Volume 26 Number 3
Nurse practitioners and their use of low-frequency ultrasound debridement in the management of chronic wounds
Keryln Carville, Liz Howse, Margaret Edmondson, Gordana Petkovska, Pam Morey, Cate Maguire and Ann Tuvik
Keywords Nurse Practitioner, low-frequency ultrasound debridement.
Abstract
Acute and chronic wounds constitute a considerable care challenge and a financial burden on the health system and wounded individuals, regardless of care setting. The explicit and implicit costs associated with chronic wounds can be monumental, as are the detrimental impacts on a person’s quality of life and wellbeing. A nurse practitioner (NP) coordinated Advanced Wound Assessment Service was established by Silver Chain in Perth, in March 2013. Ongoing successful client outcomes for those with previous non-healing wounds led to an expansion in this service with three clinics and the employment of four NPs. The criteria for referral to a NP is a non-healing or deteriorating wound or an atypical clinical presentation. The NPs work in collaboration with the client, community nursing teams, general practitioners, medical specialists and allied health professionals to develop and implement evidence-based management plans that improve healing outcomes, prevent complications and reduce hospital admissions. They undertake comprehensive assessments and, when clinically indicated, they utilise contact low-frequency ultrasound debridement (LFUD) for the removal of necrotic or infected tissue or biofilm. A three-year retrospective audit found significant reduction in healing times when NPs utilised LFUD in the management of chronic wounds.
Introduction
Wound healing is a complex phenomenon that is influenced by intrinsic and extrinsic factors that impact on the person, their wound and their wound healing environment1. The healing trajectory is orchestrated by various cytokines, growth factors, proteases and extracellular matrix components2. Proteases, such as matrix metalloproteases (MMPs) are enzymes from the metalloendopeptidase group. In healing wounds they degrade the extracellular matrix components of clot and scar that are found in a wound following injury. Their role is to promote physiological wound debridement and facilitate cellular migration and remodelling in healing wounds. However, MMPs and serine proteases, which are found in increased numbers in chronic wounds have been demonstrated to be responsible for the degradation of extracellular matrix, growth factors and cytokines necessary for healing3,4. Other wound-related factors that contribute to wound chronicity include prolonged inflammatory responses, increased bacterial burden and the presence of biofilm and necrotic tissue1,3,4.
Comprehensive assessment and wound bed preparation has long been the ‘gold standard’ for the management of chronic wounds and the latter involves debridement of necrotic or infected tissue and biofilm3,4. There are various methods of debridement and they include: autolytic, chemical, mechanical, surgical/sharp, conservative sharp, larvae, hydrosurgical and low-frequency ultrasound debridement (LFUD)1,4. Both non-contact (MIST®) and contact (Soring Sonoca® and Debriflo UWI®) LFUD are used to debride wounds5. However, contact LFUD devices appear to be the option currently available in Australia. The non-thermal effects of ultrasound that aid debridement are cavitation or oscillating micro-gas bubbles and acoustic streaming, which dislodges the necrotic tissue from the wound bed and which, in turn, is suctioned or rinsed from the wound6,7. In addition, low-frequency ultrasound (LFU) has been shown to be effective in reducing the wound bacterial burden6 and accelerating wound healing6,7.
Silver Chain is the largest not-for-profit community nursing service in Western Australia and wound management is core business. On any given day an average of 2500 clients with over 3500 wounds are managed in the home or clinic environment. Leg and foot ulcers comprise a large number of these wounds. Venous leg ulcers generally respond positively to best practice wound management and lower leg compression therapy; however, approximately 20% of these leg ulcers fail to respond8.
The Advanced Wound Assessment Service
Silver Chain clients with chronic wounds who fail to heal despite best practice treatment, or who have a deteriorating wound are either referred to a nurse practitioner (NP) Advanced Wound Assessment Service (AWAS) or their medical governance for further assessment and treatment10. The AWAS was established by Silver Chain in Perth in March 2013 and began with one NP and one clinic. Clients with non-healing venous leg ulcers were the main reason for referral to the AWAS in 2014, with 75 clients aged 32–90 years (average age 67 years). Fifty-nine of these clients had not been diagnosed as having a venous leg ulcer prior to AWAS referral and were therefore not receiving optimal compression bandaging therapy. Of the 75 clients referred, 9 clients were considered as having limited potential to complete healing due to other underlying medical conditions, with 13 having potential to heal and the remaining 53 clients healed as a result of treatment. Healing was defined as 100% epithelialisation. The average days of treatment prior to AWAS referral was 99 days (range 1–791 days) and the average days to heal following diagnosis and appropriate management was 57 days (range 4–205 days). Thirty-four clients underwent LFUD treatment in conjunction with compression therapy to achieve healing. All clients referred to the AWAS had a comprehensive health history review and those with leg wounds underwent lower leg assessments, which included bilateral ankle/brachial pressure index or absolute toe pressures. However, 10 clients were referred for further vascular diagnostic investigations and 8 clients were referred to vascular surgeons for further management. Other interventions as clinically indicated in this cohort included antibiotic therapy, topical corticosteroid treatment and 4 clients were referred to an infectious diseases physician for targeted ongoing antibiotic treatment9,10.
Similar successful outcomes were demonstrated amongst clients with other wound types who attended this AWAS in 2015. These outcomes and client satisfaction led to the service being expanded, and three AWAS clinics, which were coordinated by four NPs, were established across the metropolitan area by 201610. The NPs provide comprehensive health and wound assessments, referral for targeted diagnostic investigations or medical specialist review and implementation of evidence-based wound management. The wound assessments are recorded electronically at point of care on ComCare Mobile Wound Module®, which facilitates ongoing and rigorous audits and benchmarking of treatment outcomes. The NPs work in collaboration with the client, community nursing teams, general practitioners, medical specialists and allied health professionals to develop and implement management plans that improve healing outcomes, prevent complications and reduce hospital admissions.
When clinically indicated, the NPs perform sharp debridement or LFUD for removal of necrotic or infected tissue or biofilm11-13. Although LFUD is considered by some to be relatively painless, it is usual protocol to apply topical analgesia such as EMLA™ or topical lignocaine 4% to the wound bed for 20 minutes prior to debridement treatments. The contact LFUD is delivered at 30–50 kHz by a handheld Sonoca® probe, using normal saline solution as the coupling medium. The LFU is applied to the wound bed via the probe for 20 seconds per mm2 ulcer area. The NPs wear personal protective clothing, masks and sterile gloves and perform an aseptic surgical procedure14. Sterile drapes are used to provide a controlled procedural environment and to protect against splashing of fluids or contamination of couches or equipment and dispersal of spray into the local atmosphere. Infection control practices are rigorously adhered to throughout the procedure. The LFUD is usually performed weekly until signs of necrosis and localised infection are eliminated. An average of four to six treatments per client episode of treatment is usual, but is subject to each client’s clinical presentation. After each LFUD treatment, an antimicrobial dressing is usually applied with a secondary absorbent pad to reduce the risk of infection. If a venous leg ulcer is being treated, compression bandaging as clinically indicated by vascular assessment and client tolerance (the recommended sub-bandage pressure is 30–40 mmHg)15 will also be applied.
Evaluating Outcomes
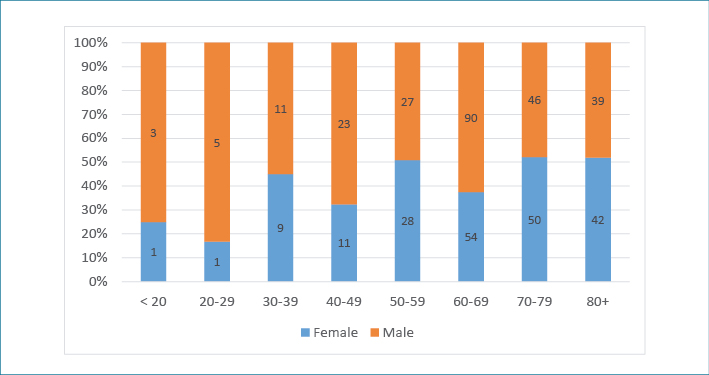
In October 2017, a retrospective audit of all clients who were treated with LFUD in the three AWAS clinics from March 2013 to September 2016 was undertaken. There were 348 clients with 432 wounds of mixed aetiologies who underwent comprehensive health and wound assessments and LFUD. Males comprised 55.8% and females 44.3%. The mean age of clients was 65.2 years and the median 76 years, with a range from 17 to 95 years (Figure 1).
Figure 1: Age and gender of clients
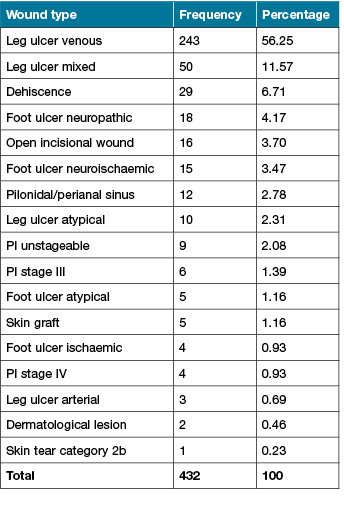
The largest number of wounds treated were wounds of the lower limb (n=348) and in particular, venous leg ulcers (n=243). Other wound types treated are presented in Table 1.
Table 1: Wound types treated with LFUD
Many clients had their wounds for a considerable length of time prior to referral to the community nursing service or review by a NP. The mean length of time between clients acquiring the wound to the first LFUD being performed was 344.1 days. The length of time following the last LFUD treatment to healing was 115.6 days (Table 2). The mean number of treatments received were 3.7 and the median was 2.0.
Table 2: Number of days before the first LFUD and after the last LFUD
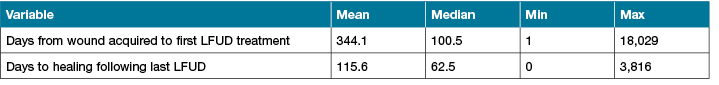
One 90-year-old client had a significantly long-standing wound for 18,029 days. He had acquired a compound fracture as a 19-year-old, which developed into an extremely chronic wound. Regardless of treatment by a multitude of medical specialists and community nurses over the intervening years, his wound remained unhealed. However, during the LFUD treatments his wound reduced in size and the number and frequency of dressing changes and his wound pain were significantly reduced.
Thirty-two clients healed whilst attending the AWAS and the majority of clients (58.4%, n=247) were referred back to the primary community nurses with a revised care plan for ongoing best practice care with expectations that the wounds would heal and 89.8% of the 58.4% did so. Another 19.6% (n=83) clients were referred back to the primary nurses with a revised care plan for ongoing maintenance wound management and little expectation that they would heal; however, 24.0% of these wounds subsequently healed.
There were 4.49% (n=19) clients who declined further LFUD and reasons for this were recorded as either client difficulties with mobilisation and attending clinics or non-compliance with planned treatment. There were 3.31% (n=14) clients who were unresponsive to LFUD and further diagnostic investigations confirmed a diagnosis of malignancy or other complication or confounding co-morbidity that required management by a plastic surgeon or palliative physician. No adverse events to LFUD were reported.
LFUD Episodes and Treatments Performed
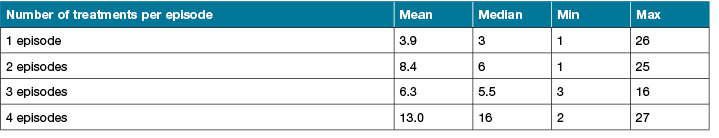
The number of episodes or series of LFUD treatments per client were a mean 1.1, median 1. However, the number of individual LFUD treatments within each episode, which was determined following clinical assessment and response outcomes, is outlined in Table 3.
Table 3: Number of LFUD treatments per episode
Wound Healing Outcomes
The care delivered by the NPs and the use of LFUD produced significant improvements in wound healing:
- 67% (n=290) of total wounds which had received LFUD healed.
- 90% of wounds transferred back to the primary community nurse following LFUD went on to heal.
- 24% of wounds which were transferred back to the primary nurse for evidence-based care with maintenance as their goal, actually healed.
- 33% of wounds were ongoing and these clients were referred for further investigations in consultation with their medical practitioner.
While the overall healing outcomes were impressive, it was the individual outcomes for some clients that were truly outstanding. One client who had a VLU for 4,198 days healed after NP comprehensive assessment and management including LFUD treatments in 39 days. Similar outcomes were experienced by 11 other clients with very long-standing leg ulcers (see Figure 2). These findings provide further evidence of the therapeutic benefits of LFUD in the management of chronic wounds16. Of equal importance, this review demonstrated the need for a definitive clinical diagnosis for all wounds, which should guide implementation of best practice wound management.

Figure 2: Leg ulcer present for 427 days, healed in 110 days after LFUD
Conclusion
Wound management is more than the application of a dressing. It requires a comprehensive and collaborative approach to care. This is the principle that governs the Silver Chain NP’s practice. The retrospective audit revealed that there were 348 clients with 432 wounds of mixed aetiologies but the highest number of wounds were venous leg ulcers, who attended the AWAS and underwent LFUD. Of the 432 wounds, 290 (67%) healed following the LFUD treatment and 24% of wounds, which were referred back to the primary community nurse for maintenance care and not expected to heal, subsequently healed. The audit demonstrated significantly improved healing times and we assume clients experienced significant advancement in wellbeing and quality of life. Furthermore, the potential implicit and explicit costs associated with the management of chronic wounds has been reduced.
Conflict of Interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
Author(s)
Keryln Carville*
RN, PhD, STN(Cred)
Silver Chain Group, WA, Australia
Email Keryln.carville@silverchain.org.au
Liz Howse
RN, MN, NP, MN(NP), STN
Silver Chain Group, WA, Australia
Margaret Edmondson
RN, NP, MN, STN
Silver Chain Group, WA, Australia
Gordana Petkovska
RN, NP, MN(NP), STN
Silver Chain Group, WA, Australia
Pam Morey
RN, NP, MN(NP), STN
Silver Chain Group, WA, Australia
Cate Maguire
RN
Silver Chain Group, WA, Australia
Ann Tuvik
RN
Silver Chain Group, WA, Australia
* Corresponding author
References
1. Carville K. Wound Care Manual, 7th edn. Osborne Park, WA: Silver Chain Foundation, 2017.
2. Chin C, Schultz G, Stacey M. Principles of wound bed preparation and their application to the treatment of chronic wounds. Primary Intention 2003;11(4):171–182.
3. Leaper D, Schultz G, Carville K, Fletcher J, Swanson T, Drake R. Extending the TIME concept: what have we learning in the past 10 years? Int Wound J 2012;9(Suppl.2):1–19.
4. Schultz G, Sibbald R, Falanga V et al. Wound bed preparation: A systematic approach to wound management. Wound Repair Regen 2003;1(2):Suppl(S1–S8).
5. Australian and New Zealand Horizon Scanning Network. Horizon scanning technology prioritising summary low frequency ultrasound debridement. Australian Government Department of Health: Horizon Scanning, 2007. Available from http://www.horizonscanning.gov.au
6. Tan J, Abisi S, Smith A, Burnand K. A painless method of ultrasonically assisted debridement of chronic leg ulcers: a pilot study. Eur J Vasc Endovasc Surg 2007;33:234–238. Retrieved from http://www.sciencedirect.com
7. Breuing K, Bayer L, Neuwalder J, Arch M, Orgill D. Early experience using low-frequency ultrasound in chronic wounds. Ann Plast Surg 2005;55:183–187.
8. Smith J, Maguire C. Community Wound Project. Unpublished report. Osborne Park, WA: Silver Chain Group, 2017.
9. Howse L. Silver Chain Kingsley Client Review. Unpublished report. Osborne Park, WA: Silver Chain Group, 2014.
10. Howse L. Silver Chain Advanced Wound Assessment Service Review. Unpublished report. Osborne Park, WA: Silver Chain Group, 2014.
11. Wolcott R, Kennedy J, Dowd S. Regular debridement is the main tool for maintaining a healthy wound bed in most chronic wounds. J Wound Care 2009;18(2):54–56.
12. Madhok B, Vowden K, Vowden P. New techniques for wound debridement. Int Wound J 2013;10:247–251.
13. Keast D, Swanson T, Carville K, Fletcher J, Schultz G, Black J. Top 10 tips: understanding and managing wound biofilm. Wounds Int 2014;5(2). Retrieved from www.woundsinternational.com
14. Wounds Australia. Australian Standards for Wound Management. Osborne Park, WA: Cambridge Media, 2016.
15. Australia Wound Management Association and New Zealand Wound Healing Society. Australian and New Zealand Clinical Practice Guideline for Prevention and Treatment of Venous Leg Ulcers. Osborne Park, WA: Cambridge Media, 2011.
16. Voigt J, Wendelken M, Driver V, Alvarez O. Low-frequency ultrasound (20–40 kHz) as an adjunctive therapy for chronic wound healing: a systematic review of the literature and meta-analysis of eight randomized controlled trials. Int J Low Extrem Wounds 2011;10(4):190–199. Retrieved from http://ijlew.sagepub.com



