Volume 32 Number 2
The effectiveness of a silicone tape intervention in reducing N95 mask-related pressure injuries for healthcare professionals in an inpatient hospice setting
Yee Y Chang, Joshua Lai, Joyce LK Goo
Keywords healthcare professionals, COVID-19, N95 mask, silicone tape, facial device related pressure injuries
For referencing Chang YY, Lai J and Goo JLK. The effectiveness of a silicone tape Intervention in reducing N95 mask-related pressure injuries for healthcare professionals in an inpatient hospice setting. Wound Practice and Research. 2024;32(2):100-107.
DOI
10.33235/wpr.32.2.100-107
Submitted 9 November 2023
Accepted 20 February 2024
Abstract
During the COVID-19 pandemic, healthcare professionals in Singapore were required to wear N95 masks as part of their personal protective equipment. This led to multiple cases of facial device-related pressure injuries (DRPIs).
Aim A quality improvement project was conducted to investigate the effectiveness of silicone transparent adhesive tape in reducing DRPIs in an inpatient hospice setting.
Method A pre-intervention survey was conducted to determine the prevalence of DRPIs among healthcare professionals, and a post-intervention survey was administered to assess the effectiveness and staff perceptions regarding of the use of prophylactic silicone adhesive tape.
Results Overall, 67.2% (n=45) of healthcare professionals had one or more DRPIs, during the pre intervention survey which resulted in discomfort, lowered their self-esteem, and reduced their ability to concentrate. Following the application of the prophylactic silicone adhesive tape to the facial nasal bridge and bilateral cheekbones (n=29), 82.7% (n=24) of participants reported greater comfort and would recommend the intervention to others, as it improved their physical and mental well-being, and their ability to concentrate at work.
Conclusion The prophylactic application of transparent adhesive silicone tape under respiratory masks during COVID-19 has been shown to be a successful intervention in the inpatient hospice setting. Its continued use whenever facial masks need to be worn is recommended.
Introduction
The COVID19 pandemic presented an unprecedented public health challenge to the world. In March 2020, the World Health Organization (WHO) declared the COVID-19 infectious disease as a global pandemic1 as high transmissibility led to a dramatic increase in COVID-19 cases worldwide. The COVID-19 respiratory droplets can be transmitted via coughing, sneezing, contact with contaminated surfaces, or even through inhaled aerosols. It is essential for healthcare professionals to protect themselves by wearing a secure, well-sealed mask prior to entering clinical areas. In Singapore, stringent public health measures were instituted to limit the spread of the virus, such as mandating all healthcare professionals to wear personal protective equipment, which included the N95 mask. As a result, the incidence of device-related pressure injuries (DRPIs) increased during the COVID-19 period across most healthcare sectors,2-4 however, limited reports focus on community settings.
DPRIs are defined as facial skin injuries, skin tears, and lesions among clinical teams due to prolonged wearing of personal protectives masks and are commonly reported in various clinical settings.
They are also sometimes called device-related pressure ulcers (DPRUs). The international consensus panel noted that: “A DRPU, which is caused by a device or object, is distinct from a PU [pressure ulcer], which is caused primarily by body weight forces. The localised nature of device forces results in the appearance of skin and deeper tissue damage that mimics that of the device in shape and distribution.”2(pS5)
In a Singapore Inpatient Hospice and Palliative Care Service (IHPCS), healthcare professionals had to adhere to strict requirements to wear PPE. Due to the prolonged period of use, it was not long before staff complained of mask-related DRPIs. When N95 masks are immobilised on facial skin with elasticated string, frictional forces and pressure are applied at the device-skin interface, leading to visible tissue damage of the skin’s surface, as well as subdermal damage. In addition, excessive sweating and moisture retention in the N95 mask during respiration can lead to overhydration of the skin, softening and increasing the permeability of the stratum corneum. This decreases the skin’s tolerance, increasing susceptibility to damage.2
Common sites for facial DRPIs included the nasal bridge, cheekbones, and chin.4-6 To address the DRPI-related discomfort, pain, and potential complications,7 staff reported using various types of tapes or dressings; including adhesive plaster, micropore tape, semi-permeable film, hydrocolloid sheets, foam dressings, and, in some instances, gauze (Figure 1). However, literature has shown that the frequent use of strong adhesive products may amplify the risk of skin stripping or medical adhesive-related skin injuries (MARSIs).4,8 The National Pressure Injury Advisory Panel (NPIAP)9 stated that applying thick or porous outer foam dressing increases the risk of N95 mask air leakage, potentially resulting in virus contamination when wearing the mask. Several published reports discussed the use of prophylactic dressings to reduce these complications; however, in many instances, mask fit was reported to be compromised.3,7

Figure 1. (a) Healthcare professionals self-managed facial device-related pressure injuries with adhesive plaster
(b) Other topical products were also used, without an Occupational Safety and Health Administration mask fitting test
Considering the significant pain caused by DRPI and MARSIs, and the permanent scarring and distress they cause, there was a pressing need to test viable strategies that could mitigate these issues as soon as possible. With its ability to conform to the skin easily with consistent adhesion over time, and its breathable and waterproof properties, medical-grade silicone adhesive tape lowers surface tension, and is suitable for sensitive skin. These qualities were considered to ensure ease of repeated application and removal without causing MARSIs11 and discomfort.
To examine if the silicone tape has the potential to reduce facial DRPIs, a quality improvement project was undertaken. Specifically, the aim of the project was to reduce N95 mask-induced facial DRPI in an inpatient hospice setting by piloting the usage of silicone adhesive tape when wearing the N95 mask. By preventing the N95 mask from contacting the skin directly, the primary objective was to determine if there was a reduction in pain intensity associated with facial DRPIs when the silicone adhesive tape was used. The secondary objectives were to determine if there was an association between the duration of N95 mask wearing, mask type and the presence of DRPIs.
Methods
Given the problem’s urgency, the management approved the project but closely supervised the team to ensure data confidentiality and protocol adherence (Figure 2). A small working group led by two nurse clinicians, one of whom is a wound ostomy continence practitioner, was formed to undertake this initiative. A survey was conducted to quantify the scope of the problem before initiating the intervention and a post-intervention survey was administered to evaluate its effectiveness and staff’js satisfaction. Both surveys were hosted online. A convenient sample of healthcare professionals were invited to participate in the intervention.
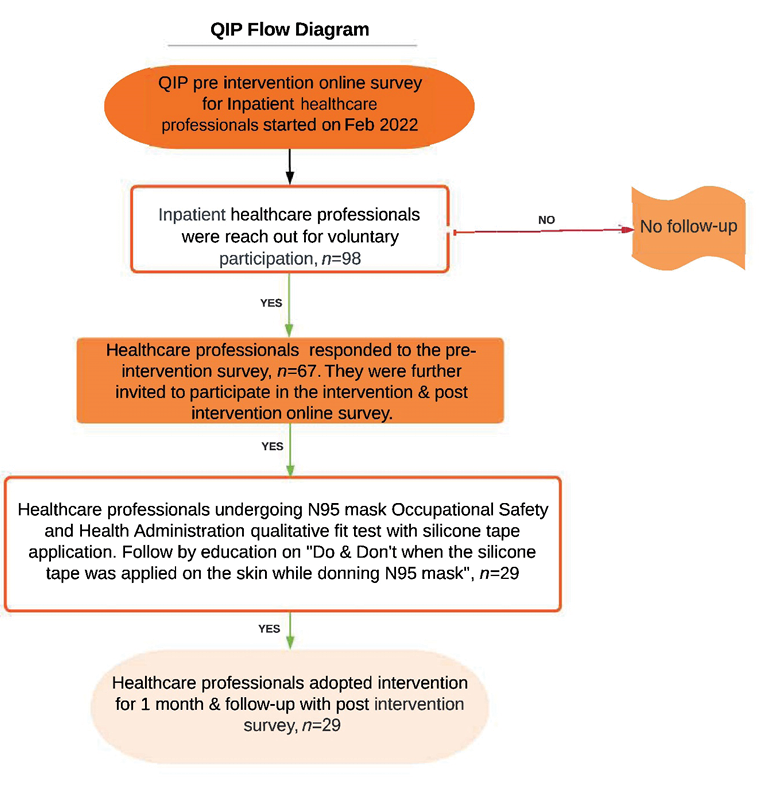
Figure 2. Quality improvement project (QIP) flow diagram
The NPIAP9 suggests that N95 masks must be re-fitted when dressing products are used in-situ; hence, upon completion of the pre-intervention survey, participants were invited to undergo the N95 mask Occupational Safety and Health Administration (OSHA) qualitative fit test12 with silicone adhesive tape applied on facial skin to specific anatomical locations (nose bridge, cheekbones, or both) under the N95 mask. All participants were required to perform a seal check before the mask fit test13 (Figure 3). At the time of the project, the models of N95 masks used in the hospice were BYD™, Halyard FluidShield™ regular, 3M™ 1870+, 8110, 8210, 1860, and 1860S.
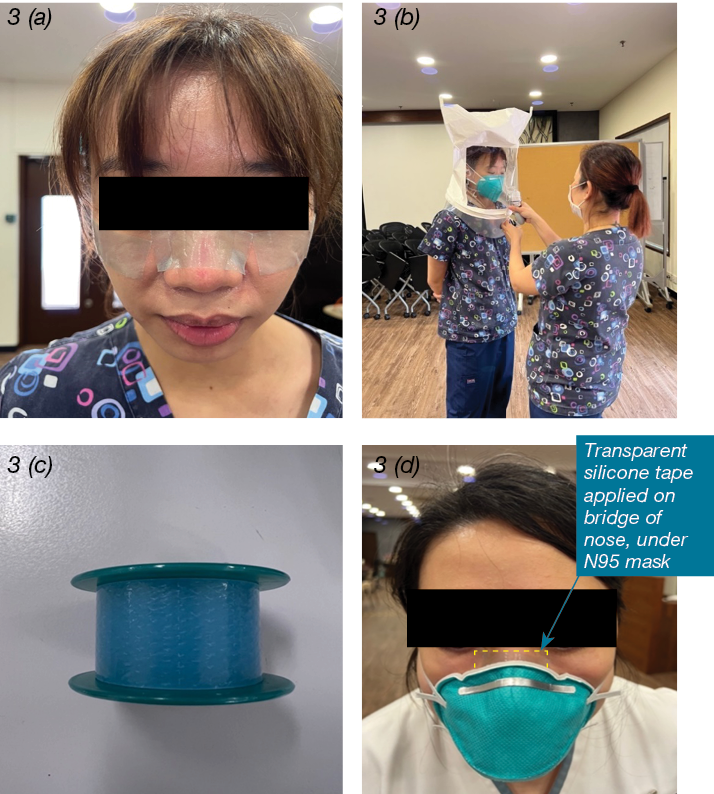
Figure 3. (a) Application of transparent silicone tape on facial nose bridge and bilateral cheekbones, (b) Undergoing N95 mask Occupational Safety and Health Administration qualitative fit test, (c) Transparent silicone tape 2.5cm width as intervention, (d) Silicone tape applied on facial pressure points under the N95 mask
In addition, the working group developed educational materials to guide participants on the “Dos and don’ts when the silicone tape was applied on the facial skin while donning the N95 mask” (Figure 4). Participants were advised to apply the silicone tape for one month while wearing their masks. At the end of the one month, they were asked to complete a post-intervention survey to measure the effectiveness of and evaluate their perceptions and satisfaction towards the intervention.
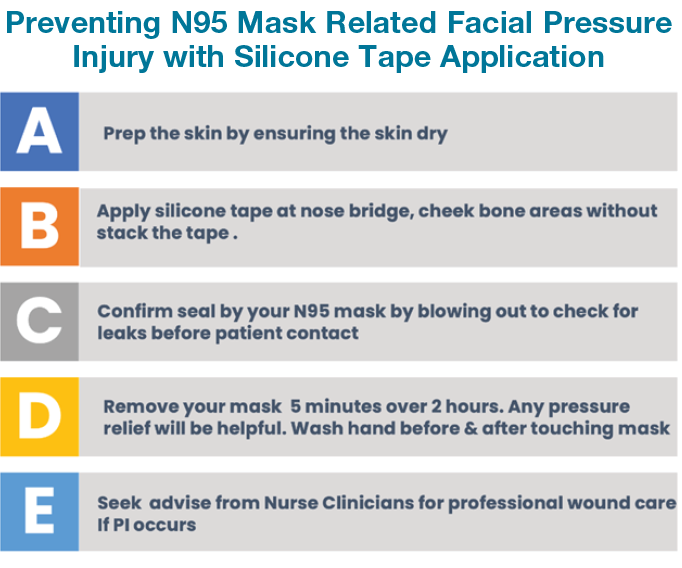
Figure 4. Dos and don’ts when the silicone tape was applied on the facial skin while donning the N95 mask”
Data Collection and Statistical Analysis
The online survey included questions on demographic as well as the types of N95 masks worn, the incidence of skin injuries caused by wearing N95 masks, the duration of mask-wearing, and the pain intensity pre and post-intervention using a numerical rating scale. Participants were asked to rate their level of pain when wearing an N95 mask on a scale of 0 to 10. Semi-structured questions were used to elicit responses to problems that arose with wearing N95 masks, and their perceptions, and usefulness of the intervention (Appendix 1). The survey was administered via two methods: (1) an email to all inpatient-facing healthcare professionals and (2) a quick response (QR) code to the survey pasted on the inpatient ward nurses’ counter, tea room, and clinical offices. Data collection occurred during the first two weeks of February 2022. Participation was voluntary. Verbal consent was sought from participants to use their photos and data was de-identified. Participants’ demographic and characteristics of DRPIs were summarised using descriptive statistics.
A paired sample t-test was used to compare pain intensity pre and post-intervention, while an independent samples t-test was used to analyse the relationship between duration of N95 mask wearing and the presence of DRPI. To examine the relationship between the type of N95 mask worn and the presence of DRPI, a chi-square test was performed. All analyses were performed using IBM SPSS® Statistical Software Version 25.0. P<0.05 was considered statistically significant.
Qualitative Analysis
The open-ended responses were analysed using Thematic Analysis (TA), based on the six step framework developed by Braun and Clarke.14 The responses were first read multiple times to ensure familiarity before being coded semantically. The codes were then examined with codes that shared similar characteristics grouped to generate initial themes and sub-themes using an inductive approach. The themes and sub-themes were then refined iteratively by re-reading the responses, so that a meaningful picture that was coherent with the dataset as a whole, and that addressed the project objectives, was provided. To ensure anonymity, serial numbers were used when particpants’ responses had to be quoted in the report.
Results
Out of 98 patient-facing healthcare professionals employed in the hospice, 68.4% (n=67) responded to the pre-intervention survey: 94% (n=63) were females and 85%, (n=57) were nurses. The rest of the sample, 15%, (n=10) consisted of medical social workers, allied health therapists, a pharmacist, a pharmacy technician, and a doctor.
The prevalence of DRPIs was 67.2% with 45 healthcare professionals reported having at least one DRPI. A total of 93 DRPI were identified; 37.6% (n=35) on the bridge of the nose, 27.9% (n=26) each on the zygomatic arch and ear, and 6.5% (n=6) on the mandible (Table 1).
Table 1: Demographic and characteristics of DRPIs observed (Pre-intervention)
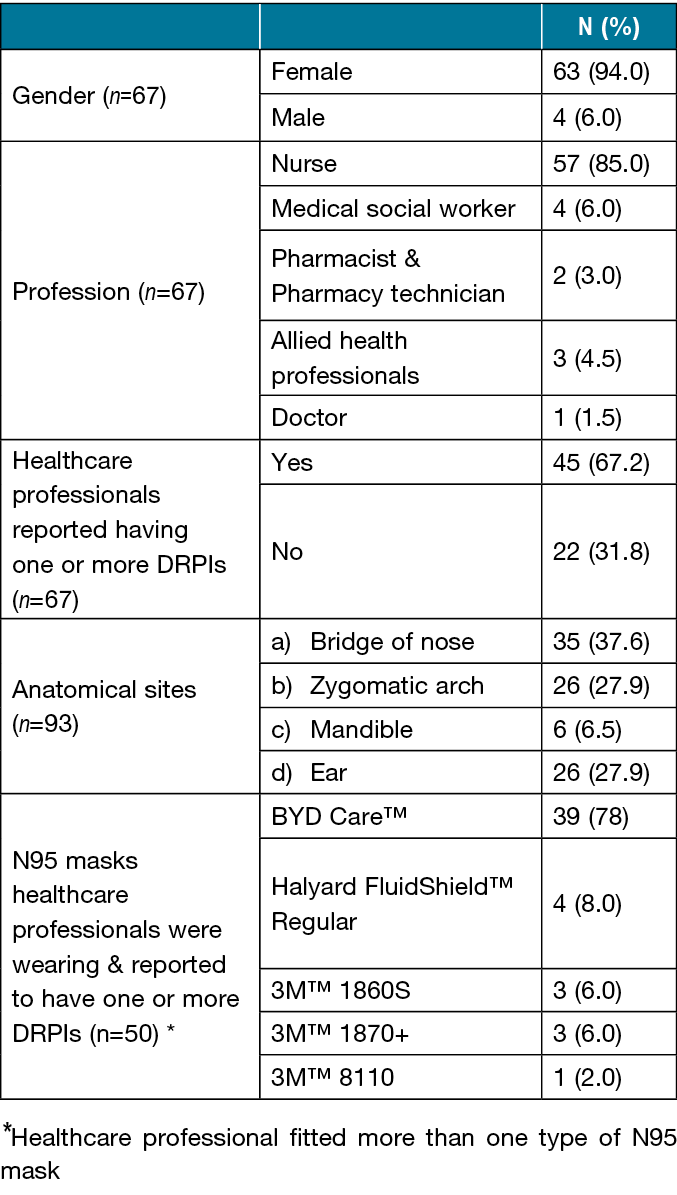
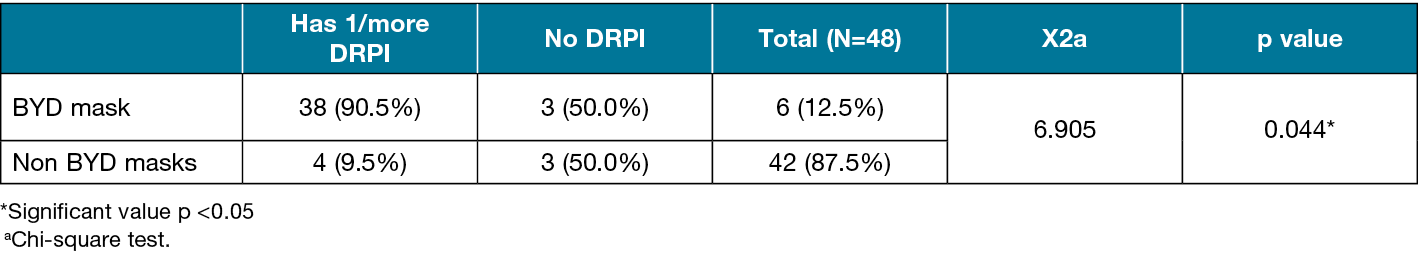
For healthcare professionals who had reported having one or more DRPIs, BYD Care™ (Precision Manufacture Co. Ltd) N95 mask was reported by most to be most likely to cause skin redness, facial skin injury, blisters, lesions, or ulcers on the face upon wearing (n=39; 78%). In contrast, only 8% (n=4) reported having problems with Halyard FluidShield™ Regular, and 6% (n=3) each reported issues with 3M™ 1860S and 1870+. Only one participant perceived 3M™ 8110 to cause DRPIs.
Among the 45 respondents who had facial DRPIs, 49% (n=22) did not apply employ any strategies to prevent N95 mask-related DRPIs before donning the mask. For those who tried to reduce the occurrence and severity of the lesions, seven participants used more than one strategy. The participants shared that they applied skin moisturiser, 41% (n=13) and 28% (n=9) used adhesive plaster. A minority of the participants applied gauze and tissue paper, 9.3% each (n=3), to cushion the bony prominences. Only one participant applying hydrocolloid sheet, silicone tape, medicated ointment or cream, skin barrier protective cream.
Overall, 43.3% (n=29) of the healthcare professionals indicated that N95 mask-related DRPIs had adversely impacted their lives and participated in the intervention, as well as the post-intervention survey. The mean pain score reduced significantly from 3.97 (SD=2.50) pre-intervention to 2.20 (SD=1.81) post-intervention, p =0.003 (Table 2).
Table 2: Pre and post-intervention pain score
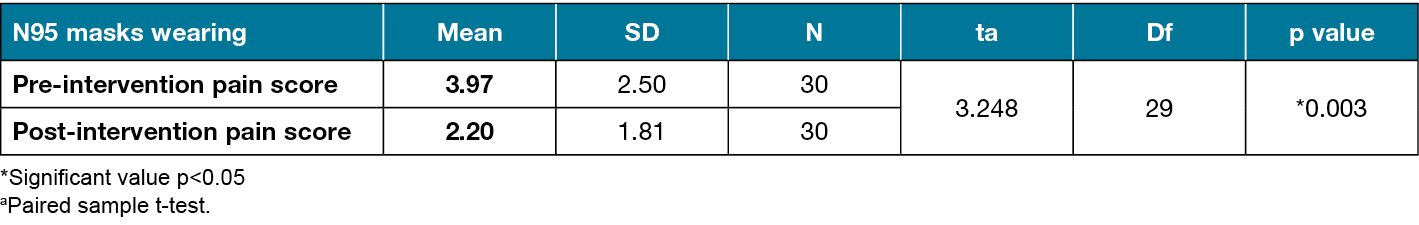
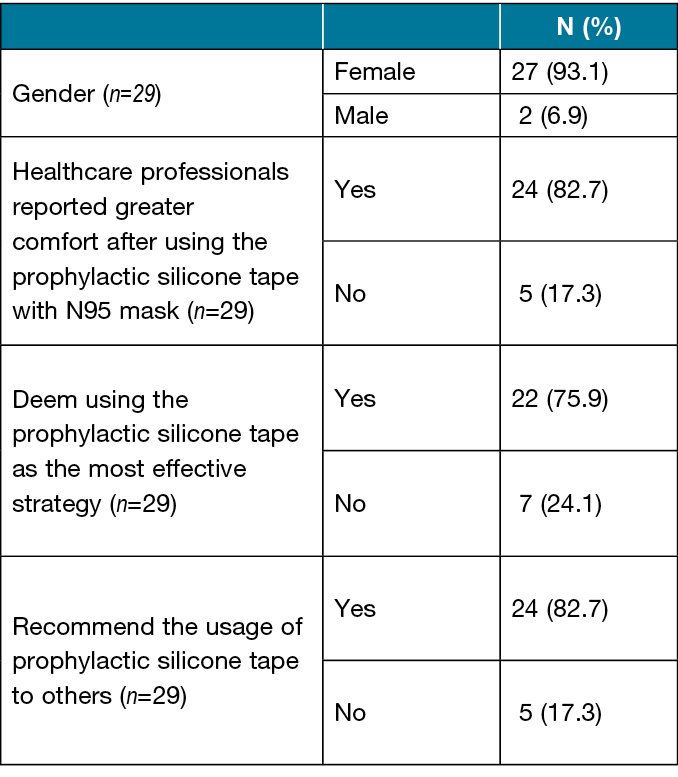
In addition, 82.7% (n=24) of healthcare professionals reported greater comfort after applying the silicone tape with N95 mask wearing and stated they would recommend the intervention to others. Among those who used the silicone adhesive tape, 75.9% (n=22) stated that the tape was the most effective solution for minimising the discomfort caused by N95 masks (Table 3).
Table 3: Demographic and participants’ responses towards the intervention (Post-intervention)
Of the 45 participants who had DRPIs, 62.2% (n=28), reported wearing N95 masks for an average duration of 2 to 4 hours during the pandemic. There was no statistically significant difference in the duration of mask wearing between healthcare professionals who had one or more DRPIs [mean (SD) = 3.89 (1.03)] and those who had none [mean (SD): 3.82 (0.80) hours], p =0.778 (Table 4). However, there was a statistically significant association between mask type and presence of DRPIs. A significantly higher proportion of participants who wore BYD masks had DRPIs (90.5%) compared to those who wore non-BYD masks (9.5%), p = 0.044 (Table 5).
Table 4. Average duration of N95 mask wearing with DRPIs development
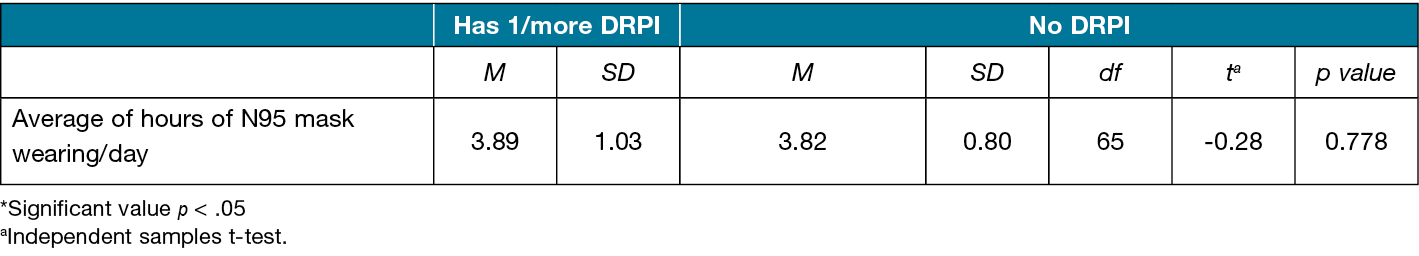
Table 5. DRPIs and N95 mask types
Open-ended responses
Before the intervention, participants reported experiencing feelings of discomfort, poor self-esteem, and reduced work performance because of the DRPIs associated with mask wearing.
Discomfort
Pain due to the prolonged wearing of N95 masks was significant among participants’ responses.
001: “It’s very uncomfortable and painful when there is redness.”
Poor self-esteem
Mask-induced pressure injuries resulted in unsightly scars on their faces. Facial injuries significantly affected participants’ self-esteem.
003: “It makes me more concerned with my skin. I’m unsure whether it will leave a permanent mark or not after donning.”
Reduced work performance
Participants shared that the discomfort and irritation related to the N95 mask were significant distractions that led to poorer work concentration.
007: “Constant adjusting of the mask is irritating and obscures my sight as well because if [not] fitted properly, moisture fogs up my glasses.”
After a month of applying the silicon tape, participants shared that the intervention improved their quality of life. Specifically, it improved their well-being and ability to concentrate at work.
Improved wellbeing
Participants perceived an improvement in both physical and mental well-being. The reduction in pain and discomfort improved their physical wellbeing, while the reduction in psychological distress improved their self-esteem and mental well-being.
001: “Feels painless whenever I apply it and also easy to apply it.”
002: “It lessens my worry of having facial skin tears due to pressure from the N95 mask.”
Improved ability to concentrate at work
With the addition of silicon tape to the mask-wearing routine, participants reported that the increased comfort enabled them to focus and concentrate at work. Consequently, their mood improved.
001: “Easy to breathe and comfortable. Happy to work during our shift.”
002: “Felt more comfortable and able to focus more on my work.”
Participants also provided feedback regarding the intervention. Although they appreciated the intervention, the silicone tape has its limitations and suggested areas for improvements.
Appreciation for intervention
Participants expressed their heartfelt gratitude towards the management for coming up with the silicone tape intervention to ease the discomfort caused by the N95 masks.
002: “Silicone tape is very useful for N95 masks during our working place. Feel free and comfortable and good to breathe.”
Limitations of silicone adhesive tape
While the intervention was generally well-received, for some individuals, their unique circumstances affected the use of the silicone tape.
001: “Not suitable for my skin type.”
002: “If the face is too sweaty or oily during sponging/showering patient or wound dressing procedure, the silicone tape can easily wear off too.”
Suggestions for improvement
Participants highlighted some suggestions to improve the intervention based on their experiences and observations.
001: “[mask] should be changed if sweating. Or else itchy.”
002: “I think the silicone tape needs to be thicker.”
Discussion
The nurse management team in an inpatient hospice in Singapore initiated a quality improvement project when the healthcare professionals gave feedback that they were experiencing significant discomfort during their shifts due to N95 mask-induced DRPIs. In total, 67.2% (n=45) of healthcare professionals reported having at least one DRPI. The rate was comparable to the study by Jiang et al5 who included both doctors and nurses and demonstrated a prevalence of 60.2% and 59.1%, respectively. The results demonstrates N95 mask-induced DRPIs was a significant issue within the organisation, and the problem needed to be addressed adequately. The N95 masks used by clinicians in the hospice were supplied by the Singapore Agency for Integrated Care (AIC). Considering the severe shortage of N95 masks at the height of the pandemic, clinicians were thankful for the generous support rendered by the government. However, prolonged and improper fitting of the supplied masks could cause facial DRPIs and significant distress to the healthcare professionals.
The organisation offered a variety of mask types but vertical flat-fold shaped masks (BYD) appeared to be associated with DRPIs, potentially causing greater discomfort. This type of mask made up of two elastic strings at either side of the mask’s edge with a strong metal piece at the nasal bridge location. As most Asians tend to have flatter nasal bridges, it is necessary to tighten the mask strings at greater seal pressure and set the stiff nose clip more firmly in order to obtain a good seal so that protection is not compromised. Because of the greater vertical shearing force, localised skin distortions could ensue.
In order to defeat the pandemic, the organisation had to guarantee the highest level of safety for healthcare professionals tending to patients.7,16 With approval from the upper management, the silicone tape intervention was adopted to lessen the discomfort experienced by staff on the ground.
Medical-grade silicone tape is known for its hypoallergenic composition, adaptability, atraumatic removal capability, comfort, and long-lasting adhesion. The impacted staff enthusiastically embraced the silicone tape intervention, in spite of certain drawbacks, like poor stickiness on oily skin. The transparent appearance of the tape was well-received for aesthetic reasons which improved healthcare professionals’ compliance with the intervention.
Additionally, silicone adhesives offer a safe and effective level of adhesion on facial skin compared to hydrocolloid and other adhesive dressings. Its adhesiveness does not get stronger over time,10 and daily application and removal of silicone tape has not been associated with any reports of trauma or pain. The majority of participants reported a reduction in pain when silicone tape was applied to pressure points on the face while wearing an N95 mask. They also reported greater comfort and would recommend it to others if proven to be effective. This project demonstrated that empathy and astute observations are crucial catalysts for constructive change in the workplace. Besides obtaining the gratitude of employees, the organisation benefitted indirectly from a supportive and compassionate management culture.
Future work in this field
With the stablilisatin of the COVID-19 situation both locally and globally, Singapore declared COVID-19 as endemic in February 2023 with less stringent safety precautions required in the community setting. Given that silicone tape has been demonstrated in this study, and anecdotally in clinical practice, to have the potential to prevent pressure injury when used as a prophylactic skin protection beneath high-risk locations, such as the nasal bridge,19 as well as the generally favourable experiences reported by study participants, the intervention was extended to palliative care patients who are at a high risk of acquiring a DRPI, such as those utilising long-term non-invasive ventilation (NIV).12,18
Literature has shown that using protective dressings, such as silicone on the skin, on a frequent basis is critical for decreasing device-related skin damage and NIV interface air leak.17 Although the number of patients on long-term NIV in an inpatient hospice setting is small, additional research to support this assumption in palliative care patients is warranted, as skin injuries that cause discomfort are expected to significantly affect a patient’s quality of life with social and psychological sequelae. In addition, discomfort and the difficulty maintaining NIV interfaces in place to form a suitable seal while caring for the pressure injury may impair tolerance to NIV and treatment success.17
During the peak of the COVID-19 pandemic, N95 masks were in short supply globally and resources in the inpatient hospice were limited. Given the potential for mask type to be associated with the presence of DRPIs, the considerations in mask procurement in future pandemics should be multi-faceted and not just dependent on its efficacy in preventing transmissibility. This will ensure that healthcare professionals’ physical and emotional well-being are taken care of, even as the organisation adheres to safety regulations.
The silicone tape was a timely intervention during a time when healthcare professionals were required to wear N95 masks for extended periods. While it had its limits, the impacted workers recognised the efforts by the organisation’s management to preserve their safety while ensuring their comfort and wellbeing in the midst of the pandemic and were genuinely grateful.
Limitations
As the survey was conducted in a single inpatient hospice, the generalisability of the results may be limited. Furthermore, because the study sample was predominantly female, the data may not represent the views of male healthcare professionals whose facial structures and pain tolerance may differ.
Additionally, due to the voluntary nature of study participation, there could be section bias. The 67 healthcare professionals who responded to the survey could have a vested interest in pressure injury topics or strong feelings about the intervention and outcome. The self-reporting nature of the study could also threaten the external validity of the findings. Moreover, as participants were followed up a month after using the silicone tape, there could be recall bias. While this limitation was recognised during the project’s conceptualisation, adopting a self-reported study design was inevitable considering the COVID-19 safety measures implemented at the time of the study. Additionally, mandatory mask regulations will likely compel most participants to apply the silicone tape regularly when prolonged mask-wearing during the height of the pandemic.
As the survey was only conducted in English, which is not the first language of many of the recruited participants, their limited language proficiency potentially impacted the richness of open-ended responses. Despite the language barrier, many participants still attempted to elaborate on their feeling towards the intervention. Lastly, as the study team members are from the management, participants may have had reservations about providing negative feedback regarding the intervention for fear of potential repercussions in their performance appraisal. However, the balanced mix of reactions received, suggested that most participants were forthcoming with their feedback. Response bias was likely minimal.
Future studies using a mixed-methods study design with a clear hypothesis is recommended to more definitively determine the effectiveness of the silicone tape intervention. It is also important to consider a balanced gender mix and the utility of intervention in other populations, such as patients or other healthcare professionals.
Conclusions
In summary, this quality improvement project demonstrated the management team’s commitment to ongoing innovation in the face of uncertainty to reduced pain associated with mask wearing experienced by inpatient healthcare professionals. The intervention aimed to support healthcare professionals in difficult situations, by enhancing resilience and mitigating difficulties. It is also hoped that the knowledge gained can be adapted to clinical care of patients in practice.
Acknowledgements
The authors would like to acknowledge the participants that took part in this project and thank them for their time and invaluable contribution. Special thanks to Ms Tay Ri Yin, Ms Lydia Quah, Ms Madelina Lim, Dr Mervyn Koh, the Medical Director, and Ms Chin Soh Mun, the former Director of Nursing, for supporting and facilitating this project. .
Conflict of interest
The authors declare no conflicts of interest.
Ethics statement
An ethics statement is not applicable.
Funding
The authors received no funding for this quality improvement project.
Author(s)
Yee Y Chang1*, Joshua Lai2, Joyce LK Goo3
1Master in Nursing, Wound, Ostomy and Continence Practice, Dover Park Hospice, 1 Tan Tock Seng Link, TTSH Integrated Care Hub, Singapore 307382
²Bachelor of Psychology, Dover Park Hospice, 1 Tan Tock Seng Link, TTSH Integrated Care Hub, Singapore 307382
3Master in Nursing, Dover Park Hospice, 1 Tan Tock Seng Link, TTSH Integrated Care Hub, Singapore 307382
*Corresponding author email yeeyee_chang@doverpark.sg
References
- Ministry of Health Singapore: General Information About Covid-19 [Internet]. Singapore: Ministry of Health; 2021 [updated 2022 March 28; cited 2022 September 5]. Available from: https://www.moh.gov.sg/covid-19/general
- Gefen A, Alves P, Ciprandi G, Coyer F, Milne C, Ousey K, Ohura N, Waters N, Worsley P. Device-related pressure ulcers: SECURE prevention. J Wound Care 2020;29(Sup2a): S1–S52. doi: 10.12968/jowc.2020.29.Sup2a.S1
- Coyer F, Coleman K, Hocking K, Leong T, Levido A, Barakat-Johnson M. Maintaining skin health and integrity for staff wearing personal protective equipment for prolonged periods: a practical tip sheet. Wound Practice & Research [Internet]. 2020 Jun 1;28(2). Available from: https://doi.org/10.33235/wpr.28.2.75-83
- Jiang Q, Song S, Zhou J, Liu Y, Chen A, Bai Y, et al. The prevalence, characteristics, and prevention status of skin injury caused by personal protective equipment among medical staff in fighting COVID-19: a multicenter, Cross-Sectional study. Adv Wound Care [Internet]. 2020 Jul 1;9(7):357–364. Available from: https://doi.org/10.1089/wound.2020.1212
- Jiang Q, Liu Y, Song S, Wei W, Bai Y. Association between N95 respirator wearing and device-related pressure injury in the fight against COVID-19: a multicentre cross-sectional survey in China. BMJ Open [Internet]. 2021 Feb 1;11(2):e041880. Available from: https://doi.org/10.1136/bmjopen-2020-041880
- Aloweni F, Bouchoucha S, Hutchinson A, Ang SY, Toh HX, Suhari NAB, et al. Health care workers’ experience of personal protective equipment use and associated adverse effects during the COVID-19 pandemic response in Singapore. J Adv Nurs [Internet]. 2022 Feb 15;78(8):2383–2396. Available from: https://doi.org/10.1111/jan.15164
- Moore Z, McEvoy N, Avşar P, McEvoy L, Curley GF, O’Connor T, et al. Facial pressure injuries and the COVID-19 pandemic: skin protection care to enhance staff safety in an acute hospital setting. J Wound Care [Internet]. 2021 Mar 2;30(3):162–170. Available from: https://doi.org/10.12968/jowc.2021.30.3.162
- Ratliff CR. Descriptive study of the frequency of medical adhesive–related skin injuries in a vascular clinic. J Vasc Nurs [Internet]. 2017 Jun 1;35(2):86–89. Available from: https://doi.org/10.1016/j.jvn.2017.01.00
- National Pressure Injury Advisory Panel (NPIAP). Position statement on preventing injury with N95 masks [Internet]. 2020. Available from: https://cdn.ymaws.com/npiap.com/resource/resmgr/position_statements/Mask_Position_Paper_FINAL_fo.pdf
- Santos AS, Terra AC, Nogueira JC, Noronha K, De Oliveira Marcatto J, Andrade MV. Silicone tape versus micropore tape to prevent medical adhesive-related skin injuries: systematic review and meta-analysis. J Brasileiro De Economia Da Saúde [Internet]. 2019 Dec 1;11(3):271–282. Available from: https://doi.org/10.21115/jbes.v11.n3.p271-82
- Cutting K. Impact of adhesive surgical tape and wound dressings on the skin, with reference to skin stripping. J Wound Care [Internet]. 2008 Apr 1;17(4):157–162. Available from: https://doi.org/10.12968/jowc.2008.17.4.28836
- U.S. Department of Labor. 1910.134 App A – Fit Testing Procedures (Mandatory). Occupational Safety and Health Administration [Internet]. Available from: https://www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.134AppA
- 3M Science Applied to Life. Respirator protection: fit testing [Internet]. Singapore (SG): 3M Science Applied to Life; 2023 [updated 2023; cited 2023 Aug 13]. Available from: https://www.3m.com.sg/3M/en_SG/respiratory-protection-sg/support/center-for-respiratory-protection/fit-testing/
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol [Internet]. 2006 Jan 1;3(2):77–101. Available from: https://doi.org/10.1191/1478088706qp063oa
- Ryan GW, Bernard HR. Techniques to identify themes. Field Methods [Internet]. 2003 Feb 1;15(1):85–109. Available from: https://doi.org/10.1177/1525822x02239569
- Beng TS, Kim CLC, Shee CC, Ching D, Liang TJ, Kumar MKN, et al. COVID-19, Suffering and Palliative Care: a review. Am J Hosp Palliat Care [Internet]. 2021 Sep 16;39(8):986–995. Available from: https://doi.org/10.1177/10499091211046233
- Alqahtani JS, AlAhmari MD. Evidence based synthesis for prevention of noninvasive ventilation related facial pressure ulcers. Saudi Med J [Internet]. 2018 May 1;39(5):443–452. Available from: https://doi.org/10.15537/smj.2018.5.22058
- Schindler C, Mikhailov T, Fischer K K, Lukasiewicz G, Kuhn E, Duncan L. Skin integrity in critically ill and injured children. Am J Crit Care [Internet]. 2007 Nov 1;16(6):568–574. Available from: https://pubmed.ncbi.nlm.nih.gov/17962501/
- Tayyib N, Asiri MY, Danic S, Sahi SL, Lasafin J, Generale LF, et al. The effectiveness of the SKINCARE bundle in preventing Medical-Device related pressure injuries in critical care units: a clinical trial. Adv Skin Wound Care [Internet]. 2021 Feb 1;34(2):75–80. Available from: https://doi.org/10.1097/01.asw.0000725184.13678.80
Click here to download Apendix 1: N95 Mask related Pressure Injury Survey



