Volume 24 Number 1
Keeping feet in remission after healing of diabetic foot ulcers: a qualitative study of patients’ experiences
Magdalena Gershater, Ylva Wessman
Keywords diabetic foot ulcer, foot self-care, group sessions, qualitative study, re-ulceration
For referencing Gershater M, Wessman Y. Keeping feet in remission after healing of diabetic foot ulcers: a qualitative study of patients’ experiences. Journal of Wound Management 2023;24(1):10-17.
DOI
https://doi.org/10.35279/jowm2023.24.01.04
Submitted 7 October 2022
Abstract
Background Re-ulceration is common after healing of a diabetic foot ulcer (DFU) and patient education alone has not significantly reduced this risk. People living with diabetes and a DFU in remission often suffer from comorbidities and other diabetes-related complications. We wished to gain insights into these people’s experiences of living with feet in remission in order to understand how they prevent re-ulceration themselves.
Objective To explore experiences of people with diabetes regarding keeping feet in remission after healing of DFU.
Methods A qualitative explorative study was performed. A total of 49 people took part in participant-driven group sessions inspired by problem-based learning. The sessions were recorded and analysed by content analysis.
Results The overarching theme – feelings of frustration when losing self-determination in the footsteps of diabetes – was substantiated by four categories: 1) deeper insights of the need of prevention; 2) vulnerability to external factors; 3) reminders of daily limitations; and 4) recurring dependence on others.
Conclusion People living with diabetes and feet in remission expressed feelings of frustration. They experienced loss of self-determination in their lives and should be offered various educational interventions to adapt to daily challenges. Nurses in diabetes have an essential role in meeting these people’s complex and individual needs throughout life.
Implications for clinical practice Registered nurses should take patients’ feelings of frustrations into consideration when performing nursing interventions and educational activities for patients, next of kin and healthcare providers.
Key messages
- People living with diabetes and diabetic foot ulcer (DFU) in remission have a high risk of re-ulceration due to comorbidity and other diabetes-related complications.
- The aim was to explore experiences of people with diabetes mellitus with regard to keeping feet in remission after healing of DFU.
- They expressed feelings of frustration and loss of self-determination in their lives.
- Healthcare professionals (HCPs) should have this in mind when performing educational activities for patients, next of kin and HCPs.
Introduction
One of the primary goals of diabetes care is to prevent amputations as a consequence of diabetic foot ulcer (DFU) in people with diabetes1–3. After healing of a DFU, the foot is considered in remission; it is of utmost importance to avoid re-ulceration as previous ulceration is a significant risk factor for future ulceration4,5. Interventions to reduce the impact of diabetes foot complications have not yet been adequately proven, but different methods have been explored. The latest review on prevention of DFU suggests that “integrated foot care” may reduce the risk of a recurrent DFU5. It includes structured activities such as educational group sessions, regular follow-up visits, the use of appropriate footwear and, in some cases, reconstructive surgery5,6. In order to gain knowledge of what people with feet in remission need to handle, their own experience of living with feet in remission should be investigated.
The risk of developing DFU increases after a long duration of the disease7. The yearly incidence is estimated to be 2%, with the lifetime incidence between 19–34%5,6. The main background risk factors for development of DFU is diabetic peripheral neuropathy (DPN) with impaired sensation, muscle atrophy and reduced sweating1. Boulton et al8 and Chin et al9 have demonstrated that almost half of the people with diabetes experienced no symptoms of DPN, and consequently there may be a delay in recognition of a DFU. In a large study of 2489 patients with DFU7, 92% of the patients had DPN, thus stress ulcers and traumatic ulcers were common types of ulceration. This result indicates people’s unawareness of injuries to the feet and that ill-fitting shoes constitute important factors of the aetiology of DFU. Volmer-Thole and Lobmann10 described additional risk factors as triggering factors, including injuries from footwear, concussion damages, walking barefoot, cutting nails inappropriately, and poorly fitting socks and insoles.
People living with DFU often suffer from comorbidities such as cardiovascular diseases and diabetes-related complications9. They constitute a fragile group who need targeted foot preventive education11, particularly after experiencing a lengthy healing process from their recent DFU. This long period of healing has a negative impact of their quality of life12. Insufficient general knowledge in diabetes self-care, and specifically in foot care, could be one reason for the poor understanding of the necessity of foot self-care13–16.
According to present guidelines from the International Working Group on the Diabetic Foot (IWGDF)5, foot self-care should include: daily washing of the feet; careful drying between the toes; proper nail cutting; lubrication of the skin; daily foot inspections looking for redness, deformities and blisters; avoiding chemical agents or bandages for removing calluses; not walking barefoot indoors or outdoors; not wearing tight socks; and avoiding exposure of the feet to excessive cold or heat. These necessary tasks in foot self-care can be experienced as an extensive action beyond what has been perceived as diabetes self-care17.
Bus and van Netten18 showed that people with diabetes need continuous support to follow the advice of performing foot self-care when precipitating factors are assumed not to be resolved. They recommended identifying and highlighting existing barriers in self-care to help the people with diabetes find solutions. However, in another study by van Netten et al6, the participants described experiences of HCP providing contradictory self-care advice with regards to the choice of footwear. In summary, people living with diabetes tend to be left to themselves to solve their everyday challenges in keeping their feet undamaged.
Patient education
According to IWGDF guidelines5, people at risk of DFU should be offered a structured, organised and repeated education. A mixture of methods is recommended with either group sessions or individual encounters performed with a holistic approach by educators in diabetes care. The guidelines contain a detailed description of the aim and content of the education. Furthermore, the International Diabetes Federation (IDF)3 recommended that DFU preventive education should cover the following themes – motivation, methods of self-care, seeking help earlier, and social consequences. However, specifics of how this is supposed to be implemented were not presented.
Friberg and Hansson Scherman19 emphasised the need for pedagogical knowledge to sharpen critical reflection. Education should be based on the person’s life experiences, which could contribute to a complex and challenging learning situation. Williams and Pace20 suggested that problem-based learning (PBL) may offer an opportunity to influence people’s behaviour in chronic diseases, i.e. diabetes, asthma and arthritis. PBL is based on a lifetime perspective and emphasises awareness of changes over time. Nevertheless, there seems to be a limited number of studies that evaluated both the effect of education on re-ulceration in DFU5,21 and the personal experiences of living with DFU in remission. Previous qualitative studies have explored care-seeking behaviour, attitudes and knowledge15,16, but those studies have targeted persons with ongoing DFU. Life after healing therefore seems to have been an under-researched area.
Inspired by PBL, we assumed that patient-driven group education could identify people’s perceived problems by activating and reflecting on prior knowledge and past experiences13,24. The aim of the present study was to explore experiences of people with diabetes mellitus with regard to keeping feet in remission after healing of DFU.
Methods
This is a qualitative study using content analysis according to Berg26 of the experiences of persons with diabetes living with feet in remission after a DFU who participated in patient-driven group discussion22.
Participants and recruitment
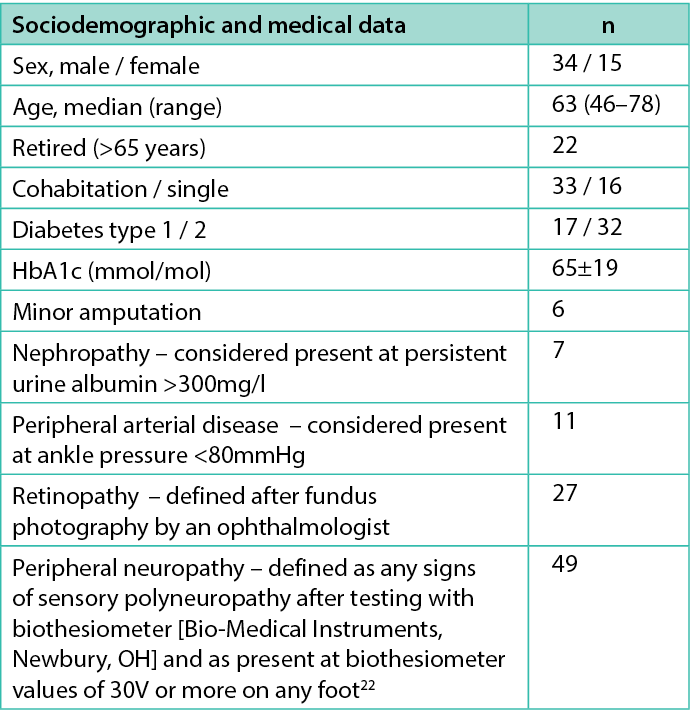
The participants in the present study were recruited from a diabetes foot clinic at a university hospital in Sweden and had been included in an RCT to evaluate the effects of patient education on re-ulceration22. After the healing of the DFU, all participants had been provided with adjusted shoes and individually fitted insoles for outdoor and indoor use and had been recommended regular visits to chiropodists. They also had been advised to contact the diabetes foot clinic in the event of any unexpected foot-related symptoms. A consecutive sampling was used, and people fulfilling the following inclusion criteria were invited to participate in the study: diabetes mellitus; DPN; age 35–79 years; and a healed DFU (Wagner grade ≥1) below the ankle, with or without minor amputations. A total of 61 people were allocated to group sessions, but only 49 took part due to logistical problems and health events (Table 1).
Table 1. Participant characteristics (n=49)
Study design
The participants were divided consecutively into ten groups for men and four groups for women, with two to five participants in each group. Each person participated on one occasion in one group session. In accordance with the findings of Hjelm et al23, separate groups for men and women were organised due to observations that men and women have different attitudes towards health perception, choice of shoes, and foot self-care. All sessions were held in a room at the diabetes foot clinic where they would not be disturbed, and they were led by a registered nurse experienced in diabetes and foot care (the second author).
The sessions began with socialising over fruit and coffee. The participants actively took part in discussions which began with the open question ‘Where do foot ulcers come from?’ followed by questions to each other and to the nurse. This allowed the participants to share their trajectory of ulceration and the healing process, thus creating trust in their own capability to manage different kinds of everyday situations. The session continued with the participants sharing their experiences with methods of self-care, how and when to seek help earlier, and social consequences. The conversations proceeded based upon the participants’ experiences of authentic situations, and questions and comments were occasionally addressed to the nurse who steered the conversation within these topics. Audio recordings were made of each session; duration varied from 60–75 minutes. The study was performed according to Consolidated Criteria for Reporting Qualitative Research (COREQ)24.
Ethical considerations
There is always a risk of violating personal integrity when people in a vulnerable group share their experiences. To overcome this, the participants were informed prior to the group sessions, verbally and in writing, about the study design, its voluntary nature, and confidentiality. Participants could withdraw at any time without consequences for future care. All participants signed informed consent documents. To ensure confidentiality, all personal identifiers were removed from the transcription. Neither of the authors had any previous relationship with the participants. The study was performed in accordance with World Medical Association(WMA) Declaration of Helsinki25 and approved by the Regional Ethical Board.
Data analysis
The audio-recorded data were transcribed ad verbatim and analysed with qualitative content analysis covering both manifest and latent levels. The first step of the process was an independent reading and rereading of the whole text. In the second step, the text was split into meaningful units and condensed without losing its core. This was done by the authors individually, then, after follow-up discussions, consensus was reached. The third step involved coding and analysing the data, minutely and with openness. Codes were developed and inductively identified in order to organise the data, and theoretical notes were written down. In the fourth step, the codes were grouped into subcategories, manifest level, by identifying similar phrases and patterns. Categories were developed by further organisation and interpretation of the data. The third and fourth steps required repeated discussions among the authors in order to reach an agreement. Finally, in the fifth step, an overarching theme was identified, the latent level26.
Results
Overarching theme
Feelings of frustration when losing self-determination in the footsteps of diabetes represent the overarching theme that permeated the participants’ stories of their experiences. Feelings of frustration grew from the increasing awareness of having had a poor understanding of the severity of DFU (with its increased risk of ulceration) and generally insufficient knowledge of how diabetes-related complications and comorbidity could impact their lives. They realised that it was necessary to prevent re-ulceration with regular foot self-care and use of appropriate footwear. These insights arose from their experiences during the strenuous and lengthy healing process, which was discussed during the group sessions.
Furthermore, the feelings of frustration were exacerbated by vulnerability to frequent and unavoidable external trauma and daily limitations when living with progressive DPN and impaired vision. The recurring dependence on others, with need for support from family and various diabetes-care professionals, was pronounced as an underlying frustrating element. The analysis is summarised in four categories and 13 subcategories (Figure 1) which are presented in italics under the associated category in the results.
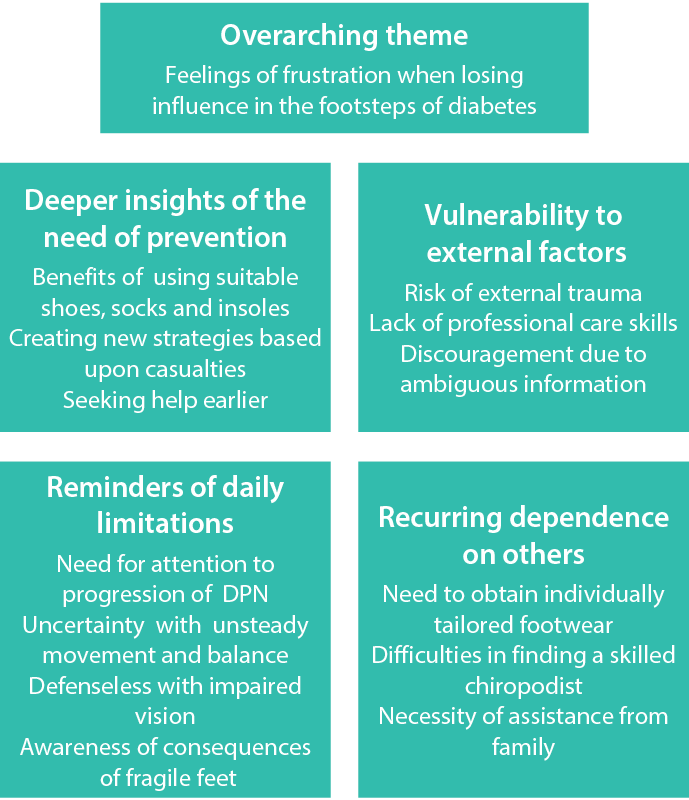
Figure 1
Category 1: Deeper insights of the need of prevention
The findings described their expressed frustration, but also a hint of enthusiasm as participants shared suggestions of self-care activities with each other. A new epoch in the participants’ lives was illuminated when they described how they realised their previous lack of understanding of the importance of foot-care. They now experienced a need for pragmatic, careful and recurrent foot-care, the choice of appropriate shoes, and their own plan of action which would lead them to seek help earlier. The subcategory ‘Benefits of using suitable shoes, socks and insoles’ illuminated frequent needs to preserve and manage the healed foot and the experiences of these advantages. According to one male [M] participant:
... it’s easy get hit on your feet... you don’t notice it... before I got these slippers... I hit the edges and legs of the bed, and chair legs... therefore, these slippers are so good – M1.
Another subcategory, ‘Creating new strategies based on casualties’, presented uncertainty about the causes of DFU and the impact of diabetes as a whole. The participants believed symptoms from DPN to be a primary cause of DFU and expressed the need to find new strategies to facilitate daily life:
... to lubricate the feet... you can put a small piece of plastic on the floor, put the ointment on it, and rub your foot in it – F1.
... I had a problem with those diabetic socks. They didn’t have elastic and bunched up under the foot like a crease... so I constantly stepped on it... and suddenly I had an ulcer – M6.
Participants’ awareness of the seriousness of their condition, where their own actions were not sufficient and they could require urgent support from others, was presented within the subcategory ‘Seeking help earlier’. The participants’ experiences involved a prolonged process of healing that affected everyday life and discussed how these experiences could be avoided:
... it is often pressure injuries and with reduced sensation. It is surprising when you take off the socks... you see blood coming there... then you bring out the little kit and apply what you have... and if it doesn’t work... you call the foot clinic the next day – M2.
Category 2: Vulnerability to external factors
This category represented threats that can easily expose fragile feet to new injuries. One example was a collision with a folding cart on the bus. Other external factors are injuries in the home environment that sometimes could have been prevented. The subcategory ‘Risk of external trauma’ includes common daily outdoor incidents such as accidents resulting from uneven pavement or being hit by a cart. Participants experienced this as a feeling of being exposed to uncontrollable events:
... my big toe erupted... it was red and swollen... I did not know what happened... I went four or five weeks before I was sent for an X-ray. The big toe was crushed... I imagine that I was run over by a folding cart on the bus... I just know it was very crowded – F2.
The participants also related experiences from lack of care skills or of misinformation from within the healthcare system. These experiences consistently generated feelings of frustration. Participants spoke of the subcategory ‘Lack of professional care skills’ where they encountered a lack of both experience and knowledge when seeking primary care for a DFU. The participants expressed a need for safe care as well as the feeling of being properly cared for:
... I feel that they [medical staff in primary care] do not have experience with older diabetic people who have three, four, or five concomitant diseases. They are not qualified enough for us – F3.
A further subcategory, ‘Discouragement due to ambiguous information’, included experiences of contradictory information about free of charge shoes and insoles, where the informants required equal and accurate care:
... I get mad for real. I know someone else who has gotten shoes for free, and I say this: ... either you should pay, or you should not – F5.
Category 3: Reminders of daily limitations
The participants were reminded daily of their diabetes and its consequences in form of complications. This was expressed as difficulties with lack of stability when moving, feeling defenceless when suffering from impaired vision, and the sense of not being well-dressed with nice shoes. The limitations could also be experienced as depressing, such as when a visit to the sauna with friends must be cancelled because new ulcers have suddenly been discovered. Furthermore, a classic situation is wearing new shoes while on vacation in warmer latitudes where the feet tend to swell, and a blood blister unexpectedly develops and ruins the vacation. Another important issue expressed by the participants regarding everyday life was the subcategory ‘Need for attention to progression of DPN’. Symptoms of DPN were a reminder to observe any changes in sensitivity of the feet, and thus the importance of daily inspections of the feet:
... we have no sensation in our feet because we have our nerve damage... so we do not feel that we have a rock in the shoe... even though we have shaken the shoe... and then the injury comes quite quickly – M3.
A feeling of insecurity when walking without assistance, and knowing that others would certainly notice this vulnerability, was presented in the subcategory ‘Uncertainty with unsteady movement and balance’. They expressed a feeling of embarrassment when they described their experiences of uncontrolled movement:
... it is a remarkable thing and I don’t know if I’m alone about it? I fall, over and over again, because I stumble... last week I lay flat on the ground outside the supermarket... and that’s not exactly what you want – F3.
Impaired vision increases the risk of accidents in and around the home, and participants repeatedly expressed feeling emotions relating to the subcategory ‘Defenceless with impaired vision’. This could be due to another diabetes-related complication, diabetic retinopathy. The male participants agreed that the worst threat to their freedom and self-confidence was losing their driver’s licence. Other situations could also be a challenge:
... it is difficult to climb stairs, for example... going up stairs goes well but down is a problem... then they (the steps) come together and I have to feel every step... and they are not marked – M4.
... to be able to care for [the feet], it is a prerequisite that you can see... – M5.
The participants described feelings relating to the subcategory ‘Awareness of consequences of fragile feet’ and the necessity of being alert and protecting their feet. The risk of a new DFU is a constant threat, but there may be a human tendency to ignore the consequences or an uncertainty about the seriousness of the situation:
... I didn’t know how serious it was because it took a while before I called... so now I know I need help... immediately! – M2.
Category: 4 Recurring dependence on others
The final category demonstrated that a need for individualised footwear, a well-trained chiropodist, and assistance from the family were necessary factors for keeping the feet in remission. The subcategory ‘Need to obtain individually tailored footwear’, represented the participants’ experiences of a variety of obstacles to obtaining personalised footwear. They described their needs for alternative shoes, but what they had been offered varied between the participants. Most had been offered a limited selection of designs and limited opportunities to try the shoes on, but a few participants had managed to obtain handmade shoes. Moreover, the female participants were frustrated by not being able to use nice shoes and feel well-dressed:
... I find it difficult to look in the catalogues and choose shoes. I want to be able to try them on... but they have no shoes you can try... surprised when you say that you have been given the opportunity to make decisions about the appearance of the custom-made shoes... there seems to be a big difference between orthopaedic technicians – F4.
The participants were aware of the importance of a skilled chiropodist. However, in the subcategory ‘Difficulties in finding a skilled chiropodist’, they wondered if the chiropodists had been trained specifically to work with people who have diabetes, and were uncertain about what expectations they should have. They shared information with each other about where to find a good chiropodist:
... so it is difficult to find someone [chiropodist] that is good... they claim to offer “medical foot care” but it’s not what I was told I needed... when I talked to them here [at the foot clinic] – M1.
The final subcategory, ‘Necessity of assistance from family’ could present the main element of dependence when living with fragile feet, where the people closest to the participant were deemed crucial:
... my wife takes care of my feet... cuts my nails... lubricates and ensures that there are no strange marks – M4.
Discussion
Despite suffering from complications and comorbidities, the participants in the present study tried to cope by learning important strategies to prevent re-ulceration, and they expressed frequent needs for adequate care from HCP. Our results correspond with Beattie et al13, where the participants expressed an overwhelming feeling of loss of control contributing to multifaceted impact in daily life. Furthermore, in the present study, the participants showed a persistent zest for life in spite of health conditions associated with comorbidities and the risk of re-ulceration. Continuous efforts to try to resolve daily problems were described. This finding contrasts with Beattie et al13 where a wider perspective of negative emotions could be a hindrance to activity. However, we agree with Greenwell et al27 who identified that the need for emotional management to overcome the feeling of frustration was an essential contribution within self-care. This is an area that needs further exploration.
A clear statement was revealed by the participants, that they did not have the overall picture of what to expect from a long life with diabetes and its complications. This issue is also elucidated in the study by Probst et al28, concerning people living with recurrent venous leg ulcers. Those participants confirmed insufficient knowledge of both general and specific nature pathophysiology and preventive self-care. A lack of understanding greatly complicates people’s outcome of foot self-care, where adherence and quality of life also could be affected. Diabetes education for people with long-standing diabetes should not just focus on metabolic control but also embrace a life-long perspective of the disease.
Armstrong et al4 claimed a need for a good understanding of the factors predicting re-ulceration. One of the most common obstacles for prevention of DFU is the lack of awareness of the association between diabetes and DPN and its impact on daily life21. This is in line with Wessman and Bahtsevani’s17 study showing a lack of awareness how symptoms of DPN could contribute to daily limitations and difficulties. Participants described pain, impaired sensations, and unsteady balance in the feet as hindrance. Unsteady movement and balance (and hence increased risk for trauma) can also be linked to another diabetes complication – retinopathy. The vast majority of the participants in the present study were diagnosed with retinopathy or had some other form of impaired vision. The participants’ frustration of loss of freedom, for example with reduced mobility and independence when no longer driving a car, has also been shown by Devenney and O’Neill29.
Coping strategies when living with diabetic vision loss stress the importance of acceptance as the first step towards solving the challenges of self-care30,31. The challenges of living with impaired vision need to be taken into consideration in all educational efforts for people with a diabetic foot in remission.
The participants in the present study often experienced a new DFU from minor trauma even though they tried to be aware of potentially dangerous situations, practise foot self-care, and follow the recommendations by wearing protective slippers every day. Waaijman et al33 conveyed that 63% of their participants were exposed to a new DFU. They stressed the importance of using selected shoe devices to protect and offload the pressure of the foot. Our findings show that the prescribed shoes could be experienced as ill-fitting, uncomfortable and unattractive, especially among the female participants. One strategy was to wear old, comfortable shoes with an awareness of increased risk of re-ulceration. Tan et al34 revealed that a holistic perspective is required to support security and acceptance among people with diabetes and high risk of DFU. Jarl et al35 suggested that HCP should pay more attention to women and their negative attitude toward therapeutic shoes. It seems valuable to highlight adaptation to therapeutic shoes as a medical intervention, not just an article of clothing. This needs to be developed further.
The impression that nurses and physicians in primary care had less experience and knowledge about DFU was described in the present study. The participants expressed new insight into the importance of seeking help early, needing to feel safe, and being provided with reliable information and care that specifically recognises their vulnerable feet. Our findings correspond to studies by Tan et al16 and Chithambo and Forbes36 where participants described how low awareness among both patients and HCP presented numerous obstacles that contributed to delay in seeking help for DFU. We assume that this request for adequate foot care within primary care might reflect differences in healthcare organisations between countries.
Further education for an extended group of nurses who care for this vulnerable group has been suggested7,22,32. In a study performed in the Nordic countries exploring implementation of clinical guidelines of DFU among HCP, only 39% of the respondents had implemented guidelines for treatment of DFU. Organisational problems and inadequate leadership were described which can contribute to a noticeably deteriorating quality of care37. Implementation of clinical guidelines is a prerequisite for evidence-based care and for preventing DFU and re-ulceration.
Another topic that influenced the participants was dependence on support in self-care from relatives and HCP. These experiences are consistent with findings by Meric et al31 which indicated extended difficulties when becoming dependent on others and a feeling of losing control over their lives. Our participants shared these experiences with the additional underlying feeling of being without the necessary support and thus at risk of new DFU. Leksell38 concluded from studies of blind diabetic participants that their own abilities, empowerment and resources need to be highlighted in diabetes care. This conclusion can illustrate that HCP should make opportunities visible instead of just focusing on obstacles when performing person-centred diabetes care. Finally, Delmar et al39 showed that self-control and self-reliance are meaningful values when living with a chronic disease. These issues are important to discuss during the visits to illustrate the all-embracing phenomena when living with any chronic condition.
We concur with Hicks et al40 who suggested group sessions as supportive prevention for people in remission from DFU. We find that these group sessions could maintain a deeper understanding of the overall picture of both diabetes disease and DFU. Coffee et al14 recommended individualised education rather than “one-size-fits-all”. Their findings advocate improved communication between the person and HCP and emphasised the importance of the person’s own decision-making. Recommendations partly concern person-centred care, but they need to be supplemented by a deeper approach in the learning process.
Friberg and Hansson Scherman19 discussed the need to abandon behaviourism and the concept of compliance in education and welcome pedagogical knowledge. The objective is to reach the person in their current life situation with a chronic disease. They suggest ignoring old manners of compliance and creating conditions with a new approach with the person participating in a life-long learning process. Vatankhah et al41 questioned if a repeated face-to face pedagogical method with written and oral components could be effective as a preventive method. The results showed a great impact on both improved knowledge and practice of foot self-care. Education was repeated after 6 months; this might emphasise the important of repetitive pedagogical interventions.
Gökdeniz and Şahin42 reported that some behavioural changes can be observed if the person acquires knowledge of foot care, makes the appropriate changes in foot care behaviour, and receives more knowledge of self-care in diabetes. To meet the individualised needs, we propose early and repeated education for these people. Group sessions inspired by PBL could be an option for the participants to learn from each other’s experiences and embrace person-centred care.
Finally, we must reconsider that these people are a high-risk population for re-ulceration and constitute a vulnerable group. They experience limitations and need to adapt to the consequences of diabetes, both DPN and retinopathy. All efforts to reduce re-ulceration are of great importance and should be targeted at the needs of each person11. Bus and van Netten18 expressed their powerful commitment by stressing an urgent need for further interventions to accommodate the rising need of both primary and secondary prevention of DFU.
Limitations
The aim of the study was not to separate people living with type 1 or type 2 diabetes. The advantage of dividing could be to focus on the insights from the life-long perspective of people with type 1 diabetes, which we propose for future studies. The study was conducted in 2008–2009; however, few studies on this topic have been published and the result is relevant for development of future patient education interventions to prevent ulceration and re-ulceration in the diabetic foot.
Trustworthiness was described as the enriched findings by quotations from the original material to elucidate confirmability. To strengthen credibility, the authors had continuing discussions throughout the process of analysis, where the process was discussed in detail. Finally, the results of the study represented a limited number of participants from a small study area and probably cannot be transferred to other contexts.
Conclusion
We need to remember that people living with diabetes and DFU in remission have a high risk of re-ulceration due to comorbidity and diabetes-related complications. They expressed feelings of frustration and experienced loss of self-determination in their lives. Patient-centred care requires that HCPs take these experiences into consideration when designing tailor-made education and introduce elements of support to meet those unmet needs that create the frustration. Various educational strategies and collaborators with pedagogical elements are needed to accommodate people in their crucial efforts adapting to daily challenges.
Implications for clinical practice or future research
- HCPs should take patients’ feelings of frustrations into consideration when performing nursing interventions and educational activities for patients, next of kin and HCPs.
- We promote an individualised approach as all people with diabetes represent unique lives with unique needs and not simply a diagnosis. For this reason, it might be fruitful to offer individual sessions in addition to or instead of group sessions. The individual sessions could be comprised of face-to-face intervention with a person-centred approach. For those people who wish to join in a group session inspired by PBL, it seems that the participants obtained benefits by exchanging experiences and advice with each other.
- Studies evaluating patient education intervention should be designed in consultation with those targeted for the intervention and should be based on educational theory.
Acknowledgement
We would like to express our gratitude to the participants for their interest in our study.
Conflict of Interest
The authors declare no conflicts of interest.
Funding
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
The design of the study was developed by the second author (MAG) in close collaboration with the diabetes foot team. The second author also conducted and led the group sessions. Both authors (YW, MAG) analysed the data and discussed the drafts until consensus. Both authors (YW, MAG) read and approved the final manuscript.
Appendix
https://doi.org/10.1093/intqhc/mzm042 COREQ
We confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story.
Author(s)
Magdalena Gershater*1, Ylva Wessman2
1Malmö Universitet, Malmö, Sweden
2Care Science Malmö University, Faculty of Health and Society, Malmö, Sweden
*Corresponding author email magdalena.gershater@mau.se
References
- American Diabetes Association (ADA). Management of diabetic foot complications; 2018 [cited 2022 Sep 18]. Available from: https://professional.diabetes.org/sites/professional.diabetes.org/files/media/foot_complications_monograph.pdf
- National Board of Health and Welfare. National guidelines on diabetes; 2018 [cited 2022 Sep 18]. Available from: https://www.socialstyrelsen.se/kunskapsstod-och-regler/regler-och-riktlinjer/nationella-riktlinjer/riktlinjer-och-utvarderingar/diabetes/om-riktlinjerna/
- International Diabetes Federation (IDF). The diabetic foot; 2020 [cited 2022 Sep 18]. Available from: https://www.idf.org/our-activities/care-prevention/diabetic-foot.html
- Armstrong DG, Boulton AJM, Bus S. Diabetic foot ulcers and their recurrence. N Engl J Med 2017;376(24):2367–2374. doi:10.1056/NEJMra1615439
- International Working Group on the Diabetic Foot (IWGDF). Guidelines; 2019 [cited 2022 Sep 18]. Available from: https://iwgdfguidelines.org/guidelines/guidelines/.
- van Netten JJ, Raspovic A, Lavery LA, Monteiro-Soares M, Rasmussen A, Sacco ICN, Bus SA on behalf of the International Working Group on the Diabetic Foot (IWGDF). Prevention of foot ulcers in the at-risk patient with diabetes: a systematic review. Diabetes Metab Res Rev (Suppl.) 2019;1–22 [cited 2022 Sep 18]. Available from: https://iwgdfguidelines.org/wp-content/uploads/2020/03/van-Netten_et_al-2020-IWGDF-prevention-systematic-review.pdf
- Gershater MA, Löndahl M, Nyberg P, Larsson J, Thörne J, Eneroth M, Apelqvist J. Complexity of factors related to outcome of neuropathic and neuroischaemic/ischaemic diabetic foot ulcers: a cohort study. Diabetologia 2008;52(3):398–407. doi:10.1007/s00125-008-1226-2
- Boulton AJ, Vileikyte L, Ragnarsson-Tennvall G, Apelqvist J. The global burden of diabetes foot disease. Lancet 2005;366(9498):1719–1724. doi:10.1016/S0140-6736(05)67698-2.
- Chin YF, Huang TT, Hsu BR. Impact of action cues, self-efficacy and perceived barriers on daily foot exam practice in type 2 diabetes mellitus patients with peripheral neuropathy. J Clin Nurs 2012;22(1–2):61–68. doi:10.1111/j.1365-2702.2012. 04291.x
- Volmer-Thole M, Lobmann R. Neuropathy and diabetic foot syndrome. Int J Mol Sci 2016;17(6):1–11. doi:10.3390/ijms17060917
- Lincoln NB, Radford KA, Game FL, Jeffcoate WJ. Education for secondary prevention of foot ulcers in people with diabetes: a randomized controlled study. Diabetolog 2008;51:1954–1961. doi:10.1007/s00125-008-1110-0
- Hjelm K, Apelqvist J. Influence of beliefs about health and illness on self-care and care-seeking in foreign-born people with diabetic foot ulcers: dissimilarities related to origin. J Wound Care 2016;25(11):602–616. doi:10.12968/jowc.2016.25.11.602
- Beattie AM, Campbell R, Vedhara K. ‘What ever I do it’s lost cause’. The emotional and behavioural experiences of individuals who are ulcer free living with the threat of developing further diabetic foot ulcers: a qualitative study. Health Expect 2012;17:429–439. doi:10.1111/j.1369-7625.2012.00768.x
- Coffey L, Mahon C, Gallagher P. Perceptions and experiences of diabetic foot ulceration and foot care in people with diabetes: a qualitative meta-synthesis. Int Wound J 2018;16:183–210. doi:10.111/iwj.13010
- Oni D. Foot self-care experiences among patients with diabetes: a systematic review of qualitative studies. Wound Manag Prev 2020;66(4):16–25. doi:10.25270/wmp.2020.4.1625.
- Tan TW, Crocker RM, Palmer KNB, Gomez C, Armstrong DG, Marrero DG. A qualitative study of barriers to care-seeking for diabetic foot ulceration across multiple levels of the healthcare system. J Foot Ankle Res 2022;15(1):56. doi:10.1186/s13047-022-00561-4.
- Wessman Y, Bahtsevani C. Living with challenges in the shadow of diabetes: an interview study among adults with diabetic peripheral neuropathy. NJNR 2019;40(2):1–8. doi:10.1177/2057158519881751
- Bus SA, van Netten JJ. A shift in priority in diabetic foot care and research: 75% of foot ulcers are preventable. Diabetes Metab Res Rev 2016;32(suppl.1):195–200. doi:10.1002/dmrr.2738
- Friberg F, Hansson Scherman M. Can a teaching and learning perspective deepen understanding of the concept of compliance? A theoretical discussion. Scand J Caring Sci 2005;19(3):274–279. doi:10.1111/j.1471-6712.2005. 00341.x
- Williams B, Pace AE. Problem based learning in chronic disease management: a review of the research. PEC 2009;77:14–19. doi:10.1016/j.pec.2009.03.004
- Dorresteijn JA, Kriegman DM, Assendelft WJ, Valk GD. Patient education for preventing diabetic foot ulceration. Cochrane Databases Syst Rev 2014;16(12). doi:10.1002/14651858.CD001488.pub5
- Gershater MA, Apelqvist J, Alm Roijer C. Re-ulceration is common in persons with diabetes and healed foot ulcer after participant-driven education in group: a randomized controlled trial. Adv Wound Care 2023 Mar;12(3):117–126. doi:10.1089/wound.2021.0007
- Hjelm K, Nyberg P, Apelqvist J. Gender influences beliefs about health and illness in diabetic subjects with severe foot lesions. J Adv Nurs 2002;40(6):673–684. doi:10.1046/j.1365-2648.2002.02427.x
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. IJQH 2007;19(6):349–357. doi:10.1093/intqhc/mzm042
- World Medical Association. WMA Declaration of Helsinki: ethical principles for medical research involving human subjects; 2013 [cited 2022 Sep 18]. Available from: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/
- Berg BL. Qualitative research methods-for the social sciences. 7th ed. Boston, MA: Pearson; 2009.
- Greenwell K, Sivyer K, Vehara K, Yardley L, Game F, Chalder T, Richards G, Drake N, Gray N, Weinman J, Bradbury K. Intervention planning for the REDUCE maintenance intervention: a digital intervention to reduce re-ulceration risk among patients with a history of diabetic foot ulcers. BMJ Open 2018;8(5):1–11. doi:10.1136/bmjopen-2017-019865
- Probst S, Séchaud L, Bobbink P, Buerhrer Skinner M, Weller CD. The lived experience of recurrence prevention in patients with venous leg ulcers: an interpretative phenomenological study. J Tissue Viability 2020;29(3):176–179. Available from: https://pubmed.ncbi.nlm.nih.gov/31974010/
- Devenney R, O’Neill S. The experiences of diabetic retinopathy: a qualitative study. BJHP 2011;16:707–721. doi:10.1111/j2044-8287.201002008.x
- Sturrock BA, Rees G, Lamoureux EL, Wong TY, Holloway E, Fenwick EK. Individuals’ perspectives on coping with vision loss from diabetic retinopathy. Optom Vis Sci 2018;95(4):362–372. doi:10.1097/OPX.0000000000001209
- Meric M, Ergun G, Meric C, Demirci I, Azal Ö. It is not diabetic foot: it is my foot. J Wound Care 2019;28(1):30–37. doi:10.12968/jowc.2019.28.1.30.
- Gershater MA, Pilhammar E, Alm Roijer C. Documentation of diabetes care in home service in a Swedish municipality: a cross-sectional study on nurses’ documentation. Scand J Caring Sci 2011;25(2):220–2. doi:10.1111/j.1471-6712.2010. 00812.x
- Waaijmann R, de Haart M, Arts M, Wever D, Verloux AJWE, Nollet F, Bus SA. Risk factors for plantar foot ulcers recurrence in neuropathic diabetic patients. Diabetes Care 2014;37(6):1697–1705. doi:10.2337/dc13-2470
- Tan S, Horobin H, Tunprasert T. The lived experience of people with diabetes using off-the-shelf prescription footwear in Singapore: a qualitative study using interpretative phenomenological analysis. J Foot Ankle Res 2019;12(19):1–12. doi:10.1186/s13047-019-0329-y
- Jarl G, Alnemo J, Tranberg R. Gender differences in attitudes and attributes of people using therapeutic shoes for diabetic foot complications. J Foot Ankle Res 2019;12(21):1–7. doi:10.1186/s13047-019-0327-0
- Chithambo T, Forbes A. Exploring factors that contribute to delay in seeking help with diabetes related foot problems; a preliminary qualitative study using Interpretative Phenomenological Analysis. IDN 2015;12(1):20–26. doi:10.1179/2057331615Z.0000000006
- Gershater MA, Kirketerp-Møller K, Juutilainen V, Julsrud Berg T, Löndahl M. The use of clinical guidelines during the treatment of diabetic foot ulcers in four Nordic countries. EWMA J 2016;16(2):23–26. Available from: https://www.diva-portal.org/smash/get/diva2:1401734/FULLTEXT01.pdf
- Leksell J. Diabetes-related blindness: studies of self-management, empowerment and health [doctoral dissertation]. Sweden: University of Uppsala; 2005. Available from: https://www.avhandlingar.se/avhandling/1c904ccef2/
- Delmar C, Bøje T, Dylmer D, Forup L, Jacobsen C, Møller M, Sønder H, Pedersen BD. Independence/dependence: a contradictory relationship? Life with a chronic illness. Scand J Caring Sci 2006;20(3):261–268. doi:10.1111/j.1471-6712.2006.00403.x
- Hicks CW, Canner JK, Mathioudakis N, Lippincott C, Sherman RL, Abularrage CJ. Incidence and risk factors associated with ulcer recurrence among patients with diabetic foot ulcers treated in a multidisciplinary setting. J Surg Res 2020;246:243–250. doi:10.1016/j.jss.2019.09.025
- Vatankhah N, Khamseh ME, Noudeh YJ, Aghili R, Baradaran HR, Haeri NS. The effectiveness of foot care education on people with type 2 diabetes in Tehran, Iran. Prim Care Diabetes 2009;3(2):73–77. doi:10.1016/j.pcd.2009.05.003
- Gökdeniz D, Şahin ZA. Evaluation of knowledge levels about diabetes foot care and self-care activities in diabetes individuals. Int J Low Extrem Wounds 2020;Jul(27):1–10. doi:10.1177/1534734620926266
