Volume 29 Number 4
The relationship between pressure injuries and dynamic buttock pressure distributions during performance in wheelchair basketball athletes
Tomonori Maeda, Nao Tamai, Takeo Minematsu, Hiroshi Noguchi, Koichi Yabunaka, Gojiro Nakagami, Mitsuso Neya and Hiromi Sanada
Keywords pressure injury, prevalence, disability, dynamic condition, pressure distribution
For referencing Maeda T et al. The relationship between pressure injuries and dynamic buttock pressure distributions during performance in wheelchair basketball athletes. Wound Practice and Research 2021; 29(4):211-218.
DOI
https://doi.org/10.33235/wpr.29.4.211-218
Submitted 31 May 2021
Accepted 3 September 2021
Abstract
Objectives Complex actions are thought to be risk factors for pressure injuries (PIs) in wheelchair basketball athletes. However, no study has been conducted on the characteristics of dynamic pressure distributions during performance. This study aimed to identify the characteristics of dynamic pressure distributions and to determine the parameters that relate to PIs in wheelchair basketball athletes.
Method This cross-sectional study was conducted in November 2017 at the training camp of the national team in Japan. The study participants were 14 elite wheelchair basketball athletes who had joined the training camp. A wound, ostomy and continence nurse (WOCN) and a sonographer evaluated the presence of PIs by inspection and ultrasonography. Pressure distributions under static and dynamic conditions were measured using sheet-type sensors.
Results Sixteen PIs were found in five (35.7%) of the 14 participants. Participants with PIs showed distribution of high pressure in unilateral/bilateral ischium and belting regions. In three participants who had PIs on the buttocks, total high-pressure periods were 60.25, 68.33 and 155.16 seconds, respectively. Maximum high-pressure periods were 12.10, 2.53 and 23.53 seconds. The numbers of high-pressure periods were 242, 190 and 706 times. Under dynamic conditions, these parameters were higher than those of participants without PIs.
Conclusions Our findings suggested that continuous and/or repetitive high-pressure loading was related to the occurrence of PIs during performance. Further prospective studies are required to establish the methods to predict and prevent PIs in wheelchair basketball athletes.
Introduction
Disabled sports are effective for improving the physical, mental and social conditions of people with disabilities1,2. However, participation in sports can also be a risk factor for several physical disorders such as joint pains and traumatic injuries3. Among these injuries, pressure injuries (PIs) have a serious impact because they lead not only to pain, discomfort, distress and deterioration of quality of life but also to systemic infection and mortality4–7. PIs occur more often in wheelchair sports than in other disabled sports because of long-term sitting during performance and complicated actions such as a sudden stops, dashes, quick turns and crashes8. Although studies on the prevalence of PIs in wheelchair sports are rare, an extremely high prevalence of 27.3–75% has been reported in men’s and women’s wheelchair basketball3,9,10. These surveys support the need for intensive intervention to prevent PIs in these athletes.
External forces trigger PIs. Several studies on PIs in elderly populations and patients with spinal cord injuries indicate that understanding the pressure distribution on the support surfaces is the primary step for PI prevention11,12. These studies measured and assessed pressure distributions under static conditions. In contrast, few studies of dynamic pressure distributions on the wheelchair seat are available. Most recently, Peters13 reported the characteristics of dynamic pressure distributions in wheelchair racers and revealed factors associated with peak pressure on the sports wheelchair under static conditions and pseudo performance conditions on a wheelchair treadmill. However, the characteristics of dynamic pressure distributions that accompany complex actions have not been studied during actual performance. Moreover, no study has been conducted to show the relationship between dynamic pressure distributions and PIs.
This study aimed to identify the characteristics of dynamic pressure distributions and to determine parameters that indicate PIs in wheelchair basketball athletes. This study is a first step to establish preventive care for PIs in these athletes.
Materials and methods
Outline
This cross-sectional study was conducted in November 2017 at the training camp of the Japanese men’s national wheelchair basketball team. Study participants were elite wheelchair basketball athletes who had joined the training camp. Athletes who were assessed as having a health condition and/or were deemed otherwise unsuitable to participate by the team staff were excluded from the study. After obtaining informed consent, researchers conducted body measurements and interviews. This study was approved by the research ethics committee of the Graduate School of Medicine, The University of Tokyo (No. 11765-(3)).
Skin assessment
A wound, ostomy and continence nurse (WOCN) evaluated the presence of PIs on the skin in contact with parts of the wheelchair and graded their severities according to the international pressure injury classification system14. Deep tissue injuries (DTIs) were identified by ultrasonographic examination (Noblus, Hitachi Aloka Medical, Tokyo, Japan)15. A sonographer took B‑mode images of bilateral ischial tuberosities using ultrasonographic diagnostic equipment with a linear-array (5–18MHz) transducer (Hitachi Aloka Medical). Gain and tissue depth for later quantitative image analysis were maintained at constant levels. A hypoechoic feature was considered as subcutaneous tissue damage15.
Demographic data
A researcher interviewed participants to collect information on age, height, cause and duration of disability, sensory disturbances, assistive devices for daily life, history of PIs, history of skin flaps, and career length in wheelchair basketball. Wheelchair cushions were examined, and body weight was measured using the original weighing system consisting of four load-cell sensors16. Triceps skinfold thickness and arm muscle circumference were measured by a caliper (Adipometer, Abbott Japan Co. Ltd., Japan) and the Insertape (Abbott Japan). Stratum corneum hydration and skin pH on ischial regions were measured three times by the Mobile Moisture (Courage + Khazaka Electronic GmbH, Cologne, Germany) and the Skin Check Portable pH Tester (Hanna Instruments, Woonsocket, RI, USA). The thickness of subcutaneous tissue, which is the distance from the skin surface to the ischial surface, was recorded using ultrasonography with a linear-array or curved linear-array (2–5MHz) transducer (Hitachi Aloka Medical) under pressure-loaded and unloaded conditions and measured three times using the ImageJ (National Institutes of Health, Bethesda, MD, USA). The averages of three measurements were used.
Pressure measurement
Pressure distributions on basketball wheelchairs under static conditions were measured using the CONFORMat (Nitta Corporation, Osaka, Japan). A 30-second pressure distribution was recorded at 10Hz in a stable sitting posture after calibration of the sensor.
Dynamic pressure distributions during motion and ball skill training were measured using the High Speed I-Scan system (Nitta Corporation). A sensor sheet was individually cut to adjust to the wheelchair seat of the participant, and a cotton sheet was attached on the surface of the sensor to prevent slipping during performance. Following calibration of sensors, dynamic pressure distributions were recorded at 15, 20, or 30Hz during performance. Simultaneously, the actions of the participants were recorded using a digital video camera (Sony Corporation, Tokyo, Japan).
Analysis method
In the analysis of both static and dynamic pressure distribution data, signals ≤5mmHg were excluded for noise cancelling. For smoothing of pressure distribution data, the average pressure of a neighbouring 2×2-pixel square was applied for each pixel. A frame showing the highest peak pressure in the smoothed data that average pressure of a neighbouring 2×2-pixel square was chosen as a representative among 30-second records under static pressure conditions. Signals ≥115mmHg were defined as high pressures in the pressure distributions with and without data smoothing according to a previous study17.
The distribution of high pressures without smoothing was qualitatively categorised into pressure distribution patterns in the representative frame of the static pressure distributions and all frames of the dynamic pressure distributions. The frequency of each pressure distribution pattern was individually calculated in the dynamic pressure distributions.
For the quantitative analysis, 5-minute data of dynamic pressure distribution data synchronised with the actions of the participants were recorded using a digital video camera was extracted because the longest duration of continuous recording was <6 minutes in a participant due to breakdown of sensors by their intense movement during performance. Smoothed pressure distributions were used for the following measurements – the area (cm2) with a pressure distribution of >5mmHg on the buttocks region (contact area), the average pressure of the contact area, and the maximum pressure on the ischial region (peak pressure). Parameters under dynamic conditions were extracted from the transition of peak pressure (Figure 1). Continuous high pressure was defined as a high-pressure period. Total duration (seconds) and maximum duration (seconds) of the high-pressure period were calculated, and the number (times) of high-pressure periods was counted.
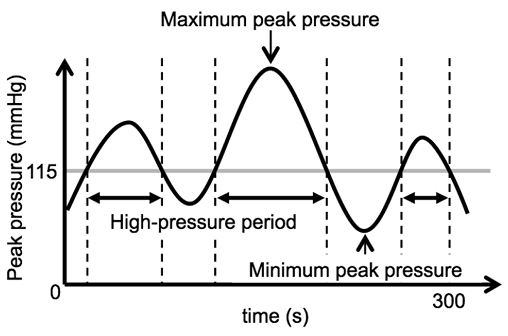
Figure 1. Transition of peak pressure during performance
Characteristics of participants and PIs are shown descriptively. Data are shown as medians (range) or numbers (%). Parameters of pressure distributions were compared among the data from three or four individuals and as medians (ranges) of the other participants. When individual data were out of the range of the data of other participants, we decided that they indicated a difference.
Results
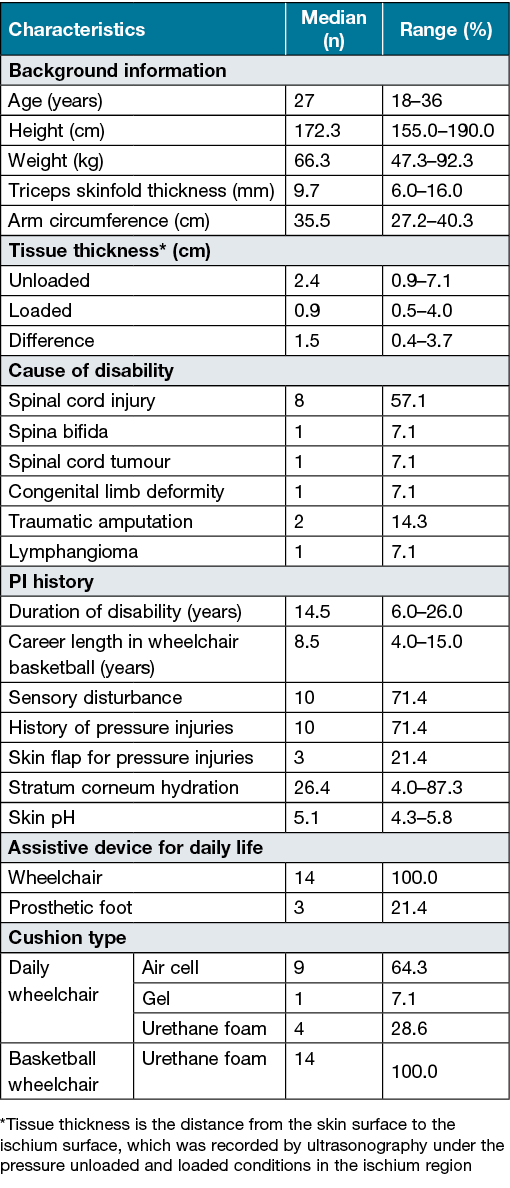
All the athletes who participated in the training camp were recruited, and none of them met the exclusion criteria of this study. The median (range) age of the participants was 27 years (18–36 years). The major cause of disability was spinal cord injury (57.1%). Ten participants (71.4%) with spinal cord injury, spina bifida or spinal cord tumour had sensory disturbance and a history of PIs. The median (range) tissue thicknesses unloaded and loaded were 2.4cm (0.9–7.1cm) and 0.9cm (0.5–4.0cm), respectively. Nine participants (64.3%) used air cell-type cushions, one participant (7.1%) used a gel-type cushion, and four participants (28.6%) used urethane foam-type cushions for their daily wheelchairs. All participants used urethane foam-type cushions for their basketball wheelchairs. The median (range) career length in wheelchair basketball was 8.5 years (4–15 years) (Table 1).
Table 1. Characteristics of participants (n=14)
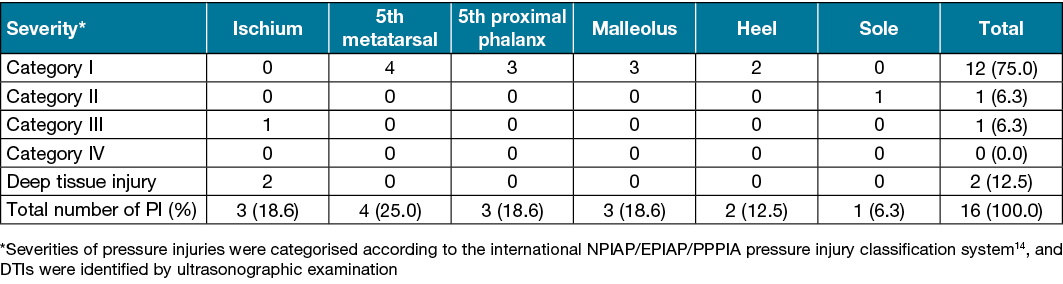
The participants had PIs on the skin region in contact with the wheelchair. The total number of PIs was 16 in five (35.7%) of the 14 participants, including 12 Category I PIs (75.0%), one Category II (6.3%), one Category III (6.3%) and two DTIs (12.5%) (Table 2).
Table 2. Severities and locations of PIs in wheelchair basketball athletes (n=14)
A researcher obtained 269,554 frames of images of static and dynamic pressure distributions. Distributions of high-pressure areas were categorised into 10 patterns as follows: (a) absence of high pressure, (b) unilateral ischium, (c) bilateral ischium, (d) unilateral greater trochanter, (e) unilateral ischium + unilateral greater trochanter, (f) unilateral femur, (g) unilateral ischium + unilateral femur, (h) belting region, (i) unilateral ischium + belting region, and (j) bilateral ischium + belting region (Figure 2). Because ischial PIs were more severe than the other regions, we focused on the ischial PIs of the respondents (IDs) 5, 7 and 11 in the following analysis.
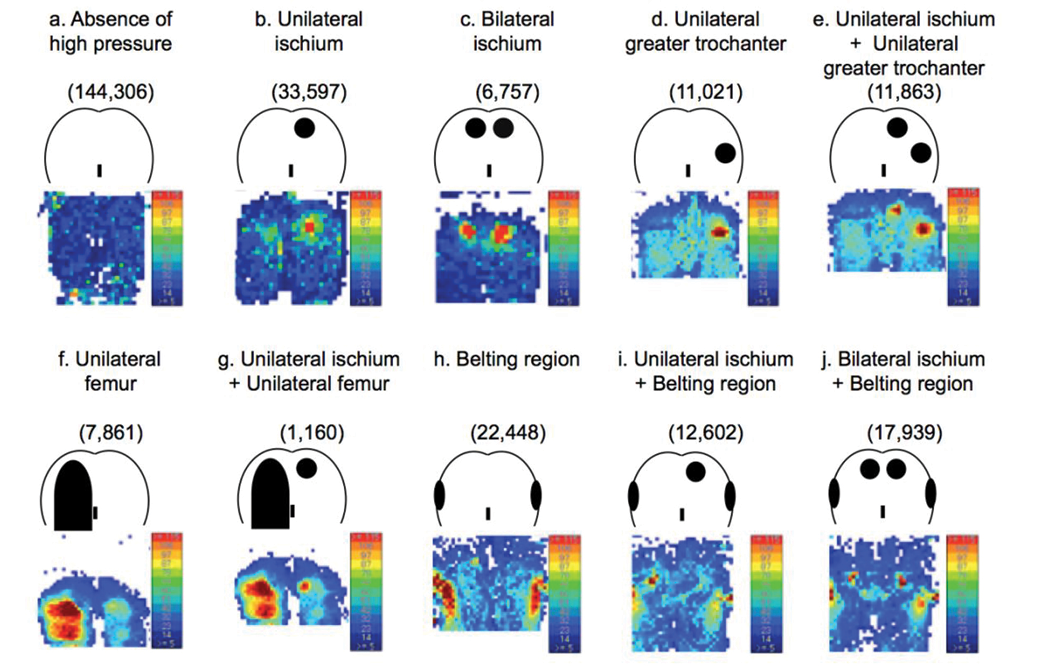
Figure 2. Buttock distribution pattern of high pressure areas under dynamic conditions. Raw data (lower images) and categorised distribution patterns (upper illustrations) of high pressure areas on buttocks are shown (a–j). The numbers of frames of pressure distribution are described in parentheses
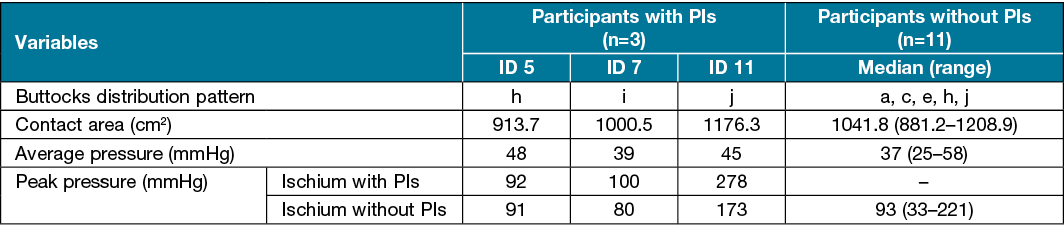
Under static conditions, buttock distribution patterns in athletes with PIs were (h), (i) and (j). Buttock distribution patterns in athletes without PIs were (a), (c), (e), (h) and (j). Contact areas for IDs 5, 7 and 11 were 913.7, 1000.5 and 1176.3cm2, respectively. The median (range) contact area of the participants without PIs was 1041.8cm2 (881.2–1208.9cm2) which suggested no difference in contact area between the participants with and without PIs. Average pressures for IDs 5, 7 and 11 were 48, 39 and 45mmHg, respectively. The median (range) average pressure of participants without PIs was 37mmHg (25–58mmHg), which suggested no difference in average pressure between participants with and without PIs. Peak pressures for IDs 5, 7 and 11 were, respectively, 92, 100 and 278mmHg on the ischia with PIs, and 91, 80 and 173mmHg on the ischia without PIs. The median (range) peak pressure for participants without PIs was 93mmHg (33–221mmHg), which suggested a higher peak pressure on the ischia with PIs for ID 11. A high pressure of ≥115mmHg was observed in one of the three on both sides of ischia for participants with PIs and for five of the 11 ischia of the participants without PIs (Table 3).
Table 3. Static condition parameters of pressure distributions on the buttocks of wheelchair basketball athletes (n=14)
Under dynamic conditions, buttock distribution patterns (i) and (j) were observed in all participants with PIs and in one participant without PIs (ID 4) (Table 4). Therefore, the quantitative parameters of ID 4 were compared individually with the median (range) parameters of other participants without PIs, as well as those of participants with PIs. Maximum peak pressures under dynamic conditions for IDs 5, 7 and 11 were, respectively, 144, 205 and 129mmHg on the ischia with PIs, and 107, 161 and 129mmHg on the ischia without PIs. The maximum peak pressure for ID 4 was 115mmHg. The median (range) maximum peak pressure was 79mmHg (range, 45–186mmHg) in participants without PIs, which suggested higher maximum peak pressures on the ischial region with PIs in ID 7. Average peak pressures for IDs 5, 7 and 11 were, respectively, 73, 78 and 90mmHg on the ischia with PIs, and 32, 42 and 74mmHg on the ischia without PI. The average peak pressure for ID 4 was 38mmHg. The median (range) average peak pressure of the participants without PIs was 38mmHg (27–67mmHg). Thus, the average peak pressures in all participants with PIs were judged to be higher than those for participants without PIs, except for ID 4. ID 4 showed no difference from the other participants without PIs (Table 5).
Table 4. Frequency of buttock pressure distributions on the buttocks under dynamic conditions in wheelchair basketball athletes (n=11)
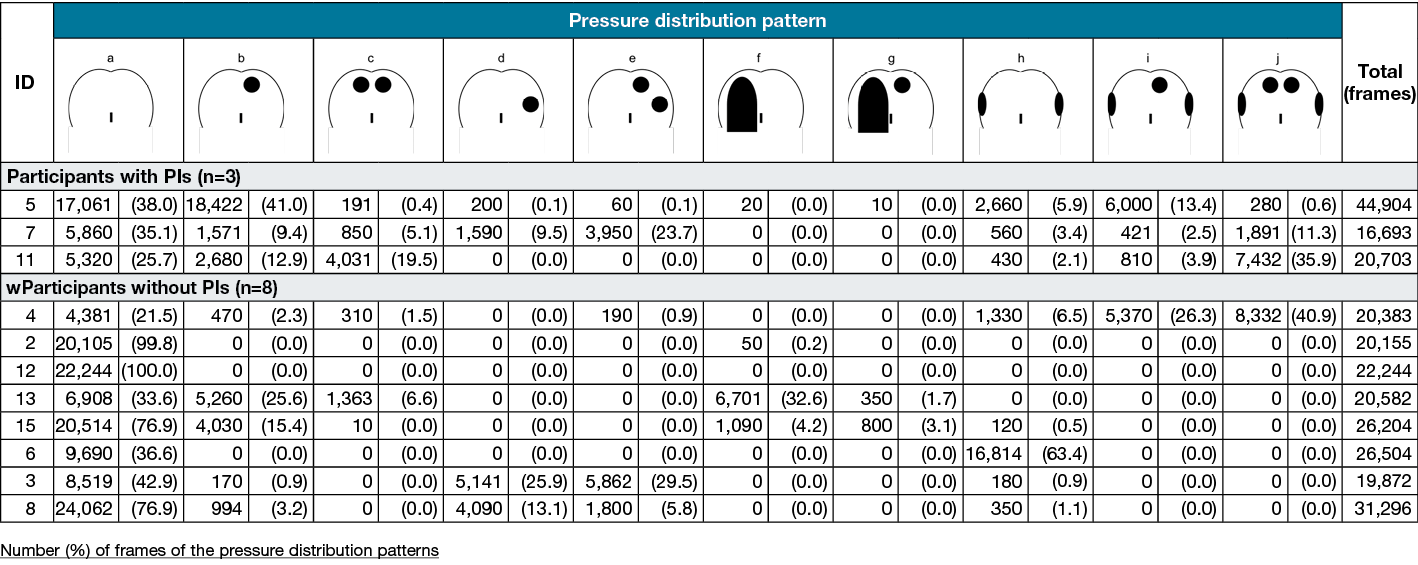
Table 5. Dynamic condition parameters of pressure distributions on the buttocks of wheelchair basketball athletes (n=11)
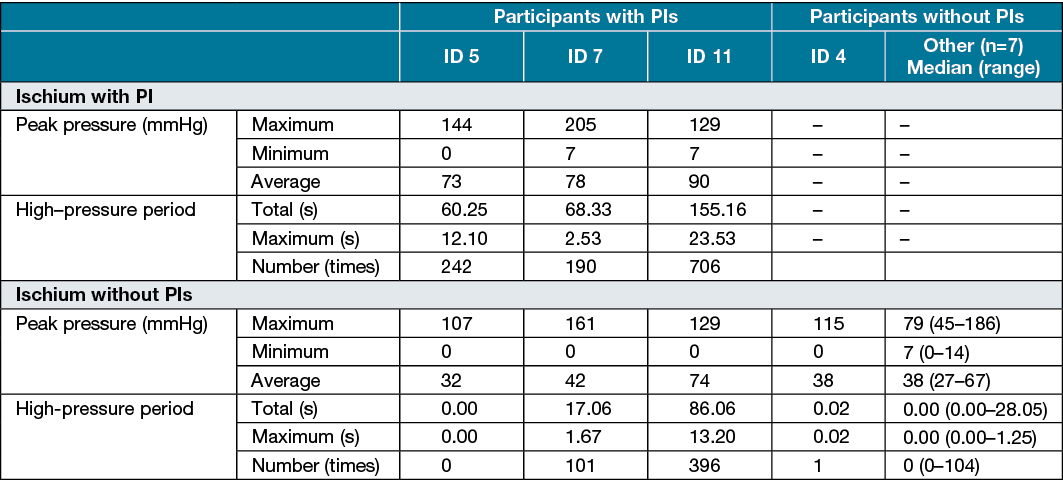
Total high-pressure periods for IDs 5, 7 and 11 were, respectively, 60.25, 68.33 and 155.16 seconds on the ischia with PIs and 0.00, 17.06 and 86.06 seconds on the ischia without PIs. The total high-pressure period for ID 4 was 0.02 seconds. The median (range) total high-pressure period in participants without PIs was 0.00 seconds (0.00–28.05 seconds). The maximum high-pressure periods for IDs 5, 7 and 11 were, respectively, 12.10, 2.53 and 23.53 seconds on the ischia with PIs and 0.00, 1.67 and 13.20 seconds on the ischia without PIs. The maximum high-pressure period for ID 4 was 0.02 seconds. The median (range) maximum high-pressure period for participants was 0.00 seconds (0.00–1.25 seconds). The numbers of high-pressure periods for IDs 5, 7 and 11 were, respectively, 242, 190 and 706 on the ischia with PIs, and 0, 101 and 396 on the ischia without PIs. The number of high-pressure periods for ID 4 was one. The median (range) number of high-pressure periods for the participants without PIs was 0 (0–104). All parameters related to high-pressure periods were higher in all participants with PIs compared with participants without PIs.
Discussion
This study was the first to investigate the association between ischial PIs and dynamic buttock pressure distributions during actual performance in wheelchair basketball athletes. Qualitative and quantitative analyses of static pressure distributions showed no distinctive features for participants with PIs, but the investigation of dynamic pressure distributions indicated continuous or repetitive, or both continuous and repetitive, high-pressure loading on ischia for participants with PIs during performance. Total high-pressure periods, maximum high-pressure periods, and number of high-pressure periods were possible indicators to predict PI occurrence in wheelchair basketball athletes.
The prevalence of buttock PIs was 21.4% in this study, which was lower than previously reported for wheelchair users with spinal cord injury (26.4–29.4%) and wheelchair athletes (27.3–75.0%)3,9,10,18,19. We considered this finding to reflect the relatively high awareness of participants and team staff on PI prevention in this study.
Because basketball wheelchairs are made to order for each player, the shapes of seat surfaces are not uniform. We individually adjusted the sensors to the wheelchair seat of each athlete by using a cut‑able sheet-type sensor. We also confirmed that measurements with this sensor were similar to the sensor used for measurement of static pressure distributions. We devised a way to fix the sensor sheet on the wheelchair seat and used a wireless logger. Participants said they did not feel uncomfortable and could perform as usual. Therefore, data from this study are thought to reflect pressure distributions during actual situations.
High pressure was observed on the PI-side ischia in one of three athletes with PIs and in five of 11 athletes without PIs under static conditions. These results suggest that the cut‑off value for evaluating the static pressure distributions of wheelchair basketball athletes should be higher. In the analysis of dynamic pressure distributions, the high-pressure period reflected this cut‑off value. All parameters related to the high-pressure period were higher in the ischia with PIs than in those without PIs, which suggests that 115mmHg is a beneficial cut‑off value to evaluate the risk of PIs during performance.
Static pressure distributions did not identify any differences between the participants with and without PIs. In contrast, all athletes with PIs and one (12.5%) of eight athletes without PIs had bilateral/unilateral ischium and belting region pressure distributions. When athletes drive a wheelchair forward in a frontward tilting posture, the pressure generally elevates on the belting region, and lessens on the ischial region. Nonetheless, high pressure was simultaneously detected on both the belting and ischial regions for participants with PIs. Our results suggest the importance of pressure relief consistent with athletes’ motions during performance. Quantitative parameters related to the high-pressure period clearly distinguished between participants with and without PIs. The assessment of dynamic pressure distributions is important to predict the occurrence of PIs in wheelchair basketball athletes.
In this study, five (35.7%) of 14 wheelchair basketball athletes had PIs. Conventionally, PIs are recognised as the localised damage of skin and/or underlying tissue due to self-weight. In addition, tissue damage by contact with medical devices such as nasal oxygen tubes, casts and splints are also recognised as a type of PI termed medical device-related PIs (MDRPIs)20,21. In this study, injuries due to pressure and/or shear on parts of the wheelchair were also included as PIs. Most PIs were wheelchair-related (10 of 14 of the PIs) on athletes’ feet and lower extremities, which suggests that these wounds are also a crucial problem for wheelchair basketball athletes. However, wheelchair-related PIs are not specific to wheelchair basketball athletes, because people with spinal cord injuries also frequently have PIs on their feet (79 of 106; 74.5%) and lower extremities (23 of 106; 21.7%)22. More detailed surveys and elucidation of associated factors are required for the several kinds of wheelchair users.
Limitations
This study had some limitations. A statistical analysis could not be included because of the small sample size. We could only observe pressure distributions, not shear stress. Further studies are required to address the statistical relationship between pressure distributions and PI occurrence for each motion during performance. Furthermore, the development of a standardised and convenient pressure distribution measurement system under dynamic conditions would be beneficial for predicting PI occurrence in wheelchair athletes.
In the future, we need to do further research to reduce the high pressures identified by this study. For example, education to promote pressure relief or development of cushions when playing a game to reduce the high pressure could be considered.
Conclusion
The prevalence of PIs was 35.7% in elite wheelchair basketball athletes from the training camp of the Japanese national team. They had PIs on the skin in contact with some parts of their wheelchair and on the ischial region. Ischial PIs were more severe than the other PIs. The qualitative analysis of buttock pressure distributions suggests that frequent loading on the ischium and belting regions during performance are associated with PIs. Dynamic condition parameters including average peak pressure, total high-pressure periods, number of high-pressure periods, and maximum high-pressure periods were higher in all participants with PIs than those without PIs. Our study showed a characteristic pressure distribution for participants with PIs under dynamic conditions, but not under static conditions. These findings can contribute to establishing a means for predicting PI occurrence in wheelchair basketball athletes.
Acknowledgments
The author would like to thank the elite wheelchair basketball athletes and staff for their kind cooperation.
Funding
This study was supported by a Sasakawa Scientific Research Grant from the Japan Science Society and YAMAHA Motor Foundation for Sports.
Conflict of interest
Takeo Minematsu and Misako Dai belong to the Department of Skincare Science which receives support from Saraya. Co. Ltd. Nao Tamai and Koichi Yabunaka belong to the Department of Imaging Nursing Science which receives support from FUJIFILM Corporation. Hiroshi Noguchi belongs to the Department Life Support Technology (Molten) which recieves support from Molten Corporation.
Author(s)
Tomonori Maeda MHS, RN1
Nao Tamai PhD, RN2,3
Takeo Minematsu PhD1,3
Hiroshi Noguchi PhD4
Koichi Yabunaka PhD, RT2
Gojiro Nakagami PhD, RN3,5
Mitsuso Neya PhD6
Hiromi Sanada* PhD, RN, WOCN, FAAN3,5
Department of Gerontological Nursing/Wound Care Management, Graduate School of Medicine,
The University of Tokyo, Hongo 7-3-1, Bunkyo-ku,
Tokyo 113-0033, Japan
Email hsanada@g.ecc.u-tokyo.ac.jp
hsanada-tky@umin.ac.jp
1Department of Skincare Science, Graduate School of Medicine, The University of Tokyo, Japan
2Department of Imaging Nursing Science, Graduate School of Medicine, The University of Tokyo, Japan
3Division of Care Innovation, Global Nursing Research Center, Graduate School of Medicine, The University of Tokyo, Japan
4Department of Life Support Technology (Molten), Graduate School of Medicine, The University of Tokyo, Japan
5Department of Gerontological Nursing/Wound Care Management, Graduate School of Medicine, The University of Tokyo, Japan
6Health and Training Science Course, Faculty of Sport Study, Biwako Seikei Sport College, Japan
* Corresponding author
References
1. Carless D, Peacock S, Mckenna J, Cooke C. Psychosocial outcomes of an inclusive adapted sport and adventurous training course for military personnel. Disabil Rehabil 2013;35(24):2081– 8.
2. Barak S, Mendoza-Laiz N, Fuentes MTG, Rubiera M, Huyzler Y. Psychosocial effects of competitive Boccia program in persons with severe chronic disability. J Rehabil Res Dev 2016;53(6):973–88.
3. Rocco FM, Saito ET. Epidemiology of sportive injuries in basketball wheelchair players. Acta Fisiátrica 2006;13(1).
4. Redelings MD, Lee NE, Sorvillo F. Pressure ulcers: more lethal than we thought? Adv Skin Wound Care 2005;18(7):367–72.
5. Spilsbury K, Nelson A, Cullum N, Iglesias C, Nixon J, Mason S. Pressure ulcers and their treatment and effects on quality of life: hospital inpatient perspectives. J Adv Nurs 2007;57(5):494–504.
6. Kivesley NJ, Chow AW. Infected pressure ulcers in elderly individuals. Clin Infect Dis 2002;35(11):1390–6.
7. Essex HN, Clark M, Sims J, Warriner A, Cullum N. Health-related quality of life in hospital inpatients with pressure ulceration: assessment using generic health-related quality of life measures. Wound Rep Regen 2009;17(6):797–805.
8. Klenck C, Gebke K. Practical management: common medical problems in disabled athletes. Clin J Sport Med 2007;17(1):55–60.
9. Shimizu Y, Mutsuzaki H, Tachibana k, Tsunoda K, Hotta K, Fukaya T, et al. A survey of deep tissue injury in elite female wheelchair basketball players. J Back Musculoskelet Rehabil 2017;30(3):427–34.
10. Mutsuzaki H, Tachibana K, Shimizu Y, Hotta K, Fukaya T, Karasawa M, et al. Factors associated with deep tissue injury in male wheelchair basketball players of a Japanese national team. Asia Pac J Sports Med Arthrosc Rehabil Technol 2014;1(2):72–6.
11. Gutierrez EM, Alm M, Hultling C, Saraste H. Measuring seating pressure, area, and asymmetry in persons with spinal cord injury. Eur Spine J 2004;13(4):374–9.
12. Urasaki M, Nakagami G, Sanada H, Kitagawa A, Tadaka E, Sugama J. Interface pressure distribution of elderly Japanese people in the sitting position. Disabil Rehabil Assist Technol 2011;6(1):38–46.
13. Peters JA. The influence of position and user characteristics on peak skin pressure in elite wheelchair racers. Master thesis of the University of Illinois; 2017.
14. National Pressure Injury Advisory Panel, European Pressure Ulcer Advisory Panel, Pan Pacific Pressure Injury Alliance. Prevention and treatment of pressure ulcers/injuries; clinical practice guideline. NPIAP/EPUAP/PPPIA; 2019.
15. Aoi N, Yoshimura K, Kadono T, Nakagami G, Iizuka S, Higashino T, Sanada H. Ultrasound assessment of deep tissue injury in pressure ulcers: possible prediction of pressure ulcer progression. Plastic Reconstruc Surg 2009;124(2):540–50.
16. Araki D, Osada T, Nakauchi Y, Kawaguchi T. Proposal of body movement variation analysis technique on bed for fall prevention. Transact JSME (in Japanese) 2017;83(856):17–00210.
17. Brienza DM, Karg PE, Geyer MJ, Kelsey S, Trefler E. The relationship between pressure ulcer incidence and buttock-seat cushion interface pressure in at-risk elderly wheelchair users. Arch Phys Med Rehabil 2001;82(4):529–33.
18. Adriaansen JJ, Ruijs LE, Koppenhagen CF, Asbeck FW, Snoek GJ, Kuppevelt D, et al. Secondary health conditions and quality of life in persons living with spinal cord injury for at least ten years. J Rehabil Med 2016;48(10):853–60.
19. Kovindha A, Kammuang-lue P, Prakongsai P, Wongphan T. Prevalence of pressure ulcers in Thai wheelchair users with chronic spinal cord injuries. Spinal Cord 2015;53(10):767–71.
20. Chen L. The risk management of medical device-related pressure ulcers based on the Australian/New Zealand Standard. J Int Med Res 2018;46(10):4129–39.
21. Kayser SA, Vangilder CA, Ayello EA, Lachenbruch C. Prevalence and analysis of medical device-related pressure injuries: results from the international pressure ulcer prevalence survey. Adv Skin Wound Care 2018;31(6):276–85.
22. Scheel-Sailer A, Wyss A, Boldt C, Post M, Lay V. Prevalence, location, grade of pressure ulcers and association with specific patient characteristics in adult spinal cord injury patients during the hospital stay: a prospective cohort study. Spinal Cord 2013;51(11):828–33.



