Volume 24 Number 2
An education program for pressure injury recognition and assessment utilising constructivism teaching method
Monica Stankiewicz, Joan Webster, Marianne Wallis, Mandy Tallot and Wendy Chaboyer
Keywords Constructivism theory, education, pressure injury recognition and assessment.
Abstract
Background: Constructivism theoretical framework was used as the fundamental base in developing a nursing education program. This required education of research assistants employed as outcome assessors for a pressure injury prevention study. Outcome assessors were required to correctly identify pressure injury stages and whether or not a pressure injury developed throughout the project.
Objectives: To evaluate the knowledge developed by outcome assessors as a consequence of engaging in the education program.
Methods: The education program was delivered to 25 outcome assessors across five sites in Australia. A purpose-designed instrument was developed for the education day’s program, which included 27 pre-test and post-test questions. A paired samples t-test was used to compare changes in pre-test and post-test scores.
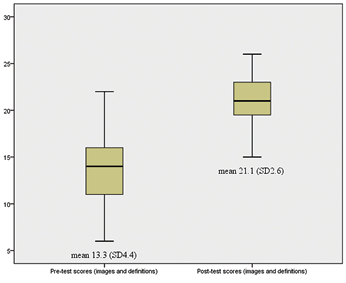
Results: The success of the education day was highlighted by higher post-test scores, compared with the scores obtained prior to pressure injury education. The combined pre-test score was 13.3 (SD±4.4) compared with a higher post-test score of 21.1 (SD±2.6) (p<0.02).
Conclusion: Through the use of constructivism theoretical educational framework, outcome assessors were able to improve their knowledge about pressure injury assessment and staging. Pre-test scores were lower than post-test scores, indicating increased knowledge as a result of the education session.
Introduction
Pressure injuries (PIs) are a common and difficult to treat problem among hospitalised patients, especially those who have restricted movements1,2. Cochrane reviews evaluating interventions aimed at preventing PIs from developing in the first place have generally concluded that evidence is limited by underpowered studies of low quality3-5. Consequently, there is little evidence to indicate which, if any, interventions are the most effective in preventing PIs.
In an effort to contribute to the evidence base and to test an intervention that may help to prevent hospital-acquired PIs, we planned a large, multicentred cluster randomised trial. During preparation for the trial, we recognised that knowledge about PIs among the outcome research nurses (ORN) who were recruited to assess the study’s outcome, varied considerably. So, in line with the Good Clinical Practice guidelines for the conduct of clinical trials6, we provided specific training to the ORNs in correctly classifying PI. The education sessions were aimed at improving PI identification and staging skills of the ORNs and had no impact on prevention. The purpose of this paper is to describe this training and evaluation of its impact on the ORNs.
The development of nursing education programs that acknowledge the nurse’s current level of knowledge and clinical experience requires a modern paradigm for teaching7,8. Historically, education has been delivered as a ‘teacher delivers all information’ method, which fails to take into account the learner’s current knowledge and professional experiences9,10. In continuing professional development and upskilling nurses, the use of constructivism theory assists in the delivery of a framework for education, encompassing various levels of nursing skill and experience, through education, reflection and mentorship7,8.
Russian social theorist Vigotsky, suggested people understand and develop through “the relationship between thought and word … a continual movement back and forth from thought to word and from word to thought”11,p.125. Applying this type of constructivist approach to teaching leads to viewing the learner as actively involved in constructing knowledge, fostering a critical approach to thinking and building upon their current knowledge and understanding9,10. In this approach, the teacher is a model and coach, who first gains an understanding of the learner’s current knowledge and then builds on this knowledge; an approach known as ‘scaffolding’ new learning on current understanding9,10.
The use of a constructivism theoretical framework in the context of this PI educational program aimed to build on the nurse’s current skin assessment skills, solidifying their knowledge about PIs and improving assessment and diagnosis of stages of PIs. Through this method, we avoided the didactic delivery of information, but rather used the educational experience of group discussion and reflection. Examples of didactic teaching at local institutions include one hour of theory for PI assessment delivered to new employees and annual national bedside auditors, which have the same aim: to improve PI assessment skills. On the other hand, examples of how ORNs were coached through the education program included providing time for nurses to discuss PIs encountered in their clinical experience and discussing the suspected causes and symptoms of tissue damage, which would enable an accurate description and classification of the PI. Their experiences were incorporated into the activities of the day to improve knowledge and assessment skills. This allowed the nurses to be active participants in their learning, through problem solving, teaching each other, allowing each other’s different experiences to guide their learning, with the most confident nurses able to guide and support others. When compared with traditional teaching, this allowed the nurses to gain knowledge from other sources rather than having knowledge imposed on them from one source.
Materials and methods
Education evaluation design
The evaluation utilised differences between pre-test and post-test scores. The aim of the education was to improve ORNs’ knowledge and assessment skills in identifying and assessing PIs. Activities and group discussions were encouraged to expand on knowledge, addressing any deficits and enhance the learners’ experiences through multiple dimensions of adult learning.
Participants and setting
The education program was delivered to nursing staff employed for a multisite cluster randomised trial that included eight hospitals across three states in Australia. Participants were ORNs, with backgrounds including wound care nurse specialists, general nursing staff and student nurses.
Teaching content
The concepts taught included PI definition, classifications and frequent causes of injury. A PI is defined as an area of localised damage due to three individual or combined factors: shear, friction and pressure12-15. PI typically occur over a bony prominence12,13,15. Other patient factors may contribute to further tissue destruction based on individual physiological changes; for example malnutrition, poor circulation, medications and tissue moisture14. Six PI stages have been identified, as shown in Table 1.
Table 1: Pressure Injury Classification (Pan Pacific Clinical Practice Guideline for the Prevention and Management of Pressure Injury (Ulcer), 2012; Sibbald et al., 2011)
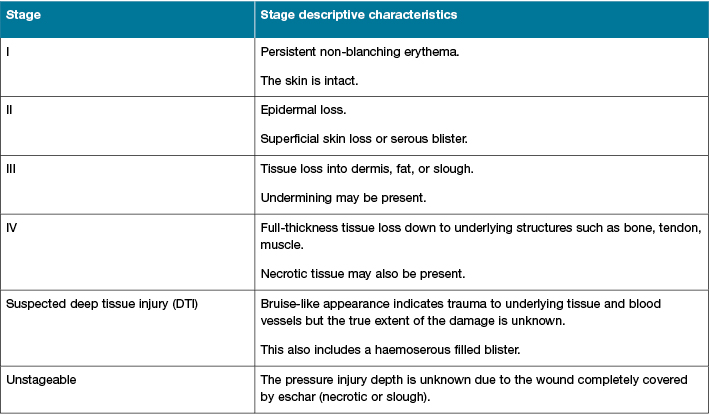
PI depth, despite staging, also depends on location of the injury. For example, a Stage 3 PI depth may differ from the buttock to the back of the head, deep versus shallow damage12,13. Injuries located in the mucosa due to the presence of medical equipment, are also classified as a PI but remain an entity of their own2,16. This is due to the absence of characteristics related to the six stages of pressure injury such as bone, tendon or the presence of slough, which is more likely to be senescent blood cells rather than devitalised tissue2.
Measures
Typically the Pressure Ulcer Knowledge Test (PUKT) has been utilised by many nursing educators and wound care clinicians to determine outcomes of teaching sessions for improvement in PI knowledge17-21. However, this test consists of many measures for PIs including staging, prevention and management questions, the latter two being irrelevant for our educational purpose.
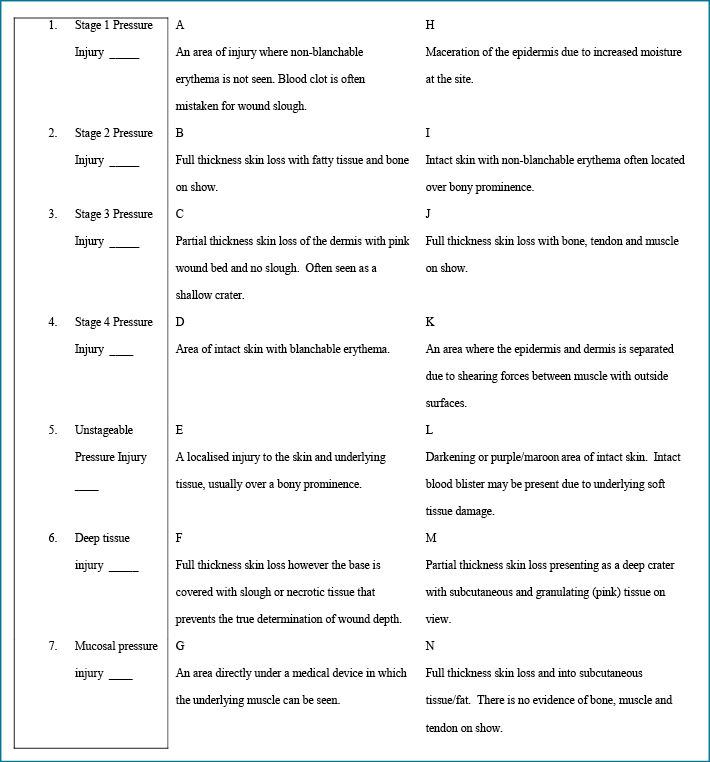
Therefore, a purpose-designed test was developed for the education day’s program including seven questions related to the definition of PI stages. The purpose-designed test also included a total of 14 multiple-choice definitions, and the most correct answers were the ones that accurately described key characteristics of the wound bed and tissue injury, for each of the seven PI categories (Figure 1). There were also 20 images of wound types and skin lesions, and nurses were required to identify whether a PI was present or not; and, if so, the PI stage. Both the pre-test and post-test questionnaires included the same definitions and images. Inter-rater reliability (IRR) of outcome assessors was assessed separately and results of the IRR will be reported, along with other results, at the end of the trial.
Figure 1: Testing tool: definitions (image of test)
Procedure
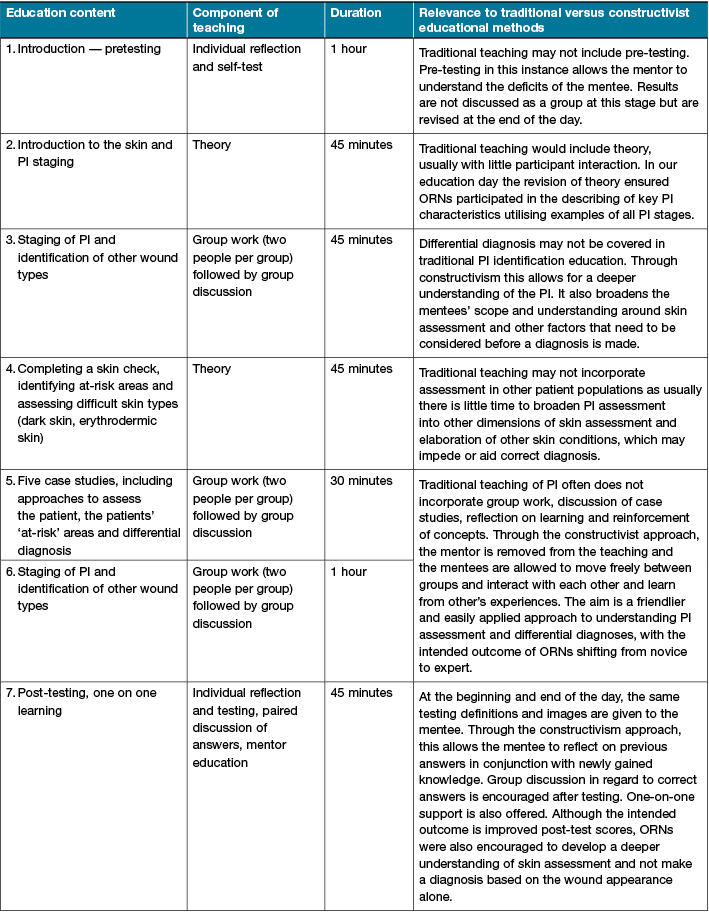
The education program was delivered to all participants over a five and a half hour period in one day. Table 2 shows the structure of the education day, including time involved with each component. The education sessions were initially trialled with five nursing staff (including two chief investigators) to streamline the education prior to delivery to the larger research team; results from this initial trial were excluded from the final analyses. At commencement of the trial’s education day, pre-tests were given to the participants; and at the end of the education day post-tests were given to measure the difference in participant knowledge and success of the education session. Participants who did not obtain 100% accuracy on the post-test scores were given time to reflect and discuss post-test scores with their peers and then given further education on the day by the educator.
Table 2: Education day format
Ethical considerations and consent
The education preparation and education days conformed to the ethical guidelines of the 1975 Declaration of Helsinki as training of research staff in assessing PI was a requirement by all hospital and university Human Research Ethics Committees that approved the trial. Additionally, Good Clinical Practice requires that research staff are trained with appropriate education and tools to deliver good-quality research. Therefore, the participants were educated as a part of their preparation for the research project and participation in the project implied consent22.
Analysis
De-identified data were entered into the SPSS software, version 18 (Chicago: SPSS Inc., 2009). All data were cleaned and cross-checked for accuracy. Descriptive statistics were used to explore participant skill level and are reported as counts and percentages. Paired samples t-tests were used to compare the difference in pre-test and post-test scores for test-definitions, test-images and combined scores.
Results
A full day of PI education was provided to 25 participants. Group numbers ranged from four to six participants, in five separate sessions. The skill mix consisted of principal investigator (n=1, 4%), wound care specialist (n=3, 12%), nursing students (n=2, 8%) and general trained nurses (n=19, 76%).
The lowest possible score for the pre-test and post-test scores was zero and the highest score was seven. The mean pre-test score was 3.8 (SD±2.4). Following the education session, the mean post-test score increased to 6.7 (SD±3.5). This difference was statistically significant (p<0.001).
For the PI images, the lowest possible score was zero and the highest score was 20. The mean pre-test score was 9.7 (SD±4.0). Following the education session, the mean post-test score increased to 14.3 (SD±3.9). This difference was statistically significant (p<0.001).
Finally, we combined the PI definition and image scores; where the lowest possible score was zero and the highest score was 27. Figure 2 shows the difference in pre-test and post-test scores which was statistically significant (p<0.02).
Figure 2: Combined scoring (imagery and definition), pre-test and post-test scores
Discussion
This is the first published study to assess the change in nurses’ knowledge of PI staging from a PI education day, based on a sound theoretical framework. Constructivism in teaching is a useful education method that incorporates many facets of human learning to improve knowledge. Participants appeared to be fully engaged and the delivery method resulted in a significant increase in the outcome assessors’ knowledge. Additionally, we learned from this teaching and learning style that the written word (through definitions) was the most effective strategy for memorising what was learned on the day. This format may be useful for other areas of nursing education, particularly where the subject matter is constant and critical thinking or planning is not required.
Although the images component of the test produced lower change scores between pre- and post-intervention testing, individual discussions with participants after post-testing indicated that imagery was also useful to improve nurses’ levels of knowledge and assessment skills. For example, when participants were asked to discuss incorrect post-test scores, it was clear that images provided for the testing tool were misinterpreted. These participants were able to describe, with 100% accuracy, a PI stage but had not associated that stage with the image provided. This may indicate that post-test scores may have been higher if a ‘real’ PI had been assessed, rather than a two-dimensional image.
Interestingly, a recently published study between two groups of nurses found that those who received traditional-based learning achieved higher mean scores than those who received computer-based learning, when pre-test and post-test scores where compared at the end of the PI education sessions18. Our study supports earlier findings reported by Sinclair and colleagues23, who also completed pre-testing and post-testing of a PI educational day. Although Sinclair and colleagues23 did not focus on the educational theory used to develop and deliver the education, they did report that the educational day included multidimensional learning including video, role play, the use of protocols and guidelines for staff reflection, lectures and case study group discussions. Like our study, Sinclair’s23 study indicated that an increase in knowledge had been obtained. Altun and Zencirici17 also reported knowledge improvement identified through pre-test and post-testing. However, they delivered an educational session for only three hours, with a lecture-structured education session. Unfortunately, we do not know if there would be differences in outcome assessors’ knowledge from our educational day if we delivered a three-hour lecture; or if a three-hour lecture would have been a sufficient mode of delivery to instil confidence in outcome assessors’ ability to correctly assess and stage PIs.
Whether our program or any other program results in a sustained knowledge change is unclear, but a study by Pieper and Mott24 reported highest levels of knowledge for PI staging and PI assessment by nursing staff who attended the most recent educational sessions. Therefore, our education day was designed to enhance the learning experience via a multidimensional approach as close to the start of the study to enhance recovery of information for our purposes of the research project. Also, it was necessary that our outcome assessors followed a consistent process when conducting a skin assessment. Therefore, a full day of education was provided.
In regard to the potential differences occurring in nursing learning style, theoretical (such as text-based) versus visual, there have been several studies that report nurses learn predominantly through kinaesthetic or visual learning styles25-30. A quality improvement activity by Frankel28 delivered questionnaires on preferred styles of learning to 61 nurses. Frankel28 reported that nurses preferred to learn through visual (n=34) or kinaesthetic (n=17) learning. This was also supported by a comparative study by Bostrom and Hallin25, who reported differences in learning styles between teacher and nursing student; again nurses favoured “learning by doing”. However, a longitudinal study by Fleming and colleagues27 reported that nursing students had variation in learning styles depending on age and year of nursing education; therefore no significant learning style could be isolated in the cohort. This finding by Fleming and colleagues27 was similar to outcomes reported by Esche and colleagues18, who were able to separate nurses’ learning preferences by age groups. That is, mature-aged nurses preferred traditional-based learning (in the classroom) versus computer-based learning as a preference expressed by younger nursing staff. However, overall, retention of knowledge gained from PI education was highest in the traditional-based learning group when compared with those who undertook computer-based learning. These variations in learning style support the mixed style of constructivism education delivered through our PI education program, as the nursing community, both clinical and research, were diverse in age and clinical experience. In this instance, the mixed group of participants required a mixed teaching style, such as constructivism-based teaching.
Constructivism-based teaching covers many facets of teaching to improve one’s learning capabilities29. In utilising a constructivism framework, theory was delivered to assist with filling deficits in knowledge, and visual-kinaesthetic learning style was used to improve memory and critical thinking. The importance of critical thinking by nurses for translating and reflecting upon theoretical knowledge to embed in practice is well documented26,28,30. In this instance, participants were encouraged to self-regulate knowledge and interpret findings which were pertinent to study outcomes: the identification and staging of PIs.
Although this paper reports on outcomes from an education day for a cohort of nurse researchers, the methods may be translated to the wider nursing community. The importance of improving PI assessment, management and prevention is a national and international health priority; with the responsibility for improvement mostly falling onto the nursing discipline20. There is a clear need for effective education in this area. For example, there is evidence of knowledge deficits among nurses about current evidence-based practice and updated staging, prevention and management guidelines14,20. There have also been recent changes incorporating the suspected deep tissue injury (SDTI) and unstageable PIs, and mucosal PIs. These changes indicate that PI education cannot be a ‘one-off’ session during a nurse’s career but that constant updating is required to maintain knowledge, and sustain best and current practice.
In regard to our study, the education day was essential to minimise misclassification of PI. However, there are also implications for the wider nursing and health care community. The misclassification of PIs may lead to poor health outcomes to the patient due to inappropriate management. Incorrectly diagnosing PIs may also lead to financial penalties for the institution where wrong diagnosis has been made, for example the inability to distinguish between PI damage and a leg ulcer, or other wound aetiologies31. Thus, an education day like we have described here could be used in clinical practice to promote better assessment of PI.
Limitations
Firstly, the education program was limited by the use of images rather than PIs present in real people or simulation mannequins. However, this limitation would have affected both pre-test and post-test scores, yet improvements were evident despite the use of images. Additionally, further learning appeared to have occurred after the post-test was completed, with participants accurately discussing their assessments of various images. In saying this, perhaps with more funding for education, the use of PI simulation devices or time spent with real patients may have enabled the participants to articulate their true knowledge level. In regard to long-term effects of the education day, we relied on the daily skin inspections completed by ORNs to enhance PI assessment and diagnosis; however, we did not obtain follow-up tests to assess this knowledge objectively.
Secondly, the multiple-choice questions relating to PI stage definitions may have also been a limitation. Participants may have attained high post-test scores if they were able to describe their understanding of various PI stages rather than selecting a best-fit answer, where the participants’ ability to critically describe the PI stages may have been limited by multiple-choice answer selection. In saying this, there may have been differences in pre-test and post-test scores based on nursing experience, junior nurse versus wound clinician; however, as tests were de-identified, we were unable to make inferences between nursing experience and knowledge gained in this area.
Finally, the use of the same pre-test and post-test may be considered a limitation due to memory recall bias. However, the use of constructivism approach to learning encouraged the nurses to reflect on the knowledge gained throughout the education day and allowed them to challenge their own approach in skin assessment and PI diagnosis.
Conclusion
The use of a constructivism framework to guide the development of an educational program aimed at improving PI assessment and diagnosis (staging of PI and whether or not a wound is a PI) is an effective way for improving nursing knowledge. Outcomes reported in this study highlight that mixed education sessions consisting of theoretical and visual cues increased the participants’ abilities to assess and diagnose PIs and PI stages. Although participants obtained higher post-test scores when PI definitions were used, they were also able to accurately describe PI and wound imagery, further supporting the benefits of constructivism framework in the design of educational programs with nurses.
Acknowledgements
Education/research was conducted at the following institutions:
The Royal Brisbane and Women’s Hospital, Qld, Australia
Gold Coast University Hospital, Qld, Australia
Nambour Hospital, Sunshine Coast, Qld, Australia
St Vincent’s Hospital, Sydney, NSW, Australia
The Austin Hospital, Melbourne, Vic, Australia
Author(s)
Monica Stankiewicz*
RN, Graduate Diploma Wound Care, Master of Applied Science (Research), Master of Nursing Science (Nurse Practitioner)
Wound Management — Dermatology Nurse Practitioner
Private Practice, Brisbane, Qld
48 Clare Place, The Gap, Brisbane
Qld 4061, Australia
Mobile 0430 168 010
Email mon.stankiewicz@gmail.com
Joan Webster
BA, RN
Director of Research and Development Unit
The Royal Brisbane and Women’s Hospital, Brisbane, Qld, Australia
NHMRC Centre of Research Excellence in Nursing Interventions for Hospitalised Patients (NCREN), Editor, Cochrane Wound Group, Cochrane Collaboration
Marianne Wallis
PhD, RN
Professor of Nursing
University of the Sunshine Coast, Qld, Australia
Mandy Tallot
Master of Critical Care, RN
Clinical Nurse
Project Manager, INTACT, Griffith University and Gold Coast Hospital, Qld, Australia
Wendy Chaboyer
PhD, RN
Director, NHMRC Centre of Research Excellence in Nursing Interventions for Hospitalised Patients (NCREN), Griffith University, Gold Coast Campus
Qld, Australia
* Corresponding author
References
- McInnes E, Chaboyer W, Allen T et al. Acute care patient mobility patterns and documented pressure injury prevention — an observational study and survey. Wound Practice and Research 2013;21(3):116–25.
- National Pressure Ulcer Advisory Panel. Prevention and treatment of pressure ulcers: Quick reference guide. Page 1–75. National Pressure Ulcer Advisory Panel; 2014 [cited 2014 February 1]. Available from http://www.npuap.org/resources/position-statements/ April 2014
- Moore Z, Cowan S. Risk assessment tools for the prevention of pressure ulcers. Cochrane Database Sys Rev 2014;2
- Moore Z, Webster J. Dressings and topical agents for preventing pressure ulcers. Cochrane Database Sys Rev 2013;8
- Gillespie B, Chaboyer W, McInnes E, Kent B, Whitty J, Thalib L. Repositioning for pressure ulcer prevention in adults. Cochrane Database Sys Rev 2014;4.
- World Health Organisation. Handbook for Good Clinical Research Practice (GCP): Guidance for Implementation. Page 87–91, 115–120. World Health Organisation; 2002 [cited 2014 February 1]. Available from http://apps.who.int/prequal/info_general/documents/GCP/gcp1.pdf
- Hampton M. Constructivism applied to psychiatric-mental health nursing: An alternative to supplement traditional clinical education. Int J Mental H Nurs 2012;21:60–68.
- Hunter J, Krantz S. Constructivism in cultural competence education. J Nurs Educ 2010;49(4):207–214.
- Applefield J, Huber R, Moallem M. Constructivism in theory and practice: Toward a better understanding. High School J 2001;84(2):35–53.
- Brandon A. Constructivism theory analysis and application to curricula. Nurs Edu Persp 2010;31(2):89–92.
- Vigotsky L. Thought and language. Cambridge: MIT Press. 1965
- Dunk A, Gardner A, Waddington G. Anatomical location of injury in stage 1 and stage 2 heel pressure injuries — a pilot study. Wound Practice and Research 2012;3:130–141.
- Mackintosh R, Gwilliam A, Williams M. Teaching the Fruits of Pressure Ulcer Staging. J Wound, Ost Cont Nurs 2014;41(4):381–387.
- Australian Wound Management Association, New Zealand Wound Care Society, Hong Kong Enterostomal Therapists Association & Singapore Wound Healing Society. Pan Pacific Clinical Practice Guideline for the Prevention and Management of Pressure Injury. Page 1–124. Cambridge Media Osbourne Park, Western Australia; 2012 [cited 2014 February 1]. Available from www.awma.com.au April 2012.
- Sibbald G, Krasner D, Woo K. Pressure ulcer staging revisited: superficial skin changes & Deep Pressure Ulcer Framework. Adv skin wound care 2011;24(12):571–580.
- Coyer F, Stotts N, Blackman V. A prospective window into medical device-related pressure ulcers in intensive care. Int Wound J 2013;1–7.
- Altun I, Zencirci A. Knowledge and management of pressure ulcers: impact of lecture-based interactive workshops on training of nurses. Adv Skin Wound Care 2011;24(6):262–266.
- Esche C, Warren J, Woods A, Jesada E, Iliuta R. Traditional classroom education versus computer-based learning: How nurses learn about pressure ulcers. J Nurse Prof Devel 2015;31(1):21–27.
- Chianca T, Rezende J, Borges E, Nogueira V, Caliri M. Pressure ulcer knowledge among nurses in a Brazilian University Hospital. Ost Wound Manage 2010;56(10):1–11.
- Larence P, Fulbrook P, Miles S. A survey of Australian Nurses’ knowledge of pressure injury/pressure ulcer management. J Wound, Ost Cont Nurs 2015;0(0):1–11.
- Pieper B, Zulkowski K. The Pieper-Zulkowski Pressure Ulcer Knowledge Test. Adv Skin Wound Care 2014;27(9):413–420.
- Chaboyer W, Bucknall T, Webster J, McInnes E, Banks M, Wallis M, Gillespie B, Whitty J, Thalib L, Roberts S, Cullum N. INTroducing A Care bundle To prevent pressure injury (INTACT) in at-risk patients: A protocol for a cluster randomised trial. Int J Nurs Studies 2015;52(11):1659–1668.
- Sinclair L, Berwiczonek H, Thurston N, Butler S, Bulloch G, Ellery C, Giesbrecht G. Evaluation of an evidence-based education program for pressure ulcer prevention. J Wound Ost Cont Nurs 2004;Jan/Feb:43–50.
- Pieper B, Mott M. Nurses’ knowledge of pressure ulcer prevention, staging, and description. Adv Wound Care 1995;8(3):34–48.
- Bostrom L, Hallin K. Learning style difference between nursing and teaching students in Sweden: A comparative study. Int J Higher Edu 2013;2(1):22–34.
- Chikotas N. Theoretical links supporting the use of problem-based learning in the education of the nurse practitioner. Nurs Edu Perspec 2008;29(6):359–362.
- Fleming S, McKee G, Huntley-Moore S. Undergraduate nursing students’ learning styles: A longitudinal study. NET 2011;31(5):444–449.
- Frankel A. Nurses’ learning styles: promoting better integration of theory into practice. Nurs Times 2009;105(2):24–27.
- Hossein K, Fatemah D, Fatemah O, Katri V, Tahereh B. Teaching style in clinical nursing education: a qualitative study of Iranian nursing teachers’ experiences. Nurse Edu Prac 2010:8–12.
- Yildirim B, Ozkahraman S. Critical thinking in nursing and learning styles. Int J Human Social Sci 2011;1(18):127–133.
- Courtney B, Ruppman J, Cooper H. Save our skin: initiative cuts pressure ulcer incidence in half. Nurs Manage 2006;April:36–45.



