Volume 5 Number 2
Hypocalcaemia on admission is independently associated with morbidity and mortality in trauma patients
Lucy Bridge-Dubarry, Gavin Smith
Keywords hypocalcaemia, trauma patients, fluid resuscitation, lethal diamond
For referencing Bridge-Dubarry L & Smith G. Hypocalcaemia on admission is independently associated with morbidity and mortality in trauma patients. JHTAM 2023; 5(2):10-13.
DOI
https://doi.org/10.33235/JHTAM.5.2.10-13
Submitted 9 May 2023
Accepted 18 September 2023
Abstract
Hypocalcaemia, acute coagulopathy, hypothermia and metabolic acidosis comprise the ‘lethal diamond’, a predictor of mortality in trauma patients. Appreciating the role of hypocalcaemia in the lethal diamond is key to improving outcomes for trauma patients. Current first responder clinical practice guidelines are largely inadequate in addressing the potential for hypocalcaemia, and rarely include measurement of serum calcium, leading to many trauma patients with untreated hypocalcaemia arriving at a hospital’s emergency department. Vasudeva et al.1 conducted a retrospective cohort study that provided an analysis of the link between hypocalcaemia and morbidity and mortality in trauma patients. A critique of this article has been undertaken to inform first responder practice, education and policy development.
Introduction
Worldwide, 11% of all deaths are attributed to traumatic injury1. Of all trauma-associated morbidity and mortality, haemorrhagic shock is the most significant and the most preventable1. The impact of haemorrhagic shock on hypocalcaemia is multifactorial, through initial loss of circulating calcium via exsanguination, chelation of remaining calcium due to the citrate present in resuscitative blood products, and the dilution of serum via crystalloid resuscitation1. Identification of factors impacting hypovolaemic resuscitation can lead to the evolution of therapeutic interventions and resuscitation protocols.
To understand the impact of hypocalcaemia in the setting of major trauma it is necessary to revisit the lethal triad concept (hypothermia, acidosis and coagulopathy)2. Ionised calcium plays an important role in platelet function, haemostasis and cardiac contractility, each of which may negatively impact survivability from major trauma. The introduction of packed red blood cells or large volumes of crystalloid fluid during resuscitation also creates an environment where ionic calcium dilution may be precipitated, thus contributing to acidosis, hypoperfusion and ultimately death in this cohort.
The lethal diamond concept (Figure 1) provides clarity in understanding the role calcium plays in coagulopathy and haemodynamic stability during resuscitation of trauma patients, thus enabling a more complete understanding of the implications of major trauma on physiology and survival3. Vasudeva et al.1 conducted a retrospective cohort study exploring the impact of hypocalcaemia (serum calcium below 2.1mmol/L) utilising a 5-year sample of major trauma patients – those assessed with a Shock Index (SI) of equal to or greater than 1 – on arrival at an Australian major trauma centre (MTC). This study identified a significant association between hypocalcaemia on admission to hospital and morbidity and mortality at discharge1. In this article, a critique of Vasudeva et al.’s study1 will be provided to better inform first responder practice, education and policy development.
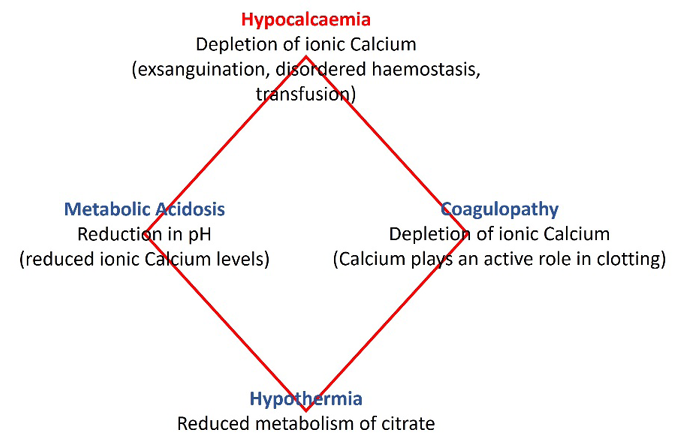
Figure 1. The lethal diamond
Study synopsis
Aim
The study by Vasudeva et al.1 sought to evaluate the association between hypocalcaemia and mortality and morbidity in major trauma patients, which in turn may have implications for changes to current resuscitation practice for first responders.
Method
This study employed a retrospective cohort study design of major trauma patients presenting to a metropolitan Tier 1 MTC (the Alfred Emergency Trauma Centre). The sample consisted of 226 patients who presented between 1 July 2014 and 30 June 2018 with an assessed SI of equal to or greater than 1. Exclusion criteria included pre-hospital blood administration, failure to measure ionised calcium measurement on admission, <18 years old or with SI <1. Data was manually collected by the researchers from the Alfred Trauma Registry and the Alfred Applications and Knowledge Management Department in Melbourne, Australia using strict exclusion criteria (Table 1).
Table 1. Study exclusion criteria (n=15547)

Quantitative data such as clinical measurements of patients including SI, international normalised ratio (INR) and systolic blood pressure (SBP) were gathered (Figure 2) and analysed. Statistical analysis included the use of descriptive statistics, multivariate logistic regression to ascertain independent associations, goodness of fit, and variance inflation factor to exclude multicollinearity. Statistical significance was represented by p<0.05, and STATA software was employed for data analysis.
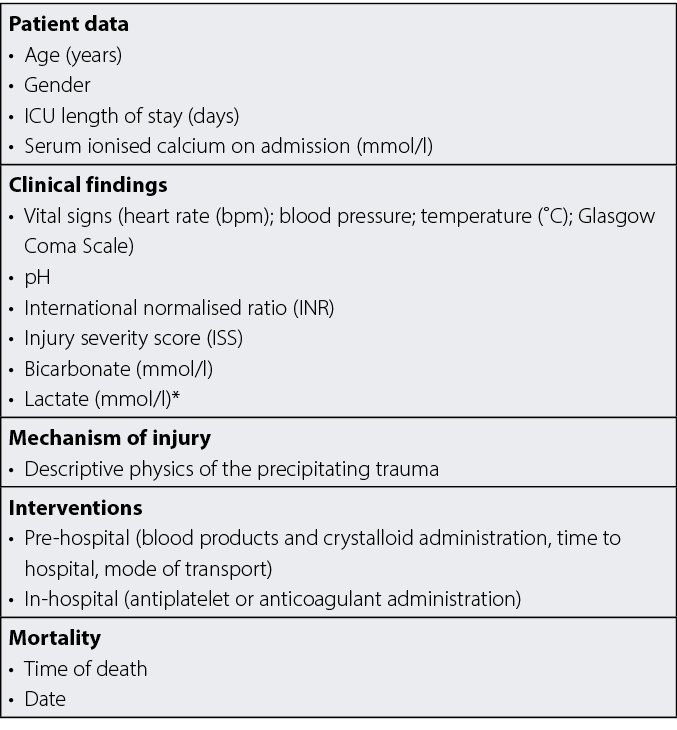
Figure 2. Interventions and outcomes
Results
Statistically significant correlations were noted in patients with hypocalcaemia (and SI >1) on admission and coagulopathy (OR 2.9; 95% CI: 1.01–8.3, p=0.048), blood transfusions required (62.5% in hypocalcaemic versus 37.5% in normocalcaemic patients, p<0.001) and mortality (25.6% of hypocalcaemic versus 15.0% of normocalcaemic patients, p<0.047). Other variables were also noted to be statistically significant for the presence of hypocalcaemia on initial assessment in hospital and included higher injury severity score (ISS) (p<0.001), lower Glasgow Coma Scale (GCS) (p<0.001), lower SBP (p<0.009), and lower bicarbonate (p<0.003). Further, patients with an ISS >45 (OR 0.27; 95% CI: 0.09–0.84, p=0.024), a GCS <9 (OR 3.7; 95% CI: 1.2–11.3, p<0.001), or bicarbonate measurement (OR 0.72; 95% CI: 0.60–0.86, p<0.001) were more likely to suffer coagulopathy.
Hypocalcaemia was commonly identified in presenting trauma patients and was associated with acute traumatic coagulopathy leading to higher mortality and morbidity in this patient cohort. The study findings suggest merit in further research through randomised controlled trials to mitigate the impact of hypocalcaemia in trauma patients. The Critical Appraisal Skills Program (CASP) Cohort Study Checklist was employed to guide and provide rigour to this critique (see Supplementary Item 1).
Critique and application to first responders
Identifying evidence-based elements of change to resuscitation protocols supports continuous improvement in resuscitation practice, and positively impacts patient outcomes. It is understood that hypocalcaemia resulting from hypovolemia and fluid resuscitation may lead to further adverse outcomes for trauma patients1,4–8, including but not limited to, platelet disruption, issues with cardiac contractility and further haemostatic imbalance1. The study by Vasudeva et al.1 provided additional context and evidence to existing research regarding the impact of hypocalcaemia in major trauma patients that can be applied to inform clinical practice guideline development and increase the seamless provision of goal-centred care between the pre-hospital and hospital settings1,3–8.
Although promising, the study by Vasudeva et al.1 is not without limitations. Given the retrospective nature of this study design, investigators faced prior knowledge of exposure and disease among participants during data collection, and thus selection bias may be present. Mitigation was attempted in this study through the de-identification of quantitative data during analysis and subsequent results presentation. The study relied on a 5-year sample of patients within the catchment area of one of two major trauma hospitals in the State, and the reported sample size may reflect the incidence of major trauma in this region or the absence of inclusion of the second MTS in the study. Additionally, future studies may wish to evaluate the ongoing health status of patients beyond their discharge from hospital to identify additional consequences for morbidity that could be considered within the broader impact of mitigating hypocalcaemia in the pre-hospital setting. Patients were reported as alive or dead upon discharge, resulting in a binary outcome measure, and capturing results of instances of morbidity and other adverse outcomes proved challenging. This study did address length of stay in the ICU and the requirement of blood transfusions; however, further analysis through additional studies is warranted to confidently suggest morbidity values.
Mortality associated with hypocalcaemia in major trauma was reported at 25.6% compared to 15% of non-hypocalcaemic major trauma patients (p<0.047), which approximated findings from prior studies1,3,4,6–8. The findings were generalisable to the local population of the studied trauma centre catchment area; however, as this study reports a retrospective cohort with a relatively small sample size (Level 2b within the Hierarchy of Evidence9), clinicians should be guided by recommendations but conscious of new information whilst remaining sensitive to patient preferences7. By identifying acute hypocalcaemia on admission to a major metropolitan trauma centre, it can be inferred that hypocalcaemia is not commonly corrected in the pre-hospital setting. This study supports the findings from earlier studies that early measurement and subsequent pre-hospital administration of calcium in haemorrhagic trauma can mitigate adverse outcomes, including mortality3,5.
Existing fluid resuscitation protocols are unclear as to whether calcium should be administered as part of standard pre-hospital trauma resuscitation practice1,7. Some Australian first responders such as Air Ambulance Victoria employ measurement of ionised calcium in the hypovolaemic trauma setting, enabling administration of 2g within the clinical guideline (and a further 1–2g should the patients calcium level remain below 1.12mmol/l, or routinely following 4 units of packed red blood cells)10. Other emergency rescue services and military personnel currently do not. Whilst an argument could be made that without administering citrated blood products such as whole blood (WB) or packed red blood cells (PRBCs), there is no need for an additional protocol, this study demonstrates that hypocalcaemia can be exacerbated by crystalloid resuscitation alone, and that pre-hospital providers are currently aware of (and responding to) the potential for hypocalcaemia in trauma patients within their clinical guidelines10.
First responders typically work in unpredictable and austere environments and resourcing them appropriately gives them and their patients the best opportunity for positive outcomes. Understanding the association between hypocalcaemia and comorbidities in trauma patients helps inform future practice by providing evidence to support the administration of calcium in a trauma setting. This could apply to first responders including civilian and military operators, trauma centres, resuscitation teams, emergency departments, or any emergency service. In austere environments with expected prolonged pre-hospital care, first responders may need to provide more definitive care during fluid resuscitation. This includes identifying and correcting all elements of the lethal diamond.
It is notable that routine capture of pre-hospital serum calcium measurements, and subsequent appropriate calcium administration in major trauma patients, would likely mitigate the impact of hypocalcaemia in this cohort. There is a need for first responders to recognise the signs and symptoms of hypocalcaemia (e.g., prolonged QT interval arrhythmias), the underlying mechanisms (i.e., the clotting cascade), and risk factors (e.g., hypovolemic shock) to positively benefit ongoing care11. Data already exists demonstrating the merits of different methods of administering treatment (e.g., calcium gluconate vs calcium chloride)4. Finally, factors including cost of provision of measurement devices, consumables, training, storage and maintenance need to be addressed to provide an effective solution.
Further research through randomised controlled trials would provide a basis for assessing the potential impact of measurement and treatment of hypocalcaemia in the pre-hospital context, thus providing benefit to ongoing hospital care of the major trauma patient, and in turn reducing mortality and morbidity in this patient cohort. The implications of such research would also provide an opportunity for additional avenues of seamless care between the pre-hospital and hospital settings to further benefit patient outcomes overall. This study contributes to igniting further enquiry that will ultimately provide better care for trauma patients.
Acknowledgements
The authors would like to acknowledge Army School of Health staff and Hannah Mills for their support.
Conflict of interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
Author(s)
Lucy Bridge-Dubarry*1, Gavin Smith2
1 Army School of Health, Australian Army, Latchford Barracks, VIC, Australia
2 Registered MICA Paramedic (MICA 19), Ambulance Victoria, VIC, Australia; Adj. Senior Research Fellow, Translational Medicine and Public Health, Monash University, VIC, Australia; Adj. A/Prof., School of Medicine, Griffith University, QLD, Australia; Associate Editor, Proceedings, Royal Society of Victoria, VIC, Australia
*Corresponding author email lucy.bridge-dubarry@defence.gov.au
References
- Vasudeva M, Mathew JK, Fitzgerald MC, Cheung Z, Mitra B. Hypocalcaemia and traumatic coagulopathy: An observational analysis. Vox Sanguinis 2019;115(2):189–95.
- Mikhail J. The trauma triad of death: hypothermia, acidosis, and coagulopathy. Am Assoc Crit Care Nurse 1999;10(1):85–94.
- Wray JP, Bridwell RE, Schauer SG, Shackleford SA, Bebarta VS, Wright FL. The diamond of death: hypocalcaemia in trauma and resuscitation. Am J Emerg Med 2021;41:104–9.
- Blackney D. Administration of calcium in trauma. J Paramed Pract 2022;14(7):279–86.
- Ditzel RM, Anderson JL, Eisenhart WJ, Rankin CJ, DeFeo DR, Oak S. A review of transfusion- and trauma-induced hypocalcaemia. J Trauma Acute Care Surg 2020;88(3):434–9.
- Kronstedt S, Roberts N, Ditzel R, Elder J, Steen A, Thompson K. Hypocalcaemia is a predictor of mortality and transfusion. A scoping review of hypocalcaemia in trauma and hemostatic resuscitation. Transfusion 2022;62(1).
- Moore HB, Tessmer MT, Moore EE, Sperry JL, Cohen MJ, Chapman MP, et al. Forgot calcium? Admission ionised-calcium in two civilian randomised controlled trials of prehospital plasma for traumatic haemorrhagic shock. J Trauma Acute Care Surg 2020;88(5):588–96.
- Webster S, Todd S, Redhead J, Wright C. Ionised calcium levels in major trauma patients who received blood in the emergency department. Emerg Med J 2016;33(8):569–72.
- Evans D. Heirarchy of evidence: a framework for ranking evidence evaluating healthcare interventions. J Clin Nurs 2002;12(1):77–84.
- Ambulance Victoria. Clinical practice guidelines for ALS and MICA paramedics; 2019.
- Vasudeva M, Mathew JK, Groombridge C, Tee JW, Johnny CS, Maini A, et al. Hypocalcaemia in trauma patients: a systematic review. J Acute Care Surg 2020;90(2):396–402.