Volume 29 Number 4
A new district nursing model improves venous leg ulcer healing rates
Alice Bourke and Natalie Scott
Keywords community nursing, compression therapy, leg ulcers, Doppler assessment, healing rates
For referencing Bourke A and Scott N. A new district nursing model improves venous leg ulcer healing rates. Wound Practice and Research 2021; 29(4):206-210.
DOI
https://doi.org/10.33235/wpr.29.4.206-210
Submitted 2 August 2021
Accepted 23 September 2021
Abstract
Background The predominant aetiology of lower leg ulcers (VLU) are caused by venous insufficiency. In 2016 a new district nursing model was introduced using nurses specialising in leg ulcer assessment and management. The specialist nurses provided district nurse education on leg ulcers and conducted vascular assessments to identify venous ulcer aetiology, enabling early compression therapy to increase healing rates and prevent wound chronicity.
Method A retrospective electronic chart audit was conducted to determine if the new model diagnosed and treated VLUs earlier. All newly presenting lower leg wounds entering the service over a period of 7 months were reviewed, with healing rates studied up to 24 weeks.
Results Healing rates of all lower leg wounds were 84% with an average heal time of 9.7 weeks. The time to heal for recurrent ulcers was the same as new wound presentations. Of interest, Māori and Pacific Island (Pasifika) patients ulcerated at a younger age compared to European patients.
Conclusion A nurse-led model facilitated early diagnosis and treatment of VLUs to reduce healing time. The correlation of Māori and Pasifika patients presenting younger with leg ulcers necessitates further research to determine if there is an ethnicity causation factor in these populations.
Introduction
A venous leg ulcer (VLU) is defined as an open skin lesion affecting the leg or foot that is affected by venous hypertension; these ulcers account for 70% of all lower leg ulcers1. VLUs have high recurrence rates and can lead onto chronic wounds if not managed appropriately; hence early identification to treat and prevent these is essential for a person’s quality of life, and to reduce the financial burden on the person and healthcare system1,2. VLU prevalence rates increase with ageing2–4 and, in the older person, age-associated changes can lead onto chronic wounds5.
The Capital Coast District Health Board (CCDHB) serves an estimated population of 324,000 in the lower half of the North Island in New Zealand. CCDHB projects a 33% population growth in the 70–79 age group, and a 59% growth in the 80+ age group by 20306; VLU rates would be expected to increase with our ageing population. A large proportion of the CCDHB district nursing service workload is managing lower leg wounds, with referrals received from general practices, hospitals and aged care facilities. This is supported by research results from the United Kingdom (UK) where wound care is estimated to consume up to 65% of community nurses’ time and specialist wound services have shown to increase VLU healing rates4. An Australian cross-sectional survey reported that the most common chronic wound seen in general practice were leg ulcers7. This survey also reported that practice nurses manage leg ulcers for up to 3 months and, if failed to heal, would then refer to a vascular surgeon or specialist wound clinic7. A New Zealand observational study found community patients with leg ulcers referred to an outpatient vascular department had low rates of ankle–brachial pressure index (ABPI) measurements performed and use of compression therapy8.
Background
A previous 52-week retrospective audit involving 288 patients enrolled with the district nursing service from May 2015 to May 2016 showed VLUs had an average heal time of 27 weeks. Additionally, recurrent ulcers took 45 weeks to heal which was 1.7 times longer than new ulcer presentations. This audit included all lower leg wounds, both new referrals and patients with existing wounds. To benchmark these results we used the UK healing targets for VLUs as follows; 100% of simple leg ulcers should be healed by 12 weeks (or minimum ≥70% healed within 18 weeks), and 100% complex leg ulcers healed within 18 weeks (or minimum ≥70% healed within 24 weeks)4,9. This audit indicated our healing rates were longer than the UK targets and required a concerted effort to improve.
Education
Previous to this audit the wound clinical nurse specialist (WCNS) had identified the need for early VLU diagnosis and treatment and submitted a successful proposal to the CCDHB for a specialist wound care team (SWCT) in March 2016. The team consisted of the WCNS who supported the education and training for the five part-time appointed SWCT members in lower leg vascular assessment over a period of 2 years as each nurse commenced the role. Investment in Doppler equipment and wound measurement and data collection for each base was implemented. Following the ANZ guideline for identification and management of VLUs2 a comprehensive leg ulcer assessment form was developed which included clinical, pain and leg ulcer history, examining the legs for venous and arterial indicators, CEAP classification, wound and skin assessment, and ABPI to support diagnosis1,2,4. The SWCT then implemented a VLU training program for 70 district nurses; Doppler assessment was included for approximately 20 of the district nurses with practice supported by the SWCT.
Clinical practice
In accordance with the ANZ guideline and CCDHB protocol, all non-healing lower leg wounds, or patients who had an ABPI reading below 0.8 or above 1.2, were referred onto the specialist vascular team2. Patients diagnosed with a VLU (ABPI 0.8–1.2) received compression bandaging. Patients with arterial calcification (ABPI>1.3) had toe–brachial pressures (TBPI) performed and the findings discussed with a vascular surgeon to determine if compression therapy could be commenced. Compression therapy included Coban 2, Coban 2 Lite10, compression hosiery ulcer kits, and Juxta Lite, an adjustable inelastic compression wrap11. As supported in the literature, to help reduce ulcer recurrence rates patients received one pair of compression hosiery funded by the CCDHB1,2,4. For patients in financial difficulty income assistance was sought to assist with ongoing hosiery costs.
All patients received written information sheets on the importance of skin care and compression hosiery post-healing12,13. The service implementation of ‘Silhouette’, a wound capture, measurement and data system, has played a significant role in enabling the nurses to monitor the leg ulcer trajectory with precise wound measurement and tracking, informing healing or non-healing trends and enabling early referral to specialists if wound closure was not progressing14.
Audit objectives
The primary objective was to determine if newly referred patients with lower leg wounds received early diagnosis and treatment. The secondary aim was to determine VLU healing rates using compression therapy.
Inclusion criteria
- New patients referred to the community service and over 18 years of age.
- Patients consenting to standard electronic leg ulcer data being captured by the district nurse.
- Patients who had received a comprehensive leg ulcer assessment and were in compression therapy.
Exclusion criteria
- Other lower leg wounds that were not of venous aetiology such as arterial leg ulcers, diabetic foot ulcers, and cancerous lesions.
Method
A retrospective audit was registered and approved by the CCDHB and conducted from 1 October 2017 to 30 April 2018; no additional funding was provided for this audit. As standard practice at CCDHB, an existing district nurse database was utilised to collect patient data. Data were captured by the district nurse or SWCT who conducted the assessment in the patient’s home or district nurse clinic.
All lower leg wounds were identified by the use of standard statistical coding used by the district nursing service. As standard practice, informed written consent was required for wounds to be assessed and measured using Silhouette™, an electronic 3D wound-imaging tool. Patient healing rates were analysed up to 25 weeks from service entry.
Data were analysed using SPSS Statistics 25.0. Categorical variables were expressed as frequencies and proportions. Time to Doppler assessment and time to heal were analysed with mean averages and standard deviation provided. The relationship between time to Doppler and time to heal was analysed with the non-parametric Spearman’s Rho test. Continuous variables were analysed by means of the analysis of variance (ANOVA) and independent student’s t test.
Results
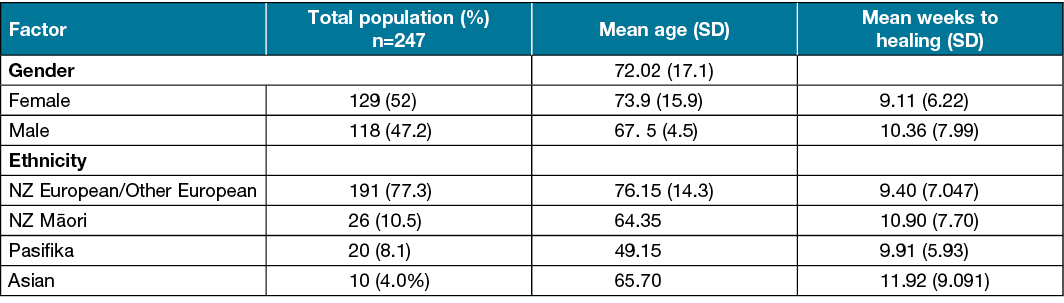
Over the 7-month audit period seven patients died; data from these patients was included in the overall analysis. A total of 247 new patients’ referrals with lower limb wounds were received during this period – the average patient age was 72 years, the mean male age was 67.5 versus female 73.9 (Table 1). The mean age of Pasifika was significantly lower at 49.15 and NZ Māori at 64.35 compared to European (Table 1).
A one-way between groups analysis of variance was conducted to explore the differences in ethnicity and age which showed a significant difference in age differences between European versus NZ Māori and Pasifika (p<0.05). The results indicate that Māori and Pasifika presented with leg ulcers at a much younger age compared to Europeans. There was no significant difference in time to heal and ethnicity.
Table 1. Age vs heal time and ethnicity data
Doppler assessment
A total of 134 (54%) patients were assessed as requiring a Doppler/vascular assessment. The time for a Doppler across the service was an average of 3.94 weeks from date of referral. This is well within the current CCDHB Lower Limb Protocol of 6 weeks from date of referral. Not all patients would be expected to have a Doppler assessment if they had received a previous Doppler within 12 months prior to the new referral. In addition, some patients with lower leg ulcers were unable to have a Doppler performed, such as those patients who were at end of life, or those for whom a Doppler was too painful to perform or had an inability to lie flat. Specialist vascular referral was initiated for some of these patients based on the nurses’ clinical judgement regarding appropriateness of treatment.
Relationships between time to receive a Doppler and time to heal was investigated using the non-parametric Spearman’s Rho statistical test. Results showed a medium correlation between the two (r=0.190, n=111, p=0.046).
Aetiology of wounds
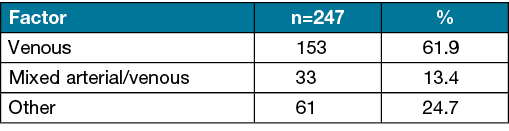
A total of 61.9% of all presenting lower leg wounds were of venous aetiology (Table 2). Other wound types included skin tears and lower leg cellulitis and included unrecorded data.
Table 2. Wound aetiology
Healing rates
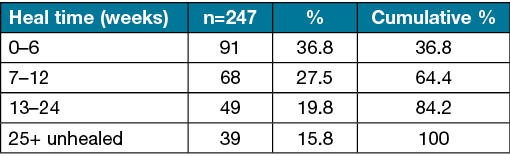
A total of 219 (89%) patients had healed wounds at the end point of data analysis; healing time ranged from less than 1 week to 43 weeks. An average heal time overall for the 219 patients was 9.70 weeks with SD 7.12. Figure 1 shows that the healing rates are reasonably well distributed over the 0–24 week time period, with only a few numbers of patients taking longer than 24 weeks to heal. For data analysis purposes, time for healing were then collated into ‘heal time’ categories (Figure 1 and Table 3); all wounds that did not heal in the 24-week period were collated with those non-healing in the 24+ time period.
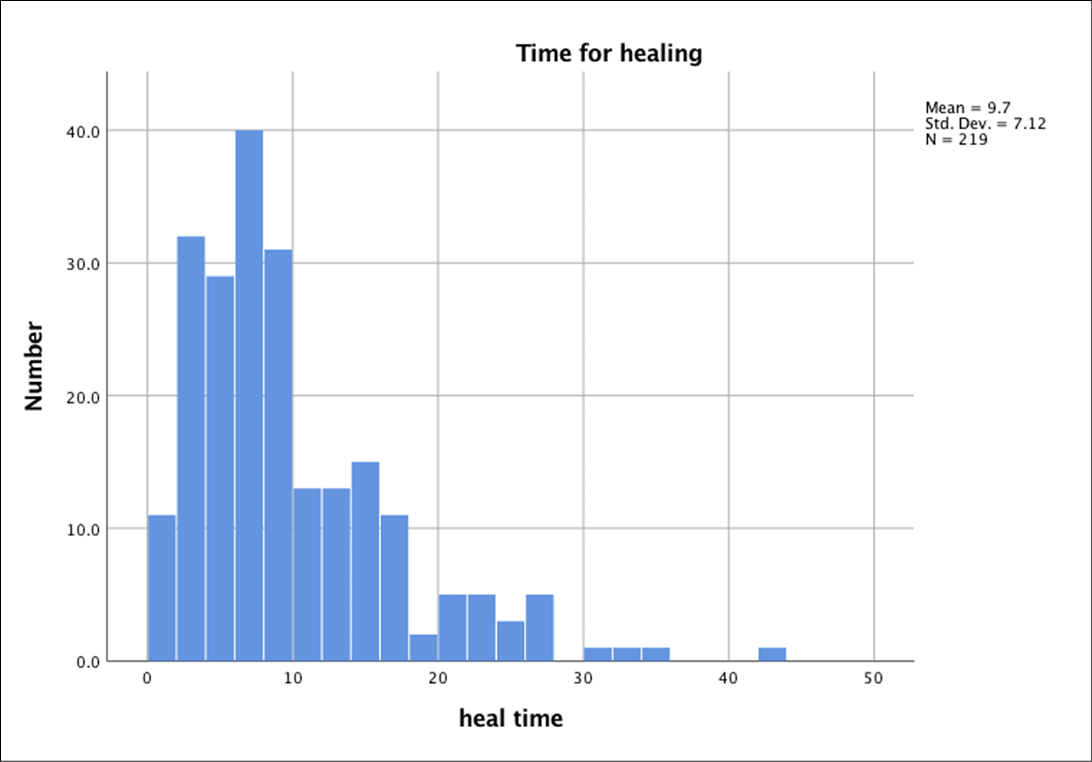
Figure 1. Healing time over weeks
Table 3. Heal time categories
Recurrence vs new leg ulcer rates
Of the 247 patients, 128 patients (51.8 %) presented with a recurrent ulcer and 55 (22.2%) presented with a new ulcer; 64 (25.9 %) patients had unrecorded data. The audit found healing time was faster for recurrent ulcers (9.98 weeks) compared to new presenting leg ulcers (11.5 weeks), although this was not significant (p=0.225).
Compression therapy
A total of 122 patients (49.4%) received compression therapy, 47.4% did not, with unknown data for 3.2 %. The average heal time for those in compression was 11.82 weeks (SD 7.42); this compared with an average heal time of 8.65 weeks (SD 6.73) for those not in compression. A t test showed no statistical difference between times to heal between those in compression versus those not in compression.
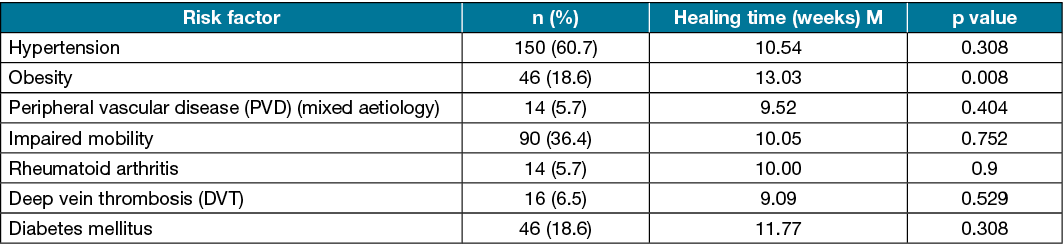
Risk factors
Risk factors were analysed in terms of percentages; hypertension at 60.7% and lower leg oedema at 63.2 % were the most presenting risk factors in our population (Table 4). An independent t test was conducted to compare risk factors and healing times; obesity was the only significant risk factor linked to a slower healing time (p=0.008).
Table 4. Risk factors vs healing time
Discussion
This audit provided data to compare with our previous audit. Results showed improved healing rates for all presenting wounds of 84% at 24 weeks, although a limitation is the first audit was conducted over 1 year and this audit was over 7 months and included new referrals only.
The audit relied on data retrieved from wound codes entered into medical records by the district nurses. The audit did not include the following factors: ulcer duration; if the ulcers were simple or complex; whether multiple ulcerations were present on the limbs of the same patient; and what type of compression systems were used. Of the 247 patients audited, just under 50% received compression therapy; this lower percentage may be attributed to patients already healing and hence were not referred on for further investigation. Patient preference may also have influenced the application of compression.
The average healing rate for VLUs using compression therapy was 11.82 weeks which is within the UK 12-week healing target for simple VLUs9. The differences in healing rates between those in compression and those not are likely due to non-complex wounds not requiring compression, hence there would have been a greater proportion healed in the first 4–6 weeks. This audit found similar healing rates of recurrent ulcers to new presenting ulcers; this may be attributed to earlier identification and treatment. Since recurrent VLUs could be considered more complex to heal, this finding is pleasing and highlights the need for ongoing education, skin care, and funding for compression hosiery post-healing to reduce this rate in this high-risk group1,2,4,9. Although a benefit analysis was not performed, healing wounds faster improves a person’s quality of life and is associated with reduced healthcare costs1,2.
Obesity as a risk factor of chronic venous insufficiency is well documented1,2; the link to slower healing times in our patient group was not explored further and hence it is unclear if this is related to other factors such as reduced mobility, other comorbidities, or concordance with compression.
The audit highlighted the prolonged referral process (up to 9 months) for patients outside 0.8–1.2 Doppler range and for non-healing wounds to be reviewed by the vascular service. Since this audit, a new initiative includes regular virtual meetings with the vascular surgeon and SWCT to determine if these patients can commence compression treatment earlier.
NZ Māori and Pasifika people have poorer health outcomes and die younger15, yet the impact of VLUs in these populations is not published2. This audit indicated, for Māori and more so for Pasifika, that they presented with leg ulcers at a younger age; further research is needed in determining potential ethnicity causation, and prevention and management strategies.
Conclusion
The audit data supports that our new nursing model did, in most cases, provide earlier leg ulcer assessment and diagnosis and did improve healing rates for new and recurrent leg ulcers, hence reducing the risk of chronic wounds developing. Auditing can provide insights into the population you serve, and the effectiveness of care and delivery. An educated and responsive team can provide early lower leg assessment and diagnosis and provide best practice treatment to improve leg ulcer healing rates in the community and reduce the burden on secondary and tertiary healthcare services.
Acknowledgements
Dr Lisa Woods, Victoria University; Capital Coast District Health Board Decision Support Unit; Capital Coast District Nursing Service; Mandy Pagan, wound clinical nurse, Specialist Southern District Health Board, Invercargill; Cathy Hammond, wound clinical nurse specialist, Nurse Maude Christchurch.
Conflict of interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
Author(s)
Alice Bourke*1 MNurs RN
Email alice.bourke@ccdhb.org.nz
Natalie Scott1 MNurs, RN Clinical Nurse Specialist
1Capital Coast District Health Board (CCDHB), Wellington, New Zealand
* Corresponding author
References
- O’Donnell TF, Passman MA, Marston WA, Ennis WJ, Dalsing M, Kistner RL, et al. Management of venous leg ulcers: clinical practice guidelines of the Society for Vascular Surgery® and the American Venous Forum. J Vasc Surg 2014;60(2):3S–59S.
- Australian Wound Management Association and the New Zealand Wound Care Society. Australian and New Zealand clinical practice guideline for prevention and management of venous leg ulcers. Wounds Australia; 2011. p. 136.
- Graham ID, Harrison MB, Nelson EA, Lorimer K, Fisher A. Prevalence of lower-limb ulceration: a systematic review of prevalence studies. Adv Skin Wound Care 2003;16(6):305–16.
- Harding K, Dowsett C, Fias L, Jelnes R. Simplifying venous leg ulcer management. Consensus recommendations. Wounds Int 2015. Available from: http://www.woundsinternational.com/
- Gould L, Abadir P, Brem H, et al. Chronic wound repair and healing in older adults: current status and future research. J Am Geriatr Soc 2015;63(3):427–438.
- Capital & Coast District Health Board. CCDHB Health System Plan 2030. Available from https://www.ccdhb.org.nz/news-publications/publications-and-consultation-documents/ccdhb-health-system-plan-2030.pdf
- Weller C. Evans S. Venous leg ulcer management in general practice. Practice nurses and evidence based guidelines. Aust Fam Physic 2012;41(5):331–7.
- Benoiton LA, Schmidt E, Tarr GP, Thomson IA, Rennie SC, van Rij AM. Assessment and management of leg ulcers in the community and an outpatient clinic. NZ Med J 2012;126(1368):24–34.
- Wounds UK. Guidelines for practice optimising venous leg ulcer services in a changing NHS: a UK consensus. Wounds UK 2013; Available from: www.wounds-uk.com
- Schuren J, Bernatchez SF, Tucker J, Schnobrich E, Parks PJ. 3M Coban 2 layer compression therapy: intelligent compression dynamics to suit different patient needs. Adv Wound Care 2012;1(6):255–8.
- Medi UK Ltd. A quick guide to the juxta range. 2017. Available from: https://www.mediuk.co.uk/fileadmin/Storage/Documents/UK/97D83_juxta_guide_UK_final.pdf
- Australian Wound Management Association and the New Zealand Wound Care Society. Treating venous leg ulcers. 2013. Available from: vlu_patient_info-managing-vlu-2013.pdf
- Australian Wound Management Association and the New Zealand Wound Care Society. Preventing venous leg ulcers. 2013. Available from: vlu_patient_info-preventing-vlu-2013.pdf
- Fletcher J. The use of electronic data capture devices in wound care settings. Wounds UK 2012;8(4):119–24.
- New Zealand Ministry of Health. Reducing inequalities in health. Ministry of Health; 2002. p. 1–53. Available from: https://www.health.govt.nz/system/files/documents/publications/reducineqal.pdf



