Volume 25 Number 4
Evidence summary: Pressure Injuries: preventing heel pressure injuries with prophylactic dressings
Emily Haesler
November 2017
Clinical question
What is the best available evidence on prophylactic dressings to prevent pressure injuries (PIs) of the heel?
Summary
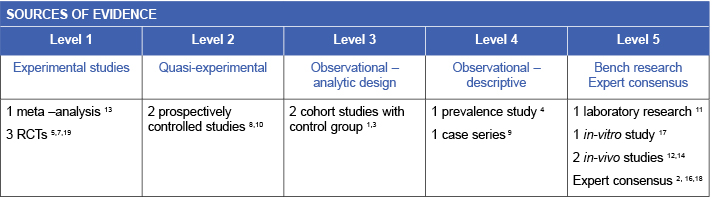
Heels are a common anatomical location in which PIs occur. Due to their small surface area and minimal tissue protection over the bony prominence, interface pressure at the heel is high when an individual is lying in bed, particularly when that individual has reduced mobility1 (Level 3.c evidence). There is evidence to indicate that suspending the heels using a foam cushion block2 or heel suspension boots2-4 reduces the incidence of heel PIs (Level 1.c evidence).
Clinical practice recommendations
- Apply a prophylactic dressing to the heels to prevent heels PIs in individuals with limited mobility, particularly those in critical care or undergoing surgery. (Grade B)
- Consider selecting a multi-layer polyurethane foam dressing with a silicone border for preventing heel PIs due to its construction qualities. (Grade B)
Considerations when using prophylactic dressings on the heels
The following recommended practices should be considered when using prophylactic dressings:
- Inspect skin underneath the prophylactic dressing at least daily.2 Some prophylactic dressings are designed to be easily removed and reapplied to facilitate skin inspection without causing medical adhesive related skin injury2, 11 (Level 5).
- Prophylactic dressings with multiple layers may be more effective in reducing the impact of pressure, shear and friction forces on the skin11-14 (Levels 1 and 5).
- Consider the effect of a prophylactic dressing on skin microclimate.15 Ability to absorb moisture is thought to contribute to the efficacy of a prophylactic dressing7, 16, 17 (Level 5).
- Consider applying a net stocking or over the prophylactic dressing to protect the dressing.3, 5, 7, 9 (Levels 1, 3 and 4).
- Apply the prophylactic dressing to clean, dry skin.18 (Level 5)
- Continue to use a pressure redistribution support surface and elevate the heels in conjunction with a prophylactic dressing2 (Level 5).
- Using a prophylactic dressing on the heels is likely to be cost-effective.5, 19 (Level 1)
Background
The heel is an anatomical location that experiences a high incidence of PIs due to its small surface area and low amount of subcutaneous tissue over the bony prominence.2,3 The heel is afforded minimal protection from tissue while sustaining high levels of interface pressure,1 particularly when the individual is in supine position. During both intended and unintended movement in a bed, the heel is susceptible to friction and shear, further increasing the risk of PI development. Large prevalence studies have identified that the heels closely follow the sacrum as the second most common anatomical location for PIs.4, 5 Individuals with reduced mobility, particularly individuals who are sedated, are at the highest risk of heel PIs.2, 6
Evidence
Prophylactic dressings to prevent heel pressure injuries
Applying preventive dressings to the heel appears to relieve shear and friction forces. There is evidence that a prophylactic dressing applied to the heels is effective in reducing the incidence of heel PIs in immobile individuals in critical care7,8 (Levels 1 and 2) or long term care3, 5, 9 (Levels 1, 3 and 4). Evidence for effectiveness of different types of prophylactic dressings is reported below.
Polyurethane foam dressings
Application of a multi-layer polyurethane foam dressing with a silicone border to volunteers with healthy skin decreased the interface pressure between the heel and a standard viscoelastic hospital mattress.1 (Level 3).
A multi-layer polyurethane foam dressing with a silicone border applied to the heels appears to be effective in reducing incidence of heel PIs in the intensive care unit (ICU). A comprehensive protocol that included regular skin assessment, the prophylactic dressing and a pressure redistribution support surface decreased incidence of heel PIs by about 9% compared with no prophylactic dressing (3.1% versus 12.5%, p=0.002). When combined with a sacral prophylactic dressing, the number needed to treat to prevent one PI was ten7 (Level 1).
A multi-layer foam hydrocellular prophylactic dressing also showed good effect in a long term care setting when compared to simple protective bandaging (3% versus 44%, relative risk [RR] 13.42, 95% confidence interval [CI] 3.31 to 54.3)5 (Level 1).
A hydropolymer foam dressing applied to the heels of individuals undergoing surgical procedures anticipated to take longer than 90 minutes (n=117) was associated with a significantly lower rate of heel PIs (8.5% versus 36.5%, p=not reported) compared with individuals who had shorter surgery duration and received no preventive dressing (n=23). Selective use of other preventive interventions may have influenced the results10 (Level 2).
Polyurethane film
A polyurethane film has also been trialled for preventing PIs for individuals in critical care. After a mean hospital stay of 24 days, fewer heels that received a prophylactic film dressing had a PI (6% versus 18%, p<0.001). The mean time to experience a PI for heels treated with the prophylactic polyurethane film dressing was 19.2 days (95% CI 17.3 to 21). Concurrent management strategies were not clearly reported8 (Level 2).
Protective bandaging
Use of gauze pads and wraps bandaged around the heel and ankle was not as effective as a multi-layer foam hydrocellular prophylactic dressing in long term care settings. Over 40% of individuals treated with a protective bandage experience a heel PI, compared to only 3% who received the prophylactic dressing (RR 13.42, 95% CI 3.31 to 54.3). An economic analysis showed an overall higher financial cost associated with bandaging, when considering material costs and labour5 (Level 1).
Heel pads
Silicone heel pads designed to fit over the heel and held in place with tubular bandages appear to have some impact on reducing damage to subcutaneous heel tissue, potentially preventing development of heel PIs. Two reports on the intervention indicated positive findings for dermal water content at the heel, assessed using deep ultrasound for older adults who wore the device for one month. The impact on heel PI incidence was not reported3, 9 (Levels 3 and 4).
Methodology
This evidence summary is based on a structured database search combining search terms that describe heel PIs with search terms related to prophylactic dressings. Searches were conducted in EMBASE, Pubmed, Medline, Scopus and the Cochrane Library. Evidence published up to June 2017 in English was considered for inclusion. Retrieved studies were appraised for relevance and rigour using Joanna Briggs Institute appraisal tools. 20
Author(s)
Emily Haesler
References
- Miller SK, Sharma N, Aberegg LC, Blasiole KN, Fulton JA. Analysis of the Pressure Distribution Qualities of a Silicone Border Foam Dressing. Journal of Wound, Ostomy, & Continence Nursing, 2015. Jul-Aug;42(4):346-51.
- National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel, Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Haesler E, editor. Osborne Park, Western Australia: Cambridge Media; 2014.
- Knowles A, Young S, Collins F, Hampton S. Report on a clinical evaluation of the KerraPro Heel silicone heel pad. Journal of Wound Care, 2013;22(11):599-607.
- Vanderwee K, Clark M, Dealy C, Gunningberg L, Defloor T. Pressure ulcer prevalence in Europe: a pilot study. J Eval Clin Pract, 2007;13(2):227-32.
- Bou JET, Rueda López J, Camañes G, Herrero Narváez E, Blanco Blanco J, Ballesté Torralba J, Martinez-Esparza EH, García LS, Soriano JV. Preventing pressure ulcers on the heel: a Canadian cost study. Dermatol Nurs, 2009;21(5):268.
- Rajpaul K, Acton C. Using heel protectors for the prevention of hospital-acquired pressure ulcers. Br J Nurs, 2016. Mar;25(6 Suppl):S18-26.
- Santamaria N, Gerdtz M, Sage S, McCann J, Freeman A, Vassiliou T, De Vincentis S, Ng AW, Manias E, Liu W, Knott J. A randomised controlled trial of the effectiveness of soft silicone multi-layered foam dressings in the prevention of sacral and heel pressure ulcers in trauma and critically ill patients: the border trial. Int Wound J, 2015;12(3):302-8.
- Souza TSd, Reichembach Danski MT, Johann DA, Marques De Lazzari LS, Mingorance P. Prevention’s pressure ulcers heel with transparent polyurethane film. Acta Paulista de Enfermagem, 2013;26(4):345-52.
- Knowles A, Skinner R, Young S, Hampton S. Pressure-reducing pads effectively prevent and reverse signs of category 1 pressure damage. Journal of Community Nursing, 2013;27(4):52-9.
- Bots CM, Apotheker BFG. The prevention of heel pressure ulcers using a hydropolymer dressing in surgical patients Journal of Wound Care, 2004;13(9):375-8.
- Call E, Pedersen J, Bill B, Black J, Alves P, Brindle CT, Dealey C, Santamaria N, Clark M. Enhancing pressure ulcer prevention using wound dressings: what are the modes of action? Int Wound J, 2015;12:408-13.
- de Wert LA, Schoonhoven L, Stegen JHCH, Piatkowski AA, van der Hulst RR, Poeze M, Bouvy ND. Improving the effect of shear on skin viability with wound dressings. J Mech Behav Biomed Mater, 2016. July 01;60:505-14.
- Huang L, Woo KY, Liu LB, Wen RJ, Hu AL, Shi CG. Dressings for preventing pressure ulcers: A Meta-analysis. Advances in Skin and Wound Care, 2015;28(6):267-73.
- Levy A, Frank MBO, Gefen A. The biomechanical efficacy of dressings in preventing heel ulcers. Journal of Tissue Viability, 2015;24(1):1-11.
- Evan C, Justin P, Brian B, Craig O, Martin F-P. Microclimate impact of prophylactic dressings using in vitro body analog method. Wounds, 2013;25(4):94-103.
- Black J, Alves P, Brindle CT, Dealey C, Santamaria N, Call E, Clark M. Use of wound dressings to enhance prevention of pressure ulcers caused by medical devices. Int Wound J, 2015;12(3):322-7.
- Call E, Pedersen J, Bill B, Oberg C, Ferguson-Pell M. Microclimate impact of prophylactic dressings using in vitro body analog method. Wounds 2013;25(4):94-103.
- Black J, Clark M, Dealey C, Brindle CT, Alves P, Santamaria N, Call E. Dressings as an adjunct to pressure ulcer prevention: Consensus panel recommendations. Intl Wound J, 2015;12(4):484-8.
- Santamaria N, Liu W, Gerdtz M, Sage S, McCann J, Freeman A, Vassiliou T, Devincentis S, Ng AW, Manias E, Knott J, Liew D. The cost-benefit of using soft silicone multilayered foam dressings to prevent sacral and heel pressure ulcers in trauma and critically ill patients: A within-trial analysis of the border trial. Int Wound J, 2015;12(3):344-50.
- The Joanna Briggs Collabortion. Handbook for Evidence Transfer Centers – Version 4. The Joanna Briggs Institute, Adelaide. 2013.



