Volume 26 Number 1
Evidence summary: Pressure injuries: active support surfaces for preventing and treating pressure injuries
Emily Haesler
Keywords pressure injury, pressure ulcer, decubitus ulcer, support surface, alternating pressure, low air loss
Feb 2018
Questions
What is the best available evidence on active support surfaces to reduce the risk of pressure injuries (PIs)?
What is the best available evidence on active support surfaces to promote healing for existing PIs?
Summary
Active support surfaces are technologically advanced mattress or bed systems designed to promote pressure redistribution and microclimate control, thereby reducing the risk of PIs, or promoting healing in existing PIs. There is good evidence that an alternating pressure mattress is superior to a standard hospital mattress1 (Level 1a evidence). There is also evidence that alternating pressure mattresses and other types of active support surfaces are not inferior to high specification foam mattresses and other reactive support surfaces for preventing PIs1 (Level 1.c evidence). Some evidence suggests existing PIs may have faster healing rates on an active support surface2-5 (Level 1c evidence).
Clinical practice recommendations
- Consider using an alternating pressure support surface for individuals at high risk of developing a PI, particularly when regular repositioning is not possible. (Grade B)
- Consider using an active support surface for individuals with a full thickness PI, particularly when regular repositioning is not possible. (Grade B)
Background
Active support surfaces are support surfaces that provide a high technology option for mattress and bed system design.1, 6 An active support surface is a powered surface that alternates the anatomical area sustaining the highest applied pressure loads.6 This category of support surfaces includes alternating pressure mattresses, low air loss beds and air-fluidised beds. In contrast, a reactive support surface only changes the pressure distribution in reaction to the applied load.6
Alternating air pressure mattresses are designed with air cells of various number and size that inflate and deflate on programmed cycles, alternating the anatomical region subjected to the highest interface pressures. While evidence in the past suggested that air mattresses with smaller cells were insufficient in achieving adequate reduction in interface pressure,6 this guidance is not relevant to modern alternating pressure mattresses that are more advanced than early models.7 An air-fluidised support surface is a fluid-like surface achieved by forcing air into beads and a low air loss surface has a continuous flow of air. These surfaces are designed to increase immersion and envelopment,7 and many also have features that control microclimate.6
Evidence
Alternating pressure mattresses compared with standard foam mattresses
A Cochrane review1 reported a meta-analysis of two small randomised controlled trials (RCTs) comparing alternating pressure air mattress and standard hospital mattresses in individuals with high PI. Pooled findings indicated that alternating pressure mattresses were associated with a lower risk of developing any PI (relative risk [RR] 0.31, 95% confidence interval [CI] 0.17 to 0.58, p<0.0001)1 (Level 1a evidence).
Alternating pressure mattresses compared with other reactive support surfaces
The Cochrane review1 reported nine RCTs that compared an alternating pressure mattress to a reactive support surface, including water mattresses, static air mattresses and high specification viscoelastic foam mattresses. None of these individual studies identified differences in PI rates1 (non-pooled data, level 1c evidence).
The review presented a meta-analysis of four RCTs comparing alternating pressure mattresses to high specification foam mattress overlays, which showed no significant difference in PI risk (relative risk [RR] 0.91 95%, CI 0.72 to 1.16)1 (Level 1a evidence).
However, one recent RCT8 (N=76) comparing an alternating pressure air mattress with a high specification viscoelastic foam mattress found an effect for the alternating pressure mattress. Rate of PIs was higher using the high specification foam mattress (35.1% versus 5.1%), translating to a 7 to 8 times lower risk of experiencing a PI if an alternating pressure mattress was used (hazard ratio 7.57, 95% CI 1.67 to 34.38, p=0.009). The participants were older adults in long term aged care and had been assessed as being at high risk of a PI (Braden scale score ≤ 14), but without an existing PI. In this trial, concurrent preventive strategies including regular repositioning were performed infrequently,8 which may have contributed to the findings (Level 1c evidence).
Lower level evidence reporting outcomes for older adults at high risk of PI reported effectiveness of alternating pressure mattresses in preventing new PI development or preventing worsening of skin condition. These studies were conducted over up to three months and had no comparator groups9, 10 (Level 3.e, and 4.b & 4.d evidence respectively).
Low air loss beds and air fluidised beds
The evidence on low air loss beds and air fluidised beds reports effectiveness of these products in promoting superior outcomes for individuals with existing Stage 2 or greater PIs compared with other active support surfaces and standard hospital mattresses2-5 (Level 1c evidence). Improved likelihood of reaching full healing5 and faster PI healing rates2-4 have been reported (Level 1.c evidence). Reduced rate of PI-related hospital admissions11 and healthcare resources4, 11 have also been reported when air fluidised beds were used to manage individuals with existing PIs (Level 1c evidence).
Most of the available evidence on these types of support surfaces was published over 20 years ago and report dated technologies and comparator support surfaces. There is no recent evidence comparing low air loss beds and air fluidised beds with contemporary high specification foam mattresses.
Considerations in using active support surfaces
The following recommended practices should be considered when using active support surfaces:6 (Level 5b evidence)
- Regularly evaluate PI risk and skin condition and re-evaluate the support surface if pressure redistribution is inadequate for the individual’s needs.
- Regularly reposition individuals where possible, avoiding positioning on an existing PI.
- Check that the support surface does not bottom out in any bed configuration (i.e. inclined or flat).
- Ensure that active support surfaces are maintained according to manufacturer’s instructions.
Methodology
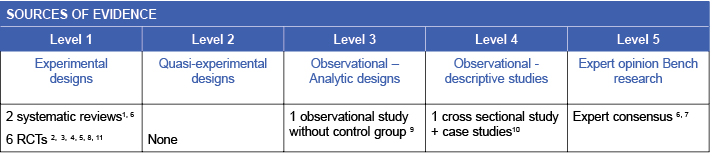
This evidence summary is based on a structured database search combining search terms that describe pressure injuries with search terms related to support surfaces. Searches were conducted in EMBASE, PubMed, Medline, Scopus and the Cochrane Library. Evidence published up to June 2017 in English was considered for inclusion. The development of this evidence summary is based on the Joanna Briggs Institute methodology.12
Related evidence summaries
JBI 18874 Pressure injuries: Preventing heel pressure injuries with positioning
JBI 18875 Pressure injuries: Preventing heel pressure injuries with prophylactic dressings
JBI 18873 Pressure injuries: Preventing medical device related pressure injuries

Author(s)
Emily Haesler
Wound Healing and Management Node
References
- McInnes E, Jammali-Blasi A, Bell-Syer SEM, Dumville JC, Middleton V, Cullum N. Support surfaces for pressure ulcer prevention. Cochrane Database Syst Rev, 2015;9(CD001735). (Level 1a evidence).
- Munro BH, Brown L, Heitman BB. Pressure ulcers: one bed or another? Geriatr Nurs, 1989;10(4):190-2. (Level 1c evidence).
- Allman RM, Walker JM, Hart MK, Laprade CA, Noel LB, Smith CR. Air-fluidized beds or conventional therapy for pressure sores. A randomized trial. Ann Intern Med, 1987;107(5):641-8. (Level 1c evidence).
- Jackson BS, Chagares R, Nee N, Freeman K. The effects of a therapeutic bed on pressure ulcers: an experimental study. J Enterostomal Ther, 1988;15(6):220-6. (Level 1c evidence).
- Ferrell BA, Osterweil D, Christenson P. A randomized trial of low-air-loss beds for treatment of pressure ulcers. JAMA, 1993;269(4):494-7. (Level 1c evidence).
- National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel, Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Haesler E, editor. Osborne Park, Western Australia: Cambridge Media; 2014.(Level 1b and 5b evidence).
- National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel, Pan Pacific Pressure Injury Alliance. 2016. Small Cell Technology in Alternating Pressure Mattresses. Available from: http://internationalguideline.com/statements#small_cell. [Accessed 2017 September] (Level 5b evidence).
- Sauvage P, Touflet M, Pradere C, Portalier F, JMichel J-M, Charru P, Passadori Y, Fevrier R, Hallet-Lezy A-M, Beauchêne F, Scherrer B. Pressure ulcers prevention efficacy of an alternating pressure air mattress in elderly patients: E²MAO a randomised study. J Wound Care, 2017;26(6):304-12. (Level 1c evidence).
- Meaume S, Marty M. Pressure ulcer prevention and healing using alternating pressure mattress at home: the PARESTRY project. J Wound Care, 2015;24(8):359-65. (Level 3e evidence).
- Gleeson D. Evaluating an alternating mattress on an elderly rehabilitation ward. Br J Nurs, 2015;24(12):S42-7. (Levels 4b & 4d evidence).
- Strauss MJ, Gong J, Gary BD, Kalsbeek WD, Spear S. The cost of home air-fluidized therapy for pressure sores. A randomized controlled trial. J Fam Pract, 1991;33(1):52-9. (Level 1c evidence).
- The Joanna Briggs Collaboration. Handbook for Evidence Transfer Centers – Version 4. The Joanna Briggs Institute, Adelaide. 2013.



