Volume 25 Number 1
Impact of hospital-acquired pressure injuries on hospital costs – experience of a tertiary hospital in Singapore
Lim Mei Ling and Ang Shin Yuh
Keywords pressure injuries, Cost, hospital-acquired, acute care.
Background
The prevention of hospital-acquired pressure injury (HAPI) remains a challenge for healthcare institutions around the world. Given the negative impact of pressure injuries on health outcomes, it is widely recognised that prevention is better than treatment of pressure injuries. However, with finite healthcare resources, management often needs to know what kind of financial return or cost avoidance it can achieve for investment in quality improvement programs1. Henceforth, an estimate of local costs of HAPI is important in informing future investment decisions on prevention strategies.
Singapore General Hospital (SGH) is a 1500 patient-bed, tertiary care, university-affiliated teaching hospital. A not-for-profit institution, SGH is wholly owned by the government of Singapore and is the flagship hospital of the public healthcare system. In SGH, the occurrence of HAPI is recognised as a nursing-sensitive quality indicator. Incidences are reported and the prevalence rate is monitored for quality assurance purposes. HAPI had been associated with increased hospitalisation costs. The total hospitalisation bills of the patients depends largely on the type of procedures and the ward requested during their stay in the hospital. There are four ward types (A1, B1, B2, C) in SGH. The wards differ by the hospital bed costs and the amenities provided. A higher ward class allows patient to enjoy more privacy (single-bed room), better facilities (air-conditioned room with attached bathroom, television and phone set) and choice of cuisine in the hospital2. Patients also receive different amounts of government subsidies based on the ward they choose. For example, a patient who stays in the C class ward (9-bed room) can receive up to 80% government subsidies, and a patient who choose a B2 class ward (6-bed room) can get up to 65% government subsidies off their total hospitalisation bill3.
Literature Review
A literature review was performed using the databases of PubMed with the following terms: “pressure ulcers”, “pressure injuries”, “decubitus ulcer” “acute hospital” and “costs”; coupled with a hand search of relevant literature. The search was done in January 2017. Articles were included if they fulfilled the following criteria: (1) the study looked at the cost of hospital-acquired pressure injuries; and (2) papers published in the English Language. Papers selected for retrieval were assessed by two independent reviewers for methodological validity prior to inclusion in the review using the economic evaluation checklist from the Critical Appraisal Skills Programme (CASP)4.
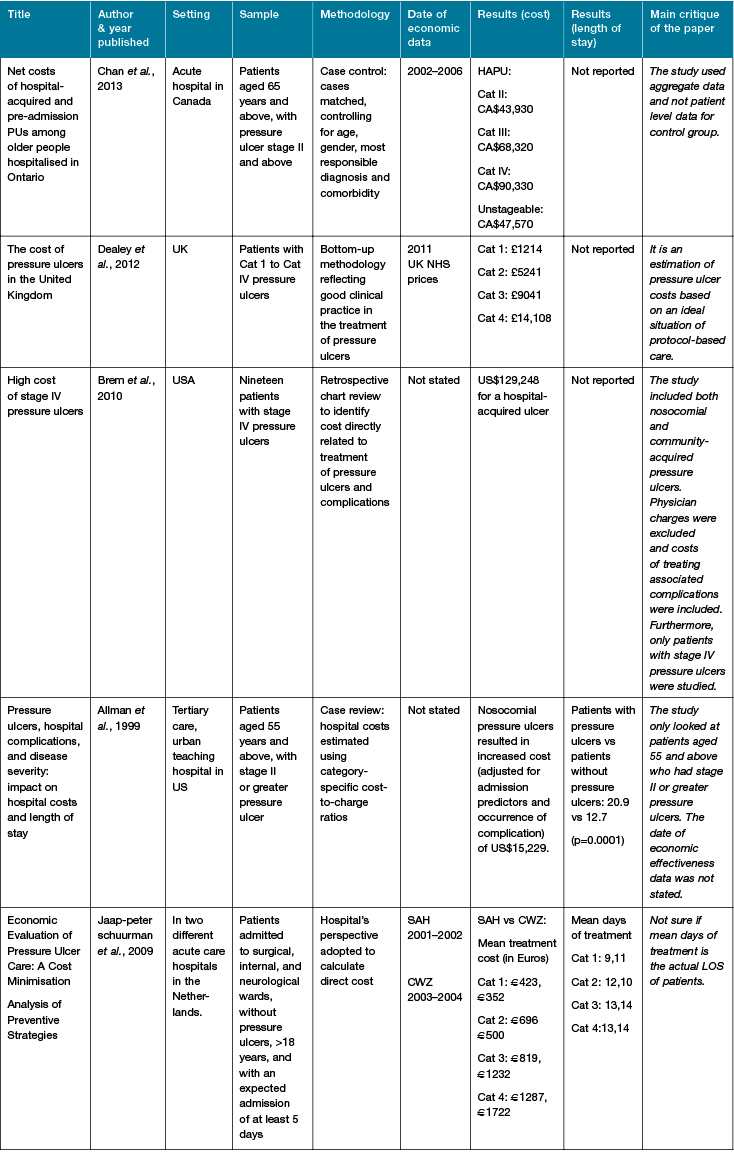
Several studies5-9 were found to have provided an estimate of the costs of HAPI (Table 1). In general, the hospitalisation costs and length of stay (LOS) of patients with pressure injuries were reported to be higher than patients without any pressure injuries. However, these studies were conducted across various settings and different methodological approaches were used.
Table 1: Summary of costs studies
Hence, the quality and reporting structure of the studies varied widely. To date, no studies have been done to look at the cost of HAPI in Singapore. Insights to the cost of HAPI can help to inform management and leadership of the economic impact of preventing HAPI, and enable better resource allocation in the hospital. Understanding the economic impact of HAPI would also help the healthcare organisations to be more focused on preventive care of pressure injury and serve as an impetus for clinicians to focus on pressure injury prevention measures. Efforts to promote the prevention of pressure injury is much needed to improve care quality, reduce hospitalisation stay and healthcare costs for both the patient and healthcare institution.
Aim
To provide an estimate of the costs of hospital-acquired pressure injuries in a tertiary teaching hospital in Singapore at Year 2014 price.
Method
Setting
This study was conducted in the adult inpatient wards of an acute care hospital in Singapore.
Ethical consideration
This study was approved by SingHealth Centralised Institutional Review Board (CIRB Ref: 2015/2408).
Participants
Patients who met the following criteria were included in the study: patients who acquired pressure injury during their hospital stay and discharged in the year of 2014 (Case); and patients who did not acquire pressure injury during their hospital stay and discharged in the year of 2014 (Control). Patients who were admitted with pressure injury and developed new ones while being in hospital were excluded from the study.
Design
A retrospective case-control study was carried out. Patients who acquired pressure injury (Cases) during their hospital stay were identified through the Electronic Incident Reporting system (Risk Management System; RMS) or nurse audit records. Pressure injury incidents were reported in the RMS by nurses. All registered and enrolled nurses at the participating wards underwent annual pressure injury assessment training and were competent to assess patients for pressure injuries. A final review of the pressure injury would also be done by the nurse clinician at the ward level to ensure that the right category pressure injury is documented and reported. These cases were matched to in-patient controls (patients who did not develop pressure injury) by age within five years, gender, admission department (for example, department of internal medicine, general surgery, orthopaedics department) and ward class.
The economic perspective of the healthcare provider was adopted. Only direct costs incurred in the acute care hospital was calculated. Direct costs such as consumables, drugs, facility fees, bed charges, laboratory investigations, treatment fees and doctors’ fees were included. Other costs such as loss of functional status, pain, disability, reduced quality of life, dependence on others, or loss of occupational productivity were not considered. Given that SGH is a not-for-profit institution, cost was based on patients’ gross hospitalisation fees (without government subsidies). The gross total hospitalisation fees would also account for the difference in fees level among the patients staying in different ward types. Demographic data such as age and gender of the patients were also obtained from the electronic health records.
Data Analysis
Categorical variables (age group, gender, pressure injury category) were described with frequencies and percentages. The total gross hospitalisation fees and LOS of patients with different categories of HAPI were described in means and standard deviations. T-tests were used to assess the differences in hospitalisation fees between patients with and without HAPI. All costs were reported in Year 2014 Singapore dollars.
Results
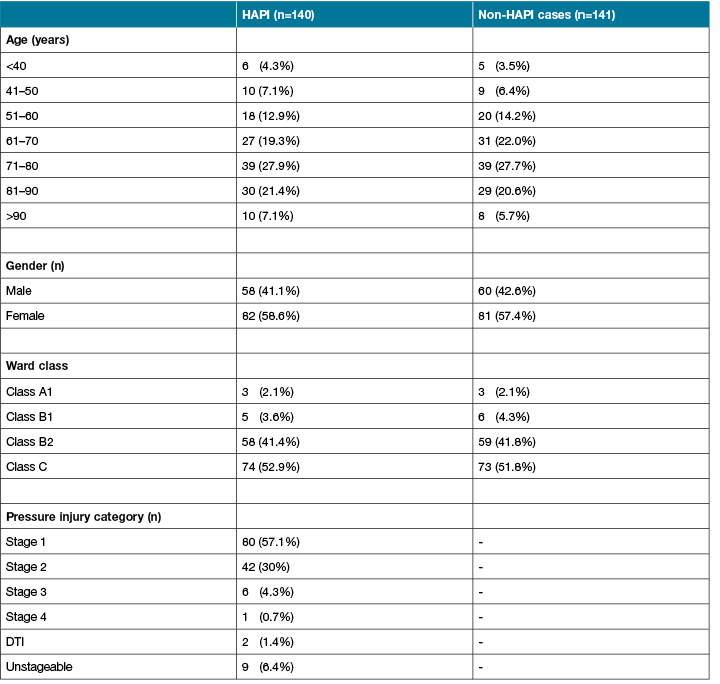
One hundred and forty patients who acquired pressure injury during their hospital stay were included in the analysis. Another 141 patients who did not have HAPI were matched for by gender, age, admission discipline and ward class. The mean age of the patients who acquired pressure injury was 70.7 (SD= ±15.7) years old and those without any pressure injury was 70.1 (SD= ±15.0) years old. More than half of the patients who developed HAPI were females (58.6%) and stage 1 pressure injury was the most commonly reported HAPI (57.1%) among the patients recruited (Table 2).
Table 2: Patients’ demographics
Compared with those without HAPI, patients with HAPI experienced significantly higher average hospitalisation fees and LOS (S$35,936 vs S$6,266, p <0.0005; 30 days vs 6 days, p <0.0005) (Table 3). Patients with stage 2 HAPI was found to have the highest increase in hospitalisation fees and LOS when compared to their matched control cases. The mean hospitalisation fees of patients with stage 2 HAPI was also the highest (S$48,917) as compared to others (Table 4).
Table 3: Mean (gross) hospitalisation fees (in year 2014) and LOS of patients with and without HAPI
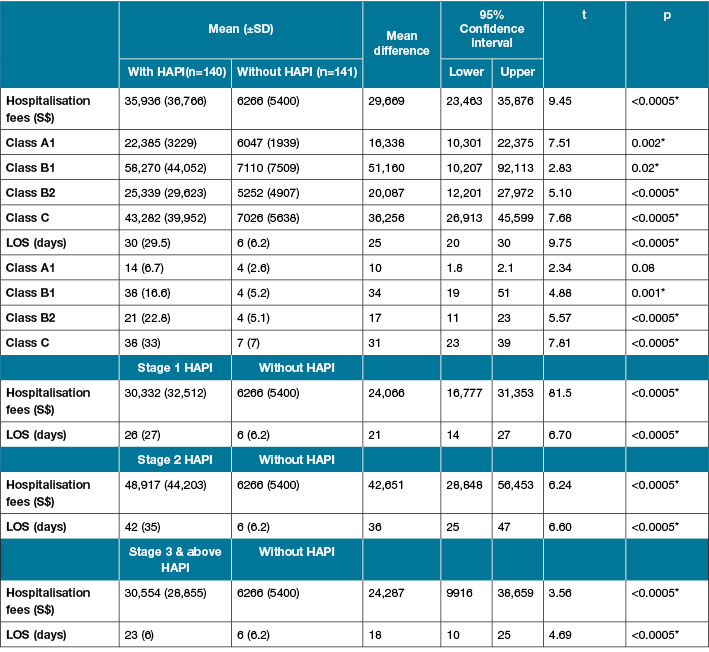
*Significant value p< 0.05
^Stage 3 & above includes: stage 3, stage 4, DTI and unstageable PI
Table 4: Gross hospitalisation fees (without government subsidies) and LOS of patients with HAPI
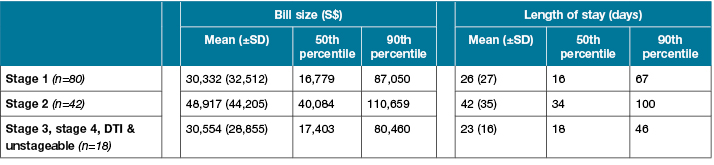
*Bill size = gross amount (before subsidies)
Discussion
Our study was the first to calculate the hospitalisation cost of HAPI in Singapore’s acute care setting. Similar to other studies5,8, our results showed that patients with HAPI incur higher hospitalisation fees and LOS as compared to those without HAPI. However, it was challenging to compare the results of our study with most previous studies due to methodological differences. For example, a recent cost study10 was conducted in Singapore to look at the cost of chronic wound management in a tertiary hospital. The mean cost per patient was S$5456 for pressure injury (unspecified), S$4546 for stage 3 pressure injury and S$13,138 for stage 4 pressure injury. However, it was unclear whether the study included community-acquired pressure injuries or only hospital-acquired ones. The previous study adopted service-based top-down gross costing method and included both direct and indirect costs. (Direct costs include hospital stays, inpatient surgical treatment, medications, wound dressing, investigation costs and consultations; while indirect costs included income loss during hospitalisation and income loss during sick leave.) In contrast, our study looked at the total hospitalisation fees of patients with HAPI. Likewise, in another cost study7, although only patients who had HAPI were recruited, the study only focused on patients aged 55 and above who had stage 2 or greater pressure injuries and the date of economic effectiveness data was not stated. Hence, the different costing methods and inclusion criteria led to different estimates of the cost of pressure injuries and it made in difficult to compare the results across studies.
Past research showed that patients with a higher grade of pressure injury tend to have more co-morbidities and poorer prognosis, hence naturally would incur higher costs as their wounds take a longer time to heal and they have a longer LOS6,9. However, the hospitalisation fees and LOS of our patients with stage 3 and above HAPI were relatively lower as compared to patients with stage 2 HAPI. This could be due to the small number of our patients with stage 3 and above HAPI. Also, data on other outcomes such as mortality was not collected. HAPI had been associated with higher risk of death for patients11. Our recruited patients with stage 3 and above HAPI might have passed away during the hospitalisation and henceforth resulting in the lower hospitalisation costs and shorter LOS as compared to those with a stage 2 HAPI.
Besides, the proposed study only took into account the cost of providing care (reflected in gross hospitalisation fees) in the inpatient acute care setting. We recognised that a significant proportion of the cost of pressure injuries was likely to be accrued after the patient was discharged. We were also unable to account for the difference in amenities charges across the different ward types in this study.
Conclusion
Patients with HAPI incurred more direct hospitalisation costs and longer LOS as compared to patients without HAPI. HAPI is expensive for both the patients and the healthcare institutions. This study highlights the importance of preventing HAPI and serve as a basis for future research to look at the cost-effectiveness of pressure injury prevention in the local acute care setting. Our study confirmed that HAPI adds to the economic burden of the healthcare system. However, there needs to be a standardised methodological approach to ease the comparison of healthcare cost across different healthcare systems.
Acknowledgements
The authors would like to thank SingHealth Deputy Group Chief Finance Officer Mr Wong Loong Kin, and Mr Asfak Mundayadankandy Puthiyapurayil (IHIS) for their support of and contributions to this study.
Author(s)
Lim Mei Ling*
RN, BSc
Nursing Division, Singapore General Hospital
Bowyers Block B Level 2, 31 Third Hospital Avenue, Singapore 168753
Email lim.mei.ling@sgh.com.sg
Ang Shin Yuh
RN, MBA
Nursing Division, Singapore General Hospital
* Corresponding author
References
- Agency for Healthcare Research and Quality. Return on Investment Estimation [Internet]. 2016 [cited 2016 Dec 28]. Available from: https://archive.ahrq.gov/professionals/systems/hospital/qitoolkit/f1-returnoninvestment.pdf
- Ministry of Health Singapore. Hospital Admission Guide [Internet]. 2009 [cited 2017 Mar 1]. Available from: https://www.moh.gov.sg/content/dam/moh_web/Publications/Educational Resources/2009/Hospital Admission Guide.pdf
- Ministry of Health Singapore. Hospitalisation and Day Surgery [Internet]. 2014 [cited 2016 Dec 28]. Available from: https://www.moh.gov.sg/content/moh_web/home/pressRoom/Current_Issues/2014/s-3ms-resources/hospitalisation-and-day-surgery.html
- Critical Appraisal Skills Programme (CASP). Economic Evaluations Checklist [Internet]. 2014 [cited 2016 Oct 10]. p. 1–6. Available from: http://media.wix.com/ugd/dded87_3b2bd5743feb4b1aaac6ebdd68771d3f.pdf
- Chan B, Ieraci L, Mitsakakis N, Pham B, Krahn M. Net costs of hospital-acquired and pre-admission PUs among older people hospitalised in Ontario. J Wound Care [Internet]. 2013;22(7):341–2, 344–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24159655
- Dealey C, Posnett J, Walker a. The cost of pressure ulcers in the United Kingdom. J Wound Care [Internet]. 2012;21(6):261–2, 264, 266. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22886290
- Brem H, Maggi J, Nierman D, Rolnitzky L, Bell D, Rennert R et al. High cost of stage IV pressure ulcers. Am J Surg 2011;200(4):473–7.
- Allman RM, Goode PS, Burst N, Bartolucci AA, Thomas DR. Pressure ulcers, hospital complications, and disease severity: impact on hospital costs and length of stay [Internet]. Adv Wound Care 1999;12:22–30. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=10326353
- Schuurman J, Schoonhoven L, Defloor T, van Engelshoven I, van Ramshorst B, Buskens E. Economic evaluation of pressure ulcer care: a cost minimization analysis of preventive strategies. Nurs Econ 2009;27(6):390–400, 415.
- Tan B-K, Tan EW, Chong S-J, Chang VJ. An economic evaluation of chronic wound management in a tertiary hospital. Wound Pract Res 2016;24(3):130–6.
- Lyder CH, Wang Y, Metersky M, Curry M, Kliman R, Verzier NR et al. Hospital-acquired pressure ulcers: results from the national Medicare Patient Safety Monitoring System study. J Am Geriatr Soc 2012 Sep;60(9):1603–8.



