Volume 25 Number 2
Systematic review of the impact and treatment of malnutrition in patients with chronic vascular wounds
Lucy Stopher and Shirley Jansen
Keywords chronic wound, wound healing, malnutrition, vascular.
Abstract
Background: Chronic wounds affect at least 1.9% of the population, significantly impairing quality of life for sufferers and placing a large financial burden on the health system1,2. Adequate nutrition is required for wound healing and many patients with chronic wounds are significantly malnourished.
Methods: A systematic search of the literature was conducted utilising the Medline, PubMed, Cochrane Library and CINAHL Plus databases. The terms malnutrition and nutrition in alternate searches were used in various combinations with the Boolean phrase ‘AND’ to find applicable articles: chronic wound, wound healing, ulcer, diabetic, venous, arterial and foot. A total of 20 articles fit the criteria to review.
Results: This review has established that it is likely that malnutrition contributes to wound severity and limb loss; however, this is only level 3 evidence2-4. This review has identified a paucity of consistent evidence of the influence of nutrition on wound healing.
Conclusions: There are limited good-quality, randomised controlled trials (RCTs) to assess the impact of nutrition or malnutrition on wound healing in patients with vascular wounds. More research is required to evaluate the impact of education and/or supplementation on rates of healing in the different wound types.
Introduction
Malnutrition is known to impair wound healing in patients admitted to hospital and in the community setting5,6. Around 1.9% of the Australian population are known to suffer from leg ulcers, foot wounds and pressure injuries, the management of which imposes a large financial burden on the health care system, with around $2.85 billion per annum spent managing chronic wounds in Australia1. A systematic review was conducted to establish the current evidence regarding the prevalence of malnutrition in patients with chronic vascular wounds and the evidence for management of these patients. Understanding the prevalence of malnutrition in this patient group will enable health care providers to introduce effective screening and educational tools to optimise each patient’s nutritional status. As malnutrition is known to impair wound healing, improvement of nutritional status in patients with chronic vascular wounds should result in faster healing times.
Background
Physiology of wound healing
Wound healing consists of four overlapping phases: haemostasis, inflammation, proliferation and maturation7,8. If these phases progress normally, a patient’s wound will heal without concern. When an injury occurs, the haemostasis phase is initiated, which involves vasoconstriction and activation of platelets at the site to stop bleeding7. Fibrin and growth factors are then released and the wound progresses into the inflammatory stage. Neutrophils, macrophages and lymphocytes work to reduce inflammation and engulf bacteria to prevent infection7. Metalloproteases are essential to wound healing by breaking down the protein, allowing new tissue growth by assisting with angiogenesis, tissue migration, contraction and remodelling8,9. An abundance of metalloproteases in the wound base can lead to protein destruction and has the potential to prevent fibroblast activation and collagen formation, therefore preventing epithelisation and transition into the remodelling phase8,9.
Nutrition can have a significant impact on wound healing. Protein is required for collagen synthesis, so if protein levels are depleted, collagen production will be inadequate and formation of granulation tissue delayed7. If the patient has poor nutritional intake, the release of growth factors into the wound bed is impaired, preventing the progression of the wound from the inflammatory phase7. Malnutrition also reduces the ability to combat increasing bacterial levels, prompting an overstimulation of lymphocytes and neutrophils, keeping the wound in the inflammatory stage of healing7,8. Sufficient intake of protein and essential vitamins and minerals will enable the release of sufficient growth factors and collagen for tissue growth and wound healing7.
Patient knowledge
Patient education regarding the influence of nutrition on wound healing may improve the quantity and quality of oral intake in patients with chronic wounds without other interventions such as supplementation being necessary10. This should then positively impact the wound healing process10.
Assessment of patient knowledge and understanding of the role of nutrition in wound healing needs to be part of future research. Studies may benefit from including a control group who receive education on increasing their intake of certain nutrients through their regular food intake. This may establish whether increased oral intake, instead of costly supplemental drinks, provides the desired benefit of improved health and wound healing. The cost of supplemental drinks can be considerable and would need to be borne by the health care service and/or patient, usually over many weeks.
Access to good nutrition involves a complex set of socio-economic factors, including mobility, co-morbidities, location, isolation, support networks and so on. There may be many barriers to accessing adequate nutrition for wound healing10. These need to be taken into account in study design.
In order to plan further research, a systematic review of the literature was conducted to establish what evidence exists to support the management of this complex patient group.
Literature Review
Search strategy
To establish current best practice, a review of the literature was conducted utilising the Medline, PubMed, Cochrane Library and CINAHL Plus databases. The terms malnutrition and nutrition in alternate searches were used in various combinations with the Boolean phrase ‘AND’ to find applicable articles: chronic wound, wound healing, ulcer, diabetic, venous, arterial and foot. Additional searches with patient education and education were also conducted. The search was limited to the last seven years and papers needed to be available in full text and in the English language.
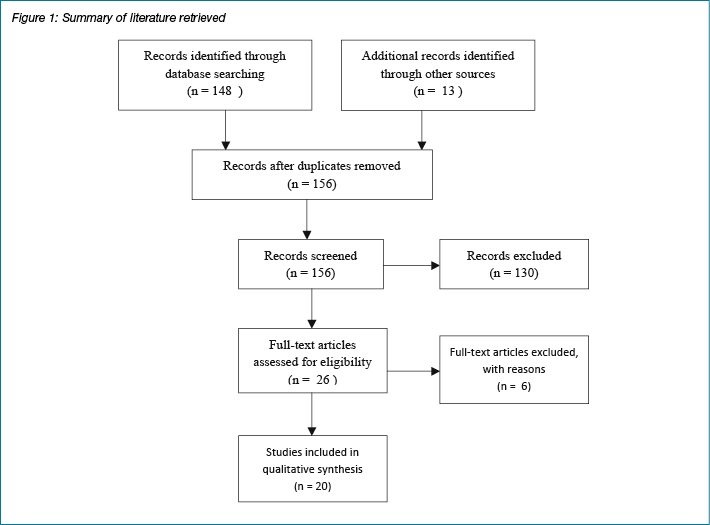
Summary of literature retrieved
A total of 156 articles were found in the initial searches. Of these, 136 papers were found to be irrelevant to the topic; or discussion papers that were not primary studies or literature reviews. Criteria for inclusion were studies assessing the impact of malnutrition or supplemental nutrition on wound healing. When multiples of articles were eliminated, this left 20 articles for analysis. There were: 10 randomised controlled trials (RCTs), four prospective studies, three retrospective studies and three pre- and post-intervention studies.
Impact of malnutrition on wound healing
Gau et al.2 assessed the nutritional status of 478 patients with diabetic foot ulcers in a prospective study and found that malnutrition significantly increased the risk of limb loss2. For every one point decrease in the patient’s malnutrition score, the risk of limb loss increased by 23% (n=150 amputations out of 328 patients, p<0.001)2. This large, well-designed study has given invaluable evidence for the negative effect of malnutrition on outcomes in patients with diabetic foot ulcers2. Wojcik et al.3 conducted a prospective study (n=31), which assessed the nutritional status of patients with chronic venous leg ulcers or pressure ulcers found that "...increasing wound severity was associated with decreased intakes of vitamin A, vitamin K, magnesium, and protein" in the clients’ diet (p<0.001)3. Banks et al.11 found that malnourished patients have an increased risk of developing a pressure injury in a large multicentre study (n=3047). This well-conducted observational study established that the risk and severity of pressure injury increased with the severity of malnourishment as measured with the Subjective Global Assessment Tool (p<0.001)11.
Iizaka et al.12 attempted to establish a visual assessment of a patient’s level of malnutrition by evaluating the colour of the granulation tissue in a patient’s wound. This prospective study on 42 patients found that the colour of granulation tissue was affected by multiple factors including haemoglobin level, presence of diabetes mellitus and dietary intake and therefore not a reliable marker of malnutrition.
The relationship between serum albumin levels and wound healing is a complex one. In a retrospective study of 82 patients, the nutritional supply of the patient did not appear to be related to the serum albumin levels, despite correlation of inflammation and wound healing with serum albumin levels13. It is well documented that serum albumin level is of poor predictive value for nutritional status due to its lack of specificity and, therefore, is unlikely to be a helpful marker in treating malnutrition and promoting wound healing10,14. A large multicentre observational study attempted to assess whether patients’ energy and protein intake could be linked to pressure ulcer severity and healing4. However, this study used serum albumin levels, body mass index and arm circumference to assess each patient’s nutritional status; none of which are validated tools for assessment10,14,15. Although the authors found that patients who had a higher protein and energy diet had a reduction in wound severity, this requires replication utilising an evidence-based malnutrition assessment tool such as the Subjective Global Assessment4.
There is little in the literature pertaining to the prevalence of malnutrition in patients with arterial leg ulcers. This group of elderly patients with multiple co-morbidities and mobility issues are probably at higher risk of malnutrition than patients with other causes for tissue loss16.
Nutritional supplementation strategies
Three RCTs were conducted in rats on diets with varying levels of protein to assess wound healing rates17-19. These three RCTs found that a high-protein diet was associated with statistically significant increased growth factor production, angiogenesis and/or wound contraction rates17-19.
An RCT of 60 patients with pressure ulcers, receiving enteral feeds, were assigned to receive standard nutrition or optimised nutrition which incorporated increased energy and protein20,21. This was reported both as a primary study and separately as a cost-effectiveness study. Patients receiving the optimised feeds were found to have an increased healing rate (p<0.05) which was found to be cost-effective due to reduced requirements for wound care and products20,21. This has demonstrated that, regardless of the level of malnourishment, patients with pressure ulcers benefit from increased calorie and protein intake and that this intervention is cost-effective due to the reduction in wound care products and nursing time20,21. This was supported by a moderately sized, double-blind, RCT of well-nourished patients with Stage three or four pressure injuries receiving oral nutrition supplement or a non-caloric placebo (n=200)22. The authors found that patients receiving the interventional supplement had a significant decrease in wound size (p≤0.016), decreased wound severity (p≤0.033) and decreased time spent on nursing interventions (p≤0.022)22. These two studies suggest that patients with severe pressure ulcers (Stage three or higher) would benefit from nutritional support20,22. Further trials selecting or stratifying for wound aetiology are required to establish whether this should become best practice in wound management.
Cereda et al.23 conducted a moderately sized (n=200), multicentre randomised double-blinded controlled trial comparing the impact of two oral nutritional supplements on wound area reduction and wound healing rates in patients with pressure ulcers. Patients randomised to receive the vitamin-enriched intervention supplement, containing arginine, zinc, selenium and vitamins C and E, demonstrated decreased wound area when compared with the control formula that contained similar protein and caloric content (p=0.017)23.
A study of patients with diabetic foot ulcers assessed wound healing with a nutritional supplement versus a control in an RCT (n=270)24. Although there was no significant improvement in wound healing across the whole group, the patients with reduced peripheral arterial supply (ankle-brachial index of less than 1.0 for the purposes of this trial) and patients with low albumin did show significant improvements in wound healing (p=0.008 and p=0.03 respectively)24. This demonstrates that risk stratification of patients could aid in risk assessment and treatment24. Brewer et al.25 conducted a small pre- and post-intervention study on spinal cord injury patients who had pressure ulcers. The intervention group, who received a supplement containing 9 g of arginine, had a significantly improved healing time (p=0.006). However, a larger trial is required in this area as the control group was not studied prospectively25.
Arginine also decreased pressure ulcer severity in both well nourished (n=11) and malnourished patients (n=12) in a small randomised control trial conducted by Leigh, Desneves26. This trial found that patients receiving 4.5 g or 9 g of arginine daily over three weeks had decreased pressure ulcer severity (p<0.001) with no difference between the doses (p=0.991)26.
A small, single-centre RCT (n=24) compared a standard nutritional supplement with a wound-specific supplement enriched with 4.5 g of arginine. Surprisingly, the standard supplement, which contained similar levels of protein and kilojoules, demonstrated significantly superior wound healing rates than the arginine-enriched wound-specific supplement (p=0.044)27. Wong, Chew-Childs28 hypothesised that nutritional support, supplemented with specialised amino acids, would improve wound healing in patients with pressure ulcers. This was tested on 23 patients with Stage two, three or four pressure ulcers and no statistically significant difference was found in wound severity or size of the wound when compared with patients receiving standard nutritional support (n=23)28. These studies highlight the need for larger RCTs to establish whether arginine and other amino acids play a significant role of wound healing, independent of increased protein or caloric intake.
Patient education
When searching for literature on the education of patients in malnutrition and the effects on wound healing, very little was found. One pilot study, however, investigated the tolerance of a patient educational program regarding nutrition and the impact on prevention of pressure injuries (n=66). This pilot study found improvement in caloric and protein intake of the intervention group between day one and day three of the study (p<0.05)29. It would be beneficial to re-assess these patients at longer follow-up intervals to ensure the intervention has a long-term benefit. Once this pilot study has been trialled on a larger scale, it may enable the program to be trialled in the treatment of various wound aetiologies rather than only prevention of pressure injuries.
Discussion
This review has established that malnutrition contributes to wound severity and limb loss; however, this is only level 3 evidence2-4. Whilst these links between malnutrition and poor wound healing have been consistently reported, this review has identified a paucity of level 1 evidence of the influence of nutrition on wound healing and a lack of standardisation of confounding variables including malnutrition scores and wound healing outcomes. Therefore, there is a poor evidence base upon which to suggest which interventions, if any, are worthwhile pursuing prospectively. Although it is clear that nutritional intervention is important in wound healing, future studies must standardise for confounding variables.
Patients with chronic wounds have an increased risk of infection and increased rate of admission to hospital1. Chronic wounds can be very painful, require frequent dressings and impact significantly on quality of life, particularly the physical, social and psychological domains1. Reduction in the time to heal a chronic wound would therefore benefit the patient and the health care system1. Patients often have multiple contributory factors to poor healing and complex care is required to optimise as many of these factors as possible. Taking some simple steps to recognise and treat malnutrition is possible and may favourably influence wound healing6.
This literature review has identified the potential for health care providers to significantly impact wound healing and patient outcomes by implementing a screening process to identify patients with malnutrition. There is potential for an RCT involving patients with chronic arterial wounds. A three-way RCT would allow high-protein, high-calorie supplementation to be compared with patient education alone and with controls.
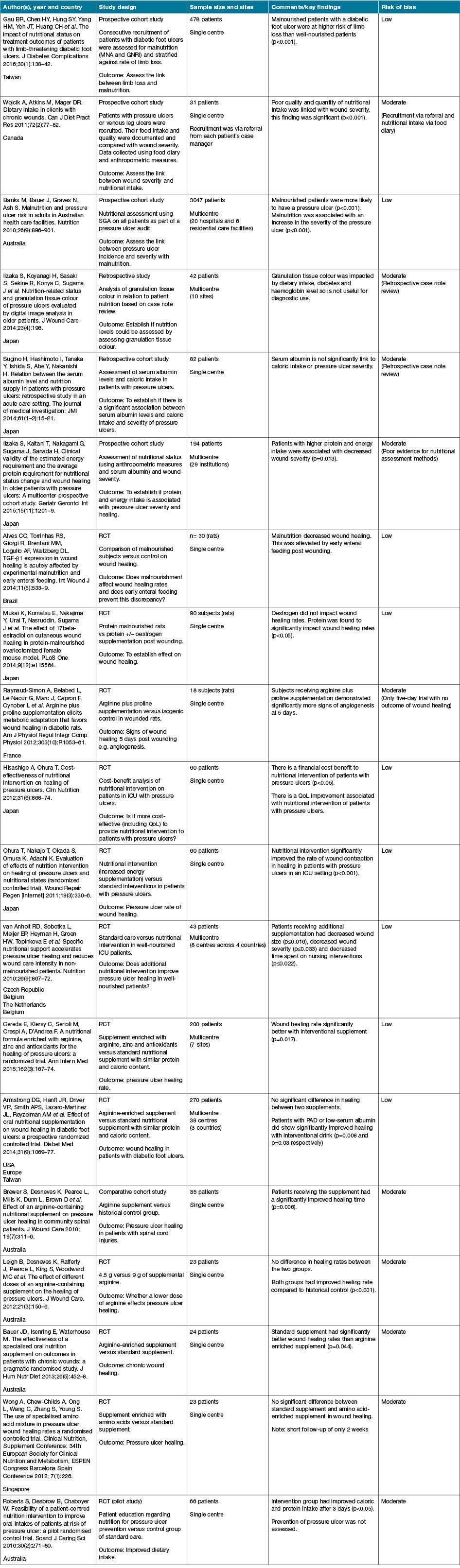
Table 1: Summary of studies
Conclusion
There are limited good-quality RCTs to assess the impact of nutrition or malnutrition on wound healing in patients with diabetic, venous or arterial ulcers. More research is required to evaluate the impact of education and/or supplementation on rates of healing in the different wound types. When planning further research, careful attention to trial design will need to address the multiple factors influencing access to, and intake of, appropriate nutrition in order to minimise confounding factors. This will ensure the results will be a valuable addition to everyday practice.
Author(s)
Lucy Stopher*
BNurs, MClinNurs
Clinical Nurse Consultant
Department of Vascular and Endovascular Surgery, Sir Charles Gairdner Hospital, Perth, WA;
School of Nursing and Midwifery, Edith Cowan University, WA;
Email Lucy.Stopher@health.wa.gov.au
Shirley Jansen
MBChB, FRACS, FRCS, PhD
Department of Vascular and Endovascular Surgery, Sir Charles Gairdner Hospital, Perth, WA;
Centre for Population Health Research, Curtin University, WA;
Faculty of Health and Medical Sciences, University of Western Australia, WA;
Heart Research Institute, Harry Perkins Institute of Medical Research, WA, Australia
* Corresponding author
References
- Kapp S, Santamaria N. Chronic wounds should be one of Australia’s National Health Priority Areas. Aust Health Rev 2015;39(5):600.
- Gau BR, Chen HY, Hung SY et al. The impact of nutritional status on treatment outcomes of patients with limb-threatening diabetic foot ulcers. J Diabetes Complications 2016;30(1):138–42.
- Wojcik A, Atkins M, Mager DR. Dietary intake in clients with chronic wounds. Can J Diet Pract Res 2011;72(2):77–82.
- Iizaka S, Kaitani T, Nakagami G, Sugama J, Sanada H. Clinical validity of the estimated energy requirement and the average protein requirement for nutritional status change and wound healing in older patients with pressure ulcers: A multicenter prospective cohort study. Geriatr Gerontol Int 2015;15(11):1201–9.
- Wu M-L, Courtney MD, Shortridge-Baggett LM, Finlayson K, Isenring EA. Validity of the Malnutrition Screening Tool for older adults at high risk of hospital readmission. J Gerontol Nurs 2012;38(6):38–45.
- Thiruvoth FM, Mohapatra DP, Sivakumar DK, Chittoria RK, Nandhagopal V. Current concepts in the physiology of adult wound healing. Plast Aesthet Res 2015;2:250-6.
- Thompson M, Fitridge R. Mechanisms of Vascular Disease: A Reference Book for Vascular Specialists: University of Adelaide Press; 2011, 587 p.
- Schultz GS, Sibbald RG, Falanga V et al. Wound bed preparation: a systematic approach to wound management. Wound Repair Regen 2003;11(Suppl 1):S1–28.
- Gibson D, Cullen B, Legersetee R, Harding K, Schultz G. MMPs made easy. Wounds Int 2009;1(1).
- Sherman AR, Barkley M. Nutrition and wound healing. J Wound Care 2011;20(8):357.
- Banks M, Bauer J, Graves N, Ash S. Malnutrition and pressure ulcer risk in adults in Australian health care facilities. Nutrition 2010;26(9):896–901.
- Iizaka S, Koyanagi H, Sasaki S et al. Nutrition-related status and granulation tissue colour of pressure ulcers evaluated by digital image analysis in older patients. J Wound Care 2014;23(4):198.
- Sugino H, Hashimoto I, Tanaka Y, Ishida S, Abe Y, Nakanishi H. Relation between the serum albumin level and nutrition supply in patients with pressure ulcers: retrospective study in an acute care setting. J Med Invest 2014;61(1–2):15–21.
- Bouillanne O, Hay P, Liabaud B, Duche C, Cynober L, Aussel C. Evidence that albumin is not a suitable marker of body composition-related nutritional status in elderly patients. Nutrition 2011;27(2):165–9.
- Isenring EA, Bauer JD, Banks M, Gaskill D. The Malnutrition Screening Tool is a useful tool for identifying malnutrition risk in residential aged care. J Hum Nutr Diet 2009;22(6):545–50.
- Molnar JA, Underdown MJ, Clark WA. Nutrition and chronic wounds. Adv Wound Care 2014;3(11):663–81.
- Alves CC, Torrinhas RS, Giorgi R, Brentani MM, Logullo AF, Waitzberg DL. TGF-β1 expression in wound healing is acutely affected by experimental malnutrition and early enteral feeding. Int Wound J 2014;11(5):533–9.
- Mukai K, Komatsu E, Nakajima Y et al. The effect of 17beta-estradiol on cutaneous wound healing in protein-malnourished ovariectomized female mouse model. PLoS One 2014;9(12):e115564.
- Raynaud-Simon A, Belabed L, Le Naour G et al. Arginine plus proline supplementation elicits metabolic adaptation that favors wound healing in diabetic rats. Am J Physiol Regul Integr Comp Physiol 2012;303(10):R1053–61.
- Hisashige A, Ohura T. Cost-effectiveness of nutritional intervention on healing of pressure ulcers. Clin Nutrition 2012;31(6):868–74.
- Ohura T, Nakajo T, Okada S, Omura K, Adachi K. Evaluation of effects of nutrition intervention on healing of pressure ulcers and nutritional states (randomized controlled trial). Wound Repair Regen [Internet]. 2011;19(3):[330–6 pp.]. Available from: http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/239/CN-00783239/frame.html.
- van Anholt RD, Sobotka L, Meijer EP et al. Specific nutritional support accelerates pressure ulcer healing and reduces wound care intensity in non-malnourished patients. Nutrition 2010;26(9):867–72.
- Cereda E, Klersy C, Serioli M, Crespi A, D’Andrea F. A nutritional formula enriched with arginine, zinc, and antioxidants for the healing of pressure ulcers: a randomized trial. Ann Intern Med 2015;162(3):167–74.
- Armstrong DG, Hanft JR, Driver VR et al. Effect of oral nutritional supplementation on wound healing in diabetic foot ulcers: a prospective randomized controlled trial. Diabet Med 2014;31(9):1069–77.
- Brewer S, Desneves K, Pearce L et al. Effect of an arginine-containing nutritional supplement on pressure ulcer healing in community spinal patients. J Wound Care [Internet]. 2010; 19(7):[311–6 pp.]. Available from: http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/834/CN-00759834/frame.html.
- Leigh B, Desneves K, Rafferty J et al. The effect of different doses of an arginine-containing supplement on the healing of pressure ulcers. J Wound Care 2012;21(3):150–6.
- Bauer JD, Isenring E, Waterhouse M. The effectiveness of a specialised oral nutrition supplement on outcomes in patients with chronic wounds: a pragmatic randomised study. J Hum Nutr Diet 2013;26(5):452–8.
- Wong A, Chew-Childs A, Ong L, Wang C, Zhang S, Young S. The use of specialised amino acid mixture in pressure ulcer wound healing rates a randomised controlled trial. Clin Nutrition Supplement Conference: 34th European Society for Clinical Nutrition and Metabolism, ESPEN Congress Barcelona Spain Conference Start: 20120908 Conference End: 20120911 Conference Publication: (varpagings) [Internet]. 2012; 7(1):[226 p.]. Available from: http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/756/CN-00835756/frame.html.
- Roberts S, Desbrow B, Chaboyer W. Feasibility of a patient-centred nutrition intervention to improve oral intakes of patients at risk of pressure ulcer: a pilot randomised control trial. Scand J Caring Sci 2016;30(2):271–80.



