Volume 42 Number 2
Assessment of peristomal body profile to ensure the right fit to help prevent leakage
Anne Steen Hansen, Janice Colwell, Werner Droste, Grethe Vendelbo and Sarah James-Reid
Keywords ostomy, peristomal skin complications, fit to body, leakage, peristomal body profile
For referencing Hansen AS et al. Assessment of peristomal body profile to ensure the right fit to help prevent leakage. WCET® Journal Supplement 2022;42(1)Sup:s8-11
DOI
https://doi.org/10.33235/wcet.42.1.sup.s8-11
Submitted 15 March 2022
Accepted 12 April 2022
Abstract
Peristomal skin complications (PSCs) are a frequent issue for patients living with an ostomy. A common cause of PSCs is leakage of stomal effluent, which 76% of the patients experience at least once a month. To improve the quality of life (QoL) of people living with an ostomy, the underlying cause and predisposing factors for leakage must be identified and addressed during the selection of an ostomy solution. The aim of this publication is to highlight the importance of assessing the peristomal body profile (PBP) when finding the right ostomy solution and preventing leakage.
According to a recent consensus among ostomy care nurses, the pouch seal security and peristomal skin integrity are the most important factors to determine an optimal ostomy solution. Therefore, the patient assessment should include an evaluation of the peristomal area and type of stoma and output. The Peristomal Body Profile Terminology (BPT) was established to assist health practitioners to determine the PBP according to the area around the stoma, as well as the position of the stoma opening in relation to the skin.
Incorrect fit with consequential leakage can occur when the PBP is not considered in a structured way when selecting the ostomy solution. The most appropriate ostomy solution will vary according to the patient’s PBP and preference. Therefore, it is crucial for the patients to actively engage in the assessment of their PBP together with the ostomy care nurse, to find the most appropriate ‘fit to body’ solution.
Abbreviations
PSCs - Peristomal skin complications; QoL - Quality of life; BMI - Body mass index; PBP - Peristomal body profile; BPT - Body Profile Terminology
Introduction
Ostomy is a lifesaving surgical procedure for patients suffering from various conditions, including colorectal cancer, Crohn’s disease, diverticulitis and ulcerative colitis. It is estimated that more than one million people live with an ostomy in the US and around 700,000 people in Europe1. Several challenges may arise following stoma surgery, such as risk of leakage and peristomal skin complications (PSCs). Nurse specialists estimate that approximately 80% of patients living with an ostomy have developed PSCs, including contact dermatitis (irritant and allergic) and infections2,3. External factors such as the COVID-19 pandemic can aggravate the issue by making patients reluctant to seek help, as revealed by a recent survey that showed that 84% of ostomy patients failed to follow up with their healthcare practitioners about their skin issues during the pandemic4.
Leakage of stomal effluent is the most common cause for PSCs in patients living with an ostomy, and around 77% of the PSCs cases are associated with the contact of stomal effluent to the skin5. Leakage is also the major concern of patients living with an ostomy. It has been reported that 76% of patients with an ostomy experienced leakage at least once every month, while 65% of patients reported leakage outside baseplate and/or onto clothes at least once in the previous year6. The consequences of leakage are both physical and mental. The physical burden comprises feelings of pain and discomfort. The burden discourages patients to pursue a routine of physical activity, which can lead to weight gain and a potential worsening of the issue.
The mental burden is due to the constant worry of leakage. The majority of patients living with an ostomy reported that they refrained from physical or social activities because of the social stigma and risk of leakage onto clothes1. The social withdrawal may cause stress, anxiety and depression episodes, as well as excessive time dedicated to ostomy care. Using a validated four domain scale to measure the quality of life (QoL) of patients living with an ostomy, Hedegaard and colleagues7 reported that all domains of the QoL scale were negatively affected by the increased frequency of leakage, namely confidence in stoma appliance, comfort, discretion and socialising. Overall, the mental burden negatively impacts QoL in ostomy patients that report regular leakages8.
In order to help patients to have a better life with an ostomy, it is essential to understand the underlying cause and predisposing factors that can lead to leakage of stomal effluent. Among the risk factors, body mass (BMI) index is closely associated with the frequency of peristomal leakage and PSCs9. The position of the stoma opening in relation to the skin surface, the shape of the skin around the stoma and the location of the stoma are also contributing factors that impact the integrity of the system and can potentially lead to leakages more frequently10. Ensuring the best fit with the individual peristomal body profiles (PBP) is also supported by the guidelines of the World Council of Enterostomal Therapists (WCET®), the Association of Stoma Care Nurses (ASCN) and the Wound, Ostomy and Continence Nursing Society (WOCN®)11–13.
The patient’s PBP and type of stoma can have a profound impact on the QoL of the patients. Therefore, it is imperative that healthcare practitioners employ a standardised method to categorise the PBP so that they can recommend the optimal ostomy solution for each patient according to their individualised needs and body type. In this article, we review the characteristics of the patients with an ostomy according to their PBP and stoma type, as well as the guidelines on patient assessment to establish the PBP.
Assessment of the peristomal body and stoma profiles: a consensus approach among health practitioners
In light of the need for a standardised method to determine the PBP, an international board of stoma care nurses aimed to build a consensus over the key factors in assessing the PBP. The intention was to create practical guidelines on how to assess PBP and raise awareness among health practitioners on the principles that should guide ostomy patient care.
In a process that involved 1225 individual responses from nurses from 27 countries, a Modified Delphi survey was undertaken, and three separate surveys were conducted online. The survey results were later ratified by 960 nurses participating at the Ostomy Days, an international education program hosted by Coloplast in Copenhagen in April 2018. The consensus achieved among the ostomy care nurses was that, in order to determine the optimal ostomy solution for each patient, the pouch seal security and peristomal skin integrity should be considered the most important factors in the decision-making process. In addition, to select the most appropriate pouching system, the patient assessment guidelines should include an evaluation of the peristomal area, the type of stoma and output, and the patient’s preference and abilities.
To achieve this goal, all nurse survey responders agreed that patients should be educated and actively engaged in their pouch change process and in the evaluation of their peristomal skin health; they also specified the need for validated tools to evaluate the PBP14. The results from this consensus-based research improved the understanding of the current needs of ostomy patients. This process facilitated establishing clinical practice guidelines to increase the QoL of the patients by recommending the ostomy solution that match their PBP and ensure the best fit11–13. Furthermore, the experience-based approach enabled a quick acceptance and implementation of PBP by ostomy care nurses15.
Based on this consensus-driven survey, a common terminology for the PBP was also required. According to the definitions set by the Body Profile Terminology (BPT), the PBP of each patient can be characterised as ‘regular’ when the area around the stoma is at the same level of the abdomen, ‘inward’ when the stoma area sinks into the abdomen and ‘outward’ when the stoma area rises from the abdomen. The position of the ostomy opening in relation to the skin surface is also relevant for the determination of PBP and can be categorised as ‘above’, ‘at the same level’ or ‘below’ the surface of the skin, as illustrated in Figure 1. With those parameters in mind, the ostomy care nurse is equipped to determine the PBP for each patient and may then recommend the optimal ostomy solution based on the individual’s need.
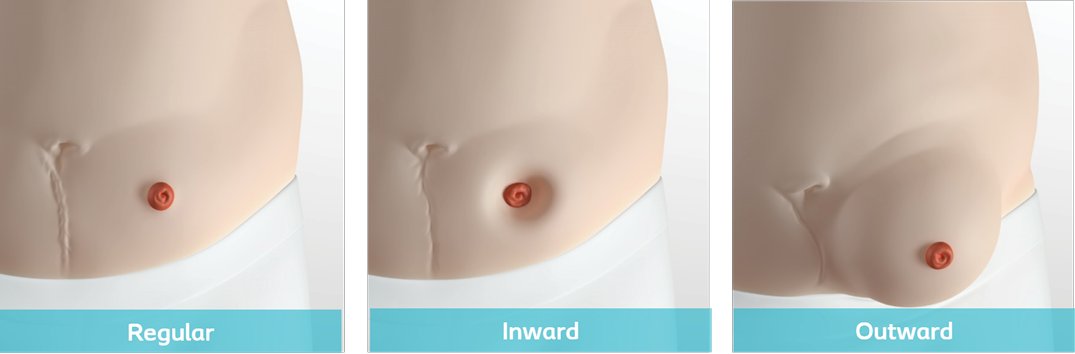
Figure 1. Peristomal Body Profile (PBP) categories. PBP can be determined according to (A) the skin area around the stoma and (B) position of the ostomy opening in relation to the surface of the skin
Future perspectives on the use of PBP in recommending new ostomy appliances
The consensus established in the survey on the PBP provides guidance to the international ostomy care community on how to identify specific PBP, which may help clear patterns in the incidence and potential causes of peristomal complications. For example, patients living with overweight and obesity have a higher predisposition to have a PBP considered ‘inward’ and ‘outward’ which, in turn, predicts a higher risk of leakage. In these cases, a convex or concave device might be an appropriate solution to ensure the best fit and prevent leakage16. Patients with normal weight BMI and a ‘regular’ PBP, on the other hand, have lower risk of leakage and, therefore, a flat base plate might be a viable solution.
Self-assessment tools, such as Coloplast’s BodyCheck17 can aid patients in finding their PBP and the most appropriate appliance. However, the role of the ostomy care nurse is essential to determine the correct ‘fit to body solution’ for each patient. A constant follow-up between the patient and the nurse can also be useful to regularly check the effectiveness of the device and to make any adjustment, if necessary. Regular check-ups are also important in case the patient’s BMI or PBP changes and a new appliance may offer a better fit.
The use of convexity to prevent leakage
Coloplast has developed a wide range of convex solutions for patients who often experience leakage. Using an objective leakage scale, the SenSura Mio Convex Soft has shown to significantly reduce the degree of leakage compared to flat appliances, while ensuring the feeling of security, comfort and body-fit16.
Convex appliances are also a viable alternative to prevent leakages in the postoperative period as they enable flattening the skin around the stoma and facilitating the stoma protrusion, directing the flow to the pouch. In fact, a survey of ostomy healthcare practitioners reported that 95% of the respondents claimed to use a convex pouching system in the 30 days following ostomy surgery, depending on the circumstances such as position of the stoma18. This indication has been the subject of debate, as some specialists warn that the use of convexity may cause mucocutaneous separation from the pressure exerted by the convex system. This idea, however, is not supported by research evidence.
To explore the available evidence and reach an agreement on the use of convex solution in the postoperative period, a group of 10 ostomy care nurses and physicians completed a scoping review identifying research-based evidence and gaps in our knowledge about the subject19. The panellists reached a consensus that convexity should be considered at any time after the ostomy surgery to secure the pouch seal and prevent leakages including in the immediate postoperative period, which was defined as days 0–8 following surgery. The panellists also agreed on eight statements that support this recommendation and identified the secure pouch seal and routine follow up visits as essential steps to prevent leakage and adapt to a life with an ostomy.
Conclusions
It is evident that a ‘one size fits all’ approach is not sufficient to prevent leakage. To provide a reliable ostomy solution, appliances with a personalised fit to the PBP hold the potential to reduce leakage. As such, the most appropriate ostomy solution will vary according to the patient’s PBP and preference. Therefore, it is crucial for the patients to be actively engaged in their pouch change process and work together with the ostomy care nurse to determine their PBP in order to find the best possible match between ostomy solution and patient´s PBP, thereby preventing PSCs.
Acknowledgements
This work was supported by Coloplast A/S. All authors were involved in reviewing and editing the manuscript, gave final approval and agreed to be accountable for all aspects of the work. The authors would like to thank Adriano Zager, PhD (Larix Sweden AB) for editorial and medical writing services.
Conflict of interest
Anne Steen Hansen is an employee of Coloplast A/S.
Funding
Editorial and medical writing services were funded by Coloplast A/S.
评估造口周围身体轮廓以确保贴合从而防止渗漏
Anne Steen Hansen, Janice Colwell, Werner Droste, Grethe Vendelbo and Sarah James-Reid
DOI: https://doi.org/10.33235/wcet.42.1.sup.s8-11
摘要
造口周围皮肤并发症(PSC)是造口患者的常见问题。PSC的一个常见原因是造口流出物渗漏,76%的患者每月至少经历一次。为了提高造口患者的生活质量(QoL),在选择造口术解决方案时必须确定和解决渗漏的根本原因和诱发因素。本出版物的目的是强调在寻找合适的造口解决方案和防止渗漏时评估造口周围身体轮廓(PBP)的重要性。
根据造口护理护士最近达成的共识,造口袋密封安全性和造口周围皮肤完整性是确定最佳造口解决方案的最重要因素。因此,对患者的评估应包括对造口周围区域以及造口类型和输出量的评估。确定造口周围身体轮廓术语(BPT)是为了帮助健康护理人员根据造口周围区域以及造口开口相对于皮肤的位置来确定PBP。
如果在选择造口解决方案时,未以结构化方式考虑PBP,则可能会发生造口袋未正确贴合,从而导致渗漏。最合适的造口解决方案将根据患者的PBP和偏好而有所不同。因此,为了找到最合适的“贴合身体”的解决方案,患者与造口护理护士一起积极参与PBP评估至关重要。
缩写
PSCs—造口周围皮肤并发症;QoL—生活质量;BMI—体重指数;PBP——造口周围身体轮廓;BPT—身体轮廓术语
引言
造口术是一种拯救生命的外科手术,适用于患有各种疾病的患者,包括结肠直肠癌、克罗恩病、憩室炎和溃疡性结肠炎。据估计,美国有超过100万人接受过造口术,而欧洲约有700,000人1。造口手术后可能会面临一些挑战,例如渗漏风险和造口周围皮肤并发症(PSC)。护理专家估计,大约有80%的造口患者出现了PSC,包括接触性皮炎(刺激性和过敏性)和感染2,3。最近的一项调查显示,COVID-19疫情等外部因素会使患者不愿寻求帮助,从而加剧这一问题,该调查显示,在疫情期间,84%的造口患者未能就其皮肤问题与他们的保健医师进行交流4。
造口流出物渗漏是造口患者出现PSC最常见的原因,大约77%的PSC病例与造口流出物与皮肤接触有关5。渗漏也是造口患者的主要担忧。据报告,76%的造口患者每月至少出现一次渗漏,而65%的患者报告称,在过去一年至少有一次渗漏在底盘外和/或衣服上6。渗漏造成生理和心理负担。生理负担包括疼痛和不适感,使患者无法进行常规的体力活动,这可能导致体重增加和问题潜在恶化。
心理负担是一直担心渗漏。大多数造口患者报告称,由于社会耻辱感和渗漏在衣物上的风险,他们避免进行体力活动或社交活动1。回避社交可能导致压力、焦虑和抑郁发作,以及用于护理造口的时间过长。Hedegaard和同事7使用经验证的四个领域量表来衡量造口患者的生活质量(QoL),并报告称,QoL量表的所有领域都受到渗漏发生率增加的负面影响,即对造口装置的信心、舒适度、自主性和社交。总体而言,从心理负担角度来说,报告频繁渗漏的造口患者的QoL受到了负面影响8。
为了帮助造口患者提高生活质量,必须了解可能导致造口流出物渗漏的根本原因和诱发因素。在众多风险因素中,体重(BMI)指数与造口周围渗漏和PSC的发生率密切相关9。造口开口相对于皮肤表面的位置、造口周围皮肤的形状和造口的位置也是影响造口袋系统完整性的因素,并可能导致更频繁的渗漏10。世界造口治疗师协会(WCET®)、造口护理护士协会(ASCN)和美国伤口、造口和失禁护理协会(WOCN®)11-13的指南也支持确保造口袋与患者造口周围身体轮廓(PBP)最佳贴合。
患者的PBP和造口类型会对患者的生活质量产生深远影响。因此,保健医师必须采用标准化方法对PBP进行分类,以便根据患者的个性化需求和体型为每位患者推荐最佳造口解决方案。在本文中,我们根据PBP和造口类型回顾了造口患者的特征,以及制定PBP的患者评估指南。
造口周围身体和造口轮廓的评估:健康护理人员的共识方法
鉴于需要一种标准化方法来确定PBP,国际造口护理护士协会旨在就评估PBP的关键因素达成共识。目的是就如何评估PBP制定实用指南,并提高健康护理人员对指导造口患者护理的原则的意识。
在涉及来自27个国家的护士的1225次个人回复的过程中,进行了改良Delphi调查,并在线进行了三次单独的调查。调查结果后来得到了参加造口日活动的960名护士的认可,这是一项由Coloplast于2018年4月在哥本哈根举办的国际教育项目。造口护理护士达成的共识是,为了确定每位患者的最佳造口解决方案,造口袋密封安全性和造口周围皮肤完整性应被视为决策过程中最重要的因素。此外,为了选择最合适的造口袋系统,患者评估指南应包括对造口周围区域、造口类型和输出量以及患者偏好和能力进行评价。
为了实现这一目标,所有针对调查给予回复的护士都同意,患者应接受教育,积极参与自身的造口袋更换过程,对自身造口周围皮肤健康进行评价;他们还指出需要使用经验证的工具来评价PBP14。这项基于共识的研究的结果提高了对造口患者当前需求的理解。这一过程有助于建立临床实践指南,通过给患者推荐与其PBP匹配并确保最佳贴合的造口解决方案来提高患者的生活质量11-13。此外,基于经验的方法使造口护理护士能够快速接受和实施PBP15。
基于这一共识驱动的调查,还需要一个通用的PBP术语。根据身体轮廓术语(BPT)设定的定义,当造口周围区域与腹部处于同一水平时,每位患者的PBP可以被描述为“正常”;当造口区域陷入腹部时为“向内”;当造口区域从腹部凸起时为“向外”。造口开口相对于皮肤表面的位置也与PBP的确定有关,可分为“高于”、“处于同一水平”或“低于”皮肤表面,如图1所示。考虑到这些参数,造口护理护士可以确定每位患者的PBP,然后根据患者个人需要推荐最佳造口解决方案。
图1.造口周围身体轮廓(PBP)类别。可以根据(A)造口周围皮肤面积和(B)造口开口相对于皮肤表面的位置来确定PBP
PBP在推荐新型造口装置中的应用前景
在关于PBP的调查中达成的共识为国际造口护理界就如何识别特定PBP提供了指导,这可能有助于明确造口周围并发症的发生率和潜在原因。例如,超重和肥胖患者更容易具有“向内”和“向外”PBP,这反过来又预示着更高的渗漏风险。在这些情况下,凸面或凹面装置可能是确保最佳贴合和防止渗漏的合适解决方案16。另一方面,体重BMI正常和PBP“正常”的患者发生渗漏的风险较低,因此,平面底盘可能是一种可行的解决方案。
自我评估工具,如Coloplast的BodyCheck17,可以帮助患者确定自身的PBP并找到最合适的装置。然而,造口护理护士对于为每位患者确定正确的“贴合身体的解决方案”至关重要。患者和护士之间的持续随访也有助于定期检查装置的有效性,并在必要时进行任何调整。定期检查也很重要,以防患者的BMI或PBP发生变化,并且新装置可能贴合更佳。
使用凸面装置防止渗漏
Coloplast为经常出现渗漏的患者开发了一系列凸面解决方案。通过使用客观的渗漏量表证明,SenSura Mio Convex Soft与平面装置相比,可显著降低渗漏程度,同时确保安全性、舒适感和身体贴合16。
凸面装置也是防止术后渗漏的可行选择,因为凸面装置可以使造口周围皮肤变平并促进造口突出,从而引液至造口袋。事实上,一项造口保健医师调查报告显示,95%的受访者声称,根据造口位置等情况,在造口术后30天内选择使用凸面造口袋系统18。这一做法一直是争议的主题,因为一些专家警告说,使用凸面装置可能会因凸面系统施加的压力导致皮肤粘膜分离。然而,这一想法并未得到研究证据的支持。
为寻找现有证据并就术后使用凸面装置达成一致,一组由10名造口护理护士和医生组成的小组完成了概况性评价,确定了基于研究的证据和我们对该主题的知识差距19。小组成员一致认为,应在造口手术后的任何时间(包括术后即刻,即术后第0-8天)均考虑凸面装置,以确保造口袋密封性并防止渗漏。小组成员还就支持这一建议的八项声明达成一致意见,并将确定造口袋密封性和进行例行随访访视视为防止渗漏和适应造口生活的必要步骤。
结论
很明显,“一刀切”的方法不足以防止渗漏。为了提供可靠的造口解决方案,与PBP个性化贴合的装置有可能能够减少渗漏。因此,最合适的造口解决方案将根据患者的PBP和偏好而有所不同。因此,至关重要的是,患者应积极参与自身的造口袋更换过程,并与造口护理护士一起确定自身PBP,以便找到最贴合患者PBP的造口解决方案,从而预防PSC。
致谢
本文得到了Coloplast A/S的支持。所有作者都参与了手稿的审查和编辑,给予了最终批准并同意对文章的各个方面负责。作者感谢Adriano Zager博士(Larix Sweden AB)提供的编辑和医学写作服务。
利益冲突声明
Anne Steen Hansen是Coloplast A/S的员工。
资金支持
编辑和医学写作服务由Coloplast A/S提供资金支持。
Author(s)
Anne Steen Hansen* BSc/ET
Coloplast A/S, Holtedam 3, 3050 Humlebæk, Denmark
Email dkasn@coloplast.com
Janice Colwell MSc/RN/CWOCN/FAAN
University of Chicago Medicine, Chicago, Il, USA
Werner Droste RN/ET
Seminaire and Beratung, Selm, Germany
Grethe Vendelbo RN/SD/ET
Hospitalsenheden Vest, Central Denmark Region, Denmark
Sarah James-Reid RGN
Ashford & St Peters NHS Foundation Trust, Lyne, Chertsey, UK
* Corresponding author
References
- Claessens I, Probert R, Tielemans C, Steen A, Nilsson C, Andersen BD, et al. The Ostomy Life Study: the everyday challenges faced by people living with a stoma in a snapshot. Gastrointestinal Nurs 2015;13(5):18–25.
- Fellows J, Voegeli D, Hakan-Bloch J, Herschend NO, Storling Z. Multinational survey on living with an ostomy: prevalence and impact of peristomal skin complications. Br J Nurs 2021;30(16):S22–S30.
- Colwell JC, McNichol L, Boarini J. North American wound, ostomy, and continence and enterostomal therapy nurses current ostomy care practice related to peristomal skin issues. J Wound Ostomy Continence Nurs 2017;44(3):257–61.
- Spencer K, Haddad S, Malandrino R. COVID-19: impact on ostomy and continence care. WCET J 2020;40(4):18–22.
- Herlufsen P, Olsen AG, Carlsen B, Nybaek H, Karlsmark T, Laursen TN, et al. Study of peristomal skin disorders in patients with permanent stomas. Br J Nurs 2006;15(16):854–62.
- Down G, Vestergaard M, Ajslev TA, Boisen EB, Nielsen LF. Perception of leakage: data from the Ostomy Life Study 2019. Br J Nurs 2021;30(22):S4–S12.
- Hedegaard CJ, Ajslev TA, Zeeberg R, Hansen AS. Leakage and peristomal skin complications influences user comfort and confidence and are associated with reduced quality of life in people with a stoma. WCET J 2020;40(4):23–9.
- Maydick-Youngberg D. A descriptive study to explore the effect of peristomal skin complications on quality of life of adults with a permanent ostomy. Ostomy Wound Manage 2017;63(5):10–23.
- Nybaek H, Bang Knudsen D, Norgaard Laursen T, Karlsmark T, Jemec GB. Skin problems in ostomy patients: a case-control study of risk factors. Acta Derm Venereol 2009;89(1):64–7.
- Gonzalez ER, Zurita CDP, Caballero GA, Rodriguez AH, Rodriguez EZ, Blazquez EG. Factors predictive of optimal peristomal skin status in patients with an ostomy: a secondary analysis. Br J Comm Nurs 2021;26(Sup12):S24–S34.
- WCET®. WCET® International Ostomy Guidelines, 2014.
- ASCN. ASCN Stoma Care National Clinical Guidelines, 2019.
- Ostomy Guidelines Task Force, Goldberg M, Aukett LK, Carmel J, Fellows J, Folkedahl B, et al. Management of the patient with a fecal ostomy: best practice guideline for clinicians. J Wound Ostomy Continence Nurs 2010;37(6):596–8.
- Colwell JC, Bain KA, Hansen AS, Droste W, Vendelbo G, James-Reid S. International consensus results: development of practice guidelines for assessment of peristomal body and stoma profiles, patient engagement, and patient follow-up. J Wound Ostomy Continence Nurs 2019;46(6):497–504.
- James-Reid S, Bain K, Hansen AS, Vendelbo G, Droste W, Colwell J. Creating consensus-based practice guidelines with 2000 nurses. Br J Nurs 2019;28(22):S18–S25.
- Kruse TM, Storling ZM. Considering the benefits of a new stoma appliance: a clinical trial. Br J Nurs 2015;24(22):S12, S4–8.
- Coloplast. BodyCheck; n.d. Available from: www.coloplast.us/Global/Ostomy/BodyCheck/BodyCheck
- Stoia-Davis J, Sims T, Colwell JC, Emodi K, Fellows J, Mahoney M, et al. Survey results on use of convex pouching system in the post-operative period. In press; 2022.
- Colwell JC, Davis JS, Emodi K, Fellows J, Mahoney M, McDade B, et al. Use of a convex pouching system in the post-operative period – a national consensus. In press; 2022.


