Volume 30 Number 4
Best practice, best products, best outcomes in community wound care: three descriptive cohorts
Keryln Carville, Janine Alan and Joanna Smith
Keywords best practice, Chronic wounds, Cost, acute wounds, community
For referencing Carville K, Alan J & Smith J. Best practice, best products, best outcomes in community wound care: three descriptive cohorts. Wound Practice and Research 2022; 30(4):196-206.
DOI
https://doi.org/10.33235/wpr.30.4.196-206
Submitted 31 October 2022
Accepted Accepted 24 November 2022
Abstract
Aim To determine the number of clients with wounds, and the types of wounds, admitted to an Australian community nursing service, and to describe their healing trajectory and cost of treatment labour and consumables.
Method Point-of-care data from three retrospective cohorts of clients admitted for community wound care between 1 November 2016 and 30 June 2021 was analysed descriptively.
Results The three cohorts comprised 41,865 clients; the median age was 74 years (interquartile range [IQR] 58–84), with 88,793 wounds. Healing is complex, and heterogeneity in healing times and costs was demonstrated as anticipated a priori. Acute wounds were the most common across all three cohorts (38–45%, 40% overall), followed by skin tears (15–17%, 16% overall), leg ulcers (13–14%, 14% overall) and foot ulcers (7–9%, 9% overall). The median length of treatment for all discharged wounds was 18–22 days. Acute wounds and skin tears had the shortest length of treatment, and benign and malignant tumours the longest. For each cohort, eight out of 10 wounds were discharged healed or were transferred to self-care. Stage 4 pressure injuries, open incisions following amputation, fistulae and venous leg ulcers (VLUs) were the most costly to manage.
Conclusion This study provides an important account of consumable and direct labour costs to treat Australian community wounds. Healing/self-care outcomes were consistently favourable.
Introduction
Acute wounds are defined as wounds that proceed through an orderly and timely reparative process with sustained restoration of anatomical integrity1. Chronic, or hard-to-heal, wounds fail to proceed along this trajectory1,2. Some authors define a healing time of longer than 1–3 months to indicate chronicity3,4. Regardless of definitional differences, acute and chronic wounds can constitute significant treatment challenges, reduce quality of life for afflicted individuals, and impose a considerable economic burden on healthcare providers across all settings5–7. The actual scope of the wound burden and the associated costs of treatment for Australians with a wound is unknown or is estimated on modelled costs, and primarily for chronic wounds8. Graves and Zheng projected the direct healthcare costs of chronic wounds in hospitals and aged care settings to be A$3 billion a year, which equated to almost 2% of Australian national healthcare expenditure in 2016–20178. However, this projection failed to take into account wounds managed by community healthcare providers8. This current study aimed to provide a detailed description of clients’ wounds managed in an Australian community nursing setting, including healing times and cost of management.
Methodology
Setting and data source
Silver Chain Group Limited (Silverchain) is a large Australian not-for-profit community care service which has been an industry leader in health and aged care in the community for over 100 years. Wound management comprises a significant component of clinical care delivered by the nurses they employ. The organisation adheres to best practice wound management, which includes the provision of contemporary wound products at no cost to clients. Furthermore, best practice is underpinned by the embedding of evidence obtained from national and international wound guidelines and standards into policies, procedures and education programs. Nurses are provided with ongoing education and resources that enable comprehensive assessment and management of complex wounds.
Silverchain utilises a purpose-built, in-house electronic management system (EMS). In 2015, the current EMS was enhanced to include the ‘Wound Module’, which is the data source for the three wound cohorts reported here. The Wound Module enables the electronic capture of comprehensive data (assessments, treatment plans, consumables used to treat and wound images) by nurses at point-of-care in wound clinics or clients’ homes, using tablet and smartphone technologies. This wound data is processed into business intelligence dashboards that are used by primary nurse providers, team leaders, managers and data integrity nurses to routinely monitor wound healing data and outcomes, and to inform the need for quick responses if data or clinical issues are identified.
Data quality
The organisation’s national rollout of the Wound Module commenced in Western Australia (WA) in 2015, followed by Queensland (QLD) in 2016 and South Australia (SA) in 2020. Wound data entry by nurses has been assessed on numerous occasions via inter-rater reliability testing. Rigour of data collection is ensured by ongoing monitoring of data and feedback to managers and nurses regarding the completeness of electronic client wound records.
Study design and selection of community-treated wounds
The study included all wound clients admitted and treated by Silverchain nurses during the defined cohort periods. Clients with wounds cared for by this organisation prior to a cohort start date were excluded, with the exception of an extended analysis in the third cohort, 3B (see below).
This study reports on three retrospective wound cohorts that were drawn from data collected at point-of-care during 1 November 2016 to 30 June 2021 and entered into the Wound Module. The scope and time period of each cohort coincided with different stages of the Wound Module rollout and were principally determined by routine business quality assurance reviews as follows:
- Cohort 1: WA metropolitan area wound cohort that describes 6 months of data from 1 November 2016 to 30 April 2017.
- Cohort 2: WA state-wide and QLD Sunshine Coast community nursing service wound cohort that describes 12 months of data from 1 July 2018 to 30 June 2019.
- Cohort 3A: WA state-wide, QLD Sunshine Coast and SA metropolitan community nursing service wound cohort that describes 12 months of data from 1 July 2020 to 30 June 2021 (the 2020/21 financial year, FY).
Cohort 3B is an extended analysis of Cohort 3A because it includes the treatment costs of any wound from 1 July 2020 to 30 June 2021 (the 2020/21 FY) (regardless of admission date and discharge outcome). This period coincided with the COVID‑19 pandemic and sequelae.
Descriptive client and wound characteristics
The general characteristics of each of the three wound cohorts were described using routinely available data from the Wound Module: client age; gender; source of wound occurrence (e.g. community, hospital); wound category (acute, leg ulcer, pressure injury, skin tear, foot ulcer, tumour, other); and wound types (within wound categories). Skin tears which result from trauma are, in effect, acute wounds; however, the organisation categorises skin tears separately as their data indicates skin tears are a large cohort of wounds in elderly community clients.
Wound outcomes measured
Three wound outcomes were measured in each cohort:
- Wound discharge outcomes for clients discharged on or before the cohort end date – healed, self-care, deceased, unhealed on discharge. Self-care refers to wounds that were either almost healed, or a protective dressing was applied and the client removed the final wound dressing.
- Length of treatment episode (days) for discharged wounds.
- The cost of wound consumables, which were automatically allocated in the Wound Module with each care plan entry. However, for comparison purposes, wound consumable costs for Cohorts 1 and 2 were indexed to equivalent 2020/21 FY costs using consumer price index (CPI) percentage change figures (for pharmaceuticals) from the Australian Bureau of Statistics9.
Wounds were defined as discharged if the date of discharge was on or before the end date of each cohort time period (except Cohort 3B). All three outcomes were assessed from this community nursing service perspective only, so they did not factor in any concurrent care from other wound care providers, nor wound duration prior to, or following admission for wound care.
For Cohorts 1 and 2, costs are reported for consumables only (not labour), because actual labour data was unavailable for this study. Consumable costs excluded the goods and services tax. For Cohort 3B, we report the cost of wound consumables plus direct nursing time costs. The actual pay rate of the nurse(s) who treated each wound and the actual duration of each wound treatment were used. This was possible because we had robust actual, not estimated, times and costs for the direct nursing staff involved in wound care for Cohort 3B. This provided an important insight into the cost impact of treating all wounds referred to this community nursing provider. This analysis excluded any indirect costs (e.g. organisational overheads, management, administration, travel, systems, training) that were additional to direct client contact, and business overheads (e.g. rent, utilities, insurances, vehicles, maintenance and repairs). Consequently, the costs reported in this paper are unsuitable for other purposes (such as contract price setting) beyond the scope of this paper.
Statistical analysis
Descriptive statistics are presented as counts and percentages for categorical variables. Continuous data (length of stay and cost outcomes) had skewed distributions and are therefore presented as medians and interquartile ranges (IQR). The IQR represents the range of values between the 25th percentile and the 75th percentile. All statistical analyses were performed using Stata version 1710. Costs were expressed in Australian dollars.
Ethics statement
Wound Cohorts 1, 2 and 3A were analysed as part of Silverchain’s routine quality assurance and evaluation activities and so were deemed exempt from ethical approval as human research. Silverchain has a proportional ethical review framework that operationalises the National Statement on Ethical Conduct in Human Research11.
Results
Cohort description
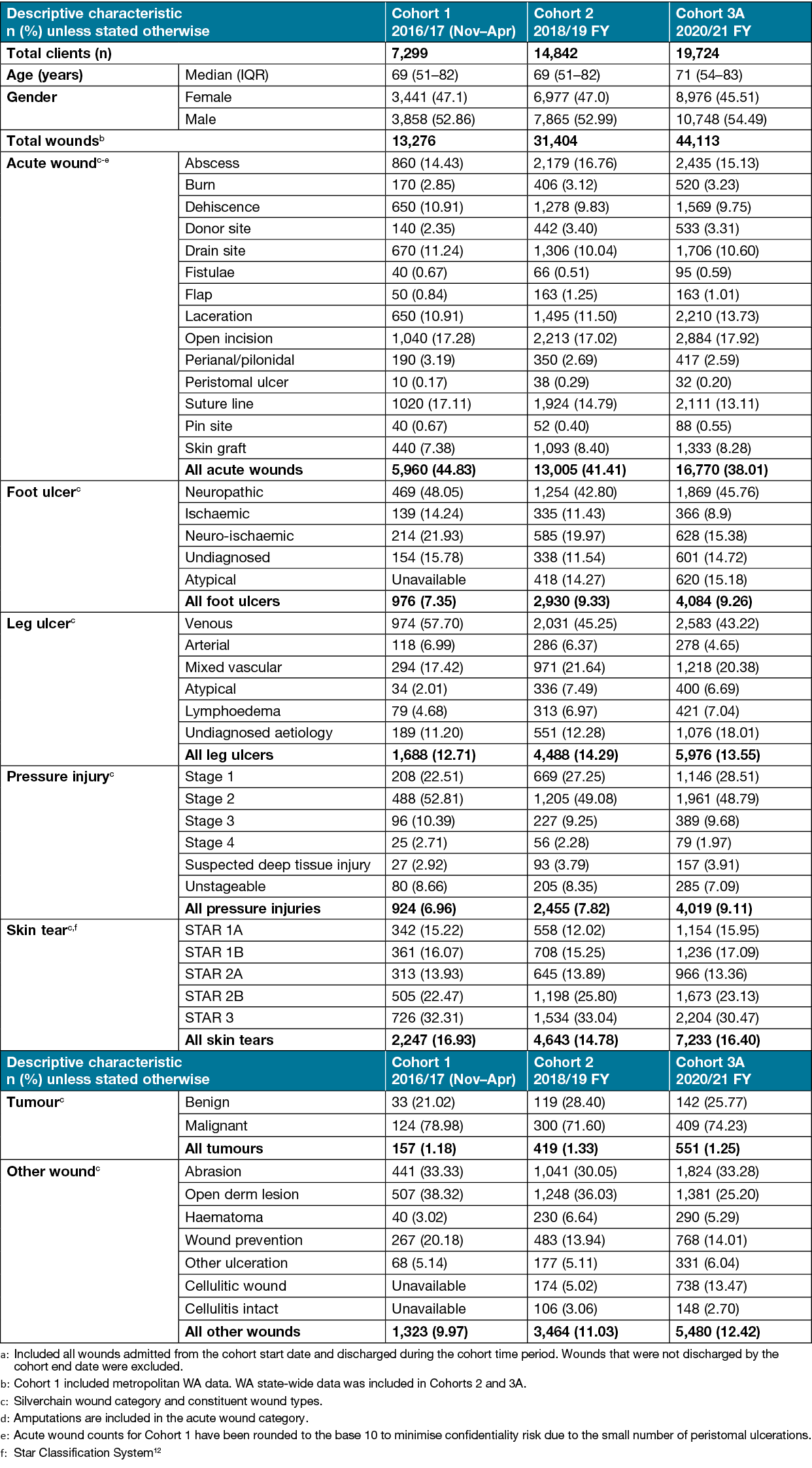
Collectively, the three cohorts comprised 41,865 clients with 88,793 wounds, from infants to centenarians. The IQR demonstrates this large age span, with 25% of wound care clients aged over 84 years. Overall, wounds were acquired in the community (64%), hospital (31%), other settings (2%), and unknown (3%). The top three most common wound categories across all three cohorts were acute wounds (38–45%, 40% overall), skin tears (15–17%, 16% overall) and leg ulcers (13–14%, 14% overall). Foot ulcers were the least common (7–9%, 9% overall). Pressure injuries comprised 7–9% (8% overall) of wounds and ‘Other’ wounds 10–12% (11% overall). Table 1 shows the full characteristics of the three cohorts. Less than 2% of wound records were excluded due to missing assessment or treatment data. This included any referral for wound care that did not eventuate due to a change in client circumstances (e.g. hospitalisation or death).
Table 1. Characteristics of three community nursing service wound cohortsa
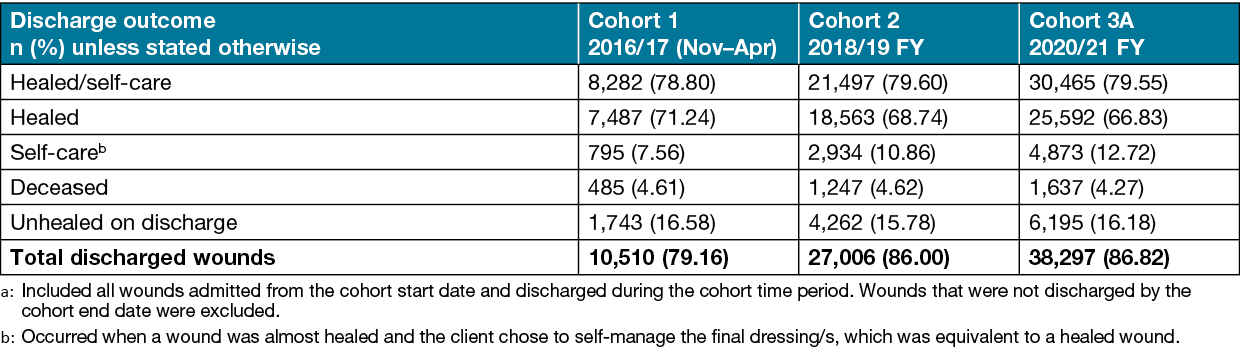
Wound discharge outcome
As shown in Table 2, there were consistent and favourable wound discharge outcomes across all three Cohorts (1, 2 and 3A). Eight out of 10 wounds were discharged healed or transferred to self-care. Self-care wounds were effectively healed wounds. This equated to 79% of wounds discharged healed or to self-care in the respective time periods for Cohort 1 and 80% for Cohorts 2 and 3A. Wounds that were unhealed on discharge occurred for a variety of reasons, including hospitalisation (any reason), wound care transfer to other providers (e.g. outclient clinic or general practitioner, [GP]), entry to residential aged care, or that the client became uncontactable or died (noting palliative care clients with wounds were included in the three cohorts).
Table 2. Wound outcomes on discharge for the three community wound cohortsa
Episode length of treatment (ELT) of discharged wounds
Tables 3 and 4 show the length of treatment calculated at an episode level (i.e. not per wound treatment/visit). The median ELT of discharged wounds varied by wound category and was broadly equivalent for Cohorts 2 and 3A, noting they were potentially treated over a longer time period (up to 12 months) and included a larger number of wounds than Cohort 1 (6 months).
Across all three cohorts, the median ELT of discharged wounds was longest for leg ulcers (29–42 days), tumours (33–35 days) and foot ulcers (26–38 days), and shortest for acute wounds (15–18 days) and skin tears (17–19 days). Over the three cohorts, the ELT of pressure injuries ranged from 20–26 days and ‘Other’ discharged wounds ranged from 18–22 days. The median ELT of discharged wounds, irrespective of wound category, was 18 days for Cohort 1 and 22 days for Cohorts 2 and 3A.
Table 3. Median ELT (days) of discharged clients for the three community wound cohortsa
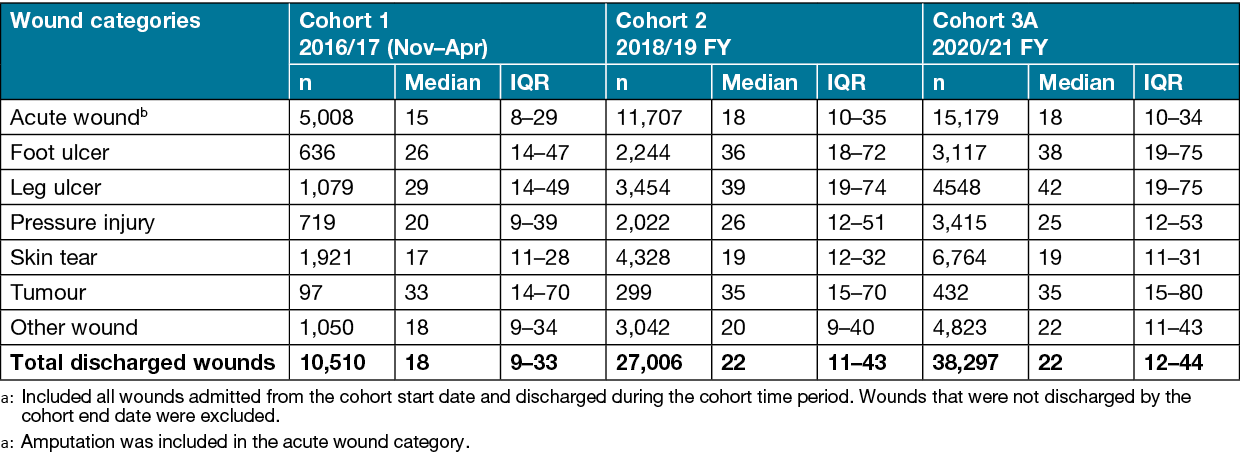
Table 4. Episode cost of discharged wounds for the three community wound cohorts (consumables only)a,b
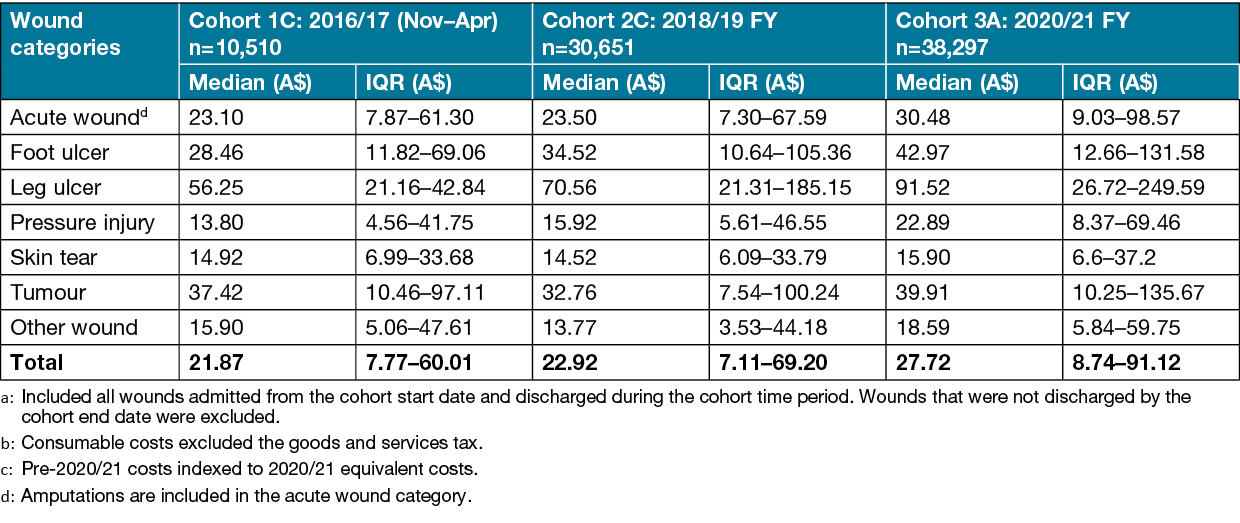
Episode consumable cost of discharged wounds (excludes direct care staff costs)
Cohort 3A (2020/21 FY) had the highest median episode wound consumable costs of all three cohorts (A$27.72), with a tenfold difference in the lower and upper bounds of the IQR (A$8.74–91.12) (Table 4). Across all cohorts, the median consumable cost of discharged wounds varied considerably within and between wound categories. Leg ulcers had the highest median consumable costs (A$91.52) per episode, noting 25% of consumable costs exceeded A$249.59. Foot ulcers had the next highest median wound consumable costs per episode; these were approximately half the consumable cost of leg ulcers across all three cohorts. Skin tears and other wounds not elsewhere classifiable had the lowest median consumable costs; they were approximately 4–5 times less costly than leg ulcers.
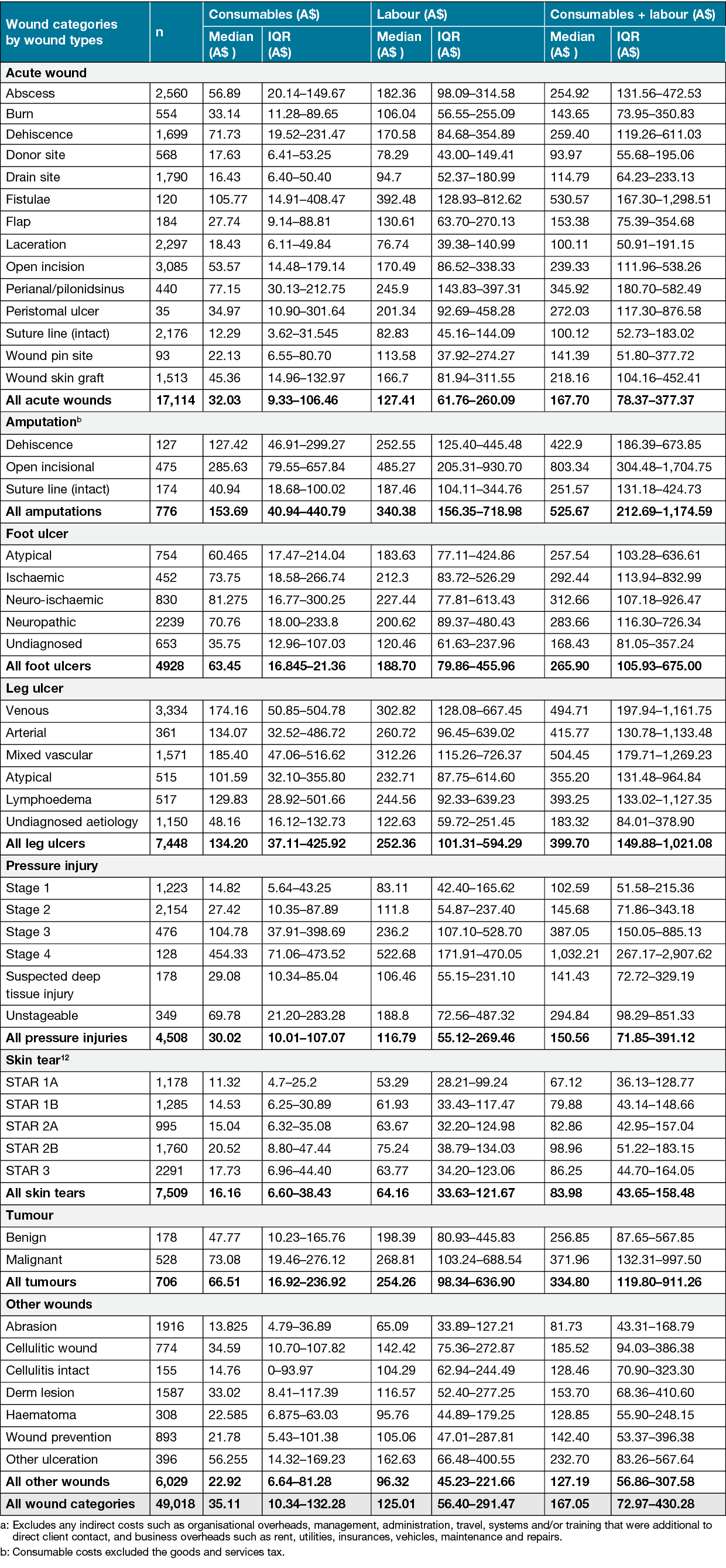
Table 5 shows the cost of wound consumables plus direct nursing time costs per wound for Cohort 3B. This includes any wound treated by this community nursing service during the 2020/21 FY, regardless of admission date and discharge status. Table 5 expands the cost perspective provided in Table 4, where the latter was confined to consumable costs for discharged wounds only. It confirms the considerable number and acuity of wounds treated across three Australian states. Per wound, the median consumable plus direct nursing costs of providing wound care during the 2020/21 FY was A$167.05, irrespective of wound category or discharge outcome, noting 25% of these costs per wound exceeded A$430.28.
Acute wounds was the largest wound category (n=17,114), with a median cost per wound of A$167.70. While there were fewer amputations (n=776) than other wound categories, they had the highest median consumable plus direct nursing costs (A$525.67), with 25% of amputations exceeding A$1,174.59 per wound. Open incisional wounds following amputations had the highest median cost of all amputations (A$803.34, IQR A$304.48–1,704.75), and was second only to Stage 4 pressure injuries (A$1,032.21, IQR A$267.17–2,907.62) as the single most expensive wound type (within a wound category). Leg ulcers were the second costliest wound category, representing 15% of all wounds and having a median cost per wound of A$399.70. One quarter of leg ulcers had costs exceeding A$1,021.08. The ratio of median consumable costs to direct nursing labour costs was approximately 1:4 respectively for most wound categories, except amputations and leg ulcers, which had higher median consumable costs.
Table 5. Cost of all community wounds treated in 2020/21 FY (consumables and direct nursing labour) regardless of admission date and discharge status (Cohort 3B)a,b
Discussion
Using point-of-care data collection, our Australian study comprised three cohorts of clients with wounds who received wound care from a community nursing provider. Collectively, Silverchain nurses managed 41,865 clients with 88,793 wounds. This finding confirms the large number of wounds treated in the community and that wound management often comprises the largest portion of community nurses’ workload13–15 and associated costs16. It has been previously reported that 70–80% of wounded individuals are treated in the community, and predominately by community nurses who spend 60% of time involved in these activities7.
Our study found acute wounds related to surgical or traumatic aetiologies (excluding skin tears) comprised the greatest number of wounds (n=35,735) across the combined cohorts. A total of 14 different wound types were included in the acute wound category. Open incisions (surgical incisions healed by secondary intention, n=6,137) and dehisced wounds (healed by secondary intention, n=3,497) constituted the greatest numbers of the acute wounds.
Skin tears, which are due to trauma, are also acute wounds. However, as they comprise the commonest wound in the elderly17,18 across all health settings12,19, it was deemed relevant to categorise skin tears separately. Nevertheless, if we combined skin tears with other acute wounds, the combined categories would increase to 56% overall (53–62%). This finding is interesting because acute wounds are also the most common wounds treated in hospitals7,19,20. Comparative investigation into the casemix and clinical care requirements of hospital versus community acute wounds may be beneficial to identify potential opportunities for hospital substitution with community-based models of wound care.
Contemporary studies about acute community wounds are uncommon. However, acute wounds were found to be the majority of wounds in a North American community cross-sectional study21. In a UK population-based study the percentage of acute wound clients (1.6 million) visited by community nurses in 2017/18 was 24%, 46% and 34% for open wounds, surgical wounds and other acute wounds, respectively22. An Australian cross-sectional study of 18 general practices in Queensland in 2011 involved 159 clients with 195 wounds who received 336 wound care episodes. It found 81.5% of acute wounds arose from surgery or trauma23. The prevalence of acute community wounds could be related to increased uptake of hospital prevention or early discharge programs to manage hospital bed use and burgeoning hospital costs. Regardless, it reflects the need for community practitioners to be knowledgeable and well resourced in the management of both acute and chronic wounds of varying complexities.
While they generally originate from acute wounds, chronic wounds do not heal in a timely or orderly reparative way. Although there is no agreed definition for what constitutes a chronic wound, they are generally hard-to-heal wounds due to intrinsic and extrinsic factors that impact on the individual, their wound or healing environment2,24. Chronic wounds have historically been perceived as the majority of wounds managed by community health providers7,13,14,25. They cause immense economic burden to individuals and the health system5,6,8,26. Chronic wounds can take years to heal, sometimes decades, often causing immense human suffering as a result of impaired quality of life, including pain, social isolation and depression27,28.
In our study, Stage 4 pressure injuries, while relatively low in number (n=128, Cohort 3B), were the most costly type of chronic wound to treat (median A$1,032/wound), with 25% of these wounds exceeding A$2,908 in 2020/21 FY. This finding underscores the importance of pressure injury prevention in high risk groups (e.g. immobile people), and identification and appropriate treatment of earlier-stage pressure injuries to prevent conversion to deeper more complex pressure injuries.
We found that leg ulcers comprised the highest number of chronic wounds at 1,688 (13%), 4,488 (14%) and 5,976 (14%) in Cohorts 1, 2 and 3A respectively. Venous leg ulcers (VLU) constituted the greatest number of leg ulcer types at 974 (58%), 2,031 (45%) and 2,583 (43%) respectively. Cohort 3B analysis also showed that VLU were equal second with mixed vascular aetiology leg ulcers insofar as being the most costly chronic wound to treat (Table 5, median A$495/wound). This is broadly consistent with other VLU literature16,29.
It has been estimated that VLU affect over 300,000 mainly older Australians and this number is likely to increase with the ageing population30. VLUs can result in lengthy wound healing times and demonstrate high recurrence rates of up to 78%30,31. Compression therapy in the form of bandages, hosiery or wraps is considered the ‘gold’ standard principle of treatment for VLUs30,32; however, there is currently no government reimbursement scheme for dressings or compression therapies for all Australians. This lack of financial support has led to considerable lobbying in the contemporary literature5,6,26,31. Cheng et al29 determined reimbursement of compression therapy for the treatment of VLUs would cost the Australian health system an additional A$270 million over 5 years, which would be substantially offset by the A$1.4 billion in cost savings. The median cost for wound management of a VLU in Cohort 3B in our study was A$495, which demonstrates relatively inexpensive care outcomes at a whole of health system level when compression bandages and wraps were supplied at no cost to clients.
Direct comparison of our wound cost findings with previously published literature is challenging due to differences in the types of wounds, care settings, wound care providers, follow-up duration, cost components and units of cost measurement. Although limited evidence is available for wound management cost comparisons in Australia, the previously mentioned UK study conducted in 2017/18 estimated that the UK National Health Service (NHS) managed 3.8 million individuals with wounds at a cost of £8.3 billion that year22. Interestingly, these authors reported 70% of these wounds healed in the study year22 compared with 79–80% of the wounds in our three cohorts which were discharged healed/self-care (virtually healed). In the United States, Medicare expenditure was conservatively estimated to be US$28 billion to US$31.7 billion for 8.2 million clients with chronic wounds in 201433.
The previously mentioned Queensland study with 336 wound care episodes in general practice in 2011 found a median cost of GP care of A$31.10, wound care products of A$9.92, and nurse time to deliver the care of A$10.3723. Another Australian study modelled the direct healthcare costs of chronic wounds in hospitals and residential care facilities in 2010/11 based on data collected from a systematic review of the literature and determined pressure injuries, diabetic foot ulcers, venous ulcers and arterial ulcers cost A$4.42 billion annually5. The mean cost of wound management to the UK NHS over 12 months was £7,300 per wound (range £6,000–13,700)34. However, costs in this study included wound consumables used to treat, district nurse and general practice nurse time to treat, GP visits, hospital outclient visits, laboratory tests and prescribed medications34. Although the additional GP reviews, laboratory tests and medications are associated with the management of wounds, there are currently national Australian schemes that cover the funding, or part thereof, for these interventions. Similar schemes that cover the cost for wound consumables are not universally available in Australia.
Our study showed favourable discharge outcomes when clients were supplied with wound care products as a component of their care. It is currently unknown whether comparable outcomes can be achieved when wound care product costs are borne by clients as an out-of-pocket expense. Importantly, many community care clients have no regular source of income other than social security payments (due to age or incapacity). Financial stress and poverty levels have worsened in Australia over the past 3 decades35. People with chronic conditions are more likely to experience severe financial hardship. High out of pocket health expenses can drive low income households into poverty, resulting in decisions to skip essential care (e.g. prescribed medications and specialist appointments) that often leads to poorer health and higher health systems costs35. From a wound care perspective, we believe sustainable government funding of both clinical labour and wound consumables is essential for optimising care outcomes and overall healthcare costs.
Strengths
A key strength of our study lies in this community nursing provider’s ability to collect point-of-care data on wound assessments, care plan interventions and actual cost of consumables used to treat. The data is contemporary and readily accessible on business intelligence dashboards that are used by primary nurse providers, team leaders, team managers, executive staff and data integrity nurses to routinely monitor wound healing data and outcomes. This data informs benchmarking of care outcomes across client cohorts, nurse teams and the Australian states where this provider operates. It also informs service planning, and the procurement and provision of best products for best clinical outcomes.
Another strength of our study was its inclusion of Cohorts 3A and 3B using data collected during the COVID‑19 pandemic. COVID‑19 profoundly impacted health service and home care activity. In Australia, this included temporary restrictions on non-urgent elective surgery36,37 and clients cancelling or delaying GP38 and home care visits until their confidence in infection control and prevention measures improved39. Anecdotally, more Silverchain clients opted for shared care of their wounds in the early days of COVID‑19 to reduce the number of contact visits. Shared care is where this community nursing provider supports appropriate clients (or their informal carers) to self-administer wound care as per a clinically informed wound care plan (with provision of wound consumables). Clinical nurses also reported treating a greater number of clients with more complex health issues in the community during the 2020/21 FY, presumably due to COVID‑related hospital admission restrictions. This potentially explains the higher median ELT (for some wound categories) and wound consumable costs (for all wound categories) in Cohort 3A.
Limitations
Whilst Cohort 3B provided an important insight into the cost of treating wounds referred to this community nursing provider, our analysis excluded any indirect nurse costs that were additional to direct client contact, and business overheads. Consequently, the costs reported here do not encompass the entire cost of service provision, which was beyond the scope of this paper. Furthermore, the IQR values reported in this study showed significant heterogeneity in costs within and between wound categories and types. Relying on the median cost alone underestimates the cost burden of community wounds. This was particularly evident in the expanded analysis conducted for Cohort 3B.
Another limitation was that only information on the management of wounds by this community nursing provider was captured, not concurrent or alternative treatments by other service providers. Additionally, the ELT for Cohorts 1, 2 and 3A included only those wounds that were admitted on or after the cohort start date and discharged on or before the cohort end date. Consequently, these cohorts excluded wounds with longer ELT (and higher costs to treat). Future wound healing and cost to treat research is warranted to understand longitudinal changes.
Conclusion
This study provides an important and actual (not estimated) account of consumable and direct labour costs to treat community wounds in Australia. Furthermore, it provides evidence about the significant number of acute wounds being managed in the community and the length of time to healing for some chronic wounds. It established that wound healing outcomes of up to 80% were achievable when nurses employed best practice wound management and clients had access to contemporary treatment consumables at no added cost to the clients.
Acknowledgements
The authors would like to thank these Silverchain staff: all nurses for their wound expertise, dedication and commitment to collecting high-quality community wound data using the Wound Module; Cate Maguire RN and Rosie Dekens RN for wound data integrity monitoring; and Professors Karen Smith and Anna Barker for their editorial assistance.
Author contribution
The authors confirm equal joint responsibility for the following – study conception and design, analysis and interpretation of the results, and draft manuscript preparation. No responsibility is claimed for data collection because this study performed secondary analysis on existing data. All authors reviewed the results and approved the final version of the manuscript.
Conflict of interest
The authors declare no conflicts of interest.
Ethics statement
The three wound cohorts were analysed as part of Silverchain’s routine quality assurance and evaluation activities and so were deemed exempt from ethical approval as human research. Silverchain has a proportional ethical review framework that operationalises the National Statement on Ethical Conduct in Human Research.
Funding
The research described in Cohort 1 in this paper was funded in part by the Federal Government via the Wound Management Innovation Collaborative Research Centre (2010–2018).
Author(s)
Keryln Carville1,2*, Janine Alan1 and Joanna Smith1
1Silver Chain Group Limited (Silverchain), Perth, WA
2Curtin University School of Nursing, Perth, WA
*Corresponding author Email Keryln.Carville@silverchain.org.au
References
- Lazarus GS, Cooper DM, Knighton DR, et al. Definitions and guidelines for assessment of wounds and evaluation of healing. Arch Dermatol 1994;130:489–493.
- Carville K. Wound care manual. 7th ed. Osborne Park: Silver Chain Nursing Association Incorporated, 2017.
- Mustoe TA, O’Shaughnessy K, Kloeters O. Chronic wound pathogenesis and current treatment strategies: a unifying hypothesis. Plast Reconstr Surg 2006;117:35s–41s. doi:10.1097/01.prs.0000225431.63010.1b.
- Sen CK. Human wounds and its burden: an updated compendium of estimates. Adv Wound Care 2019;8:39–48. doi:10.1089/wound.2019.0946.
- Kapp S, Santamaria N. The financial and quality-of-life cost to patients living with a chronic wound in the community. Int Wound J 2017;14:1108–1119. doi:10.1111/iwj.12767.
- Pacella R, Tulleners R, Cheng Q, et al. Solutions to the chronic wounds problem in Australia: a call to action. Australia Centre for Health Services Innovation, Kelvin Grove. Queensland, 2018.
- Lindholm C, Searle R. Wound management for the 21st century: combining effectiveness and efficiency. Int Wound J 2016;13:5–15. doi:10.1111/iwj.12623.
- Graves N, Zheng H. Modelling the direct health care costs of chronic wounds in Australia. Wound Prac Res 2014;22:20.
- Australian Bureau of Statistics. Consumer price index, Australia; 2022 [cited 2022 Oct 10]. Available from: https://www.abs.gov.au/statistics/economy/price-indexes-and-inflation/consumer-price-index-australia/latest-release
- StataCorp. Stata Statistical Software: Release 17. College Station, TX: StataCorp LLC, 2021.
- National Health and Medical Research Council (NHMRC). National Statement on Ethical Conduct in Human Research 2007 (Updated 2018). 2018. Canberra: The National Health and Medical Research Council, The Australian Research Council, Universities Australia.
- Carville K, Lewin G, Newall N, et al. STAR: a consensus for skin tear classification. Primary Intention 2007;15:18–28.
- Carville K, Smith J. A report on the effectiveness of comprehensive wound assessment and documentation in the community. Primary Intention 2004;12:41–44, 46–48.
- Carville K, Howse L, Edmondson M, et al. Nurse practitioners and their use of low frequency ultrasound debridement. Wound Prac Res 2018;26:122–126.
- Meaume S, Kerihuel JC, Fromantin I, et al. Workload and prevalence of open wounds in the community: French Vulnus initiative. J Wound Care 2012;21:62 64, 66 passim. doi:10.12968/jowc.2012.21.2.62.
- Urwin S, Dumville JC, Sutton M, et al. Health service costs of treating venous leg ulcers in the UK: evidence from a cross-sectional survey based in the north west of England. BMJ Open 2022;12:e056790. doi:10.1136/bmjopen-2021-056790.
- Rayner R, Carville K, Leslie G, et al. A review of patient and skin characteristics associated with skin tears. J Wound Care 2016;24:406–414.
- Rayner R, Carville K, Leslie G, et al. Skin tear risk associated with aged care residents: a cross-sectional study. Wound Prac Res 2018;26:127–135.
- Mulligan S, Prentice J, Newall N, et al. WoundsWest Wound Prevalence Survey 2011. Statewide report overview. 2011. Perth, Western Australia: Ambulatory Care Services Department of Health.
- Strachan V, Prentice J, Newall N, et al. WoundsWest wound prevalence survey 2007. Statewide report overview. 2007. Perth, Western Australia: Ambulatory Care Services Department of Health, Western Australia.
- Pieper B, Templin T, Dobal M, et al. Home care nurses’ ratings of appropriateness of wound treatments and wound healing. J Wound Ostomy Continence Nurs 2002;29:20–28. doi:10.1067/mjw.2002.120871.
- Guest JF, Fuller GW, Vowden P. Cohort study evaluating the burden of wounds to the UK’s National Health Service in 2017/2018: update from 2012/2013. BMJ Open 2020;10:e045253. doi:10.1136/bmjopen-2020-045253.
- Whitlock E, Morcom J, Spurling G, et al. Wound care costs in general practice – a cross-sectional study. Aust Fam Physician 2014;43:143–146.
- Olsson M, Järbrink K, Divakar U, et al. The humanistic and economic burden of chronic wounds: a systematic review. Wound Repair Regen 2019;27:114–125. doi:10.1111/wrr.12683.
- Rayner RL. A review of the effectiveness of a nurse-led rural community wound clinic. Primary Intention 2007;15:130.
- Australian Medical Association Research and Reform Unit. Solutions to the chronic wound problem in Australia. 2022. Barton, ACT: Australian Medical Association.
- Munro G. Causes and consideration with chronic wounds: a narrative review of the evidence. Wound Prac Res 2017;25:88–97.
- Renner R, Erfurt-Berge C. Depression and quality of life in patients with chronic wounds: ways to measure their influence and their effect on daily life. Chronic Wound Care Manage Res 2017;4:143–151. doi:10.2147/CWCMR.S124917.
- Cheng Q, Gibb M, Graves N, et al. Cost-effectiveness analysis of guideline-based optimal care for venous leg ulcers in Australia. BMC Health Serv Res 2018;18:421. doi:10.1186/s12913-018-3234-3.
- Mauck KF, Asi N, Elraiyah TA, et al. Comparative systematic review and meta-analysis of compression modalities for the promotion of venous ulcer healing and reducing ulcer recurrence. J Vasc Surg 2014;60:71S–90S.e71–72. doi:10.1016/j.jvs.2014.04.060.
- Finlayson K, Wu M-L, Edwards HE. Identifying risk factors and protective factors for venous leg ulcer recurrence using a theoretical approach: a longitudinal study. Int J Nurs Stud 2015;52:1042–1051. doi:10.1016/j.ijnurstu.2015.02.016.
- Nelson EA, Bell-Syer SE. Compression for preventing recurrence of venous ulcers. Cochrane Database Syst Rev 2014;2014:Cd002303. doi:10.1002/14651858.CD002303.pub3.
- Nussbaum SR, Carter MJ, Fife CE, et al. An economic evaluation of the impact, cost, and medicare policy implications of chronic nonhealing wounds. Value Health 2018;21:27–32. doi:10.1016/j.jval.2017.07.007.
- Guest JF, Fuller GW, Vowden P. Costs and outcomes in evaluating management of unhealed surgical wounds in the community in clinical practice in the UK: a cohort study. BMJ Open 2018;8:e022591. doi:10.1136/bmjopen-2018-022591.
- Duckett S, Stobart A, Lin L. Not so universal: How to reduce out-of-pocket healthcare payments. 2022. Melbourne: Grattan Institute.
- Australian Institute of Health and Welfare (AIHW). Australia’s hospitals at a glance. 2022. Canberra: AIHW.
- Australian Institute of Health and Welfare (AIHW). The first year of COVID-19 in Australia: direct and indirect health effects. 2021. Canberra: AIHW.
- Copp T, Isautier JMJ, Nickel B, et al. COVID-19 challenges faced by general practitioners in Australia: a survey study conducted in March 2021. Aust J Prim Health 2021;27:357–363. doi:10.1071/py21165.
- Skatssoon J. How a pandemic changed home care. Australian Ageing Agenda. 2020 [cited 2022 Oct 24]. Available from: https://www.australianageingagenda.com.au/covid-19/how-a-pandemic-changed-home-care/



