Volume 26 Number 3
Citric acid treatment of post-caesarean wound infections caused by multiple antibiotic-resistant Staphylococcus aureus
Basavraj S Nagoba, Chandrakala A Dawle (Patil), Milind S Davane and Jyoti A Dawle
Keywords S. aureus, Lower segment caesarean section, wound infections, citric acid.
Abstract
Post-caesarean wound infections are difficult to manage, especially when they are caused by multiple antibiotic-resistant Staphylococcus aureus. An attempt was made to treat post-caesarean staphylococcal wound infections with topical application of citric acid. Twenty post-caesarean patients with wound infections caused by multiple antibiotic-resistant S. aureus were treated by application of 3% citric acid once daily. Wound dressing with citric acid ointment in 18 cases resulted in complete healing after 6 to 21 applications. Topical application of citric acid was found highly effective in the treatment of post-caesarean wound infections due to multiple antibiotic-resistant S. aureus.
Introduction
Lower segment caesarean section (LSCS) is the single greatest risk factor for postpartum infection in developing countries. Women undergoing LSCS have a five to 20-fold greater risk of infection and infectious morbidity. Infectious complications following LSCS are an important cause of maternal morbidity. Post-caesarean wound infection (wound dehiscence) is one of the most important and common complications. The worldwide rate of wound infections following LSCS ranges between 3% and 15%1-3. However, the rate of infection in India ranges between 4% and 9%4,5. Wound infections following LSCS are the leading causes of maternal morbidity, prolonged hospital stay and increased health care costs, and continues to be a common postoperative complication in both the developed and developing world6-8.
Post-caesarean wound infections are caused by Staphylococcus aureus, Pseudomonas aeruginosa, Escherichia coli, Klebsiella spp., Proteus spp., et cetera. Among these bacterial pathogens, S. aureus is the most common pathogen associated with post-caesarean wound infections. These infections are difficult to manage, especially when they are caused by multiple antibiotic-resistant strains of S. aureus7,9.
Citric acid, a natural product obtained from citrus fruits, has been used as a topical agent for the treatment of a variety of wound infections caused by multiple antibiotic-resistant strains of P. aeruginosa and E. coli10,11. In the present study, an attempt has been made to treat post-caesarean wound infections caused by multiple antibiotic-resistant strains of S. aureus refractory to conventional oral or injectable antibiotic therapy and local wound care (using irrigation with hydrogen peroxide and dressing with betadine) by using topical application of 3% citric acid ointment.
Material and Methods
A prospective open study on post-caesarean wounds infected with multiple antibiotic-resistant strains of S. aureus was carried out. The study protocol was approved by the institutional ethical committee of MIMSR Medical College, Latur, India (MIMSR EC1/97) and informed consent was taken from the patients who participated in the study.
A total of 20 females in the age group of 20–40 years who developed wound dehiscence in the range of 2.5 cm to 7 cm following LSCS and post-caesarean wound infections with multiple antibiotic-resistant strains of S. aureus in significant number on pus culture and not responding to conventional treatment with injectable or oral antibiotic/s and local wound care (hydrogen peroxide + betadine) were selected for the study.
The identity of S. aureus isolates from pus culture was confirmed by standard culture techniques, that is to say, specimen of pus was inoculated on blood agar and MacConkey agar. The colonies grown after overnight incubation at 37°C were confirmed using standard biochemical reactions12. The isolates of S. aureus were subjected to antibiotic susceptibility testing by the Kirby-Bauer disc diffusion method using ampicillin (10 µg), amikacin (30 µg), cefoxitin (30 µg), ceftazidime (30 µg), ciprofloxacin (5 µg), clindamycin (2 µg), linezolid (30 µg) and netillin (30 µg)13. The isolates of S. aureus were also tested for minimum inhibitory concentration (MIC) against citric acid by broth dilution method.
All 20 cases with their consent were selected for topical application of 3% citric acid ointment. Three percent citric acid ointment was prepared by mechanical mixing of citric acid with 100% pure petroleum jelly as a base in a mortar and used for wound dressing. The wounds were surgically debrided to remove necrotic material before initiating the application of citric acid ointment, and then were irrigated and cleaned with normal saline. After this, citric acid was filled in wound dehiscence and dressed with a sterile pad. This treatment modality was used once daily until the wound healed completely or showed formation of healthy granulation tissue. The large wounds showing healthy granulation tissue were closed by suturing. The patients were called for follow-up after one week. No antibiotics were given during the course of this treatment.
Results
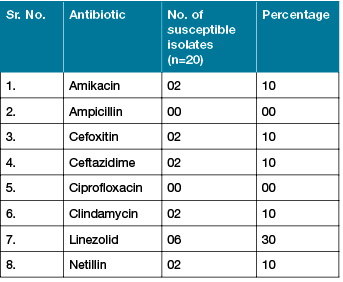
In vitro antibiotic susceptibility studies showed that out of 20 isolates, six (30%) were found to be resistant to all antibiotics tested against them. A total of 18 isolates (90%) were found to be methicillin-resistant S. aureus. Linezolid (30%) was found to be the most effective agent may be because of less exposure of S. aureus to this special reserved antibiotic, which is not much in use in India. No isolate was found to be susceptible to ampicillin and ciprofloxacin (Table 1). All the isolates of S. aureus were found to be inhibited by citric acid. The MIC to citric acid was found in the range of 900–1000 µg/ml of citric acid. Wound dressing with 3% citric acid ointment in 18 cases (90%) resulted in complete healing in 7 to 21 applications, whereas in two cases, in which wound dehiscence was very large, result was formation of healthy granulation. The number of cases and applications required for wound healing are shown in Graph 1. In two cases, wounds were closed by suturing. No adverse effects were noted in any of the patients, except for mild to moderate skin irritation in some patients. The follow-up of these cases after one week showed no signs of infections.
Table 1: Antibiotic susceptibility pattern of S. aureus isolates
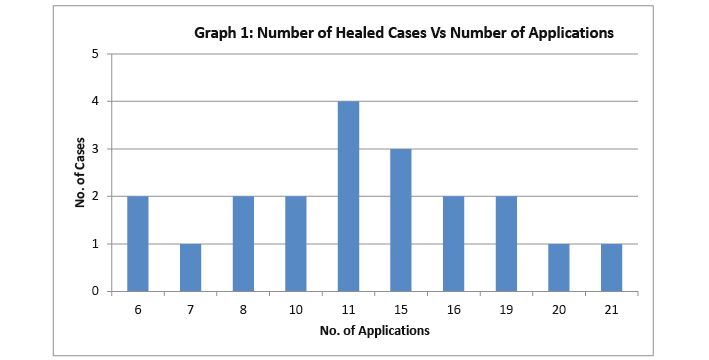
Note: In two cases with large wound dehiscence, healthy granulation tissue was formed after six applications
Discussion
Wound healing is a natural process and is taken for granted when the host–bacterium equilibrium is in balance. However, the presence of bacteria and bacterial products disturbing the host–bacterium equilibrium can cause disturbances in the normal phases of wound healing by affecting each and every phase in healing process. Thus, infection is the leading cause of non-healing of a wound. The higher levels of bacteria at a wound site prevent a timely and orderly healing trajectory. The healing, however, can be enhanced by reducing the bacterial burden14.
Although reduction of bacterial burden enhances the process of healing, it is quite difficult to reduce/eliminate bacterium from infected wounds, especially the multiple antibiotic-resistant bacteria that need special attention, and which, if not controlled, may become life-threatening. A number of experimental studies both in vitro and in animal wounds suggest that almost all antiseptic agents routinely used for local wound care may be toxic to the cells involved in the wound healing process and interfere with normal wound healing process15,16. The high levels of antibiotic present in the blood at the time of wounding clearly diminish, but do not eliminate wound infections. Antibiotics present in the blood at the time of injury are trapped in the fibrin clot, where they exert their effect, but when given later, they diffuse poorly into clotted fibrin and have little effect on bacteria present in the wound17,18.
In view of these problems, we initiated the use of citric acid for the effective treatment of wounds infected with a variety of bacteria, including multiple antibiotic-resistant strains10,11. Citric acid in a concentration of 3–5% has been reported to be highly effective in the treatment of infected wounds in animals19 and a concentration of 3% citric acid has been found optimum as far as its efficacy in the treatment of wound infections and adverse effects in the form of irritation are concerned20-23. Our earlier experience shows that the use of citric acid in a concentration of 3–5% is known to cause no adverse effects except for mild to severe irritation. It has been found to cause severe irritation in cases of venous ulcers and superficial burns and mild to moderate irritation in deep burns and traumatic wounds in non-diabetic individuals. In the present study, topical application of 3% citric acid ointment in all 20 cases was found effective in the successful elimination of multiple antibiotic-resistant S. aureus, which are otherwise very difficult to eliminate from the infection site, and successful healing of wounds without any adverse effects. This preparation of 3% citric acid prepared by triturating 3 g of citric acid in 100 g of petroleum jelly differs from RescuDerm™ in composition as well as its efficacy. The RescuDerm™ is an amorphous, organic acid-based gel containing a mixture of organic acids — acetic acid, citric acid and ethylenediaminetetraacetic acid (EDTA). However, citric acid is the only organic acid used in our study in a concentration of 3% against the concentration of 4% in a RescuDerm™. When considering efficacy also, the citric acid, as a single agent, was found more effective than RescuDerm™ containing a mixture of three different organic acids effective against marginally or moderately contaminated cutaneous wounds and comparatively less effective against heavily contaminated wounds24,25.
Conclusion
The results of the present study suggest that citric acid is effective in the successful elimination/reduction of burden of S. aureus, including multiple antibiotic-resistant strains and proves to be an effective alternative for the successful clinical management of post-caesarean wound infections caused by multiple antibiotic-resistant S. aureus. Citric acid could be useful in the prevention of post-operative wound colonisation with potential pathogens, if used as a dressing agent instead of conventional antiseptic agents since the time of operation in post-operative period. Future studies involving control group (randomised control trials) will help to achieve more useful and concrete conclusions.
Funding Sources
None.
Conflict of interest
None.
Author(s)
Basavraj S Nagoba*
PhD
Professor of Microbiology & Assistant Dean Research & Development
MIMSR Medical College, Latur, India
Email dr_bsnagoba@yahoo.com
Chandrakala A Dawle (Patil)
MD
Professor & HOD OBGY
MIMSR Medical College, Latur, India
Milind S Davane
MD
Assistant Professor, Department of Microbiology
MIMSR Medical College, Latur, India
Jyoti A Dawle
MD
Junior Resident 3
Department of OBGY
MIMSR Medical College, Latur, India
* Corresponding author
References
- Olsen MA, Butler AM, Willers DM, Devkota P, Gross GA, Fraser VJ. Risk factors for surgical site infection after low transverse cesarean section. Infect Control Hosp Epidemiol 2008;29(6):477–486.
- Schneid-Kofman N, Sheiner E, Levy A, Holcberg G. Risk factors for wound infection following cesarean deliveries. Int J Gynecol Obstet 2005;90(1):10–15.
- Opøien HK, Valbø A, Grinde-Andersen A, Walberg M. Post-cesarean surgical site infections according to CDC standards: rates and risk factors. A prospective cohort study. Acta Obstet Gynecol Scand 2007;86(9):1097–1102.
- Vijayan CP, Mohandas S, Nath AG. Surgical site infection following cesarean section in a teaching hospital. Int J Scientific Study 2016;3(12):97–101.
- Dahiya P, Gupta V, Pundir S, Chawla D. Study of incidence and risk factors for surgical site infection after cesarean section at first referral unit. Int J Contemp Med Res 2016;3(4):1102–1104.
- Declercq E, Barger M, Cabral HJ et al. Maternal outcomes associated with planned primary caesarean births compared with planned vaginal births. Obstet Gynecol 2007;109:669–677.
- Dhar H, Al-Busaidi I, Rathi B, Nimre EA, Sachdeva V, Hamdi I. A study of post-caesarean section wound infections in a regional referral hospital, Oman. Sultan Qaboos Univ Med J 2014;14:e211–e217.
- Killian CA, Graffunder EM, Vinciguerra TJ, Venzia RA. Risk factor for surgical-site infections following caesarean section. Infect Control Hosp Epidemol 2001;22:613–617.
- Al Jama FE. Risk factors for wound infection after lower segment cesarean section. Qatar Med J 2013;2012(2):26–31.
- Nagoba BS, Deshmukh SR, Wadher BJ et al. Treatment of superficial pseudomonal infections with citric acid: an effective and economical approach. J Hosp Infect 1998;40:155–157.
- Nagoba BS, Wadher BJ, Rao AK, Kore GD, Gomashe AV, Ingle AB. A simple and effective approach for the treatment of chronic wound infections caused by multiple antibiotic resistant Escherichia coli. J Hosp Infect 2008;69:177–180.
- Collee JG, Duguid JP, Fraser AG, Marmion BP, eds. Mackie & McCartney Practical Medical Microbiology, 14th edn. New Delhi: Elsevier-Churchill-Livingston, 2011.
- Bauer AW, Kirby WMM, Sherris JC, Turck M. Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol 1966;45:493–496.
- Robson MC. Wound infection — a failure of wound healing caused by an imbalance of bacteria. Surg Clin North Am 1997;77:637–650.
- Singer AD, Dagum AB. Current management of acute cutaneous wounds. N Eng J Med 2008;350:1037–1046.
- Kramer SA. Effect of povidone-iodine on wound healing: a review. J Vasc Nurse 1999;17:17–23.
- Russell RCG, Williams NS, Bulstrode CJL. Bailey and Love’s Short Practice of Surgery, 23rd edn. London: Arnold, 2000, pp. 147–162.
- Classen D, Evans R, Postotnik S, Horn SD, Menlove RL, Burke JP. The timing of prophylactic administration of antibiotics and the rise of surgical wound infection. N Eng J Med 1992;326:281–286.
- Nagoba BS, Wadher BJ, Selkar SP. Citric acid treatment of chronic wounds in animals. Int J Animal Veterinary Advances 2011;3(1): 26–28.
- Nagoba B, Gandhi R, Wadher B, Rao A, Selkar S. Simple and effective approach for the treatment of traumatic wounds in non diabetic patients: a prospective open study. Int Wound J 2013;10(5):585–589.
- Nagoba B, Patil C, Raju R et al. Citric acid treatment of post operative wound Infections in HIV/AIDS patients. J Tissue Viability 2014; 23(1):24–28.
- Nagoba B, Raju R, Wadher B et al. Citric acid treatment of surgical site infections: a prospective open study. Wound Practice & Research 2011;19(2): 82–86.
- Nagoba BS, Gandhi RC, Hartalkar AR, Wadher MJ, Selkar SP. Simple, effective and affordable approach for the treatment of burns infections. Burns 2010;36(8):1242–1247.
- Martineau L, Dosch H-M. Management of bioburden with a burn gel that targets nociceptors. J Wound Care 2013;16(4):157–164.
- Martineau L, Dosch H-M. Biofilm reduction by a new burn gel that targets nociception. J Applied Microbiol 2007;103(2):297–304.



