Volume 26 Number 3
Skin tear risks associated with aged care residents: a cross-sectional study
Robyn Rayner, Keryln Carville, Gavin Leslie and Satvinder S Dhaliwal
Keywords skin tears, elderly, demographics, clinical, residential care.
Abstract
Background: To describe the profile of aged care residents and to examine those variables that were associated with skin tears.
Method: A representative sample of 200 elderly residents were recruited into this cross-sectional study, which was conducted between February and December 2014 from four aged care facilities in Western Australia. The resident’s history of skin tears over the preceding 12-months was compared with their demographics (age, gender, place of birth) and a broad range of clinical characteristics including: body mass index, comorbidities, medications, smoking history, falls, and personal skin characteristics (purpura, ecchymosis, bruising uneven pigmentation, pseudoscars).
Results: A history of skin tears was documented for 101 (50.5%) residents during the preceding 12-months. Residents with a skin tear history were significantly older, more likely to have a skin tear on initial assessment, had a lower Braden Scale score and a lower Braden sub-score for mobility, were at higher risk of falling, had osteoporosis, used a corticosteroid inhaler, and displayed both skin purpura (≤ 20 mm.) and ecchymosis (≥ 20 mm.).
Conclusions: Aged care residents are at substantial risk of skin tears. Identification of factors associated with skin tears aids better understanding of risk factors and enables more effective targeted preventive strategies.
Background
Skin tears are commonly reported wounds associated with ageing skin1,2. They are generally defined as a “traumatic wound occurring principally on the extremities of older adults, as a result of friction alone or shearing and friction forces which separate the epidermis from the dermis (partial-thickness wound) or which separates both the epidermis and the dermis from underlying structures (full-thickness wound)”3,p.22.
The wide range of incidents and causes that are reported in the literature to be associated with skin tears are due in part to methodological differences and geographical diversity of the study populations2,4-9. Published global epidemiological data indicate that Australia (41–59%) has one of the highest prevalence rates of skin tears among aged care residents when compared to similar North America (14–22%) and Japanese (4–14%) populations2,4-8. Regardless of the geographical location of these studies, skin tears are reported to primarily occur on the upper extremities, followed by the lower extremities5,10-12. As Australia’s population aged 65 years and older is projected to grow from 15% in 2015 to 22% in 205613,14, it is likely skin tear incidents will increase.
The early identification of older individuals at risk of skin tears will potentially permit timely and targeted implementation of preventive strategies to reduce these injuries, optimise quality of life and better utilise health care resources. While a number of studies have reported determinants of skin tears4,15-17 in Australia there is a paucity of data that have explored the risk of skin tears over the extremities of aged care residents. Given the paucity of data, a cross-sectional study was undertaken to identify demographic, clinical and skin characteristics associated with a documented history of skin tears in the preceding 12 months. This report presents the demographic and clinical profile of aged care residents who participated in that study.
Methodology
Study design, setting and sample
A cross-sectional study was conducted across four residential aged care facilities (two metropolitan and two regional) that were operated by a single service provider in Western Australia. Staffing ratios and care practices were standardised across the four residential facilities. A sample size of 200 residents was determined a priori from power analysis. Residents were invited to participate if they met the inclusion criteria, were aged over 65 years and had provided informed, written consent. Residents were excluded if consent was not obtained, a connective tissue disorder, were in pain, agitated or were receiving palliative services.
Data collection
A data collection form was devised to standardise the recording of demographic (age, sex, place of birth), clinical (skin type, history of smoking, body mass index [BMI], Braden Scale scores18, falls history co-morbidities, medication, use of moisturiser) and skin characteristics (purpura, ecchymosis, bruising, uneven pigmentation, pseudoscars). Demographic data were sourced from the resident, their legal guardian or the medical records.
A review of the skin tear literature identified a lack of clarity about the definition and classification of skin characteristics9. To maintain consistency with the medical literature, precise definitions were based on the Medical Subject Heading (MeSH) controlled index terms that are listed in the US National Library of Medicine’s (NLM) biomedical literature database and Medline19. Where terminologies were not available under the MeSH headings, additional medical literature resources were searched to clarify these definitions.
Ecchymosis is a general term referring to the extravasation of blood into skin20,21. These lesions are benign, non-palpable, non-blanching and have a purplish/brown colour19,22. Purpura referred to the isolated demarcated ecchymotic lesions that occurred in the dermal layer of the skin and range in size between 2 and 20 mm. Senile purpura (also known as ecchymosis, actinic purpura, Bateman’s purpura, traumatic purpura or corticosteroid purpura) also occurred in the dermal layer skin but present as a more extensive (greater than 20 mm) and demarcated lesion23,24. The presence of purpura and ecchymosis in this study were the result of age-related skin changes and not from any underlying medical conditions.
The use of the word ‘bruise’ within the skin tear literature appears to be synonymous with the term ecchymosis17,25-29. Caution is nevertheless needed when using these terms interchangeably, as Stedman’s Medical Dictionary (2016) advises against associating the term ‘bruise’ with any haemorrhagic lesion other than that which arises from a blunt force injury. For the purpose of this study, a bruise or contusion referred to the extravasation of blood in the subcutaneous layer that resulted from a non-penetrating blunt force or crush injury30,31. These lesions have an indistinct edge and undergo characteristic discolouration until they progressively disappear. Colour changes range from red, blue and purple in the first 5 days; green after 5–7 days; and yellow about 1–2 weeks later22,32.
The extremities of aged residents were visually assessed, inspected and gently palpated to evaluate skin characteristics. All residents were assessed by a single investigator within the privacy of their own room under standardised temperature (20–22 ± 1°C) and relative humidity (40–60%) testing conditions. All skin tears in the centralised database were classified according to the validated Skin Tear Audit Research (STAR) Classification System and recorded by the service provider in an integrated database33. The STAR Classification accounts for ecchymotic skin colour changes associated with the skin tear injury such as ‘dusky, darkened’.
Analysis
Categorical data was represented by frequency (percentage) and mean ± standard deviation and median (interquartile range) for continuous variables. Chi-squared tests were conducted to evaluate the frequency data for categorical variables and the preceding 12 months’ documented history of skin tears. Independent sample t-tests were used to compare continuous data between residents with and without a history of skin tears. All tests were two-sided with a p-value less than 0.05 considered significant. The skin tears classification was obtained from the service providers integrated database to avoid removing any dressing found to be in situ on assessment. Data was analysed using the Statistical Package for the Social Sciences (SPSS® version 22)34.
Ethical approval
Ethics approval for this study was obtained from Curtin University Research and Development Human Research Ethics Committee (RD-23-13) and The Bethanie Group Inc. Governance Committee. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki and the Australian Code for the Responsible Conduct of research35,36.
Results
In total, 200 aged care residents participated in this study, which was conducted over an 11-month period between February 2014 and December 2014. Among the study population, 101 residents had a documented history of skin tears during the 12 months preceding recruitment and 99 had no recorded skin tear incident. The demographic, clinical and skin characteristics of the 200 residents are presented in Table 1: Comparison between residents with and without a documented history of skin tears.
Table 1: Comparison between residents with and without a documented history of skin tears
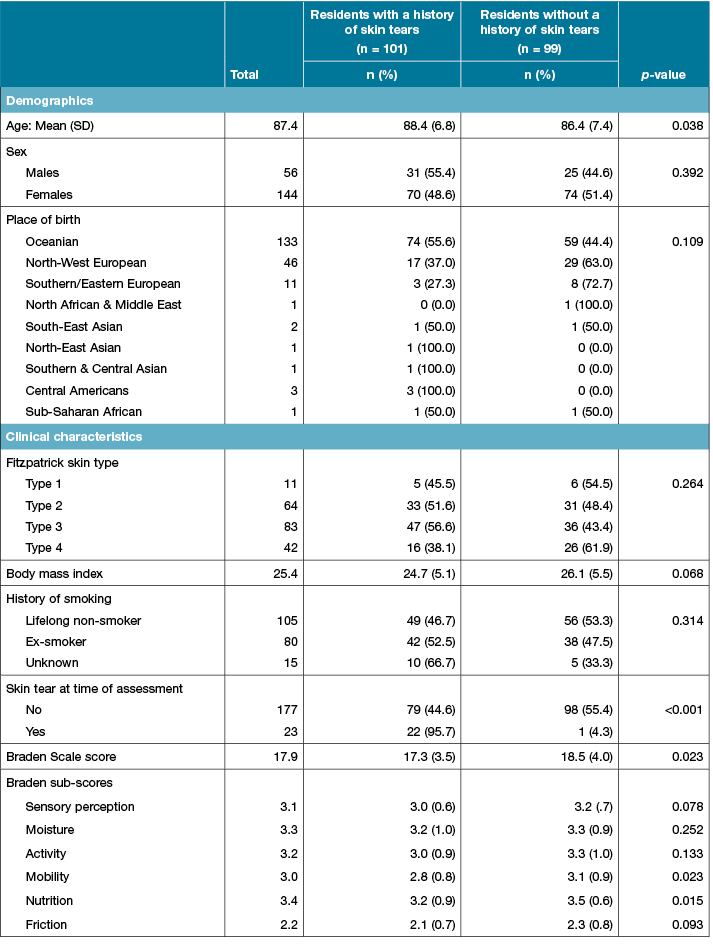
Table 1 (continued): Comparison between residents with and without a documented history of skin tears
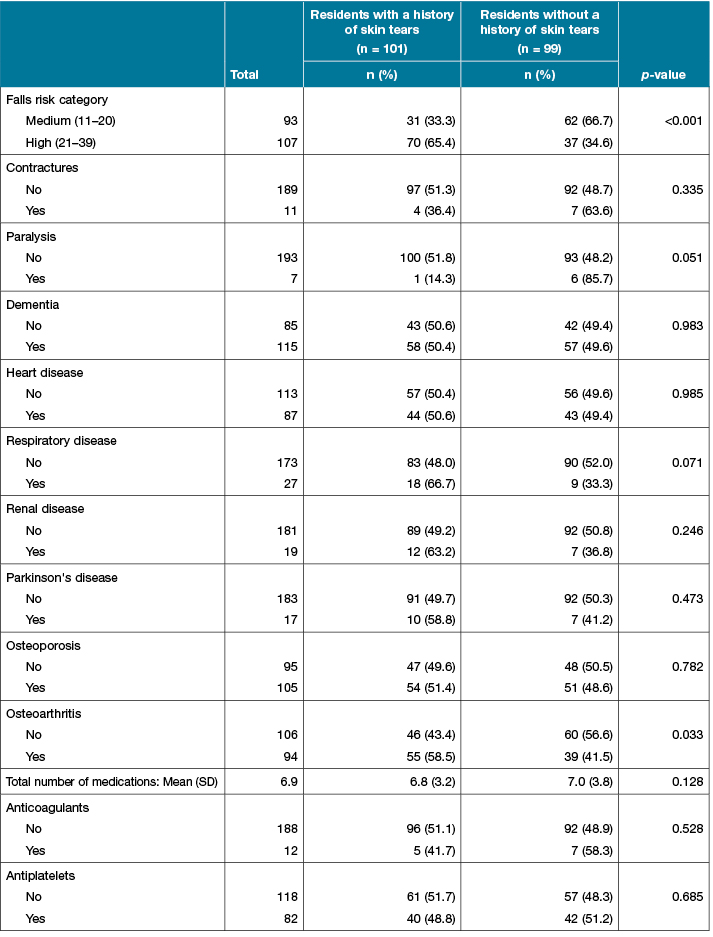
Table 1 (continued): Comparison between residents with and without a documented history of skin tears
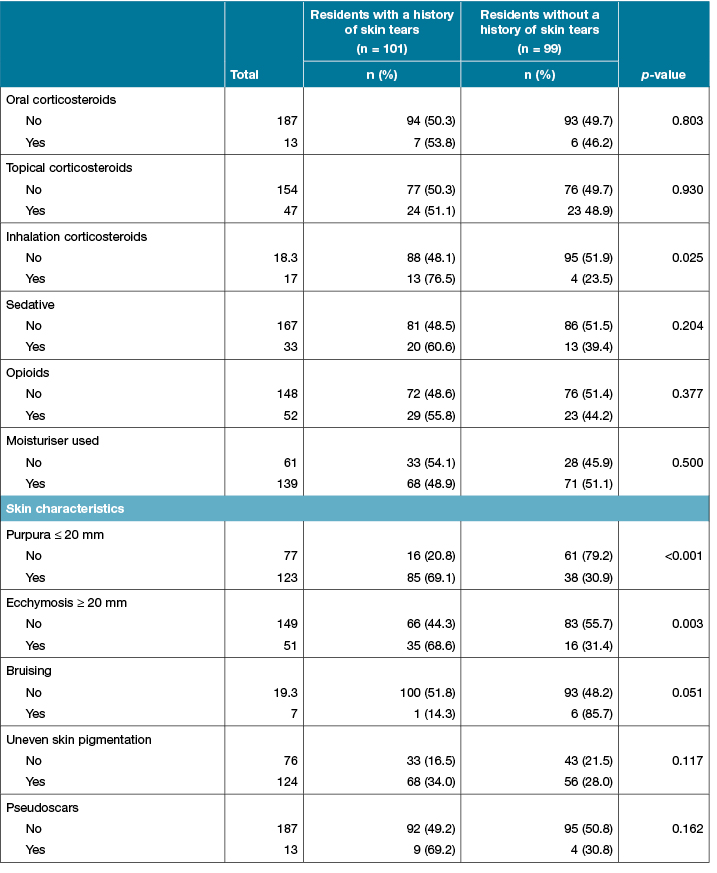
Note: n = number; % = percentages; SD = standard deviation, p-value from chi-square test for categorical variables or t-test for continuous variables.
Residents with a documented history of a skin tear in the preceding 12 months were significantly older than residents without skin tears and were more likely to have a skin tear and a lower Braden Scale score at time of the assessment. Further examination of the six Braden Scale sub-scores (sensory perception, moisture, activity, mobility, nutrition and friction) showed only mobility had a statistically significant effect. Residents with a history of skin tears were significantly less mobile than residents without a history of skin tears.
Residents with a documented history of skin tears were also significantly more likely to have osteoarthritis, be in a higher falls risk category, take inhalation corticosteroids, and display skin manifestations of purpura and ecchymosis.
Table 2 presents the number and relative proportion of residents with a skin tear at time of assessment.
Table 2: Number of skin tears at time of assessment and the proportion of residents
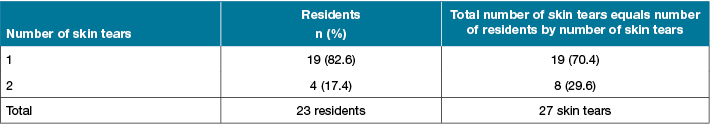
Note: Values are number of residents (%).
At the time of the assessment, 23 of the 200 residents were recorded to have a total of 27 skin tears. In total, 82.6% of residents had a single skin tear and 17.4% of residents had two skin tears. The anatomical location and the total number of skin tears at time of the assessment by gender is presented in Table 3.
Table 3: General location of total number of skin tears at time of assessment by gender
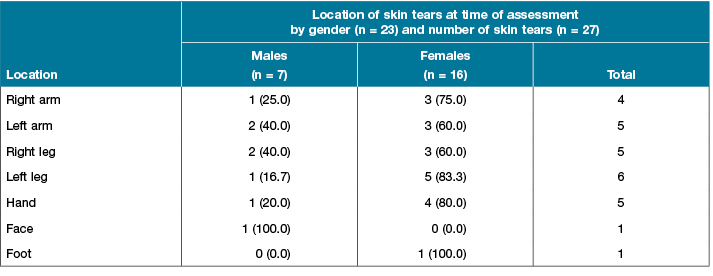
Note: Values are number of patients (%).
Skin tears were present at time of assessment in 12.5% of all males and 11.1% of all females. Of these skin tears, 51.9% occurred on the upper extremity, 44.4% on the lower extremities and 3.7% on the face.
According to the STAR Classification System, 40.7% of skin tears present at time of the assessment were classified as category 1a, 33.3% as 1b, 22.2% as 2b, and 3.7% as 3 (Table 4).
Table 4: Number and percentage of skin tears by the STAR Classification System
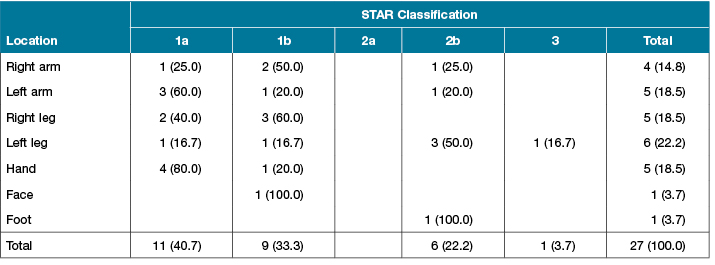
Note: Values are number of patients (%).
Discussion
This cross-sectional study presents the demographic, clinical profile and skin characteristics of 200 aged care residents, which were found to be significantly associated with a preceding 12 months’ documented history of skin tears. The study population comprised 144 females and 56 males with a total mean age of 87.4 (range 65–107) years. In terms of a preceding 12-month documented history of skin tears in this sample, skin tears occurred in 50.5% of residents, while 49.5% of residents did not have a reported injury.
There were significant differences in demographic and clinical profile between residents with a documented history of skin tears and residents without a reported history. Residents with a history of skin tears were precisely two years older than residents without a history of skin tears. This result is consistent with findings from other studies reporting age is associated with the risk of skin tears11,16,17,37. Three recent studies, which were undertaken in long-term, elderly Japanese residents, did not find any significantly difference in age between residents with and without skin tears7,8,12. It is likely that the skin of residents in this Australian study population were also subjected to substantial extrinsic ageing, which would also contribute to a progressive decline in the skin’s structural integrity.
In residents with a documented history of skin tears, 21.8% had a skin tear incident at time of the assessment. Four previous studies also reported skin tears were associated with a history of skin tears5,10,37,38. This suggests that there may be yet unknown skin property changes that leave some older individuals more susceptible to repeated skin tear injuries.
Residents with a history of a skin tear were more likely to have a lower Braden Scale score and lower Braden mobility sub-score than residents without a history of skin tears. Despite the fact that residents with a history of skin tears had a lower Braden Scale score as compared to residents without a history of skin tears, the relative prediction risk of a pressure injury was mild for both populations. Three other studies, which reported using the Braden Scale to assess mobility did not find any significant difference between the mobility score between residents with and without skin tears7,8,12. A dated study by McGough-Csarny and Kopac37 (1991), which did not use the Braden Scale, reported limited mobility to be a risk factor of skin tears. Recent research into the validity of the Braden Scale in assessing pressure injuries in long-term care facilities and in individuals aged over 80 years has questioned the use of this tool due to its low reliability in this population cohort39,40. As the relevance of the Braden Scale for use in the context of skin tears in older adults has never been validated, it is debatable whether it is the most appropriate tool to discriminate mobility, particularly in individuals aged over 80 years. Nevertheless, reduced mobility may be a marker for the risk of falling which in some older individuals can lead to skin trauma.
In this study, residents with a history of skin tears were nearly twice as likely to be documented as having a high falls risk than residents without a history of skin tears. This result is supported by a number of previous studies showing falls increase the risk of skin tears41,42. While there are numerous factors that contribute to the risk of older individuals falling43, more extensive skin changes may predispose some individuals to recurrent disruption of their skin integrity.
Residents with a history of skin tears were 1.4 times more likely to have osteoarthritis. While osteoarthritis has not previously been reported to be associated with skin tears it inhibits stability and mobility and is a common falls risk factor44,45. Older adults with osteoarthritis of the hips and knee compensate to reduce the amount of pressure on the affected joints by adopting biomechanical changes when walking46. The pelvis slopes downwards to the opposing side during the stance phase of the gait, which results in the centre of gravity moving away from the stance leg, leading to instability and an increased risk of falling46.
Likewise, residents with a documented history of skin tears were three times more likely to be taking corticosteroids in an inhaler form than residents without a history of skin tears. While the inhaled mode of steroid delivery has not previously been reported in the skin tear literature, research on the cutaneous effects of inhaled corticosteroids indicate that atrophic skin changes are similar to those that result from topical and oral corticosteroids use47. Atrophic effects of steroids includes epidermal thinning and decreased collagen synthesis of the dermal layer, which can lead to loss of skin integrity48.
Two clinical skin manifestations were identified to be significantly associated with a history of skin tears in this study. Residents with a documented history of skin tears were more than twice as likely to have clinical skin purpura and ecchymosis than residents without a documented history. These skin manifestations were consistent with other authors’ findings in the skin tear literature6,10,37. The aetiology of purpura and ecchymosis is reported to arise from increased fragility of blood vessels and a decline in dermal structural collagen associated with age-related skin changes, which impact on the mechanical integrity of skin22,49.
A strength of this cross-sectional descriptive study was the multi-site research settings from which participants were recruited. The study design included a representative sample of older adults in Western Australian aged care facilities with equal representation of residents with or without a history of skin tears. Thus, the findings could be considered to be relevant to a broader residential aged care population. Potential limitations to this cross-sectional study is the temporal association between a documented history of skin tears and identified risk factors.
Conclusion
This study identified the demographic, clinical and skin characteristics of a representative sample of 200 aged care residents, identifying factors which were found to be significantly associated with a documented history of skin tears. These associations identify variables that should be assessed among aged care residents on a routine basis, to better understand risk factors and plausibly quantify future risk of skin tears. This, in turn, will allow health care professionals to more effectively apply targeted preventive strategies to reduce the incidence of skin tears in aged care residential facilities. Reduction in skin tears will lead to improved quality of life among residents, and aged care providers can anticipate a reduction in wound care time and costs.
Acknowledgements
The authors would like to acknowledge the support of the Wound Management Innovation Cooperative Research Centre and the Australian Government’s Cooperative Research Centres Program. The authors are indebted to the residents and staff of the Bethanie Group Inc for their support to undertake this study. Our sincere gratitude to Professor Hiromi Sanada and her research team from the Department of Gerontological Nursing/Wound Care Management at the University of Tokyo for their collaboration in undertaking this research. We are particularly grateful to Dr Takeo Minematsu for assisting us with skin blotting investigations and analysis.
Conflict of Interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
RR was a recipient of a 2013 Australian Postgraduate Award, Curtin University Postgraduate Scholarship and a Wound Management Cooperative Research Centre (CRC) PhD stipend.
Author(s)
Robyn Rayner*
BSc (Nursing), Postgrad (Health Admin),
Master Wound Care, PhD, RN
School of Nursing, Midwifery and Paramedicine, Curtin University and Silver Chain Group, WA, Australia
Email R.Rayner@curtin.edu.au
Keryln Carville
RN, PhD
School of Nursing, Midwifery and Paramedicine, Curtin University and Silver Chain Group, WA, Australia
Gavin Leslie
RN, PhD, BAppSc, Post Grad Dip (Clin Nurs), FACN, FACCCN
School of Nursing, Midwifery and Paramedicine, Curtin University, WA, Australia
Satvinder S Dhaliwal
BSc (Hons), MSc, PhD
School of Public Health, Curtin University, WA, Australia
* Corresponding author
References
- Baranoski S, LeBlanc K, Gloeckner M. Preventing, assessing, and managing skin tears: A clinical review. Am J Nurs 2016;116:24–30.
- Carville K, Leslie G, Osseiran-Moisson R, Newall N, Lewin G. The effectiveness of a twice-daily skin-moisturising regimen for reducing the incidence of skin tears. Int Wound J 2014;11:446–53.
- Payne R, Martin M. Defining and classifying skin tears: Need for a common language. Ostomy Wound Manage 1993;39:16–26.
- Everett S, Powell T. Skin tears — the underestimated wound. Primary Intention 1994;2:28–31.
- LeBlanc KA, Christensen D, Cook J, Culhane B, Gutierrez O. Prevalence of skin tears in a long-term care facility. J Wound Ostomy Continence Nurs 2013;40:1–5.
- White MW, Karam S, Cowell B. Skin tears in frail elders: A practical approach to prevention. Geriatr Nurs 1994;15:95–9.
- Sanada H, Nakagami G, Koyano Y, Iizaka S, Sugama J. Incidence of skin tears in the extremities among elderly patients at a long-term medical facility in Japan: A prospective cohort study. Geriatr Gerontol Int 2015;15:1058–63.
- Koyano Y, Nakagami G, Iizaka S, Sugama J, Sanada H. Skin property can predict the development of skin tears among elderly patients: A prospective cohort study. Int Wound J 2017;14:691–7.
- Rayner R, Carville K, Leslie G, Roberts P. A review of patient and skin characteristics associated with skin tears. J Wound Care 2015;24:406–14.
- 1Payne R, Martin M. The epidemiology and management of skin tears in older adults. Ostomy Wound Manage 1990;26:26–37.
- Malone ML, Rozario N, Gavinski M, Goodwin J. The epidemiology of skin tears in the institutionalized elderly. J Am Geriatr Soc 1991;39:591–5.
- Koyano Y, Nakagami G, Iizaka S et al. Exploring the prevalence of skin tears and skin properties related to skin tears in elderly patients at a long-term medical facility in Japan. Int Wound J 2014;13:189–97.
- Australian Bureau of Statistics. Cat no. 4430.0 — Disability, ageing and carers, Australia: Summary of findings. 2015.
- Australian Bureau of Statistics. Cat no. 3222.0 — Population projections, Australia: 2012 (base) to 2101. 2013.
- Lopez V, Dunk AM, Cubit K et al. Skin tear prevention and management among patients in the acute aged care and rehabilitation units in the Australian Capital Territory: A best practice implementation project. Int J Evid Based Healthc 2011; 9:429–34.
- Lewin GF, Newall N, Alan JJ, Carville KJ, Santamaria NM, Roberts PA. Identification of risk factors associated with the development of skin tears in hospitalised older persons: A case-control study. Int Wound J 2016;13:1246–51.
- Newall N, Lewin GF, Bulsara MK, Carville KJ, Leslie GD, Roberts PA. The development and testing of a skin tear risk assessment tool. Int Wound J 2016;14:97–103.
- Braden B, Bergstrom N. Braden Scale for predicting pressure sore risk. In Agency for Health Care Policy and Research, (1992). Pressure ulcers in adults: Prediction and prevention. Ostomy Wound Manage 1988;38:67–77.
- National Library of Medicine. Searching PubMed® with MeSH®. United States National Library of Medicine, 2013, 1–2.
- Griffith RD, Falto-Aizpurua LA, Nouri K. Dermatologic etymology: Primary morphology of skin lesions. JAMA Dermatol 2015;151:69–.
- Carson HJ. Patterns of ecchymoses caused by manner of death and collateral injuries sustained in bruising incidents: Decedent injuries, profiles, comparisons, and clinicopathologic significance. J Forensic Sci 2010;55:1534–42.
- Cox NH, Piette WW. Purpura and microvascular occlusion. In: Burns T, Breathnach S, Cox N, Griffiths C (Eds). Rook’s textbook of dermatology. United Kingdom: Wiley-Blackwell; 2010, pp. 1–51.
- Norman RA, Young EM, Jr. Benign vascular lesions. Atlas of geriatric dermatology. London: Springer; 2014, pp. 243–9.
- Sandberg-Cook J, Blair G. Purpura. In: Buttaro TM, Trybulski J, Bailey PP, Sandberg-Cook J (Eds). Primary care: A collaborative practice. Missouri: Elsevier Mosby, 2013, pp. 290–2.
- Beechey R, Priest L, Peters M, Moloney C. An evidence-based approach to the prevention and initial management of skin tears within the aged community setting: A best practice implementation project. JBI Database System Rev Implement Rep 2015;13:421–43.
- Lloyd-Jones M. The prevention and management of skin tears. Nurs Residential Care 2011;13:418–22.
- Stephen-Haynes J, Carville K. Skin tears made easy. London: Wounds International 2011;2:1–6.
- Thompson-McHale S. Preventing heel ulcers, skin tears and moisture damage. Nurs Residential Care 2016;18:192–7.
- White W. Skin tears: A descriptive study of the opinions, clinical practice and knowledge base of RNs caring for the aged in high care residential facilities. Primary Intention 2001;9:138–49.
- Bilo RC, Oranje A, Shwayder T, Hobbs C. Blunt-force trauma: Bruises. Cutaneous manifestations of child abuse and their differential diagnosis. Berlin Heidelberg: Springer, 2013, pp. 63–103.
- Randeberg LL, Winnem AM, Langlois NE et al. Skin changes following minor trauma. Lasers Surg Med 2007;39:403–13.
- Pollak S, Saukko PJ. Blunt force trauma. Wiley encyclopedia of forensic science. New York: John Wiley & Sons, Ltd, 2009.
- Carville K, Lewin G, Newall N et al. STAR: A consensus for skin tear classification. Primary Intention 2007;15:18–28.
- IBM Corporation. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.
- World Medical Association. World medical association declaration of Helsinki: Ethical principles for medical research involving human subjects. J Am Med Assoc 2013;310:2191–4.
- Australian Government National Health and Medical Research Council. Australian code for the responsible conduct of research. Australian Government, 2007, pp. 1–12.3.
- McGough-Csarny J, Kopac C. Skin tears in institutionalized elderly: An epidemiological study. Ostomy Wound Manage 1998;44:14–25.
- Skiveren J, Wahlers B, Bermark S. Prevalence of skin tears in the extremities among elderly residents at a nursing home in Denmark. J Wound Care 2017;26:S32–S6.
- Chen H-L, Cao Y-J, Zhang W, Wang J, Huai B-S. Braden scale is not suitable for assessing pressure ulcer risk in individuals aged 80 and older. J Am Geriatr Soc 2015;63:599–601.
- Wilchesky M, Lungu O. Predictive and concurrent validity of the Braden scale in long-term care: A meta-analysis. Wound Repair Regen 2015;23:44–56.
- Bank D, Nix D. Preventing skin tears in a nursing and rehabilitation center: An interdisciplinary effort. Ostomy Wound Manage 2006;52:38–46.
- Chang C-M, Lin H-F, Chiang H-H. A study on the relationship between age and inpatient falls in Taiwan. Int J Nurs Pract 2015;21:605–11.
- Cheung C. Older adults, falls, and skin integrity. Adv Skin Wound Care 2017;30:40–6.
- Krauss MJ, Evanoff B, Hitcho E et al. A case-control study of patient, medication, and care-related risk factors for inpatient falls. J Gen Intern Med 2005;20:116–22.
- Health Quality Ontario. Prevention of falls and fall-related injuries in community-dwelling seniors: An evidence-based analysis. Ontario Health Technology Assessment Series 2008;8:1–78.
- Ng CT, Tan MP. Osteoarthritis and falls in the older person. Age Ageing 2013;42:561–6.
- Allen DB, Bielory L, Derendorf H, Dluhy R, Colice GL, Szefler SJ. Inhaled corticosteroids: Past lessons and future issues. J Allergy Clin Immunol 2003;112:S1–S40.
- Sarkar R, Parmar NV. Topical side effects of topical corticosteroids. In: Lahiri K (Ed). A treatise on topical corticosteroids in dermatology: Use, misuse and abuse. Singapore: Springer, 2018, pp. 251–60.
- Husain, Z., Cohen, P. J., Schwartz, R. A., & Lambert, W. C. (2011). Flexural and extensoral eruptions in dermatologic disease. Clinics in Dermatology, 29(2), 195-204. doi:10.1016/j.clindermatol.2011.01.020.



