Volume 25 Number 4
Evidence Summary: Pressure Injuries: Preventing heel pressure injuries with positioning
Emily Haesler
November 2017
Clinical question
What is the best available evidence on positioning strategies to prevent pressure injuries (PIs) of the heel?
Summary
Heels are a common anatomical location in which PIs occur. Due to their small surface area and minimal tissue protection over the bony prominence, interface pressure at the heel is high when an individual is lying in bed, particularly when that individual has reduced mobility1 (Level 3c evidence). There is evidence to indicate that suspending the heels using a foam cushion block2 or heel suspension boots2-4 reduces the incidence of heel PIs (Level 1c evidence).
Clinical practice recommendations
Offload the heels completely by distributing weight along the leg and positioning the knee in slight flexion. (Grade A)
Offload the heels using a device specifically designed for heel elevation. (Grade B)
Considerations in elevating the heels
The following recommended practices should be considered when using heel suspension devices:
- Inspect skin underneath the device at regular intervals5 (Level 5b evidence).
- Ensure that a heel suspension device is not applied too tightly, or there is a risk of PIs developing as a result of device application5 (Level 5b evidence).
- Avoid using water filled gloves or intravenous fluid bags to elevate the heels as they place undue pressure on the Achilles tendon3 (Level 5c evidence).
- Avoid pressure damage to the Achilles tendon by elevating the entire calf5 (Level 5.b evidence).
- Avoid popliteal vein compression and risk of deep vein thrombosis by positioning the knees in 5° to 10° flexion16 (Level 3e evidence).
- Consider the effect of the device on the skin microclimate. If the device significantly increases moisture and skin temperature it may not be appropriate15 (Level 5c evidence).
- Use a pressure redistribution support surface in conjunction with heel elevation5 (Level 5b evidence).
Background
The heel is an anatomical location that experiences a high incidence of PIs due to its small surface area and low amount of subcutaneous tissue over the bony prominence.5,6 The heel is afforded minimal protection from tissue while sustaining high levels of interface pressure,1 particularly when the individual is in supine position. During both intended and unintended movement in a bed, the heel is susceptible to friction and shear, further increasing the risk of PI development. Large prevalence studies have identified that the heels closely follow the sacrum as the second most common anatomical location for PIs.7, 8 Individuals with reduced mobility, particularly individuals who are sedated, are at the highest risk of heel PIs.5, 9
Evidence
Positioning to prevent heel pressure injuries
Suspending, or “floating” the heels clear of the support surface by elevating the lower leg/calf is demonstrated to be an effective strategy to relieve pressure, shear and friction forces, thereby reducing the risk of heel PIs. There is evidence that heel interface pressures can be reduced with elastic gel mats, leg elevation devices and gel heel blocks,10 but translation to a reduction in heel PIs is not reported (Level 3c evidence). Evidence for effective repositioning interventions is reported below.
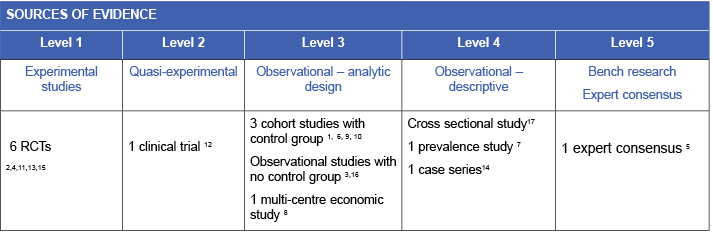
Heel suspension boots
Heel suspension boots designed from egg-crate foam to suspend the foot on an elevated pad within a protected boot space that extended up the lower leg were found to be effective in reducing the incidence of heel PIs. In this trial, older adults aged above 65 years who had undergone hip fracture surgery were randomised to the intervention (heel suspension boot, n=120) or no heel elevation device (n=119). All participants were cared for on a pressure redistribution support surface. There were no new heel PIs in the intervention group compared with 29 heel PIs (category 1 or greater) in the control group (p<0.001)4 (Level 1c evidence).
Heel suspension boots designed from polyurethane foam have been trialled in older adults. The suspension boots were applied in the ambulance and worn throughout the stay in hospital. All individuals received ongoing skin and risk assessments. Heel PIs occurred less often in individuals wearing suspension boots compared to those with no heel elevation (14.6% versus 30%, p=0.017)11 (Level 1c evidence).
The results from a study12 that compared heel suspension boots to intravenous fluid bags concurred that specially designed suspension boots are more effective (0% versus 40%, p=0.006) in preventing heel PIs (Level 2c evidence).
An observational study found zero incidence of pressure ulcers and a 50% reduction in plantar flexion contractures in sedated individuals who wore a heel elevation boot3 (Level 3.e evidence). A quality improvement report demonstrated that use of heel suspension boots for individuals at high risk of heel PI was associated with a 44% reduction in any heel PI and a 67% reduction in full thickness PIs over 12 months9 (Level 3c evidence).
It appears that there is no significant difference between different models of heel suspension boot for efficacy in preventing heel PIs13 (Level 1c evidence).
Foam cushions
A foam block cushion that supported the entire lower leg, thereby floating the heels, used with a second foam block that supported the feet to prevent foot drop was shown to be more effective in reducing incidence of heel PI than no heel elevation.2 The participants, who were all assessed as having high risk of PI, were cared for on a water mattress. There was a significant reduction in rate of any heel PI associated with heel elevation on a foam cushion (8.6% versus 55.4%, p<0.0001)2 (Level 1c evidence).
Use of an ‘eggshell’ foam pressure redistribution mat under the feet of 50 individuals at high risk of heel and/or malleoli PIs or other types of foot ulcer was reported to have positive outcomes, Individuals with impaired skin integrity at commencement of the trial showed improvements, and no individuals developed heel PIs14 (Level 4c evidence).
Standard pillows
Standard pillows were found to be as effective as a heel suspension boot in preventing PIs in one small study, but the results were unreliable due to the small sample size and method of applying the heel suspension device15 (Level 1c evidence).
There is some evidence that a standard pillow may be unreliable in maintaining the heels in an elevated position for extended periods of time, especially in more mobile individuals, or those with dementia or agitation/leg spasms.3, 4 Because pillows can be easily relocated from the heels for other positioning purposes, they may also be inappropriate for use in immobile, sedated individuals13 (Level 5b evidence).
Methodology
This evidence summary is based on a structured database search combining search terms that describe heel PIs with search terms related to positioning and suspension devices. Searches were conducted in EMBASE, Pubmed, Medline, Scopus and the Cochrane Library. Evidence published up to June 2017 in English was considered for inclusion. Retrieved studies were appraised for relevance and rigour using Joanna Briggs Institute appraisal tools.
Author(s)
Emily Haesler
References
- Miller SK, Sharma N, Aberegg LC, Blasiole KN, Fulton JA. Analysis of the Pressure Distribution Qualities of a Silicone Border Foam Dressing. Journal of Wound, Ostomy, & Continence Nursing, 2015. Jul-Aug;42(4):346-51.
- Cadue JF, Karolewicz S, Tardy C, Barrault C, Robert R, Pourrat O. Prevention of heel pressure sores with a foam body-support device. A randomized controlled trial in a medical intensive care unit. La Presse Médicale, 2008;37(1 Pt 1):30-6.
- Meyers TR. Preventing heel pressure ulcers and plantar flexion contractures in high-risk sedated patients. J Wound Ostomy Continence Nurs, 2010;37(4):372-8.
- Donnelly J, Winder J, Kernohan WG, Stevenson M. An RCT to determine the effect of a heel elevation device in pressure ulcer prevention post-hip fracture. J Wound Care, 2011;20(7):309.
- National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel, Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Haesler E, editor. Osborne Park, Western Australia: Cambridge Media; 2014.(Levels1.b and 5.b evidence).
- Knowles A, Young S, Collins F, Hampton S. Report on a clinical evaluation of the KerraPro Heel silicone heel pad. Journal of Wound Care, 2013;22(11):599-607.
- Vanderwee K, Clark M, Dealy C, Gunningberg L, Defloor T. Pressure ulcer prevalence in Europe: a pilot study. J Eval Clin Pract, 2007;13(2):227-32.
- Torra I Bou JE, Rueda López J, Camañes G, Herrero Narváez E, Blanco Blanco J, Ballesté Torralba J, Martinez-Esparza EH, García LS, Soriano JV. Preventing pressure ulcers on the heel: a Canadian cost study. Dermatol Nurs, 2009;21(5):268.
- Rajpaul K, Acton C. Using heel protectors for the prevention of hospital-acquired pressure ulcers. Br J Nurs, 2016. Mar;25(6 Suppl):S18-26.
- Malkoun M, Huber J, Huber D. A comparative assessment of interface pressures generated by four surgical theatre heel pressure ulcer prophylactics. Int Wound J, 2012;9(3):259-63.
- Baath C, Engstrom M, Gunningberg L, Muntlin Athlin A. Prevention of heel pressure ulcers among older patients - from ambulance care to hospital discharge: A multi-centre randomized controlled trial. Appl Nurs Res, 2016. May;30:170-5.
- Bales I. A comparison between the use of intravenous bags and the Heelift suspension boot to prevent pressure ulcers in orthopedic patients. Adv Skin Wound Care, 2012;25(3):125-31.
- Gilcreast DM, Warren JB, Yoder LH, Clark JJ, Wilson JA, Mays MZ. Research comparing three heel ulcer-prevention devices. J Wound Ostomy Continence Nurs, 2005;32(2):112-210.
- Bateman SD. Utilising a foam positioning device for preventing pressure ulcers on the feet. Wounds UK, 2014;10(1):78-83.
- Tymec AC, Pieper B, Vollman KA. Comparison of two pressure-relieving devices on the prevention of heel pressure ulcers. Adv Wound Care, 1997;10(1):39-44.
- Huber DE, Huber JP. Popliteal vein compression under general anaesthesia. Eur J Vasc Endovasc Surg, 2009;37(4):464-9.
- Knowles A, Young S, Collins F, Hampton S. Report on a clinical evaluation of the KerraPro Heel silicone heel pad. J Wound Care, 2013;22(11):599-607.
- The Joanna Briggs Collaboration. Handbook for Evidence Transfer Centers – Version 4. The Joanna Briggs Institute, Adelaide. 2013.



