Ahead of Print
Assessment, management and prevention of acute wounds in the Australian context: a scoping review
Kathleen Finlayson, Ut T Bui, Fiona Wood, Fiona Coyer, Kylie Sandy-Hodgetts
Keywords skin tears, burns, acute wounds, traumatic wounds, surgical wounds
For referencing Finlayson K et al. Assessment, management and prevention of acute wounds in the Australian context: a scoping review. Wound Practice and Research 2024; 32(1):to be assigned.
DOI
10.33235/wpr.32.1.to be assigned
Submitted 16 August 2023
Accepted 25 October 2023
Abstract
Aim To undertake a scoping review of research on the assessment, management and prevention of acute wounds, from both primary research studies in Australia and from worldwide synthesised evidence, in order to provide a global context of future research needs.
Methods Databases, trial registries and professional organisation websites were searched from January 2010 to April 2022 inclusive. All Australian research studies, in addition to worldwide reviews and guidelines, were included. Articles were reviewed by two independent researchers and conflicts were resolved by a third researcher. Results were synthesised in a narrative review.
Results The searches yielded 318 Australian studies and 833 international studies, the latter comprising of 680 systematic reviews (SRs), 28 evidence-based guidelines (EBGs), 79 evidence summaries and 46 consensus documents. The Australian research studies consisted mostly of cohort studies, focused on burns (46%) and surgical wounds (44%), with fewer studies on skin tears and other acute wound types. Australian studies were primarily investigating wound management or treatments (60%), with only 38% on assessment and 2% on the prevention of wounds.
Conclusions This review found research on acute wounds focused on surgical wounds and burns, with gaps in research on skin tears or traumatic wounds, wound prevention, and research in primary healthcare settings, despite the high prevalence of wounds cared for in these settings.
Introduction
Acute wounds such as surgical wounds, burns, traumatic wounds and skin tears constitute the wound types most frequently encountered by health professionals1,2. Prevalence surveys have reported the majority of wounds in hospital and outpatient community settings were acute/surgical wounds (76% and 35% in each setting respectively)1, and 56% of wounds cared for in an Australian community nursing service were acute wounds or skin tears2. Their management consumes significant healthcare resources, estimated as 1.6–2.4% of total health service costs1, with a reported cost of A$390,641 to treat a sample of 1053 acute wounds in a recent Australian study3. An acute wound can be defined as “a recent wound, of any aetiology” that is expected to progress “through the normal sequential to achieve healing”4(p.2). Definitions of acute wound types are provided in Box 15-10. However, despite their frequency of occurrence, inconsistency in management is frequently reported11,12.
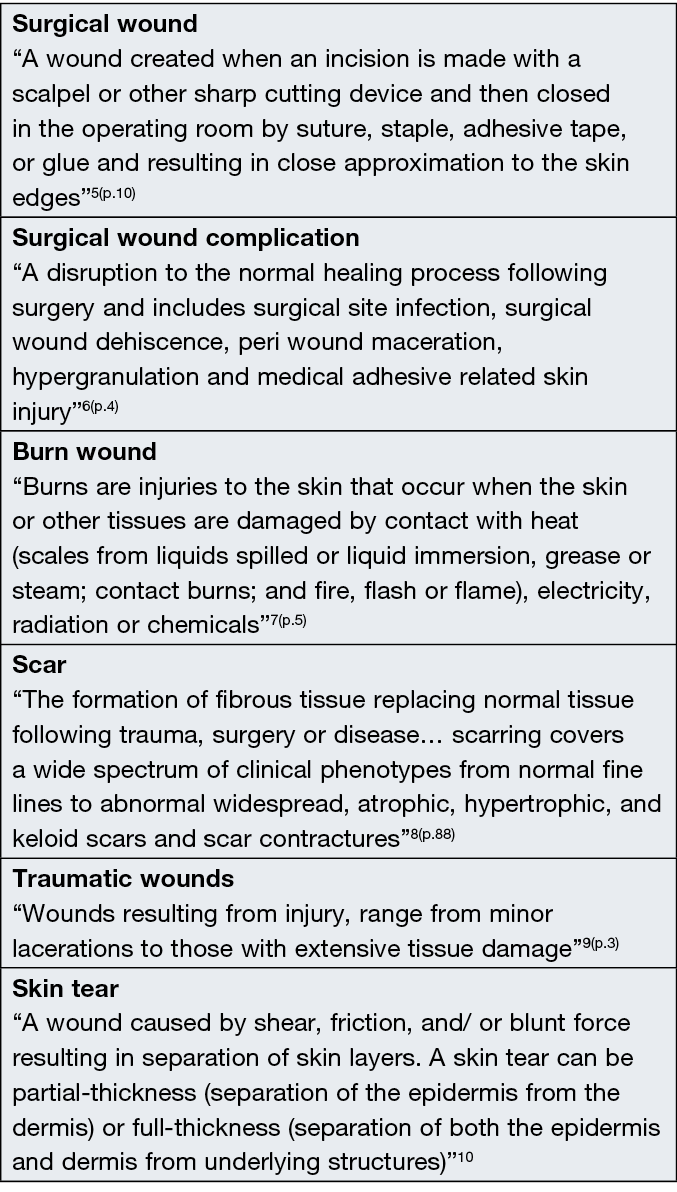
Box 1. Definitions of acute wound types
The implementation of research evidence into clinical practice has been shown to deliver safe, cost-effective wound care and improved patient outcomes13,14. Considering the high burden of acute wounds on individuals and healthcare systems outlined above, it is essential to review available research findings to provide the means to optimise care delivery and facilitate more efficient and cost-effective ultilisation of healthcare resources. The Australian Health Research Alliance Wound Care Initiative aimed to address wound care challenges, lower the health burden of wound care in Australia, and develop a national and integrated approach to wound management and research that can be readily embedded in the Australian health system. One activity under this initiative was to review research findings on wounds (acute, chronic and fundamental science of wound healing) to guide the future direction of Australian wound research through the identification of research gaps and priorities.
This scoping review aimed to identify research on the assessment, management and prevention of acute wounds, from 1) primary research studies conducted in Australia, and 2) worldwide synthesised evidence available within systematic reviews (SRs), evidence-based guidelines (EBGs), evidence summaries and consensus documents to provide a global context. The research questions guiding the review were:
- What are the characteristics of Australian research on the assessment, management and prevention of acute wounds?
- What research evidence is available in the global context in synthesised research documents and guidelines on the assessment, management and prevention of acute wounds?
- What are the research gaps specific to the assessment, management and prevention of acute wounds in Australia?
Methods
This scoping review is reported in accordance with the guidance provided by the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist15 and the Joanna Briggs Institute (JBI) scoping review methodology16. The review protocol was prospectively registered in the Open Science Framework (https://osf.io/bzs38) and published in Sandy-Hodgetts et al17.
Eligibility criteria
Inclusion criteria:
- Original qualitative or quantitative studies on the assessment, management or prevention of acute wounds conducted in Australia.
- Published in English.
- Worldwide EBGs, evidence summaries, consensus documents and SRs on the assessment, management or prevention of acute wounds.
- Human studies with adults aged from 18 years and older. Note that epidemiological studies were identified which provided data from both adults and younger age groups. These were included, as the data provided on adult wound prevalence was valuable.
- Any setting (e.g., community, general practice, outpatient department, residential aged care facilities, hospitals).
- Published between 1 January 2010 to 30 April 2022.
Exclusion criteria:
- Case series, case study or studies, editorials, general literature reviews.
- Conference abstracts, and conference proceedings.
Information sources
Sources were MEDLINE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Embase, Joanna Briggs Institute, Cochrane Library, American Psychological Association PsycInfo, Australian and New Zealand Clinical Trials Registry, International Standard Randomised Controlled Trials Registry and ClinicalTrials.gov. Websites and publications of professional associations for wound management included Wounds Australia, Wounds UK, Wounds International, Wounds Canada, European Wound Management Association, International Wound Infection Institute, International Surgical Wound Complications Advisory Panel, National Institute for Health and Care Excellence, World Health Organization, Wound Healing Society, World Union of Wound Healing Societies and New Zealand Wound Care Society.
Search strategy
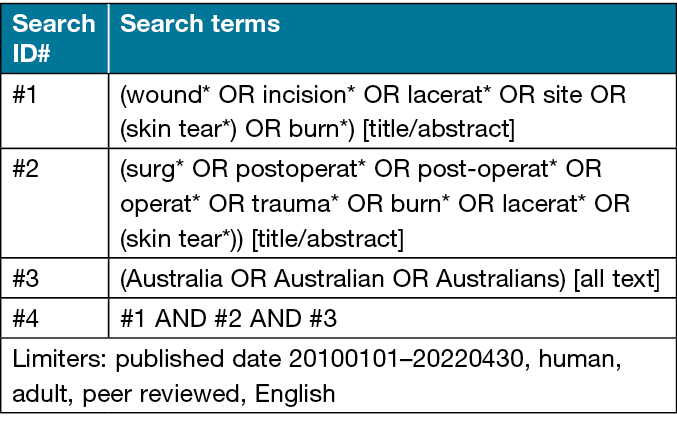
Databases and sites were searched for published literature fitting the inclusion criteria between 1 January 2010 to 30 April 2022. Key search terms were wound, incision, laceration, site, skin tear, surgical, postoperative, operative, trauma and burns. Limiters included only studies conducted with human participants, research articles, and studies published in English language. An example full search strategy is shown in Table 1.
Table 1. Search strategy example for Australian original research studies
Selection of documents
Results from searches were imported into EndNote X9. After excluding duplicates, two levels of screening were used to identify articles to be included: (i) title and abstract screening and (ii) full text screening. At each level, search results were reviewed by two independent researchers, and any disagreements reviewed by a third reviewer.
Data extraction
A data extraction tool was developed by one of the researchers and pilot tested and reviewed by two other researchers. Data were independently extracted by one researcher and cross checked against original articles by a second researcher to ensure the accuracy of extracted information. Data extracted included (i) study characteristics, (ii) research design or document type, (iii) type of acute wounds, (iv) study population, (v) focus topic and (vi) main outcomes.
Synthesis of results
Results were grouped and reported according to the type of acute wound the study or document focused on, i.e., surgical, burns, traumatic wounds, skin tears or samples with mixed types of acute wounds. Results were then organised under sections on the assessment, management or prevention of each type of wound. A narrative synthesis is reported in each section on the amount and types of studies and documents, primary focus topics, and an overview of results from the Australian studies.
Results
Following the searches, 10,543 potential articles were found. Of these, 2106 were duplicates, and 7286 articles did not fit the inclusion and exclusion criteria, including 251 articles which focused on non-wound related primary outcomes of surgical techniques. These articles are available in Supplementary file A. Of the 1151 remaining included articles, there were 318 Australian studies (294 quantitative studies and 24 qualitative studies), and 833 international studies (680 SRs, 28 EBGs, 79 evidence summaries and 46 consensus documents). Figure 1 displays the flow diagram of document inclusion. Australian documents on assessment (38%) included 120 quantitative studies and one qualitative study, documents on management (60%) included 179 quantitative studies and 11 qualitative studies, while documents on prevention (2%) included seven quantitative studies. Specific study designs of the included articles are displayed in Table 2. Due to the large number of SRs, references for the SRs are available in Supplementary file B.
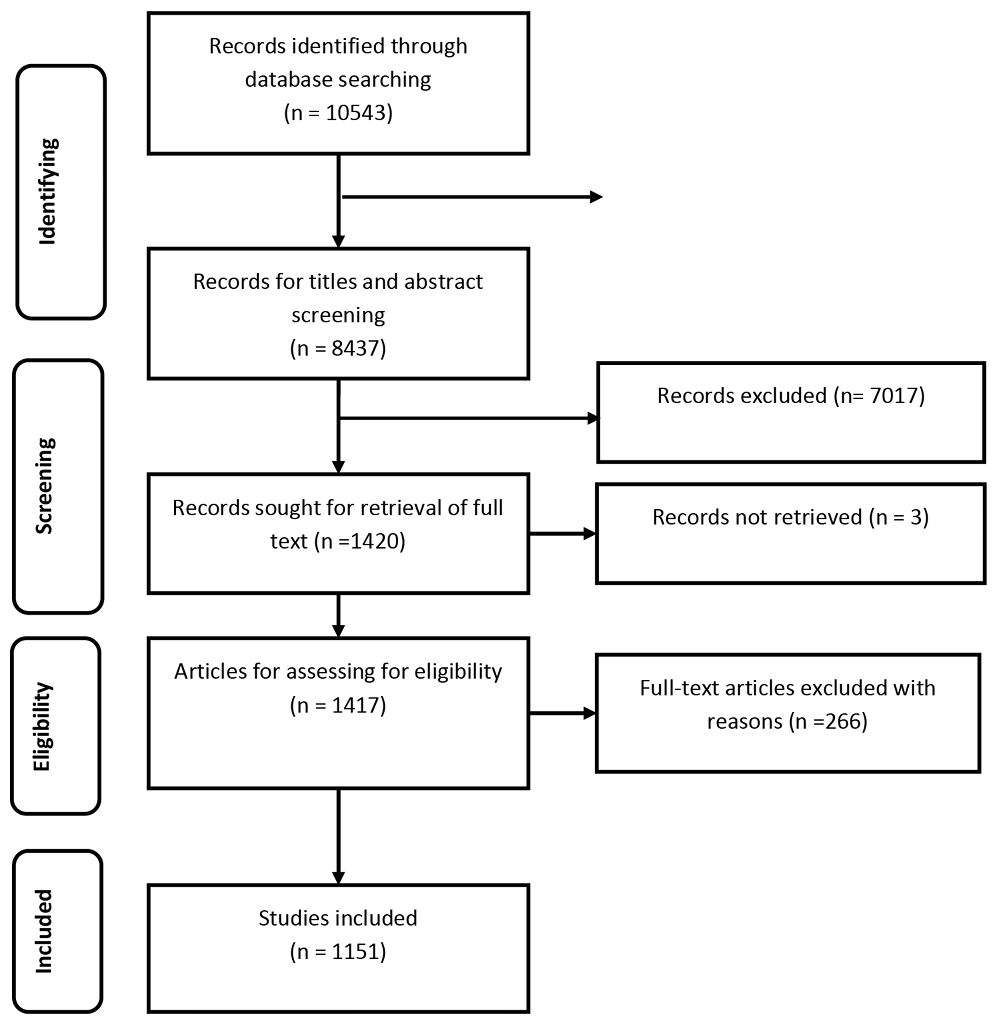
Figure 1. Full search strategy
Table 2. Study designs of included articles (n=1151)
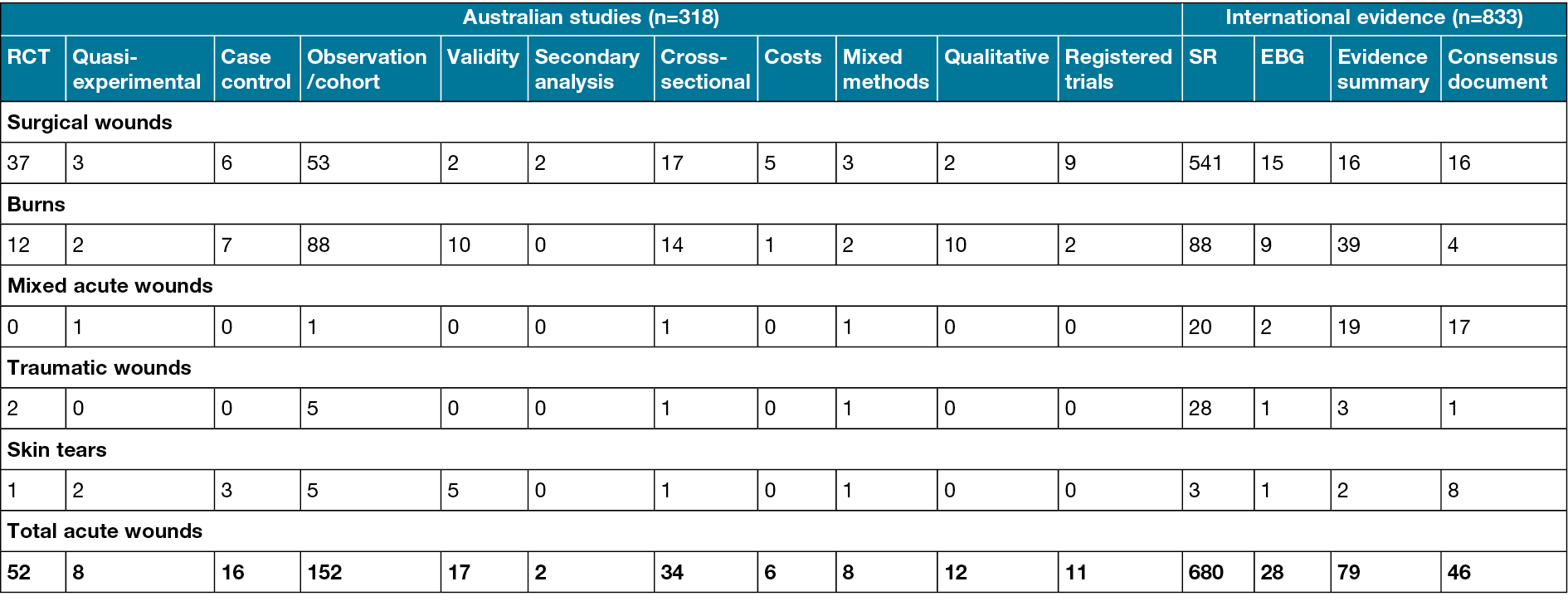
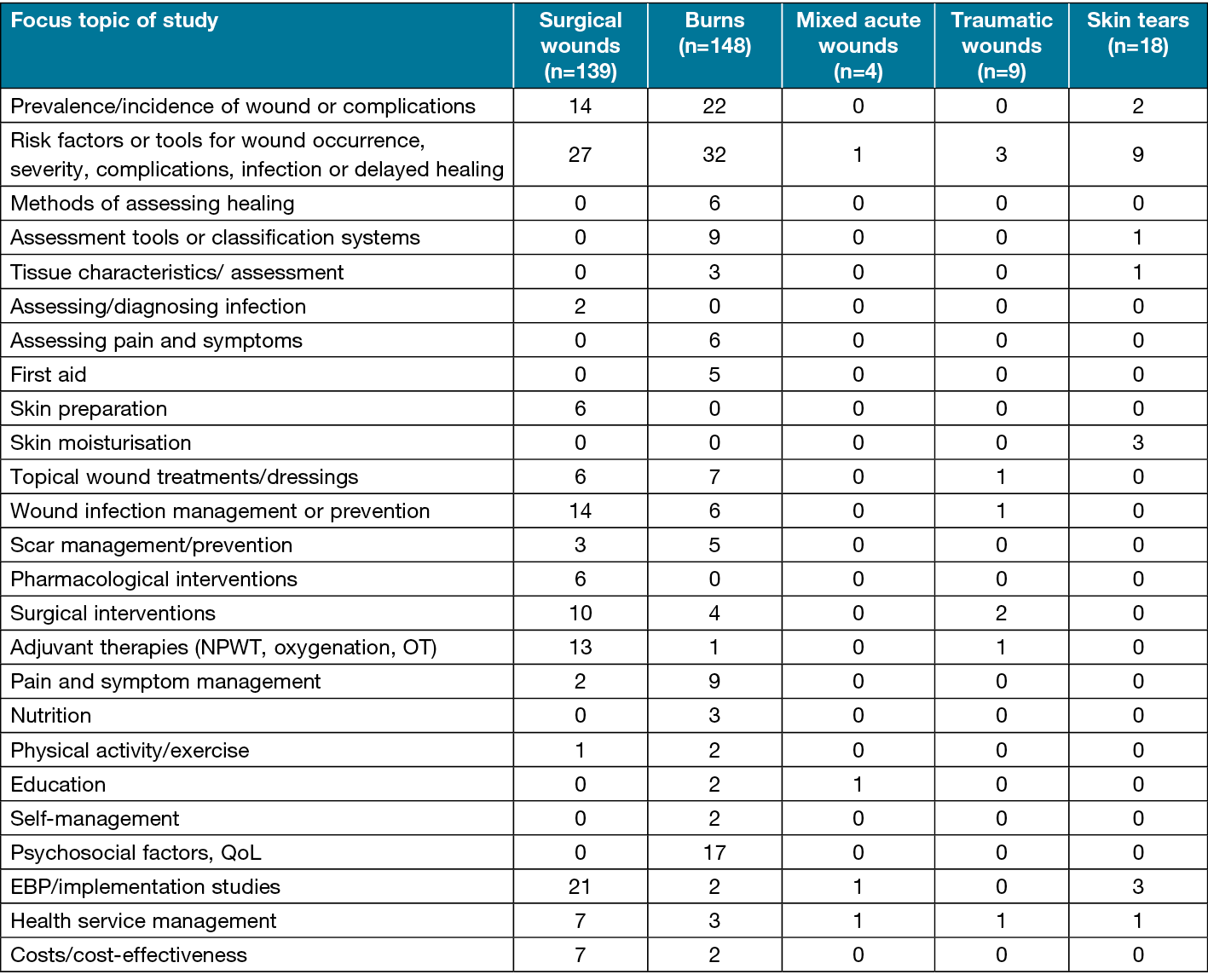
The largest number of documents were on surgical wounds (n=727, 63%), followed by burns (n=288, 25%), samples of mixed acute wound types (n=62, 5%), traumatic wounds (n=42, 4%), and skin tears (n=32, 3%). Of the Australian original research studies, 46% (n=148) were on burns, 44% (n=139) on surgical wounds, 6% (n=18) on skin tears, 3% (n=9) on traumatic wounds, and 1% (n=4) on mixed acute wound types. The most frequent research design of Australian studies was observational cohort studies (48%). Australian studies concentrated on wound management (60%), with only 38% on assessment, and 2% on the prevention of wounds.
The majority of Australian studies were conducted in hospital settings (78%), 7% were in follow-up care settings (outpatients, rehabilitation), 3% in community care, 3% in residential aged care, 3% in specialist surgery clinics, 2% in emergency care (ambulance, ED), 2% in combined settings, and 2% in general practice. Most study samples consisted of adults with wounds or adults with the possibility of developing a wound (81%), 6% were epidemiological population samples, 5% were samples of health professionals, and 4% were samples of ‘older adults’, defined as either 50 years and over, 60 years and over, 65 years and over or 70 years and over. Two studies were conducted with samples of both patients and health professionals, and one study with young adults aged 15–29 years.
The most frequent topics of investigation of Australian studies for each wound type are displayed in Table 3. An overview of the findings is reported below by wound type and area of investigation (assessment, management and/or prevention).
Table 3. Topics of investigation in Australian studies by wound type (n=318)
Surgical wounds
The largest number of documents (n=727) focused on surgical wounds, including 139 Australian studies. Study designs and topics are shown in Tables 2 & 3.
Assessment
A total of 97 documents focused on assessment of surgical wounds – 35 Australian studies, three EBGs, one evidence summary and 58 SRs.
Australian studies
Most studies on surgical wound complications focused on surgical site infections (SSI). Reported SSI incidence rates varied across type of surgery and setting, from 0.5–18.9%18–27. Two large studies found SSI rates decreased over time, i.e., SSI surveillance network data on cardiovascular, digestive, gynaecological-obstetrical, neurosurgical and orthopaedic surgery found decreased SSI rates over a median of 9 years of data28, while a Victorian surveillance program found decreased SSI rates from 2002–2013 from data on cardiac, Caesarean section, hip and knee prosthesis, colorectal, other abdominal, hysterectomy and vascular surgeries29. SSI rates varied according to procedure, with highest rates reported for colorectal survey28 and orthopaedic surgery29. In contrast, a study of pelvic exenteration found increasing SSI rates from 1994–2006 data, to 2014–2017 data30. One study of hip replacement found an 8.8% incidence of wound complications in general31.
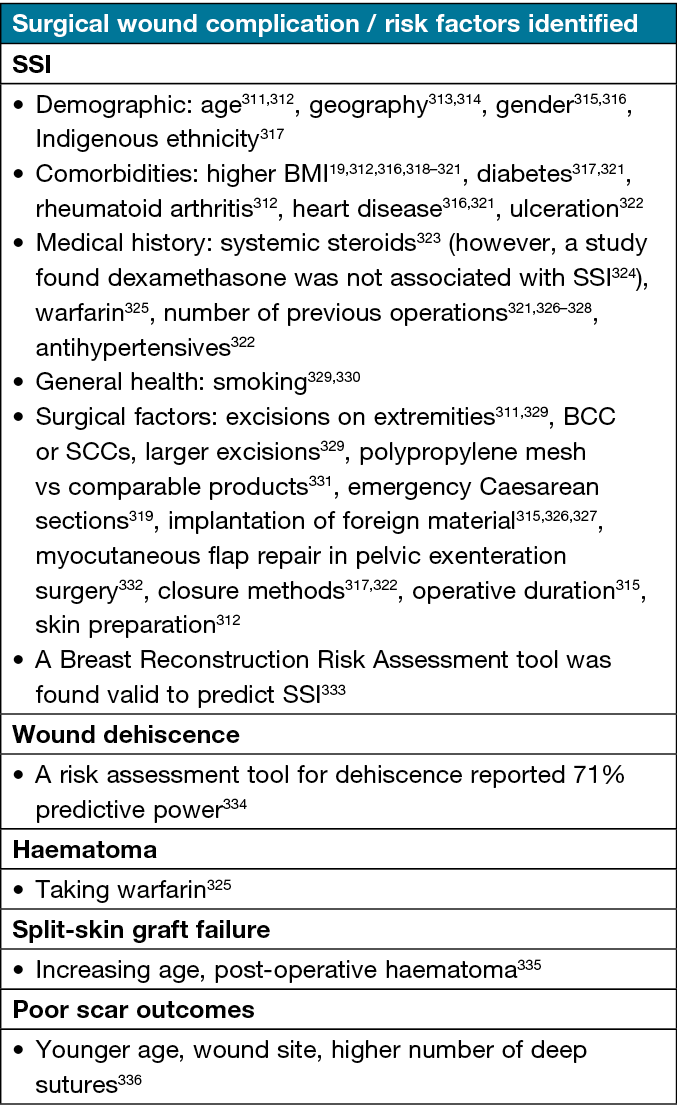
Results on risk factors for surgical wound complications are shown in Table 4. Looking at assessment tools or methods, one small 2012 study found superficial sternal wound swabs and blood cultures were useful in early diagnosis of deep sternal wound infection32, while a study of fluorescence imaging found it improved sensitivity of bacterial detection33.
Table 4. Risk factors for surgical wound complications identified in Australian studies
Worldwide reviews (SRs, EBGs, evidence summaries, consensus documents)
Three EBGs covered assessment of surgical wounds5,34,35 in addition to one evidence summary on assessing SSIs36. The SRs focused on incidence of SSIs; risk factors or assessment tools for complications; and defining SSI.
Management
Surgical wound management was investigated in 104 Australian studies, in addition to 683 SRs, 15 evidence summaries, 15 EBGs and 16 consensus documents. Designs and topics of studies are shown in Tables 2 & 3.
Australian studies
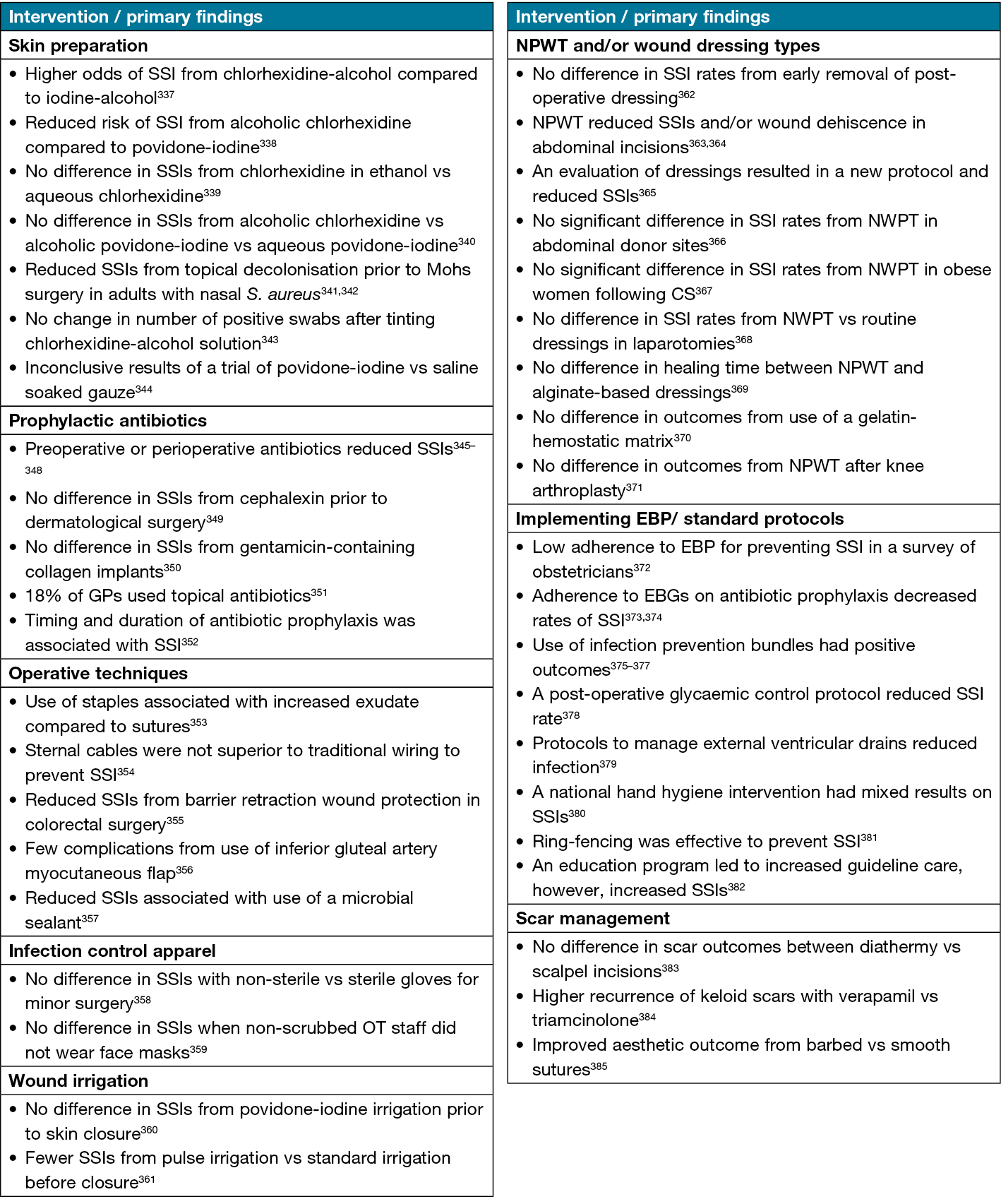
Primary findings from intervention studies to prevent wound complications are listed in Table 5. Findings on interventions to promote healing included that: there were positive outcomes from a house advancement flap for pilonidal sinus37 and V-Y advancement flaps for pretibial skin defects38; there was no improvement in healing from warming or oxygenation39; negative pressure wound therapy (NPWT) reduced the need for flap closure40; there were no differences in healing between polyurethane vs calcium alginate dressings41, or biosynthetic vs hydrocolloid dressings42; pilonidal abscess incisions took longer to heal after a midline vs lateral incision43; and there were increased complications from a 2cm excision margin compared to a 1cm margin for melanoma44. One study on pain management found intermittent wound infusion regimes were associated with greater reduction in pain scores45.
Table 5. Australian research findings on interventions to prevent surgical wound complications
On evidence-based practice (EBP), a qualitative study found barriers to EBG implementation were knowledge and skills deficits, access to protocols, suboptimal documentation and timing of education; while facilitators were active information seeking and patient participation46. Other results included that: there were significant gaps between EBGs and actual practices47–51; evaluation of implementation strategies improved EBP52,53; there were improvements adhering to antibiotic prophylaxis guidelines54; content and accuracy of documented wound assessment was variable55; and barriers in evidence-based wound management included traditional pretexts, economic factors, clinical knowledge and expertise and patient factors. Drivers were product choice, infection surveillance, interdisciplinary collaboration and regulatory mechanisms56.
On costs, studies found that: surgical wound complications were associated with significant costs57–61; NPWT for high-risk Caesarean section wounds was cost-effective62; antibiotic prophylaxis and antibiotic impregnated cement in hip arthroplasty reduced costs63; and reduced smoking rates before surgery would provide substantial economic benefits64. Studies on health service aspects reported that: wound care practice varied across clinical sites65; a checklist improved documented wound management66; wound care documentation did not meet Australian standards67; and a qualitative study reported difficulties with postoperative advice when managing after Caesarean section68. Eight trial protocols were registered without reported results, on dressings, NPWT, smartphone technology, skin preparation, surgical humidification, wound closure methods, care pathways, and topical medications69–76.
Worldwide reviews
A total of 15 EBGs covered the management of surgical wounds, 13 on SSIs5,35,77–87, and three including other surgical complications and/or strategies34,78,88. There were 15 evidence summaries covering: NPWT89; post-sternotomy mediastinitis90; skin preparation91,92; topical antibiotics93; perioperative strategies to prevent SSI94; delayed primary skin closure95; SSIs caused by methicillin-resistant Staphylococcus aureus (MRSA)96; skin graft and donor sites97; and the OT environment98–103. Consensus documents focused on: wound care and dressings104; SSI prevention105–111; skin graft donor sites112; wound dehiscence113; antibiotics after abscess excision114; NWPT115,116; wound infection117; and preventing wound complications10,118.
The SR topics included: skin preparation; glycaemic control; prophylactic antimicrobials; surgical hand antisepsis; temperature-related interventions; surgical techniques; wound closing techniques; exudate management; NPWT; debridement; infection management; dressings; platelet treatments; laser therapy; postoperative showering; care bundles; pain management; OT environment factors; nutrition; scar management; costs; and combined management protocols or pathways. Further details on the SRs are available in Supplementary File B.
Burns
Burn wound care is complex as demonstrated by the number and diversity of documents (288), with 148 Australian research studies, 88 SRs, nine EBGs, 39 evidence summaries, and four consensus documents. The study designs and topics are shown in Tables 2 & 3.
Assessment
A third (33%) of the documents looked at assessment – 72 Australian studies, four evidence summaries, four EBGs and 15 SRs.
Australian studies
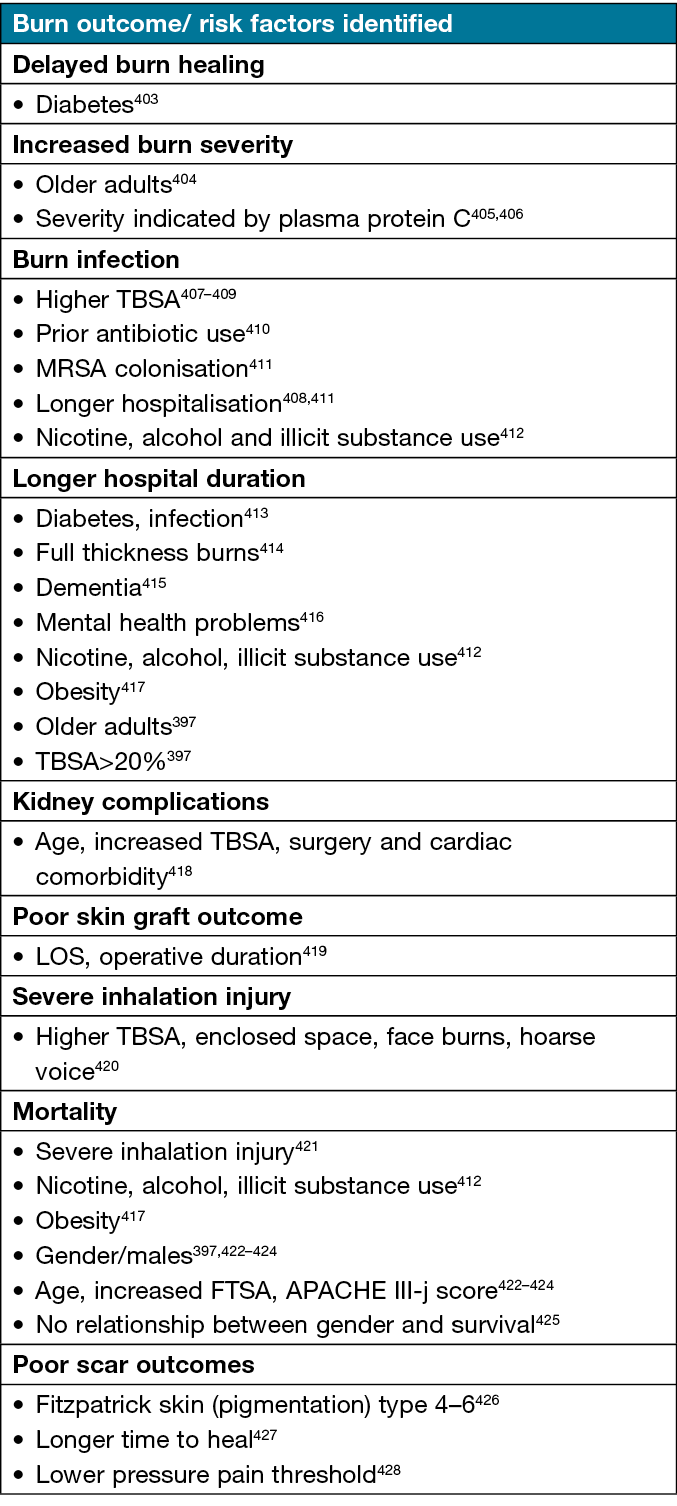
The focus and main outcomes of Australian studies on epidemiology and risk factors for poor burn outcomes are presented in Tables 6 & 7. Outcomes on burn and peri-wound assessment included that: bioimpedance spectroscopy was useful to assess oedema119,120 and progress in healing121; water displacement volumetry was reliable to assess postburn volume changes122; total body surface area (TBSA) was more accurately assessed using an online ‘Burnschart’ compared to conventional systems123; and there were significant inaccuracies in burn size estimation124. Two studies evaluated burn injury severity scores125,126, and one the Burn Specific Health Scale-B to assess recovery127.
Table 6. Australian research on epidemiological aspects of burns
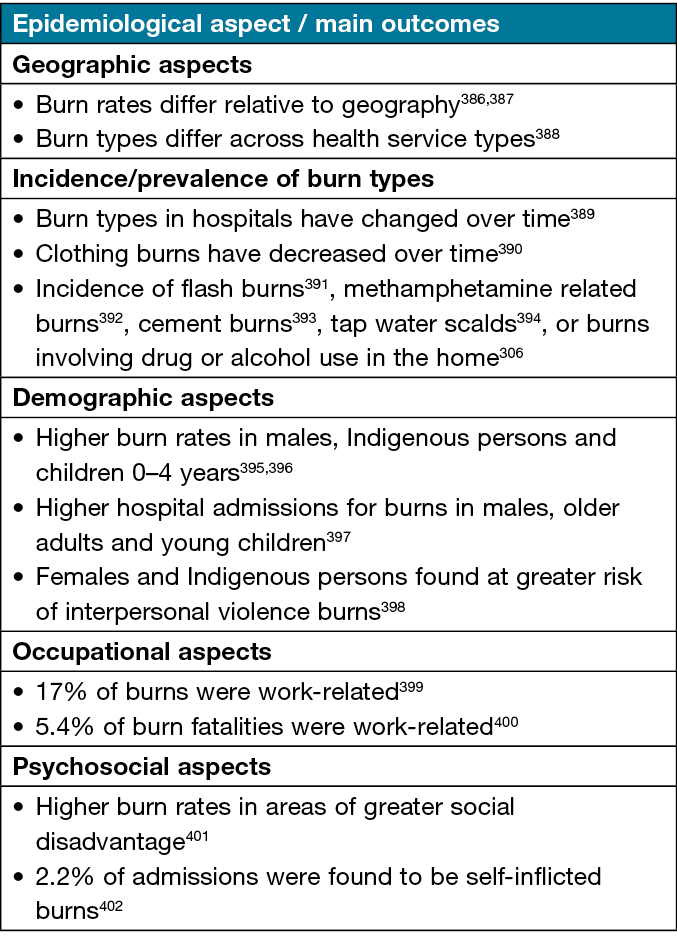
Table 7. Australian research on risk factors associated with poor outcomes from burns
Studies on psychosocial factors reported that: half of patients with burns had psychiatric, behavioural and/or drug use disorders128; persons with intentional burns had poorer outcomes129; psychosocial factors were associated with length of stay (Increased LOS)130; qualitative studies explored experiences of trauma, psychosocial adjustment and impact of burns on behavioural change re social activities131–137; patient concerns138 and depression impacted post-traumatic growth139,140; Type-D personality was associated with higher psychopathology141; hospitalised adults with burns spent two-thirds of time alone142; and attachment style was related to psychosocial recovery143.
On symptom research, predictors of fatigue were: being female; having a higher TBSA; and living in non-metropolitan areas144. Studies on pain found that: severity at 3 months predicted satisfaction with pain management145; the use of validated pain assessment tools enhanced assessment146; and pain assessment varied considerably147. A significant relationship was found between mental health and itch148, and that younger age was a predictor of itch149. A number of tools were validated, including: a dysphagia risk model150; Lower Limb Functional Index151; nomogram to predict quality of life (QoL)152; Brief Fatigue Inventory153; and Canadian Occupational Performance Measure154. On dysphagia, one study found no association between burn location and risk of dysphagia155, while another found burn area, head and neck burns, inhalation injury and ventilation were risk factors for dysphagia156.
Eight studies focused on assessment of complications, including the modified Vancouver Scar Scale157,158, Brisbane Burn Scar Impact Profile159, and photographic scar evaluation160. A positive troponin test was associated with cardiac complications161, while burn area, ICU admission and prolonged ventilation were associated with acute coagulopathy162 and increased risk of VTE163. Inhalational burns were a risk factor for infection164.
Worldwide reviews
Four EBGs, three evidence summaries, and 15 SRs covered assessment. The EBGs focused on acute pain165 or general burn assessment7,166,167. The evidence summaries focused on: clinical assessment168; TBSA assessment169; body image assessment170; and laser doppler imaging171. The SRs covered: burn microbiology; biomarkers; wound infection; measurement of burn depth or healing potential; infrared thermography; machine learning for burn assessment; and impact of burn injuries on body image or psychological outcomes.
Management
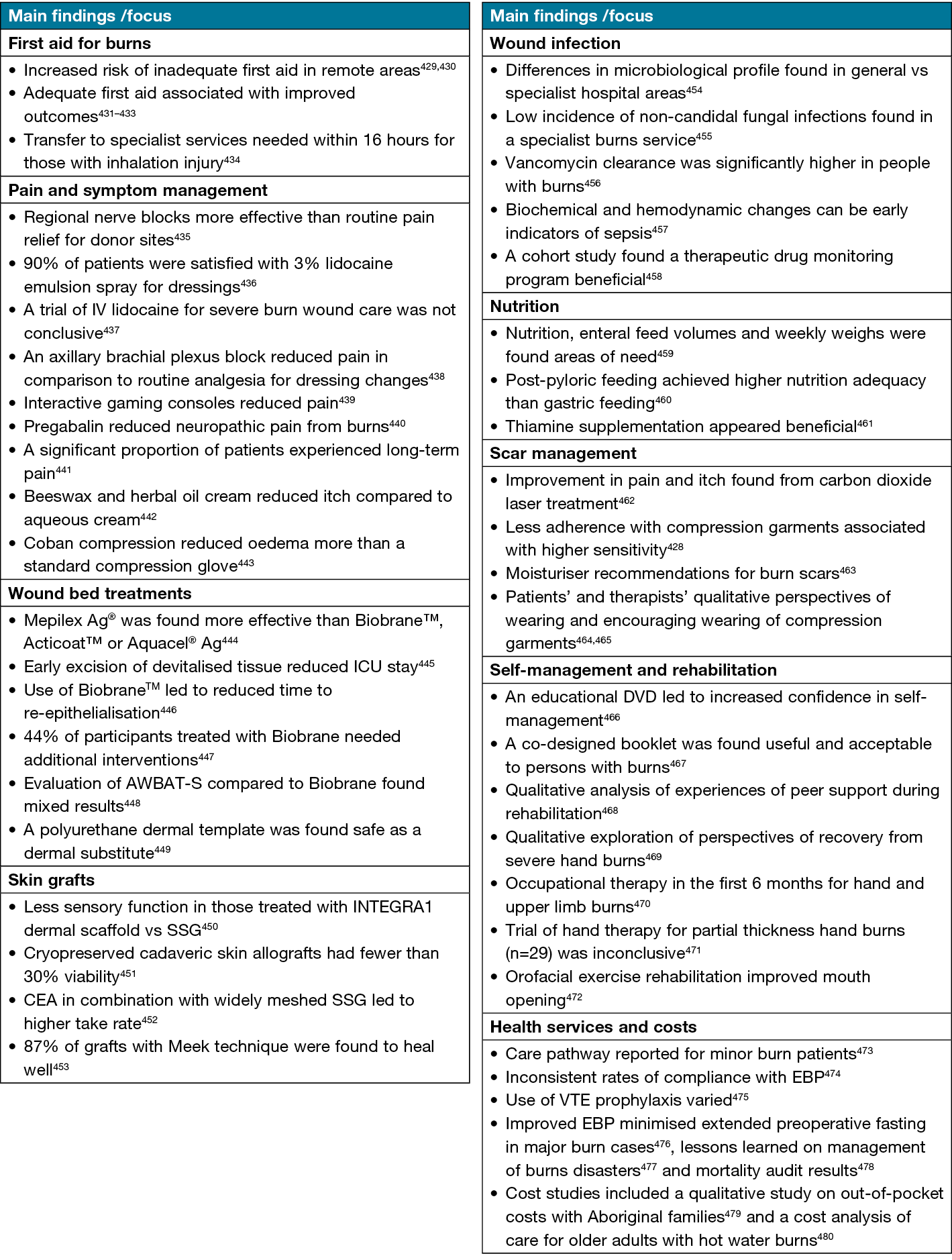
The management of burns was addressed in 192 documents – 75 Australian research studies, nine EBGs, 73 SRs, 35 evidence summaries and four consensus papers.
Australian studies
Study designs and topics are found in Tables 2 & 3, and findings on management intervention studies in Table 8.
Table 8. Australian studies on management of burns
Worldwide reviews
EBGs covered: burn management7,166,172–176; non-silicone or silicone gels177; management of noncomplex burns167; allied health and psychosocial management172; burn care under austere conditions178; and pain management165. Evidence summaries were on: first aid179–181; non-pharmacological interventions for pain and anxiety182–184; pruritus185; recombinant human growth hormone186; growth factors187; topical treatments or dressings188–194; burn surgery and grafting195–199; axillary burns200; silver-based antiseptics201; hydrotherapy202; blister management203; TNP204; health services205,206; shock wave therapy207; nutrition208,209; models of care210; liquefied petroleum gas burns211; and cement burns212. Consensus documents covered: pre-hospital management of burns213; first aid clinical guidelines214; burns care in mass casualty incidents215; and enzymatic debridement216. The SRs covered first aid; symptom management; infection; advanced biological treatments; debridement; dressings and topical treatments; adherence to treatment; nutrition and skin grafts.
Prevention
One Australian study addressed the prevention of burns, a controlled, comparative study which evaluated a targeted burn prevention message on safety knowledge and behaviour in an at-risk adult population217. One EBG provided recommendations in the prevention of burn injuries7.
Mixed acute wounds
A total of 62 documents addressed mixed types of acute wounds, including four Australian studies. Study designs and topics are shown in Tables 2 & 3.
Assessment
One Australian study found chemotherapy was significantly associated with longer healing time218. In addition, the Wounds Australia Standards provide recommendations for wound assessment, prevention and management219.
Management
A total of 59 documents addressed management – two Australian research studies, two EBGs, 19 evidence summaries, 17 consensus documents and 19 SRs.
Australian studies
A report from a mixed methods study found positive evaluations of a decision tree for products and wound management220, while a survey of nurses found around half were unaware of national wound management standards, and only 35% reported good knowledge of wound products12.
Worldwide reviews
Guidelines included a 2011 EBG on NPWT221 and national standards for wound management219. Evidence summaries covered: debridement222,223; pain management224–226; topical treatments or dressings227–237; and techniques to identify infection238. Consensus documents focused on: NPWT239,240; debridement241; exudate management242,243; wound infection244,245; aseptic technique246; dressings and topical treatments247–253; advanced cell, physical and IT based therapies254; scar management255; and team management256. The SRs focused on: wound bed management; debridement; NPWT; wound infection; dressings/topical treatments; nutrition; and adjunct interventions.
Prevention
Three documents addressed prevention of acute wounds – the Australian Standards for Wound Management219, a pre/post study of a model to promote evidence-based wound prevention257, and a SR on aloe vera for wound prevention258.
Traumatic wounds
There was a total of 42 documents on acute traumatic wounds – nine Australian studies, 28 SRs, one consensus document, three evidence summaries and one EBG. Study designs and topics are shown in Tables 2 & 3.
Assessment
Three documents addressed assessment – two Australian research studies and one SR.
Australian studies
There were two large Australian retrospective cohort studies on risk factors for obstetric perineal or anal sphincter traumatic injury. One study found ethnicity, shoulder dystocia and assisted delivery were risk factors for severe perineal tears259, while the other found gestational diabetes and a macrosomic baby combined with assisted delivery were risk factors for severe perineal tears or anal sphincter injuries260.
Worldwide reviews
One SR was found on risk factors for severe obstetric perineal trauma261.
Management
A total of 33 documents addressed management – six Australian research studies, one EBG, one consensus document, two evidence summaries and 23 SRs.
Australian studies
Two retrospective studies of lower limb traumatic wounds found improved outcomes from free-flap reconstruction within 3 days of injury and immediately following fracture fixation262 and significantly decreased deep infection rate in patients receiving NPWT compared to conventional dressings263. Another retrospective study found stable patients with single abdominal stab wounds could be safely managed with close observation without surgery264. A descriptive study of laceration repair outcomes reported good patient satisfaction with management; however, less with follow-up advice265. Studies on obstetric perineal trauma reported inconsistent health services and lack of standardised care266, and a trial of straight vs curved episiotomy scissors found no differences in outcomes267.
Worldwide reviews
One 2011 EBG focused on NPWT for traumatic wounds and reconstructive surgery268. Evidence summaries were found on the management of traumatic wounds in community settings269, and the impact of shaving on perineal wound infection270. A consensus document covered the risk, management and prevention of wound complications from birth injuries271. The SRs focused on the management of obstetric perineal trauma; preventing infection; NPWT; hyperbaric oxygen therapy (HBOT); lower extremity traumatic wounds; gunshot wounds; dog bite wounds; antiseptic solutions; haemostatic dressings; and flaps for revascularisation and soft-tissue coverage.
Prevention
Six documents addressed prevention – one Australian research study, one evidence summary and four SRs. A randomised controlled trial (RCT) found no effect from the use of a birth trainer to prevent pelvic floor trauma272. An evidence summary focused on preventing medical adhesive injury273. The SRs covered techniques to reduce perineal trauma.
Skin tears
A total of 32 documents were identified on skin tears – 18 Australian research studies, three SRs, one EBG, two evidence summaries and eight consensus documents. Study designs and topics are shown in Tables 2 & 3.
Assessment
A total of 16 documents addressed assessment – 11 Australian studies, one evidence summary, one SR and three consensus documents.
Australian studies
Two studies on skin tear prevalence reported: prevalence of 8.9% (5.5% hospital-acquired) in a hospital setting over 10 years, decreasing over time274; and 58–66% over 6 months in a retrospective study in aged care factilities275. On classification of skin tears, a multinational Delphi study (including Australia) of the validity and reliability of the International Skin Tear Advisory Panel classification system found moderate to high agreement, and added a definition of ‘skin flap’ to the system276.
Risk or prognostic factors for skin tears were identified in six studies: malnutrition277; use of heel protectors or anti-embolic stockings275; ecchymosis278,279; skin purpura278–280; haematoma278; history of previous skin tears278,280; oedema278; inability to reposition independently278; older age279; lower Braden score279; higher risk of falling279; osteoporosis279; use of corticosteroid inhaler279; history of falls in the previous 3 months280,281; elastosis280,281; and male gender280,281.
Four validity or reliability studies tested assessment tools or risk models for skin tears. A study in an aged care setting of non-invasive instruments for assessment of trans-epidermal water loss, hydration, skin thickness, elasticity, surface sebum and pH found mostly good intra-rater reliability and reproducibility with ultrasound measurements282. A prospective validation of a skin tear risk assessment tool in hospital patients found the tool did not perform well in predicting skin tears within 10 days283. However, a risk model for skin tears developed with aged care residents resulted in an area under the receiver operating characteristic curve of 0.854, sensitivity 81.7%, and specificity 81.4%280. Another study undertook a comparative analysis of predictive risk models for skin tears, finding predictive abilities ranged from AUC (Area Under the Curve) 0.67–0.85284.
Worldwide reviews
One SR found age-related skin changes, dehydration, malnutrition, sensory changes, mobility impairment, immunosuppressive medication, anticoagulants and mechanical factors were risk factors for occurrence of skin tears285. An evidence summary was identified on skin tear assessment in community settings286. Three consensus documents10–289 covered risk factors and assessment of skin tears.
Management
Ten documents addressed management – three Australian studies, one evidence summary, five consensus documents, and one EBG.
Australian studies
A protocol evaluation on emergency management of skin tears found a significant improvement in healing time290. Two pre-post studies aimed to increase implementation of EBGs – one in an acute aged and rehabilitation setting found increased compliance to guidelines and decreased prevalence of skin tears291. The second in a community setting found increased uptake of best practice in most items evaluated292.
Worldwide reviews
One EBG covered management of skin tears293 and an evidence summary covered management in community settings294. Consensus documents were found on: skin tear management10,287; management in aged skin288; lower limb skin tears294; and dressings295.
Prevention
A total of 14 documents covered prevention – six Australian papers, one SR, one EBG, and six consensus documents.
Australian studies
Four studies investigated the effectiveness of skin moisturising on prevention of skin tears. A cluster RCT of twice-daily moisturising vs usual care in aged care facilities found the intervention reduced the incidence of skin tears by almost 50%296, while a case control study of a similar intervention in an acute care setting found decreased incidence of skin tears, however, no statistically significant differences297. In contrast, a case-historical control study of twice daily moisturiser application in adults ≥65 years in an acute setting found a significant decrease in incidence of skin tears (p=0.006)298. Evaluation of a national program to increase use of emollient moisturiser to prevent skin tears in DVA (Department of Veterans Affairs) patients found increased dispensing of emollients; however, skin tear outcomes were not reported299. As noted above in the management section, two pre-post studies focused on implementation of EBGs; with regards to prevention, one in the acute aged and rehabilitation setting found decreased point prevalence of skin tears290, while the second in a community setting found increased uptake of best practice; however, it did not report incidence of skin tears291.
Worldwide reviews
A SR concluded there was inadequate evidence for recommendations on hygiene and emollients in preventing skin tears300. One EBG covered prevention of skin tears292. Six consensus documents were identified on maintaining skin integrity and prevention of skin tears10,288,301–303.
Discussion
This scoping review identified a consistent amount of Australian original research studies generated on acute wound care over the time of the review – with around 20 to 30 studies published each year between 2010–2022. The majority of Australian studies (90%) were focused on either burns or surgical wounds, with minimal studies on skin tears (6%) and traumatic wounds (3%). As surgery accounts for 25% of all hospital admissions304 and burn care also requires significant health system resources, there is a substantial impost on health service funds305, thus opportunities to reduce the impact are understandably the focus for research. This includes but is not limited to continuing education to remain abreast of the latest advances in the field and appropriate policy changes to reflect updates in EBP. Interestingly, this review revealed a paucity of research on skin tears, which is at odds with the reported prevalence of these wounds (e.g., 8.9% in an acute hospital population274, 19% in aged care settings257, 15–17% of wounds in community nursing setting2) and the subsequent demands on healthcare resources.
Results also demonstrate a gap in studies providing high level evidence, with small numbers of experimental or controlled study designs. Without evidence from these study types, there are limited opportunities to obtain robust findings from SRs, which themselves support development of clinical practice guidelines and policies. It is notable that an extremely large number of SRs were identified on surgical wounds in this review (n=541), in comparison to burns (n=88), traumatic wounds (n=28), acute wounds in general (n=20) and skin tears (n=3).
Most of the Australian studies were focused on wound assessment or management (97%), with only 2% on prevention217,257,272,290,296,297,298,299, despite the obvious potential benefits for the population and healthcare settings and resources through preventing avoidable wound types (e.g. burns, skin tears). A gap was noted in studies conducted in primary care settings, with 78% of studies conducted in hospital settings although a large proportion of care for wounds such as burns, surgical wounds, lacerations and skin tears is provided in primary health settings, including general practice, residential aged care and home/community nursing care3. The costs of wound care in these Australian primary healthcare settings is considerable2,3,61, thus an increased priority on research in primary healthcare settings is warranted to address the issue.
The identified gaps in this review, i.e., lack of research on skin tears and traumatic wounds, studies with strong research designs, studies on prevention and in studies in primary healthcare settings, provide important directions for future research. Similar gaps in studies on prevention and studies with strong research designs were found in a review on chronic wound research309. It is recommended to increase the focus of Australian wound research on prevention and prioritise resources for well designed research, particularly in community and primary healthcare settings. Outcomes from this future research are needed to form the essential building blocks for development of best practice guidelines, healthcare policy and optimal clinical practice to improve outcomes in all settings.
Limitations
This scoping review was broad within its scope, resulting in a large number of documents. As such, there are limitations to be considered such as the diversity of study designs, wound types and topics of research, populations and settings. Due to the broad nature of this scoping review, a quality evaluation was not undertaken. Our search strategies, despite testing and refining, may have not identified all eligible documents on this review topic.
Conclusions
Australian research on acute wounds has remained constant over the last decade, focused primarily on burns and surgical wounds, with relatively little research on skin tears or traumatic wounds. Results indicate additional gaps in research on wound prevention and in community and primary healthcare settings, despite the high prevalence of differing acute wound types cared for in these settings.
Conflict of interest
The authors declare no conflicts of interest.
Ethics statement
An ethics statement is not applicable.
Funding
This project was supported by funding from the Australian government under the Medical Research Future Fund. The funder had no role in the design, conduct or publication of the review.
Author contribution
All authors contributed to study design, UTB, KS-H and KF contributed to document identification and review, and KF and UTB to data analysis and synthesis. KF and UTB were responsible for manuscript preparation and all authors for feedback on the manuscript. All authors read and approved the final manuscript.
Author(s)
Kathleen Finlayson1, Ut T Bui*1, Fiona Wood2, Fiona Coyer3, Kylie Sandy-Hodgetts4,5
¹School of Nursing, Centre for Healthcare Transformation, Queensland University of Technology, Brisbane, QLD, Australia
2Burns Service Western Australia, Burn Injury Research Unit, University of Western Australia, Perth, WA, Australia
3School of Nursing, Midwifery and Social Work, The University of Queensland, Brisbane, QLD, Australia
4Centre for Molecular Medicine & Innovative Therapeutics, Health Futures Institute, Skin Integrity Research Group, Murdoch University, WA
5School of Biomedical Sciences, University of Western Australia, Perth, WA, Australia
*Corresponding author email thiut.bui@qut.edu.au
References
- Gottrup F, Henneberg E, Trangbaek R, Baekmark N, Zollner K, Sorensen J. Point prevalence of wounds and cost impact in the acute and community setting. J Wound Care 2013;22:413–4.
- Carville K, Alan J, Smith J. Best practice, best products, best outcomes in community wound care: three descriptive cohorts. Wound Prac Res 2022;30:196–206.
- Wilkie J, Carville K, Fu S, et al. Determining the actual cost of wound care in Australia. Wound Prac Res 2023;31:7–18.
- Ather S, Harding KG, Tate SJ. Wound management and dressings. In: Rajendran S, editor. Advanced textiles for wound care (2nd edition). Woodhead Publishing; 2019. p. 1–22.
- World Health Organization. Global guidelines for the prevention of surgical site infection, 2nd edition. Geneva: WHO; 2018.
- Sandy-Hodgetts K, Ousey K, Conway B, et al. International Surgical Wound Complications Advisory Panel (ISWCAP) best practice statement for the early identification and prevention of surgical wound complications. Wounds International; 2020. Available from: www.woundsinternational.com.
- Jeschke M, McCallum C, Baron D, Godleski M, Knighton J, Shahrokhi S. Best practice recommendations for the prevention and management of burns. Wounds Canada; 2018. Available from: https://www.woundscanada.ca/
- Bayat A, McGrouther DA, Ferguson MW. Skin scarring. BMJ 2003;326:88–92.
- Eliya-Masamba MC, Banda GW. Primary closure versus delayed closure for non bite traumatic wounds within 24 hours post injury. Cochrane Database Syst Rev 2013;CD008574.
- LeBlanc K, Baranoski S. Skin tears: state of the science: consensus statements for the prevention, prediction, assessment, and treatment of skin tears. Adv Skin Wound Care 2011;24:2–15.
- Ubbink DT, Brölmann FE, Go P, Vermeulen H. Evidence-based care of acute wounds: a perspective. Adv Wound Care 2015;4:286–294.
- Gillespie BM, Chaboyer W, Allen P, Morely N, Nieuwenhoven P. Wound care practices: a survey of acute care nurses. J Clin Nurs 2014;23:2618–2626.
- Cheng Q, Gibb M, Graves N, Finlayson K, Pacella RE. Cost-effectiveness analysis of guideline-based optimal care for venous leg ulcers in Australia. BMC Hlth Serv Res 2018;18:421.
- Edwards H, Finlayson K, Courtney M, Graves N, Gibb M, Parker C. Health service pathways for patients with chronic leg ulcers: identifying effective pathways for facilitation of evidence based wound care. BMC Hlth Serv Res 2013;13:86.
- Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–473.
- Peters MD, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H. Scoping reviews (2020 version). In: Aromataris E, Munn Z, editors. JBI manual for evidence synthesis. JBI; 2020.
- Sandy-Hodgetts K, Bui U, Coyer F, Weller C, Wood F, Finlayson K. Research priorities for acute wounds in adults in Australia: a scoping review protocol. Wound Practice Res 2021;29:171–175.
- Elliott TG, Thom GA, Litterick KA. Office based dermatological surgery and Mohs surgery: a prospective audit of surgical procedures and complications in a procedural dermatology practice. Australas J Dermatol 2012;53:264–271.
- Chaboyer W, Ellwood D, Thalib L, et al. Incidence and predictors of surgical site infection in women who are obese and give birth by elective Caesarean section: a secondary analysis. Aus NZ J Obstet Gynae 2022;62:234–240.
- Hines EM, Dowling S, Hegerty F, Pelecanos A, Tetsworth K. Bacterial infection of fasciotomy wounds following decompression for acute compartment syndrome. Injury 2021;52:2914–2919.
- El-Achi V, Wan KM, Brown J, Marshall D, McGee T. Readmissions for surgical site infections following Caesarean section. Aus NZ J Obstet Gynae 2018;58:582–585.
- Mobbs RJ, Phan K, Daly D, Rao PJ, Lennox A. Approach-related complications of anterior lumbar interbody fusion: results of a combined spine and vascular surgical team. Global Spine J 2015;6:147–154.
- Carter J, Philp S, Wan KM. Optimising recovery after surgery: predictors of early discharge and hospital readmission. Aus NZ J Obstet Gynae 2016;56:489–495.
- Butterworth P, Gilheany MF, Tinley P. Postoperative infection rates in foot and ankle surgery: a clinical audit of Australian podiatric surgeons, January to December 2007. Aust Health Rev 2010;34:180–185.
- Tai YJ, Borchard KLA, Gunson TH, Smith HR, Vinciullo C. Nasal carriage of Staphylococcus aureus in patients undergoing Mohs micrographic surgery is an important risk factor for postoperative surgical site infection: a prospective randomised study. Australas J Dermatol 2013;54:109–114.
- Si D, Rajmokan M, Lakhan P, Marquess J, Coulter C, Paterson D. Surgical site infections following coronary artery bypass graft procedures: 10 years of surveillance data. BMC Infect Dis 2014;14.
- Rusmir A, Salerno A. Postoperative infection after excisional toenail matrixectomy: a retrospective clinical audit. J Am Pod Med Assoc 2011;101:316–322.
- Abbas M, de Kraker MEA, Aghayev E, et al. Impact of participation in a surgical site infection surveillance network: results from a large international cohort study. J Hosp Inf 2019;102:267–276.
- Worth LJ, Bull AL, Spelman T, Brett J, Richards MJ. Diminishing surgical site infections in Australia: time trends in infection rates, pathogens and antimicrobial resistance using a comprehensive Victorian surveillance program, 2002–2013. Inf Control Hosp Epidemiol 2015;36:409–416.
- Venchiarutti RL, Solomon MJ, Koh CE, Young JM, Steffens D. Pushing the boundaries of pelvic exenteration by maintaining survival at the cost of morbidity. Br J Surg 2019;106:1393–1403.
- Vasantharao P, Fenbury D, Khan R, et al. Anterior approach to hip replacement and associated complications: an independent review. HIP Int 2020; 32: 312-317.
- Chaudhuri A, Shekar K, Coulter C. Post-operative deep sternal wound infections: making an early microbiological diagnosis. Euro J Cardiothoracic Surg 2012;41:1304–1308.
- Sandy-Hodgetts K, Andersen CA, Al-Jalodi O, Serena L, Teimouri C, Serena TE. Uncovering the high prevalence of bacterial burden in surgical site wounds with point-of-care fluorescence imaging. Int Wound J 2021; 19: 1438-1448.
- Harris C, Kuhnke J, Haley J, et al. Best practice recommendations for the prevention and management of surgical wound complications Wounds Canada 2017. Available from: https://www.woundscanada.ca/
- Smith MA, Dahlen NR. Clinical practice guideline: surgical site infection prevention. Orthopedic Nurs 2013;32:242-8.
- Sivapuram MS. Evidence summary. Surgical site infections: scoring systems. JBI EBP Database 2021;JBI-ES-732-1.
- Mackowski A, Levitt M. Outcomes of the house advancement flap for pilonidal sinus. Aust New Zeal J Surg 2017;87:692–94.
- Coombs CJ, Ng S, Stewart DA. The use of V-Y advancement flaps for closure of pretibial skin defects after excision of cutaneous lesions. Ann Plastic Surg 2013;71:402–405.
- Chiang N, Rodda OA, Sleigh J, Vasudevan T. Perioperative warming, oxygen, and Ilomedin on oxygenation and healing in infrainguinal bypass surgery. J Surg Res 2017;220:197–205.
- Lonie S, Hallam J, Yii M, et al. Changes in the management of deep sternal wound infections: a 12-year review. Aus NZ J Surg 2015;85:878–881.
- Higgins L, Wasiak J, Spinks A, Cleland H. Split-thickness skin graft donor site management: a randomized controlled trial comparing polyurethane with calcium alginate dressings. Int Wound J 2012;9:126–131.
- Solanki NS, MacKie IP, Greenwood JE. A randomised prospective study of split skin graft donor site dressings: AWBAT-D™ vs. Duoderm®. Burns 2012;38:889–898.
- Webb PM, Wysocki AP. Does pilonidal abscess heal quicker with off-midline incision and drainage? Tech Coloproctol 2011;15:179–183.
- Moncrieff MD, Gyorki D, Saw R, et al. 1 versus 2-cm excision margins for pT2-pT4 primary cutaneous melanoma (MelMarT): a feasibility study. Ann Surg Oncol 2018;25:2541–2549.
- Perry J, Byth K, Bullingham A. A retrospective cohort study of three wound catheter infusion analgesia regimes after midline laparotomy. Regional Anaes Pain Med 2022;47:222–227.
- Lin F, Gillespie BM, Chaboyer W, et al. Preventing surgical site infections: facilitators and barriers to nurses’ adherence to clinical practice guidelines. A qualitative study. J Clin Nurs 2019;28:1643–1652.
- Ding S, Lin F, Marshall AP, Gillespie BM. Nurses’ practice in preventing postoperative wound infections: an observational study. J Wound Care 2017;26:28–37.
- Lavers A, Yip WS, Sunderland B, et al. Surgical antibiotic prophylaxis use and infection prevalence in non-cosmetic breast surgery procedures at a tertiary hospital in Western Australia: a retrospective study. PeerJ 2018;2018.
- Jaber S, Rogers C, Sunderland B, et al. Appropriateness of surgical antibiotic prophylaxis for breast surgery procedures. Int J Clin Pharm 2017;39:483–486.
- Hooper TD, Hibbert PD, Hannaford NA, et al. Surgical site infection– a population-based study in Australian adults measuring the compliance with and correct timing of appropriate antibiotic prophylaxis. Anaes Int Care 2015;43:461–467.
- Bull AL, Worth LJ, Richards MJ. Impact of vancomycin surgical antibiotic prophylaxis on the development of methicillin-sensitive Staphylococcus aureus surgical site infections: report from Australian surveillance data (VICNISS). Ann Surg 2012;256:1089–1092.
- Lin F, Marshall AP, Gillespie B, et al. Evaluating the implementation of a multi-component intervention to prevent surgical site infection and promote evidence-based practice. Worldviews EB Nurs 2020;17:193–201.
- Broom J, Broom A, Anstey C, et al. Barriers–enablers–ownership approach: a mixed methods analysis of a social intervention to improve surgical antibiotic prescribing in hospitals. BMJ Open 2021;11:e046685.
- Bull AL, Worth LJ, Spelman T, Richards MJ. Antibiotic prescribing practices for prevention of surgical site infections in Australia: increased uptake of national guidelines after surveillance and reporting and impact on infection rates. Surg Infect 2017;18:834–840.
- Gillespie BM, Chaboyer W, Kang E, Hewitt J, Nieuwenhoven P, Morley N. Postsurgery wound assessment and management practices: a chart audit. J Clin Nurs 2014;23:3250–3261.
- Gillespie BM, Chaboyer W, Nieuwenhoven P, Rickard C. Drivers and barriers of surgical wound management in a large health care organisation: results of an environmental scan. Wound Prac Res 2012;20:90–102.
- Merollini KMD, Crawford RW, Graves N. Surgical treatment approaches and reimbursement costs of surgical site infections post hip arthroplasty in Australia: a retrospective analysis. BMC Hlth Serv Res 2013;13:91.
- Lydeamore MJ, Mitchell BG, Bucknall T, Cheng AC, Russo PL, Stewardson AJ. Burden of five healthcare associated infections in Australia. Antimicrob Resist Inf Control 2022;11:69.
- Peel TN, Cheng AC, Liew D, et al. Direct hospital cost determinants following hip and knee arthroplasty. Arth Care Res 2015;67:782–790.
- Stankiewicz M, Webster J, Coyer F. An evaluation of wound care product costs, from failed lower limb surgical sites compared with patients who heal immediately postoperatively. Wound Prac Res 2015;23:25–28.
- Sandy-Hodgetts K, Leslie GD, Lewin G, Hendrie D, Carville K. Surgical wound dehiscence in an Australian community nursing service: time and cost to healing. J Wound Care 2016;25:377–383.
- Tuffaha HW, Gillespie BM, Chaboyer W, Gordon LG, Scuffham PA. Cost-utility analysis of negative pressure wound therapy in high-risk Cesarean section wounds. J Surg Res 2015;195:612–622.
- Merollini KMD, Crawford RW, Whitehouse SL, Graves N. Surgical site infection prevention following total hip arthroplasty in Australia: a cost-effectiveness analysis. Am J Inf Control 2013;41:803–809.
- McCaffrey N, Scollo M, Dean E, White SL. What is the likely impact on surgical site infections in Australian hospitals if smoking rates are reduced? A cost analysis. PloS One 2021;16:e0256424.
- Gillespie BM, Walker R, Lin F, et al. Wound care practices across two acute care settings: a comparative study. J Clin Nurs 2020;29:831–839.
- Talia AJ, Drummond J, Muirhead C, Tran P. Using a structured checklist to improve the orthopedic ward round: a prospective cohort study. Orthopedics 2017;40:e663–e667.
- Gartlan J, Smith A, Clennett S, et al. An audit of the adequacy of acute wound care documentation of surgical inpatients. J Clin Nurs 2010;19:2207–2214.
- Kealy MA, Small RE, Liamputtong P. Recovery after Caesarean birth: a qualitative study of women’s accounts in Victoria, Australia. BMC Preg Childbirth 2010;10.
- Sandy-Hodgetts K. A non randomised pragmatic trial for the early detection and prevention of surgical wound complications using an advanced hydropolymer wound dressing and smartphone technology; the EDISON study. ANZCTR 2020. Int Wound J 2021; 19: 2174-2182.
- Douglas C. Type 1 keystone flap versus simple primary closure for wound closure – a prospective randomised controlled trial. Int CTR Platform 2012. ANZCTR 2012; 12612000500853, www.anzctr.org.au
- Weeden C. The STEP study: a pragmatic, randomized, controlled trial comparing two post operative management pathways in knee or hip replacement surgery. Int CTR 2016; www.who.int/clinical-trials-registry-platform
- Greenwood JE. A prospective, randomised trial to compare pain and healing between skin-graft donor site dressings: Duoderm vs AWBAT-D. ANZCTR 2010; www.anzctr.org.au
- Arachchi A. Does utilisation of surgical humidification reduce surgical site infection in colorectal surgery patients? A randomised control trial. ANZCTR 2020; www.anzctr.org.au
- Chaboyer W. ADding negative pRESSure to improve healING in obese women undergoing Caesarean section (the DRESSING trial). ANZCTR 2012; www.anzctr.org.au
- Sandy-Hodgetts K. Testing the effectiveness of negative pressure wound therapy in the at risk obstetric population for the prevention of surgical wound complications: the CYGNUS trial. ANZCTR 2018: www.anzctr.org.au
- Sandy-Hodgetts K. Effectiveness of negative pressure wound therapy (NPWT) in the prevention of post-operative surgical wound dehiscence in at risk patients following abdominal surgery: a multicentre randomised control trial. ANZCTR 2012: www.anzctr.org.au
- van Schalkwyk J, Van Eyk N. No. 247-antibiotic prophylaxis in obstetric procedures. J Obstet Gynae Can 2017;39:e293–e299.
- Bratzler DW, Dellinger EP, Olsen KM, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health-Sys Pharm 2013;70:195–283.
- Allegranzi B, Bischoff P, de Jonge S, et al. New WHO recommendations on preoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis 2016;16:e276–e287.
- Ban KA, Minei JP, Laronga C, et al. Executive summary of the American College of Surgeons/Surgical Infection Society surgical site infection guidelines 2016 update. Surg Infect 2017;18:379–382.
- Berríos-Torres SI, Umscheid CA, Bratzler DW, et al. Centers for Disease Control and Prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg 2017;152:784–791.
- Abbo LM, Grossi PA. Surgical site infections: guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant 2019;33:e13589.
- Ohge H, Mayumi T, Haji S, et al. The Japan Society for Surgical Infection: guidelines for the prevention, detection, and management of gastroenterological surgical site infection, 2018. Surg Today 2021:51.
- Shaffer WO, Baisden JL, Fernand R, Matz PG. An evidence-based clinical guideline for antibiotic prophylaxis in spine surgery. Spine J 2013;13:1387–1392.
- Borchardt RA, Tzizik D. Update on surgical site infections: the new CDC guidelines. JAAPA 2018;31:52–54.
- National Institute for Health and Care Excellence (NICE). Surgical site infections: prevention and treatment. NICE; 2021.
- Allegranzi B, Zayed B, Bischoff P, et al. New WHO recommendations on intraoperative and postoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis 2016;16:e288–e303.
- Kalliainen LK. ASPS clinical practice guideline summary on reduction mammaplasty. Plast Recon Surg 2012;130:785–789.
- Tan A, Gollop ND, Klimach SG, Maruthappu M, Smith SF. Should infected laparotomy wounds be treated with negative pressure wound therapy? Int J Surg 2014;12:26–29.
- Yu AW, Rippel RA, Smock E, Jarral OA. In patients with post-sternotomy mediastinitis is vacuum-assisted closure superior to conventional therapy? Interact Cardiovasc Thor Surg 2013;17:861–865.
- Mattis P. Evidence summary. Preoperative skin preparation: hair removal. JBI EBP Database 2019;JBI-ES-3065-1.
- Sydor A. Evidence summary. Prevention of infection: skin antiseptics prior to surgical incision. JBI EBP Database 2020;JBI-ES-2377-1.
- Moola S. Evidence summary. Surgical site infection in wound healing by primary intention (prevention): topical antibiotics. JBI EBP Database 2021;JBI-ES-1068-1.
- Podder V. Evidence summary. Surgical site infections (post Cesarean section): perioperative prevention. JBI EBP Database 2021;JBI-ES-1387-1.
- Sivapuram MS. Evidence summary. Surgical infections (abdominal incisions): primary vs delayed primary skin closure. JBI EBP Database 2021;JBI-ES-1709-1.
- Owaya A. Evidence summary. Surgical wounds infected by Methicillin-resistant Staphylococcus aureus (MRSA): antibiotic therapy. JBI EBP Database 2021;JBI-ES-1095-1.
- Slade S. Evidence summary. Skin graft: management. JBI EBP Database 2019;JBI-ES-3325-1.
- Minooee S. Evidence summary. Surgical site infection: operating room/theater environment controls. JBI EBP Database 2021;JBI-ES-603-1.
- 99. Sivapuram MS. Evidence summary. Surgical site infection: surgical scrubbing, gowning and glowing. JBI EBP Database 2020;JBI-ES-2344-1.
- Sivapuram MS. Evidence summary. Perioperative settings: traffic control. JBI EBP Database 2021;JBI-ES-1386-1.
- Marin T. Evidence summary. Surgical site infection: movement in the operating room. JBI EBP Database 2020;JBI-ES-65-1.
- Marin T. Evidence summary. Environmental control measures (surgical staff): interventions to reduce door openings to operating rooms. JBI EBP Database 2020;JBI-ES-62-1.
- Sivapuram MS. Evidence summary. Perioperative settings: environment cleaning. JBI EBP Database 2021;JBI-ES-1493-1.
- Morgan-Jones R, Cao L, Daozhang C, et al. Incision care and dressing selection in surgical wounds: findings from an international meeting in the APAC region. Wounds International; 2021.
- De Simone B, Sartelli M, Coccolini F, et al. Intraoperative surgical site infection control and prevention: a position paper and future addendum to WSES intra-abdominal infections guidelines. World J Emerg Surg 2020;15:10.
- Del Toro López MD, Arias Díaz J, Balibrea JM, et al. Executive summary of the Consensus Document of the Spanish Society of Infectious Diseases and Clinical Microbiology (SEIMC) and of the Spanish Association of Surgeons (AEC) in antibiotic prophylaxis in surgery. Cirugia española 2021;99:11–26.
- Wounds UK. Post-operative wound care: reducing the risk of surgical site infection. Wounds UK; 2020.
- O’Hara LM, Thom KA, Preas MA. Update to the Centers for Disease Control and Prevention and the Healthcare Infection Control Practices Advisory Committee Guideline for the prevention of surgical site infection (2017): a summary, review, and strategies for implementation. Am J Inf Control 2018;46:602–609.
- Pellegrini JE, Toledo P, Soper DE, et al. Consensus bundle on prevention of surgical site infections after major gynecologic surgery. Obstet Gynecol 2017;129:50–61.
- Ariyan S, Martin J, Lal A, et al. Antibiotic prophylaxis for preventing surgical-site infection in plastic surgery: an evidence-based consensus conference statement from the American Association of Plastic Surgeons. Plast Reconstruct Surg 2015;135:1723–1739.
- Badia JM, Rubio Pérez I, Manuel A, et al. Surgical site infection prevention measures in general surgery: position statement by the Surgical Infections Division of the Spanish Association of Surgery. Cirugia española 2020;98:187–203.
- World Union of Wound Healing Societies. WUWHS position document: skin graft donor site management in the treatment of burns and hard-to-heal wounds. Wounds International; 2019.
- World Union of Wound Healing Societies. Consensus document. Surgical wound dehiscence: improving prevention and outcomes. World Union of Wound Healing Societies; 2018.
- Vermandere M, Aertgeerts B, Agoritsas T, et al. Antibiotics after incision and drainage for uncomplicated skin abscesses: a clinical practice guideline. BMJ 2018;360:k243.
- Willy C, Agarwal A, Andersen CA, et al. Closed incision negative pressure therapy: international multidisciplinary consensus recommendations. Int Wound J 2017;14:385–398.
- World Union of Wound Healing Societies. Closed surgical incision management: understanding the role of NPWT. Wounds International; 2016.
- Pan A, Cauda R, Concia E, et al. Consensus document on controversial issues in the treatment of complicated skin and skin-structure infections. Int J Inf Dis 2010;14:S39–S53.
- Ousey K, Gillibrand W, Stephenson J. Achieving international consensus for the prevention of orthopaedic wound blistering: results of a Delphi survey. Int Wound J 2013;10:177–184.
- Kenworthy P, Grisbrook TL, Phillips M, et al. Bioimpedance spectroscopy: a technique to monitor interventions for swelling in minor burns. Burns 2017;43:1725–1735.
- Edwick DO, Hince DA, Rawlins JM, Wood FM, Edgar DW. Bioimpedance spectroscopy is a valid and reliable measure of edema following hand burn injury (part 1: method validation). J Burn Care Res 2020;41:780–787.
- Kenworthy P, Phillips M, Grisbrook TL, Gibson W, Wood FM, Edgar DW. Monitoring wound healing in minor burns – a novel approach. Burns 2018;44:70–76.
- Edgar DW, Briffa NK, Wood FM. Whole arm water displacement volumetry is a reliable and sensitive measure: a pilot to assess acute postburn volume change. J Burn Care Res 2016;37:e508–e514.
- Ahn CS, ONeill SP, Maitz PK. Improving accuracy of burn referrals through the use of an internet-based burns chart. Euro J Plast Surg 2011;34:331–335.
- Harish V, Raymond AP, Issler AC, et al. Accuracy of burn size estimation in patients transferred to adult burn units in Sydney, Australia: an audit of 698 patients. Burns 2015;41:91–99.
- Cheung W, Clayton N, Li F, et al. The effect of endotracheal tube size on voice and swallowing function in patients with thermal burn injury: an evaluation using the Australian Therapy Outcome Measures (AusTOMS). Int J Speech-Lang Pathol 2013;15:216–220.
- Cassidy JT, Phillips M, Fatovich D, Duke J, Edgar D, Wood F. Developing a burn injury severity score (BISS): adding age and total body surface area burned to the injury severity score (ISS) improves mortality concordance. Burns 2014;40:805–813.
- Finlay V, Phillips M, Wood F, Hendrie D, Allison GT, Edgar D. Enhancing the clinical utility of the Burn Specific Health Scale-Brief: not just for major burns. Burns 2014;40:328–336.
- Alexander W, Coghlan P, Greenwood JE. A 365-day view of the difficult patients treated in an Australian adult burn center. J Burn Care Res 2015;36:e146–e152.
- Vetrichevvel TP, Randall SM, Wood FM, Rea S, Boyd JH, Duke JM. A population-based comparison study of the mental health of patients with intentional and unintentional burns. Burn Trauma 2018;6:31.
- Knol R, Kelly E, Paul E, et al. The psychosocial complexities of acute burn patients in an Australian trauma hospital. Burns 2020;46:447–453.
- Connell KM, Phillips M, Coates R, Doherty-Poirier M, Wood FM. Sexuality, body image and relationships following burns: analysis of BSHS-B outcome measures. Burns 2014;40:1329–1337.
- Connell KM, Coates R, Wood FM. Burn injuries lead to behavioral changes that impact engagement in sexual and social activities in females. Sexuality Disabil 2015;33:75–91.
- Gullick JG, Taggart SB, Johnston RA, Ko N. The trauma bubble: patient and family experience of serious burn injury. J Burn Care Res 2014;35:e413–e427.
- Connell KM, Coates R, Wood FM. Sexuality following burn injuries: a preliminary study. J Burn Care Res 2013;34:e282–9.
- Kornhaber R, Wilson A, Abu-Qamar MZ, McLean L. Coming to terms with it all: adult burn survivors’ ‘lived experience’ of acknowledgement and acceptance during rehabilitation. Burns 2014;40:589–597.
- McLean LM, Rogers V, Kornhaber R, et al. The patient-body relationship and the “lived experience” of a facial burn injury: a phenomenological inquiry of early psychosocial adjustment. J Multidis Healthcare 2015;8:377–387.
- Johnson RA, Taggart SB, Gullick JG. Emerging from the trauma bubble: redefining ‘normal’ after burn injury. Burns 2016;42:1223–1232.
- Dowda DJ, Li F. Major concerns and issues in burn survivors in Australia. Burns Trauma 2014;2:84–87.
- Martin L, Byrnes M, Bulsara MK, McGarry S, Rea S, Wood F. Quality of life and posttraumatic growth after adult burn: a prospective, longitudinal study. Burns 2017;43:1400–1410.
- Martin L, Rea S, Wood F. A quantitative analysis of the relationship between posttraumatic growth, depression and coping styles after burn. Burns 2021;47:1748–1755.
- Mujezinovic A, Kwiet J, Kornhaber R, et al. Type-D Personality and elevated psychological symptoms in early adjustment of severe burn injury patients. Issues Mental Health Nurs 2018;39:337–343.
- Plaza A, Adsett J, Byrnes A, McRae P. Physical activity levels in hospitalised adults with burn injuries. J Burn Care Res 2021; 43:1048-1054
- Holt R, Kornhaber R, Kwiet J, et al. Insecure adult attachment style is associated with elevated psychological symptoms in early adjustment to severe burn: a cross-sectional study. Burns 2019;45:1359–1366.
- Gabbe BJ, Cleland H, Watterson D, et al. Predictors of moderate to severe fatigue 12 months following admission to hospital for burn: results from the Burns Registry of Australia and New Zealand (BRANZ) long term outcomes project. Burns 2016;42:1652–1661.
- Andrews RM, Browne AL, Wood F, Schug SA. Predictors of patient satisfaction with pain management and improvement 3 months after burn injury. J Burn Care Res 2012;33:442–452.
- Taggart S, Skylas K, Brannelly A, Fairbrother G, Knapp M, Gullick J. Using a clinical judgement model to understand the impact of validated pain assessment tools for burn clinicians and adult patients in the ICU: a multi-methods study. Burns 2021;47:110–126.
- Tracy LM, Cleland H, Cameron PA, Gabbe BJ. Pain assessment following burn injury in Australia and New Zealand: variation in practice and its association on in-hospital outcomes. Australas Emerg Care 2021;24:73–79.
- McGarry S, Burrows S, Ashoorian T, et al. Mental health and itch in burns patients: potential associations. Burns 2016;42:763–768.
- Tracy LM, Edgar DW, Schrale R, Cleland H, Gabbe BJ. Predictors of itch and pain in the 12 months following burn injury: results from the Burns Registry of Australia and New Zealand (BRANZ) long-term outcomes project. Burns Trauma 2020;8:004.
- Rumbach AF, Ward EC, Heaton S, Bassett LV, Webster A, Muller MJ. Validation of predictive factors of dysphagia risk following thermal burns: a prospective cohort study. Burns 2014;40:744–750.
- Gittings PM, Heberlien N, Devenish N, et al. The Lower Limb Functional Index – a reliable and valid functional outcome assessment in burns. Burns 2016;42:1233–1240.
- Finlay V, Phillips M, Allison GT, et al. Towards more efficient burn care: identifying factors associated with good quality of life post-burn. Burns 2015;41:1397–1404.
- Toh C, Li M, Finlay V, et al. The Brief Fatigue Inventory is reliable and valid for the burn patient cohort. Burns 2015;41:990–997.
- McKittrick A, Jones A, Lam H, Biggin E. A feasibility study of the Canadian Occupational Performance Measure (COPM) in the burn cohort in an acute tertiary facility. Burns 2021. doi:10.1016/j.burns.2021.09.005.
- Clayton NA, Nicholls CM, Blazquez K, et al. Dysphagia in older persons following severe burns: burn location is irrelevant to risk of dysphagia and its complications in patients over 75 years. Burns 2018;44:1997–2005.
- Rumbach AF, Ward EC, Cornwell PL, Bassett LV, Khan A, Muller MJ. Incidence and predictive factors for dysphagia after thermal burn injury: a prospective cohort study. J Burn Care Res 2011;32:608–616.
- Finlay V, Burrows S, Kendell R, et al. Modified Vancouver Scar Scale score is linked with quality of life after burn. Burns 2017;43:741–746.
- Gankande TU, Wood FM, Edgar DW, et al. A modified Vancouver Scar Scale linked with TBSA (mVSS-TBSA): inter-rater reliability of an innovative burn scar assessment method. Burns 2013;39:1142–1149.
- Tyack Z, Kimble R, McPhail S, Plaza A, Simons M. Psychometric properties of the Brisbane burn scar impact profile in adults with burn scars. PLoS One 2017;12:e0184452.
- Simons M, Tyack Z. Health professionals’ and consumers’ opinion: what is considered important when rating burn scars from photographs? J Burn Care Res 2011;32:275–285.
- Alexander W, Schneider H-G, Smith C, Cleland H. The incidence and significance of raised troponin levels in acute burns. J Burn Care Res 2018;39:729–735.
- Mitra B, Wasiak J, Cameron PA, O’Reilly G, Dobson H, Cleland H. Early coagulopathy of major burns. Injury 2013;44:40–43.
- Lu P, Harms K-A, Paul E, Bortz H, Lo C, Cleland H. Venous thromboembolism in burns patients: are we underestimating the risk and underdosing our prophylaxis? JPRAS 2021;74:1814–1823.
- Patel BM, Paratz JD, Mallet A, et al. Characteristics of bloodstream infections in burn patients: an 11-year retrospective study. Burns 2012;38:685–690.
- Romanowski KS, Carson J, Pape K, et al. American Burn Association guidelines on the management of acute pain in the adult burn patient: a review of the literature, a compilation of expert opinion, and next steps. J Burn Care Res 2020;41:1129–1151.
- ISBI Practice Guidelines Committee, Ahuja RB, Gibran N, et al. ISBI practice guidelines for burn care. Burns 2016;42:953–1021.
- Wounds International. International best practice guidelines: effective skin and wound management of noncomplex burns. Wounds International; 2014.
- Munn Z, Whitehorn A. Evidence summary. Burns: clinical depth assessment. JBI EBP Database 2021;JBI-ES-529-1.
- Moola S. Evidence summary. Total body surface area (TBSA) assessment in burn injuries. JBI EBP Database 2021;JBI-ES-3513-2.
- Gyi AA. Evidence summary. Burn injury: assessment for body image concerns. JBI EBP Database 2021;JBI-ES-1880-2.
- Rathnayake T, Nnaji C. Evidence summary. Burn depth assessment (partial thickness burns): laser doppler imaging (LDI). JBI EBP Database 2021;JBIES-3382-1.
- European Burns Association. European practice guidelines for burn care: minimum level of burn care provision in Europe. European Burns Association; 2017.
- Allorto N, Atieh B, Bolgiani A, et al. ISBI Practice guidelines for burn care, part 2: burns 2018;44:1617–1706.
- Koyro KI, Bingoel AS, Bucher F, Vogt PM. Burn guidelines – an international comparison. Euro Burn J 2021;2.
- Yoshino Y, Ohtsuka M, Kawaguchi M, et al. The wound/burn guidelines – 6: guidelines for the management of burns. J Dermatol 2016;43:989–1010.
- Foster K. Clinical guidelines in the management of burn injury: a review and recommendations from the organization and delivery of burn care committee. J Burn Care Res 2014;35:271–83.
- Nedelec B, Carter A, Forbes L, et al. Practice guidelines for the application of nonsilicone or silicone gels and gel sheets after burn injury. J Burn Care Res 2015;36:345–374.
- Cancio L, Barillo D, Kearns R, et al. Guidelines for burn care under austere conditions. J Burn Care Res 2017;38:203–214.
- Munn Z. Evidence summary. Burns first aid: inappropriate treatments. JBI EBP Database 2021;JBI-ES-1635-1.
- Gyi AA. Evidence summary. Burn injuries: cooling burns with water. JBI EBP Database 2021.
- Moola S, Magtoto LS. Evidence summary. Scalds: first aid management. JBI EPP Database 2021;JBI-ES-532-1.
- Minooee S. Evidence summary. Burns pain (adult): nonpharmacological interventions. JBI EBP Database 2021;JBI-ES-1519-1.
- Moola S. Evidence summary. Burn patients: music. JBI EBP Database 2021;JBI-ES-2054-1.
- Munn Z. Evidence summary. Burns rehabilitation: virtual reality. JBI EBP Database 2021;JBI-ES-1896-1.
- Manuel B. Evidence summary. Burns: pruritus (itch). JBI EBP Database 2020;JBI-ES-2096-1.
- Munn Z. Evidence summary. Burn injuries: recombinant human growth hormone. JBI EBP Database 2021;JBI-ES-623-1.
- Campbell J. Evidence summary. Dermal burns: growth factor therapy. JBI EBP Database 2021.
- Moola S. Evidence summary. Biosynthetic skin substitutes: burns/wounds care. JBI EBP Database 2021;JBI-ES-3332-1.
- Ishaque S. Evidence summary. Burn wounds: aloe vera. JBI EBP Database 2021.
- Fong E. Evidence summary. Superficial and partial thickness burn injuries: dressings. JBI EBP Database 2021.
- Dorri M. Evidence summary. Burns and donor sites: film dressings. JBI EBP Database 2021.
- Munn Z, Magtoto LS. Evidence summary. Hydrocolloids: burn wounds and donor sites. JBI EBP Database 2020;JBI-ES-3773-1.
- Moola S. Evidence summary. Partial thickness burn injuries: hydrofiber dressings. JBI EBP Database 2020;JBI-ES-2422-1.
- Gyi AA. Evidence summary. Facial burn: topical treatments. JBI EBP Database 2021.
- Rathnayake T, Mathew S. Evidence summary. Use of Tumescent technique in burn surgery. JBI EBP Database 2021;JBI-ES-3257-1.
- Le LK-D. Evidence summary. Tumescence during burn surgery. JBI EBP Database 2021;JBI-ES-2938-2.
- Manuel B. Evidence summary. Burns surgery: early excision and debridement. JBI EBP Database 2020;JBI-ES-2107-1.
- Moola S. Evidence summary. Postoperative split-thickness skin graft care in the burns unit: nursing management. JBI EBP Database 2021;JBI-ES-1891-1.
- Munn Z. Evidence summary. Hand burns: surgery. JBI EBP Database 2021;JBI-ES-1898-1.
- Munn Z, Minooee S. Evidence summary. Axilla burns: post-surgical care. JBI EBP Database 2021;JBI-ES-388-1.
- Moola S, Fong E. Evidence summary. Burns: silver-based antiseptics. JBI EBP Database 2020;JBI-ES-2090-1.
- Nnaji C. Evidence summary. Dressing changes (burns): hydrotherapy. JBI EBP Database 2019;JBI-ES-2870-1.
- Moola S. Evidence summary. Burns: blister management. JBI EBP Database 2021;JBI-ES-1248-1.
- Carstens J, Minooee S. Evidence summary. Burns: topical negative pressure. JBI EBP Database 2021.
- Munn Z, Johnston S. Evidence summary. Burn units: preparation for transfer. JBI EBP Database 2019;JBI-ES-3013-2.
- Munn Z, Moola S. Evidence summary. Burns injury follow up: use of telemedicine. JBI EBP Database 2019;JBI-ES-2783-1.
- Moola S. Evidence summary. Acute burn wounds: extracorporeal shock wave therapy. JBI EBP Database 2021;JBI-ES-645-1.
- Munn Z, Fong E. Evidence summary. Burns nutrition: micronutrients. JBI EBP Database 2019;JBI-RP-4395-1.
- Munn Z, James S. Evidence summary. Burns nutrition: immunonutrients. JBI EBP Database 2019;JBI-ES-3043-2.
- Campbell J. Evidence summary. Burn nursing: model of care. JBI EBP Database 2021.
- Munn Z. Evidence summary. Liquefiel petroleum gas burns: management. JBI EBP Database 2021;JBI-ES-1764-1.
- Munn Z, Moola S. Evidence summary. Cement burns: treatment. JBI EBP Database 2019;JBI-ES-2727-1.
- Battaloglu E, Greasley L, Leon-Villapalos J, Young A, Porter K. Management of burns in pre-hospital trauma care. British Burns Association 2019. Available from: https://fphc.rcsed.ac.uk/media/2621/burns-consensus-2019.pdf.
- British Burns Association. First aid clinical practice guidelines. British Burns Association; 2018.
- Hughes A, Almeland SK, Leclerc T, et al. Recommendations for burns care in mass casualty incidents: WHO Emergency Medical Teams Technical Working Group on Burns (WHO TWGB) 2017–2020. Burns 2021;47:349–370.
- Hirche C, Kreken Almeland S, Dheansa B, et al. Eschar removal by bromelain based enzymatic debridement (Nexobrid®) in burns: European consensus guidelines update. Burns 2020;46:782–796.
- Muller MJ, Dulhunty JM, Paratz JD, Harrison JM, Redman BR. Don’t be a flamin’ fool: effectiveness of an adult burn prevention media campaign in two regions in Queensland, Australia – an interventional study. J Trauma Acute Care Surg 2013;74:652–657.
- Khalil H, Cullen M, Chambers H, McGrail M. Medications affecting healing: an evidence-based analysis. Int Wound J 2017;14:1340–1345.
- Wounds Australia. Standards for wound prevention and management, 3rd edition. Wounds Australia; 2016.
- Rando T, Kang AC, Guerin M, Boylan J, Dyer A. Simplifying wound dressing selection for residential aged care. J Wound Care 2018;27:504–511.
- Birke-Sorensen H, Malmsjo M, Rome P, et al. Evidence-based recommendations for negative pressure wound therapy: treatment variables – steps towards an international consensus. J Plast Recon Aesth Surg 2011;64:S1-S16.
- Podder V. Evidence summary. Wound management: overview of mechanical debridement. JBI EBP Database 2019;JBI-ES-2642-1.
- Gyi AA. Evidence summary. Wound management: chemical debridement (Dakin’s solution). JBI EBP Database 2019;JBI-ES-3233-2.
- Moola S. Evidence summary. Pain management during wound care: wound care technique. JBI EBP Database 2021;JBI-ES-1607-1.
- Jayasekara R. Evidence summary. Wound management: assessment of pain during dressing change. JBI EBP Database 2021.
- Moola S. Evidence summary. Pain management during wound care: non-pharmacological adjunct interventions. JBI EBP Database 2021;JBIES-1625-1.
- Munn Z, Magtoto LS. Evidence summary. Alginate dressings: burn wounds and donor sites. JBI EBP Database 2020;JBI-ES-67-1.
- Sivapuram MS. Evidence summary. Wound infection: iodophors and biofilms. JBI EBP Database 2021.
- Koh G. Evidence summary. Wound management: dressing. JBI EBP Database 2021.
- Khanh-Dao Le L. Evidence summary. Minor acute wounds: medical-grade honey. JBI EBP Database 2021.
- Sivapuram MS. Evidence summary. Wound management: dressings – alginate. JBI EBP Database 2019;JBI-ES-3506-1.
- Le LK-D. Evidence summary. Wound care: wet-to-moist dressings. JBI EBP Database 2020;JBI-ES-2115-1.
- Gyi AA. Evidence summary. Wet-to-dry saline moistened gauze for wound dressing. JBI EBP Database 2019.
- Moola S. Evidence summary. Wound management (low resource countries) – banana leaf dressing. JBI EBP Database 2019;JBI-ES-4037-1.
- Deakin L. Evidence summary. Nanocrystalline silver dressing for wounds (other than burns and donor cites). JBI EBP Database 2020;JBIES-2163-1.
- Nguyen DH. Evidence summary. Wound management (low resource countries): hypochlorite solutions. JBI EBP Database 2020;JBI-ES-2162-1.
- Oerlemans S. Evidence summary. Wound management: hydrogen peroxide. JBI EBP Database 2019;JBI-ES-2913-1.
- Sivapuram MS. Evidence summary. Wound specimens: techniquest for identification of infections. JBI EBP Database 2021.
- Apelqvist J, Willy C, Fagerdah AM, et al. Negative pressure wound therapy. Overview, challenges and perspectives J Wound Care 2017;6.
- Kim PJ, Attinger CE, Crist BD, et al. Negative pressure wound therapy with instillation: review of evidence and recommendations. Ost Wound Manag 2015;2–19.
- Strohal R, Apelqvist J, Dissemond J, et al. Debridement. An updated overview and clarification of the principle role of debridement. J Wound Care 2013;22:S1-S52.
- Wounds UK. Best practice statement: effective exudate management. Wounds UK; 2013.
- World Union of Wound Healing Societies. Consensus document. Wound exudate: effective assessment and management. Wounds International; 2019.
- International Wound Infection Institute. Wound infection in clinical practice: principles of best practice. Wounds International; 2016.
- World Union of Wound Healing Societies. The role of non-medicated dressings for the management of wound infection. Wounds International; 2020.
- Wounds Australia. Application of aseptic technique in wound dressing procedure: a consensus document, 3rd edition; Wounds Australia 2020, https://woundsaustralia.org
- Wounds UK. Consensus round table meeting: Using Ag OxysaltsTM to prevent and manage wound infection. Wounds UK; 2018.
- Wounds UK. Best practice statement: antimicrobial stewardship strategies for wound management. Wounds UK; 2020.
- Wounds UK. Best practice statement: the use of topical antimicrobial agents in wound management. Wounds UK; 2013.
- Wounds UK. Best practice statement: the use of topical antiseptic/antimicrobial agents in wound management, 2nd edition. Wounds UK; 2011.
- Ousey K, Atkin L, Conway B, et al. Wound care and dressing selection for pharmacy teams. Wounds UK; 2021.
- Wu S, Applewhite AJ, Niezgoda J, et al. Oxidized regenerated cellulose/collagen dressings: review of evidence and recommendations. Adv Skin Wound Care 2017;30:S1-S18.
- Wounds International. International consensus: appropriate use of silver dressings in wounds. Wounds International; 2012.
- Piaggesi A, Läuchli S, Bassetto F, et al. EWMA document: advanced therapies in wound management. J Wound Care 2018;27.
- Sivapuram MS. Evidence summary. Scar management: taping. JBI EBP Database 2019;JBI-ES-3120-3.
- Moore Z, Butcher G, Corbett LQ, McGuiness W, Snyder RJ, Van Acker K. Managing wounds as a team. J Wound Care 2014;23:S1-S38.
- Edwards HE, Chang AM, Gibb M, et al. Reduced prevalence and severity of wounds following implementation of the Champions for Skin Integrity model to facilitate uptake of evidence-based practice in aged care. J Clin Nurs 2017;26:4276–4285.
- Hekmatpou D, Mehrabi F, Rahzani K, Aminiyan A. The effect of aloe vera clinical trials on prevention and healing of skin wound: a systematic review. Iranian J Med Sci 2019;44:1–9.
- Hauck YL, Lewis L, Nathan EA, White C, Doherty DA. Risk factors for severe perineal trauma during vaginal childbirth: a Western Australian retrospective cohort study. Women Birth 2015;28:16–20.
- Zeki R, Li Z, Wang AY, et al. Obstetric anal sphincter injuries among women with gestational diabetes and women without gestational diabetes: a NSW population-based cohort study. Aus NZ J Obstet Gynae 2019;59:662–669.
- Pergialiotis V, Bellos I, Fanaki M, Vrachnis N, Doumouchtsis SK. Risk factors for severe perineal trauma during childbirth: an updated meta-analysis. Euro J Obstet Gyne Reprod Biol 2020;247:94–100.
- Liu DS, Sofiadellis F, Ashton M, Macgill K, Webb A. Early soft tissue coverage and negative pressure wound therapy optimises patient outcomes in lower limb trauma. Injury 2012;43:772–778.
- Blum ML, Esser M, Richardson M, Paul E, Rosenfeldt FL. Negative pressure wound therapy reduces deep infection rate in open tibial fractures. J Ortho Trauma 2012;26:499–505.
- Lee HX, Hauser M, Jog S, Bautz P, Dobbins C. Non-operative management of isolated single abdominal stab wound: is it safe? ANZ J Surg 2018;88:565–568.
- Majer J, Valentine S, Warren J, et al. Outcomes of laceration suture repair in the emergency department. EMA 2021;33:242–249.
- Priddis HS, Schmied V, Kettle C, Sneddon A, Dahlen HG. “A patchwork of services” – caring for women who sustain severe perineal trauma in New South Wales – from the perspective of women and midwives. BMC Preg Childbirth 2014;14:236.
- Swift A, Webster J, Conroy AM, et al. Curved versus straight scissors to avoid 3rd and 4th degree perineal tears: a randomised feasibility study. Women Birth 2014;27:163–167.
- Krug E, Berg L, Lee C, et al. Evidence-based recommendations for the use of negative pressure wound therapy in traumatic wounds and reconstructive surgery: steps towards an international consensus. Injury 2011;42 Suppl 1:S1–S12.
- Sivapuram MS. Evidence summary. Primary wound closure: community settings. JBI EBP Database 2020;JBI-ES-2198-1.
- Nguyen P. Evidence summary. Risk of infection during birth: perineal shaving. JBI EBP Database 2019;JBI-ES-2873-2.
- Childs C, Sandy-Hodgett K, Broad C, Cooper R, Manresa M, Verdu-Soriano J. European Wound Management Association. Birth-related wounds: risk, prevention and management of complications after vaginal and Caesarian section birth. J Wound Care 2020;29:S2-S42.
- Kamisan Atan I, Shek KL, Langer S, et al. Does the Epi-No® birth trainer prevent vaginal birth-related pelvic floor trauma? A multicentre prospective randomised controlled trial. BJOG 2016;123:995–1003.
- Whitehorn A. Evidence summary. Medical adhesive injury: prevention. JBI EBP Database 2021.
- Miles SJ, Fulbrook P, Williams DM. Skin tear prevalence in an Australian acute care hospital: a 10-year analysis. Int Wound J 2021.
- Brimelow RE, Wollin JA. The impact of care practices and health demographics on the prevalence of skin tears and pressure injuries in aged care. J Clin Nurs 2018;27:1519–1528.
- Van Tiggelen H, LeBlanc K, Campbell K, et al. Standardizing the classification of skin tears: validity and reliability testing of the International Skin Tear Advisory Panel Classification System in 44 countries. Br J Dermatol 2020;183:146–154.
- Munro EL, Hickling DF, Williams DM, Bell JJ. Malnutrition is independently associated with skin tears in hospital inpatient setting: findings of a 6-year point prevalence audit. Int Wound J 2018;15:527–533.
- Lewin GF, Newall N, Alan JJ, Carville KJ, Santamaria NM, Roberts PA. Identification of risk factors associated with the development of skin tears in hospitalised older persons: a case-control study. Int Wound J 2016;13:1246–1251.
- Rayner R, Carville K, Leslie G, Dhaliwal SS. Skin tear risks associated with aged care residents: a cross-sectional study. Wound Prac Res 2018;26:127–135.
- Rayner RL, Carville K, Leslie G, Dhaliwal SS. A risk model for the prediction of skin tears in aged care residents: a prospective cohort study. Int Wound J 2019;16:52–63.
- Rayner RL, Carville KJ, Leslie GD, Dhaliwal SS. Clinical purpura and elastosis and their correlation with skin tears in an aged population. Arch Dermatol Res 2019;311:231–247.
- Rayner R, Carville K, Leslie G, Dhaliwal SS. Measurement of morphological and physiological skin properties in aged care residents: a test–retest reliability pilot study. Int Wound J 2017;14:420–429.
- Newall N, Lewin GF, Bulsara MK, Carville KJ, Leslie GD, Roberts PA. The development and testing of a skin tear risk assessment tool. Int Wound J 2017;14:97–103.
- Rayner R, Carville K, Leslie G, Dhaliwal SS. Models for predicting skin tears: a comparison. Int Wound J 2020;17:823–830.
- Serra R, Ielapi N, Barbetta A, de Franciscis S. Skin tears and risk factors assessment: a systematic review on evidence-based medicine. Int Wound J 2018;15:38–42.
- Moola S. Evidence summary. Skin tears (community setting): assessment. JBI EBP Database 2021.
- LeBlanc K, Baranoski S, Christensen D, et al. International Skin Tear Advisory Panel: a tool kit to aid in the prevention, assessment, and treatment of skin tears using a simplified classification system. Adv Skin Wound Care 2013;26.
- LeBlanc K, Campbell K, Beeckman B, et al. ISTAP best practice recommendations for the prevention and management of skin tears in aged skin. Wounds International; 2018.
- Vandervord JG, Tolerton SK, Campbell PA, Darke JM, Loch-Wilkinson A-MV. Acute management of skin tears: a change in practice pilot study. Int Wound J 2016;13:59–64.
- Lopez V, Dunk AM, Cubit K, et al. Skin tear prevention and management among patients in the acute aged care and rehabilitation units in the Australian Capital Territory: a best practice implementation project. Int J EB Healthcare 2011;9:429–434.
- Beechey R, Priest L, Peters M, Moloney C. An evidence-based approach to the prevention and initial management of skin tears within the aged community setting: a best practice implementation project. JBI Database SRIRs 2015;13:421–443.
- LeBlanc K, Woo K, Christensen D, et al. Best practice recommendations for the prevention and management of skin tear. In Foundations of best practice for skin and wound management. Wounds Canada; 2017.
- Mathew S. Evidence summary. Skin tears (community setting): management. JBI EBP Database 2021.
- Wounds UK. Best practice statement: management of lower limb skin tears in adults. Wounds UK; 2020.
- LeBlanc K, Baranoski S, Christensen D, et al. The art of dressing selection: a consensus statement on skin tears and best practice. Adv Skin Wound Care 2016;29:32–46.
- Carville K, Leslie G, Osseiran-Moisson R, Newall N, Lewin G. The effectiveness of a twice-daily skin-moisturising regimen for reducing the incidence of skin tears. Int Wound J 2014;11:446–453.
- Mornane C, Peck B, Terry D, Ryan M. Twice-daily moisturizer application for skin tear prevention among older adults in acute care. Adv Skin Wound Care 2021;34:1–4.
- Finch K, Osseiran-Moisson R, Carville K, Leslie G, Dwyer M. Skin tear prevention in elderly patients using twice-daily moisturiser. Wound Prac Res 2018;26:99–109.
- Moffat AK, Westaway KP, Apajee J, et al. Impact of a patient-specific national programme aimed at increasing the use of emollient moisturisers to reduce the risk of skin tears: a longitudinal cohort study. BMJ Open 2020;10.
- Cowdell F, Jadotte YT, Ersser SJ, et al. Hygiene and emollient interventions for maintaining skin integrity in older people in hospital and residential care settings. Cochrane Database Syst Rev 2020.
- Wounds UK. Best practice statement. Care of the older person’s skin. Wounds UK; 2012.
- Wounds UK. Best practice statement: maintaining skin integrity. Wounds UK; 2018.
- Beeckman D, Jill Campbell J, LeBlanc K, et al. Best practice recommendations for holistic strategies to promote and maintain skin integrity. Wounds International; 2020.
- Australian Institute of Health and Welfare (AIHW). Australia’s hospitals at a glance. Canberra: AIHW; 2022.
- Toppi J, Cleland H, Gabbe B. Severe burns in Australian and New Zealand adults: epidemiology and burn centre care. Burns 2019;45:1456–1461.
- Bui UT, Tehan P, Baraket-Johnson M, et al. Assessment, management and prevention of chronic wounds in the Australian context: a scoping review. Wound Res Pract 2023;31:120–145.
- Delpachitra M, Heal C, Banks J, Charles D, Sriharan S, Buttner P. Risk factors for surgical site infection after minor dermatologic surgery. Adv Skin Wound Care 2021;34:43–48.
- Carroll K, Dowsey M, Choong P, Peel T. Risk factors for superficial wound complications in hip and knee arthroplasty. Clin Microbiol Inf 2014;20:130–135.
- Bagheri N, Furuya-Kanamori L, Doi SAR, Clements ACA, Sedrakyan A. Geographical outcome disparities in infection occurrence after colorectal surgery: an analysis of 58,096 colorectal surgical procedures. Int J Surg 2017;44:117–121.
- Asaid R, Williams I, Hyde D, Tiang T. Infection rates following hip and knee joint arthroplasty: large referral centre versus a small elective-only hospital. Euro J Ortho Surg Trauma 2013;23:165–168.
- Gearing PF, Daly JF, Tang NSJ, Singh K, Ramakrishnan A. Risk factors for surgical site infection in free-flap reconstructive surgery for head and neck cancer: retrospective Australian cohort study. Head Neck 2021;43:3417–3428.
- Ali U, Bibo L, Pierre M, et al. Deep sternal wound infections after cardiac surgery: a new Australian tertiary centre experience. Heart Lung Circ 2020;29:1571–1578.
- Henman K, Gordon CL, Gardiner T, et al. Surgical site infections following Caesarean section at Royal Darwin Hospital, Northern Territory. Healthcare Inf 2012;17:47–51.
- Cheuk N, Worth LJ, Tatoulis J, Skillington P, Kyi M, Fourlanos S. The relationship between diabetes and surgical site infection following coronary artery bypass graft surgery in current-era models of care. J Hosp Inf 2021;116:47–52.
- Betts KS, Kisely S, Alati R. Predicting common maternal postpartum complications: leveraging health administrative data and machine learning. BJOG 2019;126:702–709.
- Gurunathan U, Rapchuk IL, Dickfos M, et al. Association of obesity with septic complications after major abdominal surgery: a secondary analysis of the RELIEF randomized clinical trial. JAMA Network Open 2019;2.
- Floros P, Sawhney R, Vrtik M, et al. Risk factors and management approach for deep sternal wound infection after cardiac surgery at a tertiary medical centre. Heart Lung Circ 2011;20:712–717.
- Penington A. Ulceration and antihypertensive use are risk factors for infection after skin lesion excision. ANZ J Surg 2010;80:642–645.
- Peel TN, Dowsey MM, Daffy JR, Stanley PA, Choong PFM, Buising KL. Risk factors for prosthetic hip and knee infections according to arthroplasty site. J Hosp Inf 2011;79:129–133.
- Corcoran TB, Myles PS, Forbes AB, et al. Dexamethasone and surgical-site infection. New Eng J Med 2021;384:1731–1741.
- McDougall CJ, Gray HS, Simpson PM, Whitehouse SL, Crawford RW, Donnelly WJ. Complications related to therapeutic anticoagulation in total hip arthroplasty. J Arthroplasty 2013;28:187–192.
- Schipmann S, Akalin E, Doods J, Ewelt C, Stummer W, Suero Molina E. When the infection hits the wound: matched case-control study in a neurosurgical patient collective including systematic literature review and risk factors analysis. World Neurosurg 2016;95:178–189.
- Baroun-Agob L, Liew S, Gabbe B. Risk factors for surgical site infections following spinal column trauma in an Australian trauma hospital. ANZ J Surg 2021;91:639–646.
- Worth LJ, Bull AL, Richards MJ. Reporting surgical site infections following primary and revision hip arthroplasty – one size does not fit all. Inf Control Hosp Epidemiol 2011;32:296–297.
- Heal CF, Buettner PG, Drobetz H. Risk factors for surgical site infection after dermatological surgery. Int J Dermatol 2012;51:796–803.
- Badiani S, Diab J, Woodford E, Natarajan P, Berney CR. Impact of preoperative smoking on patients undergoing right hemicolectomies for colon cancer. Langenbeck’s Arch Surg 2022.
- Cheng D, Bonato L, Leinkram C. Infection and recurrence rates of the C-QUR V-Patch™ in ventral hernia repairs. Hernia 2018;22:767–772.
- Jacombs ASW, Rome P, Harrison JD, Solomon MJ. Assessment of the selection process for myocutaneous flap repair and surgical complications in pelvic exenteration surgery. Br J Surg 2013;100:561–567.
- Deek RP, Lee IOK, van Essen P, Crittenden T, Dean NR. Predicted versus actual complications in Australian women undergoing post-mastectomy breast reconstruction: a retrospective cohort study using the BRA Score tool. JPRAS 2021;74:3324–3334.
- Sandy-Hodgetts K, Carville K, Santamaria N, Parsons R, Leslie GD. The Perth Surgical Wound Dehiscence Risk Assessment Tool (PSWDRAT): development and prospective validation in the clinical setting. J Wound Care 2019;28:332–344.
- Stankiewicz M, Coyer F, Webster J, Osborne S. Incidence and predictors of lower limb split-skin graft failure and primary closure dehiscence in day-case surgical patients. Dermatol Surg 2015;41:775–783.
- Kim B, Sgarioto M, Hewitt D, Paver R, Norman J, Fernandez-Penas P. Scar outcomes in dermatological surgery. Australas J Dermatol 2018;59:48–51.
- Peel TN, Dowsey MM, Buising KL, Cheng AC, Choong PFM. Chlorhexidine-alcohol versus iodine-alcohol for surgical site skin preparation in an elective arthroplasty (ACAISA) study: a cluster randomized controlled trial. Clin Microbiol Inf 2019;25:1239–1245.
- Wade RG, Bourke G, Wormald JCR, et al. Chlorhexidine versus povidone-iodine skin antisepsis before upper limb surgery (CIPHUR): an international multicentre prospective cohort study. BJS Open 2021;5.
- Charles D, Heal CF, Delpachitra M, et al. Alcoholic versus aqueous chlorhexidine for skin antisepsis: the AVALANCHE trial. CMAJ 2017;189:e1008–e1016.
- Reid FS, Stephensen B, Carroll R, Lott N, Attia J, Smith S. Antiseptic skin preparation agents to prevent surgical site infection in colorectal surgery: a three-armed randomized clinical trial. Dis Colon Rectum 2022; 65: 1391-1396.
- Smith H, Borchard K, Cherian P, Tai Y, Vinciullo C. Randomized controlled trial of preoperative topical decolonization to reduce surgical site infection for Staphylococcus aureus nasal swab-negative mohs micrographic surgery patients. Dermatol Surg 2019;45:229–233.
- Cherian P, Gunson T, Borchard K, Tai Y, Smith H, Vinciullo C. Oral antibiotics versus topical decolonization to prevent surgical site infection after mohs micrographic surgery – a randomized, controlled trial. Dermatol Surg 2013;39:1486–1493.
- Chow J, Ng J, Pun A. Effects of food colouring added to 2% chlorhexidine gluconate and 70% alcohol for surgical site antisepsis. J Periop Pract 2013;23:255–257.
- Walker SR, Smith A. Randomized, blinded study to assess the effect of povidone-iodine on the groin wound of patients undergoing primary varicose vein surgery. ANZ J Surg 2013;83:844–846.
- Rosengren H, Heal CF, Buttner PG. Effect of a single prophylactic preoperative oral antibiotic dose on surgical site infection following complex dermatological procedures on the nose and ear: a prospective, randomised, controlled, double-blinded trial. BMJ Open 2018;8:e020213.
- Brown J, Thompson M, Sinnya S, et al. Pre-incision antibiotic prophylaxis reduces the incidence of post-Caesarean surgical site infection. J Hosp Inf 2013;83:68–70.
- Butterworth P, Terrill A, Barwick A, Hermann R. The use of prophylactic antibiotics in podiatric foot and ankle surgery. Inf Dis Health 2017;22:6–11.
- Merollini KMD, Zheng H, Graves N. Most relevant strategies for preventing surgical site infection after total hip arthroplasty: guideline recommendations and expert opinion. Am J Inf Control 2013;41:221–226.
- Rosengren H, Heal CF, Buettner PG. Effect of a single preoperative dose of oral antibiotic to reduce the incidence of surgical site infection following below-knee dermatological flap and graft repair. Dermatol Pract Concept 2019;9:28–35.
- Zhao AH, Kwok CHR, Jacques A, et al. Gentamicin-containing collagen implant may reduce surgical site infections after open infrainguinal arterial revascularization. Ann Vasc Surg 2022;78:84–92.
- Heal C, Lepper P, Banks J. Topical antibiotics to prevent surgical site infection after minor surgery in primary care. Dermatol Pract Concept 2017;7:16–20.
- Badge H, Churches T, Xuan W, Naylor JM, Harris IA. Timing and duration of antibiotic prophylaxis is associated with the risk of infection after hip and knee arthroplasty. Bone Joint Open 2022;3:252–260.
- Badres IA, Suen K, Tran P. Effect of wound closure technique in proximal femoral fractures: a prospective cohort study. J Orth Trauma 2020;34:553–558.
- Dunne B, Murphy M, Skiba R, et al. Sternal cables are not superior to traditional sternal wiring for preventing deep sternal wound infection. Inter Cardiovasc Thoracic Surg 2016;22:594–598.
- Reid K, Pockney P, Draganic B, Smith SR. Barrier wound protection decreases surgical site infection in open elective colorectal surgery: a randomized clinical trial. Dis Colon Rectum 2010;53:1374–1380.
- Morrison EJ, Shoukath S, Tansley P, Grinsell D. Donor site morbidity of an islanded inferior gluteal artery myocutaneous flap with vascularized fascia lata. J Plastic Reconstruct Aesth Surg 2013;66:962–967.
- Iyer A, Gilfillan I, Thakur S, Sharma S. Reduction of surgical site infection using a microbial sealant: a randomized trial. J Thor Cardiovasc Surg 2011;142:438–442.
- Heal C, Sriharan S, Buttner PG, Kimber D. Comparing non-sterile to sterile gloves for minor surgery: a prospective randomised controlled non-inferiority trial. Med J Aust 2015;202:27–31.
- Webster J, Croger S, Lister C, Doidge M, Terry MJ, Jones I. Use of face masks by non-scrubbed operating room staff: a randomized controlled trial. ANZ J Surg 2010;80:169–173.
- Mahomed K, Ibiebele I, Buchanan J. The Betadine trial – antiseptic wound irrigation prior to skin closure at Caesarean section to prevent surgical site infection: a randomised controlled trial. Aus NZ J Obstet Gynae 2016;56:301–306.
- Nikfarjam M, Weinberg L, Fink MA, et al. Pressurized pulse irrigation with saline reduces surgical-site infections following major hepatobiliary and pancreatic surgery: randomized controlled trial. World J Surg 2014;38:447–455.
- Zhou HB, Wu Y, Wang LQ, Zou SL, Qiao YZ, Wang LX. Feasibility and safety of early removal of incisional dressings following thoracic surgery. Med Princ Pract 2012;21:379–382.
- Liu DS, Cheng C, Islam R, et al. Prophylactic negative-pressure dressings reduce wound complications and resource burden after emergency laparotomies. J Surg Res 2021;257:22–31.
- Di Re W, D., Toh JW, El-Khoury T, et al. Surgical wound infection prevention using topical negative pressure therapy on closed abdominal incisions – the ‘SWIPE IT’ randomized clinical trial. J Hosp Inf 2021;110:76–83.
- Pickles S, McAllister E, McCullagh G, Nieroba T-J. Quality improvement evaluation of postoperative wound dressings in orthopaedic patients. Int J Orth Trauma Nurs 2022;45:100922.
- Wang J, Chapman Z, Cole E, et al. Use of closed incision negative pressure therapy (ciNPT) in breast reconstruction abdominal free flap donor sites. J Clin Med 2021;10.
- Gillespie BM, Webster J, Ellwood D, et al. Closed incision negative pressure wound therapy versus standard dressings in obese women undergoing Caesarean section: multicentre parallel group randomised controlled trial. BMJ 2021;373:n893.
- Flynn J, Choy A, Leavy K, et al. Negative pressure dressings (PICOTM) on laparotomy wounds do not reduce risk of surgical site infection. Surg Inf 2020;21:231–238.
- Danne J, Gwini S, McKenzie D, Danne P. A retrospective study of pilonidal sinus healing by secondary intention using negative pressure wound therapy versus alginate or gauze dressings. Ost Wound Manag 2017;63:47–53.
- Obermair H, Janda M, Obermair A. Real-world surgical outcomes of a gelatin-hemostatic matrix in women requiring a hysterectomy: a matched case-control study. Acta Obstet Gyne Scand 2016;95:1008–1014.
- Manoharan V, Grant AL, Harris AC, Hazratwala K, Wilkinson MPR, McEwen PJC. Closed incision negative pressure wound therapy vs conventional dry dressings after primary knee arthroplasty: a randomized controlled study. J Arthroplasty 2016;31:2487–2494.
- Martin E, Beckmann M, Blythe R, Merollini K, Graves N. Adherence to best practice: preventing surgical site infection following Caesarean section in Australia. Aus NZ J Obstet Gynae 2021;61:728–734.
- Chandrananth J, Rabinovich A, Karahalios A, Guy S, Tran P. Impact of adherence to local antibiotic prophylaxis guidelines on infection outcome after total hip or knee arthroplasty. J Hosp Inf 2016;93:423–427.
- Badge HM, Churches T, Naylor JM, et al. Non-compliance with clinical guidelines increases the risk of complications after primary total hip and knee joint replacement surgery. PloS One 2021;16:e0260146.
- Bolte M, Knapman B, Leibenson L, Ball J, Giles M. Reducing surgical site infections post-Caesarean section in an Australian hospital, using a bundled care approach. Inf Dis Health 2020;25:158–167.
- Faragher I, Tham N, Hong M, Guy S, Yeung J. Implementation of an organ space infection prevention bundle reduces the rate of organ space infection after elective colorectal surgery. BMJ Open 2021;10.
- Burgess A, Fish M, Goldberg S, Summers K, Cornwell K, Lowe J. Surgical-site infection prevention after hysterectomy: use of a consensus bundle to guide improvement. J Healthcare Qual 2020;42:188–194.
- Shakeshaft AJ, Scanlon K, Eslick GD, Azmir A, Cox MR. Post-operative glycaemic control using an insulin infusion is associated with reduced surgical site infections in colorectal surgery. World J Surg 2020;44:3491–3500.
- Phan K, Schultz K, Huang C, et al. External ventricular drain infections at the Canberra Hospital: a retrospective study. J Clin Neurosci 2016;32:95–98.
- Barnett AG, Page K, Campbell M, et al. Changes in healthcare-associated infections after the introduction of a national hand hygiene initiative. Healthcare Inf 2014;19:128–134.
- Schmidt HMA, Izon C, Maley MW. Demographic screening for MRSA may compromise the effectiveness of ring fencing on a joint replacement unit. J Hosp Inf 2012;82:207–209.
- Daly JF, Gearing PF, Tang NSJ, Ramakrishnan A, Singh KP. Antibiotic prophylaxis prescribing practice in head and neck tumor resection and free flap reconstruction. Open Forum Inf Dis 2021;9:ofab590.
- Stupart DA, Sim FW, Chan ZH, Guest GD, Watters DA. Cautery versus scalpel for abdominal skin incisions: a double blind, randomized crossover trial of scar cosmesis. ANZ J Surg 2016;86:303–306.
- Danielsen PL, Gankande TU, Rea SM, et al. Verapamil is less effective than triamcinolone for prevention of keloid scar recurrence after excision in a randomized controlled trial. Acta Derm Ven 2016.
- Koide S, Smoll NR, Liew J, et al. A randomized ‘N-of-1’ single blinded clinical trial of barbed dermal sutures vs. smooth sutures in elective plastic surgery shows differences in scar appearance two-years post-operatively. J Plast Reconstr Aesth Surg 2015;68:1003–1009.
- Goltsman D, Li Z, Bruce E, Maitz PKM. Geospatial and epidemiological analysis of severe burns in New South Wales by residential postcodes. Burns 2014;40:670–682.
- Duke J, Rea S, Semmens J, Wood F. Urban compared with rural and remote burn hospitalisations in Western Australia. Burns 2012;38:591–598.
- Gabbe BJ, Watterson DM, Singer Y, Darton A. Outpatient presentations to burn centers: data from the Burns Registry of Australia and New Zealand outpatient pilot project. Burns 2015;41:446–453.
- Duke J, Wood F, Semmens J, et al. Rates of hospitalisations and mortality of older adults admitted with burn injuries in Western Australian from 1983 to 2008. Australas J Ageing 2012;31:83–89.
- Harvey LA, Connolley S, Harvey JG. Clothing-related burns in New South Wales, Australia: impact of legislation on a continuing problem. Burns 2015;41:58–64.
- Aggarwal S, Maitz P, Kennedy P. Electrical flash burns due to switchboard explosions in New South Wales – a 9-year experience. Burns 2011;37:1038–1043.
- O’Neill TB, Rawlins JM, Rea S, Wood FM. Methamphetamine laboratory-related burns in Western Australia – why the explosion? Burns 2011;37:1044–1048.
- Alexander W, Coghlan P, Greenwood J. A ten-year retrospective analysis of cement burns in a tertiary burns center. J Burn Care Res 2014;35:80–83.
- Singer Y, Tracy LM, Menezes H, et al. “The home, the bathroom, the taps, and hot water”: the contextual characteristics of tap water scalds in Australia and New Zealand. Burns 2021.
- Duke J, Wood F, Semmens J, et al. A 26-year population-based study of burn injury hospital admissions in Western Australia. J Burn Care Res 2011;32:379–386.
- Duke J, Wood F, Semmens J, Edgar DW, Spilsbury K, Rea S. An assessment of burn injury hospitalisations of adolescents and young adults in Western Australia, 1983–2008. Burns 2012;38:128–135.
- Cleland H, Fernando DT, Gabbe BJ. Trends in Victorian burn injuries 2008–2017. Burns 2022;48:703–712.
- Murphy L, Read D, Brennan M, Ward L, McDermott K. Burn injury as a result of interpersonal violence in the Northern Territory Top End. Burns 2019;45:1199–1204.
- McInnes JA, Cleland H, Tracy LM, et al. Epidemiology of work-related burn injuries presenting to burn centres in Australia and New Zealand. Burns 2019;45:484–493.
- McInnes JA, Cleland HJ, Cameron PA, et al. Epidemiology of burn-related fatalities in Australia and New Zealand, 2009–2015. Burns 2019;45:1553–1561.
- Randall SM, Wood FM, Boyd JH, Duke JM. Geographic distribution of burn in an Australian setting. Burns 2017;43:1575–1585.
- Wood R. Self-inflicted burn injuries in the Australian context. Australas Psych 2014;22:393–396.
- Lawrence E, Li F. Foot burns and diabetes: a retrospective study. Burns Trauma 2015;3:24.
- Tracy LM, Singer Y, Schrale R, et al. Epidemiology of burn injury in older adults: an Australian and New Zealand perspective. Scars Burns Heal 2020;6:2059513120952336.
- Lang TC, Zhao R, Kim A, et al. Plasma protein C levels are directly associated with better outcomes in patients with severe burns. Burns 2019;45:1659–1672.
- Zhao R, Lang TC, Kim A, et al. Early protein C activation is reflective of burn injury severity and plays a critical role in inflammatory burden and patient outcomes. Burns 2022;48:91–103.
- Park JH, Heggie KM, Edgar DW, Bulsara MK, Wood FM. Does the type of skin replacement surgery influence the rate of infection in acute burn injured patients? Burns 2013;39:1386–1390.
- Moore EC, Padiglione AA, Wasiak J, Paul E, Cleland H. Candida in burns: risk factors and outcomes. J Burn Care Res 2010;31:257–263.
- Park H-S, Pham C, Paul E, Padiglione A, Lo C, Cleland H. Early pathogenic colonisers of acute burn wounds: a retrospective review. Burns 2017;43:1757–1765.
- Vickers ML, Dulhunty JM, Ballard E, et al. Risk factors for multidrug-resistant Gram-negative infection in burn patients. ANZ J Surg 2018;88:480–485.
- Issler-Fisher AC, McKew G, Fisher OM, Harish V, Gottlieb T, Maitz PKM. Risk factors for, and the effect of MRSA colonization on the clinical outcomes of severely burnt patients. Burns 2015;41:1212–1220.
- Klifto KM, Shetty PN, Slavin BR, et al. Impact of nicotine/smoking, alcohol, and illicit substance use on outcomes and complications of burn patients requiring hospital admission: systematic review and meta-analysis. Burns 2020;46:1498–1524.
- Diab J, O’Hara J, Pye M, Parker C, Maitz PKM, Issler-Fisher A. Foot burns: a comparative analysis of diabetic and non-diabetic patients. Burns 2020;47:705–13.
- Mai L, Spilsbury K, Edgar DW, Berghuber A, Wood FM. Increased risk of blood transfusion in patients with diabetes mellitus sustaining non-major burn injury. Burns 2020;46:888–896.
- Harvey L, Mitchell R, Brodaty H, Draper B, Close J. Dementia: a risk factor for burns in the elderly. Burns 2016;42:282–290.
- Li F, Coombs D. Mental health history-a contributing factor for poorer outcomes in burn survivors. Burns Trauma 2018;6:1.
- Sayampanathan AA. Systematic review and meta-analysis of complications and outcomes of obese patients with burns. Burns 2016;42:1634–1643.
- Kimmel LA, Wilson S, Walker RG, Singer Y, Cleland H. Acute kidney injury: it’s not just the ‘big’ burns. Injury 2018;49:213–218.
- Tan H, Wasiak J, Paul E, Cleland H. Effective use of Biobrane as a temporary wound dressing prior to definitive split-skin graft in the treatment of severe burn: a retrospective analysis. Burns 2015;41:969–976.
- Dyson K, Baker P, Garcia N, et al. To intubate or not to intubate? Predictors of inhalation injury in burn-injured patients before arrival at the burn centre. EMA 2021;33:262–269.
- Aung MT, Garner D, Pacquola M, et al. The use of a simple three-level bronchoscopic assessment of inhalation injury to predict in-hospital mortality and duration of mechanical ventilation in patients with burns. Anaes Int Care 2018;46:67–73.
- Moore E, Pilcher D, Bailey M, Cleland H, McNamee J. A simple tool for mortality prediction in burns patients: APACHE III score and FTSA. Burns 2010;36:1086–1091.
- Moore EC, Pilcher D, Bailey M, Cleland H. Women are more than twice as likely to die from burns as men in Australia and New Zealand: an unexpected finding of the Burns Evaluation And Mortality (BEAM) Study. J Crit Care 2014;29:594–598.
- Moore EC, Pilcher DV, Bailey MJ, Stephens H, Cleland H. The Burns Evaluation and Mortality Study (BEAMS): predicting deaths in Australian and New Zealand burn patients admitted to intensive care with burns. J Trauma Acute Care Surg 2013;75:298–303.
- Perkins M, Abesamis GM, Cleland H, Gabbe BJ, Tracy LM. Association between gender and outcomes of acute burns patients. ANZ J Surg 2020;91:83–88.
- Wallace HJ, Fear MW, Crowe MM, Martin LJ, Wood FM. Identification of factors predicting scar outcome after burn in adults: a prospective case-control study. Burns 2017;43:1271–1283.
- Finlay V, Burrows S, Burmaz M, et al. Increased burn healing time is associated with higher Vancouver Scar Scale score. Scars Burns Heal 2017;3:2059513117696324.
- Crofton E, Meredith PJ, Gray P, Strong J. Compression garment wear and sensory variables after burn: a single-site study. Burns 2020;46:1903–1913.
- Read DJ, Tan SC, Ward L, McDermott K. Burns first aid treatment in remote Northern Australia. Burns 2018;44:481–487.
- Gong J, Tracy LM, Edgar DW, Wood FM, Singer Y, Gabbe BJ. Poorer first aid after burn is associated with remoteness in Australia: Where to from here? Aus J Rural Health 2021;29:521–529.
- Harish V, Li Z, Maitz PKM. First aid is associated with improved outcomes in large body surface area burns. Burns 2019;45:1743–1748.
- Harish V, Tiwari N, Fisher OM, Li Z, Maitz PKM. First aid improves clinical outcomes in burn injuries: evidence from a cohort study of 4918 patients. Burns 2019;45:433–439.
- Wood FM, Phillips M, Jovic T, Cassidy JT, Cameron P, Edgar DW. Water first aid is beneficial in humans post-burn: evidence from a bi-national cohort study. PloS One 2016;11:e0147259.
- Cassidy TJ, Edgar DW, Phillips M, Cameron P, Cleland H, Wood FM. Transfer time to a specialist burn service and influence on burn mortality in Australia and New Zealand: a multi-centre, hospital based retrospective cohort study. Burns 2015;41:735–741.
- Town CJ, Strand H, Johnson J, Brown J, Pelecanos A, Van Zundert A. Ultrasound-guided fascia iliaca plane block for the treatment of donor site pain in the burn-injured patient: a randomized control trial. J Burn Care Res 2021;42:981–985.
- Desai C, Wood FM, Schug SA, Parsons RW, Fridlender C, Sunderland VB. Effectiveness of a topical local anaesthetic spray as analgesia for dressing changes: a double-blinded randomised pilot trial comparing an emulsion with an aqueous lidocaine formulation. Burns 2014;40:106–112.
- Wasiak J, Spinks A, Costello V, et al. Adjuvant use of intravenous lidocaine for procedural burn pain relief: a randomized double-blind, placebo-controlled, cross-over trial. Burns 2011;37:951–957.
- Town C, Strand H, Johnson J, Van Zundert A. Ultrasound-guided axillary brachial plexus block for the management of graft site pain during dressing change in the burn injured patient: a randomized control trial. J Burn Care Res 2022.
- Parker M, Delahunty B, Heberlein N, et al. Interactive gaming consoles reduced pain during acute minor burn rehabilitation: a randomized, pilot trial. Burns 2016;42:91–96.
- Gray P, Kirby J, Smith MT, et al. Pregabalin in severe burn injury pain: a double-blind, randomised placebo-controlled trial. Pain 2011;152:1279–1288.
- Browne AL, Andrews R, Schug SA, Wood F. Persistent pain outcomes and patient satisfaction with pain management after burn injury. Clin J Pain 2011;27:136–145.
- Lewis PA, Burns GD, Webster A, et al. A randomized controlled pilot study comparing aqueous cream with a beeswax and herbal oil cream in the provision of relief from postburn pruritis. J Burn Care Res 2012;33:e195–e200.
- Edwick DO, Hince DA, Rawlins JM, Wood FM, Edgar DW. Randomized controlled trial of compression interventions for managing hand burn edema, as measured by bioimpedance spectroscopy. J Burn Care Res 2020;41:992–999.
- Aggarwala S, Harish V, Roberts S, et al. Treatment of partial thickness burns: a prospective, randomized controlled trial comparing four routinely used burns dressings in an ambulatory care setting. J Burn Care Res 2021;42:934–943.
- Moussa A, Lo CH, Cleland H. Burn wound excision within 24 h: a 9-year review. Burns 2021;47:1300-07.
- Harish V, Li Z, Maitz PKM. The optimal timing of outpatient Biobrane™ application for superficial and mid dermal partial thickness burns: evidence for the ‘12-hour rule’. Burns 2019;45:936–941.
- Hubik DJ, Wasiak J, Paul E, Cleland H. Biobrane: a retrospective analysis of outcomes at a specialist adult burns centre. Burns 2011;37:594–600.
- Greenwood JE. A randomized, prospective study of the treatment of superficial partial-thickness burns: AWBAT-S versus Biobrane. Eplasty 2011;11:e10.
- Lo CH, Brown JN, Dantzer EJG, et al. Wound healing and dermal regeneration in severe burn patients treated with NovoSorb® biodegradable temporising matrix: a prospective clinical study. Burns 2022;48:529–538.
- Anderson JR, Fear MW, Phillips JK, et al. A preliminary investigation of the reinnervation and return of sensory function in burn patients treated with INTEGRA®. Burns 2011;37:1101–1108.
- Cleland H, Wasiak J, Dobson H, et al. Clinical application and viability of cryopreserved cadaveric skin allografts in severe burn: a retrospective analysis. Burns 2014;40:61–66.
- Lo CH, Akbarzadeh S, McLean C, et al. Wound healing after cultured epithelial autografting in patients with massive burn injury: a cohort study. J Plast Reconstruct Aesth Surg 2019;72:427–437.
- Munasinghe N, Wasiak J, Ives A, Cleland H, Lo CH. Retrospective review of a tertiary adult burn centre’s experience with modified Meek grafting. Burns Trauma 2016;4:6.
- Issler-Fisher AC, Fakin RM, Fisher OM, et al. Microbiological findings in burn patients treated in a general versus a designated intensive care unit: effect on length of stay. Burns 2016;42:1805–1818.
- Katz T, Wasiak J, Cleland H, Padiglione A. Incidence of non-candidal fungal infections in severe burn injury: an Australian perspective. Burns 2014;40:881–886.
- Dolton M, Xu H, Cheong E, et al. Vancomycin pharmacokinetics in patients with severe burn injuries. Burns 2010;36:469–476.
- Paratz JD, Lipman J, Boots RJ, Muller MJ, Paterson DL. A new marker of sepsis post burn injury? Crit Care Med 2014;42:2029–2036.
- Patel BM, Paratz J, See NC, et al. Therapeutic drug monitoring of beta-lactam antibiotics in burns patients – a one-year prospective study. Therapeutic Drug Monitor 2012;34:160–164.
- Kurmis R, Heath K, Ooi S, et al. A prospective multi-center audit of nutrition support parameters following burn injury. J Burn Care Res 2015;36:471–477.
- Sierp EL, Kurmis R, Lange K, et al. Nutrition and gastrointestinal dysmotility in critically ill burn patients: a retrospective observational study. JPEN 2021;45:1052–1060.
- Falder S, Silla R, Phillips M, et al. Thiamine supplementation increases serum thiamine and reduces pyruvate and lactate levels in burn patients. Burns 2010;36:261–269.
- Douglas H, Lynch J, Harms KA, et al. Carbon dioxide laser treatment in burn-related scarring: a prospective randomised controlled trial. J Plast Reconstruct Aesth Surg 2019;72:863–870.
- Klotz T, Kurmis R, Munn Z, Heath K, Greenwood J. Moisturisers in scar management following burn: a survey report. Burns 2017;43:965–972.
- Coghlan N, Copley J, Aplin T, Strong J. The experience of wearing compression garments after burn injury: “On the inside it is still me”. Burns 2019;45:1438–1446.
- Coghlan N, Copley J, Aplin T, Strong J. How to improve compression garment wear after burns: Patient and therapist perspectives. Burns 2019;45:1447–1455.
- Finlay V, Davidoss N, Lei C, et al. Development and evaluation of a DVD for the education of burn patients who were not admitted to hospital. J Burn Care Res 2012;33:e70–8.
- Martin L, Andrews S, Rea S, Wood F. Motivating patients towards better recovery after burn: The development of a booklet to reframe perspectives. Burns 2022;49:91–99.
- Kornhaber R, Wilson A, Abu-Qamar M, McLean L, Vandervord J. Inpatient peer support for adult burn survivors – a valuable resource: a phenomenological analysis of the Australian experience. Burns 2015;41:110–117.
- Mc Kittrick A, Gustafsson L, Hodson T, Di Tommaso A. Exploration of individuals perspectives of recovery following severe hand burn injuries. Burns 2023;49:467–475.
- Ghalayini G, O’Brien L, Bourke-Taylor HM. Recovery in the first six months after hand and upper limb burns: a prospective cohort study. Aus Occ Ther J 2019;66:201–209.
- Schmitt BJ, Stiller K, Heath KE, Klotz T, Greenwood JE. The necessity for hand therapy interventions for patients with partial thickness isolated hand/forearm burns: a randomized controlled pilot trial. Burns Open 2018;2:171–177.
- Clayton NA, Ward EC, Maitz PKM. Full thickness facial burns: outcomes following orofacial rehabilitation. Burns 2015;41:1599–1606.
- Finlay V, Hendrie D, Allison GT, Phillips M, Wood FM, Edgar DW. Evaluation of a streamlined model of care for minor burn patients. J Burn Care Res 2014;35:342–348.
- Adanichkin N, Greenwood JE, McArthur A. Face care amongst patients admitted to the adult burn service: a best practice implementation project. JBI Database Sys Rev Implement Rep 2015;13:369–385.
- Tracy LM, Cameron PA, Singer Y, et al. Venous thromboembolism prophylaxis practice and its association with outcomes in Australia and New Zealand burns patients. Burns Trauma 2021;9: doi:10.1093/burnst/tkaa044.
- Giuliani S, McArthur A, Greenwood J. Preoperative fasting among burns patients in an acute care setting: a best practice implementation project. JBI Database Sys Rev Implement Rep 2015;13:235–253.
- Little M, Cooper J, Gope M, et al. ‘Lessons learned’: a comparative case study analysis of an emergency department response to two burns disasters. EMA 2012;24:420–429.
- Stefani K, Wagstaff MJD, Damkat I, Greenwood JE. Mortality data 2004–2019: an audit of the Royal Adelaide Hospital Adult Burn Service. ANZ J Surg 2021;91:77–82.
- Ryder C, Mackean T, Hunter K, Coombes J, Holland AJA, Ivers R. Yarning up about out-of-pocket healthcare expenditure in burns with Aboriginal families. Aus NZ J Pub Health 2021;45:138–142.
- Potter MDE, Maitz PKM, Kennedy PJ, Goltsman D. Perineal tap water burns in the elderly: at what cost? ANZ J Surg 2017;87:E188–E192.


