Volume 29 Number 1
Wound dressings for prevention of radiation dermatitis: a WHAM evidence summary
Emily Haesler
For referencing Haesler E for Wound Healing and Management Centre. Wound dressings for prevention of radiation dermatitis: a WHAM evidence summary. Wound Practice and Research 2021; 29(1):53-55.
DOI https://doi.org/10.33235/wpr.29.1.53-55
Clinical question
What is the best available evidence for wound dressings for preventing radiation dermatitis in people undergoing radiation therapy for cancer?
Summary
Radiation dermatitis (RD) is an acute skin reaction that occurs as a result of radiotherapy used to treat a range of different cancers. Severity of symptoms ranges from erythema to dry desquamation (dry flaky skin with itching) to moist desquamation (serous exudate, oedema and blistering). Level 1 evidence1-3 for soft silicone film dressings used to prevent RD was mixed, with some studies showing decreased severity in RD,1, 2 including reductions in pain2 and burning sensations.2 Another study reported no benefits.3 Level 1 evidence4, 5 and Level 3 evidence6 for silver nylon dressings was also mixed; the largest study4 found reduction in pruritus to be the only significant effect. This evidence suggested that using a wound dressing as barrier protection against the effects of radiotherapy appears to be as effective as using a topical moisturiser. Development of a prevention plan should be individualised.
Clinical practice reccommendations
All recommendations should be applied with consideration to the wound, the person, the health professional and the clinical context.
There is no strong evidence on the prophylactic use of wound dressings to reduce the incidence of radiation dermatitis.
Sources of evidence
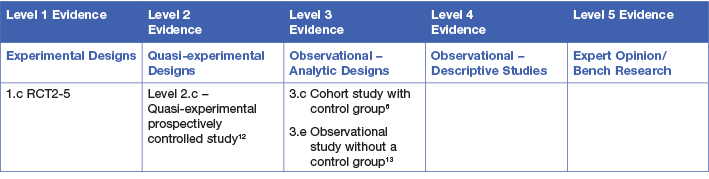
This summary was conducted using methods published by the Joanna Briggs Institute.7-11 The summary is based on a systematic literature search combining search terms related to radiation dermatitis/radiodermatitis and wound dressings and barrier films. Searches were conducted in Embase, Medline, Pubmed, the Cochrane Library and Google Scholar for evidence published up to January 2021 in English. Levels of evidence for intervention studies are reported in the table below.
Background
Radiation dermatitis is a common side effect of radiotherapy, which is a type of therapy delivered in the management of cancer. Radiation causes damage to epithelial cells and underlying structures of the skin, usually commencing early during radiotherapy and persisting up to six months following radiotherapy.14, 15 The severity of RD is related to the dose and regimen of radiation and the area of skin over which radiotherapy is administered,14-16 increasing when cell destruction occurs faster than normal cell reproduction. In early stages of RD the skin becomes warmer, itchy and erythema may present. As cumulative exposure to radiation increases, old skin becomes dry and flaky (referred to as dry desquamation). When the rate of new skin cell production cannot replace shedding cells the epidermis breaks down, becomes oedematous and exudate is present (referred to as moist desquamation).15 Pain, warmth, pruritus, burning sensations are reported by people experiencing RD.17 Consistent with outcome measures reported in the evidence, when referring to ‘grade’ of RD this evidence summary uses the Radiation Therapy Oncology Group (RTOG) scale for categorising the severity acute of RD.18
Wound dressings (films and silver nylon) are sometimes used as a barrier protection to reduce the skin symptoms associated with radiotherapy. This compares with topical preparations that are applied for their primary mechanism of moisturising the skin.
Clinical evidence
Consensus recommendations suggested that wound dressings applied for their barrier protection are a reasonable option for preventing radiodermatitis19 (Level 5).
Soft silicone film dressings
Three studies1-3 investigated the effectiveness of the same transparent soft silicone film dressing.† In the first RCT3 (n = 57) a soft silicone film dressing was compared to topical moisturiser to prevent moderate-to-severe RD in people with head and neck cancer. Treatment commenced at the start of radiotherapy and continued until grade 2.5 or greater RD (moist desquamation) occurred. There was a high withdrawal rate (46.4%) from the soft silicone film dressing group as participants experienced discomfort, feelings of tightness or were unable to adhere the dressing. There was no statistically significant difference in the rate of grade 2 RD (34.8% for dressings versus 35.7% control, p = 1.00) or grade 3 RD (4.3% versus 11.1%, p = 0.61)3 (Level 1).
In the second RCT1 people with breast cancer (n = 78 acted as their own controls), skin treated with the soft silicone film dressing had superior outcomes to skin receiving twice daily applications of aqueous cream. For skin treated with the soft silicone film dressing, 56% showed no symptoms, 36% developed grade 1 RD and 8% developed grade 2 RD. This compared to 100% of skin receiving the aqueous cream experiencing RD, with a greater number of severe cases recorded (grade 3 RD 26% versus 0%, p < 0.001). Participants reported the soft silicone film dressing, which was left in situ for up to four days during treatment, was reassuring and associated with less erythema, pruritus and pain1 (Level 1).
In the third RCT,2 participants with head and neck cancer (n = 22 across two study locations) acted as their own controls. There was a 37% reduction in incidence of moist desquamation in skin that received the soft silicone film dressing. Severity of RD assessed using the RISRAS score was statistically significantly lower for those receiving the film dressing compared to a standard protocol (2.97 ± 0.37 versus 3.68 ± 0.56, p < 0.003 for first study location and 2.62 ± 0.35 versus 4.23 ± 0.35, p < 0.008 for the second location). The soft silicone film dressing was associated with lower pain and burning sensations.2 (Level 1).
Transparent film dressings
A transparent film dressing** was tested as a prophylactic skin protection during radiotherapy in people with prostate cancer and compared to a standard protocol that included topical preparations chosen based on the severity of RD.12 Participants receiving standard treatment had profiles of significantly worse RD at completion of radiotherapy compared with those receiving the transparent film dressing (p < 0.001); however, days to development of RD were not significantly different. Some people using the film dressing experienced pruritus, erythema and folliculitis, leading to cessation of the dressing for 12% of participants12 (Level 2).
Silver nylon dressings
Three studies4-6 explored the same non-adherent, nanocrystalline silver coated nylon dressing.†† In the first, people receiving radiotherapy for lower gastrointestinal cancer were randomised to receive either a silver nylon dressing (n = 21) or standard skin hygiene (n = 19) to the perianal region. After two weeks, the average RD score was statistically significantly lower for people receiving the silver nylon dressing (p = 0.01), but this difference was no longer significant two weeks after treatment completion (p = 0.39)5 (Level 1).
In the second study, people receiving radiotherapy for perineal cancer (n = 15) had a silver nylon dressing applied from the stary of treatment until two weeks after completion of radiotherapy.6 Mean RD grade was 1.16 ± 0.40 at completion of the trial. This compared to an historical control cohort that had a mean grade of RD of 2.63 ± 0.48. In this small trial, RD grade was assessed by ten observers; there was a wide range in subjective assessments, reducing confidence in the results6 (Level 3).
In the largest trial, an RCT (n = 196), the silver nylon dressing failed to demonstrate a significant benefit compared to a skin hygiene regimen that included a moisturiser, with commencement of silver sulfadiazine on appearance of moist desquamation. In this study, the silver nylon dressing was worn continuously from the sixth day of radiation until day 14 with removal during radiotherapy and for bathing. There was no difference in incidence of moist desquamation, desquamation size or skin scores at completion of radiotherapy or one week later. However, there was a decrease in pruritus for women receiving the silver nylon dressing4 (Level 1).
† Mepitel® Film (Mölnlycke, Gothenberg, Sweden)
** FD Airwall (Kyowa Co Ltd, Osaka, Japan)
†† Silverleaf nylon dressing (Vomaris [formerly Silverleaf Medical Products], Tempe, AZ)
Considerations for use
If used, silver nylon dressings can remain in situ during administration of radiotherapy and do not appear to be associated with a bolus radiation dose.5
If used, soft silicone film dressings can stay in place for 7-10 days for most people. For some people, the film requires frequent reapplication, which is time consuming and costly. A trial period of four days is suggested to determine if soft silicone film would be appropriate.13
Conflict of interest
The authors declare no conflict of interest.
Author(s)
Emily Haesler
for Wound Healing and Management Centre, Curtin University (WHAM@Curtin)
References
- Herst PM, Bennett NC, Sutherland AE, Peszynski RI, Paterson DB, Jasperse ML. Prophylactic use of Mepitel Film prevents radiation-induced moist desquamation in an intra-patient randomised controlled clinical trial of 78 breast cancer patients. Radiother Oncol, 2014;110(1):137-43.
- Wooding H, Yan J, Yuan L, Chyou TY, Gao S, Ward I, al. e. The effect of Mepitel film on acute radiation-induced skin reactions in head and neck cancer patients: a feasibility study. Br J Radiol, 2018;91:bjr.20170298.
- Rades D, Narvaez CA, Splettstosser L, Domer C, Setter C, Idel C, Ribbat-Idel J, Perner S, Bartscht T, Olbrich D, Schild SE, Carl J. A randomized trial (RAREST-01) comparing Mepitel Film and standard care for prevention of radiation dermatitis in patients irradiated for locally advanced squamous cell carcinoma of the head-and-neck (SCCHN). Radiotherapy and Oncology, 2019;139:79-82.
- Aquino-Parsons C, Lomas S, Smith K, Hayes J, Lew S, Bates AT, MacDonald AG. Phase III study of silver leaf nylon dressing vs standard care for reduction of inframammary moist desquamation in patients undergoing adjuvant whole breast radiation therapy. J Med Radiat Sci, 2010;41(4):215-21.
- Niazi TM, Vuong T, Azoulay L, Marijnen C, Bujko K, Nasr E, Lambert C, Duclos M, Faria S, David M, Cummings B. Silver clear nylon dressing is effective in preventing radiation-induced dermatitis in patients with lower gastrointestinal cancer: Results from a phase III study. International Journal of Radiation Oncology Biology Physics, 2012;84(3):e305-e10.
- Vuong T, Franco E, Lehnert S, Lambert C, Portelance L, Nasr E, Faria S, Hay J, Larsson S, Shenouda G, Souhami L, Wong F, Freeman C. Silver leaf nylon dressing to prevent radiation dermatitis in patients undergoing chemotherapy and external beam radiotherapy to the perineum. International Journal of Radiation Oncology Biology Physics, 2004;59(3):809-14.
- Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. https://synthesismanual.jbi.global: Joanna Briggs Institute 2021.
- Joanna Briggs Institute Levels of Evidence and Grades of Recommendation Working Party. New JBI Grades of Recommendation. 2013. https://jbi.global/sites/default/files/2019-05/JBI-grades-of-recommendation_2014.pdf: Joanna Briggs Institute.
- Joanna Briggs Institute Levels of Evidence and Grades of Recommendation Working Party. JBI Levels of Evidence. 2013. https://jbi.global/sites/default/files/2019-05/JBI-Levels-of-evidence_2014_0.pdf: Joanna Briggs Institute.
- Joanna Briggs Institute Levels of Evidence and Grades of Recommendation Working Party. Supporting Document for the Joanna Briggs Institute Levels of Evidence and Grades of Recommendation. 2014. https://jbi.global/sites/default/files/2019-05/JBI%20Levels%20of%20Evidence%20Supporting%20Documents-v2.pdf: Joanna Briggs Institute.
- Munn Z, Lockwood C, S. M. The development and use of evidence summaries for point of care information systems: A streamlined rapid review approach. Worldviews Evid Based Nurs, 2015;12(3):131-8.
- Arimura T, Ogino T, Yoshiura T, Toi Y, Kawabata M, Chuman I, Wada K, Kondo N, Nagayama S, Hishikawa Y. Effect of Film Dressing on Acute Radiation Dermatitis Secondary to Proton Beam Therapy. Int J Radiat Oncol Biol Phys, 2016;95(1):472-6.
- Yee C, Lam E, Gallant F, Karam I, Czarnota G, Soliman H, Wong G, Drost L, Vesprini D, Rakovitch E, Wronski M, Leung E, Szumacher E, Carothers K, Pon K, Gonzales G, Easton L, Lewis D, Zhang L, Chow E. A Feasibility Study of Mepitel Film for the Prevention of Breast Radiation Dermatitis in a Canadian Center. Practical Radiation Oncology, 2021;11(1):e36-e45.
- Berger A, Regueiro C, Hijal T, Pasquier D, De La Fuente C, Le Tinier F, Coche-Dequeant B, Lartigau E, Moyal D, Seite S, Bensadoun RJ. Interest of supportive and barrier protective skin care products in the daily prevention and treatment of cutaneous toxicity during radiotherapy for breast cancer. Breast Cancer, 2018;12(no pagination).
- The Princess Royal Radiotherapy Review Team. Managing Radiotherapy Induced Skin Reactions. 2011. UK: St James’s Institute of Oncology, The Leeds Teaching Hospitals NHS Trust.
- Chen MF, Chen WC, Lai CH, Hung CH, Liu KC, Cheng YH. Predictive factors of radiation-induced skin toxicity in breast cancer patients. BMC Cancer, 2010;10 (no pagination)(508).
- Chan RJ, Webster J, Chung B, Marquart L, Ahmed M, Garantziotis S. Prevention and treatment of acute radiation-induced skin reactions: a systematic review and meta-analysis of randomized controlled trials. BMC Cancer, 2014;14:53.
- Collins A. Assessment and management of radiotherapy-induced skin reactions. Wounds UK, 2018;14(4):64-70.
- Russi EG, Moretto F, Rampino M, Benasso M, Bacigalupo A, De Sanctis V, Numico G, Bossi P, Buglione M, Lombardo A, Airoldi M, Merlano MC, Licitra L, Denaro N, Pergolizzi S, Pinto C, Bensadoun RJ, Girolomoni G, Langendijk JA. Acute skin toxicity management in head and neck cancer patients treated with radiotherapy and chemotherapy or EGFR inhibitors: Literature review and consensus. Crit Rev Oncol Hematol, 2015;96(1):167-82.




