Volume 29 Number 4
The STAR classification: utility for determining healing times and dressing costs associated with skin tear management
Robyn Rayner, Keryln Carville, Joanna Smith and Cate Maguire
Keywords skin tears, STAR classification, purpura, senile purpura, haematoma
For referencing Rayner R et al. The STAR classification: utility for determining healing times and dressing costs associated with skin tear management. Wound Practice and Research 2021; 29(4):190-197.
DOI
https://doi.org/10.33235/wpr.29.4.190-197
Submitted 26 August 2021
Accepted 15 September 2021
Abstract
The aim of this study was to examine healing times and dressing costs for older adults with skin tears using the Skin Tear Audit Research (STAR) classification system. This retrospective study comprised all persons aged 65 years and over who had received wound care for a skin tear from a Western Australian not-for-profit community nursing organisation between 22 June 2016 and 31 December 2018. In total, 2161 skin tear images sustained by 1300 older adults (632 females and 668 males) aged between 65–103 (median number of healing days [Mdn]=86.0) years were examined. All skin tears had been photographed and recorded in an integrated database at point of care by nurses who had received formal training in using the STAR classification. The findings from this study show that STAR subcategory 2b, which the investigators found to be associated with the presence of a haematoma under a skin tear flap, significantly (p<0.001) increased healing times (days) and wound dressing costs ($AUD) compared to other STAR categories and subcategories. The STAR classification proved efficacious for determining healing times and dressing costs associated with skin tear management.
Background
The Skin Tear Audit Research (STAR) classification system was originally developed by The Silver Chain Group and Curtin University to provide a consensus for classifying skin tears1. The STAR tool aims to provide a clinical framework to guide appropriate assessment and management of skin tears.
Aged-related skin tears predominantly occur in individuals older than 65 years2. They are defined as trauma-induced partial or full thickness wounds which primarily occur on the extremities of older persons with age-related changes to the skin’s structural and mechanical support properties, and are commonly associated with elastosis and/or ecchymosis3. Skin tears are recognised as a traumatic wound that are reported to heal within 4 weeks4. However, when skin tears do not heal in an orderly and timely manner, they have the potential to become chronic wounds5,6. Skin tears which evolve into chronic wounds generally occur on the lower extremities due to associated vascular disease1.
Even though skin tears have been reported among individuals of all ages, the underlying mechanism of injury differs between younger and older individuals3,7. In the very young, skin immaturity is considered a risk factor as skin maturity is not completed until the second year of life when increased collagen is found in the tissues7. In contrast, the longevity of skin collagen and elastin, and the cumulative effects of ageing and ultraviolet radiation, have shown to progressively degrade the physical architecture of the skin and alter the biomechanical characteristics and gross clinical appearance of skin8–11. Both physiological ageing and photoageing have been shown to increase the risk for skin tears12,13. Furthermore, the influence of age-related skin and tissue changes impact on the wound healing trajectory of haemostasis, inflammation, proliferation and remodelling and can lead to a 20–60% delay in anticipated time to wound healing14.
The Silver Chain Group is a not-for-profit community health provider and wound management is its core clinical business. The occurrence of skin tears among clients necessitates a wound assessment using the STAR classification1. This comprises three skin tear categories (1, 2 and 3) and four subcategories (1a and 1b, and 2a and 2b), which are differentiated by skin colour changes and the ability to realign the tear to the normal anatomical position without undue stretching. The terms “pale, dusky or darkened” that are used to define the skin or flap colour originated from the reliability testing of the tool that was conducted in 2006 amongst nurses who were identified to be non-experts in wound management1. Consensus on terms amongst these nurses was not achieved until ‘simple’ language was used to define skin discolouration manifestations1. Vascular manifestations reported to be associated with skin tears include purpura, senile purpura and haematoma2,15,16. These manifestations are posited to cause the dusky and darkened discolouration associated with 1b and 2b subcategories.
Despite the STAR classification having been widely used by many clinicians to classify skin tears17–21, some have advocated for a simplified tool4,22 and such a modification was devised in 201323. The simplified classification devised by the International Skin Tear Advisory Panel (ISTAP) focused on three categories of degree of tissue damage, and not discolouration of flap or surrounding skin4,22. However, skin discolouration related to purpura and senile purpura (ecchymosis) as well as haematoma2,12,13,15,16 as aligned to STAR 1b and 2b definitions is commonly associated with skin tears19,24–28. These discoloured skin manifestations can arise from trauma or underlying pathological processes.
This study aimed to investigate the impact of these variables on time (days) to healing and median total dressing costs to treat a skin tear. The true cost of healing a skin tear would nonetheless be greater if clinical expenses and organisational overheads were included. To the best of our knowledge this is the first study to examine the implication of using a skin tear classification tool for determining healing times and dressing costs to treat.
Methodology
A descriptive retrospective cohort study was conducted with the aim to determine the association between skin tears, skin discolouration due to purpura, senile purpura and haematoma, and healing times and costs to treat community clients. Wound assessments are required to be undertaken on all new clients at time of admission or for any new wound that develops in a current client. All skin tear assessments and care plan decisions are electronically recorded in Silver Chain’s ComCare® Wound Module (CWM) at point of care by nurses with formal training in using the integrated database and the STAR classification. The costs of wound treatment products are automatically aligned to care plan entries and the time for nurses to perform the wound dressings are recorded in the principle ComCare® database.
All skin tear images entered in CWN between 22 June 2016 and 31 December 2018 were identified and extracted into an Excel® file by a data operator. The Excel® file was imported into the Statistical Package for the Social Sciences® (SPSS® version 26)29 by a registered nurse with expertise in wound management and who acted as the primary reviewer. Images were initially screened by the primary reviewer to identify the STAR classification accuracy as recorded in ComCare® on admission or skin tear occurrence. The primary reviewer then classified the wound image. If there was a difference in agreement between the initial classification awarded to a skin tear on admission or occurrence and that of the primary reviewer then the skin tear image was assessed by two other clinical experts to achieve consensus.
Study population
The study population comprised all clients aged 65 years and over who had a skin tear on the upper or lower extremities during the study period, and which had healed within 48 days. Although the healing range is outside that reported for acute skin tears, it encompasses the maximum 60% change associated with delayed healing that can occur in individuals aged over 65 years14. Skin tears on the extremities were selected for review as research demonstrates skin tears primarily occur amongst individuals on these anatomical sites1,25,26,30.
Analysis
Categorical data was represented by frequency (percentage) and median and interquartile range (IQR) for continuous variables. Chi-squared tests were conducted to evaluate the frequency data for categorical variables. All tests which were two-sided with a p value less than 0.05 were considered significant. As the independent variables were not distributed normally non-parametric tests of significance were utilised. The Mann‑Whitney U test was conducted to determine any differences in healing time (days) and total costs of wound dressing consumables where the skin tear showed a haematoma under a flap compared to skin tears without a haematoma. A Kruskal‑Wallis H test and Dunn’s multiple comparison test with a Bonferroni correction for multiple comparisons were conducted to examine whether differences between STAR subcategories and healing times (days), and total dressing costs ($AUD) were significant.
Cramer’s V statistic was used to estimate the effect size for tables larger than 2x2 – a negligible (0.0–0.10), weak (0.1–0.20), moderate (0.2–0.40), relatively strong (0.4–0.60), strong (0.6–0.80) and very strong (0.8–1.0) effect31. Data was obtained from the service providers’ integrated database and analysed using the SPSS® version 2629.
Ethical approval
Ethics approval for this study was obtained from Silver Chain (129) and Curtin University Research and Development Human Research Ethics Committees (2019-0211).The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki and the Australian Code for the Responsible Conduct of research32.
Results
A total of 2,161 skin tear images from 1,300 older adults (668 males and 632 females) who received community wound care between 22 June 2016 and 31 December 2018 were examined. There was no missing data as all database fields had been populated. Age, presence of photoageing, extremity site, STAR category and vascular lesion (purpura, senile purpura, haematoma) of males and females with skin tears are presented in Table 1.
Table 1. Age, photoageing, extremity, STAR category and vascular lesion of males and females with skin tears
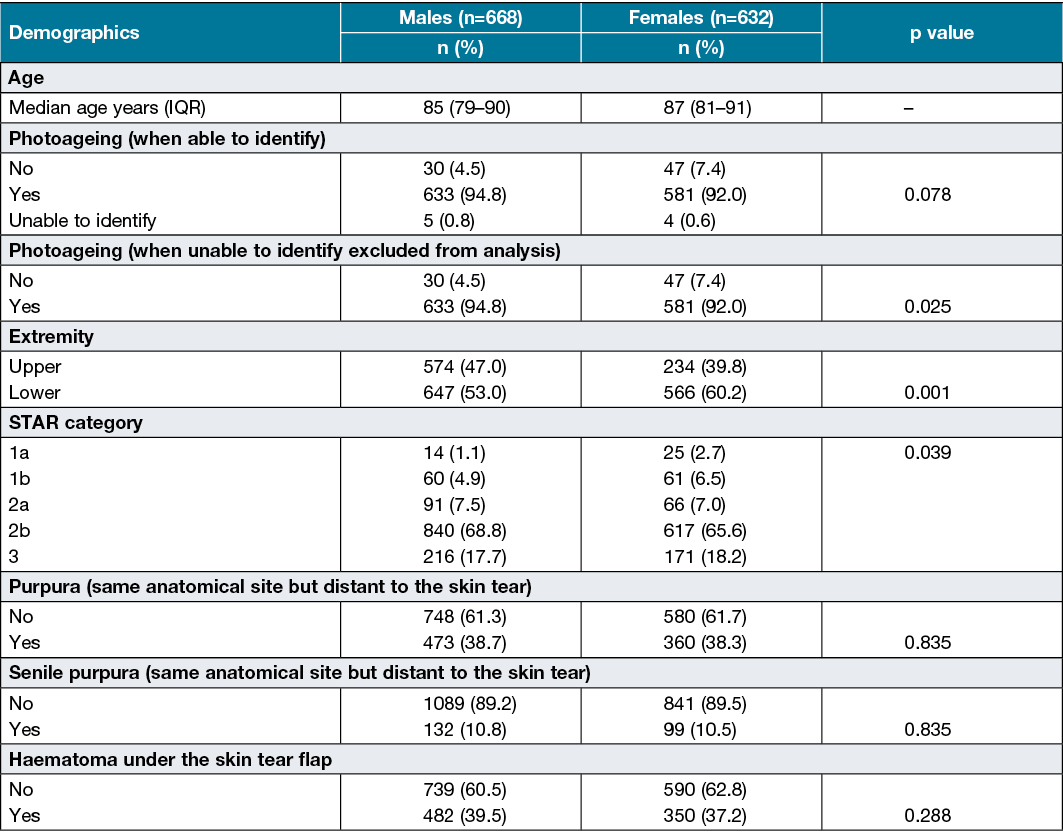
The 1,300 older adults ranged in age from 65–103 years with a median age of 86 (IQR 80–90) years. In total, skin tears occurred in 51.4% of males and 48.6% of females. Photoageing, which is associated with solar elastosis and was identified by uneven, coarse appearance, thickened, pigmented and dry scaly skin, was initially not significant in the skin tear images of males and females (Table 1). When the images of nine older adults where the presence of photoageing could not be determined were excluded from the analysis, photoageing was found to be significantly (p=0.025) associated with skin tears regardless of gender. A significantly (p=0.001) higher proportion of skin tears had occurred on the lower extremities compared to the upper extremities, and with females sustaining more skin tears than males. Regardless of gender, the majority of skin tears were classified as STAR category 2b. No statistical significance was identified between purpura, senile purpura, haematoma and skin tears. Table 2 presents the cross-tabulation results for the STAR classification and purpura. The presence of purpura was not evident at the injury but was obtained from the same anatomical site but distant to the skin tear.
Table 2. Cross-tabulation of STAR classification and purpura (same anatomical site but distant to the skin tear)
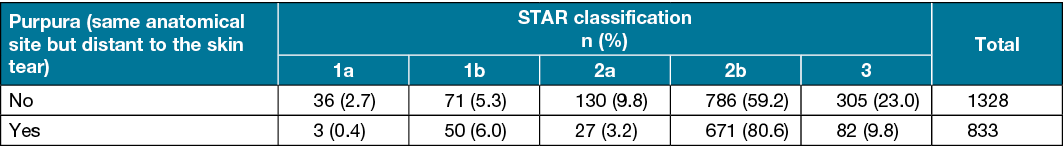
A chi-square test identified a statistically significant association between the STAR classification and purpura, X2(4)=130.161, p<0.001. Individuals with STAR subcategories 2b were significantly more likely to have purpura compared to other subcategories. The association between the STAR classification and purpura was moderate (φc=0.245). The presence of purpura was not evident at the injury but identified from the same anatomical site. A chi-square for association between the STAR classification and senile purpura was conducted. The results of the analysis are presented in Table 3.
Table 3. Cross-tabulation of STAR classification and senile purpura (same anatomical site but distant to the skin tear)
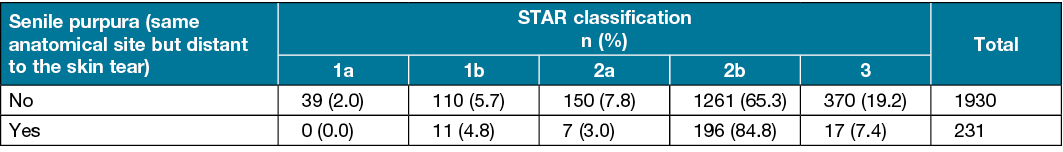
The chi-square test identified a statistically significant association between the STAR classification and senile purpura, X2(4)=39.098, p<0.001. Individuals with STAR subcategories 2b were significantly more likely to have senile purpura, which was not evident at the injury but identified from the same anatomical site, compared to other subcategories. The association between the STAR classification and senile purpura, however, was weak (φc=0.135). Excluding the nine individuals with 10 skin tears and where photoageing could not be identified, a chi-square analysis was conducted to determine associations between the STAR classification and the skin tear images which demonstrated signs of photoageing (Table 4).
Table 4. Cross-tabulation STAR classification and images showing photoageing
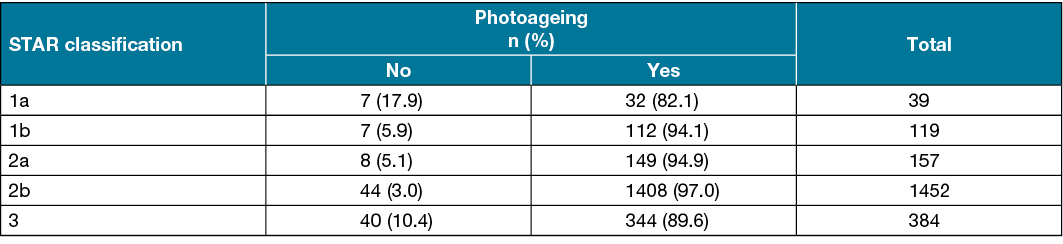
The analysis was conducted on a total of 2,151 skin tear images. The chi-square test identified a statistically significant association between the STAR classification and photoageing, X2(4)=50.206, p<0.001. Individuals with STAR subcategory 2b were more likely to show photoageing compared to other subcategories (Table 4). The association between the STAR classification and photoageing was weak (φc=0.153). A chi-square test was conducted to identify any association between the STAR classification and the presence of haematoma under a flap. The results of the analysis are present in Table 5.
Table 5. Cross-tabulation STAR classification and images with a haematoma under the skin tear flap
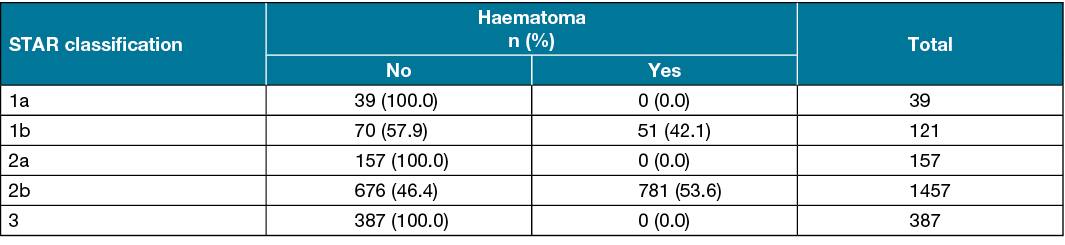
A statistically significant association was found between the STAR classification and the presence of a haematoma under the skin tear flap, X2(4)=506.012, p<0.001. Individuals with STAR subcategory 2b were significantly more likely to have a haematoma compared to other subcategories (Table 5). The association between the STAR classification and haematoma was relatively strong (φc=0.484).
A Mann-Whitney U test was run to determine if there were any difference in healing time and dressing costs (consumables only, not time for performing the intervention) for individuals aged over 65 years with a skin tear on the extremity, and with a haematoma under a flap, which healed within 48 days as compared to an individual whose skin tear healed within 48 days without a haematoma under a flap (Table 6).
Table 6. The median value and Mann-Whitney U test comparing healing time (days) and dressing costs ($AUD) for skin tears with and without haematomas under a flap
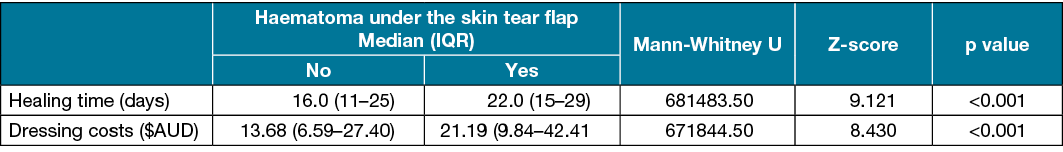
Dressing costs ranged between 7¢ (one simple, small island dressing) and $273.37 to heal a skin tear. The median healing time for skin tears with a haematoma under a flap (22 days) and without a haematoma (16 days) were statistically significantly different (U=681483.5, z=9.121, p<0.001). The median dressing cost to heal a skin tear with a haematoma ($21.19) and without a haematoma ($13.68) under a flap were also statistically significantly different (U=671844.5, z=8.430, p<0.001).
A Kruskal‑Wallis H test was run to determine if there were any differences between the STAR subcategories 1a, 1b, 2a, 2b and 3 for healing rates (days) and dressing costs. The Kruskal‑Wallis H test showed significant differences between the STAR subcategories for days to healing (p≤0.001) and total dressing costs to heal a skin tear (p≤0.001). A pairwise comparison between the STAR subcategories and the median number of days to healing was performed using Dunn’s33 procedure with a Bonferroni correction for multiple comparisons (Table 7).
Table 7. Results of post-hoc Dunn’s multiple comparisons test showing significance of difference in STAR classification subcategories for median number of days to healing
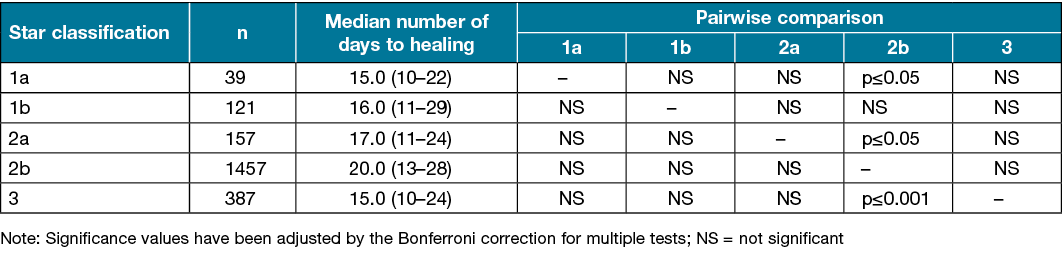
The median number of healing days increased from 1a (Mdn=15.0), to 1b (Mdn=16.0), to 2a (Mdn=17.0) to 2b (Mdn=20.0) STAR subcategories. Healing time decreased for STAR classification 3 (Mdn=15.0). The difference was statistically significant χ2(4)=50.647, p<0.001. The post hoc analysis revealed statistically significant differences in healing times: between the STAR subcategories 1a (Mdn=15.0) and 2b (Mdn=20.0) (p=0.046); between 3 (Mdn=15.0) and 2b (Mdn=20.0) (p<0.001); and between 2a (Mdn=17.0) and 2b (Mdn=20.0) (p=0.019), but not between other subcategory combinations. A pairwise comparison was also undertaken between the STAR subcategories and the median total dressing costs was performed using Dunn’s33 procedure with a Bonferroni correction for multiple comparisons (Table 8).
Table 8. Results of post-hoc Dunn’s multiple comparisons test showing significance of difference in STAR classification subcategories for median total dressing costs
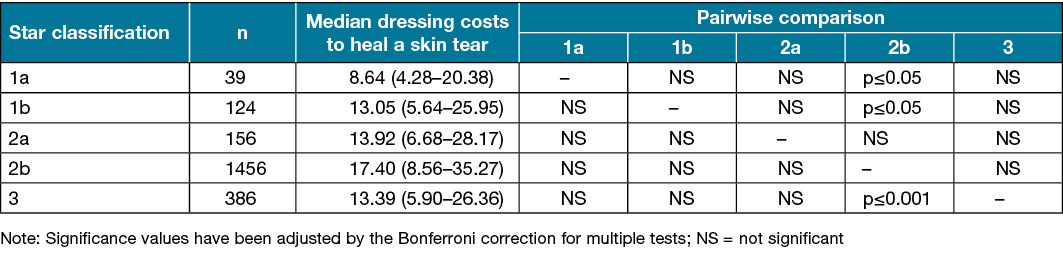
Consistent with healing time, the median total dressing costs to heal a skin tear increased from 1a (Mdn=8.64), to 1b (Mdn=13.05), to 2a (Mdn=13.92) to 2b (Mdn=17.40) STAR subcategories. The median dressing cost to heal a skin tear decreased for STAR classification 3 (Mdn=13.39). The difference was statistically significant χ2(4)=37.801, p<0.001. The post hoc analysis revealed statistically significant differences in median total dressing costs to heal a skin tear between the STAR subcategories 1a (Mdn=8.64) and 2b (Mdn=17.40) (p=0.018); between 1b (Mdn=13.05) and 2b (Mdn=17.40) (p=0.011); between 3 (Mdn=13.39) and 2b (Mdn=17.40) (p<0.001) but not between other subcategory combinations.
Discussion
The study population comprised 1,300 individuals (632 females and 668 males) aged between 65–103 years (median age=86.0), and who had a skin tear between 22 June 2016 and 31 December 2018 (Table 1). A total of 2,161 skin tear images from these 1,300 older adults were evaluated, with 43.9% of tears occurring on the upper extremities and 56.1% on the lower extremities. Regardless of gender, photoageing was present in the vast majority of skin tear images (Table 1). Both ageing and photoageing skin changes that principally occur on the extremities have shown to decrease the mechanical stability properties of skin and increase the risk for skin tears12,13,34,35.
The terms “pale, dusky or darkened” used to classify a skin tear 1b and 2b proved challenging when skin tear images were examined. Potential skin manifestations reported in the literature to be associated with the “dusky and darkened” skin hues for 1b and 2b skin tears included purpura, senile purpura and haematoma2,15,16. While the investigators did not identify any skin tear that fitted the “pale” category, a distinct difference in colour between the categories and subcategories based on the descriptor “dusky or darkened” hue was noted. While this study did not directly examine the term “dusky” in relation to skin tears, a potential cause for this characteristic hue may relate to partial venous congestion associated with the mechanical forces of oedema, haematoma, or anatomical torsion of local veins. Despite the lack of literature on the precise vascular cause of skin tear discolouration, these mechanical forces have been implicated in the dusky discolouration of compromised pedicle axial flaps36.
STAR classification and vascular manifestations
In reviewing the images, the investigators identified few images where purpura and senile purpura were within the skin tear injury. Previous research, however, showed progressive and generalised changes to the skin’s structural and mechanical properties from underlying chronological ageing, environmental and lifestyle-related influences increased the risk of purpura and elastotic skin manifestations that concomitantly increased the risk of skin tears15,16. Identification of purpura and senile purpura were obtained by reviewing other client extremity images from the same anatomical site in the CWM (Table 1). Cutaneous manifestations of purpura and senile purpura are transient in nature and arise from extravasation of blood into dermal tissue, secondary to connective tissue and blood vessel wall fragility induced by long-term exposure to ultraviolet radiation and ageing37,38.
Where purpura and senile purpura, however, was identified within the skin flap or around the wound edges, the researchers could not determine if these vascular lesions reduced the skin’s tensile strength and influenced the development of the skin tear or if they could be attributed to the injury itself. Nonetheless, recent research shows that purpura is a risk factor for skin tears due to the decline in structural integrity as a result of physiological ageing and photoageing12,13. As there was little evidence of purpura (Table 2) and senile purpura (Table 3) within the parameter of the skin tears, and the association between purpura was moderate (φc=0.245) and senile purpura was weak (φc=0.135) with the STAR classification, no additional analysis was undertaken of these clinical characteristics. The investigators also found that, despite the statistically significant (p<0.001) association between photoageing and skin tears (Table 4), the association was weak (φc=0.153) and, again, no further analysis was undertaken.
Haematoma on healing time and dressing costs.
The presence of haematoma under a skin tear flap showed a relatively strong (φc=0.484) association with the STAR subcategory 2b (Table 5) in individuals aged 65 years and over. There is, however, a paucity of studies that have examined the impact of skin tears with a haematoma under the flap on healing time and total dressing costs. An Australian non-match case control study by Lewin et al.15, which used multivariate analysis to evaluate a broad range of individual characteristics, identified haematoma as a risk factor for skin tears. A prospective cohort study of 1466 tertiary hospital patients by Newall et al.16 supported this finding. However, as the researchers collected data from nursing staff and inpatient medical records, it was unclear if the haematoma occurred at the time of injury or resulted from an underlying pathology. Moreover, the age of participants in both studies ranged from 50 years and over. In a cross-section observation study of 1153 aged care residents, Van Tiggelen et al.39 found that in univariate analysis participants with skin tears were significantly (p=0.001) more likely to have a haematoma than participants without a skin tear. None of these studies evaluated the impact of a haematomas under a skin tear flap on healing time or dressing costs.
The STAR subcategory 2b was significantly associated with longer healing time and higher dressing costs. The occurrence of a haematoma under a skin tear flap increased the median number of days for healing (Table 7) and the median total cost of dressings (Table 8). It was not unexpected that delayed skin tear healing was associated with a haematoma Table 6) as, physiologically, the collection of blood exerts pressure on underlying and surrounding tissue and thus impairs tissue perfusion which can cause necrosis40. In addition, autolysis of the haematoma can potentially provide a medium for micro-organisms that leads to infection and associated delayed healing. It was also not surprising that the total cost of dressings was directly associated with the increase time (days) to healing.
Strengths and limitations of the study
A strength of this study was the verification of the images by the investigators to determine the accuracy of the STAR classification prior to undertaking the analysis. This is the first study to examine the associations between the STAR classification subcategories and healing times and dressing costs. The findings from this study indicate that the STAR classification is a useful tool for identifying skin tear healing time and concomitant dressing costs. The study demonstrated that there was an association between the presence of a haematoma and STAR subcategory 2b. Skin tears that have a haematoma under the flap have increased healing time and total dressing costs.
The presence of purpura and senile purpura from underlying physiological ageing and photoageing likely relates to underlying morphological and physiological skin and tissue changes that reduce the mechanical and structural properties of skin with a corresponding increase in the risk for skin tears. Extrapolation of the results of this study is potentially limited to Caucasian Australians where lifestyle factors expose them to considerable UV radiation and resultant skin photoageing that increases the risk for skin tears.
Conclusion
The findings from the present study are of particular interest to all direct and indirect healthcare providers involved in managing skin tears. The STAR classification has demonstrated to be an effective tool for assessing skin tears and for providing a basis for risk stratification that determines which skin tears are likely to be more costly in terms of healing time and treatments. Additional research, however, in populations other than Caucasian Australians will determine the classification’s utility in other populations and provide more effective utilisation of the STAR classification.
Conflict of interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
Author(s)
Robyn Rayner1,2* RN, Postgrad (Health Admin), Master (Wound Care), PhD
Email Robyn.Rayner@silverchain.org.au
Keryln Carville1,2 RN, PhD
Joanna Smith1 BPsych
Cate Maguire1 RN, MPh (Candidate)
1The Silver Chain Group, 6 Sundercombe Street, Osborne Park, WA 6017, Australia
2School of Nursing, Curtin University, Perth, WA, Australia
* Corresponding author
References
- Carville K, Lewin G, Newall N, et al. STAR: a consensus for skin tear classification. Primary Intent 2007;15(1):18–28.
- Rayner R, Carville K, Leslie G, Roberts P. A review of patient and skin characteristics associated with skin tears. J Wound Care 2015;24(9):406–414.
- Rayner R, Carville K, Leslie G. Defining age-related skin tears: a review. Wound Practice Res 2019;27(3):135–143.
- International Skin Tear Advisory Panel (ISTAP). Best practice recommendations for the prevention and management of skin tears in aged skin. Wounds Int 2018:1–21.
- Goldberg SR, Diegelmann RF. What makes wounds chronic. Surg Clin North Am 2020 Aug;100(4):681–693.
- Lazarus GS, Cooper DM, Knighton D, et al. Definitions and guidelines for assessment of wounds and evaluation of healing. Wound Repair Regen 1994;2(3):165–170.
- Visscher MO, Burkes SA, Adams DM, et al. Infant skin maturation: preliminary outcomes for color and biomechanical properties. Skin Res Technol 2017;23(4):545–551.
- Verzijl N, DeGroot J, Thorpe SR, et al. Effect of collagen turnover on the accumulation of advanced glycation end products. J Biol Chem 2000 December 15, 2000;275(50):39027–39031.
- Castanet J, Ortonne J.-P. Pigmentary changes in aged and photoaged skin. Arch Dermatol 1997;133(10):1296–1299.
- Griffiths CEM. The clinical identification and quantification of photodamage. Br J Dermatol 1992;127(S41):37–42.
- Han A, Chien AL, Kang S. Photoaging. Dermatol Clin 2014;32(3):291–299.
- Rayner R, Carville K, Leslie G, Dhaliwal SS. A risk model for the prediction of skin tears in aged care residents: a prospective cohort study. Int Wound J 2019;16(1):52–63.
- Rayner R, Carville K, Leslie G, Dhaliwal SS. Clinical purpura and elastosis and their correlation with skin tears in an aged population. Arch Dermatol Res 2019;311(3):231–247.
- Sgonc R, Gruber J. Age-related aspects of cutaneous wound healing: a mini-review. Gerontol 2013;59(2):159–164.
- Lewin GF, Newall N, Alan JJ, et al. Identification of risk factors associated with the development of skin tears in hospitalised older persons: a case-control study. Int Wound J 2016;13(6):1246–1251.
- Newall N, Lewin GF, Bulsara MK, et al. The development and testing of a skin tear risk assessment tool. Int Wound J 2017;14(1):97–103.
- Edwards HE, Chang AM, Gibb M, et al. Reduced prevalence and severity of wounds following implementation of the Champions for Skin Integrity model to facilitate uptake of evidence-based practice in aged care. J Clin Nurs 2017;26(23–24):4276–4285.
- da Silva Torres F, Blanes L, Galvão TF, Ferreira LM. Development of a manual for the prevention and treatment of skin tears. Wounds 2019;31(1):26–32.
- Chang YY, Carville K, Tay AC. The prevalence of skin tears in the acute care setting in Singapore. Int Wound J 2016;13(5):977–983.
- Candeloro G. Skin tears. A quantitative study on the phenomenon and proposal for a prevention and management procedure. It J Wound Care 2017;1(2):1–66.
- Beechey R, Priest L, Peters M, Moloney C. An evidence-based approach to the prevention and initial management of skin tears within the aged community setting: a best practice implementation project. JBI Database System Rev Implement Rep 2015;13(5):421–443.
- LeBlanc KA, Baranoski S, Christensen D, et al. International Skin Tear Advisory Panel: a tool kit to aid in the prevention, assessment, and treatment of skin tears using a simplified classification system. Adv Skin Wound Care 2013;26(10):459–476.
- LeBlanc KA, Baranoski S, Holloway S, Langemo D. Validation of a new classification system for skin tears. Adv Skin Wound Care 2013;26(6):263–265.
- Johnson C, Katzman M. Managing skin tears with Medihoney®. Ostomy Wound Manage 2015;61(6):8–9.
- Koyano Y, Nakagami G, Iizaka S, et al. Exploring the prevalence of skin tears and skin properties related to skin tears in elderly patients at a long-term medical facility in Japan. Int Wound J 2014;13(2):189–197.
- Rayner R, Carville K, Leslie G, Dhaliwal SS. Skin tear risk associated with aged care residents: a cross-sectional study. Wound Practice Res 2018;26(3):127–135.
- Sanada, H, Nakagami, G, Koyano, Y, et al. Incidence of skin tears in the extremities among elderly patients at a long-term medical facility in Japan: a prospective cohort study. Geriatr Gerontol Int 2015;15(8):1058–1063.
- Minematsu T, Dai M, Tamai N, et al. Risk scoring tool for forearm skin tears in Japanese older adults: a prospective cohort study. J Tissue Viability 2021;30(2):155–160.
- IBM Corporation. Released 2019. IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp.
- Malone ML, Rozario N, Gavinski M, Goodwin J. The epidemiology of skin tears in the institutionalized elderly. J Am Geriatr Soc 1991;39(6):591–595.
- Kotrlik JW, Williams HA, Jabor MK. Reporting and interpreting effect size in quantitative agricultural education research. J Agric Educ 2011;52(1):132–142.
- Australian Government National Health and Medical Research Council. Australian code for the responsible conduct of research; 2007 [cited 2013 Jul 19]. Available from: https://nhmrc.gov.au/about-us/publications/australian-code-responsible-conduct-research-2007.
- Dunn OJ. Multiple comparisons using rank sums. Technometrics 1964;6(3):241–252.
- Escoffier C, de Rigal J, Rochefort A, et al. Age-related mechanical properties of human skin: an in vivo study. J Invest Dermatol 1989;93(3):353–357.
- Richard S, de Rigal J, de Lacharriere O, et al. Noninvasive measurement of the effect of lifetime exposure to the sun on the aged skin. Photodermatol Photoimmunol Photomed 1994;10(4):164–169.
- Zamboni WA, Baynosa RC. Compromised grafts and flaps. In: Neuman TS, Thom SR, editors. Physiology and medicine of hyperbaric oxygen therapy. Philadelphia: Elsevier; 2008. p. 373–395.
- Schwartz RA. Actinic purpura. Medscape 2019:1–7.
- Leslie TA. Purpura. In: Griffiths C, Barker J, Bleiker T, Chalmers R, Creamer D, editors. Rook’s textbook of dermatology. 9th ed. West Sussex, United Kingdom: John Wiley & Sons; 2016. p. 1–10.
- Van Tiggelen H, Van Damme N, Theys S, et al. The prevalence and associated factors of skin tears in Belgian nursing homes: a cross-sectional observational study. J Tissue Viability 2019;28(2):100–106.
- Thompson-McHale S. Haematomas: management and treatment. Wounds Essential 2015;10(1):24–28.



