Volume 27 Number 3
Defining age-related skin tears: a review
Robyn Rayner, Keryln Carville and Gavin Leslie
For referencing Rayner et al. Defining age-related skin tears: a review. Wound Practice and Research 2019; 27(3):135-143.
DOI https://doi.org/10.33235/wpr.27.3.135-143
Abstract
Skin tears are reported to be the most common wound found amongst elderly individuals, yet there is a lack of evidence and consensus on a definition for these age-related traumatic injuries. A consensus on definition is essential for benchmarking prevalence and incidence and informing clinical diagnosis, management and reporting. This paper examines the extent of similarity and heterogeneity between the published definitions of skin tears and the underpinning evidence for the same. Five criteria were used to evaluate and compare the published skin tear definitions – reference to skin pathology; cause of injury; effect of injury; site of injury; and reference to the population group being studied. As a result of the review and recent research findings, which explicitly demonstrate age-related changes to the structural and mechanical properties of skin and associated increased risk of skin tears, the authors present a new skin tear definition based on these findings. Skin tears are defined as trauma-induced partial or full thickness wounds which primarily occur on the extremities of older persons with age-related changes to the skin’s structural and mechanical support properties, and are commonly associated with elastosis and/or ecchymosis.
Introduction
Cutaneous ageing is the outcome of both intrinsic (biological) and extrinsic (photoageing, smoking) processes and increasing evidence demonstrates time, environmental exposure and lifestyle-related activities influence the structural and mechanical properties of skin1-4. Recent research demonstrates that structural and mechanical property changes increase the risk of age-related skin tears5,6.
In Australia the occurrence of skin tears is a reportable adverse skin integrity event within residential aged care facilities, and optimal maintenance of skin integrity is considered an important quality care indicator7. These health providers are required to implement a surveillance system that reports skin tear incidence and to employ efficacious prevention and management strategies7. A consensus on skin tear definition would aid clinical diagnosis and direct evidence-based efficacious care interventions.
The lack of agreement amongst authors for the usage of a single definition may explain the absence of specific terminology and a category for coding skin tears in the World Health Organization International Classification of Diseases (ICD) 10th edition. Furthermore, the absence of a specific ICD-10 code for skin tears may reinforce clinicians’ perceptions that skin tears are insignificant, and this potentially leads to under-reporting of these wounds. According to the English Oxford Living Dictionary, a definition is “an exact statement or description of the nature, scope, or meaning of something”8. A definition for age-related skin tears therefore needs to be derived from rigorous evidence which enhances identification and understanding of these wounds and informs and promotes translation into clinical practice.
There are currently three skin tear classification systems that are prominently reported in the literature. These are the Payne and Martin Classification System for Skin Tears published in 1990 and revised in 1993; the Skin Tear Audit Research (STAR) Classification System published in 2007; and the International Skin Tear Advisory Panel (ISTAP) Classification 20139-11. However, despite efforts to establish a standard classification system, there is no universally accepted definition for skin tears to support the use of these tools12-17. Moreover, the term ‘skin tear’ is not globally recognised nor universally adopted in the literature. Although ‘skin tear’ is the most commonly cited term used within the English literature, the terms ‘skin tearing’, ‘skin laceration’, ‘epidermal tear’ and ‘geri tear’ have also been used to describe synonymous or similar wounds18-21. It is worth noting that the term ‘skin tear’ is not to be confused with medical adhesive-related skin injuries (MARSIs) which is a relatively recent term for classifying skin damage caused by adhesive product removal22. A MARSI is suspected where “erythema or other forms of skin injury persist” for longer than half an hour after removal of an adhesive22. While discernible skin irritation may not be evident following the initial removal of an adhesive product, with repeated application and removal of adhesive products, epidermal cells detach to impair the skin barrier and stimulate inflammation22.
In order to formulate an evidence-based definition of skin tears a review of the literature was undertaken, and five criteria were used to critique and compare published skin tear definitions. Previous research conducted by the authors5,6 led to new insights into the five criteria used in this review involving reference to – skin pathology; cause of injury; effect of injury; site of injury; and the population group being studied. The criteria were used to provide a structured framework for critiquing the evidence for definitions and examine the extent of similarity and heterogeneity between them. The results of the authors’ previous research and this review lead to a new skin tear definition which explicitly demonstrates association between age-related structural and mechanical skin changes and the increased risk for skin tears.
Methodology
Literature review
An initial examination of the Medical Subject Headings (MeSH) developed by the National Library of Medicine was undertaken as it uses conventional wordlists for standardising medical terminologies indexed in PubMed® and Medline®. However, there was no specific MeSH term for ‘skin tears’ as these wounds have not been indexed for citation23,24. Accordingly, a broader search of the literature was undertaken which identified all articles published in PubMed, Medline, CINAHL, Embase and Scopus between January 1990 and March 2019. The search builder used ‘all fields’ in the advanced search option. Inclusion criteria were English language articles identifying the key search terms ‘ageing’, ‘skin tears’ and ‘definition’. Papers that did not relate to older persons were excluded. A hand search of key papers identified in the search was conducted to locate further definitions.
Results
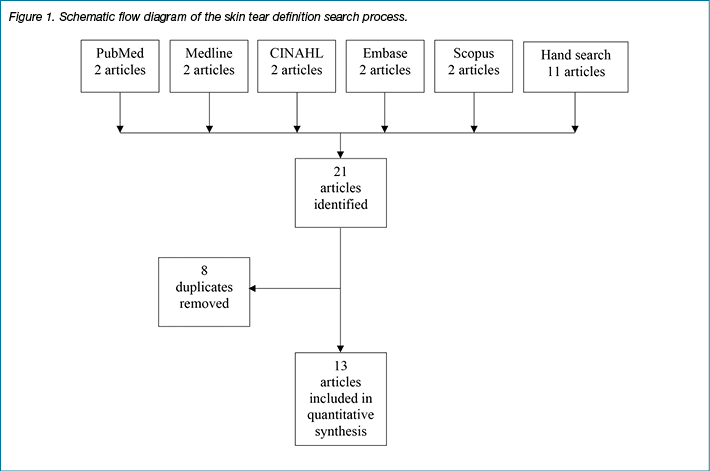
The initial database search identified 10 articles, and a further extensive hand search identified 11 additional papers. Eight of the 21 articles were subsequently excluded as they were duplicates. Only 13 articles that provided a unique skin tear definition were included in the next stage of the review. A schematic flow diagram of the skin tear definition search process is presented in Figure 1.
Skin tear definitions
All papers that provided a definition for skin tears were reviewed. No paper was excluded based on study design or quality of the evidence presented in the publication. A review of the skin tear definitions found in the literature is presented in chronological order (by year of publication) against the five predetermined criteria – reference to skin pathology, cause of injury, effect of injury, site of injury, reference population – that are listed in Table 1.
Table 1. A review of skin tear definitions identified in the English literature.
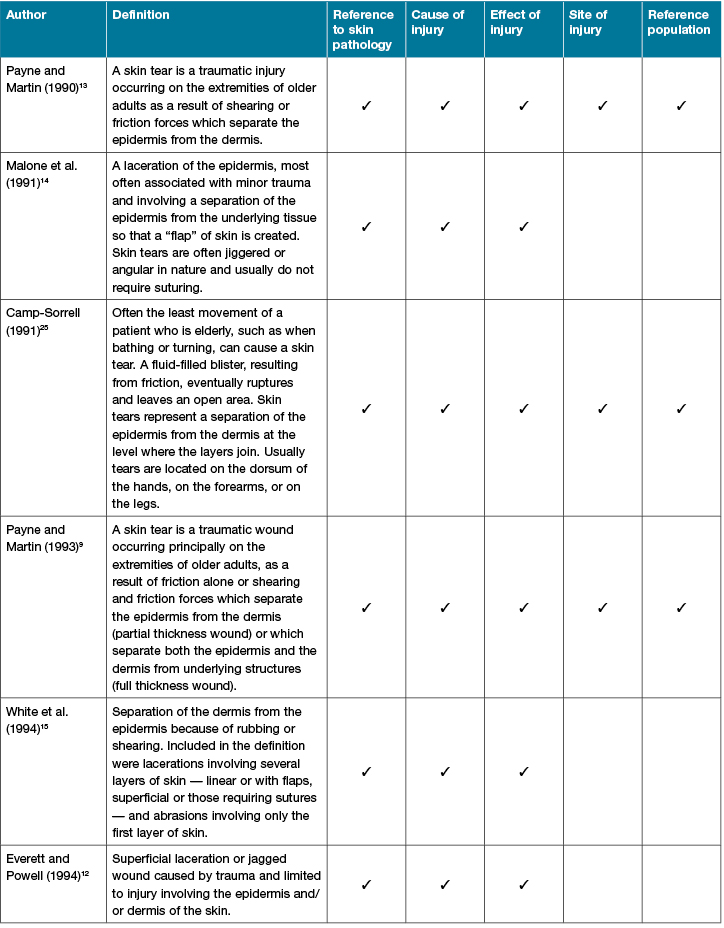
Table 1 continued. A review of skin tears definitions identified in the English literature
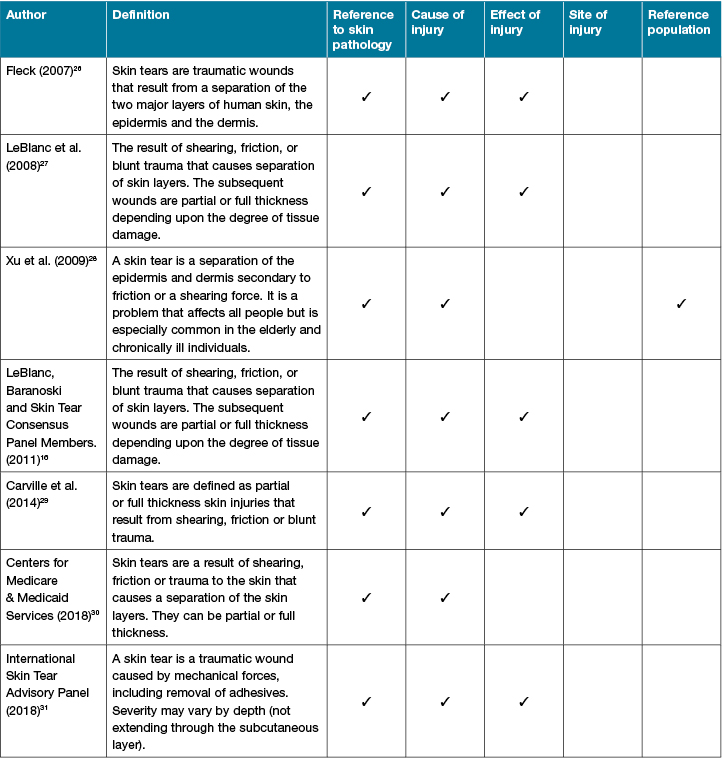
The literature review identified 13 skin tear definitions that comprised four primary articles which were published between 1990–199412-15, one critique article9, three general articles25,26,28, three best practice or consensus documents16,27,31, a case control study29, and a manual that provided guidance for using the Resident Assessment Instrument30. In the four primary articles, the definition used by authors to define skin tears was adopted prior to research undertaken for the specific purpose of determining the incidence or incidents for skin tears, identifying risk factors, or developing a classification tool12-15. Owing to lack of quantitative evidence, the operational definitions for skin tears appeared to be based on expert opinion.
There was considerable heterogeneity between the various definitions found when using the five search criteria. For example, all authors made either explicit reference to the epidermal and dermal layers of the skin, or implicitly referred to them in terms of ‘partial’ or ‘full thickness’ wounds. The ISTAP (2018), however, made only oblique reference to the epidermis and dermis by stating skin tears did not extend through to “the subcutaneous layer of the skin”. The subcutis or hypodermis is comprised of fat and loose connective tissue (elastic fibres and collagen) and supports the attachment of the integumentary system to the underlying fascia, muscles and bone32-34. All definitions made reference (explicitly or implicitly) to the cause of a skin tear in terms of shearing, friction forces, bathing, turning, rubbing, trauma, blunt forces, and mechanical forces.
The extremities were identified as the principal site for skin tears in three definitions9,13,25, while four definitions made specific reference to an older population9,13,25,28. It is proposed that reference to a population group is clinically relevant as skin tears can occur in individuals across all ages35. Visscher, Burkes, Adams, Hammill and Wickett (2017) demonstrated functional maturity of skin is not completed until the second year of life when increased collagen is found in the tissues36, and skin immaturity is considered a risk factor for skin tears in the very young. Conversely, the longevity of skin collagen and elastin and the cumulative effects of ageing and UV radiation have shown to progressively degrade the physical architecture of the skin, which alters the biomechanical behaviour and gross clinical appearance of skin37-40 with an associated increase in the risk for skin tears5,6.
Some skin tear definitions appear to be synonymous with a laceration or an abrasion12,14,15. Lacerations are defined by the National Library of MeSH as “torn, ragged, mangled wounds”41. Conversely, skin abrasions refer to an injury to the epidermal layer of the skin that are caused by friction forces42. Both descriptions, however, may also refer to the initial clinical appearance of traumatic skin tears.
Payne and Martin (1990) in their seminal paper were the first authors to operationalise the term ‘skin tears’ in older adults and devise a clinical classification system for skin tears. The definition was based on age-related skin changes reported in a journal article and book43,44 and was initially used in an unpublished pilot study to describe nursing interventions for skin tears13. The operational definition encompassed pathology (separation of the epidermis from the dermis), cause (shearing or friction forces), effect (traumatic injury), site of injury (extremities) and population group (older adults) of these wounds. Subsequently, the definition was used to guide a 3-month descriptive study to devise a classification system and identify factors that increased the risk for skin tears in 10 individuals aged between 58-105 years13.
Three years later these authors amended the definition to increase the reliability and usability of the classification system9. While the revised definition encapsulated the same five criteria, Payne and Martin (1993) identified three main issues with the original definition. The first definition limited the injury site to the extremities; however, subsequent research identified skin tears occurred on other locations including the head and trunk14. The second issue revolved around the terms “shearing and friction forces” and whether the original wording limited the definition to partial thickness wounds and did not encompass full thickness injuries. Likewise, the authors’ third concern related to linear tears, which they reported occurred in wrinkles or furrows and also resulted in full thickness skin loss. The Payne and Martin (1993) revised definition provided a historical perspective on skin tears and over the next 2 decades was to become the most cited skin tear definition45-48.
Another definition from Malone et al. (1991) included skin pathology (separation of the epidermis), a cause (trauma), and an effect (laceration of the epidermis; flap of skin) and was developed for the purpose of identifying baseline data on the incidence and risk factors for skin tears in a long-term aged care facility. Included in this definition for the first time was the term “flap” which provided a visual image of the separated tissue layers. These authors, however, interchanged the term skin tears with “laceration”. Malone et al. (1991) had extracted the information from 321 skin tear episodes recorded in incident reports compiled over a 12-month period.
Even though Camp-Sorrell (1991) did not provide a precise definition for skin tears (see Table 1), their description was included as it provided a historical perspective of the difficulty in defining these wounds. Camp-Sorrell’s (1991) expansive skin tear description, cited in a summary for the general management of skin tears, addressed the five criteria and it is the only description that made reference to “a fluid-filled blister”. A subsequent review of the literature by the authors did not identify any published article that made explicit reference to blisters and skin tears. Camp-Sorrell’s (1991) explanation in fact highlighted the clinical challenge associated with differentiating between skin tears and blisters caused by other aetiologies such as stage II pressure injuries49. Stage II pressure injuries present with partial loss of dermal tissue that may display an intact or ruptured blister50; however, potentially, a misdiagnosis can result in inappropriate management.
The White et al. (1994) skin tear definition included reference to the skin’s pathology (separation of the dermis from the epidermis), a cause (rubbing and shearing), and an effect (lacerations and abrasions). Lacerations were considered where there were multiple layers of skin loss, whereas abrasions were limited to loss of the epidermis15. It was unclear, however, whether skin tears were differentiated from laceration and abrasion or if the terms were used interchangeably. Nevertheless, their definition did not gain general acceptance, possibly due to this ambiguity.
Everett and Powell (1994) also developed their own definition for the specific purpose of investigating the incidence for skin tears in an aged and disabled population. This definition included reference to skin pathology (epidermis and/or dermis), cause of injury (trauma), and effect (superficial laceration or jagged wound) of injury. The authors also made direct reference to lacerations which, as previously noted, refer to “torn, ragged, mangled wounds”41. The utility of Everett and Powell’s (1994) definition was limited by indistinctness of wound type, and lack of inclusion of injury site and population group. However, it would be nearly 25 years before the literature differentiated between skin tears and lacerations31. In 2018, the ISTAP stressed that lacerations encompassed soft tissue tearing. This distinction indicates that lacerations can involve more extensive tissue types than skin tears since soft tissue comprises of muscle, adipose tissue, fibrous tissue, blood vessels and peripheral nerves51.
Likewise, Fleck (2007) proposed a definition which was cited in a general article for the prevention and management of skin tears. Their definition included only the first three of our criteria – reference to skin pathology (separation of the epidermis and dermis), cause of injury (trauma), and effect of injury (wound), with no reference to a site of injury nor population group.
In a Best Practice Recommendations for the Prevention and Treatment of Skin Tears document LeBlanc et al. (2008) provided a definition of skin tears which included the term “blunt trauma” and noted that partial or full thickness injury depended on the “degree of tissue damage”. The scope of the definition included skin pathology (separation of skin layers), a cause (shear, friction or blunt force), and an effect (partial or full thickness wounds). This definition was later adopted by the Skin Tear Consensus Panel in 201116.
In a general article for the management of skin tears, Xu et al. (2009) proposed a definition which included reference to skin pathology (separation of epidermis and dermis), cause of injury (friction or shearing force), and population (elderly and chronically ill individuals). Unfortunately, this definition was limited by the lack of direct reference to the effect or manifestation of the injury.
The Carville et al. (2014) definition which was used to conduct a case control study, referenced skin pathology (partial or full thickness), a cause (shearing, friction or blunt trauma), and effect (skin injuries) relationship. The definition arose from combining two previous definitions9,16. Likewise, the lack of clarity around the precise manifestation of the injuries may have limited the uptake of this definition.
The Centers for Medicare and Medicaid Services' (2018) simple definition encompassed the pathology (separation of the skin layers, either partial or full thickness) and cause (shearing, friction or trauma) of skin tears, but provided limited clinical value for the novice practitioner. No explanation was provided on how this definition was devised.
More recently, ISTAP (2018) proposed a definition that encompassed skin pathology (severity may vary by depth, for example not extending through the subcutaneous layer), cause of injury (mechanical forces), and effect (traumatic wound) of injury but omitted reference to a site of injury and population group31. The advisory panel did, however, note the influence of mechanical forces in causing skin tears. The inclusion of “removal of adhesives” highlights the debate and inconsistency in the literature around the concept of MARSI for classifying adhesive-related skin damage22.
Discussion
A revised skin tear definition
This review demonstrates the historical context and lack of quantitative research findings for supporting definitions for skin tears in older adults. The five criteria used in this review of skin tear definitions made reference to – skin pathology; cause of injury; effect of injury; site of injury; and the population group being studied. The criteria provided a structured framework for critiquing the evidence for definitions. Only three definitions satisfied all criteria; however, the evidence for inclusion was founded on empirical knowledge of the time rather than rigorous research.
In comparison, the authors’ of this review published the findings of a 6-month prospective cohort study which was undertaken in Australia to identify factors that predicted the risk for skin tears6. The findings identified male gender, a history of skin tears, a history of falls, clinical elastosis, and clinical purpura as significant risk factors for age-related skin tears6. Multivariable analysis was conducted to better understand the inclusion of the two skin characteristics, elastosis and purpura, into the risk prediction model5. The analysis identified three individual variables (ageing, gender, smoking), three clinical skin variables (uneven skin pigmentation, cutis rhomboidalis nuchae, history of actinic keratosis), and one transepidermal skin property variable (collagen type IV) that significantly predicted the risk of skin elastosis5. Cutaneous manifestation of elastosis of the dorsal forearm was associated with photoaged-related skin changes and increased skin stiffness. Photoaged skin changes on exposed skin surfaces altered the underlying mechanical properties of skin and increased skin stiffness which altered skin elasticity and ultimately contributed to the risk of skin tears.
In contrast, four individual characteristics (age, history of skin tears, history of falls, antiplatelet therapy) and three skin properties (pH, subepidermal low echogenicity band of the dorsal forearms, skin thickness) were found to predict the risk of purpura5. Purpuric lesions of the dorsal forearm were associated with aged-related skin changes and decreased skin thickness, conceivably as a result of loss of dermal collagen. The reduction in skin thickness most likely impaired the skin’s structural integrity and ability to resist mechanical forces and contributed to the risk of skin tears5.
The study showed that underlying the clinical manifestations of elastosis and purpura were progressive changes to the skin’s structural and mechanical properties from the effects of chronological ageing, environmental, and lifestyle-related influences5.
For the purpose of their research Rayner et al. (2019)6 defined elastosis as coarse, thickened, scaly, dry and rigid texture skin that manifested across photo-exposed sites when compared to adjacent non-exposed skin sites52,53. The researchers also referred to ecchymosis as benign, non-palpable skin lesions that were either round or irregular in shape and had a purplish/brown colouration23,54. Lesions that measure less than 2 mm in diameter are commonly referred to as petechiae and were not assessed by the researchers. The two commonly ecchymotic manifestations of ageing skin that were reported in the skin tear literature were purpura and/or senile purpura13,15,55-57. Rayner et al. (2019)6 classified purpura as any isolated ecchymotic skin lesion that ranged in size between 2–20 mm, while ecchymosis – which is also known as senile purpura, actinic purpura, Bateman’s purpura, or traumatic purpura or corticosteroid purpura – referred to the more extensive ecchymotic lesions that manifested across exposed skin surfaces58-60.
Ecchymosis result from the extravasation of blood cells secondary to vascular fragility and a decline in connective tissue support of the vascular plexus, from aged-related and photoaged-related dermal changes54,61. Within the skin, the microcirculation is primarily located in the papillary plexus of the dermis, with the relative thickness of the blood vessel walls protecting the vascular bed from shearing forces62. Exposed skin surfaces, such as the dorsal forearms and hands, have accelerated aged-related decline in collagen and elastic fibres that lead to decreased connective support of microvascular tissue63,64. The cumulative exposure of skin to UV radiation is reported to contribute to the manifestation of purpuric skin lesions65-67.
The use of the word ‘bruise’ within the skin tear literature appears to be synonymous with the term ecchymosis15,46,55,68-72. Within the medical literature, a bruise, otherwise known as a contusion, refers to localised extravasation of blood that arises from a non-penetrating blunt force or crush injury that causes characteristic bluish-purple discolouration of the skin and subcutaneous tissue23,73,74. Bruises initially appear with a bluish-purple discolouration that progressively dissolves within 2–3 weeks54. These lesions undergo characteristic colour changes that range from red, blue and purple in the first 5 days, to green after 5–7 days, to yellow after 1–2 weeks54. Caution is needed when interchanging these terms (bruising and ecchymosis), with Stedman’s Medical Dictionary advising against associating the term ‘bruise’ with any haemorrhagic lesion other than that which arises from a blunt force injury75.
The findings from the authors' previous research and this review suggest skin tears occur more commonly in elderly individuals and that current published skin tear definitions do not accurately reflect aged-related skin changes, cause, effect, common site of injury or population affected by the injury. Therefore, the following skin tear definition based on the findings of the authors’ work and this review criteria is presented:
“Skin tears are defined as trauma-induced (cause) partial or full thickness wounds (effect) which primarily occur on the extremities (site of injury) of older persons (population) with age-related changes to the skin’s structural and mechanical support properties (skin pathology), and are commonly associated with elastosis and/or ecchymosis”.
This review only examined skin tear definitions published in the English literature which may have excluded pertinent material published in another language. Any future review should therefore consider identifying definitions published in languages additional to English.
Conclusion
This review compares published skin tear definitions against five criteria – skin pathology, cause of injury, effect of injury, site of injury, and reference to a population group – to evaluate their utility. The new definition builds upon research that advances knowledge of skin properties and aged skin characteristics and skin tear occurrence in Caucasians. Replication of this study in other populations may provide new insights and evidence for age-related skin changes and their associations with skin tears across ethnicities.
Conflict of Interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
Author(s)
Robyn Rayner*
RN, BSc (Nursing), Postgrad (Health Admin), Master Wound Care, PhD
School of Nursing, Midwifery and Paramedicine, Curtin University, WA, Australia
Silver Chain Group, WA, Australia
Email: R.Rayner@curtin.edu.au
Keryln Carville
RN, PhD
School of Nursing, Midwifery and Paramedicine, Curtin University, WA, Australia
Silver Chain Group, WA, Australia
Gavin Leslie
RN, BAppSc, Post Grad Dip (Clin Nurs), PhD, FACN, FACCCN
School of Nursing, Midwifery and Paramedicine, Curtin University, WA, Australia
* Corresponding author
References
- Pawlaczyk M, Lelonkiewicz M, Wieczorowski M. Age-dependent biomechanical properties of the skin. Postępy Dermatologii i Alergologii 2013;5:302–6.
- Lynch B, Bonod-Bidaud C, Ducourthial G, Affagard J-S, Bancelin S, Psilodimitrakopoulos S, et al. How aging impacts skin biomechanics: a multiscale study in mice. Sci Rep 2017;7(1):13750.
- Tu Y, Quan T. Oxidative stress and human skin connective tissue aging. Cosmetics 2016;3(28).
- Kim KS, Park H-K, Lee J-W, Kim YI, Shin MK. Investigate correlation between mechanical property and aging biomarker in passaged human dermal fibroblasts. Microsc Res Tech 2015;78(4):277–82.
- Rayner RL, Carville KJ, Leslie GD, Dhaliwal SS. Clinical purpura and elastosis and their correlation with skin tears in an aged population. Arch Dermatol Res 2019;311(3):231–47.
- Rayner R, Carville K, Leslie G, Dhaliwal SS. A risk model for the prediction of skin tears in aged care residents: a prospective cohort study. Int Wound J 2019;16(1):52–63.
- Australian Government & Australian Aged Care Quality Agency. Assessment module compilation. Parramatta: Australian Aged Care Quality Agency; 2014. p. 1–64.
- English Oxford living dictionaries online [Internet]. Definition. 2016 [cited 2016 Oct 22]. Available from: https://en.oxforddictionaries.com/ definition/definition.
- Payne R, Martin M. Defining and classifying skin tears: need for a common language. Ostomy Wound Manage 1993;39(5):16–26.
- Carville K, Lewin G, Newall N, Haslehurst P, Michael R, Santamaria N, et al. STAR: A consensus for skin tear classification. Primary Intention 2007;15(1):18–28.
- LeBlanc KA, Baranoski S, Holloway S, Langemo D. Validation of a new classification system for skin tears. Adv Skin Wound Care 2013;26(6):263–5.
- Everett S, Powell T. Skin tears: the underestimated wound. Primary Intention 1994;2(1):28–31.
- Payne R, Martin M. The epidemiology and management of skin tears in older adults. Ostomy Wound Manage 1990;26(1):26–37.
- Malone ML, Rozario N, Gavinski M, Goodwin J. The epidemiology of skin tears in the institutionalized elderly. J Am Geriatr Soc 1991;39(6):591–5.
- White MW, Karam S, Cowell B. Skin tears in frail elders: a practical approach to prevention. Geriatr Nurs. 1994;15(2):95–9.
- LeBlanc KA, Baranoski S, Skin Tear Consensus Panel Members. Skin tears: state of the science: consensus statements for the prevention, prediction, assessment, and treatment of skin tears. Adv Skin Wound Care 2011;24(9):2–15.
- Cuzzell JZ. Clues: bruised, torn skin. Am J Nurs 1990;90(3):16–8.
- Yaar M, Gilchrest BA. Ageing and photoageing of keratinocytes and melanocytes. Clin Exp Dermatol 2001;26(7):583–91.
- Gottlieb NL, Penneys NS. Spontaneous skin tearing during systemic corticosteroid treatment. JAMA 1980;243(12):1260–1.
- Cuzzell JZ. Readers’ remedies for pressure sores. Am J Nurs 1986;86(8):923–4.
- Kennedy P, Kerse N. Pretibial skin tears in older adults: a 2 year epidemiological study. J Am Geriatr Soc 2011;59(8):1547–8.
- Yates S, McNichol L, Heinecke SB, Gray M. Embracing the concept, defining the practice, and changing the outcome. Setting the standard for medical adhesive-related skin injury interventions in WOC nursing practice. J Wound Ostomy Continence Nurs 2017;44(1):13–7.
- National Library of Medicine. Searching PubMed® with MeSH®. United States National Library of Medicine 2018:1–2.
- Rayner R, Carville K, Leslie G, Roberts P. A review of patient and skin characteristics associated with skin tears. J Wound Care 2015;24(9):406–14.
- Camp-Sorrell D. Skin tears: what can you do? Oncol Nurs Forum 1991;18(1):135.
- Fleck CA. Preventing and treating skin tears. Adv Skin Wound Care 2007;20(6):315–20.
- LeBlanc KA, Christensen D, Orsted HL, Keast DH. Best practice recommendations for the prevention and treatment of skin tears. Wound Care Canada 2008;6(1):14–30.
- Xu X, Lau K, Taira BR, Singer AJ. The current management of skin tears. Am J Emerg Med 2009;27(6):729–33.
- Carville K, Leslie G, Osseiran-Moisson R, Newall N, Lewin G. The effectiveness of a twice-daily skin-moisturising regimen for reducing the incidence of skin tears. Int Wound J 2014;11(4):446–53.
- Centers for Medicare & Medicaid Services. (2018). Long-term care resident assessment instrument (RAI) 3.0 User’s manual. Version 1.16. Retrieved from https://downloads.cms.gov/files/1-MDS-30-RAI-Manual-v1-16-October-1-2018.pdf
- International Skin Tear Advisory Panel. Best practice recommendations for the prevention and management of skin tears in aged skin. Wounds International 2018:1–21.
- Menon GK. Skin basics: Structure and function. Lipids and skin health. New York: Springer; 2015. p. 9–23.
- Menon G, K, Fartasch M. Structural and functional correlations of skin barrier in health and disease. Toxicology of the Skin. Florida: CRC Press; 2010: p.110–30.
- Wojcinski ZW, Rews-Jones L, Ibrahim Aibo D, Dunstan R. Skin. In: Sahota PS, Popp JA, Hardisty JF, Gopinath C, editors. Nonclinical safety assessment. Florida: CRC Press; 2013. p. 831–94.
- Serra R, Ielapi N, Barbetta A, de Franciscis S. Skin tears and risk factors assessment: a systematic review on evidence-based medicine. Int Wound J 2017;15(1):38–42.
- Visscher MO, Burkes SA, Adams DM, Hammill AM, Wickett RR. Infant skin maturation: preliminary outcomes for color and biomechanical properties. Skin Res Technol 2017;23(4):545–51.
- Verzijl N, DeGroot J, Thorpe SR, Bank RA, Shaw JN, Lyons TJ, et al. Effect of collagen turnover on the accumulation of advanced glycation end products. J Biol Chem 2000;275(50):39027–31.
- Castanet J, Ortonne J-P. Pigmentary changes in aged and photoaged skin. Arch Dermatol 1997;133(10):1296–9.
- Griffiths CEM. The clinical identification and quantification of photodamage. Br J Dermatol 1992;127(S41):37–42.
- Han A, Chien AL, Kang S. Photoaging. Dermatol Clin 2014;32(3):291–9.
- National Library of Medicine. Lacerations. Retrieved from https://www.ncbi.nlm.nih.gov/mesh/68022125 (accessed October, 2016).
- Das J. Trauma in otolaryngology. Singapore: Springer; 2018. p. 13–29.
- Fenske NA, Lober CW. Structural and functional changes of normal aging skin. J Am Acad Dermatol 1986;15(4):571–85.
- Porth C. Pathophysiology: concepts of altered health states. Philadelphia: JB Lippincott; 1986.
- Holmes R, Davidson MW, Thompson BJ, Kelechi TJ. Skin tears: care and management of the older adult at home. Home Healthc Nurse 2013;31(2):90–101.
- Lloyd-Jones M. The prevention and management of skin tears. Nurs Residential Care 2011;13(9):418–22.
- Gray D, Stringfellow S, Cooper P. Pilot RCT of two dressing regimens for the management of skin tears. Wounds UK 2011;7(2):26–31.
- Becker S. Examining the evidence: a systematic review of the literature related to skin tears in the older person. Adelaide: University of South Australia; 2003.
- LeBlanc K. Clinical challenges of differentiating skin tears from pressure ulcers. EWMA J 2016;16(1):17–23.
- European Pressure Ulcer Advisory Panel, National Pressure Ulcer Advisory Panel, Pan Pacific Pressure Injury Alliance. Prevention and treatment of pressure ulcers: quick reference guide. In: Haesler E, editors. Perth: Cambridge Media; 2014. p. 1–72.
- Houghton OP. Joint space, bone, soft tissues, and special techniques. In: Allen DC, Cameron RI, editors. Histopathology specimens: clinical, pathological and laboratory aspects. Cham: Springer International Publishing; 2017. p. 477–91.
- Patterson JW. Disorders of elastic tissue. Weedon’s skin pathology. 4th ed. China: Elsevier Health Sciences; 2016. p. 381–403.
- Raimer SS, Sanchez RL, Hubler Jr WR, Dodson RF. Solar elastotic bands of the forearm: an unusual clinical presentation of actinic elastosis. J Am Acad Dermatol 1986;15(4, Part 1):650–6.
- Cox NH, Piette WW. Purpura and microvascular occlusion. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook’s textbook of dermatology. Oxford: Wiley-Blackwell; 2010. p. 1–51.
- Lewin GF, Newall N, Alan JJ, Carville KJ, Santamaria NM, Roberts PA. Identification of risk factors associated with the development of skin tears in hospitalised older persons: a case-control study. Int Wound J 2016;13(6):1246–51.
- Newall N, Lewin GF, Bulsara MK, Carville KJ, Leslie GD, Roberts PA. The development and testing of a skin tear risk assessment tool. Int Wound J 2017;14(1):97–103.
- Skiveren J, Bermark J, LeBlanc J, Baranoski J. Danish translation and validation of the International Skin Tear Advisory Panel Skin Tear Classification System. J Wound Care 2015;24(8):388–92.
- Norman RA, Young EM, Jr. Benign vascular lesions. Atlas of Geriatric Dermatology. London: Springer; 2014. p. 243–9.
- Sandberg-Cook J, Blair G. Purpura. In: Buttaro TM, Trybulski J, Bailey PP, Sandberg-Cook J, editors. Primary care: a collaborative practice. Missouri: Elsevier Mosby; 2013. p. 290–2.
- Lotti T, Ghersetich I, Comacchi C, Panconesi E. Purpuras and related conditions. J Eur Acad Dermatol Venereol 1996;7(1):1–25.
- Husain Z, Cohen PJ, Schwartz RA, Lambert WC. Flexural and extensoral eruptions in dermatologic disease. Clin Dermatol 2011;29(2):195–204.
- Roddie IC. Circulation to skin and adipose tissue. Comprehensive physiology. New York: John Wiley & Sons Inc; 2011.
- Leo MS, Sivamani RK. Cosmeceutical treatments for purpura. Cosmeceuticals and active cosmetics. 3rd ed. Florida: CRC Press; 2015; 365–8.
- Gloster Jr HM, Gebauer LE, Mistur RL. Photodermatoses. Absolute dermatology review. Cham: Springer; 2016. p. 423–7.
- Kocsard B. Extravascular tissue factors in purpura. Australas J Dermatol 1967;9(2):189–97.
- Minkis K, Swary JH, Alam M. Photoaging. Cosmetic dermatology. New York: John Wiley & Sons Ltd; 2016. p.13–22.
- Durai PC, Thappa DM, Kumari R, Malathi M. Aging in elderly: chronological versus photoaging. Indian J Dermatol 2012;57(5):343–52.
- Thompson-McHale S. Preventing heel ulcers, skin tears and moisture damage. Nurs Residential Care 2016;18(4):192–7.
- Beechey R, Priest L, Peters M, Moloney C. An evidence-based approach to the prevention and initial management of skin tears within the aged community setting: A best practice implementation project. Joanna Briggs Institute Database of Systematic Reviews & Implementation Reports 2015;13(5):421–43.
- White W. Skin tears: a descriptive study of the opinions, clinical practice and knowledge base of RNs caring for the aged in high care residential facilities. Primary Intention 2001;9(4):138–49.
- Stephen-Haynes J, Carville K. Skin tears made easy. Wounds Int 2011; 2(3):1–6.
- Lopez V, Dunk AM, Cubit K, Parke J, Larkin D, Trudinger M, et al. Skin tear prevention and management among patients in the acute aged care and rehabilitation units in the Australian Capital Territory: a best practice implementation project. Int J Evid Based Healthc 2011;9(4):429–34.
- Bilo RC, Oranje A, Shwayder T, Hobbs C. Blunt-force trauma: bruises. Cutaneous manifestations of child abuse and their differential diagnosis. Berlin Heidelberg: Springer; 2013. p. 63–103.
- Randeberg LL, Winnem AM, Langlois NE, Larsen ELP, Haaverstad R, Skallerud B, et al. Skin changes following minor trauma. Lasers Surg Med 2007;39(5):403–13.
- Stedman’s Medical Dictionary [Internet]. Philadelphia (PA): Lippincott Williams & Wilkins; 2016. Bruise; [cited 2016 Aug 5]. Available from http://stedmansonlinecom/2016.



