Volume 39 Number 2
Impact of chronic osteomyelitis on wound healing and the quality of life of the patient with a chronic wound
Swapna Johnson-Kunjukutty and Carmel Delille
Keywords Chronic osteomyelitis, spinal cord injury, psychological impact
For referencing Johnson-Kunjukutty S and Delille C. Impact of chronic osteomyelitis on wound healing and the quality of life of the patient with a chronic wound. WCET® Journal 2019; 39(2):34–40
DOI https://doi.org/10.33235/wcet.39.2.34-40
Abstract
Spinal cord injury (SCI) patients have a higher risk of developing pressure injury secondary to limited mobility and lack of sensation. The James J Peters Medical Center is one of several regional spinal cord injury centres in the Veterans Affairs System. Veterans with SCI receive comprehensive care. Hospital- and community-acquired pressure injuries (HAPIs and CAPIs) can progressively advance to chronic stage IV pressure injury complicated with osteomyelitis. Chronic wounds that become infected can lead to sepsis if the wounds are not managed properly. The management of chronic wounds represents a significant financial burden for any health care system and a challenge for providers whose goals are to avoid prolongation of hospital stay, avoid complications, and minimise disruption in the patient’s life. A focus of the primary physician is to establish a rehabilitation plan that facilitates the patient to resume activities of daily living post injury and have a productive life in their community. However, despite the collaborative effort of the SCI team, the sudden change in the patient’s mobility can also have a detrimental impact on the patient’s mental status as well.
Introduction
The patient presented shows the pathogenic nature of spinal cord injury (SCI), the difficulty in managing, and the impact these wounds had on his quality of life. Even though the development of a pressure injury is widely known in the medical community, the complexity of the patient’s medical conditions, the complications encountered along the way in the management of this patient’s wounds, and the variability in diagnostic test results have largely contributed to delaying the healing trajectory. The anxiety and the depression the patient experienced since the development of his wounds are most likely linked to the chronicity of the wounds as well. This article is intended to raise awareness of the impact of chronic wounds on the individual’s quality of life and the challenges faced by clinicians who cared for him.
Case Presentation
Joe is a 34-year-old, African-American, male veteran, who sustained T3 SCI that resulted in paraplegia after a motorcycle accident in 2004. He presented to James J Peters Medical Center in April 2009 with general malaise, ill feeling for one month, fever and chills. He had developed four pressure injuries at different stages of tissue degradation at home. The initial measurements of the wounds are as follows:
- Left trochanter: initially unstageable and progressed to stage IV pressure injury that measured 8 cm x 8.5 cm x 1.5 cm (Figure 1).
- Left gluteal: stage IV pressure injury that measured 4 cm x 4.5 cm x 3 cm with undermining from 3 to 8 o’clock that extended to 3 cm at 3 o’clock (Figure 2).
- Right trochanter: stage IV pressure injury that measured: 12 cm x 10 cm x 2.5 cm (Figure 3).
- Right gluteal: stage II pressure injury that later progressed to a stage IV pressure injury (Figure 4).
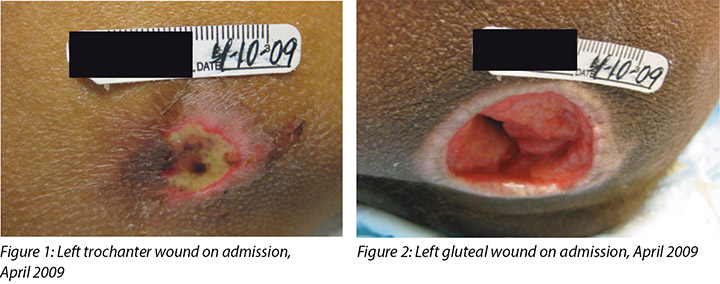
The admitting diagnosis was sepsis secondary to an infected stage IV pressure injury on left gluteal, greater trochanter of right femur. A bone scan obtained confirmed the presence of osteomyelitis of the left gluteal and the greater trochanter region of the right femur. The patient received initial treatment in the intensive care unit (ICU) and was transferred to the SCI unit two days later.
Treatment
The patient was admitted to the ICU and empirically treated with broad-spectrum Vancomycin and Zosyn based on the clinical suspicion of wound infection. Bone cultures were not obtained prior to the administration of antibiotics. An infectious disease (ID) consultation was requested five days after admission, and the recommendation was to continue with the current selection of antibiotics for two weeks and switch to Levofloxacin PO for six weeks. He had surgical debridement of the left gluteal and left trochanter. A year later he had surgical excision and debridement of the right gluteal bone and the right trochanter.
The proximity of the bilateral gluteal wounds to the rectum predisposed this patient to recurrent infection from faecal contamination. He remained hospitalised for an extended period of time due to chronic osteomyelitis. In the interim, Joe’s wound management included: culture of bone which grew Staphylococcus aureus (MRSA), wounds and bone debridement, 16 weeks of Bactrim DS, and application of several topical wound modalities. For a while there was a decrease in sedimentation (SED) rate, prealbumin improved, and over all, his physical appearance improved. However, he remained concerned and reluctant to get out of bed and he declined any involvement in recreational activities that were available to him.
The chronicity of his condition remained critical within his pelvis. In February 2011, Joe was reassessed for osteomyelitis by gallium scan and found to have positive results. The ID consultant recommended PICC line placement for six weeks of Daptomycin to treat the persistent MRSA found on wound cultures. In late 2011, Joe developed sepsis from the PICC line and consequently was transferred to the ICU for two weeks. Upon his return to the SCI unit, his care was assigned to another physician. The issues identified on transfer of care were: iron deficiency, poor appetite, bouts of nausea, and chronically low pre-albumin. The patient appeared withdrawn and communicated his needs in very short sentences. He denied any depressive symptoms and declined offers to be seen by psychologist. Joe expressed interest in going home.
In December 2011, Joe went back to the operating room for excision and wound debridement of both gluteal pressure injuries and multiple bone biopsies after magnetic resonance imaging (MRI) confirmed the presence of chronic osteomyelitis. The bone biopsies grew MRSA and Acinetobacter baumannii. The patient developed tongue swelling to cephalosporins, so the ID physician recommended giving Daptomycin and Imipenem for 10 days followed by Bactrim DS for an extended course, with the duration to be determined by response on follow-up imaging.
Gastroenterology consultation was requested for evaluation of chronic inflammation and persistent weight loss. It was determined that the patient did not have inflammatory bowel disease and a colonoscopy was not recommended. A nutritional consultation was made subsequently and the patient’s caloric intake was monitored. Furthermore, an appetite stimulant was prescribed. No improvement was noted in the patient's weight in the next four weeks that followed.
Joe’s case was discussed with the interdisciplinary team, consisting of physicians, a general surgeon, a certified wound ostomy nurse, a dietitian, a psychologist, several occupational and physical therapists, and a social worker to provide a holistic approach. A trial of enteral feeding via nasogastric tube was initiated at night with continued oral intake during the day. As a result, the patient gained weight and there was noticeable improvement in the wounds' appearance. Specifically, the wound bed appeared 100% granular and the wound edges were contracting. A PEG tube was placed and Joe was in charge of doing the supplemental feeding in addition to his regular oral intake.
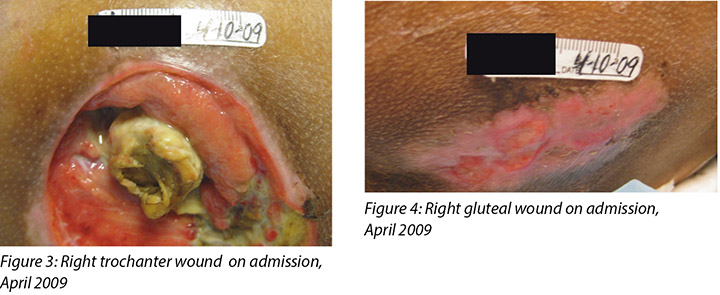
After a while, Joe did not adhere with the prescribed instructions and consequently a significant reduction in his weight was apparent and deterioration in the wounds' bed was noticeable as well. In our team discussion it was decided that a change in Joe’s environment and the company of relatives might contribute in lifting his spirit. The patient was encouraged initially to spend the weekend at home with the ultimate goal of achieving total reintegration into the community. Joe was discharged home in 2013, nearly four years after his SCI admission, with three wounds:
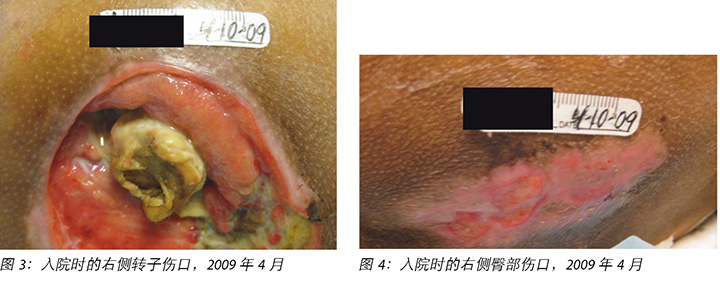
- Right trochanteric wound 1.7 cm L x 0.9 cm W x 0.6 cm D (Figure 5).
- Right gluteal wound measured: 4.2 cm L x 3 cm W x 1.7 cm D with undermining circumferentially with the deepest part documented at 3.3 cm at 12 o’clock (Figure 6).
- Left gluteal wound 1.5 cm L x 1.2 cm W x 2.2 cm D, with undermining circumferentially that it extended to 3.1 cm at 12 o’clock (Figure 7).
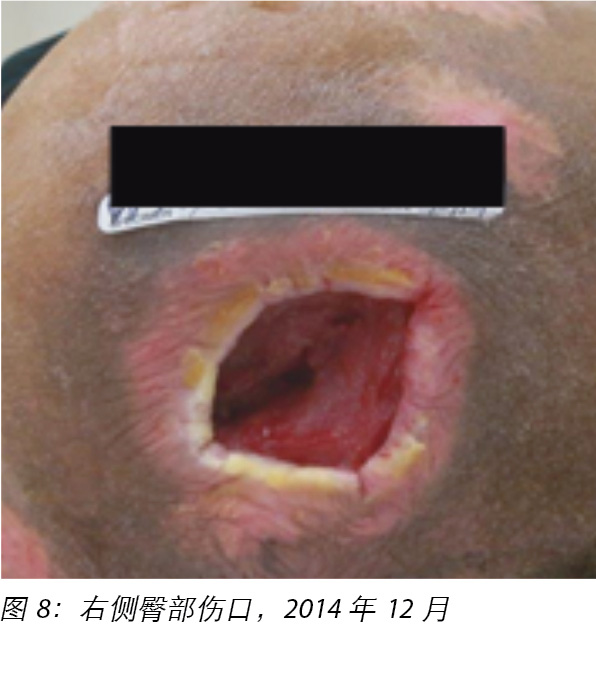
At home, Joe had easier access to his food preferences and his nutritional status improved without the need of supplementation. He freely maintained his weekly schedule for follow-up assessments at the SCI outpatient clinic, with routine blood work including CBC, BMP, prealbumin, ESR and CRP obtained at least monthly. He continued to improve. His right trochanteric wound intermittently closed and re-opened. His left gluteal wound healed. His right gluteal wound periodically showed some improvement and then there was some regression in the healing process (Figure 8).

Two and a half years after discharge, an MRI of the pelvis was ordered; the findings were consistent with chronic osteomyelitis involving the right hip, predominately the right acetabulum posterior and medial walls. Findings were similar when compared with a diagnostic test obtained 18 months earlier. Joint effusion was present. An ID physician was therefore consulted. Her impression was:
Underlying osteomyelitis is clearly chronic in nature. Patient completed several courses of antibiotic in the past and administering another course of antibiotics will likely not cure his underlying osteomyelitis. The last culture was positive for an ESBL proteus mirabilis, which could be treated with Ertapenem IV daily. However, I recommend treatment only if patient is symptomatic with pain and erythema (like an exacerbation of his chronic osteomyelitis). Chronic suppressive antibiotics have been prescribed for chronic osteomyelitis; however, previous cultures grew an ESBL. There are no good oral options available and I do not think long term suppression is necessary, unless patient has frequent exacerbations. Would check quantitative C-reactive protein (CRP) and ESR now and definitely if he is taking any kind of AB (in case he becomes symptomatic). Otherwise no need to treat the patient with antibiotics for chronic osteomyelitis.
The provider, in agreement with the ID physician, did not support administration of long-term antibiotic suppression therapy, unless the patient experienced frequent exacerbations. Joe’s quantitative CRP and ESR were closely monitored, and antibiotic treatment was considered based on clinical presentations. The wound on the right gluteal showed slow but gradual improvement.
Two years later, a gallium scan was inconclusive for osteomyelitis (Figure 9). A year later, Joe received another short course of antibiotics for a wound infection based on culture results. Over the past years, the treatment plan for this patient included a variety of evidence-based dressings available on the market, namely: Collagenase, Medihoney™, Plurogel™, Collagen, Oasis™, and Biologics Epifix™, Grafix™, and Hyalomatrix™ dressings were applied with the goal of achieving complete wound healing.

In December 2016, Joe developed another abscess between the right gluteal and the right trochanteric wounds. This abscess was drained and a few weeks later a tiny opening was noted that connects to the right gluteal wound, which formed a tract into the right medial fossa (Figure 10). This finding was confirmed by an MRI.

This superficial wound, unlike the previous abscess did not heal. Over the course of eight weeks, several topical treatments were applied, none of which were successful in facilitating the desired outcome. Since the wound showed no improvement, an MRI of the pelvis was ordered, which showed some mild marrow signal changes within the posterior column of the right acetabulum adjacent to this soft tissue process. Overall, marrow signal changes within the right acetabulum are decreased from the previous scan. At the time of the MRI, the impression was that there was overall improvement because of the decrease in marrow signal changes.
Joe’s case was discussed during the wound care board committee. The committee suggested that biofilm might be the culprit impeding wound healing based on the clinical course. Their recommendation included pulse lavage followed by application of Plurogel™. This method was tried for one month without improvement. Next, a consultation for hyperbaric oxygen therapy was suggested but this treatment option was contraindicated because of Joe’s past history of spontaneous pneumothorax.
The patient was referred to another institution for a second opinion. After reviewing MRI reports, the consulting wound care MD, in tandem with the radiologist at that health care facility, concurred that Joe still had chronic osteomyelitis, and recommendations included surgical debridement, a prolonged course of antibiotic and hyperbaric oxygen therapy concurrently. Hyperbaric oxygen was not pursued because of the patient’s previous history of spontaneous pneumothorax. The consultant stated clearly that osteomyelitis of the pelvis in most cases is incurable. Aggressive debridement of the pelvis may result in poor sitting balance, which would have a devastating effect on Joe’s overall well-being.
Follow-up wound assessment of all the wounds conducted revealed that the wound beds were covered with friable and pale tissue. A wound culture and sensitivity obtained initially grew multidrug-resistant MRSA, and later Proteus. The treatment plan included Bactroban and Bactrim for MRSA, but no improvement was observed after two weeks. Subsequently Ertapenem was added to treat the Proteus. He received Ertapenem 1 gm intramuscular daily administered by a visiting nurse. Joe’s case was presented at an ID departmental meeting, and a decision was made to administer a prolonged course of antibiotics based on Joe’s clinical presentation.
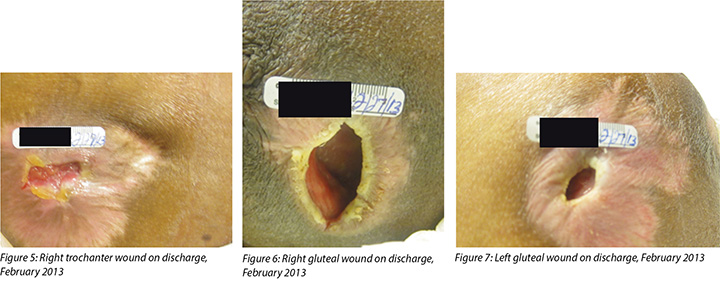
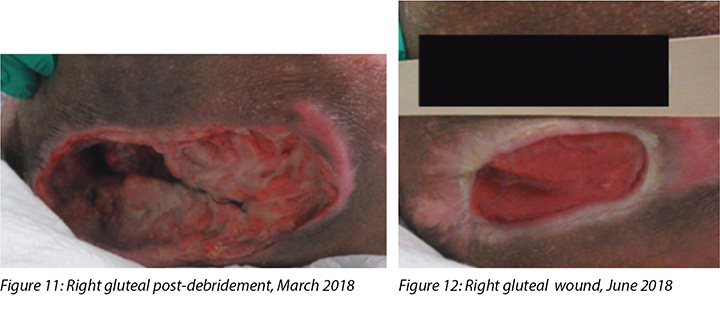
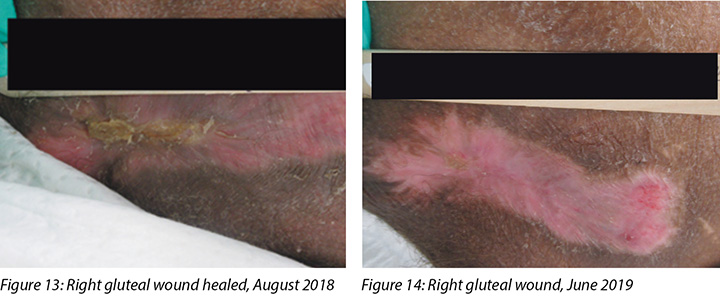
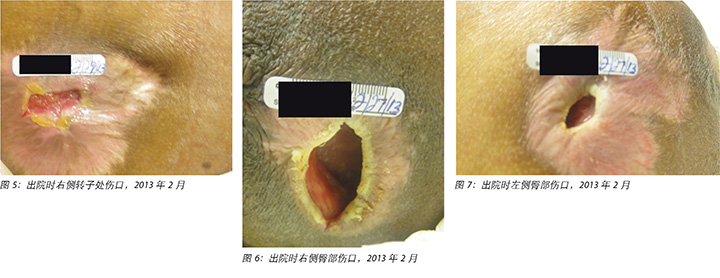
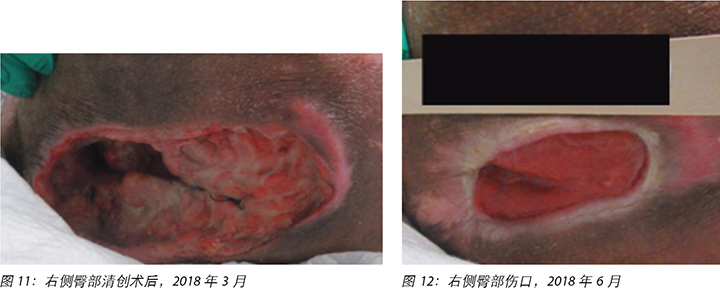
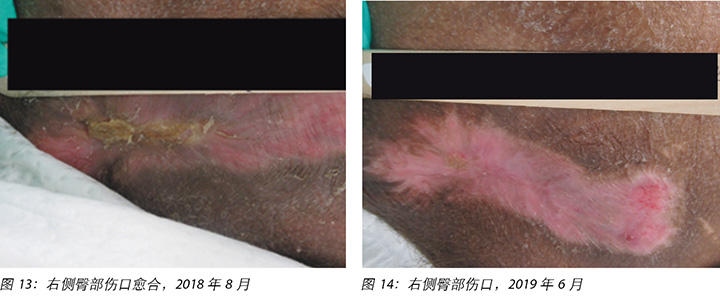
After six months, the right gluteal wound had stalled and a decision was made to admit Joe and he finally agreed to proceed with a colostomy formation prior to an aggressive surgical debridement to facilitate management of the wound. In March 2018, bone cultures were taken at the time of debridement and showed persistent MRSA (Figure 11). Joe was given two doses of once-weekly Dalbavancin followed by four doses of once-weekly Oritavancin (Figure 12). His inflammatory markers improved and his wound healed by August 2018 (Figure 13). Joe’s inflammatory markers were continually monitored and subsequently he was commenced on chronic suppressive therapy with minocycline 100 mg orally twice a day. Figure 14 represents complete right gluteal wound closure.
As health care providers, the treating multidisciplinary team had so many unanswered questions. At what point did the conversion from acute to chronic osteomyelitis occur? Was Joe not treated sufficiently? Could this have been managed differently? What about imaging? Why does it not provide a clear picture?
Discussion
Labs to detect bone infection
It is known that X-rays do not reveal early osteomyelitis. They are effective in showing the damage caused by osteomyelitis such as sequestra; however, they do not expose the current activity level of the infection1. A computerised axial tomography (CAT) scan may depict intramedullary and soft tissue gas, sequestra, sinus tracts, and foreign bodies. However, CAT scanning is insufficient for the assessment of the activity of the process1. Nuclear imaging has high sensitivity for detecting evidence of inflammation and therefore tends to be more reliable for evaluation of acute infection than chronic infection. MRI has increased sensitivity and negative predictive value in osteomyelitis, especially for early disease1. MRI often lags behind clinical improvement and sometimes it can remain abnormal in appearance for months post therapy1. It is important to remember that imaging is intended to support the diagnosis, but is not exclusively diagnostic; it must be put in perspective with the entire clinical picture.
In Joe’s case, his inflammatory markers were always high, so it was difficult to use that as a guide. On review, the last MRI report showed some:
... mild bone marrow signal changes within the posterior column of the right acetabulum adjacent to this soft tissue process, which may represent reactive marrow changes. In comparison, overall marrow signal changes within the right acetabulum are decreased from the previous examination.
The radiological findings did not clearly report osteomyelitis; consequently, the ordering physician interpreted this report as clinical improvement because of the decrease in marrow signal. In retrospect, one can conclude that the findings are consistent with chronic osteomyelitis.
Antibiotic therapy
The choice of antibiotic selection, administration route and duration of treatment for osteomyelitis remain debatable, resulting in different recommendations from different infectious disease physicians. It is generally accepted that the adequacy of debridement with a wide excision remains the most important clinical predictor of a successful outcome2,3. In Joe’s case, taking him back to the operating room was a concern because aggressive debridement in that affected area would most likely have resulted in poor sitting balance in addition to a larger wound. Having all of his care at one centre provided continuity in the management of his care, and provided quick access to all his records, including previous antibiotic regimens. Joe developed allergies to two classes of antibiotics, including sulfa drugs and cephalosporins. Therefore, treatment options were limited. Our ID team recommended Oritavancin because in recent studies it has been well tolerated and has good efficacy. It is also effective for S. aureus and effective in treating osteomyelitis4,5. We did an initial two weeks of Dalbavancin because it is similar to Oritavancin while we were awaiting procurement of Oritavancin6.
Quality of life issues
As clinicians and providers, after reflecting on the challenges of managing chronic wounds and overcoming obstacles that impede healing, we must consider the impact of chronic wounds on the patient. For Joe, the feeling of success and failure, and the uncertainty of his overall prognosis led to separate issues. When an individual believes that he is powerless in controlling what happens in his life, the adaptive skills become restrictive and often ineffective7.
In the hospital settings, Joe would try to be compliant with all pressure injury preventative measures. He would be very attentive to the wound care instructions and would enquire about indication for dressings and compare the benefits of one dressing over another. Joe did not demonstrate any obviously unhealthy behaviours; however, periodically he would neglect his appearance, not shaving or cutting his hair. He would often refuse the meals served at the hospital, or let the cans of supplement accumulate at the bedside. His sleeping pattern was inconsistent. At times he would pretend to be asleep to avoid talking or interacting with the nursing staff. For instance, he would state that he is remaining in bed to expedite the healing process. He planned his life around his wound care schedule. Often he verbalised that he “is waiting for the wound to heal” to initiate involvement in social settings and school enrolment. Often time his mood would be affected by the discussion about the status of the wounds. He would become quiet and withdrawn if it was reported that the wound did not show any improvement or become talkative and friendly if he received positive feedback.
It is documented that psychological distress may exert a clinically relevant impact on wounds8. Stress has been known to reduce the amount of inflammatory mediators, prolonging the inflammatory stage of healing, thus increasing the overall healing8. Staff repeatedly reminded him that we do not have a time frame for his wound to achieve complete closure, and strongly discouraged him to place his life on hold.
Goals of care
A shared goal of our SCI multidisciplinary team was to continually encourage the patient entrusted to our care to adapt, advance, and to achieve their maximum potential after the injury. All care plans are focused towards achieving that goal. We work collaboratively to maximise the patient’s quality of life to be the best it can be. Oftentimes in hospital settings the patient’s medical condition takes priority. However, we need to consider factors such as sleep deprivation, psychological distress, stress, depression, pain, the length of hospital stay, and their impact on the patient’s social life.
Joe’s wounds below the level of his SCI deprived him of the ability to feel pain. It is reported that pain receptors are still triggering in those areas, thus causing local inflammatory responses that may inhibit the healing process9,10. The literature also reveals that limited sleep decreases growth hormone secretion that results in decreasing monocyte migration, activation of microphages and protein deficiency. Consequently, capillary formation, collagen synthesis, and wound remodelling are decreased8.
Depression also has been linked to a delay in wound healing8. Joe never had a positive depression screen, but social isolation was apparent in his avoidance of activities or refusal to participate in trips arranged by the recreational therapist. His behaviour could be attributed to depression, but he denied depressive symptoms. Joe is a very clean individual and was very concerned about his surroundings being contaminated; the amount of exudate and the odour emanating from the wound have significantly contributed to self-social isolation. These aspects of chronic wounds have prevented him from considering companionship or having a meaningful relationship with a woman.
The importance of providing social support and reducing stress for Joe was crucial in promoting healing of his wounds. The multidisciplinary team strived to promote self-confidence in Joe by reminding him of his resilience, and his strength in overcoming and surviving his injury11. It was continually reinforced that those two elements are key to achieving positive adaptation and experiencing an enjoyable life in the community.
Conclusion
People with SCI are prone to developing pressure injuries because of their limited mobility and lack of sensation. The wounds developed in this population of patients are often chronic or recurrent. Infected wounds can lead to sepsis and are often affected with secondary osteomyelitis. The management of these wounds is complex and they represent a tremendous financial burden for the medical institution. In addition, they significantly disrupt the patient’s way of life despite the provider’s best efforts to encourage and assist the patient in regaining some type of control in their environment and having a normal, productive life.
The SCI multidisciplinary team has witnessed the detrimental impact of these types of chronic wounds on our patient’s quality of life, and the presence of osteomyelitis in these wounds render their management even more complex. Joe’s case helped the SCI team realise that sometimes too much emphasis is placed on radiologic diagnosis. The literature states that imaging is considered a supportive test but is not diagnostic. It is crucial that a comprehensive multidisciplinary approach be implemented from the beginning to ensure that a positive outcome is achieved, thus avoiding lasting complications. During the journey in managing Joe’s wounds, the SCI team realised the importance of identifying and selecting a treatment plan that would be most beneficial for Joe’s overall well-being. The goal was to ensure that complete wound closure was achieved promptly, to enable Joe to reach his maximum potential post injury.
Health service providers and clinicians must always consider the possibility that chronic osteomyelitis may be the causative factor in chronic, non-healing soft tissue wounds12. To ensure the appropriate treatment is implemented early, to mitigate long-term effects and avoidable suffering for the patient and to shorten hospital stay and contain costs, a definitive diagnosis is essential. As clinicians, it is clear that the management of complex wounds requires interprofessional collaboration to address every component that may impede wound healing. When in doubt, clinicians should not hesitate to request consultation from other expert providers to ensure that the patient is well informed and receives the best possible care.
Acknowledgements
We would like to thank the SCI and ID teams at James J Peters VAMC as well as Dr Kathleen Capitulo for support, encouragement and comments on earlier versions of the manuscript.
Conflict of Interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
慢性骨髓炎对伤口愈合的影响和慢性伤口患者的生活质量
Swapna Johnson-Kunjukutty and Carmel Delille
DOI: https://doi.org/10.33235/wcet.39.2.34-40
摘要
脊髓损伤(SCI)患者由于行动受限和缺乏感觉发生压力性损伤的风险较高。James J Peters医疗中心是退伍军人事务系统中的几个偏远地区的脊髓损伤中心之一。患有SCI的退伍军人接受全面护理。医院和社区获得性压力性损伤(HAPI和CAPI)可逐步进展为伴有骨髓炎的慢性IV期压力性损伤。如果伤口管理不当,感染的慢性伤口会导致败血症。对于任何医疗保健系统来说,慢性伤口管理都是一个重大的经济负担,而且对于那些旨在避免延长住院时间、避免并发症并尽量减少对患者生活产生干扰的医疗服务提供人员来说是一项挑战。主治医师重点关注的是制定一个康复计划,以帮助患者在受伤后恢复日常生活中的活动,并在他们的社区中过上充实的生活。然而,尽管SCI团队共同努力,患者的行动能力突然变化也可能对患者的精神状态产生不利影响。
前言
本文介绍的患者患有脊髓损伤(SCI),在管理损伤方面有难度,并且这些伤口对他的生活质量产生了影响。尽管压力性损伤的发展在医学界广为人知,但是患者症状的复杂性、在管理伤口过程中遇到的并发症,以及诊断检测结果的可变性在很大程度上导致了愈合延迟。患者因伤口发展而经历的焦虑和抑郁很可能与慢性伤口有关。本文旨在提高人们的认识,使人们了解慢性伤口对个人生活质量的影响以及经治临床医生所面临的挑战。
病例介绍
乔是一名34岁非洲裔美国男性退伍军人,在2004年因摩托车事故后出现T3 SCI,最终导致截瘫。他于2009年4月来到James J Peters医疗中心,当时全身不适,有一个月感觉不适,并且有发烧和寒战症状。在家中时,他在组织退化的不同阶段发生了四次压力性损伤。伤口的初始测量如下:
- 左侧转子:最初是不明确分期的伤口,并且进展到IV期压力性损伤,测量大小为8 cm × 8.5 cm × 1.5 cm(图1)。
- 左侧臀部:IV期压力性损伤,测量大小为4 cm × 4.5 cm × 3 cm,3点钟至8点钟方向有潜行伤口,在3点钟方向延伸到3 cm(图2)。
- 右侧转子:IV期压力性损伤,测量大小为:12 cm x 10 cm x 2.5 cm (图3)。
- 右侧臀部:II期压力性损伤,后来发展为IV期压力性损伤(图4)。
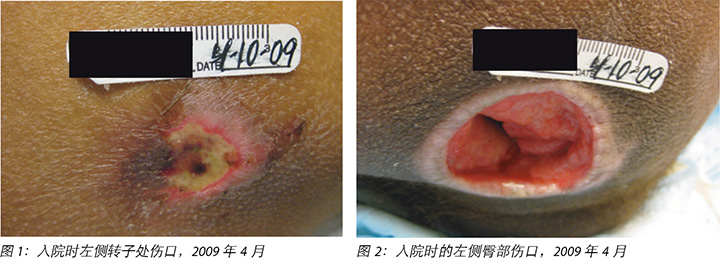
入院诊断为败血症,继发于左侧臀部、右侧股骨大转子感染的IV期压力性损伤。骨骼扫描结果证实左侧臀部和右侧股骨大转子存在骨髓炎。患者在重症监护病房(ICU)接受了初始治疗,两天后转移到了SCI治疗科。
治疗
由于临床怀疑伤口感染,患者入住ICU后接受广谱万古霉素和呱拉西林(Zosyn)经验性治疗。在施用抗生素之前未获得骨培养物。入院后的第五天,要求进行了感染病(ID)科会诊,建议是继续在两周内使用目前选择的抗生素,并改为口服左氧氟沙星六周。患者接受了左侧臀部和左侧转子外科清创术。一年后,患者接受右侧臀部和右侧转子手术切除和清创术。
双侧臀部伤口与直肠非常靠近,这使患者易于从粪便污染引起反复感染。由于慢性骨髓炎,他长时间住院。在此期间,乔的伤口管理包括生长金黄色葡萄球菌(MRSA)的骨培养、伤口和骨清创、16周复方新诺明(Bactrim DS),以及应用多种局部伤口治疗方式。在一段时间内,红细胞沉降(SED)率下降,前白蛋白得到改善,而且总体外观改善。然而,他仍然担心而且不愿下床,拒绝参与任何可以参加的娱乐活动。
他骨盆内的慢性症状仍然较为严重。2011年2月,乔通过镓扫描重新评估骨髓炎,结果为阳性。感染病顾问建议进行经外周静脉穿刺中心静脉置管(PICC),用达托霉素六周,以治疗伤口培养物中持续存在的MRSA。2011年底,乔因PICC置管引发败血症,因此被转移到ICU两周。在返回SCI科时,为其分配了另一位经治医生。在移交护理时发现的问题包括:缺铁、食欲不振、恶心发作以及前白蛋白含量长期低下。患者似乎变得沉默寡言,并以非常短的语句传达需求。他否认任何抑郁症状,并拒绝接受心理学家会诊。乔表示希望回家。
2011年12月,在磁共振成像(MRI)证实乔患有慢性骨髓炎后,他回到了手术室,对两处臀肌压力性损伤都进行了切除和伤口清创术,并进行了多处骨活检。骨活检生长出MRSA和鲍曼不动杆菌。患者服用头孢菌素后出现舌头肿胀,因此感染病医生建议服用达托霉素(Daptomycin)和亚胺培南(Imipenem)10天,然后以较长的疗程服用复方新诺明,持续时间根据后续成像结果确定。
患者接受肠胃病科会诊,以评估慢性炎症和持续性体重减轻。经确认,患者没有炎症性肠病,不建议进行结肠镜检查。随后进行了营养学会诊,并监测了患者的热量摄入情况。此外,还开了食欲促进剂。在接下来的四周内,患者的体重没有得到改善。
与跨学科团队讨论了乔的病例,该团队由医师、普通外科医生、认证的伤口造口护士、营养师、心理学家、几名职业和物理治疗师以及提供整体方法的社会工作者组成。在夜间开始通过鼻胃管进行肠内喂饲试验,并在白天持续口服摄入。结果,患者体重增加,伤口外观明显改善。具体来说,伤口床呈现100%颗粒状,伤口边缘正在收缩。除了常规经口摄食外,乔还通过PEG管自行补充摄入热量。
一段时间后,乔没有遵循规定的指示,因此他的体重明显减轻,并且伤口床的恶化也很明显。我们团队经讨论后决定要为乔改变环境,而且亲属的陪伴可能有助于提升他的精神。最初鼓励患者在家度过周末,最终目标是完全重新融入社区生活。因SCI入院将近四年后,乔于2013年出院,有三处伤口:
- 右侧转子伤口 1.7 cm 长 x 0.9 cm 宽 x 0.6 cm 深(图5)。
- 右侧臀部伤口测量大小:4.2 cm 长 x 3 cm 宽 x 1.7 cm 深,向四周潜行,最深部分为12点钟位置处3.3 cm(图6)。
- 左侧臀部伤口1.5 cm 长 x 1.2 cm 宽 x 2.2 cm 深,向四周潜行,在12点钟位置延伸至3.1 cm(图7)。
在家里,乔更容易获得他喜爱的食物,他的营养状况得到了改善,无需补充摄入。他自由地坚持每周前往SCI门诊接受随访评估,至少每月接受一次常规血液检查,检查包括全血细胞计数(CBC)、基础代谢检查(BMP)、血清前白蛋白、红细胞沉降率(ESR)和C-反应蛋白(CRP)。他继续得到了改善。右侧转子伤口间歇性地闭合后又开裂。左侧臀部伤口已愈合。右侧臀部伤口周期性地显示出一些改善,然后在愈合过程中有一些倒退(图8)。
在出院两年半后,对骨盆进行了MRI检查;检查结果符合右侧髋部骨髓炎,主要是在右侧髋臼后壁和内侧壁处。结果与18个月前获得的诊断测试相似。存在关节积液。因此,请了一位感染病医师进行会诊。她的会诊意见是:
骨髓炎的性质显然是慢性的。患者在过去完成了几个疗程的抗生素治疗,开始另外一个疗程的抗生素治疗可能无法治愈骨髓炎。上一种培养物对于超广谱β -内酰胺酶奇异变形杆菌呈阳性,可以每天静脉注射(IV)厄他培南(Ertapenem)进行治疗。但是,我建议只有在患者出现疼痛和红斑症状(如慢性骨髓炎恶化)时才进行治疗。对慢性骨髓炎采用长期抑制性抗生素;然而,以前的培养物生长出了ESBL。没有较好的口服药物选择,我不认为有必要长期使用抑制性抗生素,除非患者的病情频繁加重。现在检查定量C-反应蛋白(CRP)和红细胞沉降率(ESR),如果他正在使用任何一种抗生素(AB),那么肯定要检查(如果出现症状)。否则无需用抗生素治疗患者的慢性骨髓炎。
经治医师同意感染病医师的意见,不支持长期使用抗生素抑制疗法,除非患者的病情频繁加重。对乔的定量C反应蛋白和红细胞沉降率进行了密切监测,并根据临床表现考虑抗生素治疗。右侧臀部伤口显示缓慢但渐进性的改善。
两年后,镓扫描显示不确定是否有骨髓炎(图9)。一年后,根据培养结果,乔接受了另一个针对伤口感染的短期抗生素疗程。在过去几年中,该患者的治疗计划包括市场上可获得的各种循证的敷料,即:使用了Collagenase、Medihoney™、Plurogel™、Collagen、Oasis™、Biologics Epifix™、Grafix™和Hyalomatrix™敷料,目的是实现完全的伤口愈合。

2016年12月,乔在右侧臀部和右侧转子伤口之间出现了另一个脓肿。脓肿引流几周后,注意到有一个小开口连接到右侧臀部伤口,这个开口形成了一条通道,与右内侧窝连通(图10)。这一发现得到了MRI的证实。

与以前的脓肿不同,这个浅表伤口没有愈合。在八周时间内,应用了几种局部治疗方式,其中没有一种成功获得期望的疗效。由于伤口没有显示改善,因此实施了骨盆MRI检查。检查结果显示,在与该软组织过程相邻的右侧髋臼后柱内有一些轻微的骨髓信号变化。总体而言,与之前的扫描相比,右侧髋臼内的骨髓信号变化有所减少。MRI检查发现,由于骨髓信号变化减少,总体印象是有所改善。
乔的病例在伤口护理委员会成员之间进行了讨论。委员会认为,基于临床病程,生物膜可能是阻碍伤口愈合的罪魁祸首。他们的建议包括脉冲灌洗,然后使用Plurogel™。这种方法尝试了一个月,但是没有得到改善。接下来建议进行高压氧治疗,但由于乔有自发性气胸病史,这种治疗方案属于禁忌。
患者被转介到另一家机构,以获取第二种意见。在查看MRI报告后,会诊的伤口护理医学博士和该医院放射科医生都一致认为患者仍然患有慢性骨髓炎,建议实施外科清创术,长期同时进行抗生素和高压氧治疗。由于患者既往有自发性气胸病史,因此未进行高压氧治疗。会诊医师明确指出,在大多数情况下骨盆骨髓炎是无法治愈的。对骨盆进行激进清创可能导致坐姿平衡不良,这将严重损害患者的整体福祉。
对所有伤口进行的随访评估显示,伤口床上覆盖有脆性和苍白的组织。伤口培养和药敏试验最初生长出多药耐药MRSA,后来生长出变形杆菌。治疗方案包括针对MRSA使用百多邦(Bactroban)和复方新诺明,但两周后没有观察到改善。随后,加入厄他培南治疗变形杆菌。他每天由一名家访护士通过肌肉注射1克厄他培南。在感染病科会议上提出了乔的病例,会议决定根据乔的临床表现进行长期抗生素疗程。
六个月后,右侧臀部伤口的愈合停滞,于是决定让乔入院,他最终同意在进行激进外科清创术之前进行结肠造口术,以便于伤口管理。在2018年3月,在清创时采集了骨培养物,培养显示持续性MRSA(图11)。乔被给予两剂达巴万星(Dalbavancin),一周一次,然后是四剂奥利万星(Oritavancin),一周一次(图12)。2018年8月,炎症标志物得到了改善,伤口已愈合(图13)。继续监测炎症标志物,随后开始长期抑制疗法,每天口服米诺环素100毫克,共两次。图14显示出右侧臀部伤口完全闭合。
作为医师,多学科治疗团队有许多未能解答的疑问。急性骨髓炎是从什么时候开始转变为慢性骨髓炎的?患者没有接受足够的治疗吗?此病例可以用不同的方式管理吗?成像方面呢?为什么它没有提供清晰的图片?
讨论
检测骨感染的实验室检查
我们已经知道,X射线不能揭示早期骨髓炎。X射线可以有效地显示由死骨片等骨髓炎引起的损伤;但是,无法显示当前的感染活动水平1。计算机轴向断层成像(CAT)扫描可描绘骨髓内和软组织气体、死骨片、窦道和异物。但是,CAT扫描不足以评估所述过程的活动1。核成像能够非常灵敏地检测炎症的存在,因此比起慢性感染,用于评估急性感染更可靠。MRI的灵敏度已有所增加,对骨髓炎,尤其是早期疾病的预测效果不佳1。MRI通常滞后于临床改善,有时在治疗后数月内可能仍然显示异常1。要记住的重要一点是,成像旨在为诊断提供支持,但不能作为排他性诊断;必须将其与整个临床症状结合在一起考虑。
在此病例中,炎症标记物始终很高,所以很难用作为指导。在审查时,最后的MRI报告显示出:
...在与软组织过程相邻的右侧髋臼后柱内有一些轻微骨髓信号变化,这可能代表反应性骨髓变化。相比之下,右侧髋臼内骨髓信号的总体变化与之前的检查相比有所减少。
放射科检查的结果未明确报告骨髓炎;因此,由于骨髓信号减少,要求进行放射科检查的医生将该报告解释为临床改善。现在回想,可以得出结论,这些发现符合慢性骨髓炎。
抗生素治疗
对于骨髓炎治疗,抗生素选择、给药途径和持续时间选择仍有争议,导致不同感染病医师推荐不同的疗法。人们普遍认为,通过广泛切除充分进行清创术仍然是治疗成功的最重要的临床预测指标2,3。对于乔的病例,手术是一个令人担忧的问题,因为对患病区域进行激进清创很可能导致坐姿平衡不良以及伤口扩大。他的所有护理都在一个中心内进行,这能为他提供连续的护理管理,并能快速获取他的所有病例记录,包括以前的抗生素治疗方案。乔对两类抗生素出现了过敏,包括磺胺类药物和头孢菌素。因此,治疗方案有限。我们的感染病团队推荐了奥利万星,因为在最近的研究中,它具有良好的耐受性和良好的疗效。它对金黄色葡萄球菌也有效,并且能有效治疗骨髓炎4,5。我们在等待采购奥利万星时,最初使用了达巴万星两周,因为它与奥利万星相似6。
生活质量问题
作为临床医生和护理人员,在反思慢性伤口的管理和克服阻碍治愈的障碍的挑战之后,我们还必须考虑慢性伤口对患者的影响。对乔来说,成功和失败的感受以及总体预后的不确定性导致了不同的问题。当一个人认为他无力控制自己生活中所发生的事情时,适应能力就会受到限制,并且往往无效7。
在医院环境中,乔会尝试遵守所有压力性损伤的预防措施。他会非常关注伤口护理说明,会询问敷料的适应症,并比较各种敷料的好处。乔没有表现出任何明显的不健康行为;然而,他会周期性地忽视自己的外表,不剃须或剪发。他经常拒绝医院提供的饭菜,或者让食品罐头在床边堆积。他的睡眠不规律。有时他会假装睡着以避免与护理人员交谈或互动。例如,他会说他要继续留在床上以加快治疗过程。他是围绕自己的伤口护理计划安排生活的。他经常说自己“正在等伤口愈合”,然后再开始参与社会环境和报名读书。他的心情常常会受到关于伤口状况的讨论而影响。如果报告说伤口没有显示出任何改善,他就会变得安静和沉默寡言,或者如果获得正面的反馈,他就会变得健谈和友好。
据记载,心理上的痛苦可能对伤口产生临床相关的影响8。已知压力可以减少炎症介质的数量,延长愈合的炎症阶段,从而使整体愈合的时间加长8。工作人员一再提醒他,我们不知道他的伤口什么时候能完全闭合,并强烈建议他不要暂停生活。
护理目标
我们SCI多学科团队的共同目标是继续鼓励我们的患者在受伤后去适应、推动生活,并发挥他们最大的潜力。所有的护理计划都致力于实现这一目标。我们协同工作,以最大限度地提高患者的生活质量,让患者拥有尽可能最好的生活。通常在医院环境中,患者的疾病是优先的。但是,我们需要考虑睡眠不足、心理困扰、压力、抑郁、疼痛、住院时长及他们对患者的社交生活的影响等因素。
乔的伤口低于他的脊髓损伤(SCI)水平,使他无法感受到疼痛。据报告,疼痛感受器仍在这些区域触发,从而引起局部炎症反应,这可能会抑制愈合过程9,10。文献还揭示,睡眠时间受限减少了生长激素分泌,导致单核细胞迁移减少、小噬细胞激活减少以及蛋白质缺乏。因此,毛细血管形成减缓、胶原合成减少,并且伤口重塑减缓8。
抑郁也与伤口愈合延迟有关联8。乔在抑郁症筛查中从未有过阳性结果,但他避免参与活动或拒绝参加由娱乐治疗师安排的旅行,由此可以清楚看出他的社交孤立。他的行为可能是因为抑郁症,但他否认抑郁症状。乔是一个非常干净的人,非常担心他的周围环境受到污染;伤口渗出物的量以及伤口散发的气味在很大程度上促使他社交孤立。慢性伤口的这些方面使他不去考虑寻找伴侣或与女性建立有意义的关系。
为乔提供社会支持,以帮助他减轻压力非常重要,对于促进伤口愈合至关重要。本多学科团队通过让乔认识到他有自己的韧性,以及克服和战胜伤病的力量,以此努力提升他的自信心11。这两个要素是积极适应伤病并在社区中享受愉快生活的关键,这一点不断得到了证实。
结论
脊髓损伤(SCI)患者由于行动受限和缺乏感觉而容易发生压力性损伤。在这一患者群体中,伤口的发生通常是长期或复发性的。伤口受感染可导致败血症,并且经常受到继发性骨髓炎的影响。这些伤口的管理很复杂,对医疗机构来说是巨大的经济负担。此外,这些伤口极大地破坏了患者的生活方式,尽管医师尽最大努力鼓励和帮助患者,使他们对自己所处的环境拥有一定程度的控制,并让他们过上正常、充实的生活。
SCI多学科团队目睹了这些类型的慢性伤口对患者生活质量的不利影响,以及这些伤口中存在的骨髓炎使得伤口的管理更加复杂。乔的病例帮助SCI团队意识到,有时候他们太依赖于放射学诊断结果了。文献指出,成像是一种支持诊断的测试,但并非诊断性的。重要的是,要从一开始就实施全面的多学科方法,以确保取得积极成果,从而避免持久的并发症。在管理乔的伤口的过程中,SCI团队意识到确定和选择最有利于患者整体健康的治疗计划是非常重要的。治疗目标是确保快速实现伤口完全闭合,以使患者在伤后实现最大愈合。
护理人员和临床医生必须始终考虑到,慢性骨髓炎可能是慢性、非愈合性软组织伤口的致病因素12。为了确保及早实施适当的治疗,以减轻对患者的长期影响和可避免的痛苦、缩短住院时间和控制成本,必须做出明确的诊断。作为临床医生,很明显的是,复杂伤口的管理需要跨专业协作,以解决可能阻碍伤口愈合的方方面面。当存有疑问时,临床医生应当毫不犹豫地向其他专家咨询,以确保患者充分了解情况,并获得最佳的护理。
致谢
我们感谢James J Peters VAMC的脊髓损伤(SCI)团队和感染病(ID)团队以及Kathleen Capitulo博士对本文稿的早期版本提供支持、鼓励和评论。
利益冲突
作者声明没有利益冲突。
资助
作者未因该项研究收到任何资助。
Author(s)
Swapna Johnson-Kunjukutty
MD, IIWCC-NYU
James J Peters VAMC, Bronx, NY, USA
Columbia University School of Medicine, New York, USA
Carmel Delille
RN, MSN, MHA, CWON
The James J Peters VAMC, Bronx, NY, USA
Correspondence to Swapna Johnson-Kunjukutty
Email Swapna.Johnson-Kunjukutty@va.gov
References
- Khan AN. Chronic osteomyelitis imaging. Medscape 2017 September. https://emedicine.medscape.com/article/393345-overview
- Spellberg B & Lipsky BA. Systemic antibiotic therapy for chronic osteomyelitis in adults. Clin Infect Dis 2012 Feb; 54(3):393–407 https://www.ncbi.nlm.nih.gov/pubmed/22157324
- Panteli M & Giannoudis PV. Chronic osteomyelitis: what the surgeon needs to know. EFORT Open Rev 2016 May; 1(5):128–135 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5367612/
- Brade KD, Rybak JM & Rybak MJ. Oritavancin: A new lipoglycopeptide antibiotic in the treatment of gram-positive infections. Infect Dis Ther 2016 February; 5. https://link.springer. com/article/10.1007%2Fs40121-016-0103-4
- DelapoRightas DJ, Estrada SJ & Darmelio M. Successful treatment of methicillin susceptible Staphylococcus aureus osteomyelitis with oritavancin. Pharmacotherapy 2017 Aug; 37(8):e90–e92. https:// www.ncbi.nlm.nih.gov/pubmed/28543367
- Rappo U, Puttagunta S, Scevchenko V et al. Dalbavacin for the treatment of osteomyelitis in adult patients: a randomized clinical trial of efficacy and safety. Open Forum Infect Dis 2019 January; 6(1), https://academic.oup.com/ofid/article/6/1/ofy331/5235615
- Rohatinsky N, Goodridge D, Rogers MR, Nickel D & Linassi G. Shifting the balance: conceptualizing empowerment in individuals with spinal cord injury. Health Soc Care Community 2017 Mar; 25(2):769- 779 https://www.ncbi.nlm.nih.gov/pubmed/27400830
- House SL. Psychological distress and its impact on wound healing: an integrative review. J Wound Ostomy Continence Nurs 2015 Jan– Feb; 42(1):38–41 https://www.ncbi.nlm.nih.gov/pubmed/25549307
- Woo Y. Exploring the effects of pain and stress on wound healing. Adv Skin Wound Care January 2012; 25(1):38-44 https://www.nursingcenter.com/cearticle?an=00129334-201201000- 00010&Journal_ID=54015&Issue_ID=1287313
- Bechert K & Abraham SE. Pain management and wound care. J Am Coll Certif Wound Spec 2009 Apr; 1(2):65–71. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3478916/
- Ousey K & Edward K-L. Exploring resilience when living with a wound — an integrative literature review. Healthcare (Basel) 2014 Sep; 2(3):346–355. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4934596/
- Lalani T & Schmitt SK. Osteomyelitis in adults: Clinical manifestations and diagnosis. UpToDate Literature review current through: May 2019. Updated 28 March 2019 https://www.uptodate.com/contents/osteomyelitis-in-adults-clinical-manifestations-and-diagnosis


