo B, Duesund Helland M, Pang C, Kendell M, Beales D. Significant other interactions in people with chronic low back pain: Subgrouping and multidimensional profiles. Br J Pain. 2022 Jun;16(3):326–40.
- Duenas M, Ojeda B, Salazar A, Mico JA, Failde I. A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res. 2016 Jun;Volume 9:457–67.
- Upton D. Pain, wound care and psychology: the missing link? Wounds. 7(2):119–22.
- Gethin G, Probst S, Stryja J, Christiansen N, Price P. Evidence for person-centred care in chronic wound care: A systematic review and recommendations for practice. J Wound Care. 2020 Sep 1;29(Sup9b):S1–22.
- Frescos N. Pain assessment tools for chronic lower limb wounds: A scoping review. Wound Pract Res. 2019 Mar 31;27–35.
- Rayyan [Internet]. [cited 2023 Oct 19]. Available from: https://www.rayyan.ai/
- De Laat EH, Scholte Op Reimer WJ, Van Achterberg T. Pressure ulcers: diagnostics and interventions aimed at wound-related complaints: a review of the literature. J Clin Nurs. 2005 Apr;14(4):464–72.
- Herber OR, Schnepp W, Rieger MA. A systematic review on the impact of leg ulceration on patients’ quality of life. Health Qual Life Outcomes. 2007 Dec;5(1):44.
- Purcell A, Buckley T, King J, Moyle W, Marshall AP. Topical Analgesic and Local Anesthetic Agents for Pain Associated with Chronic Leg Ulcers: A Systematic Review. Adv Skin Wound Care. 2020 May;33(5):240–51.
- Da Costa Ferreira SA, Serna González CV, Thum M, Da Costa Faresin AA, Woo K, De Gouveia Santos VLC. Topical therapy for pain management in malignant fungating wounds: A scoping review. J Clin Nurs. 2023 Jul;32(13–14):3015–29.
- Gutierrez Y, Pourali SP, Kohn AH, Jones ME, Rajkumar JR, Armstrong AW. Topical opioid use in dermatologic disease: A systematic review. Dermatol Ther [Internet]. 2021 Nov [cited 2023 Sep 21];34(6). Available from: https://onlinelibrary.wiley.com/doi/10.1111/dth.15150
- Warden V, Hurley AC, Volicer L. Development and Psychometric Evaluation of the Pain Assessment in Advanced Dementia (PAINAD) Scale. J Am Med Dir Assoc. 2003 Jan;4(1):9–15.
- Measuring Pain in the Clinic [Internet]. European Pain Federation. [cited 2023 Nov 30]. Available from: https://europeanpainfederation.eu/measuring-pain-in-the-clinic/
- Monica 1776 Main Street Santa, California 90401-3208. 36-Item Short Form Survey Instrument (SF-36) [Internet]. [cited 2023 Nov 30]. Available from: https://www.rand.org/health-care/surveys_tools/mos/36-item-short-form/survey-instrument.html
- Chren MM. The Skindex Instruments to Measure the Effects of Skin Disease on Quality of Life. Dermatol Clin. 2012 Apr;30(2):231–6.
- Phsyiopedia pain [Internet]. [cited 2023 Oct 4]. Pain Score 0–10 Numerical Rating. Available from: https://www.physio-pedia.com/File:NRS_pain.jpg
- Taylor LJ, Herr K. Pain intensity assessment: a comparison of selected pain intensity scales for use in cognitively intact and cognitively impaired African American older adults. Pain Manag Nurs. 2003 Jun;4(2):87–95.
- Karcioglu O, Topacoglu H, Dikme O, Dikme O. A systematic review of the pain scales in adults: Which to use? Am J Emerg Med. 2018 Apr;36(4):707–14.
- Nemeth KA, Graham ID, Harrison MB. The Measurement of Leg Ulcer Pain: Identification and Appraisal of Pain Assessment Tools: Adv Skin Wound Care. 2003 Sep;16(5):260–7.
- Newbern S. Identifying Pain and Effects on Quality of Life from Chronic Wounds Secondary to Lower-Extremity Vascular Disease: An Integrative Review. Adv Skin Wound Care. 2018 Mar;31(3):102–8.
- Jenkins S. The assessment of pain in chronic wounds (part 2). Assess Pain Chronic Wounds Part 2. Vol 16/ 2020(No 4):36–44.
- Leren L, Johansen E, Eide H, Falk RS, Juvet LK, Ljoså TM. Pain in persons with chronic venous leg ulcers: A systematic review and meta-analysis. Int Wound J. 2020 Apr;17(2):466–84.
- Bourbonnais F. Pain assessment: development of a tool for the nurse and the patient. J Adv Nurs. 1981 Jul;6(4):277–82.
- Poquet N, Lin C. The Brief Pain Inventory (BPI). J Physiother. 2016 Jan;62(1):52.
- Noonan L, Burge S. Venous Leg Ulcers: Is Pain a Problem? Phlebology. 1/1998:14–9.
- Rutherford C, Nixon JE, Brown JM, Briggs M, Horton M. The Leeds Assessment of Neuropathic Symptoms and Signs Scale (LANSS) is not an adequate outcome measure of pressure ulcer-related neuropathic pain. Eur J Pain. 2016 Nov;20(10):1710–20.
- Kogure T, Sumitani M, Abe H, Hozumi J, Inoue R, Mietani K, et al. Ischemic Ulcer Pain Is Both Nociceptive and Neuropathic Pain Based on a Discriminant Function Analysis Using the McGill Pain Questionnaire. J Pain Palliat Care Pharmacother. 2017 Apr 3;31(2):98–104.
- Beaufait D, Nelson E, Landgraf J, Hayes R, Kirk J, Wasson J, et al. COOP measures of functional statues. In: Tools for primary care research. Newbury Park, Calif: Sage Publications; 1992. (Research methods for primary care).
- Nelson CR, Siegel AF. Parsimonious Modeling of Yield Curves. J Bus. 1987 Jan;60(4):473.
- Jensen MP, Karoly P. Self-Report Scales and Procedures for Assessing Pain in Adults. In: Turk DC, Melzack R, editors. Handbook of pain assessment. 3rd ed. New York: Guilford Press; 2011.
- Centre for Epidemiologic Studies Depression Scale (CES-D), NIMH [Internet]. [cited 2023 Oct 26]. Available from: http://www.chcr.brown.edu/pcoc/cesdscale.pdf
- Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl Psychol Meas. 1977 Jun;1(3):385–401.
- Boulet J, Boss MW. Reliability and validity of the Brief Symptom Inventory. Psychol Assess J Consult Clin Psychol. 1991 Sep;3(3):433–7.
- Abbott A. The Coping Strategy Questionnaire. J Physiother. 2010;56(1):63.
- Pergolizzi J, Ahlbeck K, Aldington D, Alon E, Coluzzi F, Dahan A, et al. The development of chronic pain: physiological CHANGE necessitates a multidisciplinary approach to treatment. Curr Med Res Opin. 2013 Sep;29(9):1127–35.
- The Leed Assessment of Neuropathic Symptoms and Signs (LANSS) Pain Scale. In [cited 2023 Oct 26]. Available from: https://www.researchgate.net/profile/Nick-Plunkett-2/publication/301483225/figure/fig2/AS:566832529711104@1512154814885/LANSS-scale-Reproduced-with-permission-of-M-Bennett-Source-Bennett-M-The-LANSS-Pain.png
- Bennett MI, Attal N, Backonja MM, Baron R, Bouhassira D, Freynhagen R, et al. Using screening tools to identify neuropathic pain. Pain. 2007 Feb;127(3):199–203.
- Palfreyman SJ, Tod AM, Brazier JE, Michaels JA. A systematic review of health-related quality of life instruments used for people with venous ulcers: an assessment of their suitability and psychometric properties. J Clin Nurs. 2010 Oct;19(19–20):2673–703.
- Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994 Mar;23(2):129–38.
- Song CY, Lin SF, Huang CY, Wu HC, Chen CH, Hsieh CL. Validation of the Brief Pain Inventory in Patients With Low Back Pain. Spine. 2016 Aug 1;41(15):E937–42.
- Caraceni A, Cherny N, Fainsinger R, Kaasa S, Poulain P, Radbruch L, et al. Pain Measurement Tools and Methods in Clinical Research in Palliative Care. J Pain Symptom Manage. 2002 Mar;23(3):239–55.
- Hjermstad MJ, Fayers PM, Haugen DF, Caraceni A, Hanks GW, Loge JH, et al. Studies Comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for Assessment of Pain Intensity in Adults: A Systematic Literature Review. J Pain Symptom Manage. 2011 Jun;41(6):1073–93.
- Tyler EJ, Jensen MP, Engel JM, Schwartz L. The reliability and validity of pain interference measures in persons with cerebral palsy. Arch Phys Med Rehabil. 2002 Feb;83(2):236–9.
- Euroqool [Internet]. [cited 2023 Oct 19]. EQ-5D. Available from: https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/
- Walters SJ, Morrell CJ, Dixon S. Measuring health-related quality of life in patients with venous leg ulcers. Qual Life Res. 1999;8(4):327–36.
- Woo K. Pain during dressing change: how does attachment style affect pain in the older adults? [Internet]. University of Toronto; 2009 [cited 2023 Dec 4]. Available from: https://tspace.library.utoronto.ca/bitstream/1807/17843/3/Woo_Kevin_Y_200906_PhD_thesis.pdf
- Magai C, Cohen CI. Attachment Style and Emotion Regulation in Dementia Patients and their Relation to Caregiver Burden. J Gerontol B Psychol Sci Soc Sci. 1998 May 1;53B(3):P147–54.
- Chlan L, Savik K, Weinert C. Development of a Shortened State Anxiety Scale From the Spielberger State-Trait Anxiety Inventory (STAI) for Patients Receiving Mechanical Ventilatory Support. J Nurs Meas. 2003 Dec;11(3):283–93.
- Barrett S. ‘Heal not hurt’: piloting an initiative on wound pain assessment. Br J Community Nurs. 2007 Jun;12(Sup3):S18–21.
- Maida V, Ennis M, Kuziemsky C. The Toronto Symptom Assessment System for Wounds: A New Clinical and Research Tool. Adv Skin Wound Care. 2009 Oct;22(10):468–74.
- Woo KY, Sibbald RG. The Improvement of Wound-Associated Pain and Healing Trajectory With a Comprehensive Foot and Leg Ulcer Care Model. J Wound Ostomy Continence Nurs. 2009 Mar;36(2):184–91.
- White RJ. Pain assessment and management in patients with chronic wounds. Nurs Stand. 2008 Apr 16;22(32):62–8.
- Frescos N. Assessment of pain in chronic wounds: A survey of Australian health care practitioners. Int Wound J. 2018 Dec;15(6):943–9.
- Leren L, Eide H, Johansen EA, Jelnes R, Ljoså TM. Background pain in persons with chronic leg ulcers: An exploratory study of symptom characteristics and management. Int Wound J. 2022 Oct;19(6):1357–69.
- Breuer B. Epidemiology of pain. In: Pappagallo M, editor. The neurological basis of pain. New York: McGraw-Hill, Medical Publ. Division; 2005.
- Turk DC, Melzack R, editors. Handbook of pain assessment. 3rd ed. New York: Guilford Press; 2011. 542 p.
- IASP Internation Association for the Study of Pain [Internet]. [cited 2023 Oct 19]. Faces Pain Scale – Revised. Available from: https://www.iasp-pain.org/resources/faces-pain-scale-revised/
- Dallam L, Smyth C, Jackson BS, Krinsky R, O’Dell C, Rooney J, et al. Pressure Ulcer Pain: Assessment and Quantification: J Wound Ostomy Continence Nurs. 1995 Sep;22(5):211–8.
- Freeman K. Pain measurement scales: A comparison of the visual analogue and faces rating scales in measuring pressure ulcer pain. J WOCN. 2001 Nov;28(6):290–6.
- Ren Y, Luo X, Xie C, Zhang P, Meng M, Song H. Assessment and management of pain during dressing change in patients with diabetic foot ulcers: a best practice implementation project. JBI Database Syst Rev Implement Rep. 2019 Oct;17(10):2193–201.
- Abbey J, Piller N, Bellis AD, Esterman A, Parker D, Giles L, et al. The Abbey pain scale: a 1-minute numerical indicator for people with end-stage dementia. Int J Palliat Nurs. 2004 Jan;10(1):6–13.
- Gouke C, Scherer S, Katz B, Gibson S, Farrel M, Bradbeer M. Pain in Residential Aged Care Facilities [Internet]. Australian Pain Society; 2005 [cited 2023 Nov 2]. Available from: www.apsoc.org.au/pdf/publications/pain_in_residential_aged_care_facilities_management_strategies.pdf
- Savvas S, Gibson S. Pain management in residential aged care facilities. Aust Fam Physician. 2015 Apr;44(4):198–203.
- Crellin DJ, Harrison D, Santamaria N, Babl FE. Systematic review of the Face, Legs, Activity, Cry and Consolability scale for assessing pain in infants and children: is it reliable, valid, and feasible for use? Pain. 2015 Nov;156(11):2132–51.
- Crellin DJ, Harrison D, Santamaria N, Babl FE. Comparison of the Psychometric Properties of the FLACC Scale, the MBPS and the Observer Applied Visual Analogue Scale Used to Assess Procedural Pain. J Pain Res. 2021 Mar;Volume 14:881–92.
- Peng T, Qu S, Du Z, Chen Z, Xiao T, Chen R. A Systematic Review of the Measurement Properties of Face, Legs, Activity, Cry and Consolability Scale for Pediatric Pain Assessment. J Pain Res. 2023 Apr;Volume 16:1185–96.
- King B, Barrett S. A clinical evaluation of 20 patients when using a new absorbent silicone foam wound dressing: Cutimed Siltec B. Wounds UK. 2018;14(3):76–81.
- Hegarty F, Wong M. Polymeric membrane dressing for radiotherapy-induced skin reactions. Br J Nurs. 2014 Nov 1;23(Sup20):S38–46.
- Seckam A. A multicentre, observational evaluation of the product characteristics of two absorbent foam dressings. Br J Nurs. 2019 Jun 27;28(12):S10–7.
- Alonso-Coello P, Oxman AD, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, et al. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: Clinical practice guidelines. BMJ. 2016 Jun 30;i2089.
- WHO – Palliative Care [Internet]. [cited 2023 Oct 19]. Available from: https://www.who.int/health-topics/palliative-care
- Yim E, Kirsner RS, Gailey RS, Mandel DW, Chen SC, Tomic-Canic M. Effect of Physical Therapy on Wound Healing and Quality of Life in Patients With Venous Leg Ulcers: A Systematic Review. JAMA Dermatol. 2015 Mar 1;151(3):320.
- Smith D, Lane R, McGinnes R, O’Brien J, Johnston R, Bugeja L, et al. What is the effect of exercise on wound healing in patients with venous leg ulcers? A systematic review. Int Wound J. 2018 Jun;15(3):441–53.
- Swanson T, Ousey K, Haesler E, Bjarnsholt T, Carville K, Idensohn P, et al. IWII Wound Infection in Clinical Practice consensus document: 2022 update. J Wound Care. 2022 Dec 1;31(Sup12):S10–21.
- LeBlanc K, Beeckman D, Campbell K. Prevention and management of periwound skin complications. Wounds International/ISTAP. 2021:1–21.
- Woo KY, Sibbald RG. Chronic Wound Pain: A Conceptual Model. Adv Skin Wound Care. 2008 Apr;21(4):175–88.
- Meaume S, Téot L, Lazareth I, Martini J, Bohbot S. The importance of pain reduction through dressing selection in routine wound management: the MAPP study. J Wound Care. 2004 Nov;13(10):409–13.
- Ramundo J, Gray M. Is Ultrasonic Mist Therapy Effective for Debriding Chronic Wounds? J Wound Ostomy Continence Nurs. 2008 Nov;35(6):579–83.
- Herberger K, Franzke N, Blome C, Kirsten N, Augustin M. Efficacy, Tolerability and Patient Benefit of Ultrasound-Assisted Wound Treatment versus Surgical Debridement: A Randomized Clinical Study. Dermatology. 2011;222(3):244–9.
- Chang YJR, Perry J, Cross K. Low-Frequency Ultrasound Debridement in Chronic Wound Healing: A Systematic Review of Current Evidence. Plast Surg. 2017 Feb;25(1):21–6.
- Stanisic MM, Provo BJ, Larson DL, Kloth LC. Wound Debridement with 25 kHz Ultrasound: Adv Skin Wound Care. 2005 Nov;18(9):484–90.
- Schoenbach SF, Song IC. Ultasonic debridement: a new approach in the treatment of burn wounds. Plast Reconstr Surg. 1980 Jul;66(1):34–7.
- Apelqvist J, Willy C, Fagerdahl AM, Fraccalvieri M, Malmsjö M, Piaggesi A, et al. EWMA Document: Negative Pressure Wound Therapy: Overview, Challenges and Perspectives. J Wound Care. 2017 Mar 1;26(Sup3):S1–154.
- Upton D, Andrews A. Pain and trauma in negative pressure wound therapy: a review: Pain and trauma in negative pressure wound therapy. Int Wound J. 2015 Feb;12(1):100–5.
- Upton D, Solowiej K. The impact of atraumatic vs conventional dressings on pain and stress. J Wound Care. 2012 May;21(5):209–15.
- Téot L, Lambert L, Ourabah Z, Bey E, Steenman C, Wierzbiecka E, et al. Use of topical negative pressure with a lipidocolloid dressing: results of a clinical evaluation. J Wound Care. 2006 Sep;15(8):355–8.
- Mittermayr R, Antonic V, Hartinger J, Kaufmann H, Redl H, Téot L, et al. Extracorporeal shock wave therapy (ESWT) for wound healing: Technology, mechanisms, and clinical efficacy: ESWT in wound healing. Wound Repair Regen. 2012 Jun;n/a-n/a.
- Zhang L, Weng C, Zhao Z, Fu X. Extracorporeal shock wave therapy for chronic wounds: A systematic review and meta-analysis of randomized controlled trials: Extracorporeal shock wave therapy for chronic wounds. Wound Repair Regen. 2017 Aug;25(4):697–706.
- Auersperg V, Trieb K. Extracorporeal shock wave therapy: an update. EFORT Open Rev. 2020 Oct;5(10):584–92.
- Dymarek R, Halski T, Ptaszkowski K, Slupska L, Rosinczuk J, Taradaj J. Extracorporeal shock wave therapy as an adjunct wound treatment: a systematic review of the literature. Ostomy Wound Manage. 2014 Jul;60(7):26–39.
- Klode J, Schöttler L, Stoffels I, Körber A, Schadendorf D, Dissemond J. Investigation of adhesion of modern wound dressings: a comparative analysis of 56 different wound dressings: Adhesion of wound dressings. J Eur Acad Dermatol Venereol. 2011 Aug;25(8):933–9.
- Derbyshire A. Using a silicone-based dressing as a primary wound contact layer. Br J Nurs. 2014 Nov 1;23(Sup20):S14–20.
- Beitz AJ, Newman A, Kahn AR, Ruggles T, Eikmeier L. A polymeric membrane dressing with antinociceptive properties: analysis with a rodent model of stab wound secondary hyperalgesia. J Pain. 2004 Feb;5(1):38–47.
- Davies SL, White RJ. Defining a holistic pain-relieving approach to wound care via a drug free polymeric membrane dressing. J Wound Care. 2011 May;20(5):250–6.
- Gefen A. Managing inflammation by means of polymeric membrane dressings in pressure ulcer prevention. Wounds Int. 2018;9(1):22–8.
- Kim YJ, Lee SW, Hong SH, Lee HK, Kim EK. The Effects of PolyMem(R) on the Wound Healing. Journal of the Koean Society of Plastic and Reconstructive Surgeons. 1999:1165–72.
- Tickle J. Positive clinical and patient outcomes with a nextgeneration foam dressing. Vol 12/2016(5):58–62.
- Seckam AM, Twardowska-Saucha K, Heggemann J, Süß-Burghart A, Augustin M. Clinical performance and quality of life impact of an absorbent bacteria-binding foam dressing. Br J Nurs. 2021 Mar 11;30(5):S21–30.
- Pearson WA, Prentice DA, Sinclair DL, Lim LY, Carville KJ. A novel topical therapy for resistant and early peristomal pyoderma gangrenosum. Int Wound J. 2019 Oct;16(5):1136–43.
- Liberato SMD, Souza AJGD, Costa IKF, Torres GDV, Vitor AF, Lira ALBDC. A enfermagem no manejo da dor em pessoas com úlcera venosa: revisão integrativa Nursing in the management of pain in people with venous ulcer: integrative review. Rev Pesqui Cuid É Fundam Online. 2016 Apr 4;8(2):4109–20.
- Van Hecke A, Grypdonck M, Defloor T. A review of why patients with leg ulcers do not adhere to treatment. J Clin Nurs. 2009 Feb;18(3):337–49.
- Weller CD, Buchbinder R, Johnston RV. Interventions for helping people adhere to compression treatments for venous leg ulceration. Cochrane Database Syst Rev. 2013 Sep 6;(9):CD008378.
- Gethin G, Probst S, Stryja J, Christiansen N, Price P. Evidence for person-centred care in chronic wound care: A systematic review and recommendations for practice. J Wound Care. 2020 Sep 1;29(Sup9b):S1–22.
- Thomas DC, Chui PL, Yahya A, Yap JW. Systematic review of patient education for pressure injury: Evidence to guide practice. Worldviews Evid Based Nurs. 2022 Aug;19(4):267–74.
- British Pain Society. Guidelines for Pain Management Programmes for Adults [Internet]. 2019 [cited 2023 Nov 2]. Available from: https://www.britishpainsociety.org/static/uploads/resources/files/Guidelines_for_PMP_01082019_xc33xiN.pdf
- Lindsay E. The Lindsay Leg Club Model: a model for evidence-based leg ulcer management. Br J Community Nurs. 2004 Jun;Suppl:S15–20.
- Green J, Jester R, McKinley R, Pooler A. Chronic venous leg ulcer care: Putting the patient at the heart of leg ulcer care. Part 1: exploring the consultation. Br J Community Nurs. 2018 Mar 2;23(Sup3):S30–8.
- Carlson M, Vigen CLP, Rubayi S, Blanche EI, Blanchard J, Atkins M, et al. Lifestyle intervention for adults with spinal cord injury: Results of the USC–RLANRC Pressure Ulcer Prevention Study. J Spinal Cord Med. 2019 Jan 2;42(1):2–19.
- Kane FM, Brodie EE, Coull A, Coyne L, Howd A, Milne A, et al. The analgesic effect of odour and music upon dressing change. Br J Nurs. 2004 Oct 1;13(Sup4):S4–12.
- Guidelines for Pain Management Programmes for adults: an evidence-based review prepared on behalf of the British Pain Society. London: The British Pain Society; 2013.
- Ashraf K, Haque M, Amir M, Ahmad N, Ahmad W, Sultan S, et al. An overview of phytochemical and biological activities: Ficus deltoidea Jack and other Ficus spp. J Pharm Bioallied Sci. 2021;13(1):11.
- Fox C. Honey as a dressing for chronic wounds in adults. Br J Community Nurs. 2002 Oct;7(10):530–4.
- Mwipatayi B, • Angel D, Norrish J, Hamilton M, Scott A, Sieunarine K. The use of honey in chronic leg ulcers: a literature review. Primary Intention. Vol 12/ 2004(3):107–12.
- Bardy J, Slevin NJ, Mais KL, Molassiotis A. A systematic review of honey uses and its potential value within oncology care. J Clin Nurs. 2008 Oct;17(19):2604–23.
- Dunford CE, Hanano R. Acceptability to patients of a honey dressing for non-healing venous leg ulcers. J Wound Care. 2004 May;13(5):193–7.
- Vandamme L, Heyneman A, Hoeksema H, Verbelen J, Monstrey S. Honey in modern wound care: A systematic review. Burns. 2013 Dec;39(8):1514–25.
- Yaghoobi R, Kazerouni A, Kazerouni O. Evidence for Clinical Use of Honey in Wound Healing as an Anti-bacterial, Anti-inflammatory Anti-oxidant and Anti-viral Agent: A Review. Jundishapur J Nat Pharm Prod. 2013 Jul 17;8(3):100–4.
- Oryan A, Alemzadeh E, Moshiri A. Biological properties and therapeutic activities of honey in wound healing: A narrative review and meta-analysis. J Tissue Viability. 2016 May;25(2):98–118.
- Anastasiou IA, Eleftheriadou I, Tentolouris A, Samakidou G, Papanas N, Tentolouris N. Therapeutic Properties of Honey for the Management of Wounds; Is There a Role in the Armamentarium of Diabetic Foot Ulcer Treatment? Results From In vitro and In vivo Studies. Int J Low Extrem Wounds. 2021 Dec;20(4):291–9.
- Vyhlídalová D, Kozáková R, Zeleníková R. Management of non-healing wounds with honey dressings: a literature review. Cent Eur J Nurs Midwifery. 2018 Sep 30;9(3):880–8.
- Yilmaz AC, Aygin D. Honey dressing in wound treatment: a systematic review. Complement Ther Med. 2020 Jun;51:102388.
- Dubhashi SP, Sindwani RD. A Comparative Study of Honey and Phenytoin Dressings for Chronic Wounds. Indian J Surg. 2015 Dec;77(Suppl 3):1209–13.
- Zeleníková R, Vyhlídalová D. Applying honey dressings to non-healing wounds in elderly persons receiving home care. J Tissue Viability. 2019 Aug;28(3):139–43.
- Rojczyk E, Klama-Baryła A, Łabuś W, Wilemska-Kucharzewska K, Kucharzewski M. Historical and modern research on propolis and its application in wound healing and other fields of medicine and contributions by Polish studies. J Ethnopharmacol. 2020 Nov;262:113159.
- Tsichlakidou A, Govina O, Vasilopoulos G, Kavga A, Vastardi M, Kalemikerakis I. Intervention for symptom management in patients with malignant fungating wounds – a systematic review. J BUON Off J Balk Union Oncol. 2019;24(3):1301–8.
- Ma X, Zheng C, Hu C, Rahman K, Qin L. The genus Desmodium (Fabaceae)-traditional uses in Chinese medicine, phytochemistry and pharmacology. J Ethnopharmacol. 2011 Nov;138(2):314–32.
- Li X, Xiao Q qing, Ze K, Li S, Wang Y fei, Zhou M, et al. External Application of Traditional Chinese Medicine for Venous Ulcers: A Systematic Review and Meta-Analysis. Evid Based Complement Alternat Med. 2015;2015:1–10.
- Anyanwu GO, Nisar-ur-Rehman, Onyeneke CE, Rauf K. Medicinal plants of the genus Anthocleista—A review of their ethnobotany, phytochemistry and pharmacology. J Ethnopharmacol. 2015 Dec;175:648–67.
- Ongarora BG. Recent technological advances in the management of chronic wounds: A literature review. Health Sci Rep. 2022 May;5(3):e641.
- Hofman D, Moore K, Cooper R, Eagle M, Cooper S. Use of topical corticosteroids on chronic leg ulcers. J Wound Care. 2007 May;16(5):227–30.
- Peplow PV, Chung TY, Baxter GD. Application of low level laser technologies for pain relief and wound healing: overview of scientific bases. Phys Ther Rev. 2010 Aug;15(4):253–85.
- Hart OR, Uden RM, McMullan JE, Ritchie MS, Williams TD, Smith BH. A study of National Health Service management of chronic osteoarthritis and low back pain. Prim Health Care Res Dev. 2015 Apr;16(02):157–66.
- Arumugam V, MacDermid JC, Walton D, Grewal R. Attitudes, knowledge and behaviors related to evidence-based practice in health professionals involved in pain management. Int J Evid Based Healthc. 2018 Jun;16(2):107–18.
- Jones ML, Greenwood M, Bielby A. Living with wound-associated pain: impact on the patient and what clinicians really think. J Wound Care. 2010 Aug;19(8):340–5.
- Zuccaro SM, Vellucci R, Sarzi-Puttini P, Cherubino P, Labianca R, Fornasari D. Barriers to Pain Management: Focus on Opioid Therapy. Clin Drug Investig. 2012 Feb;32:11–9.
- Mędrzycka-Dąbrowska W, Dąbrowski S, Gutysz-Wojnicka A, Basiński A, Kwiecień-Jaguś K. Nurses’ Knowledge and Barriers Regarding Pain Management. J Perianesth Nurs. 2018 Oct;33(5):715–26.
- Kuhlmann EH, Tallman BA. The Impact of Nurses’ Beliefs, Attitudes, and Cultural Sensitivity on the Management of Patient Pain. J Transcult Nurs. 2022 Sep;33(5):624–31.
- Elcigil A, Maltepe H, Eşrefgil G, Mutafoglu K. Nurses’ Perceived Barriers to Assessment and Managementof Pain in a University Hospital. J Pediatr Hematol Oncol. 2011 Apr;33(Supplement 1):S33–8.
- Rosén HI, Bergh IH, Odén A, Mårtensson LB. Patients´ Experiences of Pain Following Day Surgery – At 48 Hours, Seven Days and Three Months. Open Nurs J. 2011 Jul 6;5:52–9.
- Soyannwo OA. Enhancing effective pain control: the role of education. Pain Manag. 2011 Nov;1(6):487–9.
- Mitchell M. Home recovery following day surgery: a patient perspective. J Clin Nurs. 2015 Feb;24(3–4):415–27.
- Briggsl EV, Carrl ECJ, Whittakerl MS. Survey of undergraduate pain curricula for healthcare professionals in the United Kingdom. Eur J Pain. 2011 Sep;15(8):789–95.
- Briggs EV, Battelli D, Gordon D, Kopf A, Ribeiro S, Puig MM, et al. Current pain education within undergraduate medical studies across Europe: Advancing the Provision of Pain Education and Learning (APPEAL) study. BMJ Open. 2015 Aug;5(8):e006984.
- Shipton EE, Bate F, Garrick R, Steketee C, Visser EJ. Pain medicine content, teaching and assessment in medical school curricula in Australia and New Zealand. BMC Med Educ. 2018 Dec;18(1):110.
- Mankelow J, Ryan CG, Taylor PC, Casey MB, Naisby J, Thompson K, et al. International, multi-disciplinary, cross-section study of pain knowledge and attitudes in nursing, midwifery and allied health professions students. BMC Med Educ. 2022 Dec;22(1):547.
- Synnott A, O’Keeffe M, Bunzli S, Dankaerts W, O’Sullivan P, O’Sullivan K. Physiotherapists may stigmatise or feel unprepared to treat people with low back pain and psychosocial factors that influence recovery: a systematic review. J Physiother. 2015 Apr;61(2):68–76.
- Gardner T, Refshauge K, Smith L, McAuley J, Hübscher M, Goodall S. Physiotherapists’ beliefs and attitudes influence clinical practice in chronic low back pain: a systematic review of quantitative and qualitative studies. J Physiother. 2017 Jul;63(3):132–43.
- Gibbs MT, Morrison NMV, Marshall PWM. Biomedical Beliefs Explain the Clinical Decisions Made by Exercise-Based Practitioners for People With Chronic Low Back Pain. Spine. 2021 Jan 15;46(2):114–21.
- Ortiz MI, Cuevas-Suárez CE, Cariño-Cortés R, Navarrete-Hernández JDJ, González-Montiel CA. Nurses knowledge and attitude regarding pain: A systematic review and meta-analysis. Nurse Educ Pract. 2022 Aug;63:103390.
- Takahashi TT, Ornello R, Quatrosi G, Torrente A, Albanese M, Vigneri S, et al. Medication overuse and drug addiction: a narrative review from addiction perspective. J Headache Pain. 2021 Dec;22(1):32.
- Louw A, Nijs J, Puentedura EJ. A clinical perspective on a pain neuroscience education approach to manual therapy. J Man Manip Ther. 2017 May 27;25(3):160–8.
- Wong DL. Wong’s essentials of pediatric nursing. Eleventh edition. Hockenberry MJ, Wilson D, Rodgers CC, editors. St. Louis, Missouri: Elsevier; 2022.
- Abdel Rahman RN. Pressure Ulcer Assessment and Prevention in Oncology Settings : A Review. Middle East J Nurs. 2011 May;5(3):15–9.
- Physiopedia [Internet]. [cited 2023 Dec 15]. Short-form McGill Pain Questionnaire. Available from: https://www.physio-pedia.com/Short-form_McGill_Pain_Questionnaire
- Jensen MP, Keefe FJ, Lefebvre JC, Romano JM, Turner JA. One– and two-item measures of pain beliefs and coping strategies. Pain. 2003 Aug;104(3):453–69.
- Bouhassira D, Attal N, Alchaar H, Boureau F, Brochet B, Bruxelle J, et al. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain. 2005 Mar;114(1):29–36.
- Tulleners R, Brain D, Lee X, Cheng Q, Graves N, Pacella RE. Health benefits of an innovative model of care for chronic wounds patients in Queensland. Int Wound J. 2019 Apr;16(2):334–42.
