Volume 29 Number 4
A quality improvement initiative to reduce hospital-acquired pressure injuries (HAPI) in an acute inpatient setting by improving patient education and seating
Sascha Holbrook, Colleen O’Brien-Malone, Annette Barton and Kristie Harper
Keywords wound healing, sitting position, occupational therapy, hospitals, pressure care
For referencing Holbrook et al. A quality improvement initiative to reduce hospital-acquired pressure injuries (HAPI) in an acute inpatient setting by improving patient education and seating. Wound Practice and Research 2021; 29(4):198-205.
DOI
https://doi.org/10.33235/wpr.29.4.198-205
Submitted 21 July 2021
Accepted 26 August 2021
Abstract
Aim Hospital inpatients are encouraged to sit out of bed to maintain function and reduce deconditioning; however, this increases the risk of hospital-acquired pressure injuries (HAPI) especially if seated on incorrect surfaces. This study aimed to reduce HAPI by providing pressure redistribution cushions and enhanced education.
Methods A before and after study design was utilised where hospital inpatients were provided with a pressure care intervention. Outcome measures consisted of the Waterlow Risk Assessment (WRA), incidence, stage and location of any pressure injuries, frequency of time spent sitting out of bed and hospital length of stay (LOS).
Results A total of 105 patients were recruited, with nine pressure injuries identified (control group n=5/52 vs intervention group n=4/53). Sixty percent of pressure injuries in the control group were HAPI compared to 25% in the intervention group (p=0.44). Patients in the intervention group reported increased comfort (86% versus 56%, p=0.05) and reduced pain (10% versus 43%, p=0.03). Patients in the intervention group sat out of bed more often (2.45 versus 1.63, p=0.02) and had a 17% increase in education engagement.
Conclusions Enhanced seating and education significantly improved patient reported outcomes including comfort and pain, and increased the patients’ time out of bed.
Key points
What is already known:
- Patients within the acute hospital setting are at greater risk of HAPI.
- Hospital inpatients are encouraged to sit out of bed; however, when seated, the body weight is exerted over a smaller surface area than when lying down or reclining, increasing the risk of HAPI.
- Pressure redistribution cushions reduce the surface interface pressure by spreading the load across a larger surface area and may decrease a patient’s HAPI risk.
What this manuscript contributes:
- Improved seating and education significantly improved patient-reported outcomes, including comfort and pain. Further research is warranted to determine if this approach can reduce the incidence of HAPI sustained while sitting out of bed.
- A quality improvement initiative to reduce HAPI in an acute inpatient setting by improving patient education and seating.
Introduction
Despite being preventable, hospital-acquired pressure injuries (HAPI) still occur1,2, impacting on patient outcomes and greatly increasing the cost of hospital care3–5. In 2015–2016 the Australian Commission on Safety and Quality in Healthcare (ACSQHC) found almost 4,313 occasions of HAPI6, estimated to cost the Australian healthcare system over $900 million1,3,7. In 2020 a systematic review and meta-analysis found a global pooled HAPI rate of 8.4% (95% CI 7.6–9.3%) in 1,893,593 adults, indicating that the burden of HAPI remains substantial8,9. The most frequently occurring stages were Stage I (43.5%) and Stage II (28.0%) and the most affected body sites were the sacrum, heels and hips8.
The development of pressure injuries is multifactorial, including a combination of shear, friction, pressure and microclimate, usually over a bony prominence. Many patients within the acute hospital setting are at greater risk of HAPI due to illness, being neurologically compromised, and having reduced mobility10,11. When seated, the body weight is exerted over a smaller surface area than when lying down or reclining, increasing the risk of pressure injuries12,13. Significant weight-bearing areas when sitting include the ischial tuberosities, the sacro-coccygeal area, the greater and lesser trochanters, and the intertrochanteric crests14–16. When sitting, these vulnerable areas receive higher pressures unless the surface provides increased envelopment resulting in immersion of the body and greater spread of the load13.
Patients in the hospital setting are encouraged to sit out of bed to maintain function and reduce deconditioning12. McCarthy et al.11 report that older patients sitting out of bed for more than 2 hours cumulatively per day were most at risk of developing HAPI from sitting. Pressure injury risk can be reduced when sitting on a pressure redistribution cushion13–15; however, they are not routinely provided to all patients in the hospital setting. Pressure redistribution cushions reduce the surface interface pressure by spreading the load across a larger surface area and away from vulnerable areas16–18. Previous studies have found that an armchair with a pressure redistribution cushion significantly reduces the incidence of HAPI19,20. An Australian hospital reported reducing HAPI by 35.0% after providing every patient with a pressure redistribution cushion, underpinned by staff and patient education20. However, in comparative research, the efficacy of cushion use in reducing pressure injury incidence was found to be inconclusive15,21,22.
A non-published prevalence survey at our acute tertiary hospital in Western Australia in 2018 found 13.0% of patients had pressure injuries, with HAPI levels at 9.3%. Given the initial success of previous pressure care initiatives, we proposed to implement a preventative approach to pressure care in our hospital. This study aimed to reduce HAPI by improving pressure redistribution seating options and enhancing patient and staff education.
Methods and materials
This was a pilot study that utilised a before and after, quasi-experimental study design to examine the impact of a preventative approach to managing pressure care injuries. The research questions were:
- Could a preventative approach to managing pressure injuries, including pressure redistribution cushions and patient and staff education, in addition to usual care, result in reduced HAPI?
- Does a preventative approach to managing pressure injuries result in reduced patient-reported pain, promote increased physical activity (time out of bed) and pressure care knowledge?
Setting and sample
This study was completed in a 30-bed ward comprising of medical and oncology patients for an 18-week period. The location for the study was recommended by the hospital wound management team and clinical nurse manager in response to the prevalence of HAPI and a patient cohort that had a high HAPI risk. All patients admitted to the ward who would be sitting out of bed during their hospitalisation were eligible for inclusion. Consecutive sampling was used for patients who were >18 years old. Those excluded were patients who would not be sitting out of bed due to medical status or end of life care.
Intervention group and HAPI prevention strategies
Every patient received a pressure redistribution cushion and pressure care education that was more intensive than the usual care pressure education. On admission, the patient’s level of skin injury risk was determined by the Waterlow Risk Assessment (WRA)23, with additional consideration of any patient comorbidity. For the purpose of this study, the risk levels were classified as: not at risk, at risk or high risk. This stratification determined which pressure redistribution cushion was required to meet the patient’s needs (Figure 1). On admission to the ward, the nursing team completed the WRA, identified the level of risk, and provided the pressure education; the occupational therapist provided the appropriate cushion.
Patients identified with a WRA score of <10 were classified as not at risk. These patients were provided with the Zenith Hosplex Cushion utilised in a previous Australian study (GMS supplier)20. This low-risk flat cushion was utilised for its basic pressure redistribution property of envelopment as a preventative cushion. Patients that scored 10–14 on the WRA were considered to be at risk of HAPI and were provided with a contoured foam pressure redistribution cushion (Dynatek Owl). This cushion was also provided to patients that had a Stage I or Stage II pressure injury along with a referral to the occupational therapist.
Patients within the high risk category (15+ on the WRA) were also provided with a contoured foam pressure redistribution cushion (Dynatek Owl) and were seen by the occupational therapist. Patients that had an existing full thickness pressure injury were provided with an alternative pressure redistribution cushion such as an air floatation cushion (ROHO). If high risk patients were admitted to the ward after hours or over the weekend with a full thickness pressure injury, and it was deemed essential for them to sit out of bed, a Jay Fusion cushion (a mixture of foam and gel) was made available. These patients were re-referred to the occupational therapist for a further comprehensive seating assessment to identify which cushion was best suited to ensure patient safety and best positioning in the chair. For high risk patients, clearance to sit out of bed and sitting regimes were determined by the multidisciplinary and medical teams in collaboration with the wound management team.
All cushions for patients in the intervention group were placed on hospital high back chairs. Patients who required recliners or specialised wheelchairs were seen by the occupational therapist and set up with an appropriate seat surface with an alternative pressure redistribution cushion.
Staff and patient HAPI enhanced education
Prior to the intervention period commencing, additional education sessions were held with ward nursing staff detailing how HAPI develop, avoidance strategies, patient education required, the WRA and reviewing pressure redistribution cushion use. Education was provided to nursing staff about safe sitting principles and measuring and adjusting the height of the chair to suit the individual patient. This was to reduce the risk of sliding, friction and falls while increasing comfort. A nurse champion was identified on the ward to support staff and reinforce the intervention. A flow chart was created to enable ward staff to identify the correct pressure cushion to issue to each patient (Figure 1).
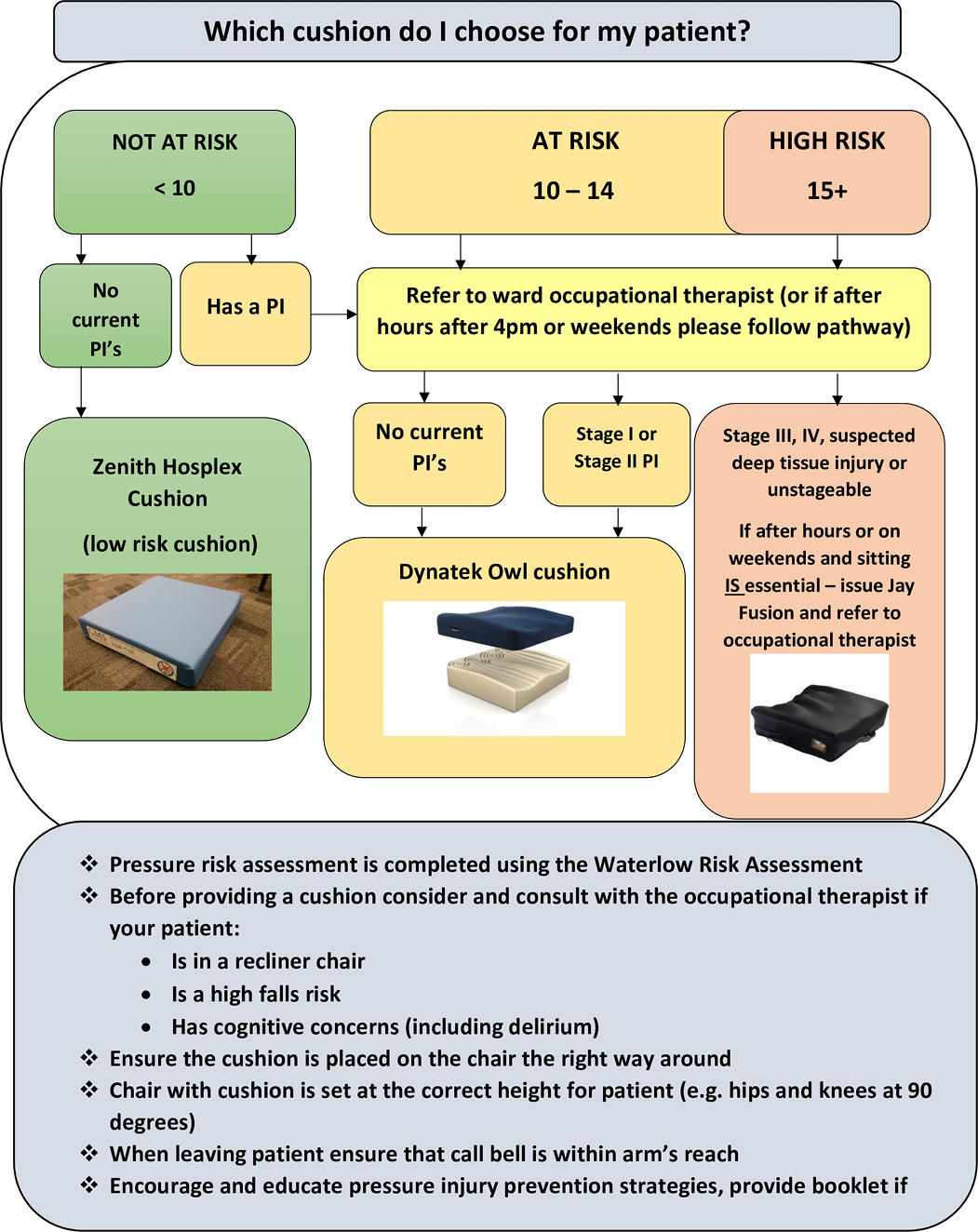
Figure 1. Intervention prescription for pressure redistribution cushion flow chart
In addition to usual care, all patients admitted to the ward within the intervention group received a pressure injury prevention 20-page booklet upon admission. Nursing and occupational therapy staff encouraged patients to review the education. This was left at the bedside to promote regular access. Patients were encouraged to avoid developing HAPI through regular movement and offloading pressure and by reducing time spent in bed. This also included additional information on the importance of diet, nutrition and skin care.
Control group
The control group received usual care following hospital guidelines for pressure injury management. All hospital inpatients received the following pressure injury prevention strategies – skin inspection within 8 hours of hospital admission and WRA on admission and throughout their care as per hospital nursing practice guidelines. However, patients did not routinely have pressure redistribution cushions or height adjusted high back chair to utilise when sitting out of bed; all patients could be referred to the ward occupational therapist if the patient required a pressure redistribution cushion (i.e. Duogels or Dynatek Owl), as per usual practice. Normal hospital policy continued for provision of support surfaces for beds, whereby patients scoring >10 on the WRA would be moved onto an appropriate air mattress. Patients deemed at lower risk (<10 on the WRA) would be provided a standard foam mattress. Information was not collected on the types of air mattresses used on each patient nor bed positioning as the standard hospital policy was followed for this. Patients did have access to a short brochure in the bedspace on pressure injury prevention strategies.
Outcome variables and data sources
A purpose designed audit sheet was developed to record study data on a daily basis. Data were collected from both medical and nursing records and face to face patient interviews. Patient information collected included general demographics, hospital length of stay (LOS), admitting diagnosis and co-morbidities. The WRA score was monitored throughout the patient’s admission. Any current wounds or pressure injuries (including stage) that were present on admission or that were HAPI were noted. Additional data collected included the type of chair a patient was utilising, the pressure cushion provided, if referral to an occupational therapist was required, and the patient’s mobility status.
A patient questionnaire including open and closed questions was utilised to collect patient feedback from a sample of patients who agreed to participate. A supporting research occupational therapist took between 10–15 minutes to complete the questionnaire with the patient. This was completed on either Day 2 or 3 of their admission. Patients were asked questions related to how much knowledge they had about pressure injury prevention, their engagement in pressure injury prevention education while in hospital (i.e. had they accessed and read the education provided [Yes/No]), comfort levels when sitting out of bed on the hospital high back chair (interval scale), how long they were able to sit for (interval scale), how many times a day they would sit out of bed (interval scale), and if they experienced pain when sitting [Yes/No]. Patients were blinded to group allocation.
Control group data were collected for an 8-week period. This was followed by a 2-week implementation and training period before data were collected for the intervention group for a further 8 weeks during the intervention phase. This quality improvement project has been described according to the Revised Standards for Quality Improvement Reporting Excellence (SQUIRE 2.0) guidelines24.
Statistical analysis
Descriptive summaries including patient age, hospital LOS and WRA score were reported as mean (standard deviation [SD]) or median (range), depending on the nature and distribution of the data and normality of distribution. Group comparisons for age and hospital LOS were compared via Mann-Whitney U tests. Group comparisons for gender, admitting diagnosis, comorbidities and HAPI were completed using chi-squared or Fisher’s exact tests, as appropriate, for categorical data and one-way ANOVA for continuous data. Group comparison of WRA score and patient-reported outcomes were analysed using univariate analysis with independent t-tests for continuous variables and chi-squared or Fisher’s exact test for non-continuous variables. p values of <0.05 were considered statistically significant. Statistical analysis was conducted using IBM SPSS version 26.0 (Armonk, NY).
Ethical considerations
This project was deemed to be of negligible risk and was exempt from review by the Sir Charles Gairdner Osborne Park Health Care Group Human Research Ethics Committee. Quality improvement approval was provided (QA33952).
Results
Enrolment and baseline characteristics
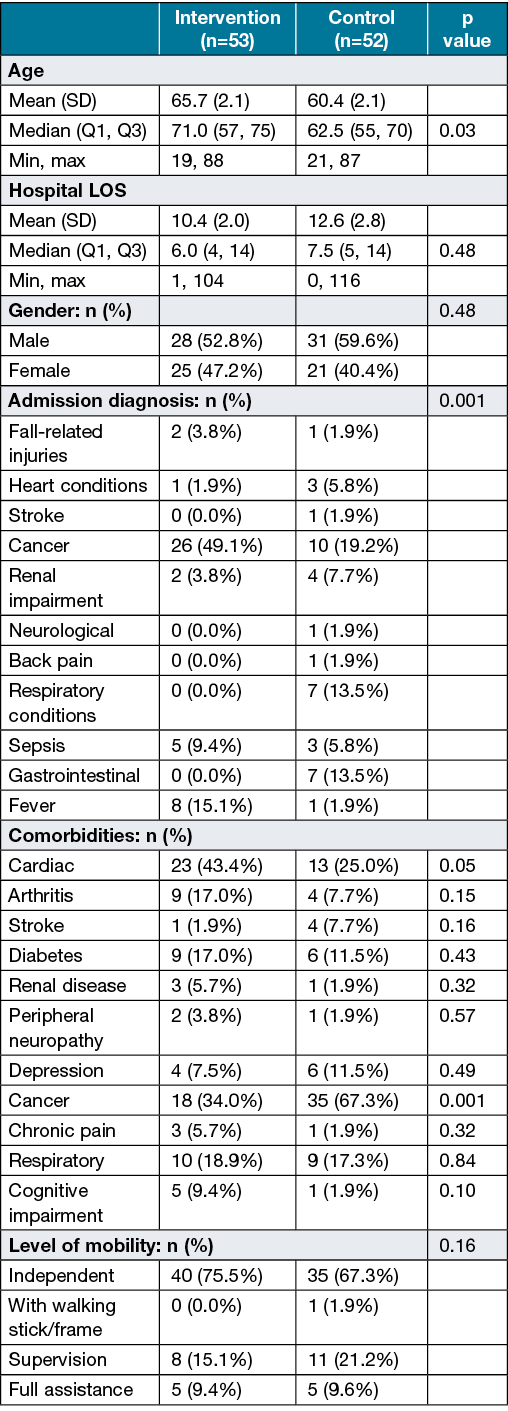
A total of 105 patients were recruited – 53 patients in the intervention group and 52 in the control group (Figure 2). The median age was 71.0 years in the control group and 62.5 years in the intervention group (p=0.03) (Table 1). Admitting diagnoses for patients enrolled in the study included cancer-related complications, respiratory and cardiac issues, along with musculoskeletal pain. A high number of patients admitted to the ward had a diagnosis of cancer and were often admitted with sepsis. Comorbidities found in both groups included arthritis, diabetes, cardiac diseases, cancer, respiratory diseases, depression and peripheral neuropathy (Table 1). The level of mobility between the two groups did not differ significantly (p=0.16), with 75.5% independently mobile in the intervention group compared to 67.3% in the control group. The median LOS was 6 days in the intervention group and 7.5 days in the control group (p=0.48). For patients that had a HAPI, the median LOS was not significantly different at 14 days compared to 10 days in patients that did not have a HAPI (p=0.60).
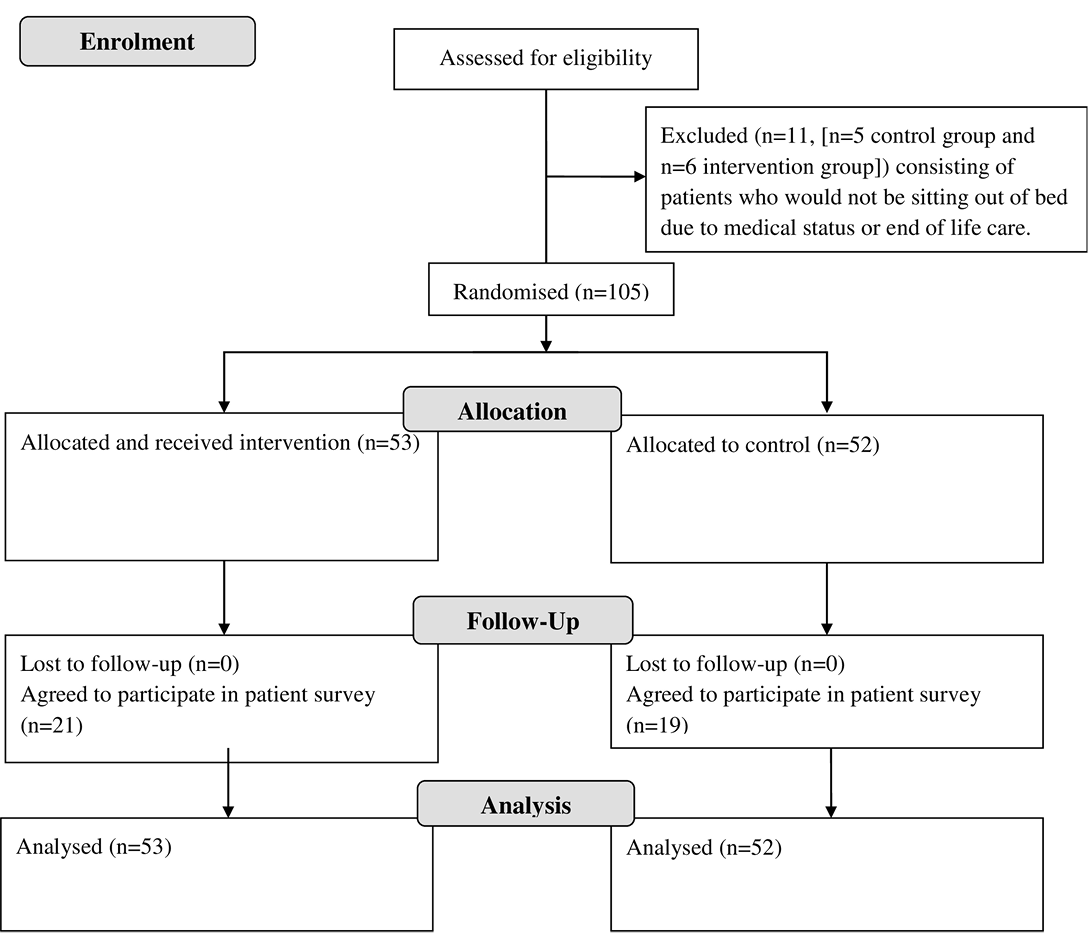
Figure 2. Consort flow chart of recruitment through to analysis
Table 1. Participant demographic information
Pressure risk and injuries
The mean (SD) WRA score on admission was significantly higher in the intervention group at 13.8 (8.3) compared to 11 (5.3) in the control group (p=0.05), indicating that the majority of patients were at risk of developing HAPI (Table 2). The number of patients per the WRA sub-categories did not significantly differ (p=0.25) between the control and intervention groups (Table 2), indicating that the groups were likely similar at baseline for risk of developing HAPI. The type of cushions provided are identified in Table 2.
Table 2: Pressure risk indicators, injuries sustained and pressure redistribution cushions supplied
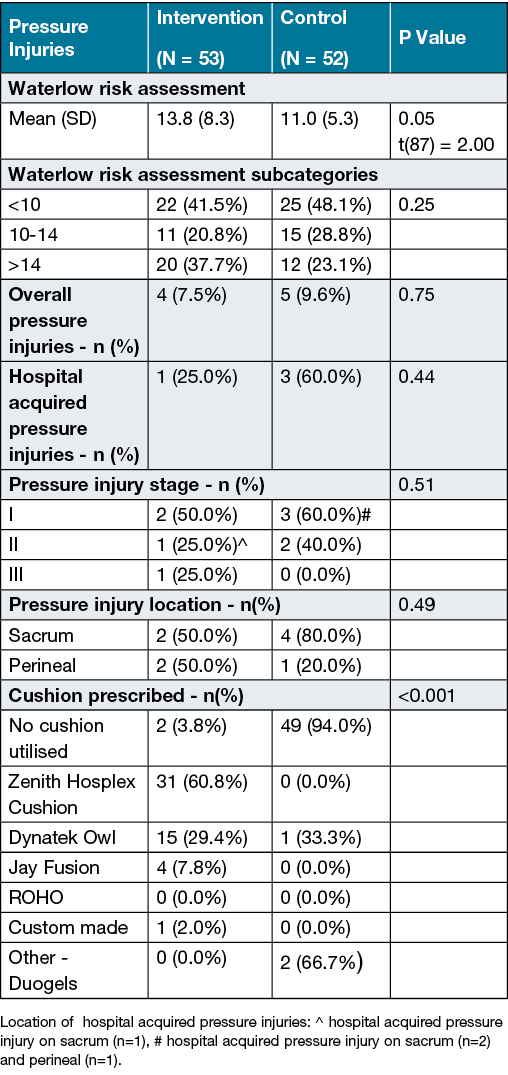
Nine (8.6%, 9/105) pressure injuries were identified during the study period (Table 2) which commenced in November 2019 (control n=5/52 vs intervention n=4/53). There was no significant difference between the groups, with 60% of pressure injuries in the control group being HAPI (n=3) compared to 25.0% in the intervention group (n=1) (p=0.44). Five males had a pressure injury (three of which were HAPI) compared to four females (one was HAPI).
In the control group, three Stage I pressure injuries were identified on sacral (n=2) and perineal areas (n=1), all three being HAPI (Table 2). There were two Stage II sacral pressure injuries identified which were present on admission. The intervention group had two Stage I pressure injuries, one located on the perineal area and the other on the sacrum, both of which were present on admission. One Stage II HAPI was identified on the sacrum; one Stage III perineal pressure injury was also identified on one patient at admission. Overall, pressure injury areas included the sacrum and perineum, which therefore need to be considered in seating.
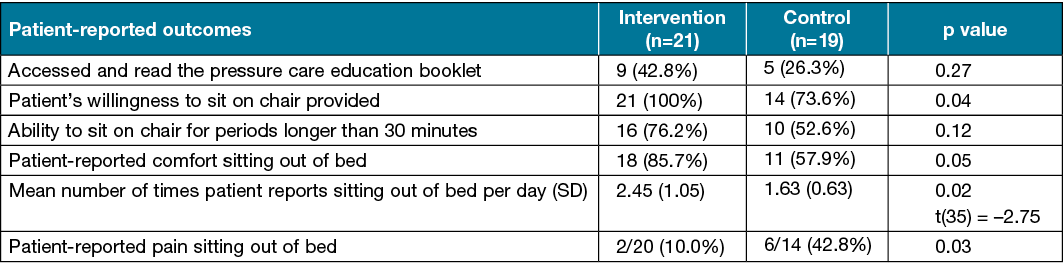
Patient questionnaire
A total of 19 patients in the control group and 21 in the intervention group agreed to provide additional feedback through the patient questionnaire. Patients in the intervention group were able to tolerate sitting out of bed for longer periods, sat out of bed more regularly throughout the day, and reported less pain when sitting out of bed (Table 3). Relative to the control group, the intervention group reported a 17.0% increase in accessing and reading the provided education material. The proportion of patients willing to sit out of bed increased significantly from 74.0–100% (p=0.04). Patient-reported comfort increased significantly by 30.0% (p=0.05), with associated pain also significantly reducing when sitting by 33.0% (p=0.03). Additionally, patients reported sitting out of bed significantly more often (p=0.02).
Qualitative feedback from patients in the control group included comments on the support the high back chairs provided (without a pressure cushion). Patients noted a lack of head support, they were uncomfortable or that the seat surface was “too hard” and that they “would rather sit on a pillow”. Additionally, one patient commented that it was hard to reposition on the high back chair surface. In the intervention group patients commented that the seating was comfortable, reduced their pain, was “soft yet firm” and provided “good pressure relief”. However, one patient reported that, by adding the pressure cushion onto the seat base, this altered the position of the lumber support in the backrest of the high back chair, resulting in decreased comfort.
Discussion
This study aimed to reduce HAPI through the provision of individually prescribed pressure redistribution cushions for all patients and by ensuring consistent and thorough patient and staff education. It involved a combined occupational therapy and nursing team approach. No significant differences were found between the two groups for the development of HAPI (Table 2). However, significant improvements in patient-reported outcomes included increased comfort, reduced pain and increased time sitting out of bed, indicating that the intervention requires further exploration (Table 3).
Table 3. Patient-reported outcomes through completion of questionnaire
Other research has implemented HAPI prevention care bundles including staff training and patient education utilising posters, brochures and educational videos25–27. Deakin et al.9 provide an education intervention care bundle to improve pressure injury prevention knowledge. This significantly increases a patient’s participation in pressure management strategies9. Likewise, we found that encouragement from nursing and occupational therapy staff was required to support patient engagement in pressure prevention. As part of our usual practice patients do have access to a short pressure care brochure in their bedspace; however, over 70% of patients did not access this as indicated in the questionnaire results. This continues to reinforce the importance of interactive, regular and engaging education to enhance a patient’s participation in their hospital care, with measures put in place to support sustainability throughout a patient’s admission.
During our study overall, four patients developed either Stage I or II HAPI, which are reportedly the most common among hospitalised patients8. Sitting out of bed is regularly encouraged in patients to reduce functional decline. It can improve musculoskeletal strength, lung and heart health, and circulation28. Hirsch29 and Graf30 identified that functional decline can start within 2 days of hospitalisation and impacts upon the level of independence required to complete daily activities31. Sitting for long periods or sitting in inappropriate seating can also increase a patient’s risk of developing HAPI13. Healthcare providers need to take action to prevent superficial tissue damage from occurring or worsening8, and patient seating needs to be considered as part of this approach.
McCarthy et al.11 found that, on average, older patients sat out of bed for 3.8 hours over an 8.5‑hour audit period in a post-acute setting, with participants sitting out of bed for a mean time of 1 hour 5 minutes. In our study we did not observe or track the amount of time patients were sitting out of bed; however, patients were asked to self-report. The study could be enhanced in future research by accurate measurement of time spent sitting out of bed through observation or activity monitors. Patients in our study were sitting out of bed on average 2.2 times per day in an acute care hospital setting, suggesting that they spend sufficient time sitting in chairs to be at risk of developing HAPI11.
Five of the patients in this study presented to hospital with existing pressure injuries, highlighting the need for strategies to support healing in the hospital setting and need for patient education (Table 2). Many factors contribute to the healing phase of a pressure injury; however, if the interface pressure on a seat surface is lessened, it is likely we can support wound healing32,33. The importance of patient and carer education and consideration of equipment for patient use at home is also required to support discharge; these patients could also be identified through outpatient settings.
It is important to note that the type of chair and cushion can influence both comfort and HAPI risk34. A range of high back chairs are used in the hospital setting. Individual prescription and setup of a bedside chair and pressure redistribution cushion is required to maximise opportunities to relieve pressure during admission.
Limitations
This study may have been strengthened by having a matched control group; however, this was not possible due to the resources available. Data were collected from a single hospital ward, impacting on the ability to generalise the findings. Different clinicians were involved in prescribing the cushions, adjusting the bedside chair set-up and supporting patient education. This may have impacted on the fidelity of the intervention; however, this was addressed through strategies such as initial group and individual staff training and a nurse champion to support the intervention at a ward level.
As previously identified, the measurement accuracy of the amount of time patients sat out of bed could be enhanced by observation or activity monitors. Future studies should consider a longer data collection period on different inpatient wards to determine if the intervention can impact on HAPI and if hospital-wide implementation would be beneficial.
Conclusion
Routine use of pressure redistribution cushions and enhanced education should be considered in the overall management of patients’ HAPI risk in the acute hospital setting. Although this study did not significantly reduce HAPI in the intervention group, there were significant improvements in patient-reported outcomes, including increased comfort, reduced pain and increased time spent sitting out of bed.
Acknowledgements
Thank you to occupational therapy and nursing ward staff and the wound management team for supporting this project. The authors would like to acknowledge Hannah Flynne and Lucy Bartlett for assistance with participant recruitment and data collection, Taylor Wright for undertaking a nurse champion role and Anita House for supporting study set up.
Conflict of interest
The authors declare no conflicts of interest.
Funding
This work was supported by the Charlies Foundation for Research. The funding source had no role in the design, completion or interpretation of the research.
Author(s)
Sascha Holbrook BSc (OT) BBA (Business Administration)
Colleen O’Brien-Malone B.App Sc. (OT)
Annette Barton B.App Sc. (OT), Grad Dip (AppSc), Masters (AppSc)
Kristie Harper* PhD, BSc (OT), PGCertHlthSc (OT)
Email Kristie.Harper@health.wa.gov.au
Occupational Therapy Department, Sir Charles Gairdner Hospital, Perth, WA, Australia
* Corresponding author
References
- Nguyen KH, Chaboyer W, Whitty JA. Pressure injury in Australian public hospitals: a cost-of-illness study. Aust Health Rev 2015;39(3):329–36.
- Australian Commission on Safety and Quality in Health Care (ACSQHC). National safety and quality health service standards [Internet]. 2nd ed. Sydney (NSW): ACSQHC; 2017. Available from: https://www.safetyandquality.gov.au/sites/default/files/migrated/National-Safety-and-Quality-Health-Service-Standards-second-edition.pdf
- Norman RE, Gibb M, Dyer A, et al. Improved wound management at lower cost: a sensible goal for Australia. Int Wound J 2016;13(3):303–16.
- Australian Commission on Safety and Quality in Health Care (ACSQHC). Preventing and managing pressure injuries [Internet]. Sydney (NSW): ACSQHC; 2020. Available from: https://www.safetyandquality.gov.au/sites/default/files/2020-10/fact_sheet_-_preventing_pressure_injuries_and_wound_management_oct_2020.pdf
- Cherry C, Moss J. Best practices for preventing hospital-acquired pressure injuries in surgical patients. Can Oper Room Nurs J 2011;29(1):6–8, 22–6.
- Australian Commission on Safety and Quality in Health Care (ACSQHC). Hospital acquired complication: pressure injury [Internet]. Sydney (NSW): ACSQHC; 2018. Available from: https://www.safetyandquality.gov.au/sites/default/files/2019-05/saq7730_hac_factsheet_pressureinjury_longv2.pdf
- Team V, Tuck M, Reeves J, et al. Pressure injury data in Australian acute care settings: a comparison of three datasets. Int Wound J 2020;17:578–86.
- Li Z, Lin F, Thalib L, Chaboyer W. Global prevalence and incidence of pressure injuries in hospitalised adult patients: a systematic review and meta-analysis. Int J Nurs Stud 2020;105:103546.
- Deakin J, Gillespie BM, Chaboyer W, Nieuwenhoven P, Latimer S. An education intervention care bundle to improve hospitalised patients’ pressure injury prevention knowledge: a before and after study. Wound Prac Res 2020;28(4):154–62.
- Coleman S, Gorecki C, Nelson EA, et al. Patient risk factors for pressure ulcer development: systematic review. Int J Nurs Stud 2013;50(7):974–1003.
- McCarthy A, Robertson V, Roberts K, Lannin NA. Audit of sitting time in older inpatients and implications for pressure-injury management. Phys Occup Ther Geriatr 2019;37(3):183–95.
- Surkan MJ, Gibson W. Interventions to mobilize elderly patients and reduce length of hospital stay. Can J Cardiol 2018;34(7):881–8.
- European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and treatment of pressure injuries/ulcers: clinical practice guideline. The international guideline. E Haesler, editor. EPUAP/NPIAP/PPPIA: 2019.
- Meaume S, Marty M, Colin D. Prospective observational study of single or multi compartment pressure ulcer prevention cushions: PRESCAROH project. J Wound Care 2017;26(9):537–44.
- Chou R, Dana T, Bougatsos C, et al. Pressure ulcer risk assessment and prevention. Ann Intern Med 2013;159(1):28–38.
- Moore Z, Van Etten M. Ten top tips: seating and pressure ulcer prevention. Int Wound J 2015;6:11–6.
- Moore Z, Van Etten M. Preventing pressure damage when seated. Wounds UK 2015;11(3):18–23.
- Gil-Agudo A, De la Peña-González A, Del Ama-Espinosa A, Pérez-Rizo E, Díaz-Domínguez E, Sánchez-Ramos A. Comparative study of pressure distribution at the user-cushion interface with different cushions in a population with spinal cord injury. Clin Biomech 2009;24(7):558–63.
- Collins F. The contribution made by an armchair with integral pressure-reducing cushion in the prevention of pressure sore incidence in the elderly, acutely ill patient. J Tissue Viability 1999;9(4):133–7.
- Victoria State Government. Pressure care case study – St Vincent’s Hospital Melbourne [Internet]. Melbourne (VIC): Victoria State Government; Available from: https://www2.health.vic.gov.au/hospitals-and-health-services/patient-care/older-people/resources/implementation/case-study-pressure-care
- Brienza D, Kelsey S, Karg P, et al. A randomized clinical trial on preventing pressure ulcers with wheelchair seat cushions. J Am Geriatr Soc 2010;58(12):2308–14.
- Mervis JS, Phillips TJ. Pressure ulcers: prevention and management. J Am Acad Dermatol 2019;81(4):893–902.
- Waterlow J. The Waterlow Pressure Sore Risk Assessment Tool [Internet]. Taunton (TA): 1985 [updated 2005]. Available from: www.judy-waterlow.co.uk
- Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. Standards for quality improvement reporting excellence 2.0: revised publication guidelines from a detailed consensus process. J Surg Res 2016;200(2):676–82.
- Soban LM, Hempel S, Munjas BA, Miles J, Rubenstein LV. Preventing pressure ulcers in hospitals: a systematic review of nurse-focused quality improvement interventions. J Jt Comm J Qual Patient Saf 2011;37(6):245.
- Chaboyer W, Bucknall T, Webster J, et al. INTroducing A Care bundle To prevent pressure injury (INTACT) in at-risk patients: a protocol for a cluster randomised trial. Int J Nurs Stud 2015;52(11):1659–68.
- van Gaal BGI, Schoonhoven L, Mintjes JAJ, et al. Fewer adverse events as a result of the SAFE or SORRY? programme in hospitals and nursing homes. Part I: Primary outcome of a cluster randomised trial. Int J Nurs Stud 2011;48(9):1040–8.
- Corcoran PJ. Use it or lose it: the hazards of bed rest and inactivity. West J Med 1991;154(5):536–8.
- Hirsch CH, Sommers L, Olsen A, Mullen L, Winograd CH. The natural history of functional morbidity in hospitalized older patients. J Am Geriatr Soc 1990;38(12):1296–303.
- Graf C. Functional decline in hospitalized older adults: it’s often a consequence of hospitalization, but it doesn’t have to be. Am J Nurs 2006;106(1).
- Hoogerduijn JG, Schuurmans MJ, Duijnstee MS, de Rooij SE, Grypdonck MF. A systematic review of predictors and screening instruments to identify older hospitalized patients at risk for functional decline. J Clin Nurs 2007;16(1):46–57.
- Sprigle S, Sonenblum S. Assessing evidence supporting redistribution of pressure for pressure ulcer prevention: a review. J Rehabil Res Dev 2011;48(3):203–13.
- Brienza DM, Karg PE, Geyer MJ, Kelsey S, Trefler E. The relationship between pressure ulcer incidence and buttock-seat cushion interface pressure in at-risk elderly wheelchair users. Arch Phys Med Rehabil 2001;82(4):529–33.
- Defloor T, Grypdonck MH. Sitting posture and prevention of pressure ulcers. Appl Nurs Res 1999;12(3):136–42.



