Volume 24 Number 2
Diabetic foot ulcer patients’ and clinicians’ experiences of care transitions from hospital to home: a study protocol
Carole Guex
Keywords qualitative research, diabetic foot, lived experiences, transition of care, care transitions
For referencing Guex C et al. Diabetic foot ulcer patients’ and clinicians’ experiences of care transitions from hospital to home: a study protocol. Journal of Wound Management 2023;24(2):26-29.
DOI
https://doi.org/10.35279/jowm2023.24.02.07
Submitted 30 June 2023
Accepted Accepted 3 July 2023
Abstract
Background Foot ulcers are an important cause of multiple hospitalisation and clinical complications in patients with diabetes. Before hospital discharge, the care transition should be planned across multiple care settings. Many problems occur during care transitions, resulting in negative patient outcomes and unnecessary readmissions.
Aim This paper presents a protocol for a qualitative study exploring the experience of care transitions from both patients’ and clinicians’ perspectives in a regional hospital context in Western Switzerland.
Methods design A qualitative descriptive design will be used to solicit patients‘ and clinicians’ perceptions of care transitions. Semi-structured interviews will be conducted with six patients with a diabetic foot ulcer (DFU) and six community nurses. Data will be analysed according to Braun and Clarke’s thematic analysis.
Discussion Exploring participants’ experiences will afford information about their role within the process, any barriers to effective care transitions, and any strategies to overcome.
Implication for clinical practice The findings of this study will be pivotal to informing and developing new and enhanced transition planning for people with DFU, with the ultimate goal of improving patient outcomes, reducing hospital readmissions and enhancing cost savings. Additionally, this study takes a unique approach as it seeks experiences of both the patient and the clinician and is in alignment with the EWMA project Living with chronic wounds.
Key messages
- This is a study protocol for a qualitative research including six diabetic foot ulcer (DFU) patients and six clinicians.
- Its aim is to explore the lived experiences of both DFU patients and clinicians during care transitions from hospital to home.
Introduction
Diabetes is a complex disease affecting around 425 million people worldwide1. This illness frequently leads to several complications such as retinopathy, neuropathy, renal and cardiovascular diseases2. One of the most severe complications is the development of a diabetic foot ulcer (DFU), often leading to multiple hospitalisations3. Approximately 15% of diabetic patients experience a DFU once in their lifetime4. Once healed, DFUs reoccur in 40% of patients within 1 year5. The reasons for this high recurrence appear to be linked to the pathophysiology and/or patients’ and clinicians’ behaviour6. A DFU reduces patients’ quality of life and can lead to lower extremity amputation or even death7. Such a wound is a burden, not only for the affected individuals, causing suffering and requiring expensive treatments, but also for their close relatives and the society as a whole8. Due to their complexity, these wounds necessitate a multidisciplinary team approach to provide comprehensive wound care within the different care settings9,10.
Patients with DFUs being discharged from the hospital to their home require a coordinated care plan involving the entire multidisciplinary team11 as its absence can lead to fragmented care and decreased quality of care12,13. Moreover, a poorly managed care transition from hospital to home increases both healthcare costs and adverse events such as amputations11,13. Tasks associated with care transitions are complex and thus require a multifaceted approach and coordinated care to improve quality and health outcomes3,14.
Ensuring a high level of person- and family-centred care is one particularly important aspect for improving quality and health outcomes during care transitions11,15. It has been shown that, with appropriate support, progressively more patients with DFUs can be treated with additional advanced healthcare interventions at home, thus improving their quality of life and reducing costs16. However, today’s healthcare system is mainly designed around an acute care paradigm. The main focus is to treat the acute health issue and not the chronic condition. Therefore, too often individuals with DFUs are discharged from acute care settings without proper care planning, with the consequence of being readmitted within a short time. Recent literature has widely explored the transition of care, with studies assessing the efficacy of discharge interventions17,18 or assessment tools for improving the discharge preparation19. Additionally, care transitions have typically been examined focusing on specific provider groups, such as nurses, physicians and patients, rather than combining the perspectives and experiences of multiple groups of people20. We therefore present a protocol aiming to explore the experiences of hospital-to-home transitions from the standpoints of both individuals with DFUs and nurses with regard to the use of coordinated transition care plans, the quality of care, and the way the hospital discharge is managed in a Western Switzerland care setting.
Methods
We will use a qualitative descriptive design in which the philosophical assumptions guiding researchers’ attitudes are embedded in an interpretive position21. A total of 12 individuals will be included – six patients with DFUs and six nurses. The Ethical Committee of the Canton of Vaud approved this study (CER-VD: 2021-02181). All participants will provide verbal consent prior to starting the interviews. To protect anonymity, fictional names will be used throughout the publication of the results.
Recruitment
Individuals with DFU
Male and female individuals with open DFUs who have been discharged from a regional hospital in Western Switzerland and are receiving care at home will be recruited. We will include adults aged 18 and older, having an existing diagnosed open DFU, having been discharged from the hospital during the last 3 weeks and having proficiency in the French language. We will exclude individuals unwilling or unable to provide consent.
Community nurses
Additionally, we will include community nurses from a homecare association having proficiency in the French language and who care or have already cared for patients with DFUs at home. We will exclude individuals unwilling to provide consent.
Data collection
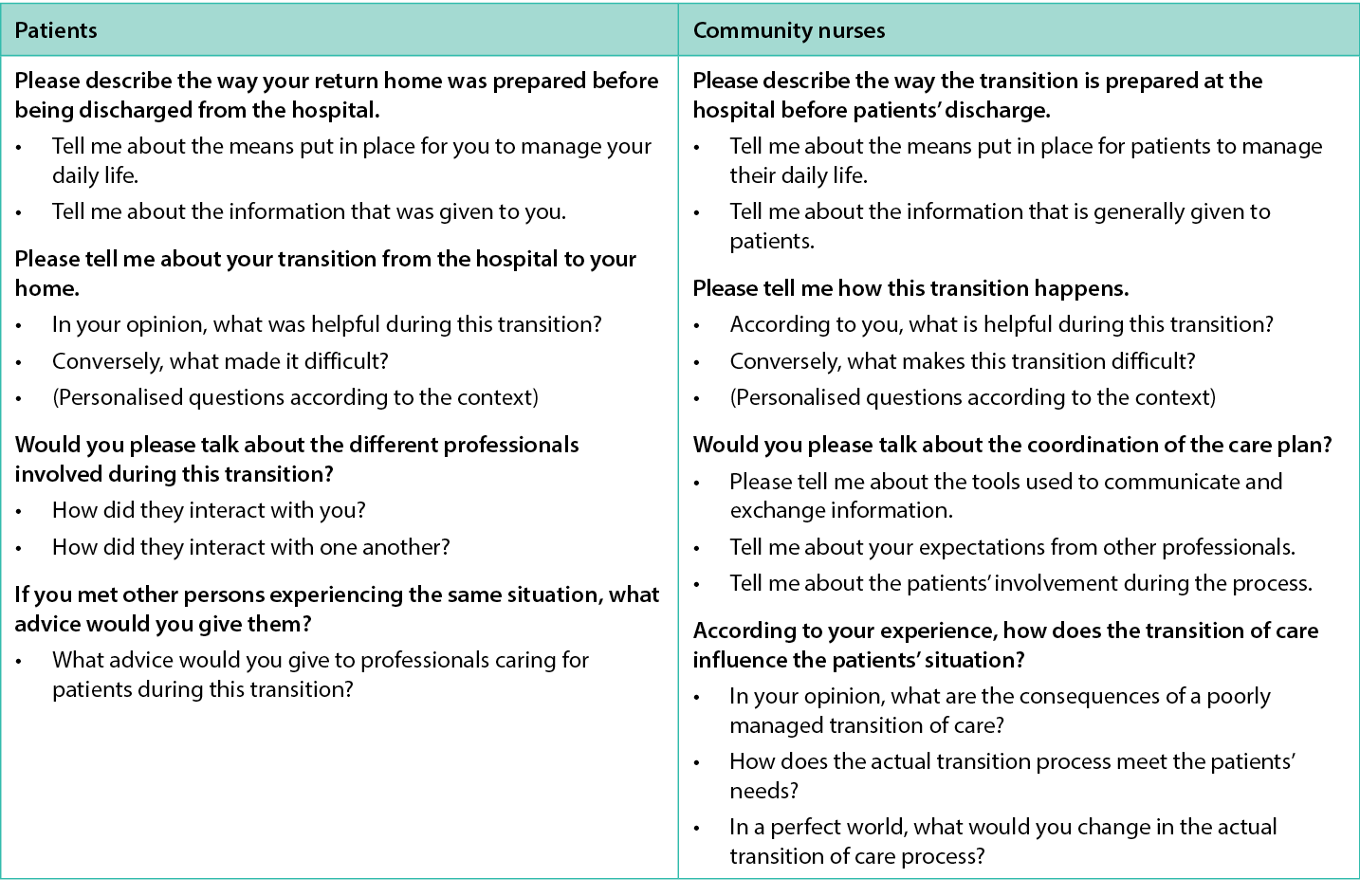
We will use a purposive sample. Then we will perform face-to-face, semi-structured, audio-recorded interviews to explore the in-depth perspectives of individuals and nurses. Both patients and nurses will be interviewed at home or respectively at the hospital. The topics of the interview guide are based on the literature and adapted by the authors (see Table 1). We will include six individuals with DFUs and six community nurses. The sample size was based on Braun and Clarke’s recommendations for a small project22, but additional participants might be included if the quality of the dataset is estimated to be insufficient.
Table 1. Interview guide: examples of questions translated from French to English by the first author.
A study nurse will screen inclusion criteria for hospitalised patients in a regional hospital in the Western part of Switzerland on their medical record basis. S/he will then meet potential participants face-to-face at the hospital for oral and written information about the study. If they accept, and after obtaining informed consent, the first author will schedule an appointment.
Nurses will be recruited through the participation of a homecare institution who will propose the participation by email. The first author will contact the nurses who demonstrate interest by phone for informed consent and appointment scheduling. The first author will perform and transcribe all the interviews. Field notes will be taken to report the atmosphere and non-verbal aspects. The first author will transcribe the interviews verbatim and the last author will check the transcripts for accuracy.
Data analysis
We will use thematic analysis according to Braun and Clarke23. During the analysis, two authors will complete five phases, 1–3 independently, then 4–5 together. A third author will be involved to discuss the results. During phase 1 (familiarisation), we will read and re-read the transcripts and field notes to develop familiarity. In phase 2 (coding), the segments which are potentially relevant will be identified, a code label will be generated, code labels will be collated and the corresponding data segments will be compiled for each code. In phase 3 (generating initial themes), we will compile codes sharing ideas in potential themes. All of the coded data relevant for each potential theme will be examined. In phase 4 (developing and reviewing themes), we will return to the full dataset in order to examine the accuracy of the potential themes for performing our analysis. We will check if each theme shares something relevant for the study and if these themes collectively highlight the most important patterns of the dataset. Some themes will be collapsed together, split, retained or discarded.
In phase 5 (refining, defining and naming themes), we will ensure that each theme is clearly demarcated and relevant to answering our research question by writing a brief synopsis about each theme. The final name of the themes will then be chosen. Demographic data and medical history data will be analysed using STATA 16®24 and presented by descriptive statistics. All interviews will be analysed using MAXQDA®25.
Rigour and Trustworthiness
To improve the rigour of this thematic analysis, we will use a computer software to systematise coding26. We applied the trustworthiness criteria for qualitative research following Lincoln and Guba27 and followed the COREQ EQUATOR guidelines28. Additionally, we will ensure reliability by writing a reflective journal (reflective diary) throughout the entire data collection and analysis process; in this way, we can keep track of any biases, assumptions and impressions we may have had. We will triangulate the analysis by means of two researchers working independently and thus enhance credibility. Verbatim quotes will guarantee the confirmability29. The last author will overview the entire work process.
Discussion
The findings of this study will generate new knowledge contributing to the further development of the wound care discipline about the transition of care from the hospital to the patients’ home and will promote the use of patient-centred concerns to inform healthcare practices. Our results will contribute to characterising both patients’ and nurses’ roles within the process, any barriers to effective care transitions and any strategies to overcome. It will enable us to develop interventions for improving this key step in the trajectory of patients with DFUs and thus improve quality of care and individuals’ health outcomes and quality of life, as well as contribute to reduced health expenditure.
In addition, we expect a more general benefit – that our results will identify the strengths and weaknesses of the actual care process in the specific study area. This will inform hereafter a quality improvement project, including implementation of the existing tools for preparing patient discharge through institutional procedures and/or the development of inter-institutional teaching sessions. Moreover, we expect that our findings will also help to identify other determinants that may have a positive impact on wound healing, DFU recurrence and patients’ quality of life, such as comprehensive therapeutic education and any new topics presented by the participants. Analysing and confronting both patients with DFUs and nurses’ perspectives on care transitions will raise questions on nursing interventions during the complex trajectory of this specific patient group and will generate information transferable to patients with other chronic diseases such as information sharing between various institutions, discharge preparation and follow-up and patient empowerment, which are key factors in reducing hospital readmissions that apply to every chronic disease.
Conflict of Interest
The authors declare no conflicts of interest.
Funding
The European Wound Management Association (EWMA) granted this study to the first author to promote innovative projects regarding DFU for “early career researchers”.
Author(s)
Carole Guex* RN, DAS in Wound Care, Camille Saini PhD, Géraldine Gschwind RN, MsC, Paul Bobbink* RN, PhD (cand.), MScN
Geneva School of Health Science, HES-SO University of Applied Sciences and Arts, Western Switzerland, Geneva, Switzerland.
*Corresponding author email carole.guex@hesge.ch
References
- International Diabetes Federation. L’atlas du diabète de la FID (IDF diabetes atlas) 9th ed; 2019. Available from: https://diabetesatlas.org/upload/resources/material/20200302_133352_2406-IDF-ATLAS-FRENCH-BOOK.pdf
- Harding JL, Pavkov ME, Magliano DJ, Shaw JE, Gregg EW. Global trends in diabetes complications: a review of current evidence. Diabetologia 2019;62(1):3–16.
- Monge L, Gnavi R, Carnà P, Broglio F, Boffano GM, Giorda CB. Incidence of hospitalization and mortality in patients with diabetic foot regardless of amputation: a population study. Acta Diabetol 2020;57(2):221–8.
- Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis. Ann Med 2017;49(2):106–16.
- Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med 2017;376(24):2367–75.
- Crawford F, Nicolson DJ, Amanna AE, Martin A, Gupta S, Leese GP, et al. Preventing foot ulceration in diabetes: systematic review and meta-analyses of RCT data. Diabetologia 2020;63(1):49–64.
- Sothornwit J, Srisawasdi G, Suwannakin A, Sriwijitkamol A. Decreased health-related quality of life in patients with diabetic foot problems. Diabetes Metab Syndr Obes Targets Ther 2018;11:35–43.
- Armstrong DG, Swerdlow MA, Armstrong AA, Conte MS, Padula WV, Bus SA. Five year mortality and direct costs of care for people with diabetic foot complications are comparable to cancer. J Foot Ankle Res 2020 [cited 2021 Feb 23];13. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7092527/
- Wu SC, Armstrong DG. Clinical outcome of diabetic foot ulcers treated with negative pressure wound therapy and the transition from acute care to home care. Int Wound J 2008;5(s2):10–6.
- Piaggesi A, Coppelli A, Goretti C, Iacopi E, Mattaliano C. Do you want to organize a multidisciplinary diabetic foot clinic? We can help. Int J Low Extrem Wounds 2014;13(4):363–70.
- Backman C, Cho-Young D. Engaging patients and informal caregivers to improve safety and facilitate person- and family-centered care during transitions from hospital to home – a qualitative descriptive study. Patient Prefer Adher 2019;13:617–26.
- McMurray J, Hicks E, Johnson H, Elliott J, Byrne K, Stolee P. ‘Trying to find information is like hating yourself every day’: the collision of electronic information systems in transition with patients in transition. Health Informatic J 2013;19(3):218–32.
- Laugaland K, Aase K, Barach P. Interventions to improve patient safety in transitional care – a review of the evidence. Work 2012;41:2915–24.
- McGaw J. A multidisciplinary approach to transition care: a patient safety innovation study. Perm J 2007 [cited 2021 Sep 13];11(4). Available from: http://www.thepermanentejournal.org/issues/2007/fall/536-transition-care.html
- Gethin G, Probst S, Stryja J, Christiansen N, Price P. Evidence for person-centred care in chronic wound care: a systematic review and recommendations for practice. J Wound Care 2020;29(Sup9b):S1–22.
- Annersten Gershater M, Pilhammar E, Alm Roijer C. Prevention of foot ulcers in patients with diabetes in home nursing: a qualitative interview study. Eur Diabetes Nurs 2013;10(2):52–7.
- Mabire C, Dwyer A, Garnier A, Pellet J. Meta-analysis of the effectiveness of nursing discharge planning interventions for older inpatients discharged home. J Adv Nurs 2018;74(4):788–99.
- Braet A, Weltens C, Sermeus W. Effectiveness of discharge interventions from hospital to home on hospital readmissions: a systematic review. JBI Database Syst Rev Implement Rep 2016;14(2):106–73.
- Mabire C, Bachnick S, Ausserhofer D, Simon M. Patient readiness for hospital discharge and its relationship to discharge preparation and structural factors: a cross-sectional study. Int J Nurs Stud 2019;90:13–20.
- Toscan J, Mairs K, Hinton S, Stolee P. Integrated transitional care: patient, informal caregiver and health care provider perspectives on care transitions for older persons with hip fracture. Int J Integr Care 2012 [cited 2021 Sep 13];12(2). Available from: http://www.ijic.org/article/10.5334/ijic.797/
- Hesse-Biber SN. The practice of qualitative research: engaging students in the research process. 3rd ed. Los Angeles: SAGE; 2017. p. 406.
- Braun V, Clarke V. Successful qualitative research: a practical guide for beginners. Los Angeles: SAGE; 2013. p. 382.
- Braun V, Clarke V. Thematic analysis: a practical guide to understanding and doing. 1st ed. Thousand Oaks: SAGE Publications; 2021.
- StataCorp. Stata Statistical software: release 16. 2019.
- VERBI Software. MAXQDA 2020. 2020.
- Tai J, Ajjawi R. Undertaking and reporting qualitative research. Clin Teach 2016;13(3):175–82.
- Guba EG, Lincoln YS. Naturalistic inquiry. Beverly Hills, CA: Sage Publications, Inc; 1985.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19(6):349–57.
- Whittemore R, Chase SK, Mandle CL. Validity in qualitative research. Qual Health Res 2001;11(4):522–37.
