Ahead of Print
The effects of a combined occupational therapy and nursing preventative approach to reduce hospital-acquired pressure injuries in an acute inpatient hospital setting: a case control study
Rachel Lommerzheim, Emily Miller, Melissa Wildman, Sascha Holbrook, Colleen O’Brien-Malone, Courtenay Harris, Kristie Harper
Keywords Hospitals; occupational therapy; pressure care; sitting position; wound healing
For referencing Lommerzheim R et al. The effects of a combined occupational therapy and nursing preventative approach to reduce hospital-acquired pressure injuries in an acute inpatient hospital setting: a case control study. Wound Practice and Research 2024; 32(1):to be assigned.
DOI
10.33235/wpr.32.1.to be assigned
Submitted 7 December 2023
Accepted 12 January 2024
Abstract
Aim Hospital-acquired pressure injuries (HAPI) are preventable yet continue to occur. This study aimed to reduce HAPI by implementing a combined occupational therapy and nursing preventive approach to pressure care management, utilising pressure redistribution cushions and enhanced patient education.
Methods A case-control design whereby inpatients in an acute hospital setting were provided with the pressure care intervention. The control group received usual care and were retrospectively audited. Outcome measures included incidence, location, and stage of pressure injuries, Waterlow Risk Assessment (WRA) scores and hospital length of stay. Nursing staff were surveyed regarding the acceptability of the intervention and implementation barriers.
Results A total of 314 patients were recruited, with 23 pressure injuries identified (control group n=13/147 vs. intervention group n=10/167, p=0.122). In the control group, 62% (n=8) of pressure injuries were hospital-acquired, compared to 10% (n=1) in the intervention group (p=0.007). One hundred percent of nursing staff that completed the survey (n=7) agreed that the intervention was acceptable. However, gaps in implementation were noted with 45% of patients initially receiving education and 38% a pressure redistribution cushion.
Conclusions The pressure care intervention significantly reduced rates of HAPI; however, barriers exist to consistently implementing these interventions which require consideration and management.
Introduction
Pressure injuries continue to be an adverse health event globally, affecting both hospital and community populations.1,2 Despite being largely preventable their frequency remains high.2,3 In 2020 the global pooled rate of hospital acquired pressure injuries (HAPI) was estimated to be 8.5%,4 emphasising the scale of the problem. In Australian public hospitals in 2020, the total estimated cost associated with pressure injuries was A$9.11 billion with the cost attributed to HAPI accounting for A$5.50 billion per annum.1 Furthermore, pressure injuries are life threatening and associated with negative health outcomes, including increased risk of infection, protracted hospitalisation, pain, disability, and poorer quality of life.5-8
Pressure injuries are defined as localised damage to the skin and/or underlying tissues due to a combination of factors, including pressure, friction, and shearing forces, usually associated with bony prominences.3 Hospitalised patients generally experience risk factors associated with pressure injuries, such as illness, reduced mobility, increased age, poor skin integrity and incontinence, emphasising the need for pressure care interventions.9,10 Pressure injuries are categorised according to the severity of damage, ranging from non-blanchable erythema where the skin remains intact (Stage I) to full thickness loss of tissue where underlying structures are visible (Stage IV).3 HAPI, particularly those in their early stages, are largely avoidable.3 However, in 2020 a systematic review and meta-analysis found that globally, 43.5% of HAPI were categorised as Stage I and 28% were categorised as Stage II,4 indicating that current efforts to prevent HAPI are not satisfactory.
There is a strong emphasis on patients in hospital settings sitting out of bed to reduce functional decline and deconditioning.11,12 This increases the risk of HAPI development as greater pressure is exerted through weight bearing structures when a person is seated.3,11 McCarthy et al13 found that older adults at greatest risk of developing HAPI were those sitting out for continuous periods of two hours or more. The risk of developing a pressure injury can be reduced through measures such as repositioning and patient education and through the use of pressure redistribution cushions as these envelop vulnerable structures and ensure a greater distribution of load.3,14,15 In their observational study, Barker et al16 implemented an evidence-based pressure injury prevention program comprised of risk assessment, use of pressure redistribution devices and enhanced staff education that demonstrated a reduction in HAPI from 12.6% in 2003 to 2.6% in 2011. An Australian hospital reported a 34% reduction in HAPI when all patients were provided with a pressure redistribution cushion in conjunction with enhanced patient and staff education.17 Despite this, the effectiveness of pressure redistribution cushions reducing the incidence of pressure injuries continues to be contested with comparable studies demonstrating inconclusive results.15,18,19
Across 2019 and 2020 a local pilot project was completed which aimed to reduce HAPI by improving pressure care seating and enhancing patient education.20 This project demonstrated initial success with 106 patients recruited over three months. Recruitment was ceased due to COVID‑19 preparations; however, the pilot results delivered a 35% reduction in HAPI in the intervention group. Patients were surveyed and reported significantly greater comfort, reduced pain and sat out of bed more often. This study aimed to build upon the previous pilot project, with replication of the pressure care intervention with a larger sample and consideration of implementation factors, such as staff adherence and interdisciplinary collaboration, that would support future wider scale roll out. As such, the primary objective was to determine if a preventative approach to managing pressure injuries, using pressure redistribution cushions, and providing enhanced staff and patient education, resulted in reduced rates of HAPI. The secondary objective was to explore adherence to the pressure management intervention protocol and staff acceptability, supporting future implementation.
Methods
This study employed an experimental case-control design to determine the effectiveness of a preventative approach to reducing HAPI. Reporting adhered to the STROBE statement for observational studies.21
Setting and sample
This study was completed at a metropolitan acute tertiary hospital on one 30-bed ward consisting of renal, gastroenterology and hepatology inpatients with the intervention phase running for 12 weeks (May to July 2021). The study location was recommended by the hospital’s wound management team and clinical nurse manager and was chosen due to the incidence of HAPI and a patient cohort that were at greater risk of developing HAPI. All patients admitted to the ward were eligible for inclusion. Patients were excluded if they were unable to sit out of bed due, for example, to their medical status, or if they were receiving end of life care. Participants in the control group were randomly selected through a retrospective audit of ward admissions between May and July 2020. A sample of 300 patients (n=150 per group) would have 80% power to detect a decrease in HAPI rates from 10% to 3% between the two independent groups using a critical α=0.05 and a one-sided test. (G*Power 3.1.9.6)
Intervention group and HAPI prevention strategies
The intervention was developed and piloted and is detailed in a previous published study.20 Each patient received a pressure redistribution cushion and enhanced pressure care education. Upon admission each patient was assessed to determine their level of pressure injury risk using the Waterlow Risk Assessment Scale (WRA).22 WRA scores were categorised into three risk levels for the purposes of this study: low risk (<10), at risk (10–14) or high risk (>14). The outcomes of the WRA determined which pressure redistribution cushion each patient received and whether a referral to occupational therapy was indicated. Ward nursing staff completed the WRA, provided the pressure redistribution cushion and pressure care education, and organised referrals to occupational therapy if required. Seating style was consistent with all pressure redistribution cushions placed on hospital high back chairs. If a patient required more supportive seating, for example a recliner chair or specialised wheelchair, they were referred to the occupational therapist for seating assessment and set-up.
Patients who were deemed to be at low-risk of developing a HAPI (WRA<10) were issued with the Zenith Hosplex cushion: a flat, low-risk cushion with rudimentary pressure redistribution properties. This cushion was chosen as it had been utilised in a previous Australian based study17 and had demonstrated good effect.20 Those patients considered to be at risk of developing HAPI, (WRA 10–14), were provided with the Dynatek Owl cushion: a commercially available contoured foam pressure redistribution cushion. The Dynatek Owl cushion was also issued to patients who were assessed to have a Stage I or Stage II pressure injury in conjunction with a referral made to the occupational therapist for further assessment. Patients deemed to be at high risk of developing a pressure injury (WRA 15+) were also provided with the Dynatek Owl cushion and referred to occupational therapy. Patients who were assessed to have a Stage III or Stage IV pressure injury were directly referred to occupational therapy for the purpose of identifying and providing complex interventions. This was also required for suspected deep tissue injuries and unstageable pressure injuries. If a patient was admitted after hours or on the weekend and needed to sit out of bed, prior to being seen by the occupational therapist, they were provided with a Jay Fusion pressure redistribution cushion, which contains foam and has gel properties.
Upon admission patients in the case group received a comprehensive 20-page pressure injury prevention education booklet, in addition to usual care and were regularly encouraged to refer to it by nursing and occupational therapy staff. The booklet could be easily accessed by patients for the duration of their hospital stay. Pressure injury prevention strategies within the booklet included promotion of frequent movement, reducing their time spent in bed and pressure offloading strategies. The importance of nutrition and skin care was also highlighted.
Staff training
Ward nursing staff were invited to attend education sessions prior to the intervention period commencing, focusing on HAPI development, prevention strategies, provision of patient education, the WRA, and use of pressure redistribution cushions. Education also focused on set up of seating, including how to adjust chair heights according to patient measurements to increase patient comfort, and increase safety by reducing the risk of friction, shear, sliding in the chair and falls. The intervention pathway was emphasised using a visual flow chart.20 To provide consistent education across staff, the session was run twice to reach as many nursing staff as possible. To target staff who were unable to attend either of the two education sessions the same education information was made available to staff by sharing the session content with the nurse manager and clinical nurse educator, providing individual training where requested, placing education posters in the staffroom, and disseminating information via staff email.
Control group
Patients in the control group received standard care as per current hospital pressure injury prevention guidelines. This included recording patients’ WRA scores upon admission and repeatedly throughout their hospital stay and having a skin inspection within eight hours of admission. Patients could be referred to occupational therapy if they required a pressure redistribution cushion, however, they did not have standard access to pressure redistribution cushions. Additionally, a brief pamphlet outlining strategies to prevent pressure injuries was provided to all patients as per hospital guidelines. This pamphlet was less comprehensive than the booklet provided to the intervention group.
Outcome variables and data sources
A data collection sheet was developed, piloted and used to capture patient information daily for the case group. Data were collected from patient records and included patient demographics, presenting diagnosis and comorbidities, level of mobility (as per WRA), and hospital length of stay (LOS). The WRA22 was completed daily by nursing staff to identify pressure injury risk factors. WRA scores reported in this study were a patients’ first score recorded upon admission, acting as a determinant of their risk of developing a pressure injury during their hospital stay. Nurses carried out daily visual skin checks to record pressure injury risk factors, and if applicable, number of HAPI and pressure injury stages. The same data collection sheet was used to extract data for the control group via a medical records audit.
This study employed a combined approach to the provision of pressure injury prevention interventions by nursing and occupational therapy staff. As nursing staff were involved with all participants they provided initial education, selected the pressure redistribution cushion and set them up as appropriate. There was one occupational therapist working on the ward who was able to see patients with complex seating needs. Staff adherence to the pressure management intervention protocol was measured by review of six points. They were: was patient pressure care education provided (yes/no); was a pressure redistribution cushion provided (yes/no); which discipline provided the cushion (occupational therapy/nursing); was the most appropriate cushion selected as per protocol (yes/no); was cushion set up appropriately on the chair (yes/no); and were additional referrals completed if required (yes/no). Daily reviews were carried out by the research assistant to monitor and record adherence. If the intervention components were not completed, the research assistant completed these to ensure intervention fidelity.
Nursing staff were also invited to complete an anonymous survey at the end of participant recruitment to review acceptability of the intervention. The survey had seven questions and included a mix of questions using a Likert scale, ‘yes/no’ questions, and opportunities for free text responses. The survey items included attendance of the information session, knowledge gained from the information session, level of confidence in providing pressure injury education, ease of implementation of the cushion provision process, and staff-perceived benefits of pressure redistribution cushions for patients. The survey was accessible to staff via the nurse manager, in the staff tearoom, and via email.
Statistical analysis
Descriptive data including WRA score, hospital LOS and patient age were reported as a mean score, with standard deviation, or median and range, depending on the nature and distribution of the data. Categorical data such as gender, pressure injury stage, and intervention adherence were reported using frequencies and percentages. To compare continuous data between the control and intervention groups, independent t-tests were used, or Wilcoxon tests when the data was not normally distributed. The 95% confidence intervals (CI) were reported as appropriate. Chi-square tests or Fisher’s exact tests were used to compare categorical data. Statistical analysis was conducted using IBM SPSS version 24.0 and p values of <0.05 were considered statistically significant.
Ethical considerations
Ethical approval was granted by Curtin University (HRE2022-0071) and by the Sir Charles Gairdner Osborne Park Health Care Group (QA40305). All patient data was de-identified and analysed in aggregate form to protect participants’ privacy and maintain confidentiality.
Results
Enrolment and baseline characteristics
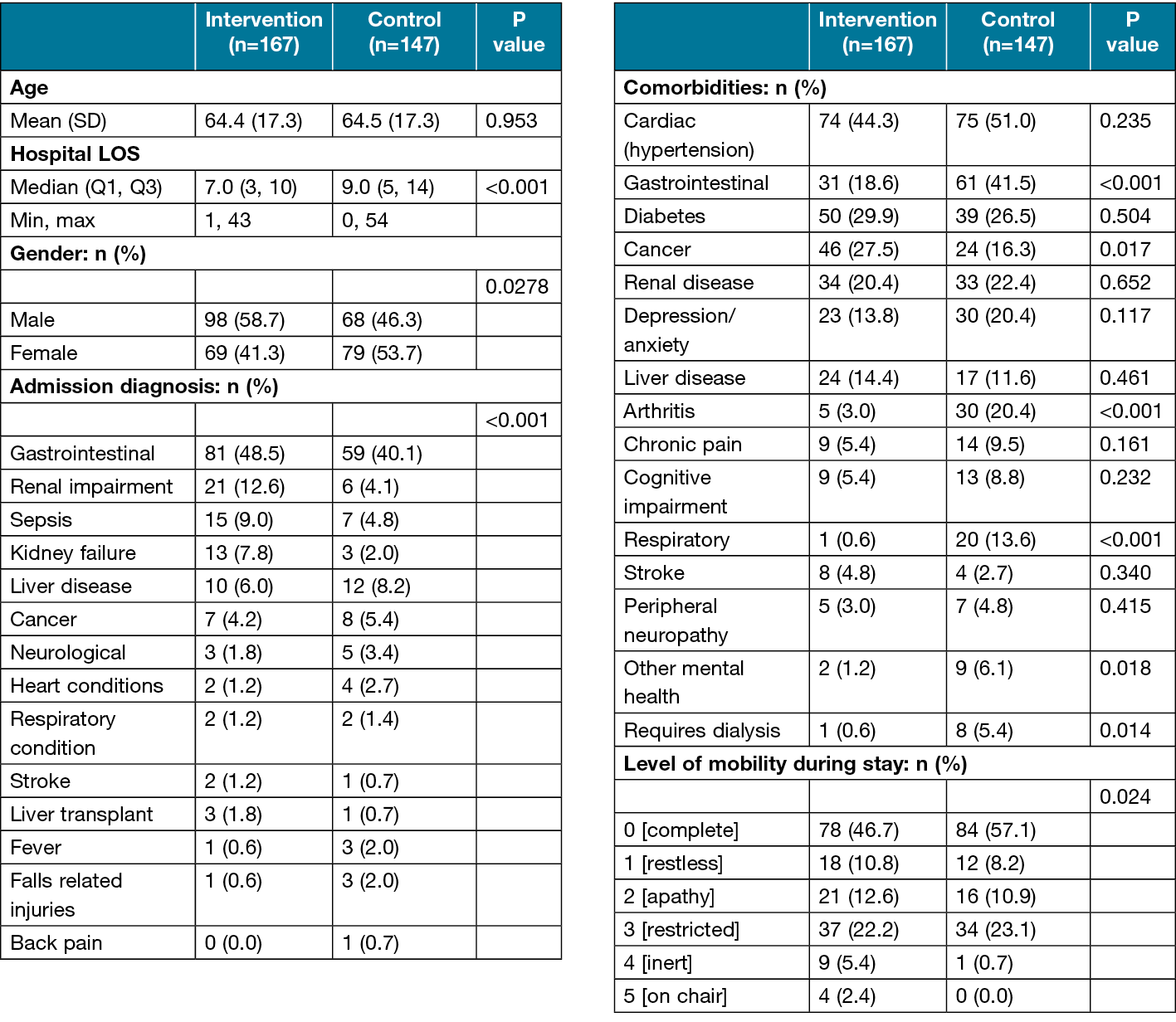
A total of 314 patients were recruited with 167 patients in the intervention group and 147 in the control group. Gastrointestinal complaints accounted for the most common admission diagnosis across both groups (n=140, 45%) followed by renal impairment (n=27, 9%) (Table 1). Comorbidities common to both groups included cardiac disease, arthritis, renal and liver disease, cancer, diabetes, depression, and gastrointestinal issues. The level of mobility between the two groups differed significantly (p=0.023), with 47% (n=78) independently mobile in the intervention group compared to 57% (n=84) in the control group.
Table 1. Patient demographic and medical information
Pressure injuries and risk
A total of 23 (7%) pressure injuries were identified during the study period (Table 2) with 10 (6.0%, 95% CI 0.01, 0.10) in the intervention group and 13 (8.8%, 95% CI 0.04, 0.13) in the control group (p=0.122). Ten percent (95% CI 0.02, 0.40) of pressure injuries in the intervention group were HAPI (n=1) compared to 62% (95% CI 0.34, 0.89) in the control group (n=8), (p=0.007). In the intervention group, one unstageable HAPI was located on the sacrum. In the control group, three Stage I sacral HAPI were identified. Four Stage II HAPI were identified and located as per: sacrum (n=3), perineum (n=1) Additionally, one patient developed a Stage II HAPI at the sacrum and right groin. The most common pressure injury areas associated with HAPI included the sacral and perineal areas, both of which need to be considered for patient seating.
Table 2. Waterlow risk assessment, pressure injuries, pressure cushions supplied per group
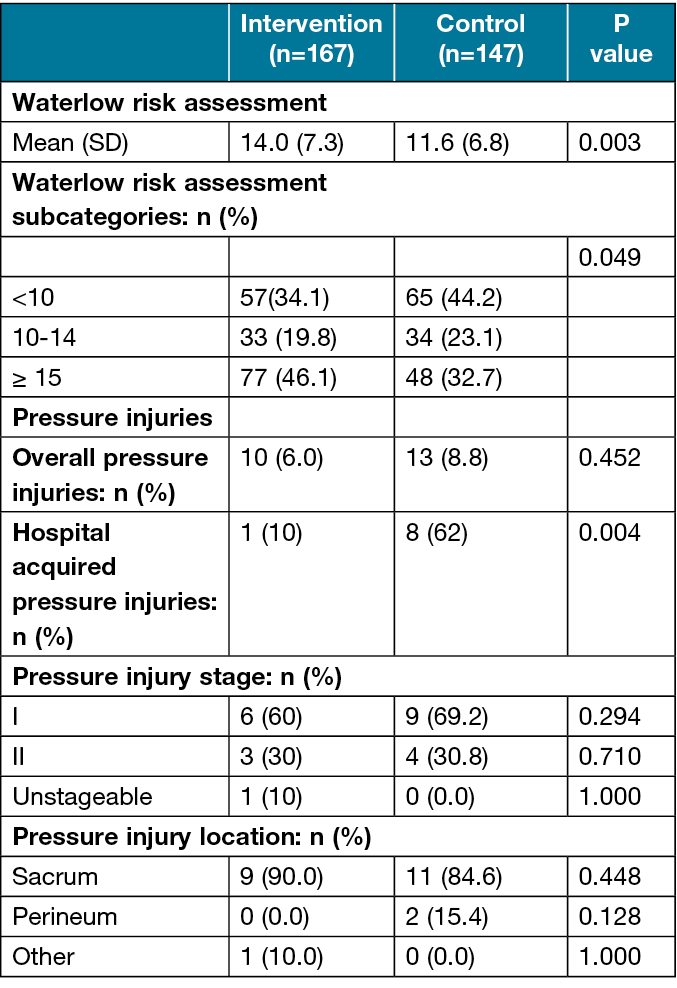
The mean (SD) WRA score on admission was significantly higher in the intervention group at 14.0 (7.3) compared to 11.6 (6.8) in the control group (p=0.003) (Table 2). Both groups sat in the ‘at risk’ (WRA 10–14) category. The number of participants in each WRA sub-category differed significantly (p= 0.0493) between the control and intervention groups, however patients in the intervention group had more patients at ‘high risk’ with 46% (n=77) scoring ≥15 compared to 33% (n=48) in the control group (Table 2).
Overall patients in the control group had a longer hospital LOS (9 versus 7 days, 95% CI -5.31, -1.51, p=<0.001, Table 1). However, for patients who developed a HAPI this difference became more evident. The LOS for the patients who developed HAPI in the intervention group (n=1) was 10 days, compared to a mean of 26 days (SD 14.1) in the control group (n=8). Combining the two groups and comparing those who developed and did not develop a pressure injury also highlighted the impact of pressure injuries on LOS, with the median LOS for those who had a pressure injury being 25 days with an interquartile range (IQR) of 27, compared to those who did not have a pressure injury, at seven days (IQR=7, 95% CI 3.3, 22.6, p=<0.001).
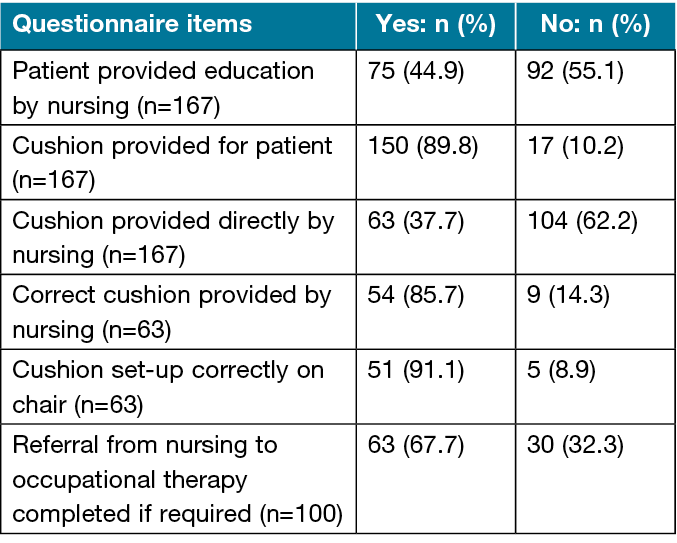
Nursing staff questionnaire and adherence with implementation of the intervention
Staff adherence to the intervention protocol identified that initial pressure care education was provided to 45% (n=75) of the participants, with 90% (n=150) given a pressure redistribution cushion (42% [n=63] by nursing staff and 58% [n=87] by the occupational therapist) (Table 3). Of the 63 cushions provided by nursing staff, 86% (n=54) were selected correctly, as per the intervention flow chart.20 Over 90% of cushions provided by nursing were set up correctly.
Fifteen ward nursing staff were invited to provide feedback through a survey with seven providing feedback, resulting in a response rate of 47%. One hundred percent of staff reported that the procedure of issuing a pressure redistribution cushion was easy to follow, and that all patients benefitted from the intervention, indicating high levels of acceptability. Concerns raised by nursing staff included remembering to implement the intervention with ongoing busy workloads and remembering to adjust the seating height for patients to maximise pressure care management.
Table 3. Staffing adherence to the intervention protocol
Discussion
The aim of this study was to determine if a HAPI preventive approach, consisting of individually prescribed pressure redistribution cushions and enhanced patient education, was effective in reducing rates of HAPI in an acute hospital setting. This study built on previous work by Holbrook et al20 and found a significant reduction in HAPI in the case group. This study found that 100% of HAPI developed in the control group were Stage I and Stage II, with previous literature emphasising that these stages of HAPI are the most commonly occurring and largely preventable when appropriate pressure care interventions are implemented.1,3,4 HAPI in the control group were primarily located on the sacral area (87.5%) and perineal area (12.5%); two body locations at greater risk of developing a pressure injury when a person is seated.3,14,15 In the intervention group one person developed an unstageable HAPI on their sacrum. They were a 65-year-old male admitted to hospital for sepsis with numerous comorbidities, including cardiac and renal disease. They required assistance with mobility and had a WRA of 15 on admission, indicating they were at high risk of developing a pressure injury.
These results are in keeping with previous literature in the area. Barker et al16 identified a reduction in pressure injury prevalence over a six year period from 12.6% to 2.6% following the implementation of a pressure injury prevention program, which included the use of pressure redistribution devices. A hospital in Victoria, Australia, demonstrated a 34% reduction in pressure injuries six months after commencing a program whereby each patient was provided with a pressure redistribution seat cushion.17 Additionally, standard provision of pressure redistribution cushions led to a reduction in severity of HAPI across the hospital.17
The importance of patients’ sitting out of bed in the acute hospital setting is well documented. Hirsch23 and Graf24 identified that functional decline can start within two days of hospitalisation and subsequently impacts a patients’ level of independence and ability to complete daily activities.25 Lying or sitting in bed for long periods of time or sitting in inappropriate seating can also increase a patient’s risk of developing a HAPI.3 McCarthy et al13 found that over an 8.5-hour audit period in a post-acute setting, participants sat out of bed, on average, for 3.8 hours, and a sustained period of one hour and five minutes. In the previous study completed by Holbrook et al20 patients sat out of bed on average 2.2 times during the day in an acute, inpatient hospital setting. Pressure care interventions, also considering seating as reviewed in this study, are therefore important to reduce HAPI while supporting patient functional maintenance in hospital.
This study explored staff implementation of the intervention protocol and acceptability. Gaps in implementation were noted, with less than half of the patients routinely provided with pressure care education and nursing staff provided cushions to 38% of eligible participants. The research assistant supporting the study was responsible for ensuring intervention fidelity and provided pressure redistribution cushions and patient education when this was missed. Nursing staff who provided feedback indicated that barriers to providing the required interventions included remembering to consistently implement the intervention and adjust the height of participants’ seating. Initial training was provided for all staff, ward signage was in place, and a two-week introduction phase was used. Pressure redistribution cushions were stored in a cupboard on the ward that was easily accessible, but not highly visible and this may have impacted on the rate of pressure cushion provision. Implementation data was collected to better understand any barriers to wider scale future use of the intervention. These findings require review and consideration in future use of the intervention protocol. Additional staff training or reminders throughout the project may have increased adherence rates.
All staff surveyed found the intervention acceptable and beneficial for patient care. This is in keeping with previous research in this area. Barakat-Johnson et al26 interviewed 20 clinical nurses working in inpatient settings in Australia to explore their experiences in delivering pressure injury prevention interventions. The main barriers highlighted included the numerous steps involved in pressure injury prevention interventions and how this increased nurses’ workloads, as well as competing demands and time constraints. It was also noted that enablers to providing pressure injury prevention interventions included consistent opportunities for education and the importance of engaging patients and their family members to increase uptake of interventions.26
Pressure injury management and treatment is estimated to cost Australian hospitals A$9.1 billion annually with expected future escalations.1,4 The financial cost of HAPI management and treatment is significantly higher than that of providing patient education and pressure redistribution cushions.1 This study demonstrated that those patients who had a pressure injury had a median LOS of 25 days, compared to seven days for patients who did not have a pressure injury. This finding is in keeping with the literature which estimates that patients who develop a pressure injury are in hospital on average for 23.9 days longer than those who do not.27 The estimated average cost of an acute hospital bed in Australia is A$2047 per night, which further emphasises the burden pressure injuries place on the healthcare system.28 In this study only one patient in the intervention group developed a HAPI compared to eight in the control group, indicating that approximately seven HAPI were prevented. The potential cost saving is significant at A$34,799 per patient (A$243,593 total) if the difference in hospital LOS between the two groups (17 days) is compared.28
During the study period, nine patients in the intervention group and seven in the control group were admitted to hospital with a pre-existing pressure injury, further highlighting the need for patient education to prevent pressure injuries occurring in the first instance, and interventions to support wound healing in the hospital environment (Table 2). Multiple factors contribute to wound healing and ensuring the interface pressure on a seat surface is reduced, increases the likelihood that pressure injury healing will occur.18,29
Limitations
A number of limitations were identified with data collected from a single hospital ward affecting the ability to generalise findings. Multiple nursing staff and clinicians were involved in providing the intervention which had the potential to impact intervention fidelity. Attempts were made to address this through initial group and individual staff training and daily checks by the trained research assistant who provided the intervention if required.
Given that the control data was retrospective, data collection relied on accurate documentation and interpretation of medical records. A piloted data collection tool was used to limit bias and support consistent data extraction. To ensure inter-rater reliability with data extraction, the three staff involved in extracting data completed two group checks.
There were uneven groups, with 147 in the control group, slightly under the sample size calculation of 150 per arm. Additionally, a case-control design was utilised which establishes correlation but cannot establish causation. Future studies could consider utilising a prospective randomised control trial to address baseline difference identified and sample size limitations. Data pertaining to length of time sitting out of bed was also not captured in this study and, therefore, it is not known how long the patient spent sitting out of bed. This study could be enhanced in the future by measuring time spent sitting out of bed, either through activity monitors or observation.
Conclusions
This study has demonstrated a significant reduction in HAPI in an acute hospital setting through the provision of pressure redistribution cushions and enhanced education for all patients. Consideration of the routine use of the HAPI prevention strategies outlined is required with clear strategies to support implementation and sustainability.
Acknowledgements
Thank you to the ward nursing staff who supported with implementing the pressure care intervention. Thank you to ward occupational therapists, Hannah Flynne and Eimear Fitzmaurice, who supported with implementation of the intervention and data collection.
Author contribution
Authors 4,5 and 7 conceived the study and secured grant funding. Authors 2,3,4,5,6 and 7 were involved in protocol development and gaining ethical approval. Authors 2,3 and 4 supported the data collection. Authors 1,2,3,6 and 7 completed the data analysis. Authors 1,2,3 and 7 wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Conflict of interest
The authors declare no conflicts of interest.
Ethics statement
Ethical approval was granted by Curtin University (HRE2022-0071) and by the Sir Charles Gairdner Osborne Park Health Care Group (QA40305). All patient data was de-identified and analysed in aggregate form to protect participants’ privacy and maintain confidentiality.
Funding
Thank you to Charlies Foundation for Research for funding this research.
Author(s)
Rachel Lommerzheim1, Emily Miller2, Melissa Wildman3, Sascha Holbrook4,
Colleen O’Brien-Malone5, Courtenay Harris6, Kristie Harper7*
1Global Public Health and Policy, Occupational Therapy Department, Sir Charles Gairdner Hospital, Perth, Australia
2Curtin University, School of Allied Health, Perth, Australia
3Curtin University, School of Allied Health, Perth Australia
4Occupational Therapy Department, Sir Charles Gairdner Hospital, Perth, Australia
5Occupational Therapy Department, Sir Charles Gairdner Hospital, Perth, Australia
6Curtin University, School of Allied Health, Perth, Australia
7Occupational Therapy Department, Sir Charles Gairdner Hospital, Perth, Australia, Curtin University, School of Allied Health, Perth, Australia, Enable Institute, Curtin University, Perth, Australia
*Corresponding author email kristie.harper@health.wa.gov.au
References
- Nghiem S, Campbell J, Walker RM, Byrnes J, Chaboyer W. Pressure injuries in Australian public hospitals: A cost of illness study. Int J Nurs Stud. 2022;130:104191.
- Australian Commission on Safety and Quality in Health Care (ACSQHC). Preventing Pressure Injuries and Wound Management [Internet]. Sydney (NSW): ACSQHC; 2020. Available from: https://www.safetyandquality.gov.au/sites/default/files/2020-10/fact_sheet_-_preventing_pressure_injuries_and_wound_management_oct_2020.pdf
- European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan Pacific Pressure Injury Alliance (EPUAP/NPIAP/PPPIA). Prevention and treatment of pressure injuries/ulcers: clinical practice guideline. The international guidelines. E Haesler, editor EPUAP/NPIAP/PPPIA: 2019.
- Li Z, Lin F, Thalib L, Chaboyer W. Global prevalence and incidence of pressure injuries in hospitalised adult patients: A systematic review and meta-analysis. Int J Nurs Stud. 2020;105:103546.
- Ahn H, Stechmiller J, Fillingim R, Lyon D, Garvan C. Bodily pain intensity in nursing home residents with pressure ulcers: Analysis of national minimum data set 3.0. Res Nurs Health. 2015;38:207–212.
- Gorecki C, Nixon J, Maddill A, Firth J, Brown JM. What influences the impact of pressure ulcers of health-related quality of life? A qualitative patient-focused exploration of contributory factors. J Tissue Viability. 2012;21:3–12.
- Cherry C, Moss J. Best practices for preventing hospital-acquired pressure injuries in surgical patients. Can Oper Room Nurs J. 2011;29(1):6–26.
- Jackson DE, Durrant LA, Hutchison M, Ballard CA, Neville S, Usher K. Living with multiple losses: Insights from patients living with pressure injury. Collegian. 2018;25(4):409–14.
- Coleman S, Gorecki C, Nelson EA. Patient risk factors for pressure ulcer development: Systematic review. Int J Nurs Stud. 2013;50(7):974–1003.
- Chung M-L, Widdel M, Kirchhoff J. Risk factors for pressure injuries in adult patients: A narrative synthesis. Int J Environ Res Public Health 2022;19(2):761.
- Surkan MJ, Gibson W. Interventions to mobilize elderly patients and reduce length of hospital stay. Can J Cardiol. 2018;34(7):881–8.
- de Foubert M, Cummings H, McCullagh R, Brueton, V, Naughton C. Systematic review of interventions targeting fundamental care to reduce hospital-associated decline in older patients. J Adv Nurs. 2021;77(12):4661–78.
- McCarthy A, Robertson V, Roberts K, Lannin NA. Audit of sitting time in older inpatients and implications for pressure-injury management. Phys Occup Ther Geriatr. 2019;37(3):183–95.
- Meaume S, Marty M, Colin D. Prospective observational study of single or multi-compartment pressure ulcer prevention cushions: PRESCAROH project. J Wound Care. 2017;26(9):537–44.
- Chou R, Dana T, Bougatsos C, Blazina I, Starmer AJ, Reitel K, Buckley DI. Pressure ulcer risk assessment and prevention: A systematic comparative effectiveness review. Ann Intern Med. 2013;159(1):28–38.
- Barker AL, Kamar J, Tyndall TJ, White L, Hutchinson A, Klopfer N, Weller C. Implementation of pressure ulcer prevention best practice recommendations in acute care: An observational study. Int Wound J. 2013;10(3):313–20.
- Victoria State Government. Pressure care case study – St Vincent’s Hospital Melbourne [Internet]. Melbourne (VIC): Victoria State Government Department of Health; 2015. Available from: https://www.health.vic.gov.au/patient-care/pressure-care-case-study-st-vincents-hospital-melbourne
- Brienza DM, Karg PE, Geyer MJ, Kelsey S, Trefler E. The relationship between pressure ulcer incidence and buttock-seat cushion interface pressure in at-risk elderly wheelchair users. Arch Phys Med Rehabil. 2001;82(4):529–33.
- Mervis JS, Phillips TJ. Pressure ulcers: Prevention and management. J Am Acad Dermatol. 2019;81(4):893–902.
- Holbrook S, O’Brien-Malone C, Sascha H, Colleen O, Barton A, Harper K. A quality improvement initiative to reduce hospital-acquired pressure injuries (HAPI) in an acute inpatient setting by improving patient education and seating. Wound Practice and Research. 2021;29(4):198–205.
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9.
- Waterlow J. Pressure sores: A risk assessment card. Nurs Times. 1985;81(48):49–55.
- Hirsch CH, Sommers L, Olsen A, Mullen L, Winograd CH. The natural history of functional morbidity in hospitalized older patients. J Am Geriatr Soc.1990;38(12):1296–303.
- Graf C. Functional decline in hospitalized older adults. Am J Nurs. 2006;106(1):58–67.
- Hoogerduijn JG, Schuurmans MJ, Duijnstee MS, de Rooij SE, Grypdonck MF. A systematic review of predictors and screening instruments to identify older hospitalized patients at risk for functional decline. J Clin Nurs. 2007;16(1):46–57.
- Barakat-Johnson M, Lai M, Wand T, White K. A qualitative study of the thoughts and experiences of hospital nurses providing pressure injury prevention and management. Collegian. 2019;26(1):95–102.
- Independent Health and Aged Care Pricing Authority (IHACPA). Activity Based Funding Admitted Patient Care 2015-2016, acute admitted episodes, excluding same day [Internet]. Sydney (NSW): IHACPA;2015-2016. Available from: https://www.ihacpa.gov.au/health-care/costing/national-hospital-cost-data-collection/national-hospital-cost-data-collection-public-sector
- Independent Health and Aged Care Pricing Authority (IHACPA). National Hospital Cost Data Collection 2015-16. acute admitted episodes, excluding same day [Internet]. Sydney (NSW): IHACPA; 2015-2016. Available from: https://www.ihacpa.gov.au/health-care/costing/national-hospital-cost-data-collection/national-hospital-cost-data-collection-public-sector
- Sprigle S, Sonenblum S. Assessing evidence supporting redistribution of pressure for pressure ulcer prevention: A review. J Rehabil Res Dev. 2011;48(3):203–13.


