Volume 39 Number 2
Experience of negative pressure wound therapy over sternal wound healing: A retrospective review
Wai Sze Ho, Wai Kuen Lee, Ka Kay Chan and Choi Ching Fong
Keywords Cardiothoracic surgery, sternal wound infection, negative pressure wound therapy
For referencing Ho WS et al. Experience of negative pressure wound therapy over sternal wound healing: A retrospective review. WCET® Journal 2019; 39(2):9–18
DOI https://doi.org/10.33235/wcet.39.2.9-18
Abstract
Objectives The aim of this study was to retrospectively review the effectiveness of negative pressure wound therapy (NPWT) in sternal wound healing with the use of the validated Bates-Jensen Wound Assessment Tool (BWAT), and explore the role of NPWT over sternal wounds and future treatment pathways.
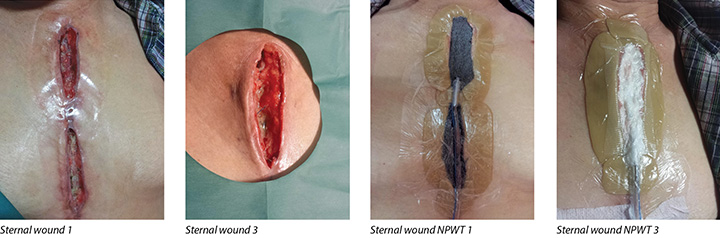
Methods Data was gathered from patients' medical records and the institution's database clinical management system. Seventeen subjects, who had undergone cardiothoracic surgeries and subsequently consulted the wound care team in one year were reviewed. Fourteen of them were included in the analysis. Healing improvement of each sternal wound under continuous NPWT and continuous conventional dressings was studied. In total, 23 continuous NPWT and 13 conventional dressing episodes were analysed with the BWAT.
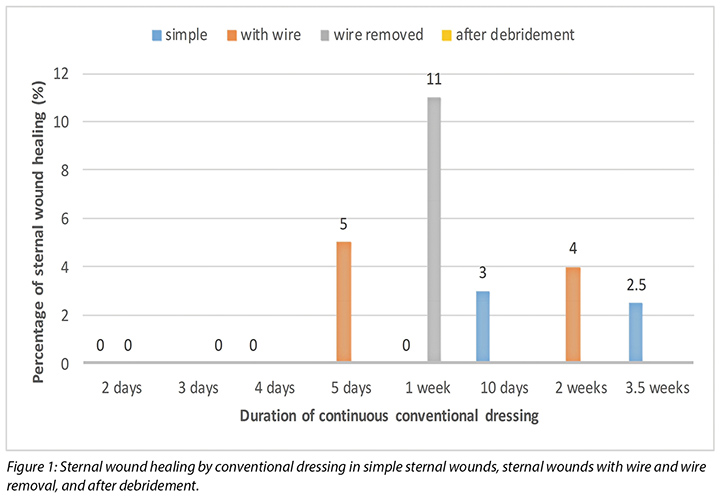
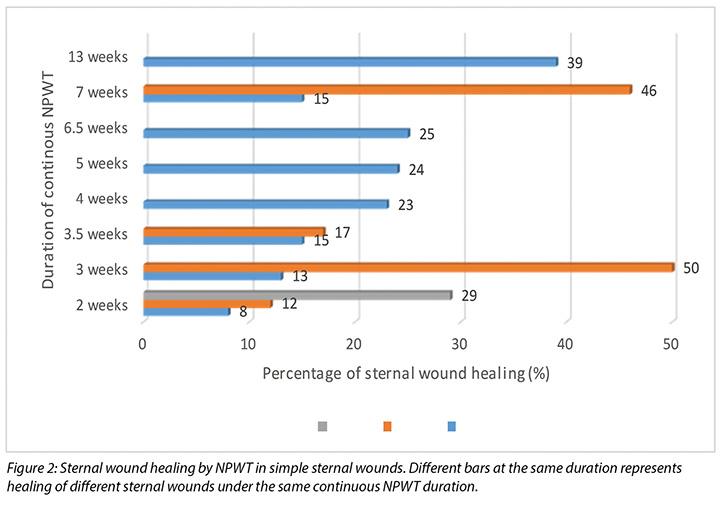
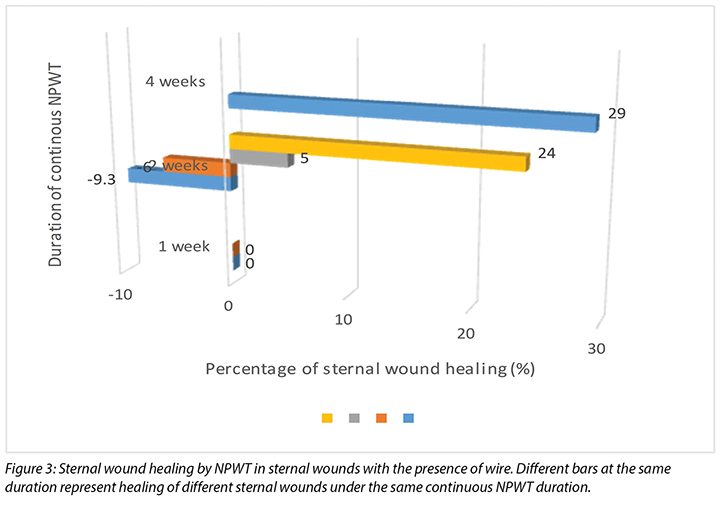
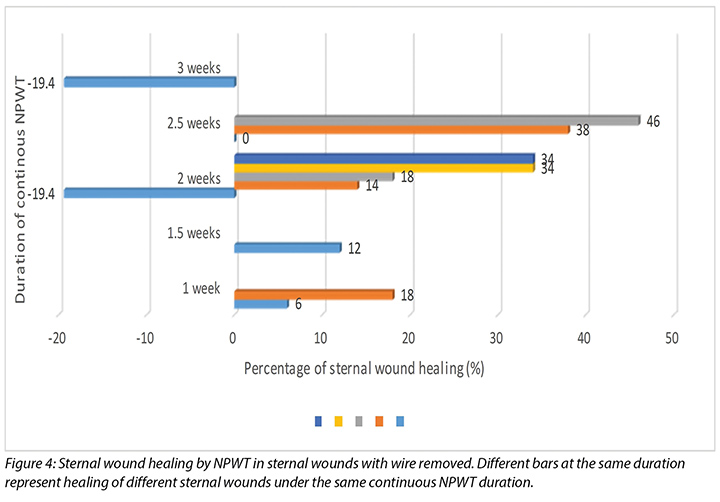
Results Among conventional dressing episodes, sternal wound improvement was 2.5–3% over 10 days to 3.5 weeks, whereas 4–5% sternal healing was achieved in 5 days to 2 weeks with sternal wire presence. Better healing at 11% in 1 week by conventional dressing was attained after sternal wire removal. In NPWT episodes, 8–29%, 13–24%, and 15–46% of healing was observed in 2 weeks, 3.5 to 5 weeks and 6 to 7 weeks, respectively. Only 39% wound healing was acquired at the 13th week of NPWT in one subject. With sternal wire present, 6%–29% wound healing progress was achieved by NPWT in 1–4 weeks, and 16–23% wound improvement in 2 to 4.5 weeks by NWPT after further surgical debridement. After sternal wire removal, 6–34% sternal wound healing occurred by continuous NPWT for 1–2 weeks, and maximum healing at 46% after 2.5 weeks of NPWT were observed.
Conclusions Better wound healing was achieved in the NPWT group in comparison to conventional dressings alone. However, suboptimal sternal wound healing by NPWT alone was observed. Removal of sternal wire may improve the effectiveness of NPWT. Successful tertiary closure after NPWT among subjects supports the important bridging role of NPWT in sternal wound healing. Factors causing stagnant sternal wound healing by NPWT alone are discussed.
Introduction
Establishment of sternotomy wounds is not uncommon among patients undergoing cardiothoracic surgeries. Even with advances in and optimal surgical techniques, as well as infection prophylaxis, the incidence of postoperative deep sternal wound infection (DSWI) has still been variously reported as 0.5–5.0% since 20011-7. Occurrence of postoperative mediastinitis was lower in patients who had undergone coronary artery bypass grafting (CABG) than that of CABG with concomitant valve surgery3,7. Sternal dehiscence and delayed sternal wound healing, especially in the presence of DSWI following sternotomy have remained constant, problematic and worrisome complications in cardiothoracic surgeries8,9.
Risk factors for DSWI have long been studied over the years. The increased risk of DSWI could be resultant from combined cardiac procedures4-9, prolonged intubation in the intensive care unit (ICU), harvest of bilateral internal thoracic artery grafting, re-operation for bleeding, obesity with body mass index (BMI) >30, diabetes, COPD, PVD and advanced age6,8,9. Using the left internal mammary artery, positive wound and blood cultures have been identified as significant risk factors for rewiring failure of post-sternotomy wounds8. Preoperative anaemia, presence of chronic viral or bacterial infection over four weeks and active infection at surgical time, previously treated infection within the past year were also predictors of DSWI5. The most common pathogens revealed in sternal wounds were Staphylococcus epidermidis (CoNS) and Staphylococcus aureus (MRSA)10, in which the latter pathogen was highly associated with increased mortality in DSWI11. Like surgical site wound infection (SSWI), delayed and suboptimal sternal wound healing can result from the presence of DSWI.
Multiple and combined conventional wound healing techniques have been adopted in sternotomy wounds for years, for instance, primary closure with or without sternal wire, debridement, wound packing, delayed closure, reconstruction of vascularised soft tissue flaps, open daily irrigation or multiple open dressing changes, or sternal re-wiring2,3,8,10,11. However, historical treatments had been reported with prolonged hospitalisation and mortality rates of 40–50%8,10. Closed-chest techniques reviewed reportedly showed failure rates of 20–66% with 7–32% mortality rates. The use of continuous irrigation with strong negative pressure ranging between 300 mmHg and 600 mmHg also resulted in treatment failure and mortality rate sustained at 12.5–52% and 7%, respectively, with an increased average length of hospital stay of 56 days. Flap reconstruction was associated with a less than 10% mortality rate in sternal wound healing9,12. As a result, conventional surgical treatments still incur complications in sternal wound healing by means of destabilising the sternum, lengthening hospitalisation and developing concomitant infection, which may result in death. While another wound care modality, negative wound pressure therapy (NPWT), has recently emerged as a clinical strategy for treating post-sternotomy mediastinitis and with promising results3, deciding the most appropriate treatment of sternal wounds, however, is still controversial.
DSWI is a devastating complication of cardiothoracic surgeries that not only impedes wound healing, but also has a mortality rate of approximately 5–47%, despite early diagnosis and treatment. Additional outcomes are prolonged hospitalisation, increased institutional costs as well as an increase in the patients' suffering2,5,11. In the United States, a surgical care improvement project (SCIP) was implemented to minimise SSWI and associated cost. The project designated DSWI as a preventable hospital-acquired infection in which no additional treatment reimbursement should be provided in 20087.
Multiple studies and reviews supported the promising results of NPWT in reducing the risk of chronic sternal infection, mortality, as well as duration of hospital stay3,4,10,13. Complications of wound dehiscence, infection, haematoma and seromas over high-risk surgical incisions which were reduced by NPWT were well supported by evidence13. Successful falling C-reactive protein (CRP) level was demonstrated in DSWI by NPWT in nine days. Bacterial counts were significantly reduced in wounds inoculated with MRSA and CoNS in four days. Instead of treating sternal wounds alone by NPWT, adoption of NPWT, followed by delayed primary closure or vascularised muscle flap, were well supported by studies with excellent clinical results6,10,14. One study reported 100% wound closure was achieved by NPWT at 14 months' follow-up noted in patients with sternal osteomyelitis, despite flap reconstruction involved in the treatment14.
Introduction of NPWT is achieved by applying a controlled subatmospheric pressure to the selected wound, through an airtight system of a porous dressing (foam or gauze) and evacuation tube in the wound, covered by an adhesive drape to create an airtight seal. The pore size of dressing (if foam) is approximately 400–600 µm, which allows for equal pressure to be applied to the wound bed. By connecting the tubing to an adjustable vacuum pump with a collection canister, the wound exudate can be withdrawn from the wound and collected2,9,11. NPWT assists in exudate removal as well as stabilisation of the chest wall and wound isolation. Wound edge approximation and wound contracture, reduction in oedema, inflammatory modulation, tissue perfusion, angiogenesis, cell proliferation and mitotic activity of skin can be facilitated by NPWT5,13.
Despite the supported advantageous features of NPWT in various wounds, studies of the effectiveness of NPWT alone over sternal wounds and any resulting improvement are limited. Instead, there is clinical evidence of the use of NPWT playing a bridging role within sternal wounds and post-sternotomy mediastinitis prior to surgical closure of these wounds10,14-16. With limited clinical evidence and a general lack of consensus on the optimal clinical procedural protocols for the management of sternal wounds with or without DSWI is lacking. This review retrospectively evaluated the outcome of NPWT alone over sternal wound healing and explored the role of NPWT as a future treatment pathway in sternal wound care.
Materials and Methods
Data source
Between January and December 2016, there were 17 inpatients who experienced complications with sternal wound healing post-cardiothoracic procedures and who consulted the stoma and wound care team for assistance with wound management. In this retrospective study, data on wound management were retrieved and reviewed from the nursing notes in the patients' medical record and from the institution’s clinical management system database.
Subject and sample selection
Three of the 17 inpatients who underwent cardiothoracic procedures and who consulted the wound care team, were excluded in our study. The excluded cases had either undergone NPWT initiated by surgeon with a subatmospheric pressure 10 to 20 mmHg only or consultation with the wound care team was discontinued because of bleeding and organ exposure. These cases were vastly different from other patients who persistently underwent NPWT with a subatmospheric pressure ranging between 80 and 125 mmHg. Sternal wounds among the selected cases were the result of non-closure of acute post-operative surgical wounds, delayed healing surgical dehiscence wounds, and post-incision and drainage of DSWI wounds. In view of the occurrence of re-exploration, surgical debridement or wire removal, discontinuing continuous NPWT, as well as multiple separate sternal wounds being managed by NPWT in the same patient, only those sternal wound episodes that were managed continuously by NPWT or conventional dressings were reviewed and evaluated. Therefore, included in this retrospective study were 23 wound episodes that used continuous NPWT and 13 wound episodes that used conventional dressing therapies.
Outcomes
The outcomes of interest included sternal wound improvement by continuous NPWT and conventional dressing episode. Wound improvement was further evaluated and compared between continuous corresponding wound care episodes with and without further surgical management, for instance, re-exploration, surgical debridement or wire removal.
Data analysis
Data was extracted from the selected patients' medical record and institution’s database. Factors related to the healing progress of sternal wounds were identified and retrieved. Sternal wound healing of each continuous NPWT and conventional dressing episode was assessed and scored with the validated Bates-Jensen Wound Assessment Tool (BWAT) and results tabulated. Components of scoring in BWAT are size, depth, edges, undermining, necrotic tissue type, necrotic tissue amount, exudate type, exudate amount, skin colour surrounding wound, peripheral tissue oedema, peripheral tissue induration, granulation tissue and epithelialisation17. Total score before and after continuous treatment was compared and then calculated as a percentage of wound improvement. The percentage change provided the information required to determine sternal wound improvement by each continuous dressing regime. The effect of NPWT, with or without further surgical management, over sternal wound healing was also identified in this review.
Results
Sample characteristics
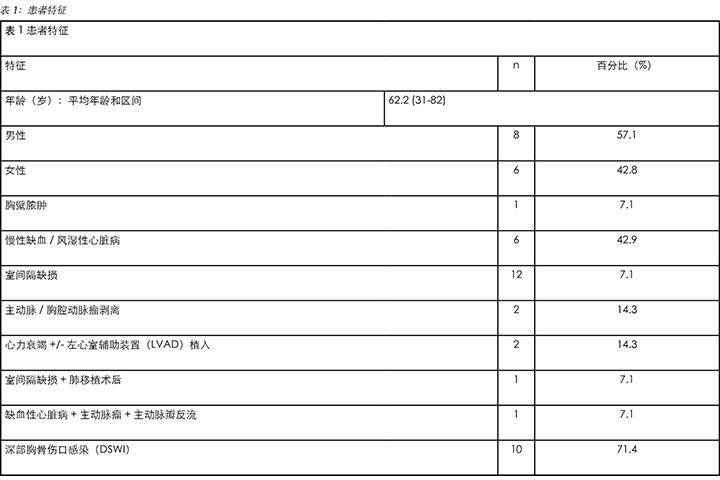
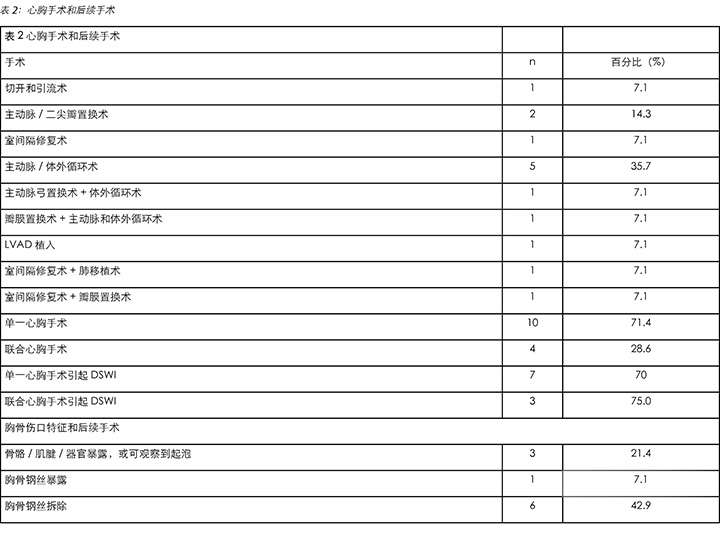
The 14 subjects included in the study were aged between 31 and 82, with a mean age of 62.2. Six patients were female (42.8%) and 8 were male (57.1%). Of the patients, 71.4% developed a DSWI. Demographic data and clinical characteristics of patients are presented in Table 1. Various cardiothoracic procedures had preceded the occurrence of sternal wounds. Of the subjects, 71.4% underwent single cardiothoracic procedures such as skin abscess drainage, heart valve replacement, ventricular septal defect repair, aorto- or cardiopulmonary bypass, and internal device implantation. Combined procedures involved 28.6% of the cases, which involved aortic valve replacement with cardiopulmonary bypass, valve replacement with coronary artery bypass, ventricular septal defect repair with lung transplant, and ventricular septal defect repair with heart valve replacement. Seven out of 10 subjects (70%) who underwent single cardiothoracic procedures developed a DSWI, whereas three out of four (75%) subjects who underwent combined procedures developed DSWIs. Exposure of internal structures such as sternal bone or tendon, with or without bubbling occurred in 21.4% of the cases. Overall, the cases of wire exposure and wire removal were 7.1% and 42.9% respectively. Details of cardiothoracic procedures undertaken are presented in Table 2.
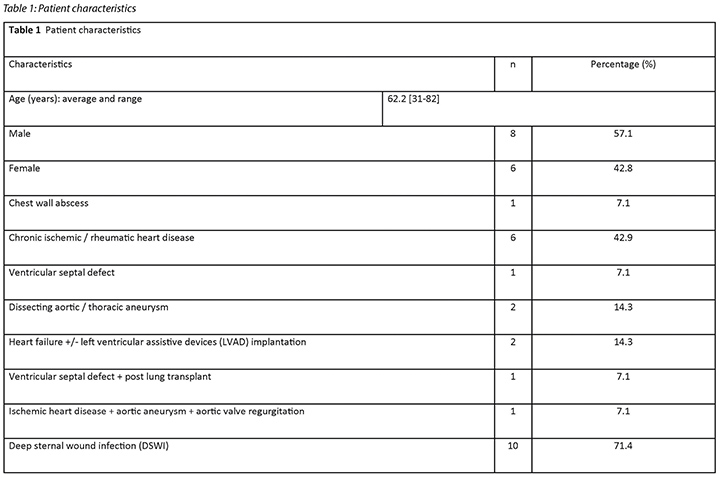
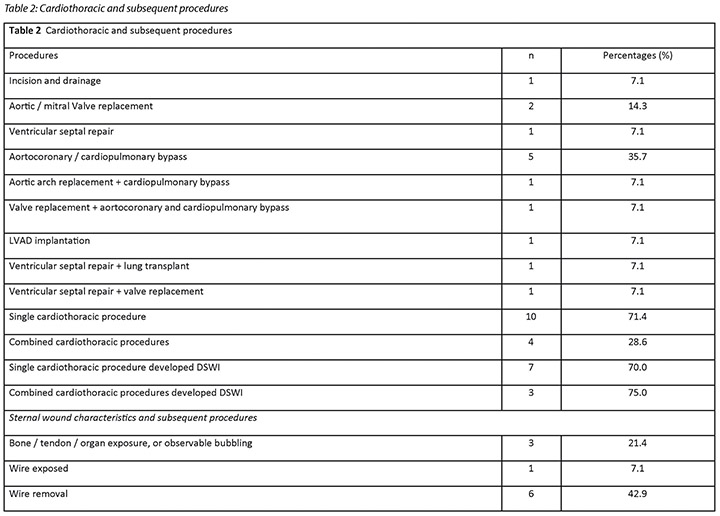
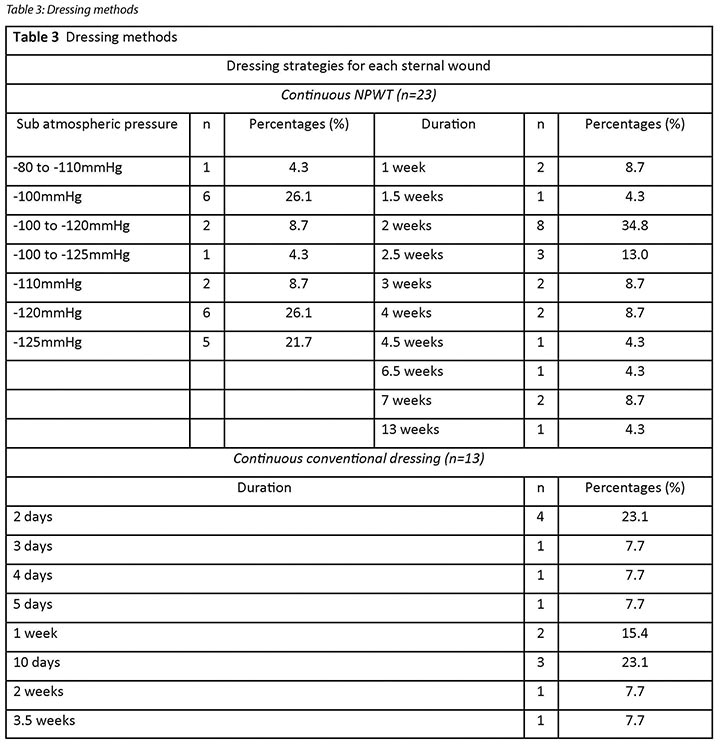
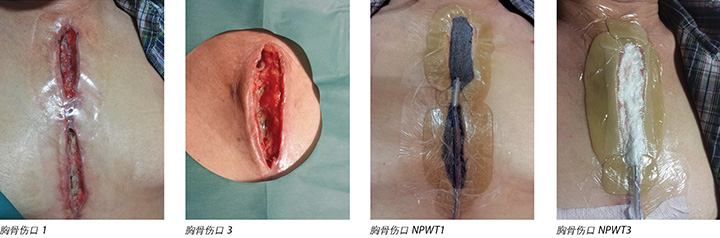
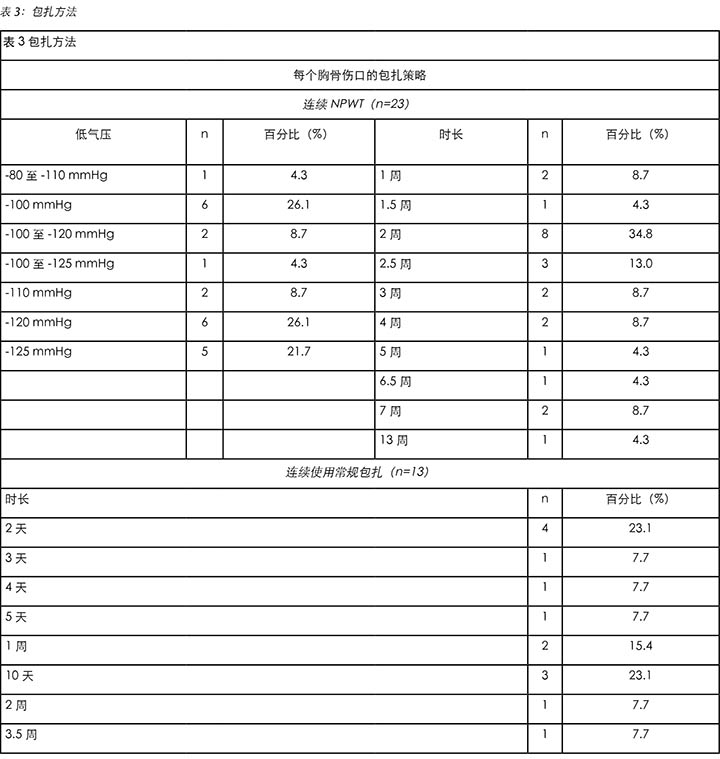
In this review, a total of 23 NPWT episodes and 13 conventional dressing episodes over sternal wounds were retrospectively reviewed (Table 3). NPWT was adopted at subatmospheric pressure of 80 to 125 mmHg. The treatment period of an episode of continuous NPWT ranged from 1 to 13 weeks. Within the NPWT group, the wound dressing was performed every 2 to 3 days by the wound care team. The treatment period for continuous conventional dressings ranged from 2 days to 3.5 weeks. Daily dressings were performed in the conventional dressing group.
Sternal wound healing
In this review, healing improvement of each sternal wound was evaluated at the end of each continuous episode of wound care. Additional wound care improvement was identified at the mid-point of the treatment period if the continuous episode of treatment was more than 2 weeks.
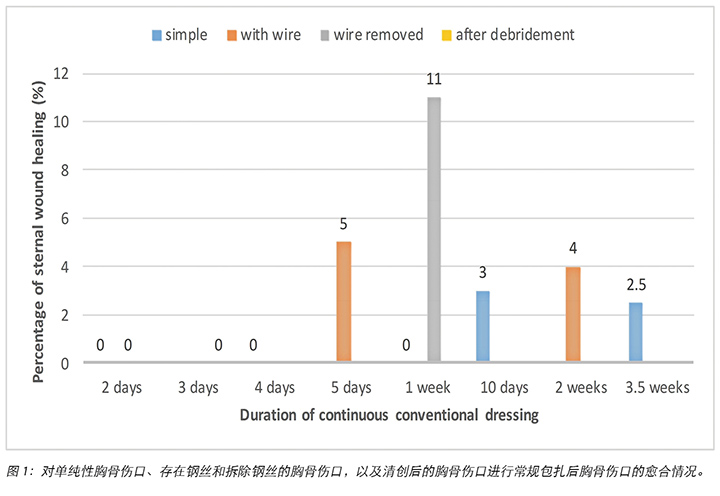
Conventional dressing
In the continuous conventional dressing care group, no sternal wound healing was achieved in 2 days to 1 week. Approximately 2.5–3% of sternal wound healing was achieved in 10 days to 3.5 weeks. With the presence of sternal wire, 4–5% of sternal wound healing was noted in 5 days to 2 weeks. No significant impaired healing was noted with the presence of sternal wires by conventional dressing regimes. However, better healing occurred in 11% of sternal wounds after removal of the sternal wire and application of conventional dressings for 1 week. In two different subjects, no significant wound improvement or signs of healing occurred in 2 days of conventional dressing after surgical debridement or wire removal respectively. There was an unsatisfactory healing effect over sternal wounds as the result of using conventional dressings. Healing of sternal wound by continuous conventional dressing is summarised in Figure 1.
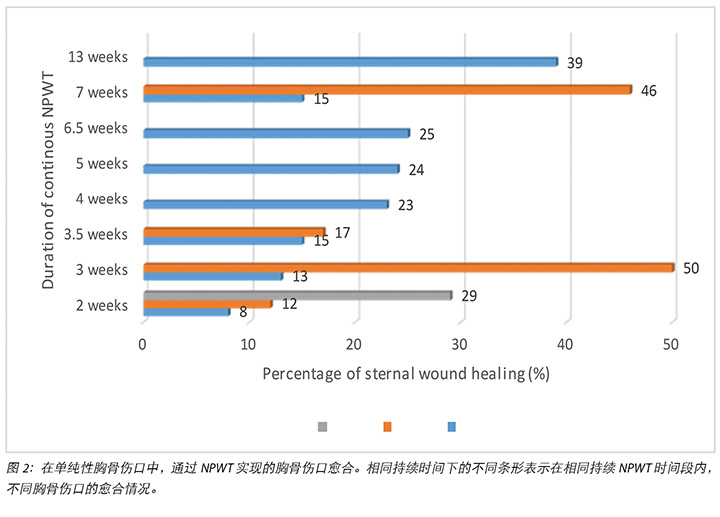
Negative pressure wound therapy
Among the continuous NPWT episodes, sternal wound healing was achieved in 8–29% of wounds in 2 weeks. With continuous NPWT for 3.5–5 weeks, an average of 13–24% wound healing was achieved. One wound achieved 50% healing within 3 weeks. In longer continuous NPWT periods of 6–7 weeks, only 15–46% of sternal wound healing was attained. A subject demonstrated 39% sternal wound healing after 13 weeks of continuous NPWT. Suboptimal wound healing of sternal wounds by continuous NPWT alone was illustrated in Figure 2.
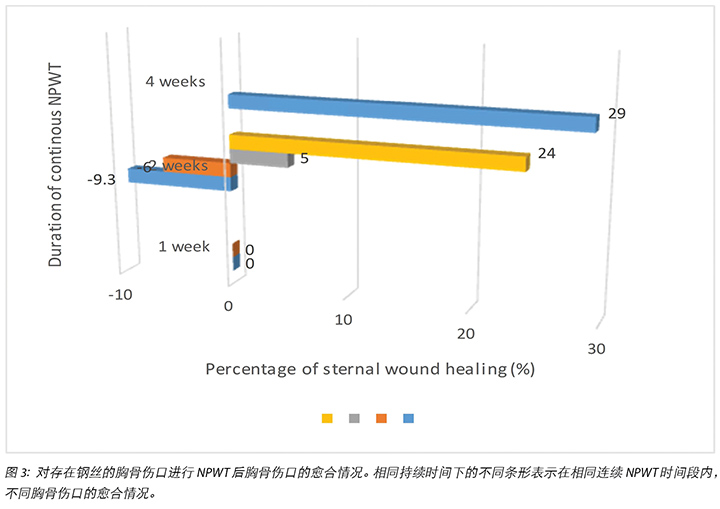
In the presence of sternal wire, wound improvement of 6–24% was identified in 1–2 weeks of continuous NPWT. A maximum of 29% of sternal wound healing was achieved after 4 weeks’ continuous NPWT (Figure 3).
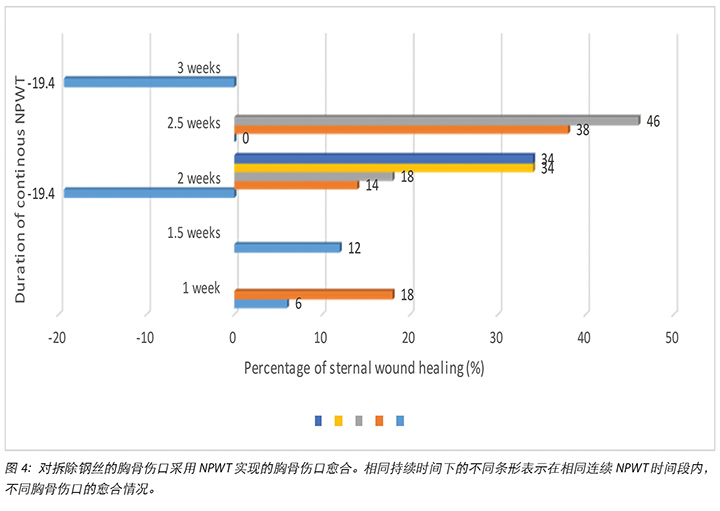
After removal of sternal wires, sternal wound healing by NPWT was slightly improved. Six to 18% of sternal wound healing was observed in 1–1.5 weeks. After 2 weeks of NPWT, an average of 14–34% of sternal wound healing was reached. Zero to 46% sternal wound healing was noted with 2.5 weeks of NPWT. However, an exceptional wound deterioration results of 19.4% wound healing by 2–3 weeks of continuous of NPWT was identified (Figure 4).
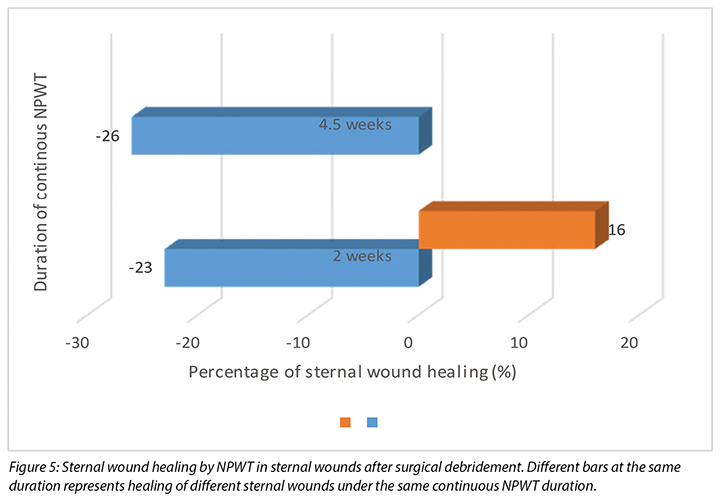
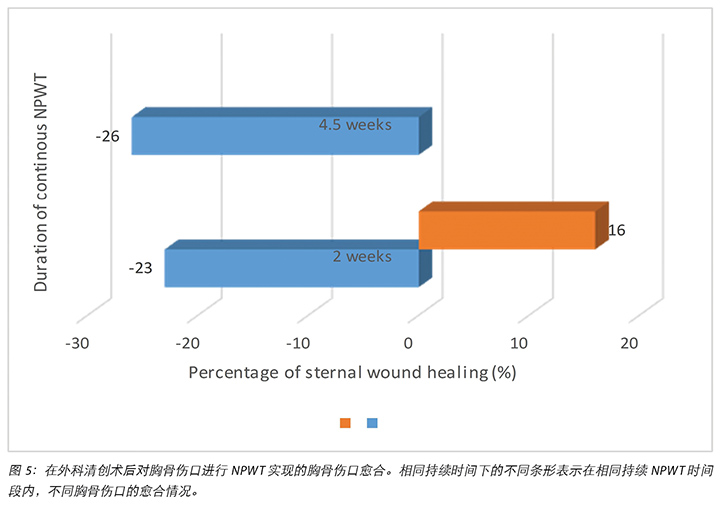
No significant improvements in sternal wound healing were identified after surgical debridement in 3 cases, where sternal wound healing ranged from 16 to 23% with 2 weeks of NPWT, and up to 26% of sternal wound healing by 4.5 weeks of NPWT (Figure 5).
On the whole, suboptimal sternal wound healing was attained by continuous NPWT in this review. The presence of sternal wire could delay sternal healing by continuous NPWT, whereas the removal of sternal wire could improve the NPWT effect over sternal wound healing.
Wound deterioration could also occur, despite NPWT and surgical debridement procedures taking place.
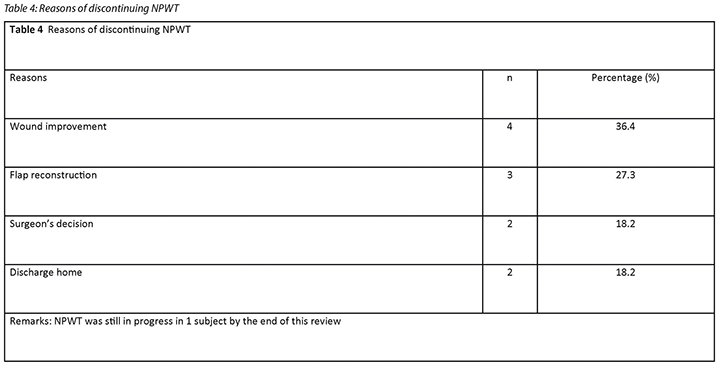
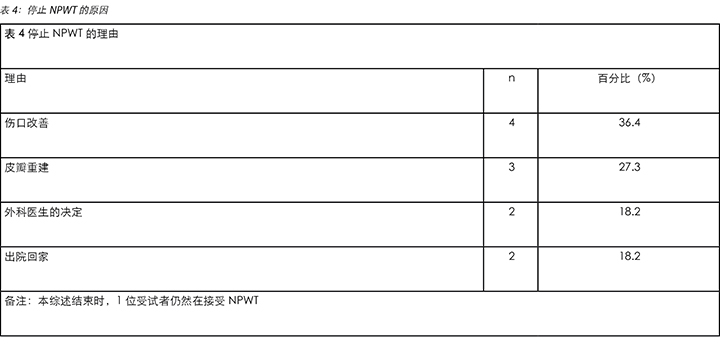
Discontinuation of NPWT
In addition to the interruptions of continuous episodes of NWPT by surgical debridement or wire-removal procedures, NPWT was discontinued for multiple other reasons at the end of wound care management (Table 4). Successful flap reconstruction for sternal wound defect (27.3%) and ideal wound progress suitable for the use of conventional dressing (36.4%) were major reasons of NWPT discontinuation. The surgeon’s medical decisions and prescription of therapy (18.2%) and discharge home (18.2%) were other causes for discontinuing NPWT. One subject was still under continuous NPWT sternal wound care at the end of this retrospective review. Apart from wound improvement by NPWT alone, flap reconstruction after NPWT played a pivotal position in sternal wound healing.
Discussion
As per the literature, post-operative DSWI was comparatively more prevalent in patients who had undergone combined cardiothoracic procedures4,7. In this review, no significant difference in DSWI incidence rate was observed between patients who underwent combined cardiothoracic procedure (75%) and those undergone single cardiothoracic procedures (70%). However, as DSWI developed in most of the selected subjects (71.4%) it illustrates its apparent incidence cannot be neglected.
In this review, our findings correlated to previous literature in which conventional dressing did not show significant positive effects on sternal wound healing. Simple sternal gap wounds, or with wire present showed similar unsatisfactory healing outcome under conventional wound care. In this review, only slightly better sternal healing outcomes occurred with the use of conventional wound care after wire removal and surgical debridement. The overall effect of sternal wound healing by conventional dressing is limited according to the previous literature and our findings.
The application of NPWT has become an evolving wound care modality for the management of sternal wounds in recent years10,11,14,15. In this review, and in comparison with conventional wound care, better sternal wound healing outcomes were achieved with the use of NPWT. Nevertheless, the healing achieved by NPWT was suboptimal in sternal wounds. In this review, less than 30% of sternal wound healing was attained by 5 weeks' continuous use of NPWT, and less than 50% of healing was observed in 6–7 weeks’ continuous NPWT. With continuous NPWT, deterioration of sternal wound healing still took place in some subjects. NPWT after surgical debridement did not facilitate better healing outcome in some sternal wounds. After sternal wire removal, improved sternal wound healing by continuous NPWT was found to occur in this review.
With prolonged NPWT, instead of complete wound healing stasis of wound healing was common among subjects. Further, the progress of sternal wound healing was slow in the NPWT group.
An analysis of the findings showed that flap reconstruction played an important role as a method of tertiary closure of sternal wounds after the application of NPWT. Despite suboptimal sternal wound healing by NPWT alone, this review supports the bridging role of NPWT in tertiary closure and healing of sternal wounds.
Previously, NPWT has been reported as a safe and reliable wound care option in the presence of DSWI, resulting in higher survival rates and lower failure rates in comparison to conventional dressings. In DSWI, prevention measures should be focused on optimising modifiable clinical factors3. Diabetic control, operation time, perioperative thermoregulation and antibiotics coverage are some of the mentioned modifiable clinical factors that can be moderated for minimising DSWI7. Bilateral internal thoracic artery grafting, the need for transfusion, emergency operations, previous episodes of stenting and postoperative inotrope usage also predicted higher risk of DSWI after sternotomy8. The presence of infection is known to inhibit wound healing. Adopting NPWT can provide benefits in treating DSWI, as well as DSWI-related mortality indirectly, by stabilising the thoracic cage, decreasing bacterial colonisation and wound oedema, promoting microvascular blood flow and granulation tissue formation and minimising exposure to infection11. Therefore, despite suboptimal sternal wound healing observed in our review, NPWT still plays an important role in facilitating sternal wound healing progress.
Multiple possible causative factors of suboptimal sternal wound healing have been discussed in the literature. Unsuccessful rewiring has been identified as having a positive relationship with positive wound cultures, positive blood cultures, devascularisation of chest wall after harvesting of left internal mammary artery and bacterial resistance6,8. Either local or systemic infection also led to unfavourable sternal wound healing results, even with debridement and rewiring. The likelihood for successful re-closure of infected sternal wounds was 3.3 times higher when three consecutive negative wound culture results were obtained8. Prolonged NPWT can stimulate recurrent infection should there be a significant shift of bacterial species. Patient-related factors such as haemodynamic condition and sternal viability, and local environmental factors such as the provision of materials and expertise, also affect NPWT’s impact on sternal wound healing4. Other factors causing suboptimal sternal wound healing and edge approximation are relatively thin skin with moderate dermal layers covering the chest18, the forces exerted by the bilateral pectoralis major muscle connecting the sternum19, persistent respiratory chest wall expansion, presence of foreign bodies such as sternal wires and exposed internal structures in the sternal wound.
In relation to the findings within this retrospective review and possible factors affecting sternal wound healing and suboptimal sternal healing by NPWT alone, it is believed that NPWT benefits sternal wound healing through its bridging role. NPWT helps in pre-conditioning and preservation of the sternum for further surgical debridement and wound healing9. This is further supported by a report of delayed sternal plating or bilateral pectoralis major flap reconstruction after NPWT was a safe choice for and resulted in successful reconstruction of sternal wounds with DSWI or sternal dehiscence20. Optimal duration of NPWT before reconstruction or further surgical repair promotes growth of granulating tissue, decreases in bacterial load as well as a fall in CRP levels. The use of NPWT still has possible side effects in wound care, such as organ or internal structural damage and bleeding, which also limits the adoption or continuation of NPWT. Careful protection of internal structures such as the heart and vessels by paraffin gauze or wound contact layers is important if NPWT is used11.
In this retrospective review, successful tertiary closure after NPWT among subjects requiring sternotomy aligns with the consensus of opinion within the literature that NPWT plays an important bridging role in the management of open sternal wounds.
The lack of disclosure of study variable and controls such as the degree of DSWI and simple sternal dehiscence, small sample sizes and retrospective nature of this study has limited our analysis of NPWT effect on sternal wound healing in a definitive way. Studies focusing directly on the effect of NPWT over sternal wound healing only are limited. There is still a need for further studies on the direct effect of NPWT over sternal wound, in larger scale, larger sample size and with better case controls, to yield potentially promising knowledge and significant results. The NPWT effect on infection control, CRP level, and complete wound healing time after NPWT followed by reconstruction among sternal wounds is worthy of future studies. Exploring optimal timing of switching from NPWT to reconstruction or repair of sternal wounds would also benefit sternal wound care in future.
Conclusion and future perspectives
Sternal wound healing is still a challenge for patients who have undergone cardiothoracic surgeries, irrespective of whether there was post-sternotomy mediastinitis, post-operative dehiscence or an open surgical wound. NPWT has been adopted successfully with more advantages than conventional dressings in the management of sternal wounds within the last decade. This retrospective review identified NPWT alone can lead to stagnation in wound healing on sternal wounds. However, as a bridging process to prepare sternal wounds for further flap reconstruction or other tertiary closure methods, NPWT did demonstrate promising functional results in sternal wound healing. Adopting NPWT as a bridge for pre-conditioning sternal wounds, followed by tertiary closure, could become a primary approach for sternal wound care. This viewpoint is supported by prior literature and the current retrospective review. Nevertheless, as previously stated, large-scale studies targeting the direct effect of NPWT over sternal wound healing are still lacking. Optimal timing for discontinuing NPWT and switching to reconstructive surgery should be further studied and explored. For instance, the amount of healthy granulation tissue, normalised CRP or white cell count level after NPWT. In the future, more research and informed understanding are required for developing an evidence-based guideline and clinical pathways on optimal sternal wound care.
Conflict of Interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
负压伤口治疗促进胸骨伤口愈合的经验:回顾性综述
Wai Sze Ho, Wai Kuen Lee, Ka Kay Chan and Choi Ching Fong
DOI: https://doi.org/10.33235/wcet.39.2.9-18
摘要
目的本研究旨在使用经过验证的Bates-Jensen伤口评估量表(BWAT)回顾性地审查负压伤口治疗(NPWT)对于胸骨伤口愈合的有效性,并探讨NPWT对胸骨伤口和未来治疗途径的作用。
方法数据采集自患者的病例记录和医院的数据库临床管理系统。对17名接受过心胸外科手术并在随后一年内接受伤口护理团队护理的受试者进行了审查。其中的14名患者被纳入了分析。研究了每个胸骨伤口在持续NPWT和持续常规包扎下的愈合改善情况。使用BWAT总共分析了23次持续NPWT和13次常规包扎。
结果采用常规包扎时,胸骨伤口在10天至3.5周内改善2.5-3%,而在存在胸骨钢丝的情况下,胸骨在5天至2周内愈合4-5%。拆除胸骨钢丝后,通过常规包扎在1周内实现更好愈合,达11%。采用NPWT时,在2周、3.5至5周和6至7周观察到的愈合分别达到8-29%、13-24%和15-46%。仅一名受试者在进行NPWT的第13周时伤口愈合39%。在存在胸骨钢丝的情况下,采用NPWT在1至4周内伤口愈合达6%-29%,在进一步外科清创术后,采用NWPT在2至4.5周内伤口改善达16-23%。在拆除胸骨钢丝后,持续采用NPWT后胸骨伤口愈合在1-2周内达到6-34%,采用NPWT 2.5周后,最大愈合达到46%。
结论与单独采用常规包扎相比,NPWT组的伤口愈合更好。然而,在仅采用NPWT时,胸骨伤口愈合情况欠佳。拆除胸骨钢丝可以提高NPWT的有效性。受试者在采用NPWT后,成功实现三期伤口闭合可支持NPWT在胸骨伤口愈合中的重要桥接作用。讨论了仅采用NPWT导致胸骨伤口愈合停滞的因素。
前言
在接受心胸外科手术的患者中,胸骨切开伤口并不少见。即使在手术技术进步并且使用最佳的手术技术以及预防感染措施的情况下,自2001年以来,术后深部胸骨伤口感染(DSWI)的发生率仍在0.5%至5.0%之间1-7。在接受冠状动脉旁路移植术(CABG)的患者中,术后纵隔炎的发生率低于伴随瓣膜手术的CABG患者3,7。在心胸外科手术中,胸骨裂开和胸骨伤口愈合延迟仍然是长期存在、未解决的且令人担忧的并发症,特别是在胸骨切开术后存在DSWI的情况下8,9。
多年来,人们一直在研究DSWI的风险因素。DSWI的风险增加可能源自心脏手术4-9、在重症监护室(ICU)长时间插管、为移植获取双侧胸内动脉、出血再次手术、体重指数(BMI)> 30的肥胖症、糖尿病、COPD、PVD和高龄等原因6,8,9。使用左侧乳内动脉时,伤口和血培养阳性已被确定为胸骨切开术后伤口重新缝钢丝失败的重要风险因素8。术前贫血、四周内存在慢性病毒或细菌感染、手术时活动性感染以及过去一年内治疗过感染也是DSWI的预测因素5。在胸骨伤口中最常见的病原体是表皮葡萄球菌(CoNS)和金黄色葡萄球菌(MRSA)10,其中后一种病原体与DSWI的死亡率增加高度相关11。与手术部位伤口感染(SSWI)一样,存在DSWI可导致胸骨伤口愈合延迟和欠佳。
多年来,一直对胸骨切开伤口采用多种伤口愈合技术,并结合了常规伤口愈合技术,例如,使用或不用胸骨钢丝的一期闭合、清创术、伤口包扎、延迟闭合、带血管软组织瓣重建、开放性每天灌注或开放性多次更换敷料,或胸骨重新缝钢丝2,3,8,10,11。然而据报道,传统疗法导致住院时间延长,并且死亡率为40-50%8,10。据报道,闭胸技术的失败率为20-66%,死亡率为7-32%。使用300 mmHg至600 mmHg范围内的强负压连续灌注也导致治疗失败,且死亡率分别维持在12.5-52%和7%,平均住院时间延长至56天。皮瓣重建术与胸骨伤口愈合的死亡率低于10%相关9,12。因此,常规手术治疗方式仍然会因为破坏胸骨的稳定性、延长住院时间以及造成伴随感染而在胸骨伤口愈合时引起并发症,这些并发症可导致死亡。虽然另一种伤口护理方式,即负压伤口治疗(NPWT),最近已成为治疗胸骨切开术后纵隔炎的临床策略并且具有良好的效果3,但是,确定最合适的胸骨伤口治疗法仍然存在争议。
DSWI是心胸外科手术的一种灾难性并发症,不仅会妨碍伤口愈合,而且即使早期诊断和治疗,死亡率也仍为约5-47%。其他后果还有延长住院时间、增加医院成本以及患者痛苦2,5,11。美国实施了一项外科护理改善项目(SCIP),以尽量减少SSWI并降低相关费用。2008年,该项目将DSWI指定为可预防的医院获得性感染,并且不会为此提供额外的治疗报销7。
多项研究和评估支持NPWT在降低慢性胸骨感染风险、死亡率以及缩短住院时间方面的良好成果3,4,10,13。有充分的证据支持NPWT能够降低高风险手术切口的伤口裂开、感染、血肿和血清肿等并发症13。对于DSWI,采用NPWT能在9天内成功降低C-反应蛋白(CRP)水平。在MRSA和CoNS定植的伤口中,细菌计数在4天内显著降低。临床研究证实,相比于单独采用NPWT治疗胸骨伤口,在采用NPWP后进行延迟一期闭合或带血管肌瓣治疗时获得优异临床结果6,10,14。一项研究报告称,对胸骨骨髓炎患者进行14个月随访后发现,NPWT实现100%伤口闭合,尽管治疗中涉及到皮瓣重建14。
采用NPWT时,在伤口中放置一个多孔敷料(泡沫或纱布)气密系统和抽空管,用粘性巾单覆盖伤口以保持气密性,再有控制地对所选伤口施加低于大气压的压力。敷料(如果是泡沫)的孔径大小约为400-600μm,以便能对伤口床施加相等的压力。通过将抽空管连接到带有收集罐的可调节真空泵,可以从伤口抽吸并收集伤口渗出液2,9,11。NPWT有助于排出渗出液以及稳定胸壁和伤口隔离。NPWT可以促进伤口边缘闭合和伤口收缩、水肿减轻、炎症调节、组织灌注,血管新生、细胞增殖和皮肤有丝分裂活动5,13。
尽管研究支持NPWT对各种伤口都有优势,但关于单独采用NPWT对胸骨伤口的有效性及任何相应改善的研究数量有限。相反,有临床证据表明,在通过手术闭合胸骨伤口之前,NPWT在胸骨伤口和胸骨切开术后纵隔炎之中发挥桥接作用10,14-16。由于临床证据有限,对处理有或没有DSWI的胸骨伤口的最佳临床手术方案缺乏普遍共识。本综述回顾性地评估了单独采用NPWT对胸骨伤口愈合的效果,并探讨了NPWT作为胸骨伤口护理未来治疗途径的作用。
材料和方法
数据来源
2016年1月至12月期间,17名住院患者在接受心胸外手术后出现胸骨伤口愈合并发症,并接受造口和伤口护理团队的帮助处理伤口。在这项回顾性研究中,通过患者病历中的护理记录和医院临床管理系统数据库检索并审查伤口管理数据。
受试者和样本选择
在本研究中,17名住院患者接受心胸手术后接受造口和伤口护理团队的帮助,有3人被排除在外。被排除的患者要么接受由外科医生实施的NPWT(低气压,只有10-20 mmHg),要么因为出血和器官暴露而停止向伤口护理团队寻求帮助。这些患者与持续接受80-125 mmHg低气压NPWT的其他患者有很大的不同。在所选病例中,胸骨伤口由于急性术后手术伤口未闭合、手术开裂伤口愈合延迟以及DSWI伤口切开和引流所致。鉴于发生了重新探查、外科清创术或钢丝拆除、停止持续NPWT,以及对同一患者的多个单独胸骨伤口采用NPWT,仅审查和评估了持续NPWT或常规包扎治疗的胸骨伤口案例。因此,本回顾性研究包括了使用持续NPWT的23次伤口治疗和使用常规包扎疗法的13次伤口治疗。
结果
值得注意的结果包括采用持续NPWT和常规包扎后的胸骨伤口改善。对伤口改善进行了进一步评估,并且比较了有和没有进一步手术处理的持续相应的伤口护理情况,这些手术处理包括重新探查、外科清创术或拆除钢丝。
数据分析
数据来自选定患者的病例和医院数据库。确定并找出了与胸骨伤口愈合进展相关的因素。评估每个持续NPWT和常规包扎治疗的胸骨伤口愈合情况,并用经验证的Bates-Jensen伤口评估工具(BWAT)评分,并将结果制成表格。BWAT评分的项目有尺寸、深度、边缘、潜行、坏死组织类型,坏死组织量、渗液类型、渗液量、伤口周围皮肤颜色、外周组织水肿、外周组织硬结,肉芽组织和上皮化17。比较持续治疗前后的总分,然后计算伤口改善的百分比。通过百分比的变化,获得确定采用每种持续包扎方案时胸骨伤口改善所需的信息。本综述还确定了在有或没有进一步手术治疗的情况下NPWT对胸骨伤口愈合的影响。
结果
样本特征
本研究包括14名受试者,年龄在31至82岁之间,平均年龄为62.2岁。6名患者为女性(42.8%),8名为男性(57.1%)。在这些患者中,71.4%的患者发生了DSWI。患者的人口统计学数据和临床特征见表1。胸骨伤口出现在多种心胸手术后。在这些受试者中,71.4%接受了单一心胸手术,如皮肤脓肿引流、心脏瓣膜置换术、室间隔缺损修复术、主动脉或体外循环术以及内部器械植入术。28.6%的病例接受联合手术,其中包括主动脉瓣置换术与体外循环、瓣膜置换术与冠状动脉搭桥术、室间隔缺损修复术与肺移植术,以及室间隔缺损修复术与心脏瓣膜置换术。接受单一心胸手术的10名受试者中有7名(70%)出现了DSWI,而接受联合手术的4名受试者中有3名(75%)出现了DSWI。21.4%的病例发生胸骨或肌腱等内部结构暴露,伴有或不伴有起泡。总体而言,钢丝暴露和钢丝拆除的病例分别为7.1%和42.9%。所进行的心胸手术详情见表2。
本综述回顾性地审查了对胸骨伤口采用的总共23次NPWT和13次常规包扎治疗情况(表3)。NPWT采用的低气压为80-125 mmHg。一次持续NPWT的治疗期为1至13周。在NPWT组中,由伤口护理团队每2至3天进行一次伤口敷料护理。持续常规包扎的治疗期为2天至3.5周。常规包扎组每天更换敷料。
胸骨伤口愈合
本综述中,在每次持续伤口护理结束时评估每个胸骨伤口的愈合改善情况。如果持续治疗时间超过2周,在治疗期的中间点观察到额外的伤口护理改善。
常规包扎
在常规包扎组中,2天至1周内没有实现胸骨伤口愈合。在10天至3.5周内,胸骨伤口大约愈合2.5-3%。在存在胸骨钢丝的情况下,5天至2周内观察到胸骨伤口愈合4-5%。在存在胸骨钢丝的情况下,采用常规包扎治疗方案时,未发现明显愈合不良。然而,在拆除胸骨钢丝并采用常规包扎1周后,胸骨伤口愈合更好,达11%。在两个不同的受试者中,在外科清创术或拆除钢丝后使用2天常规包扎,没有发生显著的伤口改善或愈合迹象。采用常规包扎时,胸骨伤口的愈合效果不令人满意。图1总结了持续采用常规包扎时的胸骨伤口愈合情况。
负压伤口治疗
采用持续NPWT时,在2周内胸骨伤口愈合8-29%。持续采用NPWT 3.5-5周时,平均伤口愈合达到13-24%。一个伤口在3周内达到50%的愈合。在6-7周的较长时间内持续采用NPWT时,仅获得15-46%的胸骨伤口愈合。一位受试者在持续采用NPWT 13周后出现39%的胸骨伤口愈合。图2显示对胸骨伤口单独持续采用NPWT后伤口愈合欠佳情况。
在存在胸骨钢丝的情况下,持续采用NPWT 1-2周时,观察到伤口改善6-24%。在NPWT持续4周后,最多可实现29%的胸骨伤口愈合(图3)。
在拆除胸骨钢丝后,采用NPWT后胸骨伤口愈合略有改善。在1到1.5周内观察到6%至18%的胸骨伤口愈合。采用NPWT 2周后,胸骨伤口愈合达到平均14-34%。采用NPWT 2.5周时,观察到胸骨伤口愈合0%至46%。然而,持续采用NPWT 2-3周后,发现个别伤口恶化结果,伤口愈合19.4%(图4)。
在3个接受外科清创术的病例中,清创术后胸骨伤口愈合未见明显改善,NPWT治疗2周后胸骨伤口愈合率为16%至23%,NPWT治疗4.5周后胸骨伤口愈合率最高,达26%(图5)。
总体而言,在本综述中,持续采用NPWT达到的胸骨伤口愈合情况欠佳。存在胸骨钢丝时,持续采用NPWT可延迟胸骨愈合,而拆除胸骨钢丝可以改善NPWT对胸骨伤口愈合的效果。
即使NPWT和外科清创术,也可能发生伤口恶化的情况。
停止NPWT
除了因外科清创术或钢丝拆除术而中断持续NWPT之外,在伤口护理结束时也因多种其他原因中断NPWT(表4)。采用皮瓣成功重建胸骨伤口缺损(27.3%)以及适合使用常规包扎的理想伤口恢复情况(36.4%)是停止NWPT的主要原因。停止NPWT的其他原因有外科医生的医疗决定和治疗处方(18.2%)以及出院回家(18.2%)。在本回顾性研究结束时,一名受试者仍在接受持续NPWT胸骨伤口护理。除了单独采用NPWT带来的伤口改善外,在NPWT后进行皮瓣重建对胸骨伤口愈合起到了关键作用。
讨论
根据文献,术后DSWI相对更常见于接受联合心胸手术的患者中4,7。在本综述中,没有在接受联合心胸手术的患者(75%)与接受单一心胸手术的患者(70%)之间观察到DSWI发生率存在显著差异。然而,由于大多数选定受试者(71.4%)都出现了DSWI,表明DSWI的明显发病率不容忽视。
在本综述中,我们的发现与先前的文献有关联性,在先前的文献中常规包扎对胸骨伤口愈合没有显著积极的效果。在常规伤口护理下,单纯性胸骨间隙伤口或伤口存在胸骨钢丝时愈合效果相似,均不令人满意。在本综述中,在拆除钢丝和外科清创术后,使用常规伤口护理方法仅稍微改善了胸骨愈合效果。根据先前的文献和我们的发现,常规包扎对胸骨伤口愈合的总体效果有限。
近年来,NPWT已成为胸骨伤口管理中的一种不断发展的伤口护理方式10,11,14,15。在本综述中,与常规伤口护理相比,采用NPWT获得的胸骨伤口愈合效果更好。尽管如此,NPWT实现的胸骨伤口愈合仍然欠佳。在本综述中,持续采用NPWT 5周后,胸骨伤口愈合率低于30%,持续采用NWPT 6-7周后,观察到的愈合率低于50%。持续采用NPWT时,一些受试者的胸骨伤口愈合仍出现了恶化。对于一些胸骨伤口,外科清创术后采用NPWT无法改善其愈合效果。在本综述中,拆除胸骨钢丝后,发现持续采用NPWT改善了胸骨伤口愈合。
随着NPWT时间的延长,伤口愈合停滞更常见,而不是完全伤口愈合。此外,NPWT组的胸骨伤口愈合进展缓慢。
结果分析表明,采用NPWT后,皮瓣重建作为胸骨伤口三期闭合的方法起到重要的作用。尽管单独应用NPWT对胸骨伤口愈合的效果欠佳,但本综述支持NPWT在胸骨伤口三期闭合和愈合中的桥接作用。
以前曾报道,存在DSWI时,NPWT是一种安全可靠的伤口护理选择,与常规包扎相比,可以提高存活率并降低失败率。存在DSWI时,预防措施应侧重于优化可修改的临床因素3。糖尿病控制、手术时间、围手术期体温调节和抗生素覆盖范围都是一些提到的可修改的临床因素,可以通过调节这些因素最大限度减少DSWI7。双侧胸内动脉移植术、需要输血、急诊手术、既往支架植入术和术后使用强心剂也预示胸骨切开术后DSWI的风险增加8。已知存在感染会抑制伤口愈合。采用NPWT有利于间接治疗DSWI并间接降低DSWI相关死亡率,通过稳定胸廓、减少细菌定植和伤口水肿、促进微血管血流和肉芽组织形成以及最小化感染风险等途径实现11。因此,尽管我们在综述中观察到胸骨伤口愈合欠佳,但是NPWT仍然在促进胸骨伤口愈合进展中起重要作用。
文献中已经讨论了导致胸骨伤口愈合欠佳的多种可能因素。已经确定重新缝钢丝失败与伤口培养物阳性、血培养阳性、获取左侧乳内动脉后造成的胸壁血供中断和细菌耐药性呈正相关6,8。即使进行清创术和重新缝钢丝,局部或全身感染也会导致不利的胸骨伤口愈合结果。当伤口培养结果连续三次阴性时,感染胸骨伤口成功重新闭合的可能性增加3.3倍8。如果细菌种类发生显著变化,长时间采用NPWT可以刺激感染复发。患者相关因素,如血液动力学状况和胸骨生存力,以及当地环境因素,如提供材料和专业知识,也影响NPWT对胸骨伤口愈合的效果4。导致胸骨伤口愈合和边缘闭合欠佳的其他因素有:胸部皮肤相对较薄导致真皮层只有中等厚度18、连接胸骨的双侧胸大肌施加力量19、胸壁随呼吸持续性扩张、存在诸如胸骨钢丝等异物以及胸骨伤口的内部结构暴露。
基于本回顾性综述中的发现,以及影响胸骨伤口愈合的可能因素和单独采用NPWT时胸骨伤口愈合欠佳,认为NPWT通过其桥接作用有益于胸骨伤口愈合。NPWT有助于对胸骨进行预先处理以及保护胸骨,以进行进一步的外科清创术和伤口愈合9。这一点进一步得到了一份报告的支持。该报告中,在确定NPWT是一个安全选项,并对存在DSWI的胸骨伤口或胸骨开裂成功重建后,延期实施胸骨钢板固定或双侧胸大肌皮瓣重建20。在重建或进一步手术修复之前,采用理想持续时间的NPWT可促进肉芽组织的生长、降低细菌负荷,并且促进CRP水平下降。在伤口护理中采用NPWT仍然可能产生副作用,例如器官或内部结构损伤和出血,这也限制了NPWT的采用或持续使用。采用NPWT时,通过石蜡纱布或伤口接触层小心保护心脏和血管等内部结构非常重要11。
在本回顾性综述中,在需要胸骨切开术的受试者中,采用NPWT后成功实现三期闭合,这与文献中的观点共识一致,即NPWT在开放性胸骨伤口的管理中起着重要的桥接作用。
由于缺乏研究变量和对照(例如DSWI的程度和单纯性胸骨裂开)、样本量小和本研究的回顾性质,这些都限制了我们以确定的方式分析NPWT对胸骨伤口愈合的影响。直接针对NPWT影响胸骨伤口愈合的研究有限。仍然需要更大规模、更大样本量和更好病例对照的进一步研究评估NPWT对胸骨伤口的直接影响,以便可能获得有价值的知识信息和重大的成果。在NPWT后对胸骨伤口实施重建术的情况下,NPWT对感染控制、CPR水平和伤口完全愈合时间的影响值得进一步研究。探索从NPWT转换到胸骨伤口重建或修复的最佳时机也将有利于将来的胸骨伤口护理。
结论和未来前景
对于接受过心胸外科手术的患者而言,胸骨伤口愈合仍然是一个挑战,无论是否出现胸骨后切开术后纵隔炎、术后伤口裂开或开放性手术伤口。在过去十年中,NPWT已被成功用于胸骨伤口管理,比常规包扎更具优势。本回顾性综述发现,单纯采用NPWT可导致胸骨伤口的伤口愈合停滞。然而,作为一个桥接过程以便为进一步皮瓣重建术或其他三期闭合方法准备胸骨伤口,NPWT确实在胸骨伤口愈合中表现出有希望的功能性结果。将NPWT作为预先处理胸骨伤口的一个桥接方法,然后进行三期闭合,可能会成为胸骨伤口护理的主要方法。这一观点得到了先前文献和本回顾性综述的支持。尽管如此,如前所述,仍然缺乏针对NPWT直接影响胸骨伤口愈合的大规模研究。应进一步研究和探索停止NPWT和切换到重建术的最佳时机。例如,实施NPWT后的健康肉芽组织量、CRP转为正常或白细胞计数水平。在未来,需要更多的研究和知情的理解,以制定关于最佳胸骨伤口护理的循证指南和临床路径。
利益冲突
作者声明没有利益冲突。
资助
作者未因该项研究收到任何资助。
Author(s)
Wai Sze Ho
Stoma and Wound Care Unit, Department of Surgery, Queen Mary Hospital, Hong Kong
Wai Kuen Lee
Stoma and Wound Care Unit, Department of Surgery, Queen Mary Hospital, Hong Kong
Ka Kay Chan
Stoma and Wound Care Unit, Department of Surgery, Queen Mary Hospital, Hong Kong
Choi Ching Fong
Stoma and Wound Care Unit, Department of Surgery, Queen Mary Hospital, Hong Kong
Correspondence to Wai Sze Ho
Email hws020@ha.org.hk
References
- Borger MA, Rao V, Weisel RD et al. Deep sternal wound infection: risk factors and outcomes. Ann Thorac Surg 1998; 65(4):1050–1056.
- Feo MD, Gregorio R, Corte AD et al. Deep sternal wound infection: the role of early debridement surgery. Eur J Cardiothorac Surg 2001; 19(6):811–816.
- Deniz H, Gokaslan G, Arslanoglu Y et al. Treatment outcomes of postoperative mediastinitis in cardiac surgery; negative pressure wound therapy versus conventional treatment. J Cardiothorac Surg 2012; 7(1):67–73.
- van Wingerden JJ, Ubbink DT, van der Horst CM & de Mol BA. Post sternotomy mediastinitis: a classification to initiate and evaluate reconstructive management based on evidence from a structured review. J Cardiothorac Surg 2014; 9(1):179–187.
- Cutrell JB, Barrows N, McBroom M et al. Risk factors for deep sternal wound infection after cardiac surgery: influence of red blood cell transfusions and chronic infections. Am J Infect Control 2016; 44(11):1305–1312.
- 6Meszaros K, Fuehrer U, Grogg S et al. Ann Thorac Surg 2016; 101(4):1418–1425.
- Sears ED, Wu L, Waljee JF et al. The impact of deep sternal wound infection on mortality and resource utilization: a population-based study. World J Surg 2016; 40(11):2673–2680.
- Golosow LM, Wagner JD, Feeley M et al. Risk factors for predicting surgical salvage of sternal wound-healing complications. Ann Plast Surg 1999; 43(1):30–35.
- Baillot R, Cloutier D, Montalin L et al. Impact of deep sternal wound infection management with vacuum-assisted closure therapy followed by sternal osteosynthesis: a 15-year review of 23,499 sternotomies. Eur J Cardiothorac Surg 2010; 37(4): 880–887.
- Sjögren J, Malmsjö M, Gustafsson R & Ingemansson R. Post sternotomy mediastinitis: a review of conventional surgical treatments, vacuum-assisted closure therapy and presentation of the Lund University Hospital mediastinitis algorithm. Eur J Cardiothorac Surg 2006; 30(6):898–905.
- Morisaki A, Hosono M, Murakami T et al. Effect of negative pressure wound therapy followed by tissue flaps for deep sternal wound infection after cardiovascular surgery: propensity score matching analysis. Interact Cardiovasc Thorac Surg 2016; 23(3):397–402.
- Berg HF, Willem GB, Brands WGB et al. Comparison between closed drainage techniques for the treatment of postoperative mediastinitis. Ann Thorac Surg 2000; 70:924 –9.
- Huang C, Leavitt T, Bayer LR & Orgill DP. Effect of negative pressure wound therapy on wound healing. Curr Probl Surg 2014; 51(7):301–331.
- Schols RM, Lauwers TMAS, Geskes GG & van der Hulst RRWJ. Deep sternal wound infection after open heart surgery: current treatment insights. A retrospective study of 36 cases. Eur J Plast Surg 2011; 34(6):487–492.
- Oeltjen JC, Panos AL, Salerno TA & Ricci M. Complete vacuum-assisted closure following neonatal cardiac surgery. J Card Surg 2009; 24(6):748–750.
- Cotogni P, Barbero C & Rinaldi M. Deep sternal wound infection after cardiac surgery: Evidences and controversies. World J Crit Care Med 2015; 4(4):265–273.
- Bates-Jensen wound assessment tool, 2001. Retrieved 18 January 2017, from http://www.geronet.med.ucla.edu>borun
- Pourtaheri N & Soltanian H. Chest wall anatomy, 2016. Retrieved 11 May 2016, from http://emedicine.medscape.com/article/2151800-overview#a2
- Costosternal anatomy, n.d. Retrieved 11 May 2016, from http://www.chiropractic-help.com/costosternal-anatomy.html
- Damiani G, Pinnarelli L, Sommella L et al. Vacuum-assisted closure therapy for patients with infected sternal wounds: a meta-analysis of current evidence. J Plast Reconstr Aesthet Surg 2011; 64(9):1119–1123.


