Volume 22 Number 1
The diabetic foot in hospitalised stroke patients: Documentation of nursing actions and the need for improvement
Ahmed Hussein, Magdalena A. Gershater
Keywords prevention, nursing, diabetic foot ulcers, diabetes mellitus, nursing documentation, Global Trigger Tool, stroke
DOI 10.35279/jowm202104.02
Abstract
Background Patients with diabetes and stroke have a high risk of injury to the paralysed side of the body, but are incapacitated and unable to maintain their self-care. In stroke units, registered nurses can assist patients through systematic assessments and nursing interventions, including preventive footcare.
Aim To explore the documentation of preventive nursing actions regarding the risk of developing foot ulcers in patients with diabetes and stroke at a neurology clinic’s inpatient ward.
Method A retrospective systematic review of computerised nursing records using the Global Trigger Tool (GTT). All records (n = 101) of patients with diabetes and stroke at the clinic between 1 January and 20 December 2015 were assessed. Descriptive statistics and manifest content analysis were used.
Results Median age: 78 years (41–93). Male/Female: n = 61/40. The records revealed insufficient documentation: Risk for foot ulcers was not documented in any of the records. The GTT showed that three patients had a documented foot ulcer, all with localisation on the same side in which the patient was paralysed. Documented nursing actions for foot ulcer prevention in bed were provided for 12 patients, but none were provided for patients sitting in a chair. Risk factors, according to the International Working Group of the Diabetic Foot, were found in 12 of the patients’ records. The nursing process was not mentioned in the records.
Conclusion Insufficient documentation indicates that the patients’ feet are not assessed and protected.
Implications for clinical practice The patients’ risk factors need to be addressed, and nurses need more education related to the diabetic foot.
Introduction
Over the course of the lifetime, a diabetes patient has a 25% risk of developing foot ulcers, and every 20 seconds, an amputation is performed somewhere in the world as a result of diabetes.1 Patients with dia-
betic foot ulcers often suffer from comorbidities such as ischemic heart disease, cerebrovascular disease, heart failure, proliferative retinopathy, uraemia, previous amputation and/or oedema.2 The most common background factor is diabetic neuropathy, which leads to decreased sensation in the lower extremities, muscle atrophy with foot deformities and diminished sweat secretions, which causes dry and cracked skin.3 The reduced sensation also makes it difficult for the patient to perceive pain after trauma; as a result, foot ulcers can occur due to minor trauma, such as kicking into the footrest or footboard of a wheelchair, or due to a developing pressure ulcer. For patients who are older, who have limited mobility, are bedbound or use a wheelchair (such as stroke patients), ulcers often occur in the heels as pressure ulcers.2,4 For patients with ischemia, the possibility of healing is reduced without the intervention of vascular surgery.2,3,5 A daily inspection of the feet is a cornerstone of patient education programmes about how to perform protective self-care activities.3 However, stroke most often results in the loss of or decreased ability to perform self-care and protect the feet independently. Previous studies of foot ulceration in stroke patients with diabetes are scarce. The prevalence of pressure ulcers (body parts undefined) has been reported to be as high as 22%.6 Registered nurses (RNs) working according to the nursing process can replace these deficiencies in self-care capacity and, if possible, help to develop patients’ capacity for self-care.7 They can also offer assisted self-care by educating nursing assistants or family members as needed. In specialised stroke units, RNs employed by inpatient wards can reduce the risk of damage to patients’ feet through off-loading in the bed or wheelchair, using foot creams and providing active oedema treatment. This process begins with regular foot inspections that can be performed while executing general nursing interventions. During the inspection, risk factors can be identified, and preventive nursing activities can be performed and documented.8 A comprehensive literature search of the PubMed, Cinahl, Google Scholar and Cochrane databases failed to uncover previous studies of the risk of foot ulcer in diabetes patients who have had a stroke. Our aim, therefore, was to explore the documentation of preventive nursing actions regarding the risk of developing any ulcers in the feet of patients with diabetes and stroke at a neurology clinic.
Methods and Materials
A retrospective descriptive review of computerised nursing records using the Global Trigger Tool (GTT)9 was conducted using both quantitative and qualitative approaches. The study was performed at the neurology clinic of a university hospital in southern Sweden. The clinic has several neurology and surgery wards and two observation divisions. All records from patients with stroke and diabetes (N = 101) who were treated at the clinic between 1 January and 20 December 2015 were systematically assessed.
Inclusion criteria
- Patients with a diagnosis of all types of stroke and all types of diabetes
- Hospitalised for more than 48 hours
- Age ≥ 18 years
Hospitals need a more effective method than self-reporting errors to identify events that cause harm to patients, in order to select and evaluate interventions for reducing harm. The GTT includes a list of known adverse events triggers and provides instructions for conducting a retrospective review of patient records using triggers to identify possible adverse events. It has been translated from English into Swedish.10 The GTT is used to conduct a systematic search of pre-defined criteria in a patient’s medical records that indicate a deviation from the normal care process. In the present study, only a minor part of the GTT was used, Care Criterion C9, which was originally developed for identifying triggers of pressure ulcers, but it can also be used for diabetic foot ulcers. This was used because corresponding instruments for diabetic foot ulcers were unavailable.
In addition to the GTT, factors that are known to cause foot injuries, according to the International Working Group on the Diabetic Foot’s (IWGDF) risk classification system3 were recorded in a free text format. Any documented foot ulcers were recorded; for example, the location, any preventative measures taken while the patient was in bed or in a wheelchair and the treatment of ongoing foot ulcers. The risk assessments carried out, or the presence of any pressure ulcers on other body parts, were also recorded. In addition, all patient records from physicians, RNs, physiotherapists and occupational therapists were read. The data were analysed using descriptive statistics (number and percentage) and manifest content analysis for the free text entries. Data were collected by the first author (AH). The second author (MAG) confirmed the data after the study was completed. The findings were also confirmed by a physician with longstanding experience with diabetic foot ulcers. None of the reviewers were involved in the clinical care of the patients whose records were assessed in the present study.
Ethical considerations
Reading patient records can be considered an intrusion on patients’ integrity, but no personal data were recorded, and the results are presented only at the group level. The study was performed to identify the risk factors of foot ulcers in a high-risk population, in hopes of improving patient safety for future patients at the clinic. The Regional Ethical Review Board in Lund, Sweden approved the study.
Results
During the study period, 853 stroke patients were treated at the clinic, of whom 136 (16%) also had a diagnosis of diabetes. There was no information at all about the patients’ feet in 35 of the records, so these were excluded from further analysis. Of the 101 remaining records, there was some foot-related information. There were 61 male patients and 40 female patients. The median age was 78 (41–93) years, and the median length of stay in the clinic was 10 (3–34) days. Fifty patients were paralysed on the right side (50%), and 51 (51%) on the left side. For patients with documented cases of ulcers on the feet (n = 3), the location of these ulcers were on the same side as the patient’s paralysis: right foot (n = 1), left foot (n = 2). These ulcers were pre-existing prior to the patients’ strokes. A manifest content analysis was performed as an examination of the records and revealed the generally insufficient state of the nursing documentation. A systematic risk assessment for foot ulcers was not documented in any of the 101 records, nor were there any other notes about the risk of foot injuries.
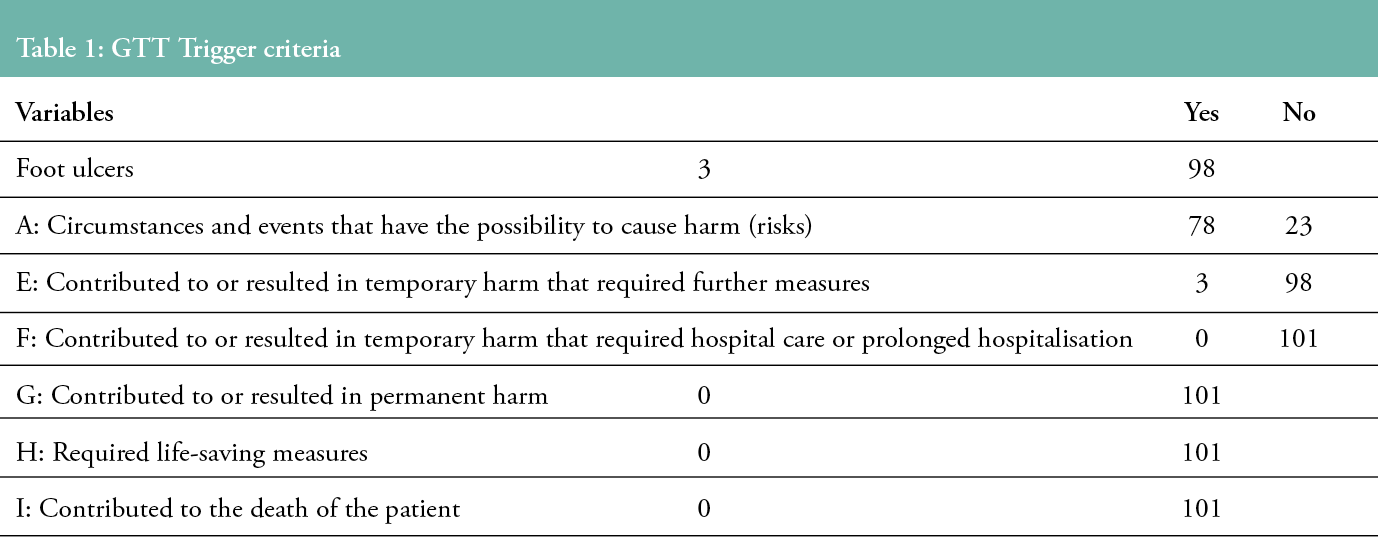
The total number of identified GTT C9 triggers was three patients with ongoing foot ulcers. There were 78 records with described risk factors and events that could cause a foot ulcer, and there were notes in three records that required measures such as a prolonged hospital stay and increased antibiotic treatment due to foot-related conditions (see Table 1).
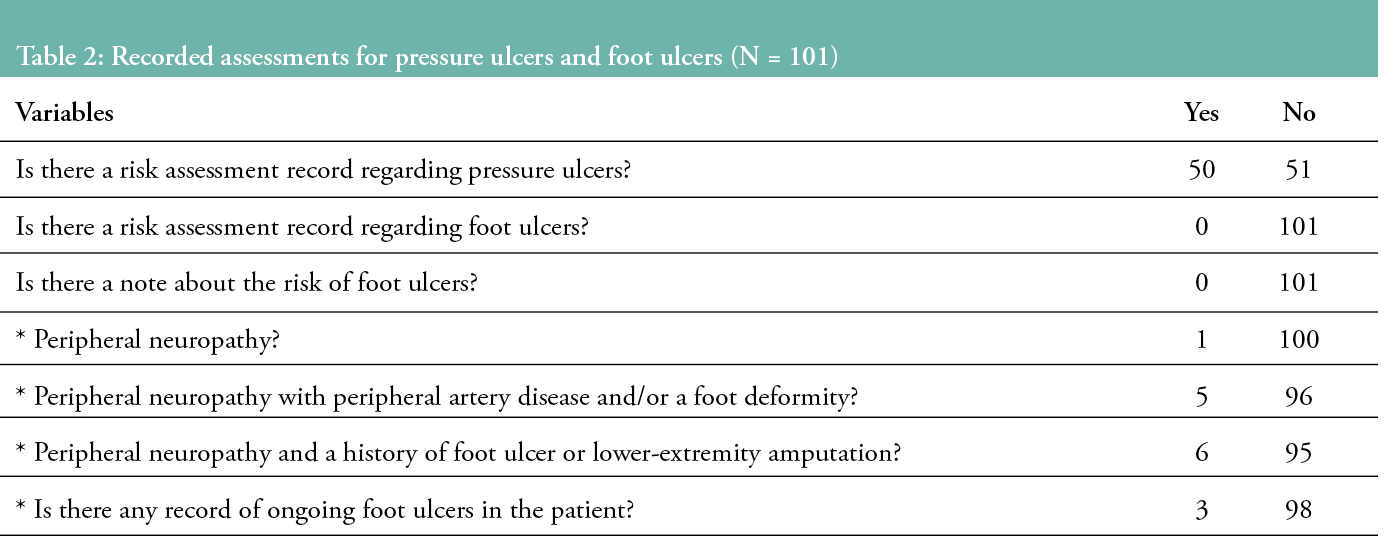
Half of the patients (n=50) were assessed for pressure ulcers according to the Norton scale.10 In one record, neuropathy was documented, five showed peripheral arterial disease and six noted a history of ulcers. These facts identified 12 patients as having risk factors for diabetic foot ulcers, as defined by the IWGDF’s3 risk classification system (see Table 2).
Documented interventions for preventing foot and pressure ulcers, such as off-loading and repositioning in bed, were found in 12 nursing records, but there were no notes regarding patients treated while in a seated position (chair or wheelchair) in any of the records. Documentation of the nursing process was not produced in any of the records.
Discussion
To our knowledge, this is the first study to use the GTT to identify foot ulcers in patients with diabetes and stroke. The GTT has been described as the most useful tool for searching for harm among hospitalised patients.12 It is able to identify more events compared to other evaluation methods,13,14 and it has good reliability, high specificity and a stable sensibility. However, the tool was not originally designed to assess the risk for diabetic foot ulcers.
The main weakness of the present study is the insufficient recording of patient records. The records showed that 16% of the stroke patients had a diabetes diagnosis, which is in line with previous estimates by Béjot and Giroud, who reported a diabetes prevalence of 10–20% in stroke patients.15 In terms of patient safety, it is a concern that 26% of the records of patients with diabetes mellitus and stroke had no notes regarding the feet. This needs to be improved, so that foot injuries in patients with diabetes and stroke can be detected.
This evaluation of the patients’ records revealed a lack of documentation regarding the assessment of feet in patients with stroke and diabetes. Thorough documentation is a crucial part of the evaluation of the quality of health care.16 Previous studies by Gershater17 and Gunningberg18 have revealed the widespread under-documentation of foot and pressure ulcers in patients with known risk factors. Lindahl stated that the evaluations should be made for all bedbound patients who are paralysed on one side, and for those with a neurological or cognitive illness.19 Moreover, this should be done within 24 hours after admission to the neurology ward. Berry and Raleigh also revealed insufficient documentation regarding foot status and the prevention of foot-related issues in long-term care settings, which may include several stroke patients with diabetes.20 Ribu revealed a lack of documentation even among patients who had an active ulcer.21 In patients who are bedbound with limited mobility, such as stroke patients, foot ulcers can appear on the heel.2,3 In the present study, the localisation of the foot ulcers was on the same side as the paralysis. This calls for the RNs to pay more attention to, observe and protect the paralysed areas of their patients’ bodies, as these patients are totally dependent on the nurse’s actions and interventions.
Given that stroke patients are critically ill, their nurses’ focus is likely on administering lifesaving procedures and treating neurological symptoms, rather than preventing ulcers on the feet. The extreme specialisation often found at university clinics calls for more interdisciplinary cooperation, and for nurses to focus on a holistic view of the patient, promoting health and preventing illness. Sometimes, this fails simply due to a lack of time in the nurses’ daily work; however, examining the feet to identify injuries or risk factors can be done quickly.22
The present study showed that only a few of the examined patient records described preventive measures regarding the off-loading of the foot in bed, and none recorded off-loading when the patient was in a wheelchair. This was also noted by Gunningberg.18 This is an area that needs to be improved in existing guidelines, so that foot ulcer prevention can be developed and evaluated.3,23
Another risk factor is injury to the foot on the paralysed side of the body, due to limited mobility.24 In the present study, the RNs used Norton to assess risk factors for pressure ulcers, but no similar instrument is available for diabetic foot ulcer assessment. One reason for these insufficient records may be that RNs are unaware of the importance of foot ulcer prevention for patients with high risk, and they may become confused about the different types of ulceration risk factors. This is an area in which the nurses’ professional role and responsibilities should be discussed. With more specialist nurses in medical care staff at the clinic, the documentation and systematic assessments of patients should increase. This, in turn, would increase the opportunities for good care. We recommend that future interview studies be conducted with nurses caring for this vulnerable patient group of people with diabetes and stroke.
The present study has revealed areas in need of improvement in specialised stroke units. The RNs working in inpatient wards can help by paying more systematic attention to the patients’ feet through regular foot inspections performed while carrying out general nursing interventions and while off-loading to and from a bed or wheelchair. They can also apply foot creams and perform active oedema treatment, followed by documentation. The limitation of the study was that data were collected from only one hospital, therefore the findings should be generalised with caution.
Key points
- Patients with diabetes and stroke are advanced in age, with comorbidities and unable to perform self-care of their feet; hence, they are dependent on others for this.
- RNs had not recorded any assessments of the feet, and assessments of pressure ulcers were largelymissing.
- Ongoing ulcers in the feet were all located on the paralysed foot.
- Shortfalls in the documentation and preventative work lead to risks to patients’ safety.
- Nurses working in specialised stroke units need improved professional knowledge regarding the systematic assessment of risk factors for foot ulceration.
Author(s)
Ahmed Hussein
RN, MScN, Diabetes Specialist Nurse
Magdalena A. Gershater
RN, PhD, Senior Lecturer, Faculty of Health and Society, Department of Care Science, Malmö University, Malmö, Sweden
Correspondence: magdalena.gershater@mau.se
Conflicts of Interest: None
References
- Boulton AJM, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J. The global burden of diabetic foot disease. The Lancet 2005; 366(9498):1719–24.
- Gershater M, Löndahl M, Nyberg P, Larsson J, Thörne J, Eneroth M, et al. Complexity of factors related to outcome of neuropathic and neuroischaemic/ischaemic diabetic foot ulcers: a cohort study. Diabetologia 2009; 52(3):398–407.
- International Working Group on the Diabetic Foot. IWGDF Guidelines on the prevention and management of diabetic foot disease. 2019. Available from: https://iwgdfguidelines.org/.
- Heinhold H, Westerfellhaus A, Kröger K. Prevalence of pressure ulcers in hospitalized patients in Germany – trends from 2005 to 2011. EWMA Journal 2014; 14(1):9–14.
- Chadwick P, Edmonds M, McCardle J, Armstrong D. Best practice guidelines: wound management in diabetic foot ulcers. Wounds International 2013; 1(9):7–20.
- Sackley C, Brittle N, Patel S, Ellins J, Scott M, Wright C, et al. The prevalence of joint contractures, pressure sores, painful shoulder, other pain, falls, and depression in the year after a severely disabling stroke. Stroke 2008; 39 (12) :3329–34.
- Orem DE. Nursing: concepts of practice. 6th ed. St. Louis: Mosby, 2001.
- Ilan R, Squires M, Panopoulos C, Day A. Increasing patient safety event reporting in 2 intensive care units: a prospective interventional study. Journal of Critical Care, 2011; 26(4):431–8.
- Institute for Healthcare Improvements (IHI). IHI global trigger tool for measuring adverse events. Cambridge, MA: IHI Publisher, 2015.
- Institute for Healthcare Improvement. Innovation series 2007 strukturerad journalgranskningför att identifiera och mäta förekomst av skador i vården enligt metoden Global Trigger Tool. Stockholm: Kommentus Förlag Publisher, 2008.
- Källman U, Lindgren M. Predictive validity of 4 risk assessment scales for prediction of pressure ulcer development in a hospital setting. Advances in Skin & Wound Care 2014; 27(2): 70–6.
- Carter M, Measuring harm levels with the Global Trigger Tool. Clinical Risk 2010; 16(4):122–6.
- Schildmeijer K, Aspects of retrospective record review – a matter of patient safety. Doctoral dissertation, Department of Health and Caring Sciences, Kalmar, Sweden: Linnaeus University, 2013.
- Doupi P, Svaar H, Bjørn B, Deilkas E, Nylèn U, Rutberg H. Use of the Global Trigger Tool in patient safety improvement efforts. Nordic experiences. Cognition, Technology & Work 2015; 17(1):45–54.
- Béjot Y, Giroud M. Stroke in diabetic patients. Diabetes Metabolism 2010; 36:S84–7.
- Moore Z, Johansen E, Van Etten M. A review of PU risk assessment and prevention in Scandinavia, Iceland and Ireland (part II). Journal of Wound Care 2013; 22(8): 423–31.
- Gershater M, Pilhammar E, Roijer C. Documentation of diabetes care in home nursing service in a Swedish municipality: A cross-sectional study on nurses’ documentation. Scandinavian Journal of Caring Sciences 2011; 25(2): 220–6.
- Gunningberg L, Ehrenberg A. Accuracy and quality in the nursing documentation of pressure ulcers. A comparison of record content and patient examination. Journal of Wound Ostomy Continence Nursing 2004) 31(6): 328–35.
- Lindahl E, Gilje F, Norberg A, Söderberg A. Nurses’ ethical reflections on caring for people with malodorous exuding ulcers. Nursing Ethics 2010; 17(6):777–90.
- Berry R, Raleigh ED. Diabetic foot care in a long-term facility. Journal of Gerontological Nursing 2004; 30(4): 8–13.
- Ribu E, Haram R, Rustøen T. Observations of nurses’ treatment of leg and foot ulcers in community health care. Journal of Wound, Ostomy and Continence Nursing, 2003; 30(6): 342–50.
- Gershater M, Pilhammar E, Alm-Roijer C. Prevention of foot ulcers in patients with diabetes in home nursing: a qualitative interview study. European Diabetes Nursing 2013; 10(2): 52–7.
- European Pressure Ulcer Advisory Panel. Prevention and treatment of pressure ulcers/injuries quick reference guide 2019. Available from: https://www.epuap.org/pu-guidelines/.
- Black, J. Preventing heel pressure ulcers. Nursing 2004; 34(11):17
