Volume 31 Number 3
Topical oxygen therapy for treating diabetic foot ulcers: a WHAM evidence summary
Emily Haesler
For referencing Haesler E for Wound Healing and Management Collaborative. Topical oxygen therapy for treating diabetic foot ulcers: a WHAM evidence summary. Wound Practice and Research 2023; 31(3):152-156.
DOI https://doi.org/10.33235/wpr.31.3.152-156
CLINICAL QUESTION
What is the best available evidence for topical oxygen therapy for treating diabetic foot ulcers (DFUs)?
SUMMARY
Topical oxygen therapy is an adjunctive therapy that seeks to improve cell proliferation in chronic wounds by delivering high concentration oxygen directly to the wound bed. Oxygen application can be via a mechanical system that delivers gaseous oxygen to the wound bed (carrier systems) or can be via topical applications (e.g., oxygen generating/releasing dressings or haemoglobin spray) that directly or indirectly increase oxygen in the wound bed. Level 1 evidence consisting of five meta-analyses1-5 on the effectiveness of mechanically delivered topical oxygen therapy demonstrated that the treatment is associated with statistically significant improvements in complete healing at 12 weeks2-5, and in the number of DFUs healed at 8—12 weeks1. These findings are supported by a narrative systematic review6, although a seventh, narrative review7 concluded that the evidence was inadequate to make recommendations. There is evidence that topical oxygen therapy delivered via mechanical systems is associated with improvement in wound healing at 12 weeks with differences over standard care of between 5% and 27%2, which may be clinically significant for some people with DFUs. Two Level 1 reviews8, 9 reported narrative results from Levels 2, 3 and 4 studies on effectiveness of haemoglobin spray for treating DFUs, but this body of evidence is currently inadequate to recommend this method of topical oxygen delivery.
CLINICAL PRACTICE RECOMMENDATIONS
All recommendations should be applied with consideration to the wound, the person, the health professional and the context.
|
Topical oxygen therapy delivered via a mechanical system could be considered as an adjunctive therapy for diabetic foot ulcers that have failed to respond to standard care (Grade B). There is no strong evidence to support the use of a haemoglobin spray for treatment of diabetic foot ulcers. |
SOURCES OF EVIDENCE
This summary, including the making of recommendations, was conducted using methods published by the Joanna Briggs Institute10-12. The summary is based on a systematic literature search combining search terms related to chronic wounds/DFUs and topical oxygen therapy/topical haemoglobin. Searches were conducted in Embase, AMED, Medline, the Cochrane Library and Google Scholar for evidence published up to 30 June 2022 in English. Due to the volume of recent systematic reviews identified on this topic, inclusion was limited to Level 1 evidence.
BACKGROUND
Topical oxygen therapy is an advanced wound healing intervention that seeks to improve wound healing by increasing the oxygen supply within the wound bed.34-36 Peripheral arterial disease, which is a complicating factor for the majority of DFUs, can lead to reduced perfusion of the wound and therefore decreased wound bed oxygenation.34 Topical oxygen delivery interventions seek to address this complication and improve healing outcomes. Oxygen is delivered locally, directly to the wound bed using either mechanical systems that deliver sustained high concentration oxygen or via oxygen-releasing/generating wound dressings or topical sprays.34-36 For mechanical systems, oxygen is delivered in a gaseous form to the wound bed using a specific system (see Table 2) that enables an oxygen gradient to develop around the wound, facilitating diffusion of oxygen into the wound bed.
Haemoglobin spray is another form of topical oxygen treatment (sometimes referred to as facilitated delivery or oxygen carrier system).34 This intervention is designed to increase oxygen supply to the wound bed through the application of a topical, aqueous, haemoglobin-containing spray.8, 9 Because haemoglobin is capable of transporting oxygen within the body, the spray is designed to promote oxygen-binding in the wound bed from the surrounding air for transport deeper into the wound bed and diffusion into cells to promote healing.9 In the laboratory, the spray has been demonstrated to increase angiogenesis, cell proliferation and collagen deposition.37 Oxygen can also be delivered via wound dressings that contain embedded pure oxygen that is released into the wound bed when the oxygen-containing dressing is in contact with moisture.35 The literature search did not identify any Level 1 evidence for these products.
Table 1: Levels of evidence for intervention studies
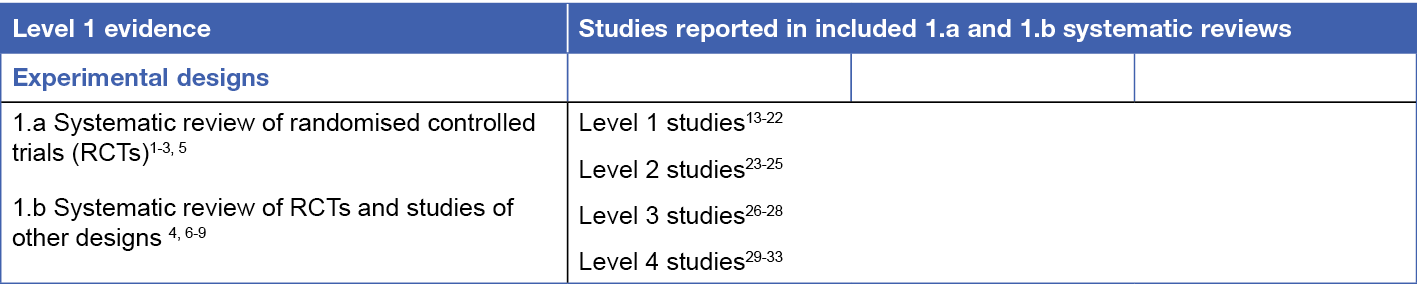
Table 2: Types of mechanically delivered topical oxygen therapy34-36

CLINICAL EVIDENCE
Topical oxygen therapy delivered via mechanical systems for treating diabetic foot ulcers
The literature search identified seven recently published systematic reviews1-7 exploring the use of topical oxygen therapy, all focused on DFUs. There was substantial cross-over in the studies included in the different reviews. The reviews variously limited inclusion eligibility to studies with randomised designs1-3, 5, and/or based on the number of participants2, outcome measures reported1, 2, 4, 5 or comparator interventions3, 4, 6. Across the reviews1-7, 11 RCTs13-22, 29 were reported, most of which were appraised as being at moderate or high risk of bias. An additional four studies23, 24, 26, 27 providing Level 2 or Level 3 evidence were reported in these reviews.
The most methodologically robust review2 included a meta-analysis that showed statistically significant results favouring use of topical oxygen therapy over sham therapy or standard care (risk ratio [RR] = 1.59 (95% confidence interval [CI] 1.07 to 2.37; p = 0.021) for complete wound healing at 12 weeks. Across the four included RCTs13-16, the difference in wound healing rates versus the comparator ranged from 5% to 27%2 (Level 1).
A second review5 included a meta-analysis of the same four RCTs13-16, reporting the same results for complete DFU healing at 12 weeks as in the above review2. Pooled results from three of the RCTs14-16 showed faster healing with topical oxygen therapy versus standard care, but this was not statistically significant (hazard ratio [HR] = 1.45, 95% CI 0.87 to 2.42, p = 0.16)5 (Level 1).
A third review1 included a meta-analysis of six RCTs13-17, 19 that showed statistically significant results favouring use of topical oxygen therapy over control for number of DFUs healed at 8—12 weeks (RR = 1.63 (95% CI 1.33 to 2.00; p < 0.00001). Five RCTs13, 15, 17-19 that reported reduction in ulcer size favoured topical oxygen therapy over control, but duration of therapy was of different lengths across the trials, so no pooled analysis was conducted. Four RCTs14-16, 19 reported healing time, with the majority showing no significant difference compared to control (Level 1).
A fourth review3 included a meta-analysis of six RCTs14-17, 20, 21 that showed statistically significant results favouring use of topical oxygen therapy over control for complete DFU healing (RR = 1.94, 95% CI 1.19 to 3.17; p = 0.04)3 (Level 1).
The next review4 reported eight studies14, 15, 17, 20, 21, 23, 24, 26 of various designs. A meta-analysis of five of the studies14, 15, 17, 20, 23 favoured topical oxygen therapy over standard care for complete healing of DFUs (odds ratio [OR] = 2.49, 95% CI 1.59 to 3.90, p = 0.04). This review4 reported that DFUs generally healed faster when treated with topical oxygen therapy but had no impact on recurrence rates (Level 1).
A sixth review6 included five studies17, 21, 23, 24, 29 of various designs. Thia review, which did not include a meta-analysis, concluded that topical oxygen therapy was associated with better healing outcomes for people with Wagner Grade 1 DFUs than for those with more severe DFUs (Level 1).
Finally, the seventh systematic review7, which underpinned recommendations from International Working Group of the Diabetic Foot (IWGDF) working group, included six studies that explored topical oxygen therapy14, 16, 17, 22, 23, 27. This review7, which did not include a meta-analysis or GRADE evaluation of the evidence, concluded there was inadequate evidence from published studies to support a recommendation to use topical oxygen therapy (Level 1).
Overall, the evidence for topical oxygen therapy has increased in recent years but remains small and subject to moderate to high risk of bias. Multiple meta-analyses1-5 demonstrate statistically significant outcomes achieved with mechanically delivered topical oxygen therapy; however, the clinical significance is unclear. Four of the reviews1-3, 5 included sensitivity analyses, three of which identified one RCT14 as significantly contributing to heterogeneity of the evidence. This study used an older oxygen delivery system that may have been less reliable2, but also included participants with less severe DFUs1. Analysis showed that the body of evidence is at risk of publication bias1, 2, 5.
TOPICAL HAEMOGLOBIN THERAPY FOR TREATING DIABETIC FOOT ULCERS
Two systematic reviews8, 9 reported on the effectiveness of topical haemoglobin spray. Both reviews8, 9 included studies conducted in participants with any type of chronic wound that used randomised, comparative or non-comparative designs and identified the same body of evidence. The first of these systematic reviews8 included 15 studies25, 28, 30-33, 38-47, most of which provided low level evidence covering the use of topical haemoglobin spray for DFUs, VLUs, PIs and mixed aetiology wounds. The second systematic review9 reported 14 studies conducted in chronic wounds25, 30-33, 38-41, 43, 44, 46, 47, all of which were reported in the review by Tayyib et.al. (2022)8 (Level 1).
Focusing on the evidence for DFUs, five of the studies were relevant25, 28, 30, 32, 33. These were low level studies (generally with no comparator group) and only reported outcomes for approximately 80 wounds, treated for between 4 and 28 weeks. All these studies showed reduction in wound size for DFUs treated with topical haemoglobin spray. In one comparative study25, the DFUs receiving haemoglobin spray displayed superior reductions in both slough and wound pain compared to an historical control group (Levels 2, 3 and 4).
CONSIDERATIONS FOR USE
In research studies the adverse events experienced by group treated with topical oxygen were similar in type and frequency to those experienced by groups receiving standard wound care1-3, 6-9. These included serious adverse events such as death that were deemed to be not related to the wound treatment.
Topical oxygen therapy should be considered as an adjunctive therapy for chronic wounds, used in conjunction with standard care including offloading and moist wound healing, and for people who are able to follow their wound management regimen1, 2.
Consider the balance between potential benefits from topical oxygen therapy and the potential increased burden of treatment (e.g., cost of equipment, clinician time and the resources required to access treatment more often for some types of topical oxygen therapy)6. The literature search was not designed to identify economic studies and the reviews did not report cost-effectiveness1-3, 6-9.
FUNDING
The development of WHAM Collaborative evidence summaries is supported by a grant from The Western Australian Nurses Memorial Charitable Trust.
CONFLICTS OF INTEREST
The author declares no conflicts of interest in accordance with International Committee of Medical Journal Editors (ICMJE) standards.
ABOUT WHAM COLLABORATIVE EVIDENCE SUMMARIES
The WHAM Collaborative evidence summaries are consistent with methodology published in Munn Z, Lockwood C, Moola S. The development and use of evidence summaries for point of care information systems: A streamlined rapid review approach, Worldviews Evid Based Nurs. 2015;12(3):131-8. Methods are provided in detail in resources published by the Joanna Briggs Institute as cited in this evidence summary. WHAM evidence summaries undergo peer review by a 20-member international multidisciplinary Expert Reference Group. More information about WHAM Collaborative methodology and the peer review process are available at: http://WHAMwounds.com
The WHAM Collaborative evidence summaries provide a summary of the best available evidence on specific topics and make suggestions that can be used to inform clinical practice. Evidence contained within this summary should be evaluated by appropriately trained professionals with expertise in wound prevention and management, and the evidence should be considered in the context of the individual, the professional, the clinical setting and other relevant clinical information.
Copyright © 2023 Wound Healing and Management Collaborative, Curtin University.
Author(s)
Emily Haesler, PhD, P Grad Dip Adv Nurs (Gerontics), BN, FWA
Adjunct Professor, Curtin Health Innovation Research Institute, Wound Healing and Management (WHAM) Collaborative, Curtin University, Bentley WA, Australia
Email emily.haesler@curtin.edu.au
References
- Sun X-K, Li R, Yang X-L, Yuan L. Efficacy and safety of topical oxygen therapy for diabeticfoot ulcers: An updated systematic review and meta-analysis. Int Wound J, 2022; 19(8):2200-09.
- Carter MJ, Frykberg RG, Oropallo A, Sen CK, Armstrong DG, Nair HKR, Serena TE. Efficacy of topical wound oxygen therapy in healing chronic diabetic foot ulcers: Systematic review and meta-analysis. Adv Wound Care, 2022;21:21.
- Thanigaimani S, Singh T, Golledge J. Topical oxygen therapy for diabetes-related foot ulcers: A systematic review and meta-analysis. Diabet Med, 2020;38(8):e14585.
- Connaghan F, Avsar P, Patton D, O’Connor T, Moore Z. Impact of topical oxygen therapy on diabetic foot ulcer healing rates: A systematic review. J Wound Care, 2021;30(10):823-9.
- Sethi A, Khambhayta Y, Vas P. Topical oxygen therapy for healing diabetic foot ulcers: A systematic review and meta-analysis of randomised control trials. Health Sciences Review, 2022;3:100028.
- Nataraj M, Maiya AG, Karkada G, Hande M, Rodrigues GS, Shenoy R, Prasad SS. Application of topical oxygen therapy in healing dynamics of diabetic foot ulcers: A systematic review. Rev Diabet Stud, 2019;15:74-82.
- Vas P, Rayman G, Dhatariya K, Driver V, Hartemann A, Londahl M, Piaggesi A, Apelqvist J, Attinger C, Game F. Effectiveness of interventions to enhance healing of chronic foot ulcers in diabetes: A systematic review. Diabetes Metab Res Rev, 2020;36 (Suppl 1):e3284.
- Tayyib N. Use of topical haemoglobin spray in hard-to-heal wound management: A systematic review. J Wound Care, 2022;31(6):520-31.
- Hu J, Guo S, Hu H, Sun J. Systematic review of the efficacy of topical haemoglobin therapy for wound healing. Int Wound J, 2020;17(5):1323-30.
- Aromataris E, Munn Z, editors. Joanna Briggs Institute Reviewer’s Manual. The Joanna Briggs Institute, 2017. https://reviewersmanual.joannabriggs.org/
- Joanna Briggs Institute Levels of Evidence and Grades of Recommendation Working Party. New JBI Grades of Recommendation. Adelaide: Joanna Briggs Institute, 2013.
- The Joanna Briggs Institute Levels of Evidence and Grades of Recommendation Working Party. Supporting Document for the Joanna Briggs Institute Levels of Evidence and Grades of Recommendation. The Joanna Briggs Institute, 2014.
- Serena TE, Bullock NM, Cole W, Lantis J, Li L, Moore S, Patel K, Sabo M, Wahab N, Price P. Topical oxygen therapy in the treatment of diabetic foot ulcers: A multicentre, open, randomised controlled clinical trial. J Wound Care, 2021;30(Supp 5):S7-S14.
- Driver VR, Reyzelman A, Kawalec J, French M. A prospective, randomized, blinded, controlled trial comparing transdermal continuous oxygen delivery to moist wound therapy for the treatment of diabetic foot ulcers. Ostomy Wound Manage, 2017;63(4):12-28.
- Frykberg RG, Franks PJ, Edmonds M, Brantley JN, Teot L, Wild T, Garoufalis MG, Lee AM, Thompson JA, Reach G, Dove CR, Lachgar K, Grotemeyer D, Renton SC, Group TWOS. A multinational, multicenter, randomized, double-blinded, placebo-controlled trial to evaluate the efficacy of cyclical topical Wound oxygen (TWO2) therapy in the treatment of chronic diabetic foot ulcers: The TWO2 study. Diabetes Care, 2020;43(3):616-24.
- Niederauer MQ, Michalek JE, Liu Q, Papas KK, Lavery LA, Armstrong DG. Continuous diffusion of oxygen improves diabetic foot ulcer healing when compared with a placebo control: A randomised, double-blind, multicentre study. J Wound Care, 2018;27(Sup 9):S30-45.
- Yu J, Lu S, McLaren AM, Perry JA, Cross KM. Topical oxygen therapy results in complete wound healing in diabetic foot ulcers. Wound Repair Regen, 2016;24(6):1066-72.
- Anirudh V, Kamath DY, Ghosh S, Bhuvana K, Sharma S, Maruthy K, Pais P, Xavier D. Topical controlled warm oxygen therapy delivered through a novel device (KADAM™) to treat diabetic foot ulcers: a randomized controlled, open, pilot trial. Indian J Surg, 2021(83):907-14.
- He S, Liang C, Yi C, Wu M. Therapeutic effect of continuous diffusion of oxygen therapy combined with traditional moist wound dressing therapy in the treatment of diabetic foot ulcers. Diabetes Res Clin Pract, 2021;174:108743.
- Niederauer MQ, Michalek JE, Armstrong DG. A prospective, randomized, double- blind multicenter study comparing continuous diffusion of oxygen therapy to sham therapy in the treatment of diabetic foot ulcers. J Diabet Sci Technol, 2017;11(5):883-91.
- Driver VR, Yao M, Kantarci A, Gu G, Park N, Hasturk H. A prospective, randomized clinical study evaluating the effect of transdermal continuous oxygen therapy on biological processes and foot ulcer healing in persons with diabetes mellitus. Ostomy Wound Manage, 2013;59(11):19-26.
- Leslie CA, Sapico FL, Ginunas VJ, Adkins RH. Randomized controlled trial of topical hyperbaric oxygen for treatment of diabetic foot ulcers. Diabetes Care, 1988;11(2):111-5.
- Blackman E, Moore C, Hyatt J, Railton R, Frye C. Topical wound oxygen therapy in the treatment of severe diabetic foot ulcers: A prospective controlled study. Ostomy Wound Manage, 2010;56(6):24-31.
- Hayes PD, Alzuhir N, Curran G, Loftus IM. Topical oxygen therapy promotes the healing of chronic diabetic foot ulcers: A pilot study. J Wound Care, 2017;26(11):652-60.
- Hunt SD. Exploring the effectiveness of topical haemoglobin therapy in the acute care setting on diabetic foot ulceration. The Diabetic Foot Journal, 2017;20(3):176–18.
- Kemp D, Hermans M. An evaluation of the efficacy of transdermal continuous oxygen therapy in patients with recalcitrant diabetic foot ulcer. J Diabet Foot Complicat, 2011;3(1):6–12.
- Heng M, Harker J, Bardakjian V, Ayvazian H. Enhanced healing and cost-effectiveness of low-pressure oxygen therapy in healing necrotic wounds: a feasibility study of technology transfer. Ostomy Wound Manage, 2000;46(3):52-62.
- Hunt SD, Elg F. Clinical effectiveness of hemoglobin spray (Granulox+) as adjunctive therapy in the treatment of chronic diabetic foot ulcers. Diabet Foot Ankle, 2016;7 (no pagination).
- Sano H, Ichioka S. Topical wound oxygen therapy for chronic diabetic lower limb ulcers and sacral pressure ulcers in Japan. Wounds Int, 2015;6:20-4.
- Bateman SD. Topical haemoglobin spray for diabetic foot ulceration. Br J Nurs, 2015;24(Supp12):S24-S9.
- Chadwick P. Pilot study: Haemoglobin sprayin the treatment of chronic diabetic foot ulcers. Wounds UK, 2014;10(4):76-80.
- Haycocks S, McCardle J, Findlow AH, Guttormsen K. Evaluating the effect of a haemoglobin spray on size reduction in chronic DFUs. Br J Nurs, 2016;25(Supp 6):S54-S62.
- Hunt S, Haycocks S, McCardle J, Guttormsen K. Evaluating the effect of a haemoglobin spray on size reduction in chronic DFUs: Clinical outcomes at 12 weeks. Br J Nurs, 2016. 23 Jun;25(12):S59-S64.
- Expert Panel Report. The role of topical oxygen therapy in the management of diabetic foot ulcers. London: The Diabetic Foot Journal, 2019.
- Dissemond J, Kroger K, Storck M, Risse A, Engels P. Topical oxygen wound therapies for chronic wounds: A review. J Wound Care, 2015;24(2):53-63.
- Frykberg RG. Topical wound oxygen therapy in the treatment of chronic diabetic foot ulcers. Medicina, 2021;57(9):31.
- Xie P, Jia S, Tye R, Xu W, Zhong A, Hong SJ, Galiano RD, Mustoe TA. Topical administration of oxygenated hemoglobin improved wound healing in an ischemic rabbit ear model. Plast Reconstr Surg, 2016;137:534-43.
- Arenberger P, Engels P, Arenbergerova M, Gkalpakiotis S, Martínez F, Anaya A, Fernandez L. Clinical results of the application of a hemoglobin spray to promote healing of chronic wounds. GMS Krankenhhyg Interdiszip, 2011;6(1):Doc05.
- Arenbergerova M, Engels P, Gkalpakiotis S, Dubská Z, Arenberger P. Effect of topical haemoglobin on venous leg ulcer healing. EWMA journal, 2013;13(2):25-36.
- Bateman SD. Use of topical haemoglobin on sloughy wounds in the community setting. Br J Community Nurs, 2015;Suppl Wound Care:S32-9.
- Norris R. A topical haemoglobin spray for oxygenating chronic venous leg ulcers: a pilot study. Br J Nurs, 2014;23(Sup20):S48-S53.
- Petri M, Stoffels I, Griewank K, Jose J, P. E, Schulz A, Pötzschke H, Jansen P, Schadendorf D, Dissemond J, Klode J. Oxygenation status in chronic leg ulcer after topical hemoglobin application may act as a surrogate marker to find the best treatment strategy and to avoid ineffective conservative long-term therapy. Mol Imaging Biol, 2018;20:1.
- Tickle J. A topical haemoglobin spray for oxygenating pressure ulcers: A pilot study. Br J Community Nurs, 2015:S12-8.
- Tickle J, Bateman SD. Use of a topical haemoglobin spray for oxygenating pressure ulcers: healing outcomes. Br J Community Nurs, 2015;20(Suppl 12):S14–21.
- Hunt S, Elg F. The clinical effectiveness of haemoglobin spray as adjunctive therapy in the treatment of chronic wounds. J Wound Care, 2017;26(9):558-68.
- Hunt SD. Topical oxygen-haemoglobin use on sloughy wounds: Positive patient outcomes and the promotion of self-care. Wounds UK, 2015;11(4):90-5.
- Hunt SD, Elg F, Percival SL. Assessment of clinical effectiveness of haemoglobin spray as adjunctive therapy in the treatment of sloughy wounds. J Wound Care, 2018;27(4):210-9.




