Volume 43 Number 1
WHAM evidence summary: traditional hypochlorite solutions
Emily Haesler, Keryln Carville
Keywords Traditional wound management, hypochlorite, Eusol, Dakin’s® solution, Milton® solution
For referencing Haesler E & Carville K. WHAM evidence summary: traditional hypochlorite solutions . WCET® Journal 2023; 43(1):35-40
DOI https://doi.org/10.33235/wcet.43.1.35-40
Clinical question
What is the best available evidence for use of traditional hypochlorite solutions for reducing wound infection and/or improving wound healing?
Summary
Traditional hypochlorites have been used to manage local wound infection since their introduction in the early 1900s1. Traditional hypochlorite solutions are those that have a high pH varying from 7.5 to 11.82-5. In contrast, recently developed hypochlorite solutions are pH-neutral, making them more appropriate for application to healing wound tissue. Level 5 bench research has demonstrated that traditional hypochlorite solutions have anti-bacterial properties;6-8 however, the effect may be short-lived9. Although Level 5 bench research has suggested that traditional hypochlorite solutions are toxic to cells and may delay wound healing,6, 8, 10, 11 Level 1 and 2 evidence2, 12-16 showed that acceptable healing outcomes can be achieved using traditional hypochlorite solutions, with one study demonstrating superior outcomes compared to an inert solution.17 Level 1 and 4 evidence12, 13, 16-20 indicated that traditional hypochlorite solutions are associated with reduction in signs and symptoms of local wound infection. Level 1 and 2 evidence13, 14, 16 showed that topical phenytoin13, 16, honey14 and nanocrystalline silver gel16 achieved better outcomes than a traditional hypochlorite solution, and these options could be considered in settings with access. The risk of delaying healing of the wound should be considered in the context of managing local wound infection and reducing the risk of spreading and systemic infection, when alternative less cytotoxic antiseptics are not available in the setting.
Clinical practice recommendations
All recommendations should be applied with consideration to the wound, the person, the health professional and the clinical context.
|
Traditional hypochlorite solutions could be applied to infected wounds in low resource settings in which less cytotoxic antiseptic solutions are not accessible (Grade B). |
Sources of evidence: search and appraisal
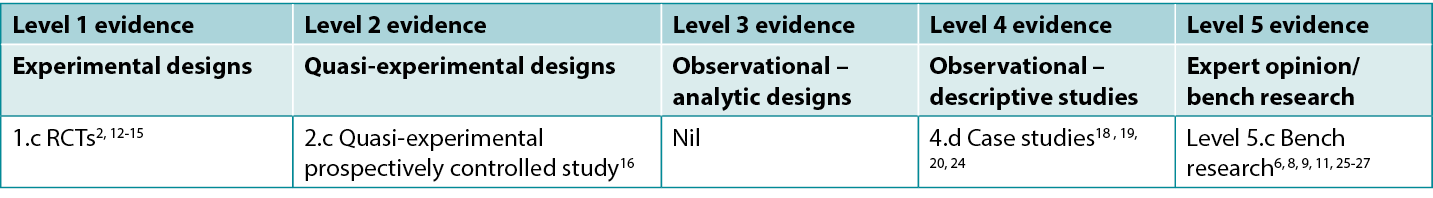
This summary was conducted using methods published by the Joanna Briggs Institute.21-23 The summary is based on a literature search combining search terms related to hypochlorites/EUSOL/Dakin’s® solution/Milton® solution and wound infection. Searches were conducted in the Cumulative Index to Nursing and Allied Health Literature (CINAHL), PubMed®, Google Scholar and Health Internetwork Access to Research Initiative (Hinari) databases and in the Cochrane Library for evidence conducted in human wounds reporting the use of traditional hypochlorite preparations published to October 2022 in English. Levels of evidence for intervention studies are reported in Table 1.
Table 1. Levels of evidence for clinical studies
Background
Traditional hypochlorites are preparations that occur as a reaction between chlorine and an alkaline salt, most commonly sodium or calcium 28, 29. They typically have a pH from 7.5 up to 11.8.2-5 Commonly used traditional hypochlorites include household bleach, Dakin’s® solution, Edinburgh University Solution of Lime (EUSOL) and Milton® solution. (N.b., no evidence on the use of Milton® solution for wound healing was identified).
Dakin’s® solution is a preparation of bleach diluted in distilled water to 0.5% concentration for clinical use. In some reports of its use, traditional Dakin’s® solution is diluted to half or quarter strength by mixing with additional water19. The preparation was developed by Henry Dakin on the war fields in France in 1915 to manage wound infection and to improve clinical outcomes for bullet and shrapnel wounds28, 30, 31. Bench research has demonstrated Dakin’s® solution has action against a range of microorganisms and biofilms, including (but not limited to) S. aureus, C. albicans, E. coli, K. pneumoniae, and P. aeruginosa6, 8, 9, 17, 25, 27 (Level 5).
EUSOL solution is made from chlorinated lime (calcium oxide) and boric acid (sodium salts) at a 0.25% concentration2, 24, 32, 33.The solution, which was also developed in the early 1900s, is traditionally used as a debriding agent and to manage infection.32, 34
Traditional hypochlorites are unstable and have a short shelf life.29, 34 They have a high pH2-5, which is associated with impaired wound healing. Both full strength (0.5%) Dakin’s® solution8 and half strength (0.25%) Dakin’s® solution6 have been reported to be cytotoxic to fibroblasts in laboratory studies, raising concerns that traditional hypochlorites at their full concentration may delay wound healing11, 16, 29-31, 34-36. To address these limitations, hypochlorites are now prepared electro-chemically to produce contemporary hypochlorites referred to as super-oxidised solutions29, 37. Although super-oxidised solutions have a longer shelf-life and a neutral pH, and they appear to have a good safety profile,29, 38 they are not universally available. In low resource settings, traditional hypochlorites are still used for managing wound infection39, 40.
Clinical evidence on dakin’s® solution
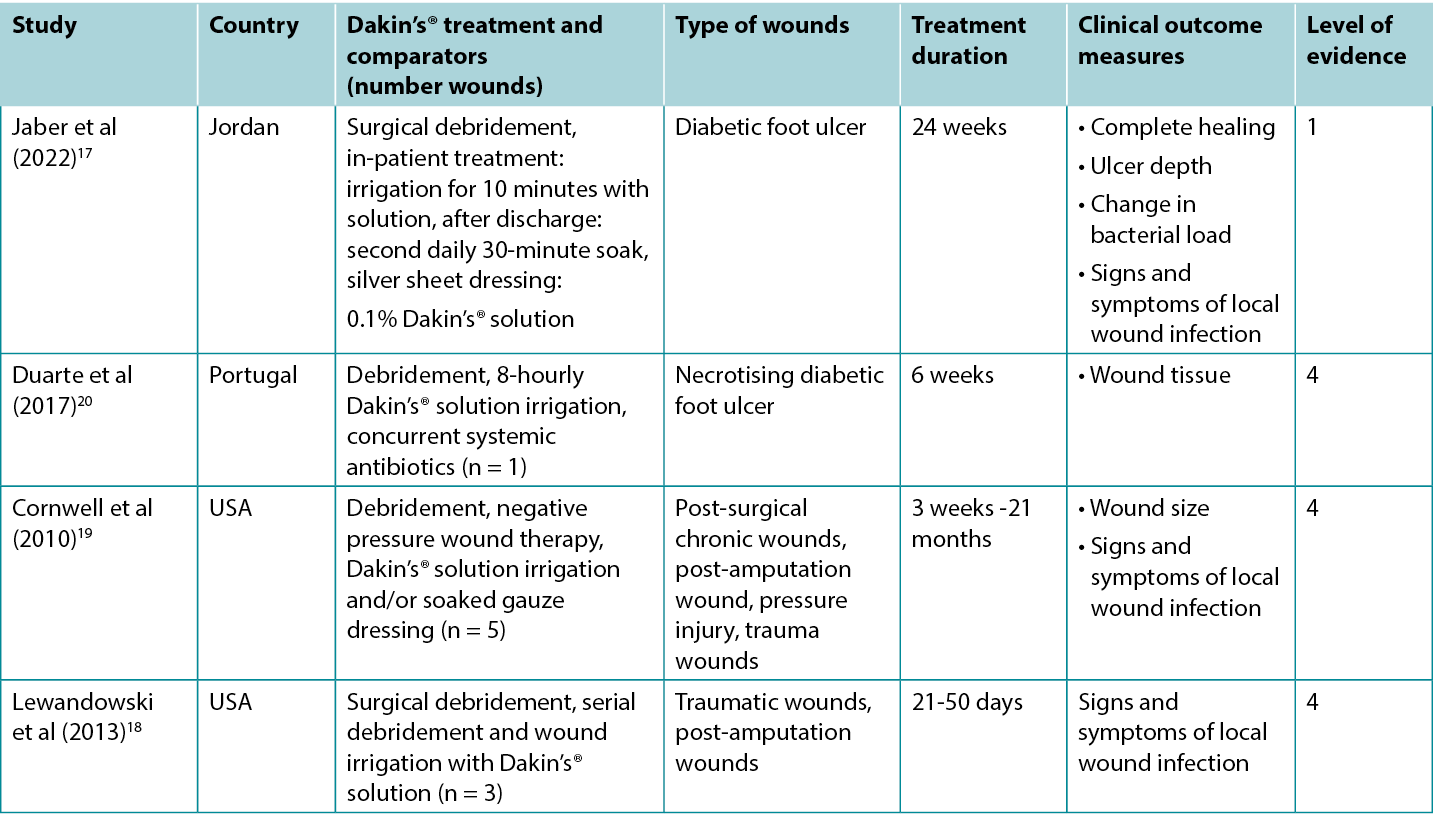
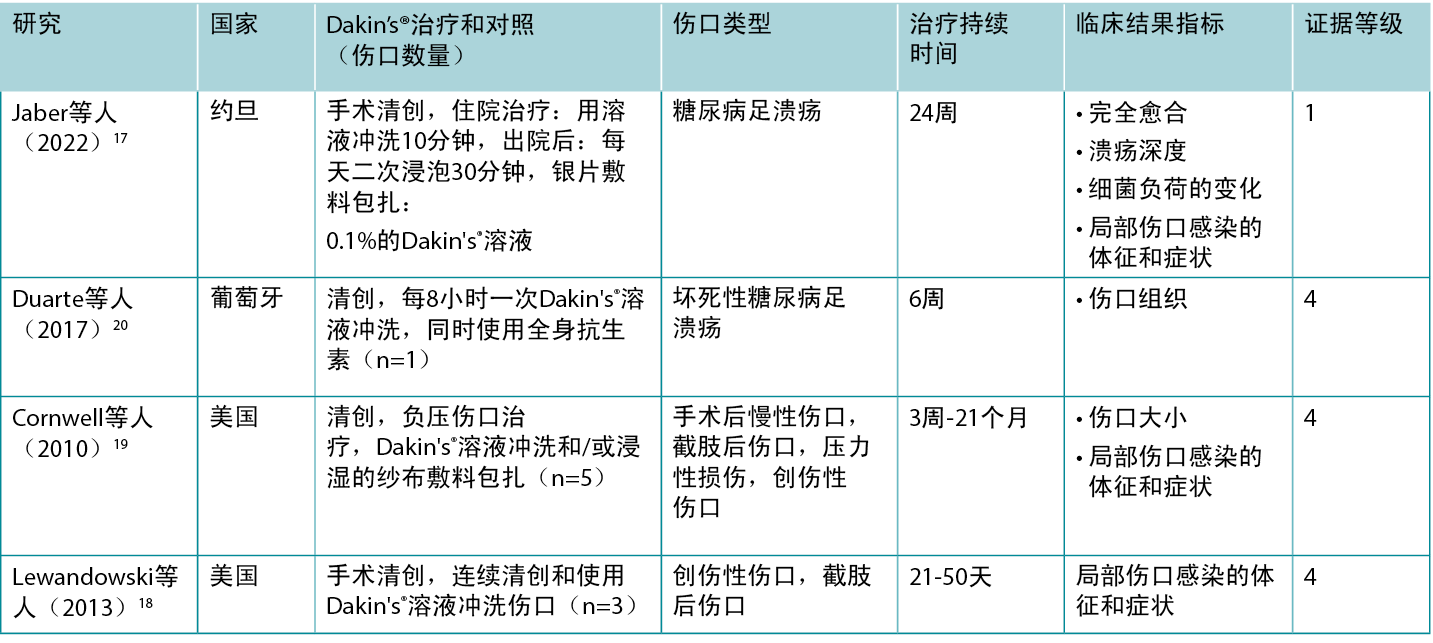
Studies reporting clinical outcomes of interest for treatment with traditional Dakin’s® solution are summarised in Table 2.
Table 2. Summary of the evidence for Dakin’s solution
Dakin’s® solution for promoting wound healing
An RCT17 at high risk of bias explored the use of Dakin’s® solution for treating infected diabetic foot ulcers (DFUs). Ulcers were surgically debrided on admission and received evidence based DFU care in conjunction with daily 10-minute irrigation with either Dakin’s® solution diluted to 0.1% concentration or normal saline, followed by application of a silver sheet dressing. Treatment was delivered in hospital for at least five days. On discharge, patients cleansed their own wounds every second day by soaking the DFU for 30 minutes in the assigned solution. Treatment continued for at least three months. Approximately 35% of DFUs treated with Dakin’s® solution were totally healed compared to 4% in the control group (odds ratio 11.9, 95% confidence interval 2.53 – 55.5, p < 0.001)17 (Level 1).
Dakin’s® solution for treating signs and symptoms of wound infection
In the RCT17 comparing Dakin’s® solution to normal saline for DFUs, quantitative wound swab analysis showed DFUs treated with Dakin’s solution had a reduction from baseline in microbial load of 1 log cycle or more after five days (statistically significant versus control, p < 0.001). Local wound infection resolved in more DFUs treated with Dakin’s® solution compared to normal saline (35.6% versus 4.4%, p = not reported)17 (Level 1).
There are numerous case reports18-20 of infected wounds of various aetiologies that have been successfully treated with regimens that include regular irrigation with Dakin’s® solution. Many of the wounds were reported to be extensive and deep, with exposed ligament and bone and/or necrotising tissue. Wounds were either confirmed or suspected to be colonised with anaerobic bacteria20 or fungal organisms18. To treat wound odour19, wound exudate19 and extensive slough18-20 (all recognised signs and symptoms of local wound infection41) wounds were surgically debrided and regularly irrigated with full, half or quarter strength Dakin’s® solution. Many of the regimens also included systemic antibiotics, serial surgical debridement, negative pressure wound therapy and split skin grafting. The cases were reported to achieve resolution of signs and symptoms of local wound infection and development of healthy granulation tissue or complete epithelialisation18-20 (Level 4).
Clinical evidence on eusol solution
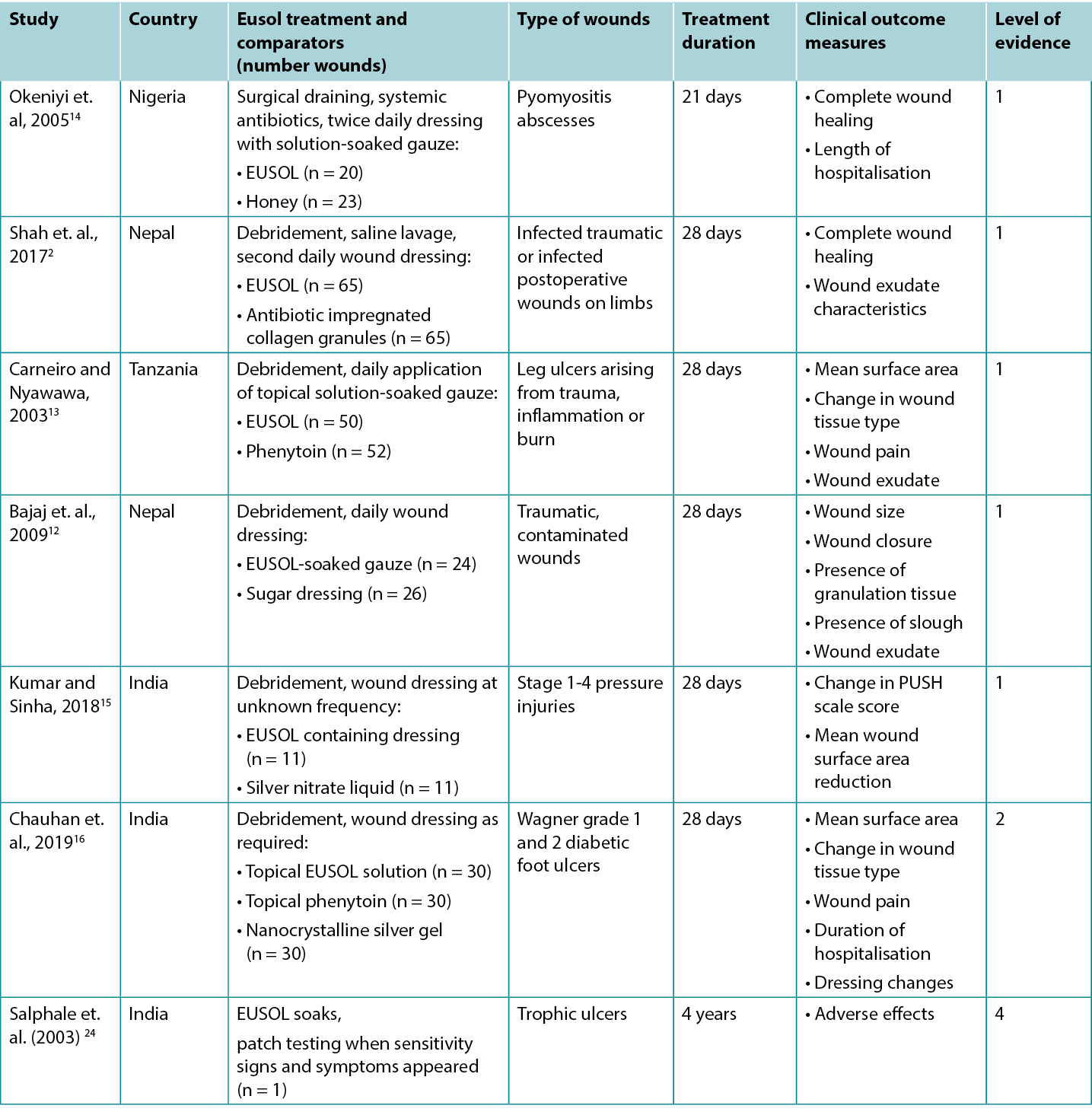
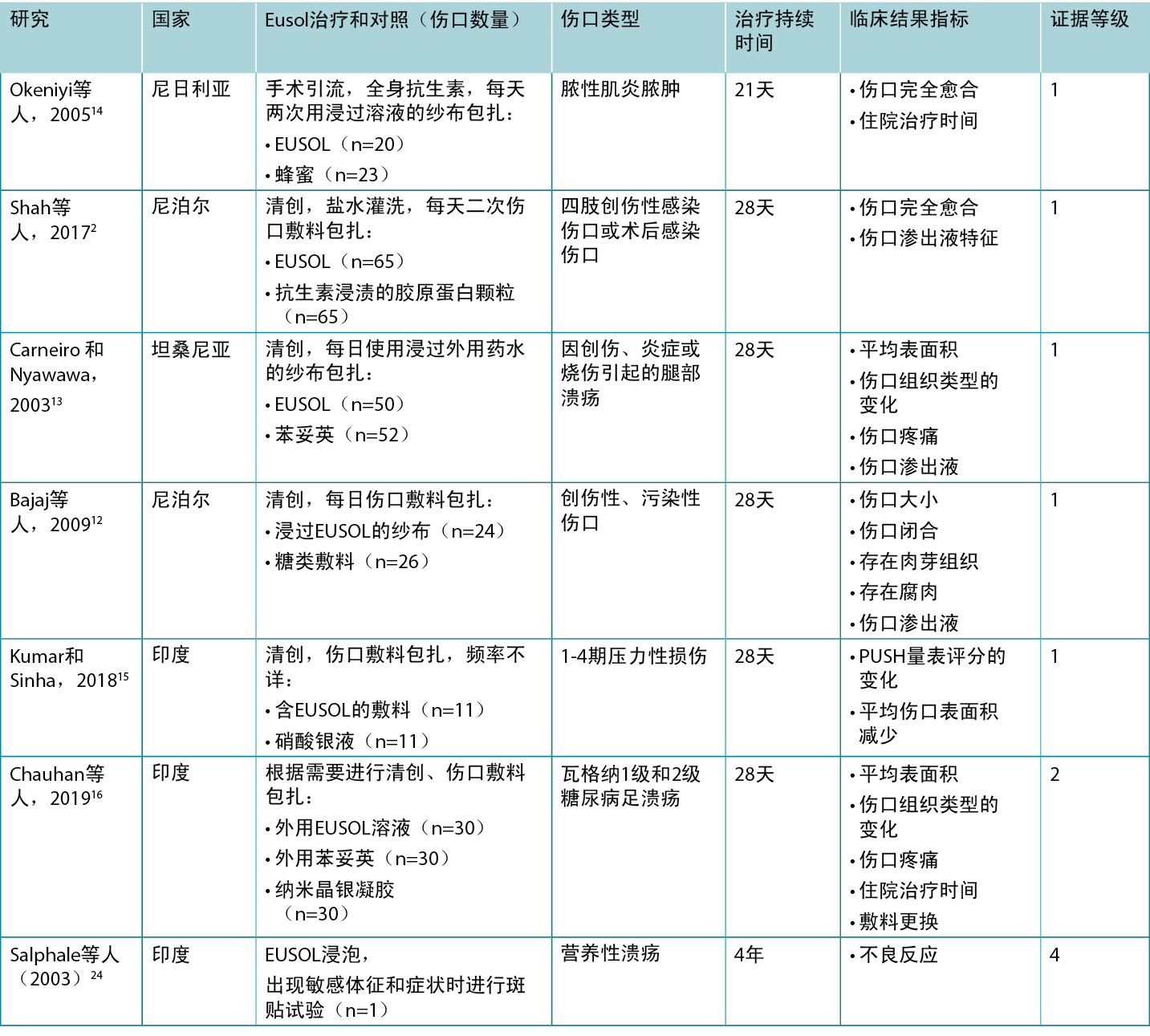
Studies reporting clinical outcomes of interest for treatment with traditional Edinburgh Solution of Lime (EUSOL) solution are summarised in Table 3.
Table 3. Summary of the evidence for EUSOL solution
EUSOL solution for improving wound healing
Five Level 1 studies and one Level 2 study provided evidence on EUSOL for improving healing of wounds of various aetiologies. In the first RCT14 (32 children with 43 wounds), which was at moderate risk of bias, open wounds (surgically excised pyomyositis abscesses) were packed twice daily with either EUSOL-soaked gauze or honey-soaked gauze. At 3-week follow-up, 55% of the EUSOL-treated abscesses achieved complete healing; compared to the 87% healing rate in the honey group (p < 0.047)14 (Level 1).
The second RCT,2 also at high risk of bias, reported use of EUSOL dressings to treat infected traumatic wounds. In this study, EUSOL was compared with an antibiotic-impregnated collagen granule dressing. At 4-week follow-up, 53.8% of the EUSOL-treated wounds were completely healed, and the remaining wounds had healthy granulation tissue. This was not statistically significantly different from the group treated with collagen granules, of which 69% completely healed, with the remainder achieving healthy granulation (p = 0.416)2 (Level 1).
A comparison of EUSOL-soaked gauze to sugar dressings is reported in a third RCT12 at high risk of bias that was conducted in traumatic, contaminated wounds (n = 50). After four weeks of daily wound dressings, wounds treated with the EUSOL dressing achieved superior results to the wounds treated with sugar dressings, including wound size reduction (p = 0.0042), achievement of granulation (p = 0.0048) and wound closure rate (p = 0.008)12 (Level 1).
In a fourth RCT13 at high risk of bias, chronic leg ulcers (n = 102) were treated daily with debridement followed by application of either EUSOL or topical phenytoin. Ulcers that achieved uniform granulation were treated with skin grafts. Wound surface area and presence of granulation tissue were evaluated weekly during the 28-day treatment period. The ulcers treated with EUSOL showed a mean reduction in surface area of about 60% over 28 days; this improvement appeared to be inferior to the topical phenytoin group (p = not reported). Although 86% of the ulcers receiving EUSOL achieved healthy granulation by 28 days, this was statistically significantly poorer outcome than the phenytoin group13 (Level 1).
The final RCT15, which was also at high risk of bias, reported a comparison of EUSOL-soaked gauze with a topical silver nitrate (0.01% w/v) liquid for treating pressure injuries (PIs) in people with spinal cord injury (n = 22). The groups were matched for severity of PIs at baseline. All Stage 1 PIs healed within two weeks of treatment. For Stage 2 PIs, those treated with EUSOL decreased in wound size by a mean of 47% after four weeks. For Stage 3 PIs treated with EUSOL, the average reduction in wound area at 4 weeks was 17%, compared with a mean size reduction of 26% for the silver-based treatment (p values = not reported). No Stage 4 PIs healed in the 4-week study duration15 (Level 1).
In a comparative study,16 which was at high risk of bias, EUSOL solution was compared to phenytoin powder and nanocrystalline silver gel for promoting healing in DFUs of Wagner grade 1 (superficial ulcer) and grade 2 (deep ulcer). The DFUs were surgically debrided as required and treated for up to four weeks with the assigned topical treatment. At 4-week follow-up, 73.33% of the DFUs treated with EUSOL solution had granulation tissue in the wound bed (p > 0.05). At baseline the mean ulcer size in the EUSOL-treated group was 16.66 cm2 ± 7.52 cm2, reducing to a mean of 7.7cm2 ± 6.65 cm2 by the end of four weeks, which may be clinically significant for patients. However, the EUSOL-treated DFUs achieved statistically significantly inferior results compared with those treated with phenytoin powder or nanocrystalline silver gel16 (Level 2).
EUSOL solution for reducing signs and symptoms of wound infection
Four of the above studies2, 12, 13, 16 reported reduction in signs and symptoms that are associated with local wound infection, including wound-associated pain, wound exudate, and a sloughy wound surface.41
In the study comparing EUSOL to topical phenytoin, the people with EUSOL-treated ulcers reported reduction in severe wound-associated pain and improvement in wound exudate by the second week of treatment13. Although the topical phenytoin group had superior outcomes at week two, there was no statistically significant difference by 28 days In the study comparing EUSOL dressings to sugar dressings, fewer wounds treated with EUSOL had a sloughy wound surface (p = 0.0034) and exudate level (p = 0.011) after four weeks.12 The infected wounds that were treated with EUSOL in the RCT by Shah et. al. (2017) 2 showed improvement in wound exudate characteristics by the fourth week of treatment and this was not statistically significantly different (p = 0.24) to the exudate profile of the antibiotic-impregnated collagen granule group2 (Level 1).
In the study conducted in DFUs,16 EUSOL solution was associated with a small reduction in pain after four weeks of treatment (mean pain score reduction of 1.87 ± 1.57 on a five-point visual analogue scale). This was unlikely to be clinically significant.16 (Level 2).
Considerations for use
Adverse effects reported with traditional hypochlorites
- Contact sensitivity to traditional hypochlorites has been observed in rare cases24 (Level 4).
- Although skin irritation,34 mild pain on application9and chemical burns with using the solution at inappropriate concentrations16 have been associated with traditional hypochlorites, these adverse events were not observed in the studies reported in this evidence summary.
Preparation of solutions in low resource settings
- A 0.5% Dakin’s® solution can be prepared with 25 mL household bleach mixed with 2 teaspoons of baking soda (bicarbonate of soda/sodium bicarbonate) in 1 L of clean water40. The solution has a short shelf-life,28, 29 and bench research has suggested the solution may provide inadequate antibacterial effect within 24 hours of preparation9. Therefore, the solution should be prepared every 24 hours40.
- A EUSOL solution can be prepared with 12.5 g sodium hypochlorite (bleaching powder) and 12.5 g of boric acid combined in 1 L of clean, lukewarm water. The solution has a short shelf life and preparation immediately before use is recommended2, 24, 32, 33.
Conflict of interest
The authors declare no conflicts of interest in accordance with International Committee of Medical Journal Editors (ICMJE) standards.
About wham evidence summaries
WHAM evidence summaries are consistent with methodology published in Munn Z, Lockwood C, Moola S. The development and use of evidence summaries for point of care information systems: A streamlined rapid review approach, Worldviews Evid Based Nurs. 2015;12(3):131-8.
Methods are outlined in resources published by the Joanna Briggs Institute21-23 and on the WHAM Collaborative website: http://WHAMwounds.com. WHAM evidence summaries undergo peer-review by an international, multidisciplinary Expert Reference Group. WHAM evidence summaries provide a summary of the best available evidence on specific topics and make suggestions that can be used to inform clinical practice. Evidence contained within this summary should be evaluated by appropriately trained professionals with expertise in wound prevention and management, and the evidence should be considered in the context of the individual, the professional, the clinical setting and other relevant clinical information.
Copyright © 2023 Wound Healing and Management Collaborative, Curtin Health Innovations Research Institute, Curtin University
WHAM证据总结:传统次氯酸盐溶液
Emily Haesler, Keryln Carville
DOI: https://doi.org/10.33235/wcet.43.1.35-40
临床问题
使用传统次氯酸盐溶液减少伤口感染和/或改善伤口愈合的现有最佳证据是什么?
摘要
传统的次氯酸盐自1900年代初期问世以来,一直用于管理局部伤口感染1。传统的次氯酸盐溶液pH值较高,从7.5到11.8不等2-5。相比之下,最近开发的次氯酸盐溶液pH值呈中性,使其更适合用于愈合伤口组织。5级实验室研究表明,传统的次氯酸盐溶液具有抗菌特性,6-8但是效果可能是较短暂9。尽管5级实验室研究表明,传统次氯酸盐溶液对细胞有毒性,并可能会延迟伤口愈合,6, 8, 10, 11但1级和2级证据2, 12-16显示,使用传统次氯酸盐溶液可以达到可接受的愈合效果。一项研究显示,与惰性溶液相比,传统次氯酸盐溶液的效果更好。171级和4级证据12, 13, 16-20表明,传统次氯酸盐溶液与局部伤口感染的体征和症状减少有关。1级和2级证据13, 14, 16显示,外用苯妥英13, 16、蜂蜜14和纳米晶银凝胶16取得了比传统次氯酸盐溶液更好的效果,在有条件的情况下可以考虑这些方案。在没有其他细胞毒性较低的消毒剂的情况下,应在管理局部伤口感染、减少扩散和全身感染风险的背景下,考虑伤口延迟愈合的风险。
临床实践建议
采用任何建议时,应考虑伤口、患者、专业医护人员和临床环境。
传统次氯酸盐溶液可用于在资源匮乏环境下处理伤口感染,在这种环境下,无法获得细胞毒性较低的消毒溶液(B级)。
证据来源检索和评价
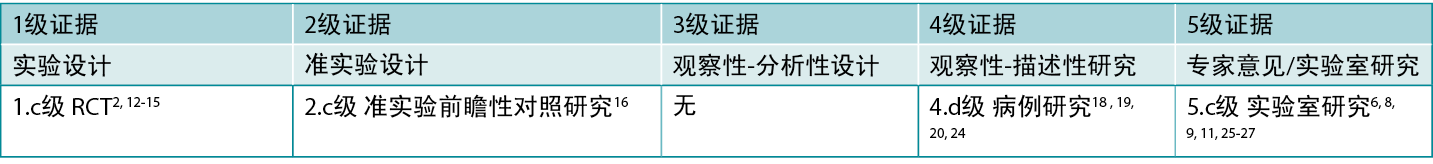
本总结采用乔安娜·布里格斯研究所发布的方法进行。21-23本总结基于文献检索,结合了与次氯酸盐/EUSOL/Dakin's®溶液/Milton®溶液和伤口感染相关的检索词。在护理与联合卫生文献累积索引(CINAHL)、 PubMed®、谷歌学术和卫生互联网共享研究成果倡议(Hinari)数据库以及Cochrane图书馆中进行了检索,寻找在2022年10月之前以英文发表的报告使用传统次氯酸盐制剂处理人体伤口的证据。表1报告了干预研究的证据等级。
表1.临床研究的证据水平
背景
传统的次氯酸盐是氯和碱性盐(最常见的是钠或钙)之间发生反应生成的制剂28, 29。它们的pH值通常在7.5至11.8之间。2-5常用的传统次氯酸盐包括家用漂白剂、Dakin's®溶液、爱丁堡大学石灰溶液(EUSOL)和Milton®溶液。(注:未发现使用Milton®溶液治疗伤口的证据)。
Dakin's®溶液是一种用蒸馏水稀释至0.5%浓度的漂白剂,供临床使用。在一些使用报告中,传统的Dakin's®溶液通过与额外的水混合稀释至一半或四分之一浓度19。该制剂由亨利·达金(Henry Dakin)于1915年在法国战场上开发,用于处理伤口感染并改善子弹伤和弹片伤的临床结果28, 30, 31。实验室研究表明,Dakin's®溶液对一系列微生物和生物膜有作用,包括(但不限于)金黄色葡萄球菌、白色念珠菌、大肠杆菌、肺炎克雷伯菌和铜绿假单胞菌6, 8, 9, 17, 25, 27(5级)。
EUSOL溶液由浓度为0.25%的氯化石灰(氧化钙)和硼酸(钠盐)制成,2,24,32,33。该溶液也是在20世纪初开发的,传统上被用作清创剂和处理感染。32,34
传统的次氯酸盐不稳定,有效期短。29, 34它们的pH值很高2-5,这与伤口愈合不良有关。据报告,在实验室研究中,全浓度(0.5%)Dakin's®溶液8和半浓度(0.25%)Dakin's®溶液6均对成纤维细胞具有细胞毒性,这引起了人们对传统次氯酸盐在全浓度下可能延迟伤口愈合的担忧11, 16, 29-31, 34-36。为了解决这些限制,现在通过电化学方法制备次氯酸盐,以生产被称为超氧化溶液的现代次氯酸盐29, 37。尽管超氧化溶液有效期较长,pH值呈中性,而且似乎具有良好的安全性特征,29, 38但它们并非普遍可及。在资源匮乏的环境中,传统的次氯酸盐仍被用于管理伤口感染39,40。
DAKINÅfS®溶液的临床证据
表2总结了报告使用传统Dakin's®溶液进行治疗的相关临床结果的研究。
表2.DakinÅfs溶液的证据总结
使用Dakin's®溶液促进伤口愈合
一项存在高偏倚风险的随机对照试验(RCT)17探讨了使用Dakin's®溶液治疗受感染的糖尿病足溃疡( DFU)。入院时对溃疡进行了手术清创,并接受循证DFU护理,并每天使用稀释至0.1%浓度的Dakin's®溶液或生理盐水冲洗10分钟,然后使用银片敷料。在医院接受治疗的时间至少为五天。出院时,患者每隔一天清洗自己的伤口,方法是将DFU在指定的溶液中浸泡30分钟。治疗至少持续三个月。在使用Dakin's®溶液治疗的DFU中,约有35%完全愈合,而对照组仅4%完全愈合(比值比为11.9,95%置信区间为2.53-55.5,P<0.001)17(1级)。
使用Dakin's®治疗溶液治疗伤口感染的体征和症状
在比较Dakin's®溶液和生理盐水治疗DFU的RCT17中,定量伤口拭子分析显示,用Dakin's溶液治疗的DFU在五天后微生物负荷较基线减少1个对数周期或更多(与对照组相比具有统计学显著性,P<0.001)。与生理盐水相比,使用Dakin's®溶液治疗的DFU有更多的局部伤口感染得到缓解(35.6% vs 4.4%,P=未报告)17(1级)。
有许多病例报告18-20表明各种病因的感染伤口通过包括定期使用Dakin's®溶液冲洗在内的方案得到成功治疗。据报告,许多伤口大而深,韧带和骨骼外露和/或坏死组织暴露在外。伤口被证实或疑似有厌氧菌20或真菌18微生物定植。为了处理伤口异味19、伤口渗出液19和大面积腐肉18-20(所有公认的局部伤口感染的体征和症状41),对伤口进行手术清创,并定期用全浓度、半浓度或四分之一浓度的Dakin's®溶液进行冲洗。许多治疗方案还包括全身抗生素、连续手术清创、负压伤口治疗和分层皮肤移植。据报告,这些病例实现了局部伤口感染体征和症状的消退,并出现了健康的肉芽组织或完全上皮化18-20(4级)。
EUSOL溶液的临床证据
表3总结了报告使用传统爱丁堡石灰溶液(EUSOL)进行治疗的相关临床结果的研究。
表3.EUSOL溶液的证据总结
使用EUSOL溶液改善伤口愈合
五项1级研究和一项2级研究提供了EUSOL改善各种病因的伤口愈合的证据。在存在中等偏倚风险的第一项RCT14(32名儿童,43个伤口)中,开放性伤口(手术切除的脓性肌炎脓肿)每天两次用EUSOL浸泡的纱布或蜂蜜浸泡的纱布包扎。在3周的随访中,EUSOL治疗的脓肿中有55%实现了完全愈合;而蜂蜜组的愈合率为87%(P<0.047)14(1级)。
第二项RCT2也存在高偏倚风险,报告了使用EUSOL敷料治疗感染的创伤性伤口的情况。在这项研究中,将EUSOL与抗生素浸渍的胶原蛋白颗粒敷料进行了比较。在4周的随访中,EUSOL治疗的伤口中有53.8%完全愈合,其余伤口有健康的肉芽组织。结果与胶原蛋白颗粒治疗组之间无统计学显著性差异,该组中69%完全
愈合,其余伤口有健康的肉芽形成(p=0.416)2(1级)。
第三项RCT12报告了EUSOL浸泡的纱布与糖类敷料的比较,该试验具有较高的偏倚风险,在创伤性污染伤口中进行(n=50)。 每天进行伤口敷料包扎持续4周后,相较于使用糖类敷料治疗的伤口,使用EUSOL敷料治疗的伤口取得了更好的效果,包括伤口尺寸减小(p=0.0042)、肉芽形成(p=0.0048)和伤口闭合率(p=0.008)12(1级)。
在第四项存在高偏倚风险的RCT13中,慢性腿部溃疡(n=102)每天接受清创治疗,然后施用EUSOL或外用苯妥英。实现均匀肉芽形成的溃疡用皮肤移植来治疗。在28天的治疗期间,每周对伤口表面积和是否存在肉芽组织进行评估。使用EUSOL治疗的溃疡在28天内表面积平均减少了约60%;这种改善似乎不如外用苯妥英组(P=未报告)。尽管接受EUSOL治疗的溃疡中有86%在28天时形成了健康的肉芽,但从统计学角度,这比苯妥英组的结果要差很多13(1级)。
最后一项RCT15也存在高偏倚风险,报告了EUSOL浸泡的纱布与外用硝酸银(0.01% w/v)液在治疗脊髓损伤患者压力性损伤(PI)方面的比较(n=22)。各组在基线时根据PI的严重程度进行匹配。所有1期PI在治疗后两周内愈合。对于2期PI,接受EUSOL治疗的患者在四周后伤口大小平均减少47%。对于使用EUSOL治疗的3期PI,第4周时伤口面积平均减少17%,而硝酸银组的伤口平均面积减少26%(P值=未报告)。在为期4周的研究时间里,4期PI均未愈合15(1级)。
在一项存在高偏倚风险的比较研究中16,研究者比较了EUSOL溶液与苯妥英粉和纳米晶银凝胶在促进瓦格纳1级(浅表溃疡)和2级(深部溃疡)DFU愈合方面的效果。根据需要对DFU进行手术清创,并使用指定的外用治疗方法进行长达4周的治疗。在4周的随访中,使用EUSOL溶液治疗的DFU中有73.33%在伤口床上有肉芽组织(P>0.05)。在基线时,EUSOL治疗组的平均溃疡尺寸为16.66 cm2Å}7.52 cm2,到第四周结束时减少到平均7.7 cm2Å}6.65 cm2,这可能对患者有临床意义。然而,使用EUSOL治疗的DFU实现的结果在统计学上显著劣于使用苯妥英粉或纳米晶银凝胶治疗的DFU16(2级)。
使用EUSOL溶液减少伤口感染体征和症状
上述研究中有四项2、12、13、16报告了与局部伤口感染相关的体征和症状的减少,包括与伤口相关的疼痛、伤口渗出液和伤口表面腐烂。41
在比较EUSOL和外用苯妥英的研究中,接受EUSOL治疗的溃疡患者报告说,在治疗的第二周,与伤口有关的严重疼痛有所减轻,伤口渗出也有所改善13。虽然外用苯妥英组在第二周有更好的结果,但到28天时没有统计学上的显著差异。在比较EUSOL敷料和糖类敷料的研究中,使用EUSOL治疗的伤口在四周后有较少的伤口表面腐烂(p=0.0034)和渗出液水平(p=0.011)。12 Shah等人(2017)2在RCT中使用EUSOL治疗的感染伤口显示,到治疗的第四周,伤口渗出液特征有所改善,与抗生素浸渍胶原蛋白颗粒组2的渗出液特征没有统计学上的显著差异(P=0.24)(1级)。
在对DFU进行的研究中,16EUSOL溶液与治疗四周后的疼痛小幅减少相关(在五点目测类比量表上,平均疼痛评分减少1.87Å}1.57)。这不太可能有临床意义16(2级)。
使用注意事项
传统次氯酸盐的不良反应报告
- 在极少数情况下观察到对传统次氯酸盐的接触敏感性24(4级)。
- 尽管皮肤刺激34、使用时轻度疼痛9以及使用不适当浓度的溶液16引起的化学灼伤与传统次氯酸盐有关,但在本证据总结中报告的研究中并未观察到这些不良事件。
在资源匮乏的环境中制备溶液
- 用25 mL家用漂白剂与2茶匙小苏打(碳酸氢钠)混合,溶于1 L清水中,可以制备0.5%的Dakin's®溶液40。该溶液的有效期很短,28, 29而且实验室研究表明,该溶液在制备后24小时内可能无法提供足够的抗菌效果9。因此,应每24小时制备一次溶液40。
- 用12.5 g次氯酸钠(漂白粉)和12.5 g硼酸混合,溶于在1升干净的温水中,可以制备EUSOL溶液。该溶液的有效期很短,建议制备后立即使用2, 24, 32, 33。
利益冲突声明
根据国际医学期刊编辑委员会(ICMJE)的标准,作者声明无利益冲突。
关于WHAM证据总结
WHAM证据总结采用的方法与以下文献中发表的方法一致:Munn Z, Lockwood C, Moola S. The development and use of evidence summaries for point of care information systems: A streamlined rapid review approach, Worldviews Evid Based Nurs. 2015;12(3):131-8.
乔安娜·布里格斯研究所21-23和WHAM合作网站(http://WHAMwounds.com)发布的资源列出了这些方法。 WHAM证据总结经过国际多学科专家参考小组的同行评审。WHAM证据总结提供了关于特定主题的最佳可用证据的总结,并提出了可用于指导临床实践的建议。本总结中包含的证据应由经过适当培训的具有伤口预防和管理专业知识的专业人士进行评价,并应根据个人、专业人士、临床环境以及其他相关临床信息考虑证据。
版权所有˝2023科廷大学科廷健康创新研究所伤口愈合和管理协作组织
Author(s)
Emily Haesler
PhD P Grad Dip Adv Nurs (Gerontics), BN, FWA
Adjunct Professor, Curtin University, Curtin Health Innovation Research Institute, Wound Healing and Management (WHAM) Collaborative
Keryln Carville
RN PhD STN(Cred) CF FWA
Professor, Silver Chain Group and Curtin University, Curtin Health Innovation Research Institute, Wound Healing and Management (WHAM) Collaborative
References
- Broughton G, Burris D. War and medicine: A brief history of the military’s contribution to wound care through World War I. Adv Wound Care, 2010;1:3-7.
- Shah AB, Maharjan R, Shrestha BP, Chaudhary P. A randomized controlled trial comparing EUSOL versus antibiotic loaded collagen granules as dressing agents in the management of traumatic infected wounds. Int J Orthop Sci 2017;3(2):157-162. DOI: 10.22271/ortho.2017.v3.i2c.24
- Alpha Medical Solutions. 2018. Milton® Anti-bacterial solution. Available from: https://www.alphamedicalsolutions.com.au/content/Milton-Anti-Bacterial-Solution-MSDS-Feb-2019.pdf. [Accessed Jan 2023].
- Ataman Chemicals. 2020. Sodium hypochlorite. Available from: https://www.atamanchemicals.com/sodium-hypochlorite_u24324/. [Accessed Jan 2023].
- Black J. Ten top tips: Wound irrigation. Wounds Int, 2022;13(2):2-4.
- Heggers J, Sazy J, Stenberg B, Strock L, McCauley R, Hernom D, Robson M. Bacterial and wound healing properties of sodium hypochlorite solutions: The 1991 Lindberg Award. J Burn Care Rehabil, 1991;12(5):420-4.
- Lessing M, McNulty A. Intermittent exposure to wound irrigation solutions disrupts P. aeruginosa and S. aureus immature biofilms in vitro. Wound Rep Reg Conf: 22nd Annual Meeting of the Wound Healing Society, 2012;20(2):A28.
- Lineaweaver W, McMorris S, Soucy D, Howard R. Cellular and bacterial toxicities of topical antimicrobials. Plast Reconstr Surg, 1985;75(3):394-6.
- Cotter J, Fader R, Lilley C, Herndon D. Chemical parameters, antimicrobial activities, and tissue toxicity of 0.1 and 0.5% sodium hypochlorite solutions. Antimicrob Agents Chemother, 1985;28(1):118-22.
- Wilson J, Mills J, Prather I, Dimitrijevich S. A toxicity index of skin and wound cleansers used on in vitro fibroblasts and keratinocytes. Adv Skin Wound Care, 2005;18(7):373-8.
- Bennett L, Rosenblum R, Perlov C, Davidson J, Barton R, Nanney L. An in vivo comparison of topical agents on wound repair. Plast Reconstr Surg, 2001;108(3):675-68.
- Bajaj G, Karn N, Shrestha B, Kumar P, Singh M. A randomised controlled trial comparing eusol and sugar as dressing agents in the treatment of traumatic wounds. Tropical Doctor, 2009;39(1):1-3.
- Carneiro P, Nyawawa E. Topical phenytoin versus EUSOL in the treatment of non-malignant chronic leg ulcers. East Afr Med J, 2003;80(3):124-9.
- Okeniyi J, Olubanjo O, Ogunlesi T, Oyelami O. Comparison of healing of incised abscess wounds with honey and EUSOL dressing. JACM, 2005;11(3):511-3.
- Kumar A, Sinha VK. Comparative study of EUSOL and Silverstream in healing of pressure sore in traumatic spinal cord injury patients. Int J Orthop Sci 2018;4(1):228-234. DOI: 10.22271/ortho.2018.v4.i1d.33
- Chauhan A, Patel BK, Sharma PP, Mehta FS. A prospective, randomized, controlled study For efficacy of phenytoin sodium powder, Eusol solution, nanocrystalline silver gel in diabetic foot ulcer. International Journal of Contemporary Surgery, 2019;7(2):1-7.
- Jaber D, Younes N, Khalil E, Albsoul-Younes A, Mismar A, Nassar M, Al-Bakri A. Effect of diluted Dakin’s solution versus standard care on diabetic foot ulcer management: A randomized controlled trial. J Am Pod Med Assoc, 2022;112(1):1-11.
- Lewandowski L, Purcell R, Fleming M, Gordon WT. The Use of Dilute Dakin’s Solution for the Treatment of Angioinvasive Fungal Infection in the Combat Wounded: A Case Series. Military Medicine, 2013;178(4):e503-e7.
- Cornwell P, Arnold-Long M, Barss S, Varnado M. The use of Dakin’s solution in chronic wounds: a clinical perspective case series. J Wound Ostomy Continence Nurs, 2010;37(1):94-104.
- Duarte B, Cabete J, Formiga A, Neves J. Dakin’s solution: is there a place for it in the 21st century? Int Wound J, 2017;14(6):918-20.
- Aromataris E, Munn Z, editors. Joanna Briggs Institute Reviewer’s Manual. https://reviewersmanual.joannabriggs.org/, Joanna Briggs Institute; 2017.
- Joanna Briggs Institute Levels of Evidence and Grades of Recommendation Working Party. New JBI Grades of Recommendation. Adelaide: Joanna Briggs Institute; 2013.
- The Joanna Briggs Institute Levels of Evidence and Grades of Recommendation Working Party. Supporting Document for the Joanna Briggs Institute Levels of Evidence and Grades of Recommendation. www.joannabriggs.org: Joanna Briggs Institute; 2014.
- Salphale P, Shenoi S. Contact sensitivity to calcium hypochlorite. Contact Derm, 2003;48(3):162.
- Doughty D. A rational approach to the use of topical antiseptics. J Wound Ostomy Cont Nurs, 1994;21(6):224-31.
- Barrigah-Benissan K, Ory J, Dunyach-Remy C, Pouget C, Lavigne JP, Sotto A. Antibiofilm properties of antiseptic agents used on Pseudomonas aeruginosa isolated from diabetic foot ulcers. Int J Mol Si, 2022;23(19).
- Huang C, Tao S, Yuan J, Li X. Effect of sodium hypochlorite on biofilm of Klebsiella pneumoniae with different drug resistance. Am J Infect Control, 2022;50(8):922-8.
- Levine JM. Dakin’s Solution: Past, Present, and Future. Adv Skin Wound Care, 2013;26(9):410-4.
- Serena T, Serena L, Al-Jalodi O, Patel K, Breisinger K. The efficacy of sodium hypochlorite antiseptic: a double-blind, randomised controlled pilot study. J Wound Care, 2022;31(2):S32-S5.
- Georgiadis J, Nascimento VB, Donat C, Okereke I, Shoja MM. Dakin’s Solution: “One of the most important and far-reaching contributions to the armamentarium of the surgeons”. Burns, 2019;45(7):1509-17.
- Ueno CM, Mullens CL, Luh JH, Wooden WA. Historical review of Dakin’s solution applications. J Plast Reconstr Aesthet Surg, 2018;71(9):e49-e55.
- Shah A. Exposure - Eusol treatment for burn wounds. Burns Incl Therm Inj, 1985;11:297-300.
- Leaper D. Eusol: Still awaiting proper clinical trials. BMJ, 1992;304(6832):930.
- Catlin L. The use of hypochlorite solutions in wound management. BJN, 1992;1(5):226-9.
- Duarte B, Formiga A, Neves J. Dakin’s solution in the treatment of severe diabetic foot infections. Int Wound J, 2020;17:277-84.
- Farrow S, Toth B. The place of Eusol in wound management. Nurs Stand, 1991;5(22):25-7.
- Eftekharizadeh F, Dehnavieh R, Noori Hekmat S, Mehrolhassani MH. Health technology assessment on super oxidized water for treatment of chronic wounds. Med J Islam Repub Iran, 2016;30:384.
- Haesler E. Evidence Summary: Super-oxidised solutions for chronic wounds. Wound Practice and Research, 2020;28(3):145-7.
- Benskin LL. A review of the literature informing affordable, available wound management choices for rural areas of tropical developing countries. Ostomy Wound Manage, 2013. Oct;59(10):20-41.
- Ottesen TD, Qudsi RA, Kahanu AK, Baptiste BJ, Woolley PM, Socci AR, Dyer GSM. The Continued Utility and Viability of Dakin’s Solution in Both High- and Low-resource Settings. Arch Bone Jt Surg, 2020. Mar;8(2):198-203.
- International Wound Infection Institute (IWII). Wound Infection in Clinical Practice. Wounds International; 2022.



