Volume 31 Number 3
Challenges faced by people with diabetes‑related foot ulcers in attending hospital‑based high risk foot services: results of a consumer survey
Vanessa L Nube, Julie Zwarteveen, Georgina Frank, Sarah M Manewell, Molly L Cocks, Purnima Rao,
Stephen M Twigg, Jennifer A Alison
Keywords chronic wound, podiatry, diabetes-related foot ulcer, access, high risk foot service
For referencing Nube VL et al. Challenges faced by people with diabetes-related foot ulcers in attending hospital-based high risk foot services: results of a consumer survey. Wound Practice and Research 2023; 31(3):99-105.
DOI
https://doi.org/10.33235/wpr.31.3.99-105
Submitted 21 May 2023
Accepted 14 July 2023
Abstract
Introduction Diabetes-related foot ulcers (DFU) are optimally managed with a team approach to addressing infection, ischaemia, pressure offloading and sharp debridement. Treatment frequency is commonly every 1–2 weeks.
Aim To investigate the actual and preferred frequency of treatment of patients, and potential factors affecting treatment attendance including perceived benefits, mobility and mode of transport.
Method A convenience sample of patients attending urban or regional high risk foot services (HRFS) for treatment were invited to participate in the survey via a QR code, on paper or via phone. The study had ethics approval No X20-0550 2020/ETH03244.
Results A total of 60 participants from three centres completed the survey. Eight (13%) attended weekly, 28 (47%) every 2 weeks, and the remainder (40%) less often; 51 (85%) indicated they would attend weekly if this hastened healing; 33 (45%) had some level of difficulty in mobility impacting their ability to attend, with 11(18%) requiring a carer or family support for them to attend; most (84%) participants drove or were driven.
Conclusions Physical mobility deficits impact patients’ ability to attend for treatment, with the majority relying on private transport to attend appointments. Family support to enable attendance was common. These factors should be considered by providers and commissioners of services.
Introduction
Interdisciplinary high risk foot services (HRFS), which include podiatry, vascular and endocrinology interventions, are known to improve outcomes for people experiencing diabetes-related foot complications1,2. The aim of these coordinated interdisciplinary teams is to provide rapid access to optimal care to help avoid unnecessary hospital admissions and amputations3–7. Key tenets of care provided within the HRFS include management of infection, local wound care including sharp debridement, assessment and management of peripheral arterial disease, pressure offloading of the wound, patient education and management of their chronic disease8. Standards for care and clinical guidelines are outlined in state, national and international documents which emphasise the need for the model of care to include rapid access and on-site teams3,4,8,9. Interdisciplinary teams are advantageous due to the emphasis on coordination and communication which may minimise the number of visits to health facilities by bringing together clinicians from different disciplines for joint consultation.
In a health environment which is seeking to deliver more care outside the hospital facilities and through telehealth, particularly in the COVID‑19 era10, the need for patients to attend face-to-face appointments to receive sharp debridement and detailed wound assessment remains necessary. From the clinicians’ perspective, the recommended frequency of sharp debridement is a key determinant of how often patients with diabetes-related foot ulcers (DFU) attend a HRFS for care, with visit and debridement frequency being virtually synonymous11. Sharp debridement is standard care in the management of DFU, typically undertaken serially to facilitate healing12–15, with weekly or second-weekly intervals representing the usual frequency when there is adequate blood flow for healing11,16. The procedure is routinely performed in the outpatient setting of the HRFS which can satisfy the requirements for infection control as well as the safety and comfort of both patient and clinician. While there is a lack of data on patients’ reasons for attending or non-attendance to HRFS, a systematic review on reasons why people with diabetes could not attend diabetes education programs identified lack of transport, distance and parking, duration of appointment and other commitments, along with physical disabilities and financial reasons, as barriers to attendance. Patients’ perception of the benefits of the consultation also influenced their decision of whether or not to attend17.
Given the high rate of co-morbidities, depressive symptoms and poor physical functioning in people with DFU18–21, the capacity of some patients to physically attend a hospital service may be a limiting factor and have a negative impact on the quality of life for some22. Patients’ preferences regarding treatment frequency, the perceived benefits, impact of mobility and how they travel to appointments are potentially meaningful areas to investigate.
The aims of the study were to: a) investigate the actual and the preferred frequency of attendance for treatment, including sharp debridement, for patients with DFU; b) understand what patients with DFU value about their clinic attendance at the HRFS; c) determine the extent to which patient-reported mobility may affect attendance; d) document the mode of transport used, duration of time spent on their clinic visit, and any out-of-pocket costs related to attendance.
Methods
A survey was developed de novo by the investigators and tested by two consumers whose input was incorporated. The study was approved by the Human Research and Ethics Committee of the lead site, with local site-specific governance approval at each of the three participating services. A patient information sheet was provided to all potential participants. Consent was enacted when the participant agreed to answer the survey questions. The three sites included two hospitals based in a capital city and one regional city hospital. Their models of care were consistent with the state-wide standards for HRFS3. All services were located within a hospital, non-admitted patient setting coordinated by a senior podiatrist and with interdisciplinary team consultations with relevant disciplines.
The estimated clinic population was n=150 patients, of which 60 participants was considered as a reasonable sample of eligible clinic patients. A convenience sample was used, with clinicians being requested to recruit to a target n=20 participants for each site. Inclusion criteria were people with DFU of minimum 4 weeks duration, attending one of three HRFS for wound management. Potential participants were given an information sheet with a QR code linked to the online survey. Participants could alternatively complete a paper version, have the treating clinician document their responses, or request that the investigator phone them to complete the survey by phone. This choice was provided to improve the uptake of the survey and eliminate the potential barriers of poor literacy, use of technology or a preference not to provide responses to their treating clinician. All responses were entered into a password protected electronic database, Research Electronic Data Capture (REDCap)23, which was generated for the study and open to the site investigators.
Survey questions were predominantly multiple choice, with the exception of home suburb, distance walked and time taken to attend location of care, and cost of parking. One multiple choice question, “How important do you believe these are to you?”, asked participants to rate the perceived importance using a 3-point Likert-style scale from ‘not important’ to ‘very important’ (and including ‘not applicable’) for the following: debriding with a scalpel (cleaning) of my foot ulcer to remove dead skin, slough etc; changing the dressing on my foot ulcer; offloading (special shoe, boot, cast or padding to protect my foot); getting a doctor to treat my infection; getting a doctor to treat my diabetes; getting a diabetes nurse educator to help manage my diabetes; learning about my feet and how to care for them. Open-ended questions asked why (if applicable) participants preferred to attend the HRFS more or less often, and lastly a question asked participants to write about the benefits and challenges of attending for treatment of a foot ulcer. The questions regarding whether participants would wish to attend more frequently if this meant their ulcer might heal faster was posed as follows:
About half (50%) of foot ulcers heal within 3 months. Whether a foot ulcer heals and how long it takes, depends on a number of factors. These can include how severe the ulcer is and how long it has been present, circulation and treatment effectiveness. If attending the foot clinic every week meant that you were likely to heal 15% faster, would you attend more often?
The multiple-choice answers were: yes, no and “I already attend every week (or more often)”.
Results
Participant demographic data
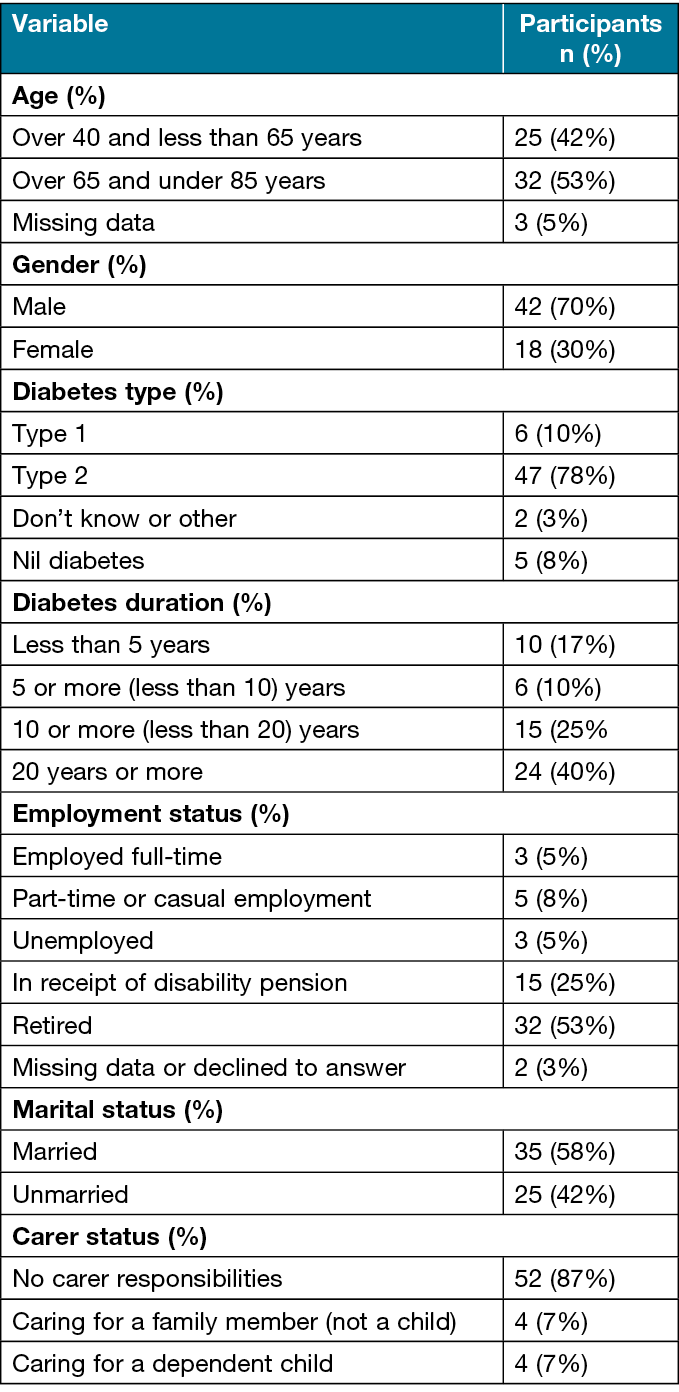
During a 10-week period (July to October 2021) clinicians approached patients to participate in the survey. Since this was during the COVID-19 pandemic, the participating HRFS followed state and national guidance with regards to hospital appointments (ref DFA). All face-to-face consultations were maintained for all initial and most follow-up consultations, with follow-up consultations replaced with telehealth where clinically indicated and deemed safe24. A total of 60 participants completed the survey from a possible 462 people who attended the services during the data collection period. Demographics for participants is given in Table 1. All participants were between 40 and 65 years of age and only eight (13%) were employed.
Table 1. Survey participant demographics
Frequency of attendance: actual and preferred
Frequency of attendance was every second week for almost half the participants (n=28). Table 2 indicates the frequency of attendance reported by respondents and their preference for how frequently they preferred to attend. A total of 12 of the 15 reporting 4-weekly attendance were from the regional city HRFS. When asked whether they would prefer to attend weekly if this were to hasten healing time by 15%, 51 (85%) indicated they would attend more often.
Table 2. Patient-reported visit frequency and preferred frequency

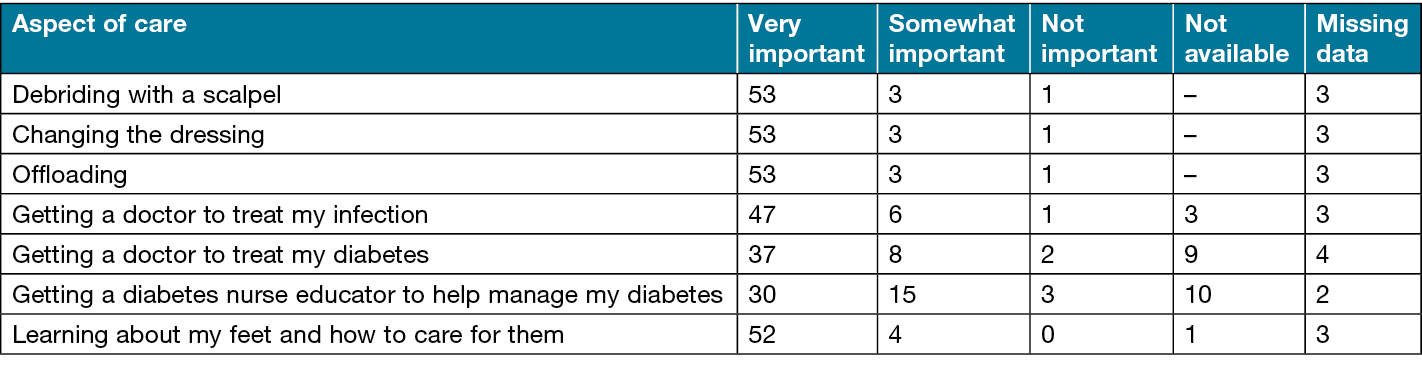
What patients valued about their consultation
Table 3 summarises the findings of the value to participants of attending the HRFS. Receipt of sharp debridement, dressing changes, pressure offloading and the education they received on foot self-care were the most highly rated. Not all participants were aware of or valued diabetes management as part of the service. It should be noted that five people who did not have diabetes completed the survey.
Table 3. Participant responses to how they rated the importance of different aspects of care within the HRFS
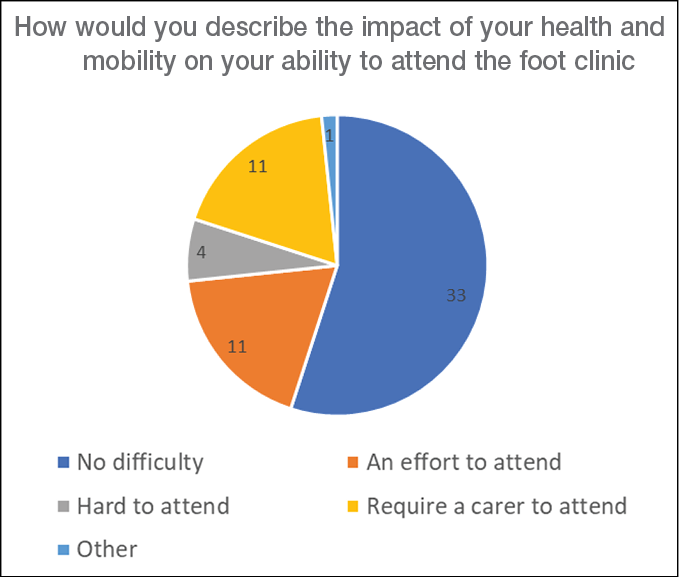
How participants perceived the impact of health and mobility on ability to attend the clinic
Around half of the participants (n=33/60) reported being “well and mobile enough to attend without difficulty”; 11 (18%) reported that they required the assistance of a family member or carer to attend the appointments (Figure 1).
Figure 1. Participant-reported impact of health and mobility on clinic attendance
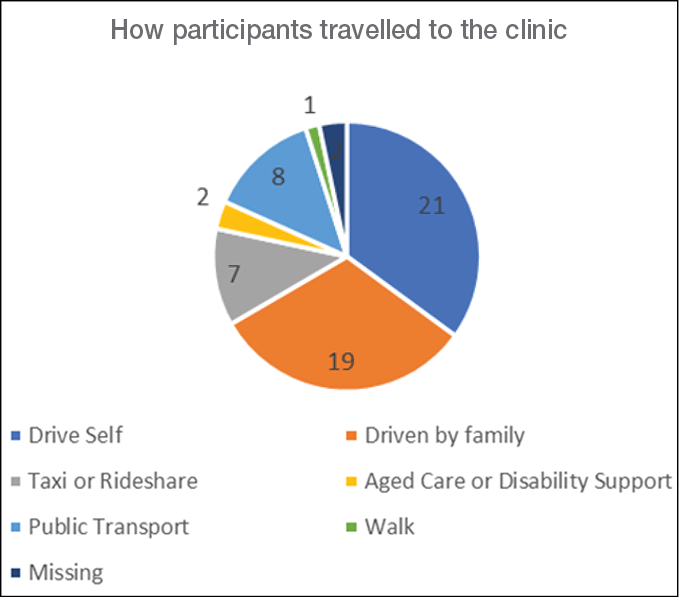
How participants travelled to the clinic
Eight (13%) participants travelled by public transport to the HRFS and reported walking an average 462 metres; seven (12%) travelled by ride-share or taxi, walking an average of 218 metres; 21 (35%) drove themselves by car, walking an average of 308 metres; 19 (32%) were driven by a family member, walking an average of 276 metres; and one walked 2km from their home to the service. Five participants used a wheelchair or scooter instead of walking from their main mode of transport into the clinic. One participant used Commonwealth Aged Care funded transport and one used their National Disability Insurance-funded support worker (Figure 2).
Figure 2. How participants travelled to their clinic appointments
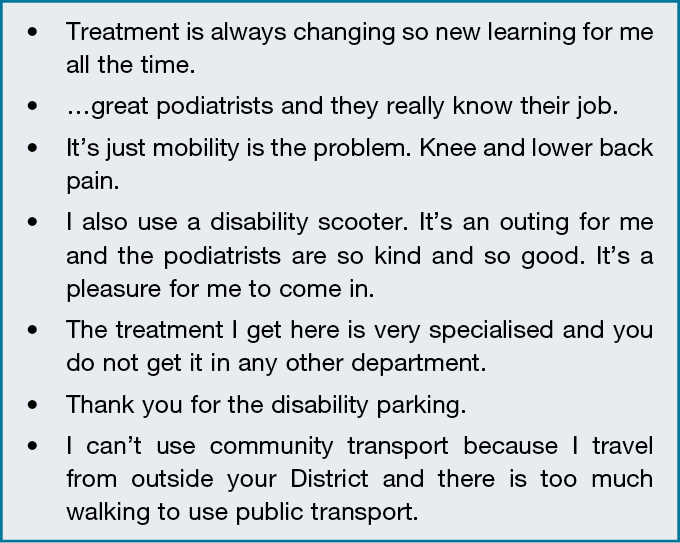
The median time participants spent on their overall visit (travel and treatment time) was 2 hours; this was the same for all centres. Those attending the large capital city centres lived predominantly within a 10km radius of the hospital, with three (8%) travelling greater than 30km. The median distance from the participants’ home to the regional city hospital was 19km and six (30%) travelled over 30km. In addition, a total of 13 participants (22%) were aware of the parking fees they had paid, with an average spend of $13 per visit. Additional comments from participants are shown in Figure 3.
Figure 3. Comments from participants
Discussion
This consumer survey found that most participants rated debridement, dressing changes, pressure offloading, management of infection, and learning about caring for their feet as very important. Management of diabetes was somewhat or very important for 82% of those with diabetes. Second-weekly attendance for treatment was most common, and weekly or second-weekly visits were preferred, which is consistent with other reports11,16. There was an indication that some participants attending less often would attend weekly if this would hasten healing by as little as 15%, suggesting this is a meaningful difference for at least some participants. However, as this question was potentially leading, the result is not conclusive.
One quarter of the participants attended every 4 weeks or less often, which may not represent standard care14. It is not known to what extent treatment every 4 weeks is based on clinician recommendation, time constraints of the service (appointments unavailable), or due to patient factors but a similar number of participants also reported 4-weekly care as their preference. In previous qualitative research, reliance on family for travel to appointments, the indirect treatment costs which include travel and parking, as well as the challenges of maintaining employment with frequent visits, have been described as having negative effects on the quality of life for people with DFU25–27.
While there is observation data and indirect evidence that more frequent debridement is beneficial in the management of DFU16,27–30, the one prospective study of sharp debridement, which controlled for visit frequency (weekly), found weekly and second-weekly sharp debridement to have similar outcomes at 12 weeks28. There was also a high drop-out rate, suggesting that the regimen of weekly visits was not acceptable or feasible for all participants. In practice, some wounds are likely to require more aggressive debridement than others due to the presence of infection, callus or more non-viable tissue11,13. The patient’s capacity and desire to attend as well as clinic resources will also impact frequency of attendance11.
A key finding of the current survey was the high number of participants who relied on a private vehicle (car) to attend the HRFS, with few using other means such as public transport. Private car was the main modality used by 84% (n=50) of respondents, and 100% of those attending the regional city hospital. Furthermore, the driving responsibility was conferred to family members of 33% of respondents.
Loss of lower extremity function for people with DFU and the restriction to mobility as recommended treatment are known issues for those experiencing foot complications20–22. Almost half of the participants in our survey reported having physical limitation affecting attendance, and travelling by car was associated with less walking, particularly if someone else drove them to the appointment. Only two respondents indicated they used age and disability supports to travel to the clinic. Reliance on social supports for transport was also identified as a key theme in small qualitative study by Palaya et al (2018)27. Our survey data further highlights the needs of this patient group with respect to transport support. This should be further explored to determine why participants, many of whom would be eligible for this assistance, were not using these supports.
In terms of access, these results suggest that not having the use of a car is a limitation for those needing HRFS care. In our survey, a quarter of study participants were in receipt of a disability pension and only three reported being in full-time employment. Both the cost of running a car (not reported) and parking costs are potential barriers to those on low incomes who would already be burdened with costs of treatment29. While there can be many influencing factors determining ease of access to services and how often, research on geographical access to healthcare services shows that distance and transport availability are important determinants of healthcare utilisation, with people in disadvantaged groups likely to rely on public transport30,31. The geographical distribution of current HRFS means that many patients are not within close proximity32,33. Where clinics exist, consideration as to distance from car parking and extending clinic hours to accommodate patients who rely on working family members to drive them to appointments may warrant consideration.
International data show that timely presentation to specialised services is associated with better outcomes for people with DFU34. However, Australian data suggests a significant proportion of patients with DFU admitted to hospital have not accessed specialised a HRFS prior to being admitted. Manewell et al35 reported that 43% of patients admitted for DFU were not known to have attended the HRFS, and Plusch et al36 found 75% of people admitted for diabetes foot infection had not accessed the HRFS. These represent missed opportunities to avoid admissions and amputations. It is not known whether physical access or transport were barriers in these instances but understanding and mitigating any impediments to access are likely to improve healing outcomes.
These survey results highlight a potential problem with physical accessibility to services and raises the question as to how accessible the services are for people with chronic illness and poor mobility who are without family, aged care or disability supports to enable attendance.
Limitations of this study is the use of non-random sampling and the higher-than-expected patient clinic numbers which meant the sample size was proportionally small. Both factors limit the generalisability of the results. There is an inherent bias towards those participants who were able to attend the HRFS. Patients with DFU who did not attend or who rarely attended were not captured in the survey. Some bias toward valuing different aspects of care is also likely. While the participants’ identifying information was not included in the responses, the majority chose to complete the survey via the phone or during their treatment visit with the clinicians, hence they were not fully anonymous. The option to complete electronically via a QR code link to the survey would have provided anonymity but was not preferred by participants, and only one participant elected to complete the survey this way. Provision of phone or treatment visit options for completing the survey enabled participation for those with impaired vision, reduced cognition, low literacy and anyone without the access or capacity to use a smart phone or computer. However, we acknowledge that participants would have been disinclined to respond in a way which was negative towards the service while in the presence of their treating clinician. Results of the question “How important do you believe these are to you?” should be interpreted with respect to the likelihood of bias.
Other variables were also not explored in this study such as unavailability of appointments, time constraints for people working or with caring responsibilities, cultural safety of the HRFS for the culturally diverse patients who attend the clinics, or preferences towards particular provider(s). Moreover, while the survey was used across three HRFS sites in the current research, it has not been validated or tested with regard to reproducibility.
Lastly, our study enrolment included five respondents (across the sites), who were being treated for chronic foot ulcers related to neurological or vascular complications but who did not have diabetes. The data from these participants were retained in the study as their non-diabetes foot care requirements were closely aligned to those of people with DFU, hence their admission under the care of the HRFS for interdisciplinary management, including debridement by a podiatrist.
Conclusions
Attending specialised interdisciplinary teams for non-admitted care of foot ulcers has been shown to help reduce the risk of hospitalisation and to improve clinical outcomes; however, in this survey, a high proportion of participants had challenges in mobility impacting their capacity to attend and used travel by private vehicle to attend, with a significant number being reliant on others to drive them. While telehealth in DFU care is becoming more commonplace post the COVID era, some aspects of care such as sharp debridement need in-person HRFS specialist care. Further research to understand the reasons for non-attendance (or infrequent attendance), potential solutions and the impact on admissions and healing outcomes is needed.
A recommendation from these data is that HRFS providers aim to mitigate potential barriers to access for new and existing clients and seek to draw on supports which may be available to patients to help attendance. Government commissioners of HRFS should consider the clients for whom they are targeted. Distance required for patients to travel to services, proximity of parking, availability of drop-off bays, public transport access and opening hours should be considered, with the aim of maximising the reach and utilisation of services which can minimise hospitalisation and amputations.
Conflict of interest
The authors declare no conflicts of interest.
Ethics statement
The study was approved by the Royal Prince Alfred Hospital Research Ethics Committee (2020/ETH03244) with local site governance approval from Royal Prince Alfred, Concord and John Hunter Hospitals.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. In-kind support was given by the hospitals of the participating authors.
Author contribution
VN designed the study, prepared the ethics submission, collected data, analysed data, wrote the paper, consulted with other authors for their review and input into the final submission, prepared the submission and is responsible for the integrity of the work. JZ was consulted and agreed to the design of the study, was responsible for conduct of the study at John Hunter Hospital, contributed substantially to the acquisition of the data, reviewed and approved the final version of the work, and shares responsibility for the integrity of the work. GF was consulted and agreed to the design of the study, was responsible for conduct of the study at Royal Prince Alfred and Concord Hospitals, collected data, reviewed the paper and shares responsibility for the integrity of the work. SM, MC and PR collected data, reviewed the submission, approved the final submission and share responsibility of the integrity of the work. ST and JA provided academic oversight as academic supervisors of VN (PhD candidate) and had input into the research design, JA is the coordinator PI on the ethics submission, ST and JA contributed to the critical review of the manuscript, approved the final submission and share responsibility for integrity of the work.
Author(s)
Vanessa L Nube1,2*, Julie Zwarteveen3, Georgina Frank1,Sarah M Manewell1, Molly L Cocks4, Purnima Rao1,4, Stephen M Twigg4–6, Jennifer A Alison6,7
1Department of Podiatry, Sydney Local Health District, Missenden Road, Camperdown, NSW, Australia
2The University of Sydney, Faculty of Medicine and Health, NSW, Australia
3Department of Podiatry, Hunter New England District, Community and Aged Care Services, Greater Newcastle Sector, Newcastle, NSW, Australia
4Diabetes Centre Royal Prince Alfred Hospital, Camperdown, NSW, Australia
5Diabetes Centre, Department of Endocrinology, Royal Prince Alfred Hospital, Camperdown, NSW, Australia
University of Sydney, NSW Australia
6The Faculty of Medicine and Health, Sydney Medical School, University of Sydney, NSW Australia
7Allied Health Professorial Unit, Sydney Local Health District, Camperdown, NSW, Australia
*Corresponding author email vanessa.nube@health.nsw.gov.au
References
- Albright RH, Manohar NB, Murillo JF, Kengne LAM, Delgado-Hurtado JJ, Diamond ML, et al. Effectiveness of multidisciplinary care teams in reducing major amputation rate in adults with diabetes: a systematic review & meta-analysis. Diabetes Res Clin Pract 2020;161:107996.
- Blanchette V, Brousseau-Foley M, Cloutier L. Effect of contact with podiatry in a team approach context on diabetic foot ulcer and lower extremity amputation: systematic review and meta-analysis. J Foot Ankle Res 2020;13(1):15.
- Endocrine Network of the Agency for Clinical Innovation. Standards for high risk foot services in NSW. In: NSW Agency for Clinical Innovation, editor. Sydney: ACI; 2011.
- National Association of Diabetes Centres. NADC collaborative interdisciplinary diabetes high risk foot service standards version 2. Melbourne: NADC; 2022.
- Joret MO, Osman K, Dean A, Cao C, van der Werf B, Bhamidipaty V. Multidisciplinary clinics reduce treatment costs and improve patient outcomes in diabetic foot disease. J Vasc Surg 2019;70(3):806–14.
- Quinlivan E, Jones S, Causby R, Brown D. Reduction of amputation rates in multidisciplinary foot clinics – a systematic review. Wound Pract Res 2014;22(3):155–62.
- Paisey RB, Abbott A, Paisey CF, Walker D, Birch R, Bowen B, et al. Diabetic foot ulcer incidence and survival with improved diabetic foot services: an 18-year study. Diabetic Med 2019;36(11):1424–30.
- Schaper NC, van Netten JJ, Apelqvist J, Bus SA, Fitridge R, Game F, et al. Practical guidelines on the prevention and management of diabetes-related foot disease (IWGDF 2023 update). Diabetes Metab Res Rev 2023:e3657.
- Boulton AJM, Armstrong DG, Kirsner RS, Attinger CE, Lavery LA, Lipsky BA, et al. Diagnosis and management of diabetic foot complications. Compendia 2018;2018(2).
- Demeke HB, Pao LZ, Clark H, Romero L, Neri A, Shah R, et al. Telehealth practice among health centers during the COVID‑19 pandemic – United States, July 11–17, 2020. Morbid Mortal Weekly Rep 2020;69(50):1902–5.
- Nube VL, Alison JA, Twigg SM. Frequency of sharp wound debridement in the management of diabetes-related foot ulcers: exploring current practice. J Foot Ankle Res 2021;14(1):52-.
- Lavery LA, Davis KE, Berriman SJ, Braun L, Nichols A, Kim PJ, et al. WHS guidelines update: diabetic foot ulcer treatment guidelines. Wound Repair Regen 2016;24(1):112–26.
- Schultz G, Bjarnsholt T, James GA, Leaper DJ, McBain AJ, Malone M, et al. Consensus guidelines for the identification and treatment of biofilms in chronic nonhealing wounds. Wound Repair Regen 2017;25(5):744–57.
- Chen P, Carville K, Swanson T, Lazzarini PA, Charles J, Cheney J, et al. Australian guideline on wound healing interventions to enhance healing of foot ulcers: part of the 2021 Australian evidence-based guidelines for diabetes related foot disease; version 1.0. J Foot Ankle Res 2022;15(1):40.
- Chen P, Vilorio NC, Dhatariya K, Jeffcoate W, Lobmann R, McIntosh C, et al. Guidelines on interventions to enhance healing of foot ulcers in people with diabetes (IWGDF 2023 update). Diabetes Metab Res Rev 2023:e3644.
- Carter MJ, Fife CE. Clinic visit frequency in wound care matters: data from the US wound registry. J Wound Care 2017;26(Sup1):S4-S10.
- Horigan G, Davies M, Findlay-White F, Chaney D, Coates V. Reasons why patients referred to diabetes education programmes choose not to attend: a systematic review. Diabet Med 2017;34(1):14–26.
- Pearson S, Nash T, Ireland V. Depression symptoms in people with diabetes attending outpatient podiatry clinics for the treatment of foot ulcers. J Foot Ankle Res 2014;7(1):47-.
- Saluja S, Anderson SG, Hambleton I, Shoo H, Livingston M, Jude EB, et al. Foot ulceration and its association with mortality in diabetes mellitus: a meta-analysis. Diabet Med 2020;37(2):211–8.
- Iseli RK, Lee EK, Lewis E, Duncan G, Maier AB. Foot disease and physical function in older adults: a systematic review and meta-analysis. Aust J Age 2021;40(1):35–47.
- Johnson NA, Barwick AL, Searle A, Spink MJ, Twigg SM, Chuter VH. Self-reported physical activity in community-dwelling adults with diabetes and its association with diabetes complications. J Diabetes Complications 2019;33(1):33–8.
- Vileikyte L. Diabetic foot ulcers: a quality of life issue. Diabetes/Metab Res Rev 2001;17(4):246–9.
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42(2):377–81.
- Diabetes Feet Australia and Australian Diabetes Society. Australian clinical triage guide: for people with diabetes-related foot disease during the COVID‑19 pandemic; 2020.
- Brod M. Quality of life issues in patients with diabetes and lower extremity ulcers: patients and care givers. Qual Life Res 1998;7(4):365–72.
- Ong EKM, Fryer C, Graham K, Causby RS. Investigating the experience of receiving podiatry care in a tertiary care hospital clinic for people with diabetes related foot ulcers. J Foot Ankle Res 2022;15(1):50.
- Palaya J, Pearson S, Nash T. Perception of social support in individuals living with a diabetic foot: a qualitative study. Diabetes Res Clin Pract 2018;146:267–77.
- Nube VL, White JM, Brewer K, Veldhoen D, Meler C, Frank G, et al. A randomized trial comparing weekly with every second week sharp debridement in people with diabetes-related foot ulcers shows similar healing outcomes: potential benefit to resource utilization. Diabetes Care 2021;44(12):e203-e5.
- Kapp S, Santamaria N. The financial and quality-of-life cost to patients living with a chronic wound in the community. Int Wound J 2017;14(6):1108–19.
- Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Comm Health 2013;38(5):976–93.
- Cui B, Boisjoly G, Wasfi R, Orpana H, Manaugh K, Buliung R, et al. Spatial access by public transport and likelihood of healthcare consultations at hospitals. Transport Res Rec 2020;2674(12):188–98.
- Agency for Clinical Innovation NSW. High risk foot service directory Sydney: NSW Health. Available from: https://aci.health.nsw.gov.au/resources/endocrine/service-directory/high-risk-foot.
- National Association of Diabetes Centres. NADC Collaborative Interdisciplinary Diabetes HHRFS Accreditation: NADC; 2023. Available from: https://nadc.net.au/hrfs-accreditation/.
- Wise, J. (2016). Early referral for foot ulcers is vital, finds audit of diabetes care. BMJ (Online), 352, i1820–i1820. https://doi.org/10.1136/bmj.i1820
- Manewell, S. M., Aitken, S. J., Nube, V. L., Crawford, A. M., Constantino, M. I., Twigg, S. M., Menz, H. B., Sherrington, C., & Paul, S. S. (2022). Length of stay and readmissions for people with diabetes-related foot ulceration admit-ted to two public tertiary referral hospitals in Australia. Wound Practice & Research, 30(2), 82–90. https://doi.org/10.33235/wpr.30.2.82-90
- Plusch, D., Penkala, S., Dickson, H. G., & Malone, M. (2015). Primary care referral to multidisciplinary high risk foot services - too few, too late. Journal of Foot and Ankle Research, 8(1), 62–62. https://doi.org/10.1186/s13047-015-0120-7



