Volume 27 Number 1
Evidence summary: Venous leg ulcers: electric stimulation therapy
Emily Haesler for the JBI Wound Healing and Management Node
For referencing Haesler E. Evidence Summary: Venous leg ulcers: Electric stimulation therapy. WP&R Journal 2019; 27(1):52-54.
DOI https://doi.org/10.33235/wpr.27.1.52-54
Question
What is the best available evidence on effectiveness of electric stimulation therapy (EST) for healing venous leg ulcers (VLUs)?
Summary
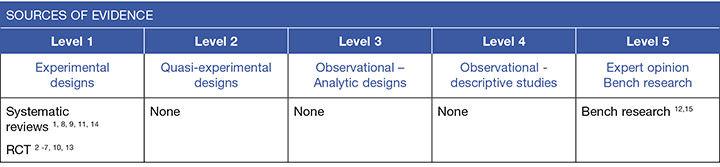
Venous leg ulcers (VLUs) are ulcers that occur on the lower leg due to venous disease. Application of electrical current to the wound through EST is thought to positively influence wound healing processes.1 Evidence from small randomised controlled trials (RCTs) suggests that EST is associated with more rapid healing of VLUs, primarily when it is used in conjunction with compression therapy.2-6 There is a very small amount of evidence suggesting EST could also be beneficial in clinical cases where compression therapy is not tolerated.4, 7 There is insufficient evidence to recommend any specific EST type or regimen over another (Level 1).
Best practice recommendation
Use electrical stimulation as an adjuvant to compression therapy and contemporary wound care for promoting more rapid VLU healing (Grade B).
Background
Venous leg ulcers occur due to venous insufficiency. Venous insufficiency describes a condition in which the venous system does not carry blood back to the heart in the most efficient manner, causing blood to pool in the veins of the lower limbs. Venous insufficiency occurs due to. 8, 9
- previous blood clots,
- impaired valves in the veins of the lower leg do not close sufficiently after each muscle contraction, allowing blood to flow back to a previous section of the vein (venous reflux), and
- calf muscle pump function not adequately assisting in returning blood to the heart.
Electric stimulation therapy (EST) is the application of electrical current to the wound bed. Application of EST is believed to increase microcirculation at the wound bed,5 increase the activity of cells involved in wound healing and inhibit the activity of pathogens1, 10 This may lead to more rapid collagen formation, particularly at wound edges leading to increased tensile strength.1
Different types of EST use direct, alternating or pulsed currents and high or low voltage.1, 11 Types of EST include pulsed electromagnetic field (PEMF), transcutaneous electrical nerve stimulation (TENS) and frequency rhythmic electrical modulation systems (FREMS). These various forms of EST are applied with the goal of either promoting healing, reducing pain or both.11
To apply EST to a VLU, two electrodes are used. An active electrode is placed on healthy peri-wound tissue5 or on saline soaked gauze directly on the wound bed.12 A passive electrode is positioned either on the opposite side of the wound or at a nearby anatomical location. The electrical current flows through the wound bed tissue.12
Evidence
In the trials2, 3, 5, 6, 10, 13 reported below (excluding one trial in which no compression was used,7 and one trial in which 39% of participants used no compression4), EST was used as an adjuvant to compression therapy. In one trial, participants were not using compression therapy above 25 mmHg pressure.4 In another trial, participants were also required to elevate their legs for at least 3 hours daily to remain in the trial6 (Level 1).
Evidence for EST to promote wound healing
High voltage FREMS (n=30) was compared to a topical preparation plus compression (n=32) and compression therapy alone (n=14) for healing VLUs in individuals with well-controlled diabetes mellitus. The EST regimen consisted of 100V, 100 Hz therapy applied for 50 minutes daily for three weeks. Complete wound healing rates were not significantly different between groups. The VLUs receiving EST displayed significantly greater reduction in wound areas (59% versus 35% for topical treatment and 25% for compression therapy alone, p<0.05)2 (Level 1).
FREMS was compared to standard wound care in another small RCT (n=39). The intervention consisted of FREMS (100 to 170 µA intensity and 0 to 300 V pulse amplitude) administered for 40 minutes, 5 days per week for 8 weeks. The intervention group achieved significant reduction in ulcer surface area compared to the control group by the third week of treatment (p<0.003)7 (Level 1).
Another small trial (n=20) explored FREMS used 5 days per week for 3 weeks compared with standard wound care. The VLUs treated with FREMS were significantly smaller compared to baseline after three weeks of treatment VLUs (mean difference 5.26±1.9cm2, p<0.005). This was a significantly greater reduction in ulcer size compared with the control group (p=0.0005). However, by five weeks, the difference in wound area was no longer significant.5
Another trial (n=64) conducted in participants with diabetes mellitus used an alternating current (bidirectional) EST at 80Hz applied for 20 minutes twice daily for three months. More ulcers receiving EST healed completely compared to VLUs receiving placebo comparator (42% versus 15%, p<0.05). There was also significantly greater reductions in wound surface area in the treatment group (59±11% versus 39±14%, p<0.05)3 (Level 1).
A small RCT (n=31) compared PEMF to a non-active treatment from a placebo device for treating long-standing VLUs. The EST regimen consisted of 0.06V/centimetre of wound bed using a biphasic pulse at 5Hz, applied for 3 hours daily for 2 months. Complete wound healing rates were not significantly different between groups. The VLUs receiving PEMF displayed significantly greater reduction in wound areas (48% versus 42%, p<0.0002)6 (Level 1).
A meta-analysis on EST in mixed chronic wounds (primarily not venous in aetiology) reported clear publication bias, with few studies with negative results being published1 (Level 1). There are some published RCTs that failed to demonstrate efficacy of EST. One trial reported on low frequency TENS (4mA, 5Hz) applied for 5 minutes, twice daily for 3 months13 and a second reported on EST (128 Hz and 300 µA with polarity changed on a 10-day cycle) applied daily for 30 mins for 100 days.10 In another RCT, EST (1-2 Hz) was administered 4 times daily in 20-minute sessions for 8 weeks.4 None of these trials showed significantly better wound healing outcomes compared with sham treatments, although all trials did demonstrate significant reduction in VLU size compared to baseline.4, 10, 13 All trials were small and not sufficiently powered. Wound size appeared to influence healing rates in two of the trials4, 10 (Level 1).
Type of EST regimen
There is only minimal evidence on the most effective type of EST. One meta-analysis14 that combined studies on wounds of different aetiology (15 studies, 4 of which included VLUs) compared bidirectional and unidirectional EST. Unidirectional EST showed a weighted mean difference (WMD) compared to sham of 30.8 (95% confidence interval [CI] 20.98 to 70.69, p<0.001; 11 studies, n=277 participants). In comparison, bidirectional EST had no significant effect (WMD 18.30, 95% CI –7.13 to 43.74, p=0.16; 4 studies, 230 participants).14 (Level 1). However, it has been proposed that different biological processes are influenced by EST throughout the healing process,10 suggesting that effectiveness of unidirectional versus bidirectional EST may relate to the stage of wound healing in which they are used.
Adverse events and considerations
Participants receiving EST in most of the RCTs reported above did not experience adverse events. In one trial, allergy and pain were reported, but not at greater rates than in comparator groups.3 In another trial, some participants experienced a slight burning sensation at FREMS electrode sites7 (Level 1).
The regimens for EST generally require daily or more frequent application of therapy, with each therapy application lasting between 5 minutes10 and 3 hours.6 Commitment to an intensive therapy regimen may be an issue for some individuals with chronic wounds5 (Level 1).
Methodology
The development of this evidence summary is based on the Joanna Briggs Institute methodology.16 A structured database search was employed using variations of the search terms describing VLUs and electric stimulation. Searches were conducted in EMBASE, Medline, AMED and the Cochrane Library for evidence from 1990 to June 2018 in English. Where high level evidence was available, lower level evidence was not reviewed.

Author(s)
Emily Haesler for the JBI Wound Healing and Management Node
References
- Barnes R, Shahin Y, Gohil R, Chetter I. Electrical stimulation vs. standard care for chronic ulcer healing: a systematic review and meta-analysis of randomised controlled trials. European Journal of Clinical Investigation, 2014;44(4):429-40. (Level ).
- Franek A, Polak A, Kucharzewski M. Modern application of high voltage stimulation for enhanced healing of venous crural ulceration. . Medical Engineering & Physics, 2000;22(9):647-55. (Level 1).
- Lundberg TC, Eriksson S, Malm M. Electrical nerve stimulation improves healing of diabetic ulcers. Ann Plast Surg 1992;29(4):328-31. (Level 1).
- Miller C, McGuiness W, Wilson S, Cooper K, Swanson T, Rooney D, Piller N, Woodward M. Venous leg ulcer healing with electric stimulation therapy: a pilot randomised controlled trial. Journal of Wound Care, 2017;26(3):88-98. (Level 1).
- Santamato A, Panza F, Fortunato F, Portincasa A, Frisardi V, Cassatella G, Valente M, Seripa D, Ranieri M, Fiore P. Effectiveness of the frequency rhythmic electrical modulation system for the treatment of chronic and painful venous leg ulcers in older adults. Rejuvenation Research, 2012. 01 Jun;15(3):281-7. (Level 1).
- Stiller MJ, Pak GH, Shupack JL, Thaler S, Kenny C, Jondreau L. A portable pulsed electro- magnetic field (PEMF) device to enhance healing of recalcitrant venous ulcers: a double-blind, placebo-controlled clinical trial. Br J Dermatol, 1992;127:147-54. (Level 1).
- Jankovic A, Binic I. Frequency rhythmic electrical modulation system in the treatment of chronic painful leg ulcers. Archives of Dermatological Research, 2008;300(7):377-83. (Level 1)
- Palfreyman S, Nelson EA, Michaels JA. Dressings for venous leg ulcers: systematic review and meta-analysis. BMJ, 2007;335(7613):244-56. (Level 1).
- O’Meara S, Cullum N, Nelson EA, Dumville JC. Compression for venous leg ulcers. Cochrane Database of Systematic Reviews, 2012(11). (Level 1).
- Junger M, Arnold A, Zuder D, Stahl H, Heising S. Local therapy and treatment costs of chronic, venous leg ulcers with electrical stimulation (Dermapulse): a prospective, placebo controlled, double blind trial. Wound Repair & Regeneration, 2008;16(4):480-7. (Level 1).
- Thakral G, LaFontaine J, Najafi B, Talal TK, Kim P, Lavery LA. Electrical stimulation to accelerate wound healing. Diabetic Foot & Ankle, 2013;4:22081. (Level 1).
- Taradaj J, Franek A, Blaszczak E, Polak A, Chmielewska D, Kro P, Dolibog P. Physical therapy in the treatment of venous leg ulcers: Biophysical mechanisms. Wounds: A Compendium of Clinical Research & Practice, 2012;24(5):138-45. (Level 5).
- Ogrin R, Darzins P, Khalil Z. The use of sensory nerve stimulation and compression bandaging to improve sensory nerve function and healing of chronic venous leg ulcers. Curr Aging Sci, 2009;2:72-80. (Level 1).
- Koel G, Houghton PE. Electrostimulation: Current status, strength of evidence guidelines, and meta-analysis. Advances in Wound Care, 2014. 01 Feb;3(2):118-26. (Level 1).
- Polak A, Franek A, Taradaj J. High-voltage pulsed current electrical stimulation in wound treatment. Advances in Wound Care, 2014. 01 Feb;3(2):104-17. (Level 5).
- The Joanna Briggs Collaboration. Handbook for Evidence Transfer Centers – Version 4. The Joanna Briggs Institute, Adelaide. 2013



