Volume 42 Number 2
Clinical outcome of injuries in people assisted in a stomal therapy nursing outpatient clinic in northeastern Brazil
Luis Rafael Leite Sampaio, Silvânia Miranda da Silva, Francisca Clarisse de Sousa, Tays Pires Dantas, Fernanda Helen Gomes da Silva, Luana de Souza Alves, Sara Teixeira Braga, José Lucas de Souza, Naftale Alves dos Santos Gadelha, Ana Maria Parente Garcia Alencar and Woneska Rodrigues Pinheiro
Keywords nursing, wounds, stomal therapy, outcome measures
For referencing Sampaio LRL et al. Clinical outcome of injuries in people assisted in a stomal therapy nursing outpatient clinic in northeastern Brazil. WCET® Journal 2022;42(2):30-35
DOI
https://doi.org/10.33235/wcet.42.2.30-35
Submitted 29 September 2021
Accepted 27 April 2021
Introduction
Wounds are a visible problem, and they affect segments of the population regardless of sex, age and ethnicity. When chronic, they present as slow healing wounds and are commonly associated with an underlying disease1,2. The available data for chronic wounds in Brazil and in the world are still in their infancy but, as a result of the ageing population, these data and the number of wounds are likely to increase. For example, a study with elderly patients seen in primary care services in a state capital in the northeast region of Brazil found a wound prevalence of 8%, specifically pressure sores (5%) and venous wounds (2.9%). The presence of chronic wounds was associated with older age, lower education and cognitive impairment status3,4.
In Brazil, complex wounds have a financial impact on the individual as well as on the public health system. They are considered a problem for the state because the cases are increasing and require greater attention from the nursing team in Brazil and associated health services5,6. In this context, the individual with wounds should be cared for in a holistic perspective by an interdisciplinary and intersectoral team. However, it needs to be emphasised that the nursing team are responsible for clinical follow-up, dressing the wounds and choosing the management based on the aspects of the wound7. Furthermore, it is imperative that the nursing team are aware of confounding factors that can intervene in the progressive improvement of wounds. Moreover, it is necessary to know the clinical characteristics of different wounds in order to offer the best practice treatment, because clinical analysis studies contribute to the description of the particularities of a population4,8,9.
Given the above, we realise the importance of clinical follow-up of the patient with wounds in a health service with trained professionals. With this aim in mind, a stomal therapy nursing outpatient clinic was created in the region of Cariri Ceará in Brazil, which operates on a non-profit basis and aims to provide specialised care for people with wounds, stomas and incontinence. With the growing demand of people seen at the stomal therapy nursing outpatient clinic of the Regional University of Cariri (URCA) seeking assistance with wound management, the question arose, “What is the clinical outcome of the wounds of people seen at this service?” Based on this guiding question, the objective is to demonstrate the healing time of wounds of people accompanied by a stomal therapy nursing service, as well as to describe the importance of specialised monitoring in the treatment of wounds.
The study is relevant for contributing to the understanding of the clinical characteristics of the participants, as well as factors that may influence healing time. Therefore, an understanding of these factors will have implications for interventions based on clinical analysis and therapeutic efficacy10,11.
Method
Study type
This study was a retrospective, descriptive, clinical audit with purposive sampling and a quantitative approach. The study was undertaken in a stomal therapy nursing outpatient clinic, and was created by an initiative of the undergraduate nursing course of a public university (URCA) aiming to provide specialised nursing care to people living with wounds, stomas and incontinence.
Inclusion and exclusion criteria
To identify the sample population, the following inclusion criteria were adopted – health records of people with wounds who received some type of assistance at the study site between July 2018 and February 2019 and who were older than 18 years of age. Incomplete health records were excluded. This resulted in a sample size of 41 participants.
Data collection
Data collected was retrospectively abstracted from the medical records of participants’ outpatient clinic admission and evaluation forms that contained sociodemographic, clinical data and macroscopic characteristics of the wound or wounds. The scripted data extraction instrument was developed by the health professionals in the stomal therapy nursing outpatient clinic. The following variables were adopted within the data extraction instrument – basic data concerning the research participant (name, age, municipality of origin), information about the current wounds (type of wound and if recurrent, location, duration, macroscopic characteristics of the wound/s), as well as a section regarding the types of products/ dressings used before and after admission to the stomal therapy nursing outpatient clinic. Data collected were tabulated using Microsoft Excel 2013, then exported to R Software and analysed using descriptive statistics for relative and absolute frequency, percentages, mean, and standard deviation. Data were organised into tables and graphs and ensuing results discussed with reference to relevant literature.
This research study adhered to the ethical precepts of the Brazilian National Health Council Resolution 466/201212. It was submitted for ethical review and was approved with opinion number 3,155,662 by the Regional University of Cariri (URCA).
Results
A total of 41 medical records of people with wounds treated at the stomal therapy nursing outpatient clinic were analysed regarding the type of wound care provided and curative treatment to promote healing. Such curative care refers to wounds with the potential for healing, in association with the treatment/control of underlying diseases.
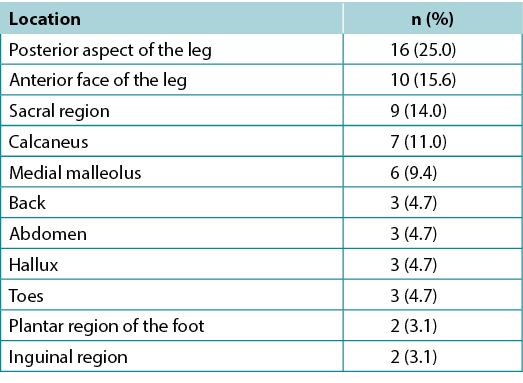
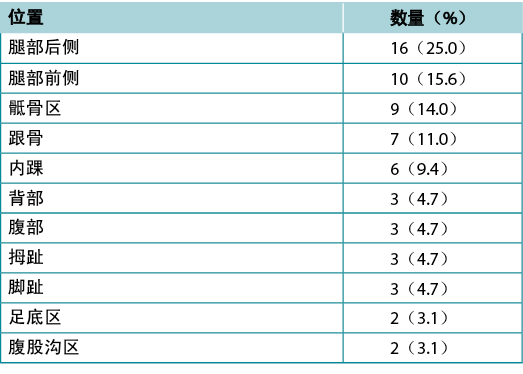
Of the 41 participants with wounds/injuries requiring curative treatment, a total of 64 injuries were counted, with an average of 1.5 (±1) per person; the period of time with the wounds/injury averaged 35.6 months. It was found that 27 (65.9%) participants had chronic wounds and 14 (34.1%) had acute wounds. As for the aetiology of the wounds/injuries, 11 (26.8%) were due to trauma, 16 (39.0%) to diabetic neuropathies, two (4.9%) to vascular compromise, five (12.2%) were pressure injuries and seven (17.1%) were classed as others. Most wounds were in the posterior aspect of the lower leg (16, 25%), followed by the anterior aspect of the leg 10 (15.6%); wounds in the sacral region accounted for nine (14%) wounds (Table 1).
Table 1. Distribution of wounds/injuries of people assisted in the stomal therapy nursing outpatient clinic
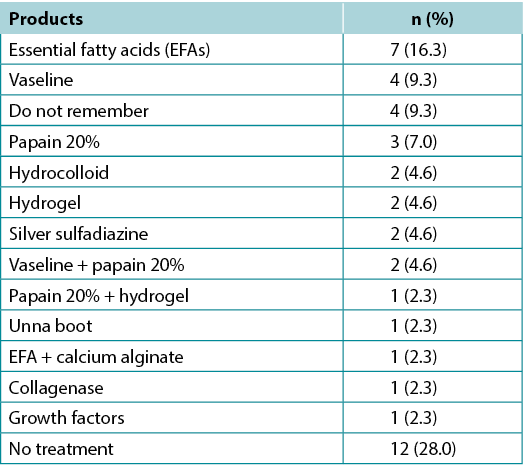
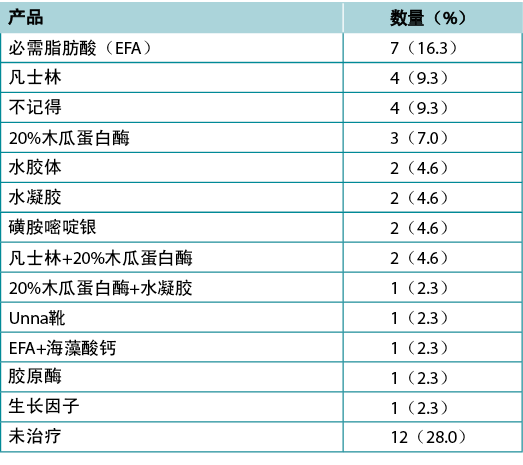
It was shown that 31 (72%) participants attending the stomal therapy nursing outpatient clinic had undergone some wound management treatment prior to admission (Table 2). When assessed on admission and the type of previous dressing treatments were recorded, it was found that seven (16.3%) participants used essential fatty acids (EFAs), four (9.3%) used vaseline and papain 20% was used by three individuals (7%). No treatments were recorded for 12 (28.0%) participants (Table 2).
Table 2. Wound dressings used by patients before the first evaluation with the stomal therapist
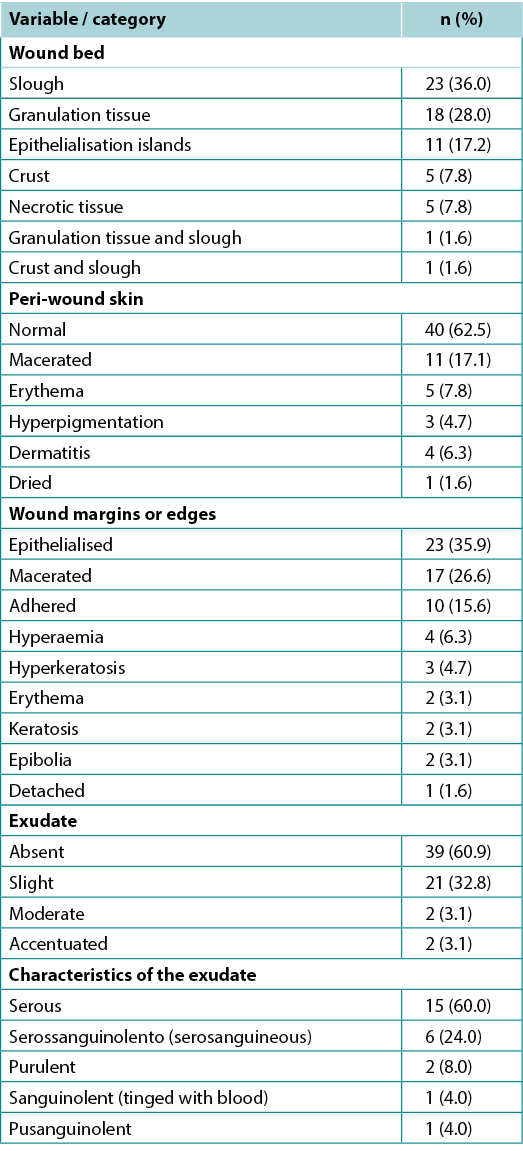
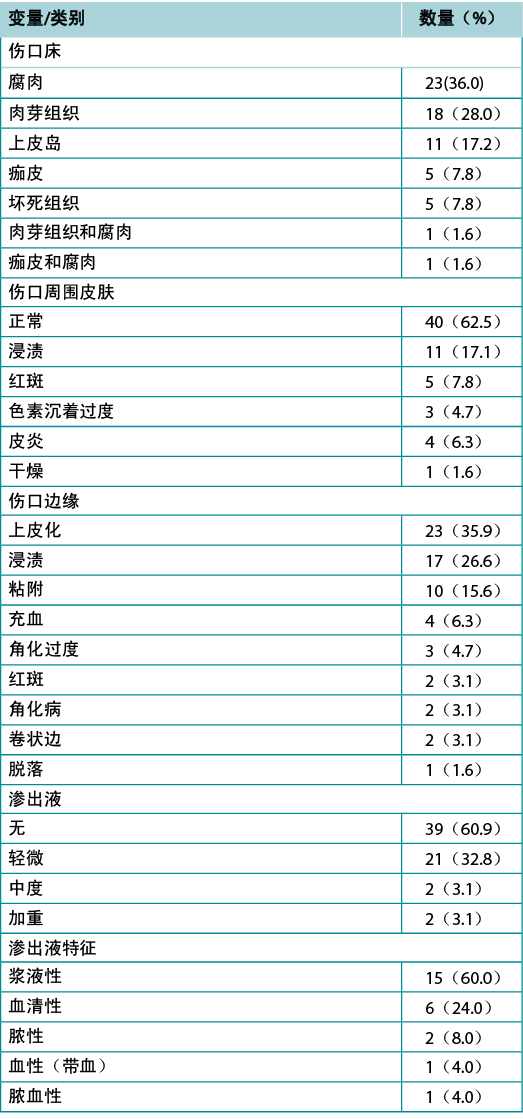
In the evaluation of the clinical characteristics of the wound bed of sustained wounds/injuries, a frequency of slough was observed in 23 (36.0%) cases, followed by granulation tissue, 18 (28%), and islands of epithelisation, 11 (17.2%). The peri-wound skin was found to be unaltered in 40 (62.5%) cases, 11 (17.1%) were macerated, and five (7.8%) with erythema. When the borders were analysed, 23 (35.9%) were epithelised and 17 (26.6%) were macerated. When the presence of exudate was verified, 21 (32.8%) had a slight quantity, 15 (60%) presented serous exudate, six (24%) were serosanguinous and two (8%) were purulent. Exudate was absent in 39 (60.9%) of the presenting cases (Table 3).
Table 3. Macroscopic characterisation of the wounds/ injuries in the stomal therapy nursing outpatient clinic
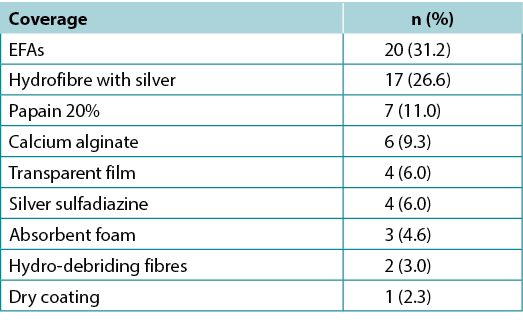
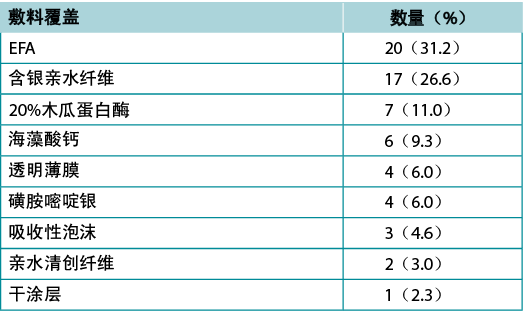
As for the topical wound treatments used in managing the wounds/injuries seen by health professionals in the stomal therapy nursing outpatient clinic, the most prescribed dressings were EFAs, 20 (31.3%), followed by hydrofibre with silver, 17 (15.7%), and papain 20% was used in seven (11%) cases (Table 4).
Table 4. Wound treatment applied to wounds/injuries in the stomal therapy nursing outpatient clinic
In terms of clinical outcomes for participants with wounds/injuries seen at the stomal therapy nursing outpatient clinic, 25 (61%) participants were discharged because their wounds had healed, nine (22%) were discharged for abandonment (lost to follow-up), four (10%) achieved improvement in wound healing outcomes, two (5%) were discharged due to death and one (2%) was discharged for referral to another health service (Figure 1).
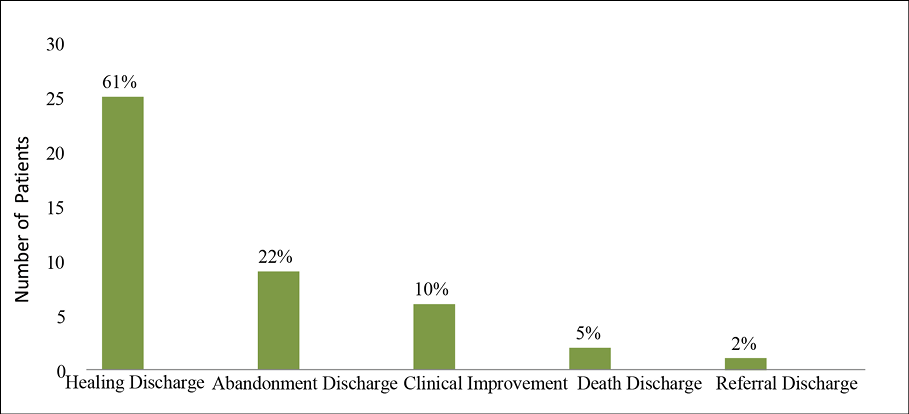
Figure 1. Clinical outcomes of wounds/injuries treated at the stomal therapy nursing outpatient clinic
Discussion
We selected 41 health records of people with wounds treated at a stomal therapy nursing outpatient clinic. Among these, 64 wounds were counted, which represents an average of 1.5 wounds per patient. The average period with the wound/injury was 35.6 months. While the current study numbers are small and therefore should be interpreted with caution, these data corroborate Brazilian literature on the subject. A study reported with 339 patients from a primary care service in the city of Teresina (Piauí) revealed that there was an average of 2.7 wounds per patient and these had an average of 30.6 months of existence13. Thus, it is clear individuals with complex wounds usually have more than one wound which can become chronic.
Chronic wounds are defined as any interruption in the continuity of a body tissue, to a greater or lesser extent, resulting from trauma or clinical conditions and associated treatments which impairs healing processes, and exceeding a duration of 6 weeks. These conditions are associated with different factors, such as vascular impairment, diabetes mellitus, systemic arterial hypertension, neuropathies, prolonged immobility, neoplasms, and nutritional alterations, requiring specialised treatment based on continuous, precise and objective assessment5.
Considered a public health problem, these chronic wounds affect 5% of the adult population in the Western world, generating high costs for health services since they involve home care, prolonged hospitalisation, complex treatments and use of adjuvant therapies, besides being associated with high rates of recurrence5.
Assessment and evaluation of the clinical characteristics of wounds on presentation and thereafter for progression of wound healing is fundamental for the prescription of evidence-based treatment. Also imperative is multidisciplinary collaboration in the management of people with wounds. In specialty stomal therapy clinics, it often becomes the responsibility of the stomal therapy nurse and other nurses to provide ongoing care. It is essential, therefore, that all health professionals understand the needs of the person with a wound, including their past and current co-morbid conditions and associated therapies in addition to the wound and wound healing requirements to promote the optimal environment for tissue repair and wound maturation healing; an endogenous process does not imply neglecting topical treatments14. The study showed that participants sought outpatient care for treatment with curative intent. Thus, it is necessary for the nursing team to act to reverse this scenario, which can help to reduce the number of cases of acute or traumatic wounds.
As for the aetiological origin, traumatic situations and diabetic neuropathy were the major triggers of tissue wounds in the participants. According to Brazilian literature, automobile accidents are the major causes of traumatic wounds/injuries13. Diabetic neuropathies were the second leading cause of the development of wounds in the participants. This condition results from deterioration in the clinical picture of diabetes mellitus, glycaemic control and unstable blood sugar levels, being responsible for the loss of sensory, motor and autonomic function, and inducement of loss of protective sensation (LOPS) facilitating the development of wounds and loss of skin integrity15. Neuropathy can also result from diseases such as leprosy, which also causes loss of sensory function and, due to LOPS can favour the appearance of ulcers such as plantar ulcers16.
The current investigation pointed out a higher frequency of wounds/injuries located in the lower limb, the anterior and posterior aspects of the leg, as the region of greatest occurrence. The lower limb wounds, commonly known as leg ulcers, are largely responsible for the majority of chronic wounds seen. In general, vascular disorders, venous and/or arterial insufficiency or mixed disease are often the underlying cause17. Although the appearance of recurrent leg ulcers is common, the study evidenced small cases, highlighting the importance of therapeutic interventions and monitoring to prevent them, e.g. compression therapy for venous leg ulcers.
There was evidence of signs of wound infection in some cases. Infections are harmful to healing because they cause further tissue injury and a decrease in collagen synthesis, making healing more difficult. Thus, the early identification of signs suggestive of local infections should be acted upon in order to apply interventions aimed at reducing damage18. The presence of non-physiological exudate may indicate infection. However, the clinical diagnosis of infection should be based on other signs and symptoms such as two or more signs of inflammation (erythema, pain, heat, swelling or induration) and obvious purulent drainage18.
Within the current study and at the initial evaluation of the wound/injury, slough was found to be present in the wound bed of most wounds/injuries. For most participants, the peri-wound skin was normal and no abnormalities were detected. However, it was identified that in 26.6% of cases there were wounds with macerated edges, where the use of inadequate dressings and exposure to moisture may be the probable cause. Maceration is known to interfere with epithelialisation of the wound19.
This study found that most participants had already received wound treatment prior to their visit to the stomal therapy nursing outpatient clinic. EFAs were the most frequently used product, followed by vaseline and papain 20%. It is known that the essential components of EFAs play an important role in healing. EFAs act in the development of granulation tissue and act as a barrier, through physical-chemical processes, which protect the skin from moisture through the regulation of water permeability in the dermis20.
On the other hand, some authors with a focus on preclinical work have already found that the use of EFAs induces an inflammatory response induced by interleukins which can interfere with the success of healing. Thus, it is emphasised that the use of such a product and its results requires the need for scientific studies to support its use based on evidence21. In short, the use of EFAs remains the most used product in this health service because of its effectiveness and low cost, followed by hydrofibre with silver, which was the second most used product. Antiseptic dressings should be considered as a first-line approach to wound infection management within standard care in the absence of clinical signs of spreading infection22. Among dressings, hydrofibre with silver is recognised as a broad-spectrum antibacterial dressing and is widely used in the clinic in the treatment of infected wounds23. Although the products identified above are widely used in health services in Brazil, they must be prescribed by trained health professionals and, when used inappropriately, they can cause damage to the wound/injury, hindering healing.
Regarding clinical improvements and wound healing outcomes of wounds seen in this study, 61.0% of wounds healed and 10.0% were observed to have improved (Figure 1). In addition, such outpatient clinics advance their importance in both curative activities and preventive interventions in relation to skin integrity, encouraging patients to develop their autonomy and responsibility in the restoration of their health and disease process.
Conclusion
This research analysed the characteristics and clinical outcomes of people who presented with wounds/injuries to a stomal therapy nursing outpatient clinic in the region of Cariri Ceará, in Brazil. Traumatic wounds were the most frequent wounds/injuries seen, with most occurring in the posterior aspect of the lower limbs and a greater presence of slough on the bed of the lesions, with epithelised edges and normal peri-wound skin. Most participants had undergone some wound treatment prior to admission, with a predominance of EFAs and vaseline as the primary dressing. In the clinical management at the outpatient clinic, the most prescribed and used products were EFAs and hydrofibre with silver.
In short, these results will help in the development of measures to address potential complications and prevention strategies related to common wounds found within Brazilian communities that are of increasing concern from a public health perspective. Specialised wound care services such as those provided within the stomal therapy nursing outpatient clinic have an important role to play in the treatment and prevention of community-acquired wounds.
Conflict of Interest / Funding
There is no financial interest which could create a potential conflict of interest with regard to the present work.
巴西东北部造口治疗护理门诊治疗患者损伤的临床结局
Luis Rafael Leite Sampaio, Silvânia Miranda da Silva, Francisca Clarisse de Sousa, Tays Pires Dantas, Fernanda Helen Gomes da Silva, Luana de Souza Alves, Sara Teixeira Braga, José Lucas de Souza, Naftale Alves dos Santos Gadelha, Ana Maria Parente Garcia Alencar and Woneska Rodrigues Pinheiro
DOI: https://doi.org/10.33235/wcet.42.2.30-35
摘要
目的 旨在研究巴西一家造口治疗护理门诊的患者伤口临床结果。
方法 对病历进行回顾性、描述性的临床审计。对造口治疗护理门诊就诊的41例伤口患者的病历进行了分析。
结果 就提供的伤口护理而言,41人(100%)接受了治愈性治疗。在41例有伤口的研究对象中,共统计了64处伤口,平均每人1.5(±1)处;伤口存在的时间平均为35.6个月。结果发现,27例研究对象(65.9%)有慢性伤口,14例研究对象(34.1%)有急性伤口。至于伤口的病因,11例(26.8%)为外伤,16例(39.0%)为糖尿病神经病变,2例(4.9%)为血管受损,5例(12.2%)为压力性损伤,7例(17.1%)被归类为其他。
结论 本次研究结果将有助于制定应对潜在并发症的措施,以及为患者需要造口治疗护理门诊医护人员帮助的伤口类型制定相关预防策略。
引言
伤口是一个明显的问题,它影响到不同性别、年龄和种族的人群。慢性伤口表现为伤口愈合缓慢,通常与潜在疾病相关1,2。巴西和世界上关于慢性伤口的现有数据仍处于初级阶段,但由于人口老龄化,这些数据和伤口数量可能会增加。例如,一项针对巴西东北部某州首府基层医疗服务中的老年患者的研究发现,伤口患病率为8%,特别是压疮(5%)和静脉伤口(2.9%)。慢性伤口的出现与年龄较大、受教育程度较低和认知障碍状态有关3,4。
在巴西,复杂的伤口对个人以及公共卫生系统都有经济影响。这被认为是整个州的问题,因为病例在不断增加,需要巴西护理团队和相关医疗服务部门给予更多关注5,6。在这种情况下,应该由跨学科和跨部门团队从整体的角度来为受伤的个人提供护理。然而,需要强调的是,应由护理团队负责临床随访、包扎伤口并根据伤口的各个方面选择管理方式7。此外,护理团队必须了解可能干扰伤口逐步改善的混杂因素。此外,为了提供最佳临床实践治疗,有必要了解不同伤口的临床特征,因为临床分析研究有助于描述一个群体的特点4,8,9。
综上所述,我们意识到由训练有素的专业人员在医疗服务机构中对伤口患者进行临床随访的重要性。有鉴于此,在巴西Cariri Ceará地区创建了一家造口治疗护理门诊,该诊所以非营利形式运营,旨在为伤口、造口和失禁患者提供专业护理。随着在Cariri地区大学(URCA)造口治疗护理门诊寻求伤口管理帮助的患者需求不断增长,出现了一个问题:“在这里就诊的患者伤口临床结局如何?”基于这一指导性问题,本文的目的是呈现接受造口治疗护理服务的患者的伤口愈合时间,并描述伤口治疗中专业监测的重要性。
该研究有助于了解研究对象的临床特征以及可能影响愈合时间的因素。因此,了解这些因素将对基于临床分析和治疗效果的干预措施产生影响10,11。
方法
研究类型
本研究是一项回顾性、描述性的临床审计,采用立意抽样和定量方法。本研究在一家造口治疗护理门诊进行,由一所公立大学(URCA)的本科护理课程发起,旨在为患有伤口、造口和失禁的患者提供专业护理。
入选和排除标准
为了确定样本人群,采用了以下入选标准——2018年7月至2019年2月期间,在研究地点接受某种类型治疗且年龄超过18岁的伤口患者的病历。排除不完整的病历。最终得到41例研究对象的样本量。
数据收集
收集的数据从研究对象门诊入院的病历和评估表中回顾性地提取,其中包含社会人口学数据、临床数据和一个或多个伤口的宏观特征。脚本化的数据提取工具由造口治疗护理门诊的专业医护人员开发。在数据提取工具中采用了以下变量-关于研究对象的基本数据(姓名、年龄、出生地),关于当前伤口的信息(伤口类型,以及如果伤口复发,其位置、持续时间,伤口的宏观特征),以及关于造口治疗护理门诊入院前后使用的产品/敷料类型的部分。使用Microsoft Excel 2013将收集的数据制成表格,然后导出到R软件,并使用描述性统计对相对和绝对频率、百分比、平均值和标准差进行分析。数据被整理成表格和图表,并参考相关文献讨论了随后的结果。
本研究遵守了巴西国家卫生委员会第466/2012号决议的伦理准则12。本研究已提交伦理审查,并得到了Cariri地区大学(URCA)的批准,意见编号为3155662。
结果
对41例在造口治疗护理门诊接受治疗的伤口患者的病历进行了分析,了解所提供的伤口护理类型和促进愈合的治愈性治疗。这种治愈性护理是指伤口愈合的同时,能治疗/控制潜在疾病。
在41例需要治愈性治疗的伤口/损伤研究对象中,共统计了64处损伤,平均每人1.5(±1)处;伤口/损伤存在的时间平均为35.6个月。结果发现,27例研究对象(65.9%)有慢性伤口,14例研究对象(34.1%)有急性伤口。至于伤口/损伤的病因,11例(26.8%)为外伤,16例(39.0%)为糖尿病神经病变,2例(4.9%)为血管受损,5例(12.2%)为压力性损伤,7例(17.1%)被归类为其他。大部分伤口位于小腿后侧(16处,25%),其次是腿部前侧10处(15.6%);骶骨区的伤口有9处(14%)(表1)。
表1.造口治疗护理门诊患者的伤口/损伤分布情况
结果显示,造口治疗护理门诊的31例(72%)研究对象在入院前接受了一些伤口处理治疗(表2)。在入院时进行评估并记录之前使用的敷料治疗类型时,发现7例(16.3%)研究对象使用必需脂肪酸(EFA),4例(9.3%)研究对象使用凡士林,3例(7%)研究对象使用20%木瓜蛋白酶,12例(28.0%)研究对象未记录任何治疗(表2)。
表2.患者在造口治疗师首次评估前使用的伤口敷料
在评估持续性伤口/损伤的伤口床的临床特征时,观察到23例(36.0%)出现腐肉,其次是18例(28%)出现肉芽组织,11例(17.2%)出现上皮岛。40例(62.5%)伤口周围皮肤无变化,11例(17.1%)出现浸渍,5例(7.8%)出现红斑。分析伤口边缘时,23例(35.9%)出现上皮化,17例(26.6%)出现浸渍。在验证有无渗出液时,21例(32.8%)有少量渗出液,15例(60%)有浆液性渗出液,6例(24%)有血性渗出液,2例(8%)有脓性渗出液,39例(60.9%)无渗出液(表3)。
表3.造口治疗护理门诊伤口/损伤的宏观特征
至于造口治疗护理门诊的专业医护人员在处理遇到的伤口/损伤时使用的局部伤口治疗,使用最多的敷料是必需脂肪酸,20例(31.3%),其次是含银的亲水纤维,17例(15.7%),而有7例(11%)使用20%木瓜蛋白酶(表4)。
表4.伤口治疗在造口治疗护理门诊的伤口/损伤中的应用
就造口治疗护理门诊的伤口/损伤研究对象的临床结局而言,25例(61%)研究对象因伤口愈合而出院,9例(22%)研究对象因放弃治疗而出院(失访),4例(10%)研究对象的伤口愈合结果有所改善,2例(5%)因死亡而出院,1例(2%)因转诊至其他医疗服务机构而出院(图1)。
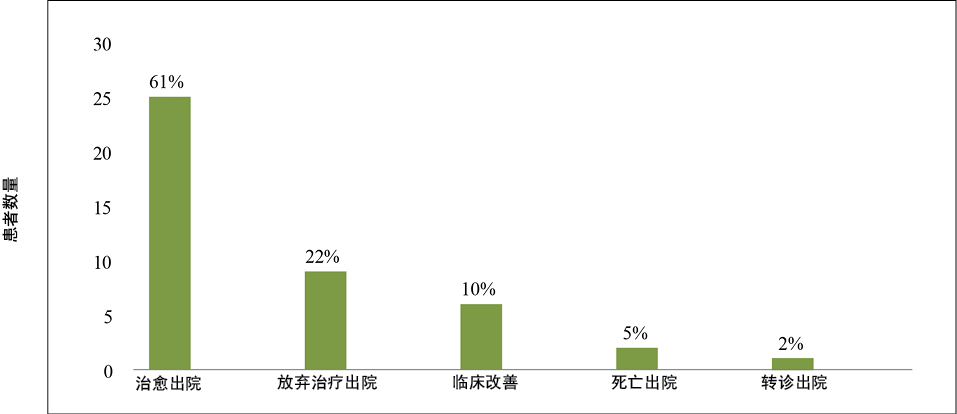
图1.造口治疗护理门诊治疗伤口/损伤的临床结局
讨论
我们选择了41份在造口治疗护理门诊治疗的伤口患者的病历。其中,共统计了64处伤口,即平均每位患者有1.5处伤口。伤口/损伤存在的平均时间为35.6个月。虽然目前的研究数量很少(因此应谨慎解释),但这些数据证实了巴西有关该问题的文献。一项针对Teresina市(Piauí)的一家基层医疗服务机构的339名患者的研究报告显示,每位患者平均有2.7处伤口,这些伤口平均存在30.6个月13。因此,很明显,有复杂伤口的患者通常有不止一个伤口,这些伤口可能会成为慢性伤口。
慢性伤口是指由于外伤或临床病症及相关治疗而引起的身体组织连续性的或多或少的中断,这种中断会损害愈合过程,且持续时间超过6周。这些病症与不同的因素有关,如血管损伤、糖尿病、全身性动脉高血压、神经病变、长期活动受限、肿瘤和营养改变,需要基于连续、精确和客观的评估进行专门治疗5。
这些慢性伤口被认为是一个公共卫生问题,影响到西方世界5%的成年人群,并产生了高昂的医疗服务费用,因为它们涉及家庭护理、长期住院、复杂的治疗和辅助疗法的使用,此外还与高复发率有关5。
评估和评价伤口的临床特征以及其后伤口愈合的进展对于制定循证治疗的处方至关重要。此外,在伤口患者管理方面开展多学科合作也是必不可少的。在专业造口治疗诊所,造口治疗护士和其他护士通常有责任提供持续护理。因此,所有专业医护人员都必须了解伤口患者的需求,包括他们过去和当前的共病病情和相关治疗,以及伤口和伤口愈合要求,以打造组织修复和伤口成熟愈合的最佳环境;内源性过程并不意味着忽视局部治疗14。研究表明,研究对象出于治愈目的寻求门诊治疗。因此,护理团队有必要采取行动扭转这种情况,这有助于减少急性或外伤性伤口的病例数量。
至于病因,外伤情况和糖尿病神经病变是研究对象组织伤口的主要诱因。根据巴西文献,汽车事故是造成外伤性伤口/损伤的主要原因13。糖尿病神经病变是研究对象出现伤口的第二大原因。这种情况是由于糖尿病临床症状恶化、血糖控制和血糖水平不稳定造成的,导致感觉、运动和自主神经功能丧失,并致使保护性感觉丧失(LOPS),从而产生伤口以及皮肤完整性丧失15。神经病变也可能是由麻风病等疾病引起,也会导致感觉功能丧失,并且由于保护性感觉丧失,可能容易出现足底溃疡等溃疡16。
当前的研究指出,位于下肢、腿部前侧和后侧的伤口/损伤发生频率较高,是发生率最高的区域。下肢伤口通常称为腿部溃疡,是大多数慢性伤口的主要原因。一般来说,血管疾病、静脉和/或动脉功能不全或混合性疾病通常是根本原因17。尽管复发性腿部溃疡的出现很常见,但本研究中仅有小部分患者出现复发的情况,强调了预防复发的治疗干预和监测的重要性,例如静脉性腿部溃疡的加压疗法。
在一些病例中,有证据表明有伤口感染的体征。而感染对愈合有害,因为它们会导致进一步的组织损伤和胶原蛋白合成减少,使愈合更加困难。因此,应及早发现提示局部感染的体征,以便采取旨在减少损害的干预措施18。非生理性渗出液的存在可能表明有感染。然而,感染的临床诊断应基于其他体征和症状,如两个或两个以上的炎症体征(红斑、疼痛、发热、肿胀或硬结)和明显的脓性溢出18。
在目前的研究中,在对伤口/损伤进行初步评估时,发现大多数伤口/损伤的伤口床都存在腐肉。对于大多数研究对象来说,伤口周围皮肤正常,未发现异常。然而,在26.6%的病例中,发现伤口边缘有浸渍,可能是因为使用不适当的敷料和暴露于潮湿环境中。而浸渍会干扰伤口的上皮化19。
本研究发现,大多数研究对象在造口治疗护理门诊就诊之前已经接受过伤口治疗。EFA是最常用的产品,其次是凡士林和20%木瓜蛋白酶。众所周知,EFA的基本成分在愈合过程中发挥着重要作用。EFA在肉芽组织的发育中发挥作用,并通过物理-化学过程起到屏障的作用,通过调节真皮层中的水分渗透性来保护皮肤免受潮湿环境的影响20。
另一方面,一些专注于临床前研究的作者已经发现,使用EFA会诱导由白细胞介素引起的炎症反应,从而干扰愈合的成功。因此,需要强调的是,使用此类产品及其结果需要进行科学研究,以支持其基于证据的使用21。简言之,由于其有效性和低成本,EFA是这项医疗服务中使用最多的产品,其次是含银的亲水纤维(第二常用的产品)。在没有传播感染的临床体征的情况下,应将抗菌敷料视为标准护理中伤口感染管理的一线方法22。在敷料中,含银的亲水纤维被认为是一种广谱抗菌敷料,在临床上广泛用于治疗感染伤口23。尽管上述产品在巴西的医疗服务中广泛使用,但必须由经过培训的专业医护人员开具处方,如果使用不当,可能会对伤口/损伤造成损害,阻碍愈合。
关于本研究中观察到的伤口的临床改善和伤口愈合结局,伤口愈合占61.0%,伤口有所改善的情况占10.0%(图1)。此外,此类门诊在与皮肤完整性有关的治愈性活动和预防性干预方面推进了其重要性,鼓励患者在恢复健康和疾病过程中发展其自主性和责任感。
结论
本研究分析了在巴西Cariri Ceará地区一家造口治疗护理门诊就诊的伤口/损伤患者的特征和临床结局。外伤性伤口是最常见的伤口/损伤,大多数发生在下肢后侧,并且病灶床存在更多腐肉,边缘上皮化,伤口周围皮肤正常。大多数研究对象在入院前接受了一些伤口治疗,主要采用EFA和凡士林作为接触性敷料。在门诊的临床管理中,开具处方和使用最多的产品是EFA和含银的亲水纤维。
简而言之,这些结果将有助于制定应对潜在并发症的措施,以及有关巴西社区内常见伤口的预防策略,从公共卫生角度来看,这些伤口越来越值得关注。专业的伤口护理服务,如造口治疗护理门诊提供的服务,在治疗和预防社区获得性伤口方面发挥着重要作用。
利益冲突声明/资助
不存在可能对当前文章产生潜在利益冲突的经济利益。
Author(s)
Luis Rafael Leite Sampaio*
Stomatherapy nurse, Teacher, Regional University of Cariri,
108 Aguinelo de Paula Damasceno St. Crato, Ceará, Brazil
Email rafael.sampaio@urca.br
Silvânia Miranda da Silva
Postgraduate student, Regional University of Cariri (URCA), Crato, Ceará, Brazil
Francisca Clarisse de Sousa
Undergraduate student in nursing, URCA, Crato, Ceará, Brazil
Tays Pires Dantas
Undergraduate student in nursing, URCA, Crato, Ceará, Brazil
Fernanda Helen Gomes da Silva
Undergraduate student in nursing, URCA, Crato, Ceará, Brazil
Luana de Souza Alves
Undergraduate student in nursing, URCA, Crato, Ceará, Brazil
Sara Teixeira Braga
Undergraduate student in nursing, URCA, Crato, Ceará, Brazil
José Lucas de Souza
Undergraduate student in nursing, Estácio de Juazeiro do Norte Faculty of Medicine, Juazeiro do Norte, Ceará, Brazil
Naftale Alves dos Santos Gadelha
Teacher, URCA, Crato, Ceará, Brazil
Ana Maria Parente Garcia Alencar
Teacher, URCA, Crato, Ceará, Brazil
Woneska Rodrigues Pinheiro
Teacher, URCA, Crato, Ceará, Brazil
* Corresponding author
References
- Ribeiro GSC, Cavalcante TB, Santos KCB, Feitosa AHC, Silva BRS, Santos GL. Internal patients with chronic wounds: a focus on quality of life. Enferm Foco 2019;10:70–75.
- Campoi ALM, Alves GA, Martins LCN, Barbosa LB, Felicidade PJ, Ferreira LA. Nursing care for patients with chronic wounds: an experience report. REFACS 2018;7:248–255.
- Lentsck MH, Baratieri T, Trincaus MR, Mattei AP, Miyahara CTS. Quality of life related to clinical aspects in people with chronic wound. Rev Esc Enferm USP 2012;52:e03384.
- Vieira CPB, Furtado AS, Almeida PCD, Luz MHBA, Pereira AFM. Prevalence and characterization of chronic wounds in elderly persons assisted in primary care. Rev Baiana Enferm 2017;31:173–197.
- Oliveira AC, Rocha DM, Bezerra SMG, Andrade EMLR, Santos AMR, Nogueira LT. Quality of life of people with chronic wounds. Acta Paul Enferm 2019;32:194–201.
- Fernandes JC, Cordeiro BC. The management of basic health units from the point of view of nursing managers. Rev Enferm UFPE online 2018;12:194–202.
- Cauduro FP, Schneider SMB, Menegon DB, Duarte ERM, Paz PO, Kaiser DE. Performance of nurses in the care of skin lesions. Rev Enferm UFPE 2018;12:2628–2634.
- Santos LJ, Silva SJ, Torres LDA, Santos MPO, Ribeiro SHP. Nursing care in the prevention of pressure: an integrative review. Braz J Health Rev 2020;3:250–255.
- Cope GF. The effects of smoking on wound healing. Wounds UK 2014;10:22S–24S.
- Bôas NC, Salomé GM, Ferreira LM. Frailty syndrome and functional disability among older adults with and without diabetes and foot ulcers. J Wound Care 2018;27:09–16.
- Nazarko L. Choosing the correct wound care dressing: an overview. J Comm Nurs 2018;32:42–52.
- Novoa PCR. What changes in research ethics in Brazil: Resolution no. 466/12 of the National Health Council. Einstein (São Paulo) 2014;12:8–10.
- Damaceno IS, Alves TM, Santos LRO, Fianco MC, Araújo SNM, Silva MNL. Characterization clinical and epidemiological of victims of motorcycle accidents. Enferm em Foco 2018;9:13–17.
- Batista MAS, Gonçalves RCM, Sousa GL. The role of nurses in the prevention, evaluation and treatment of pressure ulcers. Braz J Dev 2020;10:77757-64.
- American Diabetes Association, Standards of medical care in diabetes. Diabetes Care 2017. Available from: https://care.diabetesjournals.org/content/diacare/suppl/2016/12/15/40.Supplement_1.DC1/DC_40_S1_final.pdf.
- Batista KT, Gabriela BM, Y-Schwartzman UP, Roberti AFSSA, Rosa AG, Correia CZ. Treatment of leprosy-induced plantar ulcers. Rev Bras Cir Plást 2019;34:497–503.
- Macedo EAB, Araujo RO, Silva RAR, Sousa NL, Torres GV. Treatment of varicose ulcer of the lower limbs by surgery and Unna boot: savings for the Brazilian healthcare system. Rev Ciência e Desenvolv 2018;11:684–698.
- Hobizal KB, Wukich DK. Diabetic foot infections: current concept review. Diab Foot Ankle. 2012;3:18409.
- Alves ED. Dressings, ostomies and dermatology: a multiprofessional approach. In: Malagutti W, Kakihara CT (editors). Enfermería global. São Paulo: Martinari; 2010.
- Carvalho MS. Evidence on the use of essential fatty acids in the treatment of wounds. Undergraduate Notebook – Biological and Health Sciences – UNIT. Sergipe 2015;2:55–64.
- Lania BG et al. Topical essential fatty acid oil on wounds: local and systemic effects. Plos One: Collection Social Psychiatry. São Paulo; 2019. https://doi.org/10.1371/journal.pone.0210059.
- Metcalfe DG, Bowler PG. Clinical impact of an anti-biofilm hydrofiber dressing in hard-to-heal wounds previously managed with traditional antimicrobial products and systemic antibiotics. Burns Trauma 2020;8:1–9.
- Hosny AEM, Rasmy SA, Aboul-magd DS, Kashef MT, El-bazza Z. The increasing threat of silver-resistance in clinical isolates from wounds and burns. Infect Drug Resist 2019;12:1985–2001.


