Volume 29 Number 4
Review of necrotising fasciitis of Pfannenstiel incision with a case report
Tolga Kalayci, Esra Yaprak, Mustafa Yeni and İlker Uçar
Keywords abscess, caesarean section, fasciitis
For referencing Kalayci T et al. Review of necrotising fasciitis of Pfannenstiel incision with a case report. Wound Practice and Research 2021; 29(4):226-229.
DOI
https://doi.org/10.33235/wpr.29.4.226-229
Submitted 21 August 2021
Accepted 20 September 2021
Abstract
Necrotising fasciitis (NF), which can develop in any part of the body, is a serious and life-threatening rapidly progressive infection. In this case report, a case of NF located at a Pfannenstiel incision is presented and the treatment process of the patient is discussed. A 39-year-old primiparous woman who had a diagnosis of superimposed pre‑eclampsia was admitted to the emergency department with an eclampsia attack at 32 weeks of her pregnancy. Her medical history included diabetes mellitus and hypertension. An emergency caesarean section was performed. The patient was discharged on the 3rd day of her caesarean section without complications. On the 7th day of discharge, the patient fell in the bathroom. The patient was admitted to the emergency department on the second day of the fall due to foul-smelling discharge and wound dehiscence at the incision site. The patient was referred to the general surgery clinic and underwent emergency surgery by general surgeons with the diagnosis of NF. All necrotic tissues were removed until clean surgical margins were reached. Daily wound debridement was performed. On the 4th day of debridement, vacuum-assisted closure (VAC) treatment was started. After six sessions of VAC treatment, the patient’s wound was completely closed.
Introduction
Necrotising fasciitis (NF) is a serious and life-threatening infection characterised by rapidly progressive necrosis of the skin, subcutaneous tissues and fascia1. The synonyms of NF are flesh-eating bacteria, flesh-eating disease, or suppurative fasciitis. The annual incidence of NF varies from 0.3–15 per 100,000 population2–4. The main factors determining the course of the disease are the virulence of the causative pathogen, the age of the patient, the extent of the infection, the time of the first debridement, concomitant systemic diseases, and malnutrition5. Different terms and classifications have been used to describe NF. This variety of classifications and terminology has been based on affected anatomy, microbial cause, and depth of infection6.
At onset, NF can be difficult to differentiate from cellulitis and other superficial infections of the skin. In fact, studies have shown that only 15–34% of patients with NF have an accurate admitting diagnosis7,8. The most common reason for the delay in the diagnosis of NF is the inconsistency between clinical findings of the patients and the physical appearance of the lesion. Therefore, there is an area of infection that requires large debridement at the time of diagnosis. Cases with delayed diagnosis and treatment progress have a high morbidity and mortality. Reported mortality rates vary between 30–70% and are often related to causes such as multiorgan failure, respiratory failure, renal failure and sepsis9. NF patients with streptococcal infection are associated with an increased risk of complications and mortality of up to 80%10. Therefore, early diagnosis and surgical debridement are known contributors to improved outcomes in NF patients11. Not only do delayed diagnosis and surgical intervention influence in-hospital mortality, but the development of secondary complications also has an unfavourable impact12.
Treatment of NF is debridement that reaches healthy tissues and is repeated when necessary, and broad-spectrum antibiotherapy based on wound culture sensitivities. Vacuum-assisted closure (VAC) is also an important option for treatment in appropriate and accessible cases.
This case report presents a NF case located at a Pfannenstiel incision in a patient with diabetes mellitus and discusses the patient’s treatment process.
Case report
In June 2021, a 39-year-old primiparous woman who had a diagnosis of superimposed pre-eclampsia was admitted to the emergency department of the Erzurum Regional Education and Research Hospital, Erzurum, Turkey with an eclampsia attack at 32 weeks of her pregnancy. Her medical history included diabetes mellitus and hypertension. The patient’s visual acuity was decreased due to diabetic retinopathy. There was no history of surgery. At first examination of the patient, vital signs of the patient were as follows: blood pressure 185/80mmHg; pulse rate 122 beats per minute; oxygen saturation on room air 94%; and body temperature 38.7˚C. The patient’s weight was 120kg, and her height was 170cm (BMI 41.79). There was no laboratory pathology except high leukocyte count (18.1x103/mm3), high C-reactive protein (CRP) level (130mg/L), and HbA1C level 6.6%.
At 32w+1 of gestation, an emergency caesarean section was performed and a male neonate with birth weight of 1910g and an Apgar of 8–9 was born. The patient was discharged on postoperative Day 3 without complications. The baby was followed-up at the neonate intensive care unit due to prematurity.
On the 7th day of discharge, the patient fell in the bathroom. The patient, who only had pain at the incision site, presented to the emergency department on the second day of the fall due to foul-smelling discharge at the incision site. At examination of the wound, there was a purulent discharge and a 5cm wound dehiscence (Figure 1). The patient was referred to the general surgery clinic and underwent emergency surgery by general surgeons. On exploration, there was a partial opening with purulent discharge at the left side of the Pfannenstiel incision. In addition, there was a huge inflamed cellulitic area with crepitation. Abscess drainage was performed under general anaesthesia. Approximately 300cc purulent fluid came from the abscess area. A sample was taken from the abscess material and sent for culture. All the necrotic tissues were removed until the clean surgical margins were reached (Figure 2). The operation area was cleaned with a mixture of hydrogen peroxide and povidone iodine.
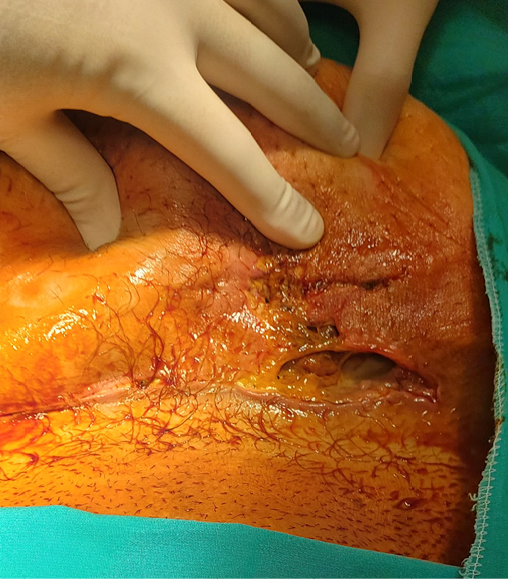
Figure 1. A 39-year-old woman admitted to the emergency department with a 5cm opening on a Pfannenstiel incision and purulent discharge

Figure 2. Wound appearance after the first debridement
Intravenous fluid treatment was started according to the BMI of the patient. Blood sugar level and blood pressure were monitored. A prophylactic antibiotic was commenced using piperacillin-tazobactam 4.5g intravenously (Q.I.D) and teicoplanin 400mg intravenously (B.D). Wound debridement and cleaning were applied to the patient for 3 days (Figure 3). On the 4th day of debridement, VAC treatment was started (Figure 4). Antibiotics were continued because Citrobacter koseri had grown in the wound culture and was sensitive to the current antibiotics. After six sessions of VAC treatment, the patient’s wound was completely closed (Figures 5 and 6). The patient was discharged on the 13th day of hospitalisation without complications.

Figure 3. Wound appearance after three sessions of debridement

Figure 4. Wound appearance at first VAC therapy

Figure 5. Wound appearance after third session of VAC therapy

Figure 6. Final view of the wound before discharge
Discussion
NF is a rare disease of the superficial fascia and subcutaneous tissue characterised by systemic toxicity and high mortality. Although the exact incidence of NF following obstetric surgical procedures is not known, NF is mostly seen after trauma or after surgical procedures13. Current literature suggests that NF can occur at any age, but it is mostly reported within the age range of 32–57 years, as in our patient14.
Although NF is common in elderly and immunocompromised patients, chronic diseases, intravenous drug use, malnutrition, obesity, malignancy, human immune deficiency virus, and long-term use of nonsteroidal anti-inflammatory and immunosuppressive drugs are also considered among the predisposing factors15. In the study by Jabbour et al., hypertension, diabetes mellitus and coronary artery disease were more prevalent among non-surviving patients9. In the present patient, the patient had uncontrolled diabetes mellitus and hypertension as chronic diseases, and obesity.
NF is mainly classified according to the anatomical region where it occurs, such as Fournier gangrene – gangrene at perineal, genital or perianal regions. Another classification is based on the number of pathogenic microbial factors – Type 1 (polymicrobial) and Type 2 (monomicrobial). Polymicrobial infections are more common, with cultures yielding a mixture of aerobic and anaerobic organisms16. Streptococcus pyogenes and Staphylococcus aureus are the usual detected pathogens6.
Diagnosis of NF is mainly based on clinical findings. NF often includes a triad of pain, tender local swelling, and fever17. However, in early period, pain and tenderness are not consistent with the physical appearance of the lesion. Pain may occur hours before infection and may be a later symptom due to diseases such as diabetes mellitus in which sensory neurons are affected. In the following days, oedema, redness, foul-smelling purulent discharge, and temperature increase are observed in the affected areas. Thin-walled haemorrhagic bullae occur in untreated and missed cases18. In cases of NF, the rate of spread of the infection can be up to 25mm/hour, with minimal changes in the overlying skin13. Therefore, early diagnosis and surgical debridement are important in treatment.
Plain x-ray films, ultrasonography (USG), computed tomography (CT) and magnetic resonance imaging (MRI) are useful imaging tools at the time of diagnosis of NF, but they are time-consuming and expensive and may not be readily available in an emergency setting. They might, however, be useful in cases where signs are equivocal, or diagnosis is in doubt. Subcutaneous gas on plain x-ray film can be seen in less than 25% of patients, and absence of gas does not exclude NF19. CT scans have a sensitivity of up to 80% in detecting necrotising soft tissue infections and deeply located abscess20. A MRI will show subcutaneous thickening with fluid collection during the diagnostic process21. However, in the present case, additional imaging methods were not required due to the diagnostic characteristics of the wound.
Treatment of NF includes multiple treatment modalities. First, surgical consultations should be urgently requested with the intention of early wound debridement for collection of tissue cultures, excision of all non-viable tissue, and delineation of the extent of the disease. In addition, until blood culture results are available, broad-spectrum antibiotics should be started to treat S. pyogenes, S. aureus, Gram-negative aerobes and anaerobic microorganisms. Then, according to the results of the culture antibiogram, the continuation and revision of the current antibiotherapy should be decided. Other important modalities in the treatment of NF are intravenous fluid replacement therapy and treatment of comorbid diseases, stabilisation of blood glucose level and blood pressure, and treatment of complications such as organ failure and shock22.
VAC therapy can be used to speed up the healing process in the treatment of cases that do not require resection after repeated debridements but have large tissue defects. In our case, VAC treatment was also used after three sessions of repeated debridement. Besides VAC therapy, hyperbaric oxygen is also an option during treatment of NF. Some studies have shown a reduction in mortality and morbidity, and the need for repeated debridement in up to two-thirds of cases with hyperbaric oxygen therapy23–25.
Conclusion
NF is a serious and life-threatening infection. Diagnosis of NF is mainly based on clinical findings. The classic and frequent manifestations associated with NF usually include a triad of pain, tender local swelling, and fever. However, in the early period, pain and tenderness are not consistent with the physical appearance of the lesion.
Treatment of NF includes wound debridement, broad-spectrum antibiotics, intravenous fluid replacement, stabilisation of blood glucose level and blood pressure, and treatment of complications. However, the most important step is early surgical extensive debridement until non-infective tissue is reached. It should be kept in mind that repeated debridements may be required and antibiotic revision may be required according to the antibiogram results.
Conflict of interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
Contributors
TK proposed the study and wrote the paper. All authors contributed to the design and interpretation of the study and to further drafts.
Author(s)
Tolga Kalayci1 MD
E-mail dr.tolgakalayci@gmail.com
Esra Yaprak2 MD
Mustafa Yeni2 MD
İlker Uçar1 MD
1Department of General Surgery, Erzurum Regional Education and Research Hospital, Erzurum, Turkey.
2 Department of Obstetrics and Gynecology, Erzurum Regional Education and Research Hospital, Erzurum, Turkey.
* Corresponding author
References
- Puvanendran R, Huey JCM, Pasupathy S. Necrotizing fasciitis. Can Fam Physic 2009;55(10):981–7.
- Chuang K-L, Liang F-W, Shieh S-J, Lu T-H. The incidence of necrotizing fasciitis in Taiwan: a nationwide population-based study. Annals Plastic Surg 2018;80(2S):S75–S8.
- Das DK, Baker MG, Venugopal K. Increasing incidence of necrotizing fasciitis in New Zealand: a nationwide study over the period 1990 to 2006. J Infect 2011;63(6):429–33.
- Glass G, Sheil F, Ruston J, Butler P. Necrotising soft tissue infection in a UK metropolitan population. Annals Royal Coll Surg Eng 2015;97(1):46–51.
- Medhi R, Rai S, Das A, Ahmed M, Das B. Necrotizing fasciitis – a rare complication following common obstetric operative procedures: report of two cases. Int J Women Hlth 2015;7:357.
- Goldstein EJ, Anaya DA, Dellinger EP. Necrotizing soft-tissue infection: diagnosis and management. Clin Infect Dis 2007;44(5):705–10.
- Wong C-H, Chang H-C, Pasupathy S, Khin L-W, Tan J-L, Low C-O. Necrotizing fasciitis: clinical presentation, microbiology, and determinants of mortality. JBJS 2003;85(8):1454–60.
- Hefny AF, Eid HO, Al-Hussona M, Idris KM, Abu-Zidan FM. Necrotizing fasciitis: a challenging diagnosis. Eur J Emerg Med 2007;14(1):50–2.
- Jabbour G, El-Menyar A, Peralta R, Shaikh N, Abdelrahman H, Mudali IN, et al. Pattern and predictors of mortality in necrotizing fasciitis patients in a single tertiary hospital. World J Emerg Surg 2016;11(1):1–10.
- Magala J, Makobore P, Makumbi T, Kaggwa S, Kalanzi E, Galukande M. The clinical presentation and early outcomes of necrotizing fasciitis in a Ugandan tertiary hospital – a prospective study. BMC Res Notes 2014;7(1):1–6.
- Kalaivani V, Hiremath BV. Necrotising soft tissue infection – risk factors for mortality. J Clin Diagnostic Res (JCDR) 2013;7(8):1662.
- Yu C-M, Huang W-C, Tung K-Y, Hsiao H-T. Necrotizing fasciitis risk factors in elderly Taiwan patients. Int J Gerontol 2011;5(1):41–4.
- Sarani B, Strong M, Pascual J, Schwab CW. Necrotizing fasciitis: current concepts and review of the literature. J Am Coll Surg 2009;208(2):279–88.
- Misiakos EP, Bagias G, Papadopoulos I, Danias N, Patapis P, Machairas N, et al. Early diagnosis and surgical treatment for necrotizing fasciitis: a multicenter study. Frontier Surg 2017;4:5.
- Artas H, Demir A, Dogan Z, Kavak B, Artas G. Role of Computed Tomography at Necrotizing Fasciitis That Develops After Cesarean Section: A Case Report. F.U. Sağ. Bil. Tıp Derg. 2014;28(2):73-75.
- Miller LG, Perdreau-Remington F, Rieg G, Mehdi S, Perlroth J, Bayer AS, et al. Necrotizing fasciitis caused by community-associated methicillin-resistant Staphylococcus aureus in Los Angeles. New Eng J Med 2005;352(14):1445–53.
- Wang J-M, Lim H-K. Necrotizing fasciitis: eight-year experience and literature review. Braz J Infect Dis 2014;18:137–43.
- Simonart T. Group a beta-haemolytic streptococcal necrotising fasciitis: early diagnosis and clinical features. Dermatol 2004;208(1):5–9.
- Lim Y-J, Yong F-C, Wong C-H, Tan AB. Necrotising fasciitis and traditional medical therapy – a dangerous liaison. Annals Acad Med Singapore 2006;35(4):270.
- Montrief T, Long B, Koyfman A, Auerbach J. Fournier gangrene: a review for emergency clinicians. J Emerg Med 2019;57(4):488–500.
- Mustatea P, Bugã C, Doran H, Mihalache O, Bobîrcã FT, Georgescu DE, et al. Soft tissue infections in diabetic patients. Chirurgia (Bucur) 2018;113:651–67.
- Taviloglu K, Yanar H. Necrotizing fasciitis: strategies for diagnosis and management. World J Emerg Surg 2007;2(1):1–3.
- Jallali N, Withey S, Butler P. Hyperbaric oxygen as adjuvant therapy in the management of necrotizing fasciitis. Am J Surg 2005;189(4):462–6.
- Bonne SL, Kadri SS. Evaluation and management of necrotizing soft tissue infections. Infect Dis Clin 2017;31(3):497–511.
- Stevens DL, Bryant AE, Goldstein EJ. Necrotizing soft tissue infections. Infect Dis Clin 2021;35(1):135–55.



