Volume 31 Number 3
Introducing a hydrofiber dressing containing ionic silver and an antibiofilm formulation to manage biofilm and to aid in the healing of a chronic left ankle wound
Ian Whiteley
Keywords wound, biofilm, chronic, hard-to-heal
For referencing Whiteley I. Introducing a hydrofiber dressing containing ionic silver and an antibiofilm formulation to manage biofilm and to aid in the healing of a chronic left ankle wound. Wound Practice and Research 2023; 31(3):146-151.
DOI
https://doi.org/10.33235/wpr.31.3.146-151
Submitted 21 March 2023
Accepted 11 May 2023
Abstract
Aims To review the progress of a chronic left ankle wound via telehealth. To initiate appropriate wound therapies and review progress towards the achievement of autolytic debridement, management of biofilm and ultimately wound healing.
Methods This is a case study to which the patient provided written consent. Telehealth was predominantly used to assess and treat this chronic wound with wound management strategies and products altered based on wound progress. Wound care was targeted at debridement, exudate management, protection of peri-wound skin, control of bacterial colonisation and treatment of biofilm.
Results Telehealth suited the patient’s lifestyle and work schedule. Telehealth did not allow for mechanical debridement, thus wound products were selected in order to facilitate autolytic wound debridement. The wound made progress with some wound care modalities; however, rapid progress was observed after switching to AQUACEL® Ag+ Extra™ and wound closure was achieved.
Conclusion When a chronic wound fails to make positive progress, biofilm should be suspected. Wound debridement should be undertaken, followed by the use of wound products aimed at managing biofilm and preventing its re-accumulation. This case study demonstrates telehealth can be an appropriate medium for treating motivated patients and was incorporated into this patient’s busy schedule.
Introduction
Chronic / hard-to-heal wounds are defined as wounds that have failed to heal properly during an amount of time that normally should be sufficient to achieve healing1. Chronic wounds may heal at a much slower rate, may only partially heal, or may reoccur after partial or complete healing. Consensus in the literature on ‘time’ as a component of the definition of a chronic wound has not been achieved; however, there are many reports that if a wound has failed to achieve anatomic and functional integrity after 3 months then it is considered to be chronic2. Patients with chronic wounds frequently report lower health-related quality of life (HRQoL) scores in domains related to the duration of the wound, decreased mobility, emotional state, and pain1,3. Furthermore, HRQoL can be adversely affected by wound complications or advancement in severity, which has also been reported to have a negative impact on mental health1. Future studies need to also capture productivity losses, as these compound the healthcare economic losses associated with chronic wounds1. While the exact prevalence of chronic wounds in Australia is unknown, it is currently estimated to be approximately 450,0004,5 and costs the health system over A$3 billion per year or approximately 2% of the health budget4. This falls within the range reported in other developed nations where chronic wounds account for 1–3% of total healthcare expenditure1.
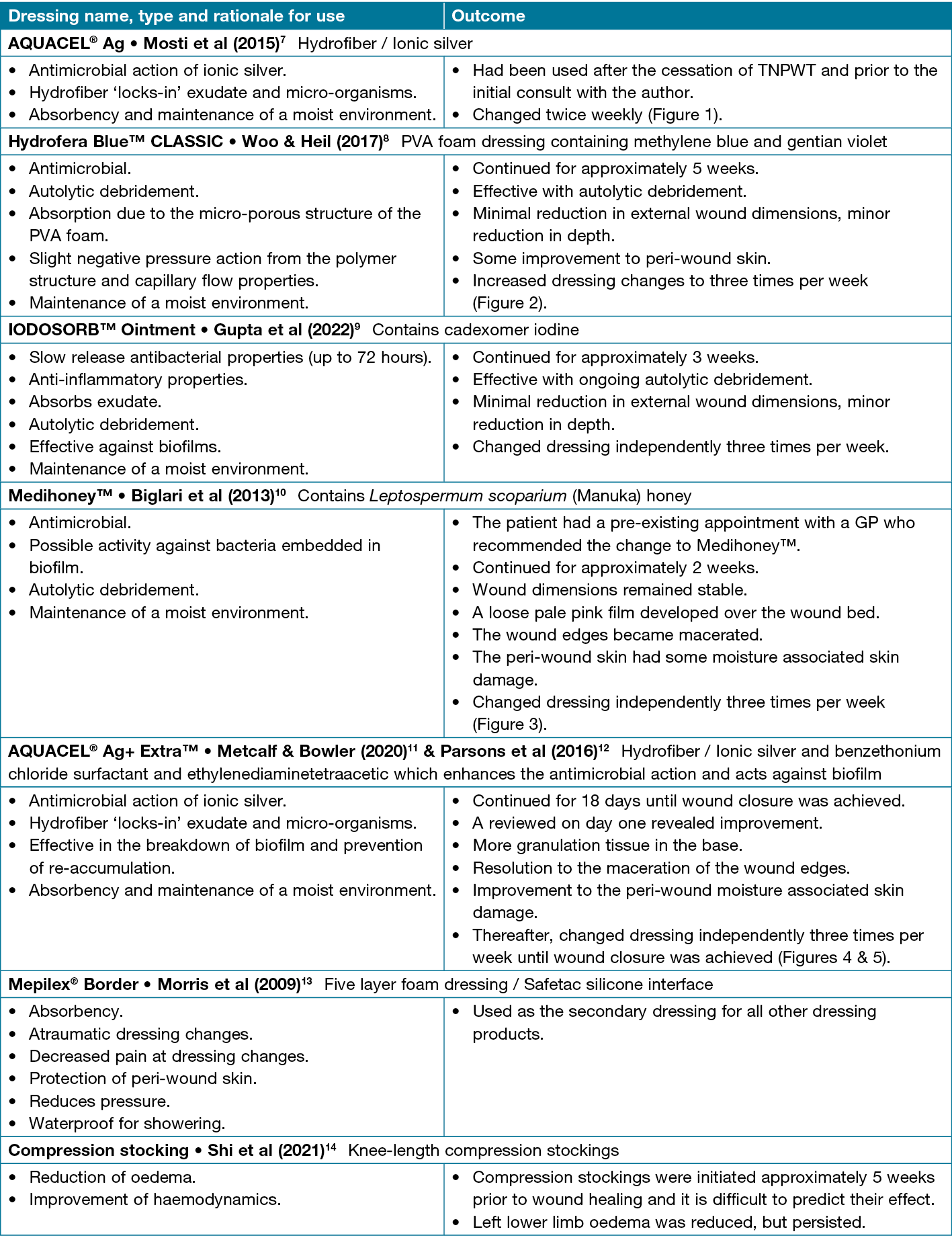
The approach in this case study was to manage exudate and prevent maceration to the peri-wound skin, perform autolytic debridement, manage bacterial burden and treat biofilm. Biofilms are microbial cells enclosed in an extracellular polymeric substance matrix that attach to the surface of wounds6. Biofilms block access to microorganisms in the wound from antibiotics and the body immune response6. While this case study mentions a number of wound products, identified in Table 1, the use of an antibacterial hydrofiber containing ionic silver and an antibiofilm formulation (AQUACEL® Ag+ Extra™) had the greatest impact on the healing of this chronic left ankle wound. An antibacterial hydrofiber containing ionic silver and an antibiofilm formulation is a hydrofiber dressing designed to create an ideal healing environment by controlling exudate15, treating bacteria and preventing biofilm from reforming16. All wound products used in this case study, and outcomes are summarised in Table 1.
Table 1. Wound products used in this case study, with reference to accompanying literature
The patient’s wound was treated at another healthcare facility for many months before being reviewed by the author for a second opinion, as skin grafting had been recommended and the patient wished to avoid further surgery.
The patient signed a NSW Health Consent form authorising the photographs/images to be used for the purpose of education and publication. This is in accordance with Local Health District policy and the photographs/images are retained and managed by the Local Health District in accordance with the State Records Act 1998 and the Health Records and Information Privacy Act 2002.
Background
This case study was written to demonstrate telehealth can be effective in allowing patients with chronic wounds to incorporate self-care into their routine and not be burdened by frequent presentations to hospital clinics for review and dressing changes. Ruth (pseudonym) works in a busy professional client services role in the central business district and was keen to limit travel to healthcare appointments. Ruth is a 51 year-old female who sustained a fracture to her left fibula on 6 January 2022, the result of a fall into a hole on a beach. The fracture was not immediately diagnosed and surgery to pin and plate the fracture was not undertaken until 27 January 2022. The wound initially presented as a blister over the surgical incision site, likely as a result of friction from the orthopaedic boot. Ruth reported the blister developed soon after she began to mobilise; she could feel the boot rubbing. The wound became infected with Pseudomonas, broke down and became a chronic ulcer. Pseudomonas is known to be a present in a high proportion of chronic wounds17.
Surgical debridement of the wound occurred during surgery to remove the pin on 27 May 2022. Topical negative pressure wound therapy (TNPWT) was applied for approximately 2 weeks in conjunction with intravenous antibiotics administered through a Baxter infusor pump and delivered via a peripherally inserted central catheter (PICC). The TNPWT was changed twice weekly at outpatient clinic appointments.
With no resolution of the wound or infection, the plate was removed on 7 July 2022 and a further debridement of the wound was performed. Post-operatively the TNPWT was reapplied for 6 days.
Once TNPWT was ceased, oral antibiotics were commenced and continued for a further 3 months. During this time dressing antimicrobial products such as an antibacterial hydrofiber containing ionic silver (AQUACEL® Ag) and an antibacterial ointment containing cadexomer iodine (IODOSORB™ Ointment) were used with limited success (Table 1)7,9. There is evidence that an antibacterial hydrofiber containing ionic silver can decrease wound size, whereas there is stronger evidence that an antibacterial ointment containing cadexomer iodine can achieve a reduction in wound size and increase the proportion of patients with healed wounds when used in conjunction with compression therapy18. The wound had become a burden to the patient’s wellbeing, with each set back causing more frustration and despair which are common emotions reported in the literature1.
As with the patient in this case study, the path to healing of a chronic wound can be a long-term process of introducing different therapies; these can achieve varied outcomes and do not always result in complete wound healing19. Patients can begin to lose hope when expert clinicians cannot provide certainty as to when their wound will heal, if ever19. Patients often feel they are losing self-control in their daily life as they require external care for their chronic wound2 which leads to hopelessness and discouragement. Patients may lose sight of future dreams which no longer seem attainable as there is uncertainty of when the next wound intervention may become necessary3.
Ruth lives alone and went through periods of pain which impacted on mobility; her usually busy social and travel routine was disrupted. Having a visible wound dressing and wearing compression stockings during the heat of summer also added to the strain of having a chronic wound and self-image concerns19. All treatment received up to this point had been through her local hospital where she had been happy with the service provided; however, it was becoming costly and time consuming with each appointment being a taxi ride from home or work.
Ruth was eventually referred to a plastic surgeon for consideration of skin grafting. Being reluctant to undergo further surgery, she sought a second opinion on wound care options from the author.
Initial assessment
During the first telehealth consultation, the examination revealed a chronic ulcer on the lateral side of the left lower leg. This measured approximately 3cm in width, 2cm in height and 0.5cm in depth. There was slough in the base and the surrounding tissue was indurated (Figure 1). A low level of exudate was reported.
Management plan/results
At the time of the initial assessment, treatment with an antibacterial foam dressing (Hydrofera Blue™ CLASSIC) was initiated and an adherent silicone foam was used as the secondary dressing (Table 1)8. The patient was encouraged to actively participate in the assessment, treatment plan and ongoing wound care19. Although Ruth had a great relationship with the nurses in the outpatient department she had been attending, she had become despondent about attending regular appointments and the disruption to her life and work schedule.
An antibacterial foam dressing has an antimicrobial action resulting from methylene blue and gentian violet and also has a negative pressure action8 which achieved autolytic debridement and a reduction in the wound depth (Figure 2). However, after several weeks, the wound progress stalled and further improvements were not achieved. At this time an antibacterial ointment containing cadexomer iodine ointment was introduced with the aim of continuing autolytic debridement and the provision of a moist antibacterial wound environment (Table 1)9. This therapy was continued for approximately 3 weeks until the patient attended a pre-existing appointment with a GP specialising in wound care who recommended the use of an antibacterial dressing containing Manuka honey (Medihoney™) with a foam dressing with a silicone border continued as the secondary dressing (Table 1)10. The wound failed to improve while being treated with an antibacterial dressing containing Manuka honey and the edges of the wound became macerated due to the added moisture (Figure 3). Therefore, it was recommended this therapy be ceased after 2 weeks.
Knee-length compression stockings were introduced as it has been demonstrated patients are more likely to experience complete wound healing18, in a shorter time, and may experience less pain and improved HRQoL with consistent use14. Despite Ruth not having been investigated for vascular insufficiency, compression stockings resulted in decreased swelling and oedema and many have contributed to improvement in the peri-wound skin condition.
Wound consults with the author’s clinic were predominantly by telehealth, with photos being shared electronically at regular intervals. The wound was being washed well in the shower between dressing changes and the patient was able to attend to dressings independently rather than going to her local wound clinic. The aim was to encourage the patient to actively participate in the assessment and treatment plan19 and to achieve autolytic debridement which is a vital part of wound hygiene in chronic wounds17. It is assumed the majority of chronic wounds contain biofilm9,17; therefore, treatment needs to involve wound therapies that treat the bacteria, disrupt the biofilm, treat residual biofilm and prevent the reformation of the biofilm11,17.
On 24 February 2023 treatment with an antibacterial hydrofiber containing ionic silver and an antibiofilm formulation was commenced with the aim of treating and preventing biofilm12 and a foam dressing with a silicone border was used as a secondary dressing (Mepilex® Border)13 (Figure 3).
The day following the introduction of an antibacterial hydrofiber containing ionic silver and an antibiofilm formulation Ruth made unscheduled contact to report she was excited as there had been a noticeable improvement. During this telehealth consultation it was evident the peri-wound moisture associated skin damage and induration had improved (Figure 4).
After a journey of 10 months with a chronic wound, closure was finally achieved (Figure 5). The wound healed within just 18 days of switching to an antibacterial hydrofiber containing ionic silver and an antibiofilm formulation. With all other factors remaining stable, this can only be attributed with the novel properties in an antibacterial hydrofiber containing ionic silver and an antibiofilm formulation.

Conclusion
In chronic / hard-to-heal wounds biofilm should be suspected. Wound cleansing and debridement should be part of routine wound care, with the aim of disrupting the biofilm, targeting the residual biofilm, and preventing re-formation; an antibacterial hydrofiber containing ionic silver and an antibiofilm formulation can play a role in achieving this. If manual debridement is required, patients will need to attend an outpatient clinic. However, in this case, the selected wound products achieved autolytic debridement. Frequent review and the provision of support via telehealth minimised the disruption to the patient’s life and achieved the desired outcome of wound healing without further surgical intervention.
Acknowledgements
I would like to acknowledge the patient who consented to the sharing of the images contained in this manuscript and for allowing me to tell her story. She also reviewed the manuscript prior to submission.
Conflict of interest
The author declares no conflicts of interest.
Ethics statement
An ethics statement is not applicable.
Funding
The authors received no funding for this study.
Author(s)
Ian Whiteley
Nurse Practitioner, Clinical Senior Lecturer, The University of Sydney (Sydney Medical School), Level 1 West,
Concord Repatriation General Hospital, Concord, NSW 2139, Australia
*Corresponding author email ian.whiteley@health.nsw.gov.au
References
- Olsson M, Järbrink K, Divakar U, Bajpai R, Upton Z, Schmidtchen A. The humanistic and economic burden of chronic wounds: a systematic review. Wound Rep Reg 2019;27:114–125.2.
- Kyaw BM, Jarbrink K, Martinego L, Car J, Harding K, Schmidtchen A. Need for improved definition of “chronic wounds” in clinical studies. Acta Derm Venereol 2018;98:157–158. doi:10.2340/00015555-2786
- Renner R, Erfurt-Berge C. Depression and quality of life in patients with chronic wounds: ways to measure their influence and their effect on daily life. Chron Wound Care Manage Res 2017;4:143–151.
- Australian Medical Association. 2022. Solutions to the chronic wound problem in Australia; 2022 [cited 2023 April 21]. Available from: https://www.ama.com.au/sites/default/files/2022-08/research-report-solutions-to-the-chronic-wound-problem-in-australia.pdf
- McCosker L, Tulleners R, Cheng Q, Rohmer S, Pacella T, Graves N, Pacella R. Chronic wounds in Australia: a systematic review of key epidemiological and clinical parameters. Int Wound J 2019;16:84–95.
- Sharma D, Misba L, Khan AU. Antibiotics versus biofilm: an emerging battleground in microbial communities. Antimicrob Resist Infect Cont 2019;8(76):1–10.
- Mosti G, Magliaro A, Mattaliano V, Picerni P, Angelotti N. Comparative study of two antimicrobial dressings in infected leg ulcers: a pilot study. J Wound Care 2015;24(3):121–127.
- Woo KY, Heil J. A prospective evaluation of methylene blue and gentian violet dressing for management of chronic wounds with local infection. Int Wound J 2017;14(6):1029–1035.
- Gupta S, Shinde S, Shinde RK. Topical management of wound: a narrative review of cadexomer iodine ointment versus povidone iodine ointment. Cureus 2022;14(4):e24598.
- Biglari B, Moghaddam A, Santos K, Blaser G, Buchler A, Jansen G, Langler A, Graf N, Weiler U, Licht V, Strolin A, Keck B, Lauf V, Bode U, Swing T, Hanano R, Schwarz NT, Simon A. Multicentre prospective observational study on professional wound care using honey (Medihoney™). Int Wound J 2013;10:252–259.
- Metcalf DG, Bowler PG. Clinical impact of an anti-biofilm hydrofiber dressing in hard-to-heal wounds previously managed with traditional antimicrobial products and systemic antibiotics. Burns Trauma 2020;8:tkaa004.
- Parsons D, Meredith K, Rowlands VJ, Short D, Metcalf DG, Bowler GP. Enhanced performance and mode of action of a novel antibiofilm hydrofiber wound dressing. BioMed Res Int 2016; Article ID 7616471.
- Morris C, Emsley P, Marland E, Meuleneire F, White R. Use of wound dressings with soft silicone adhesive technology. Paed Nurs 2009;21(3):38–43.
- Shi C, Dumville JC, Cullum N, Connaughton E, Norman G. Compression bandages or stockings versus no compression for treating venous leg ulcers (Review). Cochrane Database System Rev 2021;7. Art. No.:CD013397.
- Walker M, Bowler P, Cochrane C. In vitro studies to show sequestration of matrix metalloproteinases by silver-containing wound care products. Ostomy Wound Manage 2007;53(9):18–25.
- Bowler PG, Parsons D. Combatting wound biofilm and recalcitrance with a novel anti-biofilm Hydrofiber® wound dressing. Wound Med 2016;14:6–11.
- Murphy C, Atkin L, Swanson T, Tachi M, Tan YK, Vega de Ceniga M, Weir D, Wolcott R. International consensus document. Defying hard-to-heal wounds with an early antibiofilm intervention strategy: wound hygiene. J Wound Care 2020;29 (Suppl 3b):S1–28.
- Tricco AC, Antony J, Vafaei A, Khan PA, Harrington A, Cogo E, Wilson C, Perrier L, Hui W, Straus SE. Seeking effective interventions to treat complex wounds: an overview of systematic reviews. BMC Med 2015;13(89):1–23.
- Hussey G, Young T. The impact of psychological factors on wound healing. Wounds Int 2020;11(4):58–62.



