Volume 27 Number 1
Evidence summary: Venous leg ulcers: multi-layer compression bandaging
Emily Haesler for the JBI Wound Healing and Management Node
For referencing Haesler E. Evidence Summary: Venous leg ulcers: Multi-layer compression bandaging. WP&R Journal 2019; 27(1):49-51.
DOI https://doi.org/10.33235/wpr.27.1.49-51
Question
What is the best available evidence on effectiveness of multi-layer bandaging for healing venous leg ulcers (VLUs)?
Summary
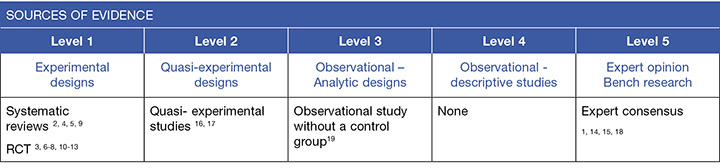
Venous leg ulcers (VLUs) are ulcers that occur on the lower leg due to venous disease. Compression therapy is recognised as gold standard treatment for promoting healing of VLUs.1, 2 The best available evidence indicates that a multi-layer bandaging system that incorporates an elastic bandage is one of the most effective compression therapy types for healing VLUs2-13 (Level 1).
Best practice recommendation
When there are no contra-indications, use multi-layer compression bandaging that incorporates a long stretch (elastic) bandage for promoting VLU healing (Grade A).
Compression therapy carries a higher risk for individuals with peripheral arterial disease, peripheral neuropathy, heart failure or vasculitic ulcers, but may still be indicated.14
Background
Venous leg ulcers occur due to venous insufficiency. Venous insufficiency describes a condition in which the venous system does not carry blood back to the heart in the most efficient manner, causing blood to pool in the veins of the lower limbs. Venous insufficiency occurs due to:2, 5
- previous blood clots,
- impaired valves in the veins in the lower leg do not close sufficiently after each muscle contraction, allowing blood to flow back to a previous section of the vein (venous reflux), and
- calf muscle pump function not adequately assisting in returning blood to the heart.
Compression therapy works by generating external pressure on the superficial veins and tissues, thereby assisting in venous return. This helps to reduce peripheral oedema and induration, and to promote lower limb wound healing.15 Compression systems usually utilise graduated pressure. Traditionally, higher pressure is attained at the ankles with pressure decreasing up the leg, although some contemporary systems use a negative pressure gradient.16, 17
Multi-layer bandaging is also referred to as 2-layer, 3-layer or 4-layer bandaging. A multi-layer system usually consists of orthopaedic padding and several layers of short stretch (inelastic, low extensibility) and/or long stretch (elastic, high extensibility) bandages.1, 18, 19 When applied, multi-layer bandaging usually has a high static stiffness index. This means that there is higher level of compression during standing or walking and a lower level of compression during rest (i.e. there is a high fluctuation in the level of pressure).1,18,19
Evidence
The type of multi-layer bandaging varied across the trials reported below. When reported, pressure was usually 40mmHg at the ankle and 20mmHg at the calf2 (Level 1).
Multi-layer bandaging compared with no compression for healing VLUs
Evidence for effectiveness of multi-layer bandaging comes three randomized controlled trials (RCT), all of which compared 4-layer bandaging with standard care that did not include any compression. The first trial found that significantly more VLUs treated with compression were healed at 12 months (risk ratio [RR] 4.0, 95% confidence internal [CI] 1.35 to 11.82, p=0.01). As well as a four times greater likelihood of healing, VLUs treated with compression also healed much faster.8 The second RCT reported significantly faster healing associated with compression in a survival analysis (adjusted hazard ratio 1.65, 95% CI 1.15 to 2.35, p<0.05, median weeks to healing 20 versus 43, p=0.03). However, this trial found no significant difference in number of VLUs healed at 12 months.6 In the third trial, VLUs treated with 4-layer bandaging were 1.8 times (95% CI 1.2 to 2.9) more likely to be healed at 12 weeks, and healing was at a significantly faster rate (p=0.006).7 Combined with studies supporting the effectiveness of other compression systems, there is good evidence that applying compression therapy will promote VLU healing2 (Level 1).
Multi-layer bandaging compared with other compression therapy for healing VLUs
A meta-analysis using a fixed-effects model that included patient data from five randomized controlled trials (RCTs) found no difference in number of VLUs that healed with 4-layer bandaging compared to short stretch bandages (RR 0.96, 95% CI 0.88 to 1.05, p=0.34). Using a fixed-effects analysis model, 4-layer bandaging was associated with significantly faster VLU healing compared with SSBs (hazard ratio [HR] 1.32, 95% CI 1.09 to 1.60, p=0.0039). However, when a random-effects model was used, there was no significant difference in healing time (HR 1.30, 95% CI 0.94 to 1.80, p=0.11).2 The analyses reported in this review supported a recommendation that a multi-component system is most effective when an elastic bandage is included in the system.2
However, another meta-analysis including 5 RCTs reported 4-layer bandages systems with an elastic component were no more effective that inelastic SSBs (HR 0.88, 95% CI 0.76 to 1.02, p=0.08).9 A third meta-analysis that included 18 RCTs, showed no significant difference in healing between elastic (3- or 4-layer) bandaging systems and SSBs alone (RR 0.98, 95% CI 0.91 to 1.06, p=0.61). When limiting this analysis to only high quality RCTs, a trend favouring elastic multi-layer bandaging for VLU healing at 12 months was reported.4 (Level 1).
In studies published more recently,3 multi-layer bandaging is shown to be as effective as compression stockings for promoting healing, with bandaging achieving results faster in some studies. Ulcers treated with 4-layer bandaging showed a mean decrease in wound area of 58.62%, which was significant compared to 20% reduction (p=0.03) for Unna’s boot and 16.66% reduction (p=0.03) for SSBs.3 In another trial, there was significant difference in VLUs that healed with 4-layer bandaging compared to compression stockings (86% vs 77%, p=0.24), although healing was faster with 4-layer bandaging (10 weeks vs 14 weeks, p=0.08).10 In another trial comparing 4-layer bandaging, 2-layer bandaging with an elastic layer and 2-layer compression stockings, there was no significant difference in time to healing between the three groups (HR 0.99, 95% CI 0.79 to 1.25, p=0.96).11 Finally, 4-layer bandaging achieved similar results to pneumatic compression therapy when compared on number of ulcers healed after 12 weeks (31.6% pneumatic compression vs 42.3% 4-layer bandaging, p=0.30).13 (Level 1).
2-layer versus 4-layer bandaging systems
The evidence suggests that there are no differences in effectiveness between 2- and 4-layer bandaging when an elastic layer is used. A meta-analysis of three RCTs showed no difference in complete healing at three months (RR 0.83, 95% CI 0.66 to 1.05, p=0.12).2 A second meta-analysis of six RCTs showed 4-layered bandaging was not significantly different from multi-layer compression with less layers (RR 1.02, 95% CI 0.84 to 1.24)4 (Level 1).
Results of these meta-analyses are also supported by more recent RCTs. An RCT12 reported a comparison between 2-layer bandaging and 4-layer bandaging. Both systems included an elastic component and achieved 40mmHg compression. After 12-weeks, the results indicated that the systems are equivalent for promoting VLU healing (44% healed with 2-layer bandaging versus 39% healed with 4-layer bandaging). Absolute wound area reduction was similar between the two compression systems.12 Ashby’s study11 also found that although no difference in healing rates, a 2-layer bandaging system that including an elastic component had a higher probability of being both clinically effective and cost effective (Level 1).
Methodology
The development of this evidence summary is based on the Joanna Briggs Institute methodology.20 A structured database search was employed using variations of the search terms describing VLUs and compression therapy. Searches were conducted in EMBASE, Medline, AMED and the Cochrane Library for evidence from 1990 to May 2018 in English. Where high level evidence was available, lower level evidence was not reviewed.
Author(s)
Emily Haesler for the JBI Wound Healing and Management Node
References
- Partsch H. Compression therapy: clinical and experimental evidence. Annals of Vascular Diseases, 2012;5(4):416-22. (Level 5).
- O’Meara S, Cullum N, Nelson EA, Dumville JC. Compression for venous leg ulcers. Cochrane Database of Systematic Reviews, 2012(11). (Level 1).
- Dolibog P, Franek A, Taradaj J, Dolibog P, Blaszczak E, Polak A, Brzezinska-Wcislo L, Hrycek A, Urbanek T, Ziaja J, Kolanko M. A comparative clinical study on five types of compression therapy in patients with venous leg ulcers. International Journal of Medical Sciences, 2014. 14 Dec;11(1):34-43. (Level 1).
- Mauck KF, Asi N, Elraiyah TA, Undavalli C, Nabhan M, Altayar O, Sonbol MB, Prokop LJ, Murad MH. Comparative systematic review and meta-analysis of compression modalities for the promotion of venous ulcer healing and reducing ulcer recurrence. Journal of Vascular Surgery, 2014. August;60(2 SUPPL.):71s-90s.e2. (Level 1).
- Palfreyman S, Nelson EA, Michaels JA. Dressings for venous leg ulcers: systematic review and meta-analysis. BMJ, 2007;335(7613):244-56. (Level 1).
- Morrell CJ, Walters SJ, Dixon S, Collins KA, Brereton LML, Peters J, et al. Cost effectiveness of community leg ulcer clinics: randomised controlled trial. BMJ 1998;316(7143):1487–91. (Level 1).
- O’Brien JF, Grace PA, Perry IJ, Hannigan A, ClarkeMoloney M, Burke PE. Randomized clinical trial and economic analysis of four-layer compression bandaging for venous ulcers. Br J Surg, 2003;90(7):794–8. (Level 1).
- Taylor A, Taylor R, Marcuson R. Comparative healing rates and cost of conventional and four-layer treatment of venous ulcers. Phlebology, 1995;10:85. (Level 1).
- Nelson EA, Harrison MB. Different context, different results: venous ulcer healing and the use of two high-compression technologies. Journal of Clinical Nursing, 2014;23(5/6):768-73. (Level 1).
- Finlayson KJ, Courtney MD, Gibb MA, O’Brien JA, Parker CN, Edwards HE. The effectiveness of a four-layer compression bandage system in comparison with Class 3 compression hosiery on healing and quality of life in patients with venous leg ulcers: A randomised controlled trial. Int Wound J 2014. February;11(1):21-7. (Level 1).
- Ashby RL, Gabe R, Ali S, Saramago P, Chuang L-H, Adderley U, Bland JM, Cullum NA, Dumville JC, Iglesias CP, Kang’ombe AR, Soares MO, Stubbs NC, Torgerson DJ. VenUS IV (Venous leg Ulcer Study IV) - compression hosiery compared with compression bandaging in the treatment of venous leg ulcers: a randomised controlled trial, mixed-treatment comparison and decision-analytic model. Health Technology Assessment, 2014;18(57):1-294. (Level 1).
- Lazareth I, Moffatt C, Dissemond J, Lesne Padieu AS, Truchetet F, Beissert S, Wicks G, Tilbe H, Sauvadet A, Bohbot S, Meaume S. Efficacy of two compression systems in the management of VLUs: Results of a European RCT. Journal of Wound Care, 2012. November;21(11):553-65. (Level 1).
- Harding K, Vanscheidt W, Partsch H, Caprini J, Comerota A. Adaptive compression therapy for venous leg ulcers: a clinically effective, patient-centred approach. Int Wound J, 2016;13(3):317-24. (Level 1).
- Harding K, et al. Simplifying venous leg ulcer management. Consensus recommendations. www.woundsinternational.com. Wounds International., 2015. (Level 5).
- Wounds International. Principles of compression in venous disease: A practitioner’s guide to treatment and prevention of venous leg ulcers. 2013. (Level 5).
- Mosti G, Partsch H. Compression stockings with a negative pressure gradient have a more pronounced effect on venous pumping function than graduated elastic compression stockings. European Journal of Vascular & Endovascular Surgery, 2011;42(2):261-6. (Level 2).
- Mosti G, Partsch H. High compression pressure over the calf is more effective than graduated compression in enhancing venous pump function. European Journal of Vascular and Endovascular Surgery, 2012. September;44(3):332-6. (Level 2 ).
- Partsch H, Schuren J, Mosti G, Benigni J. The Static Stiffness Index: an important parameter to characterise compression therapy in vivo. J Wound Care, 2016;25(Suppl 9):S4-S10. (Level 5).
- Suehiro K, Morikage N, Murakami M, Yamashita O, Ueda K, Samura M, Hamano K. Study on different bandages and application techniques for achieving stiffer compression. Phlebology, 2015;30(2):92-7. (Level 3+).
- The Joanna Briggs Collaboration. Handbook for Evidence Transfer Centers – Version 4. The Joanna Briggs Institute, Adelaide. 2013



