Volume 31 Number 3
Developing a social media-based self-management program for the prevention of diabetes-related foot ulceration in persons with diabetes: protocol steps
Helen N Obilor, Heather Ibbetson, Tom Weisz, Olena Veryha, Mariam Botros, Rosemary Wilson, Joan Tranmer, Kevin Woo
Keywords prevention, social media, diabetes-related foot ulceration, self-management education, self-management support
For referencing Obilor HN et al. Developing a social media-based self-management program for the prevention of diabetes-related foot ulceration in persons with diabetes: protocol steps. Wound Practice and Research 2023; 31(3):106-119.
DOI
https://doi.org/10.33235/wpr.31.3.106-119
Submitted 24 September 2022
Accepted 11 July 2023
Abstract
Foot ulceration continues to persist as a serious health threat among people with diabetes (PWD) due to multiple factors that include poor adherence to recommended foot self-care activities and limited access to self-management support. Given the ongoing adaptation and use of telehealth to improve patient access to health programs, there is a need to explore whether the rapidly growing social media network can engage PWD in self-management strategies to reduce their risk of diabetes-related complications such as diabetes-related foot ulceration (DFU). In this paper, we describe the development and implementation of the Diabetic Foot Care Group (DFCG), a social media-based self-management support intervention for PWD to prevent DFU. Using a co-design approach, we actively engaged both healthcare professionals (HCP) and PWD in the development and implementation activities. The DFCG comprises of four components – patient education, peer support, social interaction and active engagement. The DFCG was implemented through a private Facebook group platform. The posts’ content was patient-centred and structured to enhance self-care confidence and optimise care outcomes among PWD. In summary, social media platforms are feasible alternatives that HCP could utilise to provide continuous self-management education and support (SMES) for PWD to prevent DFU proactively.
Introduction
Globally, diabetes-related foot ulceration (DFU) is a common, complex and costly complication of diabetes associated with significant disability, poor quality of life and high mortality rates1,2. The lifetime risk of DFU in people with diabetes (PWD) is 20–34%3. Due to complications of DFU, the relative risk of lower limb amputations between PWD and those without diabetes ranges from 7.4–41.34, with Canada having a relative risk of 28.95.
Comprehensive, consistent and accessible patient education is critical to reducing the risk of DFU and empowering PWD to engage in adequate foot self-care activities6. However, there is a disparity in access to quality health promotion programs for PWD, potentially compromising their wellbeing and ability to control diabetic complications, including foot ulcers7,8. The COVID‑19 pandemic has further widened the disparity in access to health programs9. During the pandemic, PWD, particularly those with DFU, suffered10. The COVID‑19 control policies, such as the lockdown and social distancing measures, resulted in appointment cancellations, unavailability of operating rooms, delayed treatment of minor foot problems/referral, and greater possibilities of adverse diabetic-related health outcomes9–11.
Social media platforms offer some benefits that could be leveraged to improve access to foot self-management programs and reduce the risk for DFU among PWD. Over 3.6 billion people worldwide use social media for their day-to-day activities and interactions12. Social media enables people to form communities, share information and communicate virtually with other users in real-time13. In response to the COVID‑19 pandemic, many health programs transitioned to telehealth or virtual consultations using digital devices such as telephone and online platforms. However, the possibility of the current social networking platforms for delivering standard health education programs to PWD for DFU prevention is unclear. A major concern limiting the use of social media by healthcare professionals (HCP) for patient education is the high potential for misinformation14,15 and the threat to users’ privacy16.
The need for a diabetic foot care-focused social media program that is evidence-based, reliable and poses reduced privacy risk informed the creation of a social media-based DFU prevention program tagged the Diabetic Foot Care Group (DFCG). The DFCG was created as an intervention arm of a project that examined the feasibility of social media as an alternative method to engage PWD in the prevention of DFU17. The goal of the DFCG was to promote PWD access to continuous self-management education and support (SMES), with the intention to increase PWD confidence to engage in foot self-care and prevent DFU. However, most available education programs in the literature lack a description of the theoretical underpinnings and steps taken for their development/implementation. In this paper, the theoretical basis and process employed in the development and implementation of the DFCG will be presented.
The conceptual framework for the study
The development of the DFCG was guided by Bandura’s social cognitive theory (SCT). SCT posits that human behaviour occurs in a triadic pattern in which behaviour, personal attributes and environmental factors are reciprocally determining each other18. The integrity of the triadic pattern is maintained through multiple interacting cognitive factors that include self-efficacy. Self-efficacy is a regulatory factor defined as the confidence to execute the specific action required for a given behaviour. Bandura stipulates self-mastery, vicarious experiences, social persuasion and interpretation of biopsychological state as fundamental sources of self-efficacy vital for positive behaviour change18.
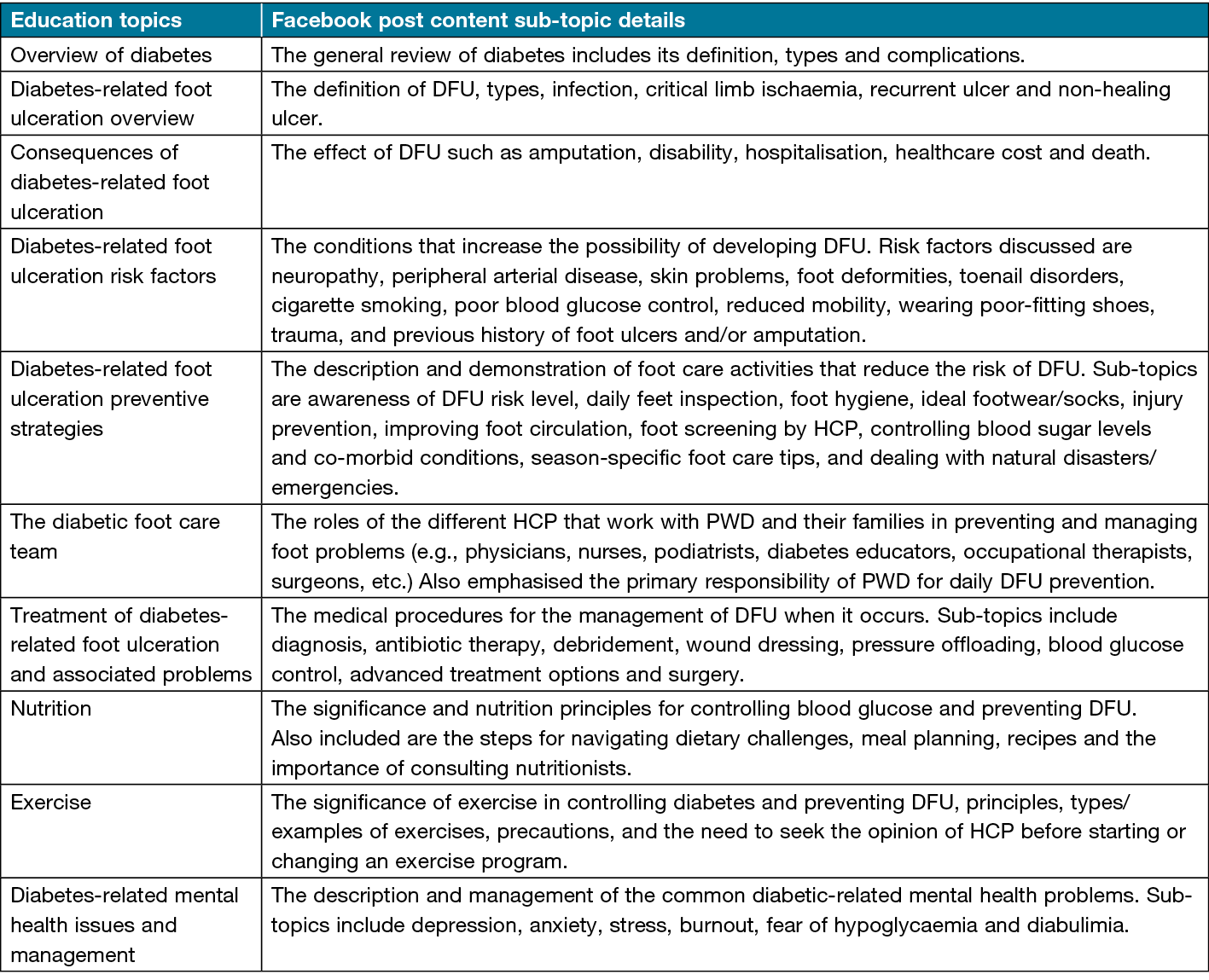
Based on Bandura’s self-efficacy sources, the DFCG comprised education, peer support, social interaction and active engagement (Figure 1). The patient education component aligned with biopsychological interpretation for PWD to holistically appraise health status and prevent complications. Peer support builds on the vicarious experience to allow PWD to learn and compare their experiences with peers for self-motivation. Furthermore, social interaction is based on social persuasion to strengthen one’s belief in making efforts toward achieving success. Lastly, active engagement is based on skill mastery to drive group members’ capacity to achieve learning goals and overcome obstacles.
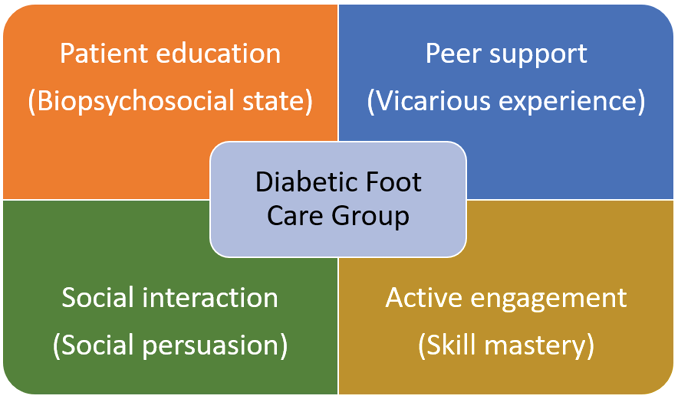
Figure 1. The DFCG components adapted from SCT’s principle of self-efficacy sources
Methods
The development of the content and structure of the DFCG’s components followed a participatory method based on the Boyd et al.19 co-design framework that involves the active involvement of partners, including patients, in the development of health programs. In compliance with the co-design principles (engage, plan, explore, develop, decide and change)19, the DFCG development involved six processes – partners’ engagement, review of literature, deciding on the social media platform, compilation of posts/links to community resources, content validation, and revision based on group members’ feedback (Figure 2).
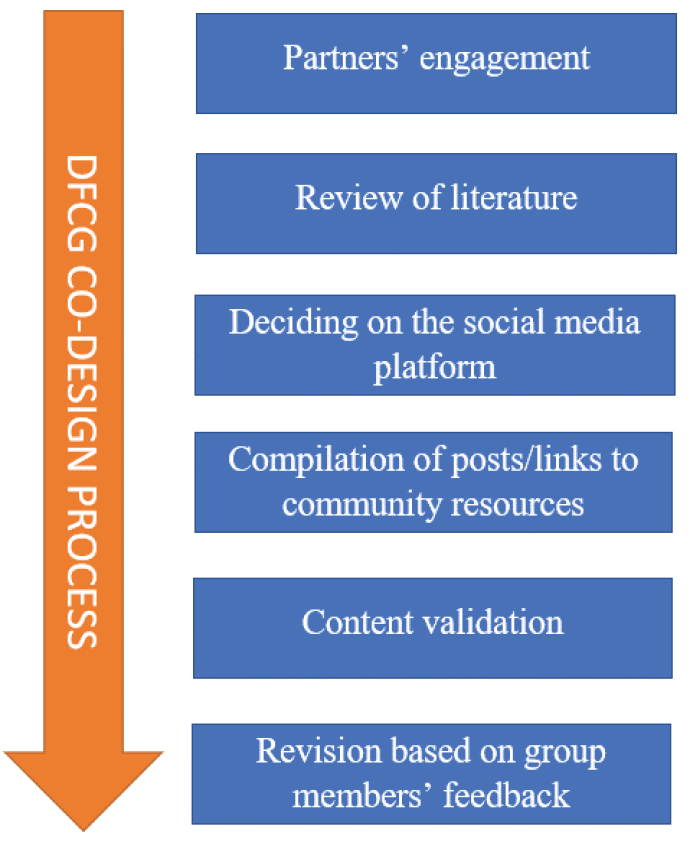
Figure 2. The DFCG development process
Partners’ engagement
The study setting was Canada. Researchers at Queen’s University collaborated with Wounds Canada to develop the DFCG. Wounds Canada is a non-governmental organisation dedicated to the advancement of wound management and prevention in Canada. A team that comprised two registered nurses (HNO and KW), one podiatrist (MB), two content creators (OV and HI), and a patient (TW) with diabetes was set up. The team’s goal was to create a social media group platform and generate evidence-based content to help PWD learn and become motivated to practise adequate foot self-care activities. The team members were selected based on their knowledge, skill and experience in diabetes foot management. The team met virtually every 2–4 weeks from April 2020 to August 2021 to brainstorm, review development activities and make decisions.
Review of literature
Current clinical guidelines for the prevention and management of DFU have emphasised the significance of continuous patient education to prevent DFU to improve diabetic foot-related outcomes6,20. However, there is a lack of direction on how patient education programs should be implemented in real-life settings. To address this knowledge gap, the decision was made to include an integrated review of the literature to identify the standard patient education topics and PWD preferences regarding the content delivered through information and communication technological (ICT) tools to guide the development of the DFCG.
Inclusion criteria
The inclusion criteria for the review followed the Joanna Briggs Institute’s PCC framework for scoping review - Population, Concept and Context21. The population considered were adult patients diagnosed with type I or II diabetes without any active DFU at recruitment. The concepts of interest explored were structured diabetic foot-based self-management programs and ICT tools. ICT tools were operationalised as hardware and software devices utilised by HCP in the identified diabetic foot self-management programs to educate and support PWD to prevent DFU. The context in this review was global, and studies conducted in all countries and healthcare settings were included. To ensure that the full breadth of literature was covered, this review considered studies of any research design that evaluated diabetic foot-based self-management programs involving ICT tool(s) with the intent to improve PWD foot self-care practices and prevent DFU. Due to resource constraints, grey literature and non-English studies were excluded.
Search strategy
Relevant research articles were identified through a systematic search in MEDLINE, Embase, PsycINFO and CINAHL databases. The search terms were developed in consultation with an expert librarian. A combination of subject headings, keywords and text words was used to search for articles published from inception to May 2020. The reference list of selected studies was manually searched for articles possibly not captured during the search. Last, an electronic search in Google and Google Scholar was undertaken to identify additional studies.
Search results
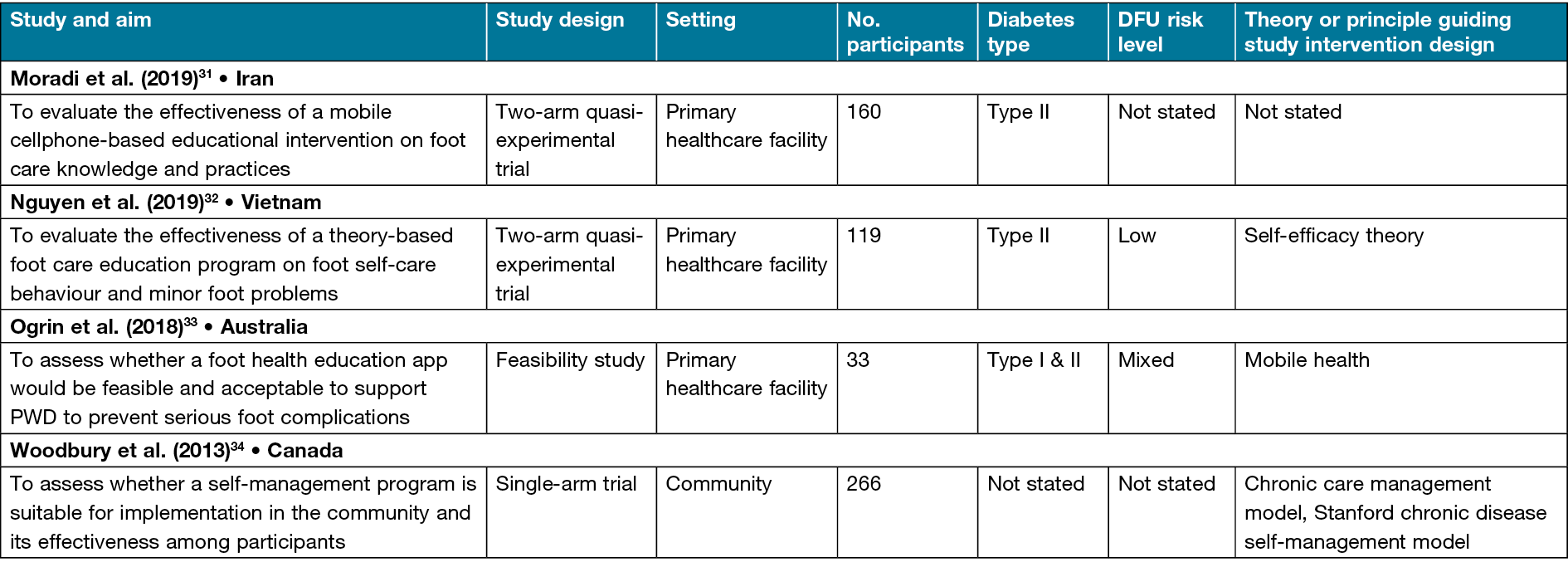
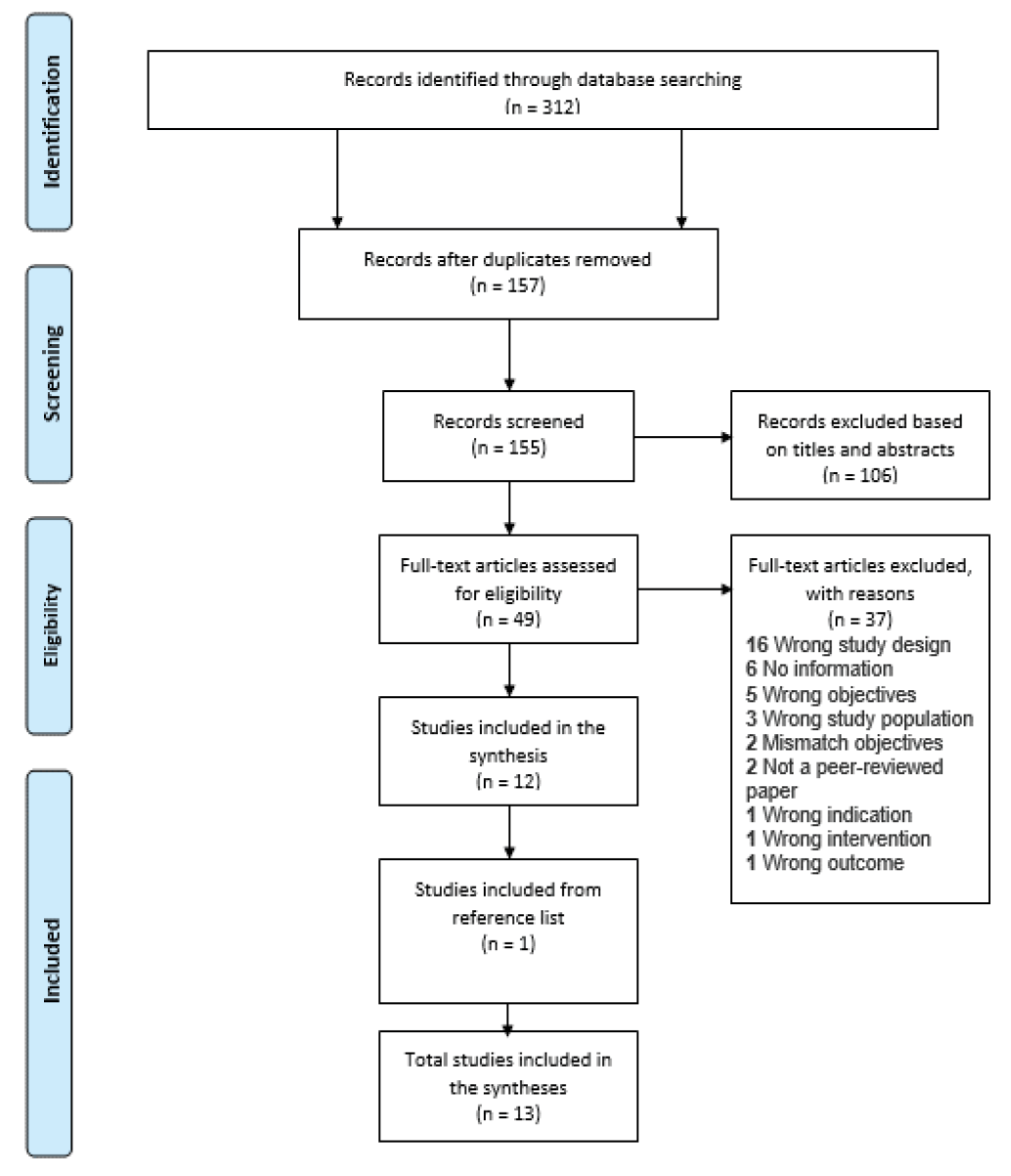
The search results were uploaded into CovidenceTM (a web-based software program for streamlining the production of reviews). The database search yielded a total of 312 citations (see Appendix 1 for the PRISMA flowchart). CovidenceTM removed 157 duplicates and 106 articles were excluded during the title and abstract screening. After the full-text review, 37 studies were excluded because they did not meet the eligibility criteria. One additional study was identified through a reference list review. A total of 13 articles with 1778 PWD were included. The characteristics of the included studies are presented in Table 122–34. The studies were conducted in eight countries, with Canada having the highest number of studies (n=4)24–26,34. Theories or guiding principles were used in ten studies to underpin the design and development of evaluated interventions22–28,32,33.
Table 1. Characteristics of included studies
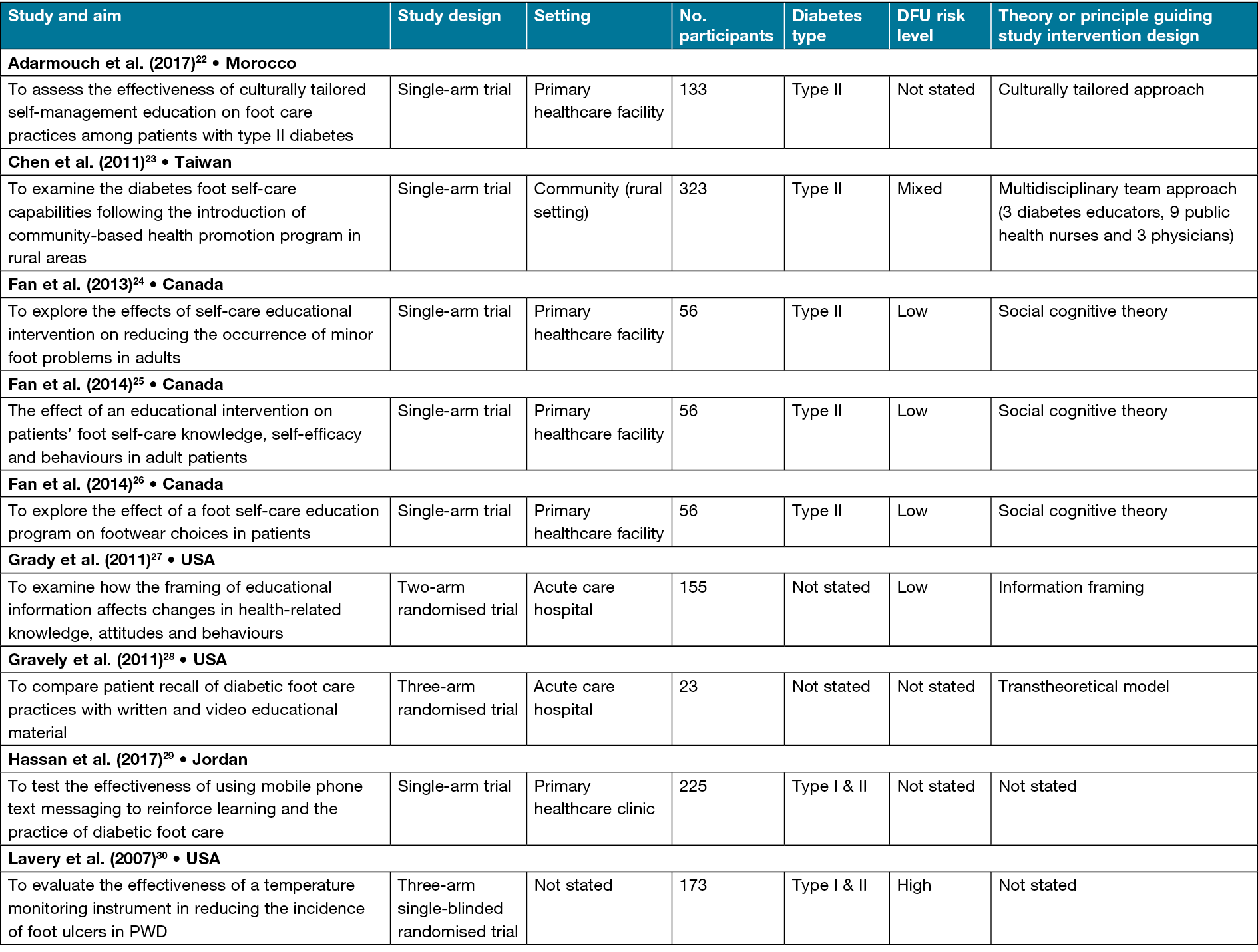
The patient diabetic foot-based self-management program details are presented in Table 2. The patient education programs’ content are categorised as general and focused. Most of the education programs focused only on diabetic foot problems and associated foot care strategies24–26,29–34. Two studies utilised general content that entailed all aspects of diabetes care, such as medication, diet, exercise, glucose monitoring and foot self-care22,23. Eight studies integrated self-management support measures that involved tailored individual counselling23, problem-solving24–26, self-monitoring aid30, self-care reminders29, motivation32, peer support34, links to community resources34 and an action plan34. Woodbury et al.34 integrated the most self-management support measures that included learning engagement activities such as case studies, hands-on and storytelling in their program named the Diabetes, Healthy Feet and You (DHFY). Eleven studies provided the details of the topics covered22,25–27,29–35. Six diabetic foot-focused education topics were identified across studies – overview of diabetes, overview of DFU, consequences of DFU, DFU risk factors, DFU preventive strategies, and the foot care team. Collectively, the studies utilised five types of ICT tools to facilitate the delivery of the identified diabetic foot-based self-management programs. The identified ICT tools are video22,27,28,30,32,24, PowerPoint22,32,34, CD-ROM22, phone23–26,29,31–33 and web portal34.
Table 2. Patient diabetic foot self-management education and support program details
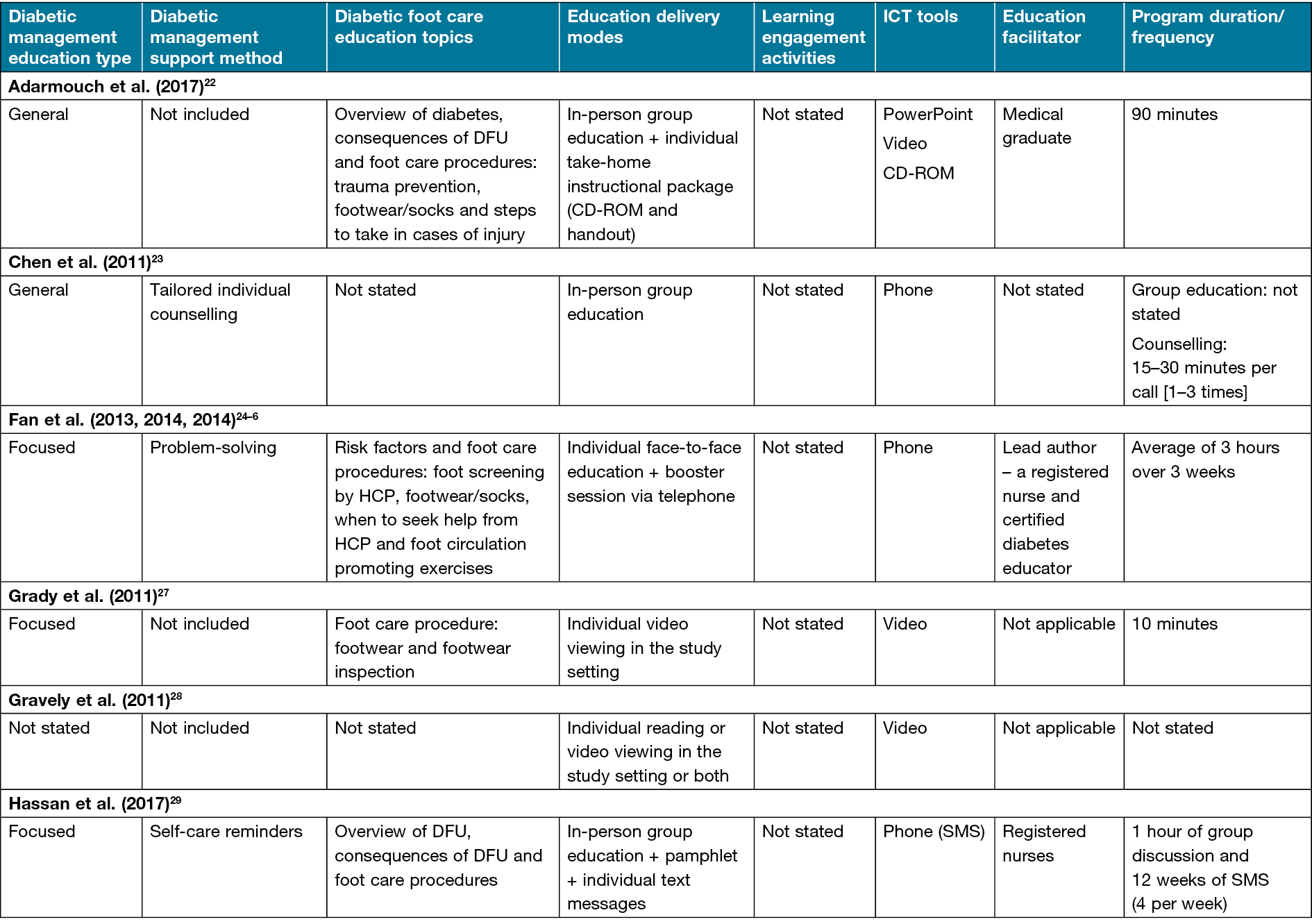
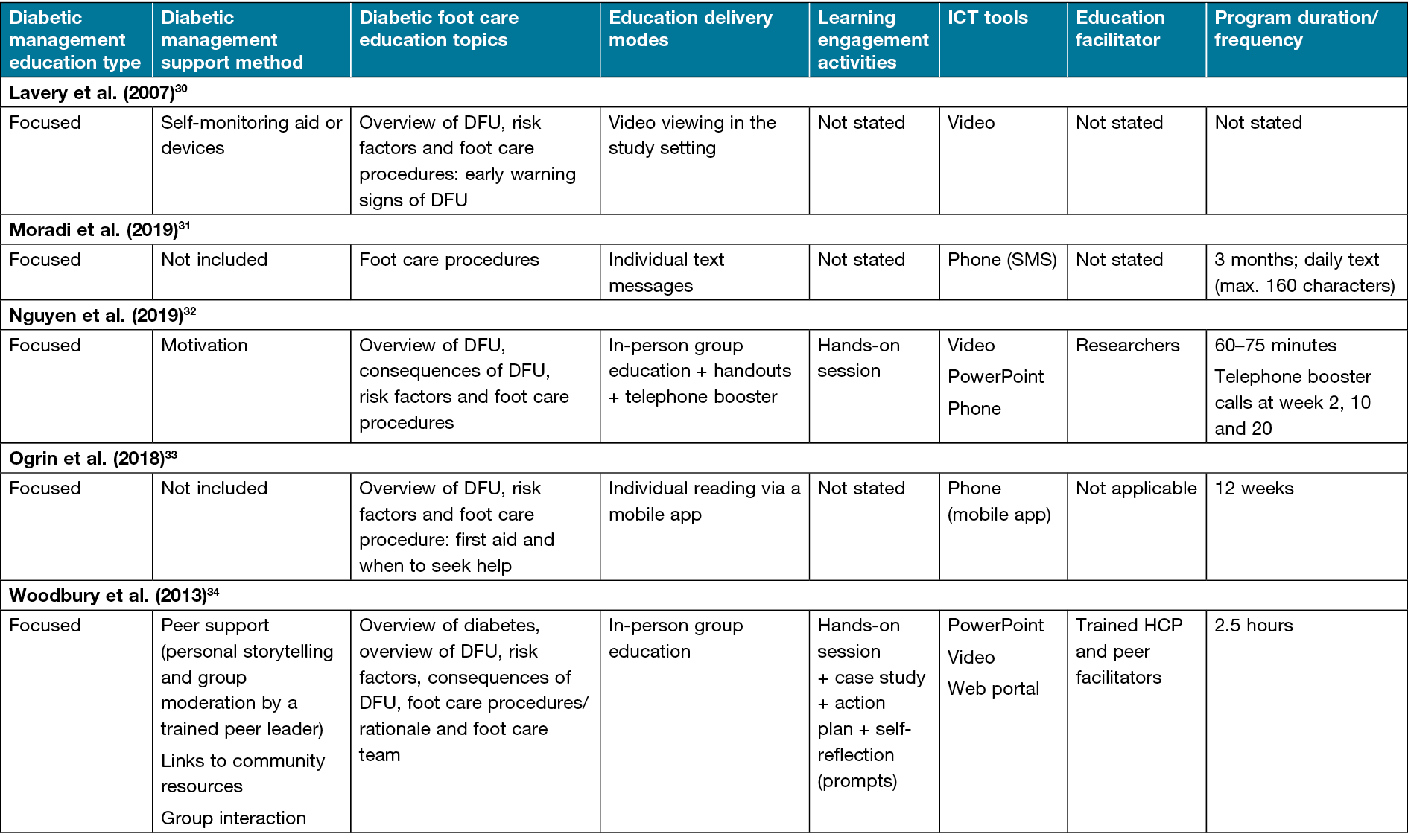
Specifically, videos and/or PowerPoint were used to present education topics22,27,28,30,32,34 and motivate34 participants. Less often, a CD-ROM and a web portal were used, respectively, for reinforcement of educational teaching22 and communication between peer facilitators and the research team34. Phones were used for varied reasons – individual education31,33, follow-up reinforcement of educational teaching24–26,29,32, counselling23, motivation32, problem-solving24–26,29,32 and self-care reminders29. Also, phones were used to call participants directly23–26,32, send short message service (SMS) texts29,31 or provide access to a mobile app33. The mode of delivery of the patient education programs varied across studies – individual23–28,30,31,33, group22,23,34 or a combination of both methods29,32. In most individual-based programs, the authors utilised non-face-to-face approaches such as video viewing27,28,30, self-reading28,29 and text messages31.
Only two studies assessed participants’ perceptions of the evaluated programs’ contents or components33,34. Ogrin et al.33 reported only participants’ perception of a mobile app, while Woodbury et al.34 reported on the whole intervention. The methods used to evaluate participants’ experiences included a structured questionnaire34 and focus group discussion33. Woodbury et al.34 reported that the participants were highly satisfied with the DHFY program, with a score range of 4.4–4.7 (scale of 0–5). Lastly, Ogrin et al.33 reported a mixed participant experience – some considered the mobile app helpful in enhancing their foot self-care knowledge and practices, whereas others remarked that the app was too basic, suitable for only newly diagnosed patients, and they would prefer it be installed on a tablet for ease of reading, group education or as a written checklist, or as one that could address all aspects of diabetes self-care and not just foot care.
Application of literature search results to DFCG content development
Based on the literature search result, Woodbury et al.’s34 DHFY program was adopted as a template to guide DFCG content development because it contained the highest number of patient education topics (n=6), self-management support measures (n=3), and engagement activities (n=4). In addition, the participant satisfaction with DHFY was high. DHFY is a 2.5-hour in-person program; however, the identified contents or components can easily be customised to a social media context compared to other studies. Also, it is a Canadian-based program, thus more appropriate for the study setting. Evidence from a quasi-experimental study among 294 adults in 12 communities across 10 provinces revealed that engagement in the DHFY led to an immediate improvement in foot self-care knowledge (7.6 to 8.4) and long‑term positive behaviour change among 97% of participants 12 months post-intervention35,36.
Finally, to ensure that the DFCG addressed all PWD concerns about diabetic foot-based self-management programs, Ogrin et al.’s33 report on participants’ preferences about their mobile app in the above section was considered and influenced the team’s decision to include additional patient education topics. Three other self-care behaviours critical for optimal blood glucose control and diabetic foot health, as recommended by the American Association of Diabetes Educators self-care behaviour framework, were added to the patient education topic list in DHFY – nutrition, exercise and diabetes-related mental health issues36.
Deciding on the social media platform
To make the DFCG program sustainable and cost-effective, the study team decided to choose from the existing free social media platforms as the intervention delivery medium rather than develop a new one. Facebook is the most widely used social media network prevalent across the age group 18 years and above in Canada37,38 and provided the platform for this study. In addition, Facebook is user-friendly, easy to set up, and has good privacy control features and administrative tools that allow group moderators to schedule posts and effectively monitor group activities39. However, to ensure that information posted in the group aligns with the group goal, all members’ posts are reviewed and approved by the group administrators before they are shared on the platform.
Maintaining participants’ privacy in the DFCG was an essential element in ensuring the protection of participants’ identities and trust in the moderators. As a result, the DFCG was hosted on a private Facebook group, meaning members can only be admitted into the group by the moderators after they request to join the group, answer the membership questions, and agree to the group rules related to spamming, harassment and members’ privacy. The membership questions require the recruited members to provide the given individual unique identification code in addition to the email with which they received formation about their allocation to the study groups. The private nature of the DFCG allowed members’ information and discussions to be only visible to group members and not the public. In addition, based on the ethical review committee’s recommendation, a document titled Facebook account set-up and privacy setting guide and a video summary of the steps were developed as one of the featured posts to empower members to secure their personal information on Facebook and reduce privacy risk. Ethical approval was obtained from Queen’s University Health Sciences and Affiliated Teaching Hospitals Research Ethics Board (NURS-487-20).
The DFCG was created in December 2020 following the steps recommended on Facebook with a profile image that reflected the group goal40. In February 2021, the group was visible in search and other places on Facebook for interested PWD to join (https://www.facebook.com/groups/diabeticfootcaregroup).
Compilation of posts/links to community resources
A pool of Facebook posts that aligned with the four DFCG components was composed to facilitate participants’ diabetic foot SMES. The composed posts were a combination of text, photos, videos and web links in the English language. The posts’ text was structured at a 6th-grade reading level to ensure readability and comprehension41. Also, the posts were worded in a non-coercive way to encourage PWD to prevent DFU. The videos helped reinforce the information presented as text to help participants retain what was learned. In addition, videos were used to demonstrate foot care procedures and present patients’ stories about diabetes and foot care experiences. All videos were free YouTube videos with sharing options, except the videos on Facebook privacy-setting demonstration and the peer leader’s journey of diabetes/role group which were developed by the lead author. Photos were used to summarise the key message of the text in the posts. Sources of photos included free-to-use Google images and the Wounds Canada image bank. Weblinks were used to direct members to credible sources of information on the internet. Lastly, the study team compiled a list of some available community resources in each Canadian province that provide support for PWD regarding diabetes management, foot care, mental health and general wellbeing in a document titled Links to community resources. The document served as a self-management support information directory for members to find and efficiently use community resources in their various locations. The document contained the name of the community resources, location and contact information.
Content validation
The study team assessed the face and content validity of the compiled posts and supporting documents for appropriateness, accuracy, ease of comprehension by PWD, and alignment with the underpinning theoretical framework, current international guidelines and topics selected.
Revision based on group members’ feedback
After 1 month of membership, PWD who joined the DFCG were asked to give feedback about the program based on their concerns or needs in an open-ended question on Qualtrics XM survey software. In addition, members of the DFCG were encouraged to contribute through prompt-based posts to comment or post their needs or concerns about the program. Ten group members who are residents in Canada provided feedback (see Table 3 for their sociodemographic/clinical characteristics). Table 4 presents a list of participants’ concerns or needs expressed through the online survey and comments in the DFCG. The expressed statements included concerns about: targeted promotional advertisements (ads); the need to expand the community resources link document; the provision of additional DFU overview information; the inclusion of information specific to daily foot care procedures, season-specific foot care precautions, and DFU treatment modalities; increasing group member engagement; the desire for program continuation; and digital device recommendation.
Table 3. Participants’ sociodemographic and clinical characteristics
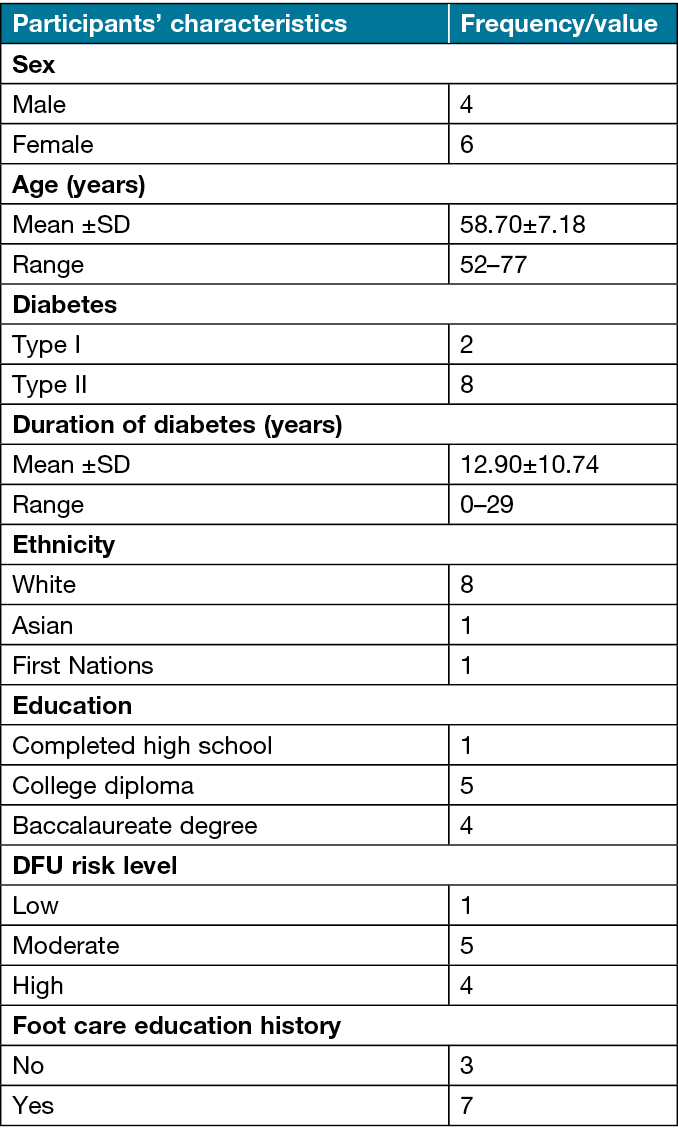
Table 4. Participants’ expressed concerns or needs
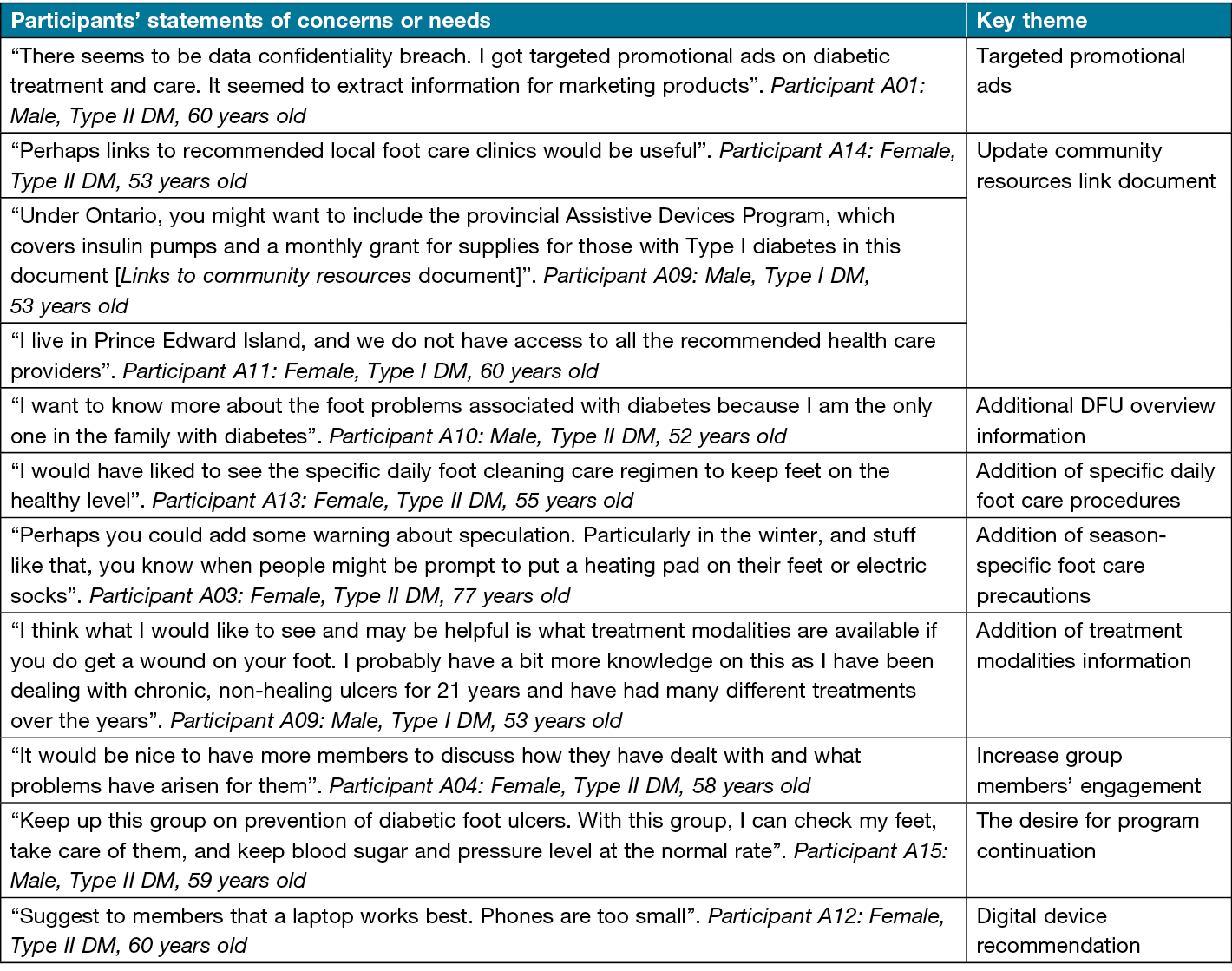
Based on the expressed concerns/needs, the study team revised the patient education content and supporting documents. A new topic, Management of DFU and associated problems, was included in the list of patient education topics. Furthermore, the existing topics Preventive foot care strategies and DFU overview were expanded to include additional sub-topics. The topic Preventive foot care strategies was broadened to include season-based foot care tips (i.e., summer, fall/autumn and winter), controlling co-morbid health conditions (e.g., hypertension), and video demonstrations of foot care routines. The topic DFU overview was expanded from the definition of DFU to include detailed information on types of DFU, infection, non-healing ulcers, etc. To increase group members’ engagement, the number of prompt-based posts was increased to promote group discussion. Lastly, the support documents Facebook account set-up and privacy-setting guide and Links to community resources were revised to address group members’ concerns about Facebook ads and additional resources, respectively.
Overall, a total of 370 posts that aligned with the four components of the DFCG were compiled as its content template (Table 5). A total of 62% of the posts focused on content that cut across the ten patient education topics – Overview of diabetes, DFU overview, Consequences of DFU, DFU risk factors, DFU preventive strategies, The diabetic foot care team, Treatment of DFU and associated problems, Nutrition, Exercise, and Diabetes-related mental health issues and management (Appendix 2). The remaining posts focused on supporting and engaging PWD to become motivated to apply what they learned in their personal lives. The support and engagement posts comprise patient stories, poll questions, prompts, action plans, hands-on practice activities, case studies, weekly summaries, and welcome posts. The posts contained text with a word count that ranged from 3–458 words (84.6±88.4). In addition, the posts included 211 photos, 67 videos and 77 weblinks. Respectively, about 20% of the content of the patient education and support/engagement posts focused on DFU preventive strategies and poll questions.
Table 5. Compiled DFCG posts’ content classification

Discussion
An essential concept of chronic disease self-management is an individual’s daily responsibility to manage their health and prevent complications43. PWD are encouraged to be responsible for their foot health to avoid ulcers. Unfortunately, this can be challenging as many PWD do not engage in recommended foot self-care activities due to the complexities of diabetes, a lack of knowledge, and the perceived burden of the unending self-care routines44. Thus, the DFCG, a social media-based self-management program on Facebook, was developed to help PWD navigate these challenges by becoming confident to assume responsibility for managing their diabetes and maintaining healthy feet. The DFCG is currently live on Facebook. The program has four major components – education, peer support, social interaction and active engagement.
Education is a vital component of the DFCG that promotes members’ ability to optimise their health and wellbeing. The primary goal of the education content is to improve the knowledge of DFU-related problems, awareness of community resources, and enhance positive foot self-care behaviours essential for PWD to maintain a healthy foot status and prevent DFU-related complications. The steps involved in implementing patient education include introductory activities, scheduling two to three posts daily on a specific topic, community resources document, and sharing information about webinars that align with the group goal.
Peer support is conceptualised as an interactive process that allows people with similar conditions, such as diabetes, to share their experiences and knowledge to support others to develop confidence and adopt recommended healthy behaviours45. In the DFCG, the peer-support component was implemented by recruiting a Wounds Canada-trained peer leader as the group co-facilitator, posting patient stories (text with videos or weblinks), and welcoming members when they joined the group. These steps facilitate the opportunity for members to reflect on and assess their lifestyles which could motivate the decision for a change. The peer leader is a person with diabetes and a member of the development team. The team selected the peer leader because of the knowledge, skills and positive experience in relation to diabetic foot self-management. The peer leader complements educational posts with personal stories and answers members’ questions in the comment section to provide emotional, informational and appraisal support.
The third component of the DFCG is social interaction, conceptualised as a technique to motivate members to take responsibility for their health and know that they are not alone46. Social interaction plays a vital role in patients’ learning because it allows them to explore their attitudes, analyse the motives behind their behaviours, and motivates them to improve their self-management skills and develop a sense of wellbeing47. An essential step in achieving social interaction in patient education is group interaction or discussion. The peer leader and the lead author (a registered nurse) facilitate and moderate the group discussion. In the DFCG, social interaction is implemented through the opportunity for PWD to connect, communicate, brainstorm and compare experiences about diabetes and foot health-related issues virtually (posts, comments and likes).
The last component of the DFCG is active engagement. We defined active engagement as the method of stimulating members’ active participation in the DFCG and interest in learning to maximise their ability to achieve diabetic foot care goals. Improved engagement of patients in self-management education content can inform healthy behavioural change, improve decision-making, and sustain patients’ adherence to HCP recommendations48. Unfortunately, despite the comprehensive documentation of the benefits of patient engagement in improving health outcomes in the literature49, information on effective strategies to facilitate engagement, especially online-based programs on chronic disease management, is scarce. Therefore, based on the experiential knowledge in developing patient education programs, the team integrated six engagement activities that comprised poll questions, prompts, action plans, hands-on practice activities, case studies and weekly summaries in the compiled posts. As a follow-up, the administrators ‘like’ or ‘write a reply’ to acknowledge group members’ efforts whenever they respond to the engagement activities.
The strength and benefits of the DFCG
This paper confirms that HCP can use social media platforms such as Facebook to deliver a structured and evidence-based foot self-management program to empower PWD in preventing foot problems. The DFCG development and implementation processes described in this paper could serve as a reference for developing and implementing future social media-based chronic disease SMES programs. In addition, the age range of participants who provided feedback for DFCG content revision suggests that social media could be an effective medium to engage both young adults and seniors with diabetes in foot self-management. Facebook posts are saved indefinitely or re-posted for continuous SMES of PWD. The DFCG’s content and activities can be accessed anytime, unlike the in-person programs, where members may permanently miss information when unable to attend the program.
Limitations of the DFCG
As with any technology-based platform, the DFCG has some limitations worth mentioning. First, participation in the DFCG requires individuals to have a Facebook account and have access to the internet and a computer or smartphone. This requirement could be challenging for people living in places with no internet or limited resources (e.g., electricity) or with low income who cannot afford the needed devices. Second, the DFCG is structured in the English language. Thus, people who do not understand English may not benefit from the DFCG. Third, a basic knowledge of using the internet and computer or phone (digital literacy) is needed for an individual to access the DFCG successfully. However, this limitation can be overcome by training individuals on how to use the required devices. Fourth, this intervention is not ideal for people who have a fear of or feel unsafe using computers or smartphones. Lastly, social media or internet usage could be associated with security or privacy risk. None of the members reported experiencing any privacy or security issues with DFCG. Therefore, group members will need to take extra measures to secure their personal information and be cautious while accessing the DFCG.
Conclusions
DFU continue to persist as a serious health problem. Empowering PWD to become proactive in preventing DFU could help improve their quality of life. Based on this premise, in 2020, researchers at Queen’s University collaborated with Wounds Canada to develop the DFCG as an alternative method to empower PWD daily to prevent foot ulcers. DFCG content is evidence-based and person-centred. Social media was seen as a possible innovative and cost-effective method to improve PWD access to daily foot SMES and optimise diabetic foot care outcomes during the COVID‑19 pandemic and beyond. The preliminary evaluation of the DFCG revealed an improvement in PWD foot self-care adherence, communication with HCP, awareness of community resources, foot health status, and physical functioning50. However, given the inherent limitations, we recommend that social media-based interventions like the DFCG should not be used alone but rather in combination with traditional self-management programs until robust empirical evidence through randomised control trials is available.
Acknowledgements
The authors wish to thank the group members who completed the survey and provided comments that informed the revision of DFCG content.
Author contribution
All authors contributed to the conception of this study. MB chaired the DFCG development/implementation meetings. HNO completed literature reviews and compiled posts. HNO, MB, OV, HI and TW prepared the community resource link document. OV organised meetings and set up the DFCG on Facebook. HNO and HI scheduled posts on Facebook. HNO and TW moderated the DFCG. HNO prepared the manuscript under the supervision of KW, JT and RW. All authors read and approved the final manuscript.
Conflicts of interest
None to declare.
Ethics statement
The study was approved by Queen’s University Health Sciences and the Affiliated Teaching Hospitals Research Ethics Board.
Funding
In-kind administrative support by Wounds Canada.
Author(s)
Helen N Obilor1*, Heather Ibbetson2, Tom Weisz2, Olena Veryha2, Mariam Botros2,
Rosemary Wilson3, Joan Tranmer3, Kevin Woo3
1School of Nursing, Queen’s University, Kingston, Ontario, Canada;
Department of Nursing, Faculty of Clinical Sciences, College of Medicine, University of Ibadan, Ibadan, Nigeria
2Wounds Canada (Canadian Association of Wound Care), Ontario, Canada
3School of Nursing, Queen’s University, Kingston, Ontario, Canada
*Corresponding author email 15hno@queensu.ca
References
- Obilor HN, Adejumo PO. Assessment of diabetic foot ulcer-related pain and its relationship to quality of life. Wound Pract Res 2015;23(3):124–31.
- Armstrong DG, Swerdlow MA, Armstrong AA, Conte MS, Padula WV, Bus SA. Five year mortality and direct costs of care for people with diabetic foot complications are comparable to cancer. J Foot Ankle Res 2020;13(1):16.
- Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. New Eng J Med 2017;376(24):2367–75.
- Narres M, Kvitkina T, Claessen H, Droste S, Schuster B, Morbach S, et al. Incidence of lower extremity amputations in the diabetic compared with the non-diabetic population: a systematic review. PLoS One 2017;12(8):e0182081.
- Imam B, Miller WC, Finlayson HC, Eng JJ, Jarus T. Incidence of lower limb amputation in Canada. Can J Pub Health 2017;108(4):e374-e80.
- Schaper NC, van Netten JJ, Apelqvist J, Bus SA, Hinchliffe RJ, Lipsky BA, et al. Practical guidelines on the prevention and management of diabetic foot disease (IWGDF 2019 update). Diabetes/Metab Res Rev 2020;36(S1):e3266.
- Cauch-Dudek K, Victor JC, Sigmond M, Shah BR. Disparities in attendance at diabetes self-management education programs after diagnosis in Ontario, Canada: a cohort study. BMC Public Health 2013;13(1):85.
- Scott A, O’Cathain A, Goyder E. Socioeconomic disparities in access to intensive insulin regimens for adults with type 1 diabetes: a qualitative study of patient and healthcare professional perspectives. Intern 2019;18(1):150.
- Casciato DJ, Yancovitz S, Thompson J, Anderson S, Bischoff A, Ayres S, et al. Diabetes-related major and minor amputation risk increased during the COVID‑19 pandemic. J Am Pod Med Assoc 2023;113(2):20–224. doi:10.7547/20-224.
- Miranda C, Zanette G, Da Ros R. Diabetic foot disease during the COVID‑19 pandemic: lessons learned for our future. Arch Med Sci Atheroscler Dis 2022;7:e94-e103.
- Riddle MC, Buse JB, Franks PW, Knowler WC, Ratner RE, Selvin E, et al. COVID‑19 in people with diabetes: urgently needed lessons from early reports. Diabetes Care 2020;43(7):1378.
- Statista. Number of social network users worldwide from 2017 to 2025 2021. Available from: https://www.statista.com/statistics/272014/global-social-networks-ranked-by-number-of-users/.
- Ventola CL. Social media and health care professionals: benefits, risks, and best practices. P&T 2014;39(7):491–520.
- Abedin T, Al Mamun M, Lasker MAA, Ahmed SW, Shommu N, Rumana N, et al. Social media as a platform for information about diabetes foot care: a study of Facebook groups. Can J Diabetes 2017;41(1):97–101.
- Abedin T, Ahmed S, Al Mamun M, Ahmed SW, Newaz S, Rumana N, et al. YouTube as a source of useful information on diabetes foot care. Diabetes Res Clin Pract 2015;110(1):e1-e4.
- Thomas RL, Alabraba V, Barnard S, Beba H, Brake J, Cox A, et al. Use of social media as a platform for education and support for people with diabetes during a global pandemic. J Diabetes Sci Tech 2023;17(2):353–363. doi:10.1177/19322968211054862
- Obilor HN, Woo K. The diabetes foot care Facebook group study. Limb Pres Can 2021;2(1):37–8.
- Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health 1998;13 (4):623–49.
- Boyd H, McKernon S, Mullin B, Old A. Improving healthcare through the use of co-design. NZ Med J 2012;125(1357):76–87.
- Embil JM, Albalawi Z, Bowering K, Trepman E. Foot care. Can J Diabetes 2018;42(2018):S222-S7.
- Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Syn 2020;18(10).
- Adarmouch L, Elyacoubi A, Dahmash L, El Ansari N, Sebbani M, Amine M. Short-term effectiveness of a culturally tailored educational intervention on foot self-care among type 2 diabetes patients in Morocco. J Clin Translat Endocrinol 2017;7:54–9.
- Chen M-Y, Huang W-C, Peng Y-S, Guo J-S, Chen C-P, Jong M-C, et al. Effectiveness of a health promotion programme for farmers and fishermen with type-2 diabetes in Taiwan. J Adv Nurs 2011;67(9):2060–7.
- Fan L, Sidani S, Cooper-Brathwaite A, Metcalfe K. Feasibility, acceptability and effects of a foot self-care educational intervention on minor foot problems in adult patients with diabetes at low risk for foot ulceration: a pilot study. Can J Diabetes 2013;37(3):195–201.
- Fan L, Sidani S, Cooper-Brathwaite A, Metcalfe K. Improving foot self-care knowledge, self-efficacy, and behaviors in patients with type 2 diabetes at low risk for foot ulceration: a pilot study. Clin Nurs Res 2014;23(6):627–43.
- Fan L, Sidani S, Cooper-Brathwaite A, Metcalfe K. Effects of a foot self-care educational intervention on improving footwear choices in those with type 2 diabetes at low risk of foot ulceration. Diabetic Foot Can 2014;2(2):4–12.
- Grady JL, Entin EB, Entin EE, Brunye TT. Using message framing to achieve long-term behavioral changes in persons with diabetes. App Nurs Res 2011;24(1):22–8.
- Gravely SS, Hensley BK, Hagood-Thompson C. Comparison of three types of diabetic foot ulcer education plans to determine patient recall of education. J Vasc Nurs 2011;29(3):113–9.
- Hassan ZM. Mobile phone text messaging to improve knowledge and practice of diabetic foot care in a developing country: feasibility and outcomes. Int J Nurs Pract 2017;23(Supplement 1).
- Lavery LA, Higgins KR, Lanctot DR, Constantinides GP, Zamorano RG, Athanasiou KA, et al. Preventing diabetic foot ulcer recurrence in high-risk patients: use of temperature monitoring as a self-assessment tool. Diabetes Care 2007;30(1):14–20.
- Moradi A, Alavi SM, Salimi M, Nouhjah S, Shahvali EA. The effect of short message service (SMS) on knowledge and preventive behaviors of diabetic foot ulcer in patients with diabetes type 2. Diabetes Metab Synd: Clin Res Rev 2019;13(2):1255–60.
- Nguyen TPL, Edwards H, Do TND, Finlayson K. Effectiveness of a theory-based foot care education program (3STEPFUN) in improving foot self-care behaviours and foot risk factors for ulceration in people with type 2 diabetes. Diabetes Res Clin Pract 2019;152:29–38.
- Ogrin R, Viswanathan R, Aylen T, Wallace F, Scott J, Kumar D. Co-design of an evidence-based health education diabetes foot app to prevent serious foot complications: a feasibility study. Pract Diabetes 2018;35(6):203–9.
- Woodbury MG, Botros M, Kuhnke JL, Greene J. Evaluation of a peer-led self-management education programme PEP talk: diabetes, healthy feet and uou. Int Wound J 2013;10(6):703–11.
- Fan X, Lv F. Psychosocial factors associated with self-efficacy for managing chronic disease in patients with chronic heart failure. Eur J Cardiovasc Nurs 2016;15(4):255–61.
- American Association of Diabetes Educators. An effective model of diabetes care and education: revising the AADE7 Self-Care Behaviors®. Diabetes Educat 2020;46(2):139–60.
- Statista. Leading social networks used by internet users in Canada as of March 2021, by province 2021. Available from: https://www.statista.com/statistics/262804/social-networks-used-by-internet-users-in-canada-provinces/.
- Statista. Distribution of social media users in Canada as of January 2021, by age group and gender 2021. Available from: https://www.statista.com/statistics/1047732/age-distribution-of-social-media-users-canada/.
- Alhabash S, Ma M. A tale of four platforms: motivations and uses of Facebook, Twitter, Instagram, and Snapchat among college students? Soc Med + Soc 2017;3(1):2056305117691544.
- Facebook. How do I create a Facebook group? 2020. Available from: https://www.facebook.com/help/167970719931213.
- Eltorai AEM, Ghanian S, Adams CA, Jr., Born CT, Daniels AH. Readability of patient education materials on the american association for surgery of trauma website. Arch Trauma Res 2014;3(2):e18161-e.
- Schaper NC, van Netten JJ, Apelqvist J, Bus SA, Hinchliffe RJ, Lipsky BA, et al. Practical guidelines on the prevention and management of diabetic foot disease (IWGDF 2019 update). Diabetes/Metab Res Rev 2020;36(S1):e3266.
- Grady PA, Gough LL. Self-management: a comprehensive approach to management of chronic conditions. Am J Pub Health 2014;104(8):e25–31.
- Obilor HN, Achore M, Woo K. The use of information communication technology tools in diabetic foot ulcers prevention programs: a scoping review. Can J Diabetes 2022;46(5):535-548.e5. doi:10.1016/j.jcjd.2021.11.009.
- Munce SEP, Shepherd J, Perrier L, Allin S, Sweet SN, Tomasone JR, et al. Online peer support interventions for chronic conditions: a scoping review protocol. BMJ Open 2017;7(9):e017999-e.
- Seyyedrasooli A, Parvan K, Valizadeh L, Rahmani A, Zare M, Izadi T. Self-efficacy in foot-care and effect of training: a single-blinded randomized controlled clinical trial. Int J Comm Based Nurs Midwif 2015;3(2):141–9.
- Odgers-Jewell K, Isenring EA, Thomas R, Reidlinger DP. Group participants’ experiences of a patient-directed group-based education program for the management of type 2 diabetes mellitus. PloS One 2017;12(5):e0177688-e.
- Oktay LA, Abuelgasim E, Abdelwahed A, Houbby N, Lampridou S, Normahani P, et al. Factors affecting engagement in web-based health care patient information: narrative review of the literature. J Med Internet Res 2021;23(9):e19896-e.
- Laurance J, Henderson S, Howitt PJ, Matar M, Al Kuwari H, Edgman-Levitan S, et al. Patient engagement: four case studies that highlight the potential for improved health outcomes and reduced costs. Health Affairs 2014;33(9):1627–34.
- Obilor H, Woo K. IDF21-0257 The feasibility of a social media-based diabetic foot ulcer prevention program during the COVID‑19 pandemic in Canada. Diabetes Res Clin Pract 2022;186.
Appendix 1. The PRISMA flowchart
Appendix 2. Description of patient education post content