Volume 25 Number 1
The management of wound odour and exudate using a multi-purpose dressing – a case series
Sebastian Probst, Camille Saini
Keywords Exudate, chronic wound, Pain, odour, maceration, multi-purpose dressing
For referencing Probst S & Saini C. The management of wound odour and exudate using a multi-purpose dressing – a case series. Journal of Wound Management 2024;25(1):43-47.
DOI
10.35279/jowm2024.25.01.04
Submitted 24 October 2023
Accepted 27 November 2023
Abstract
Background and aim The care of chronic wounds (CWs) is complex and their management is multifaceted. To manage the clinical manifestations, the performance of a multi-purpose dressing in the management of odour, exudate, pain and healing in patients with CWs attending a wound outpatient clinic was assessed.
Method A case series using descriptive statistics was conducted with 22 consecutive patients with an existing odorous CW attending a wound outpatient clinic. Participants were treated with a multi-purpose dressing.
Results All participants had a complete reduction of their wound odour between the first and the second dressing application (p<0.001). Maceration was reduced or completely eliminated in all exudative wounds (81.8%). All cases decreased in wound size during the study time (mean percentage 45.5%; SD 15.3). Pain was reduced in 55% and unchanged in 45% of wounds.
Conclusion and implication for practice Multi-purpose dressings provide a reduction of wound odour, wound area, as well as maceration area. In addition, the dressing has a more moderate impact on pain reduction.
Key messages
- To manage the clinical manifestations, the performance of a multi-purpose dressing in terms of management of odour, exudate, pain and healing in patients with chronic wounds (CWs) admitted in wound outpatient clinics was assessed.
- A total of 22 case studies from within wound care outpatients where a multi-purpose dressing was used for exudate and odour management were collated.
- A multi-purpose dressing provides a reduction of wound odour, wound area, as well as maceration area.
Introduction
Chronic wounds (CWs) affect approximately 2.21 individuals per 1,000 in the population and are often incorrectly treated1. The prevalence of chronic diseases is expected to increase in the upcoming years due to the ageing population. The most common CWs include venous, arterial or diabetic ulcers. CWs impose significant humanistic and economic burdens, both at an individual level (e.g., affecting quality of life)2,3 and at a societal level (e.g., increasing healthcare costs)4,5. The humanistic burden primarily relates to the quality of life and encompasses both physical and psychological dimensions3.
The care of CWs has become a specialty in its own due to their complex, chronic nature. The therapeutic approach to managing such wounds is multifaceted, targeting the management of risk factors and clinical manifestations such as odour or exudate. Wound odour and exudate are reported as some of the most distressing symptoms, leading to psychological discomfort and embarrassment among patients, their families and clinicians6. Unpleasant odours are caused by tissue degradation and bacterial colonisation, involving volatile agents that contain molecules capable of easy evaporation7. In wounds, such agents include organic acids as well as cadaverine and putrescine8. Malodour and its effects on individuals has been widely investigated and reported as feelings of disgust, likened to the smell of rotting meat, or as a source of stress9. Odour management is, therefore, important but challenging. A recently published systematic review by Gethin et al7. has shown that activated charcoal can be used for odour reduction.
Exudate production in a wound that is progressing normally reduces over time10. However, in CWs, it is believed to prolong the inflammatory phase and be detrimental to healing11. Overproduction may result in dressing leakage which can be unpleasant for patients. To absorb high volumes of exudate, superabsorbent dressings are used12. A randomised controlled trial demonstrated that, when applying such dressing, there is faster wound area reduction (0.45cm² per day vs. 0.2cm² per day), longer wear time (9.5 days vs. 8.1 days), and more pronounced maceration reduction (–2.07cm²) compared to standard care (–0.71cm²)13. A study from Germany confirmed these results, showing that the application of superabsorbent dressings on exudating leg ulcers can lead to an improved healing rate of 2.57% (benefit ratio 1.08)14.
However, it is important to choose a wound dressing that addresses both odour and wound exudate. Therefore, we conducted a case series to assess the performance of a multi-purpose dressing which is frequently used in clinical practice. This assessment was carried out on 22 patients with CWs in an outpatient setting over the course of dressing application.
Method
Study design
For this study a case series design was chosen. In a case series, observations are made on a series of individuals, usually all receiving the same intervention, before and after an intervention but with no control group15. This current study evaluated the effectiveness of a multi-purpose dressing in managing odour, exudate, pain and wound area evolution in patients with CWs admitted to one wound care outpatient clinic in Western Switzerland.
Treatment material
The treatment for which these case studies have been assigned is a multi-purpose dressing that is indicated for hard-to-heal and low-to-heavy exuding wounds, as well as for infected or vulnerable-to-infection wounds. This dressing is a hydrophilic, spun-bonded non-woven dressing composed of polypropylene, web treatment and additives (pigments). It has an air-formed, non-woven composite of pulp (cellulose) and cross-linked acrylate polymer with a knitted activated charcoal cloth (Curea P1 Duo Active). Polyacrylate wound dressings/pads are a relatively recent addition to the clinician’s toolbox. These dressings are highly effective for exudate management as their substantial absorbency and fluid retention can be adjusted to the need. The dressing used for this case series additionally contains a layer of activated charcoal and has the ability to sequestrate and inhibit bacteria and matrix metalloproteinases (MMPs) as well as to bind toxins in the core.
Case series
A total of 22 case studies from within a wound care outpatient clinic where a multi-purpose dressing was used for odour and exudate management were collated. Consecutive patients admitted to the participating clinic were screened for participation. Inclusion criteria were patients with a full thickness exuding odorous CW that had been present for greater than 4 weeks, being 18 years or older, and proficient in French language. Ethical approval was granted by the ethics committee of the Canton of Geneva, Switzerland (2018-01589).
The study nurses performed data entry between November 2018 to March 2020 using electronic support (EvaSys GmbH, Germany) and measured wound areas using a 3D wound imaging device16. The dressing application period was defined as the time from the start of treatment until the dressing was no longer clinically indicated, i.e., when the wound no longer produced excessive exudate. Data were collected at baseline and at the end of the dressing application period, including type of wound, area (cm²), odour (Visual Analog Scale (VAS) 0–100) as perceived by the study nurses, pain (VAS 0–10) as reported by the participants, and peri-wound skin maceration (cm²). Socioeconomic and health data were collected at baseline only.
Wound and patient characteristics were reported using descriptive statistics. Continuous variables are presented as means and standard deviations (SD) or medians and interquartile ranges (IQR) as appropriate. Categorical variables are expressed as counts and percentages. Odour, maceration, pain and wound area reductions were assessed over the dressing application period using classical tests of hypotheses for paired data. Statistical tests were two-sided, and p-values below 0.05 were considered statistically significant and conducted using STATA, version 17 (StataCorp LLC, 2021).
Results
Characteristics of study population
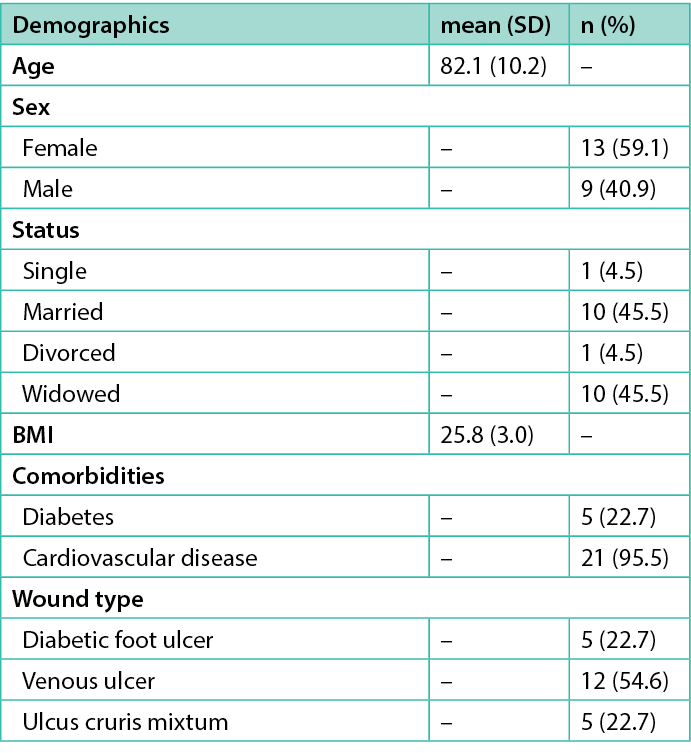
A total of 22 case studies meeting the eligibility criteria were available for analysis. The mean age was 82.1 years (SD 10.2), with slightly more females (59.1%, n=13). All cases manifested diagnosed malodourous venous ulcers (54.6%, n=12), mixed ulcers (22.7%, n=5), or diabetic foot ulcers (22.7%, n=5), all of them being exudating. Participants’ mean BMI was 25.8 (SD 3.0) and the most frequent comorbidity was cardiovascular disease (95.5%, n=21), followed by diabetes (22.7%, n=5) or a combination of both (18.2%, n=4) (Table 1).
Table 1. Characteristics of study population (n=22)
Wound odour evolution
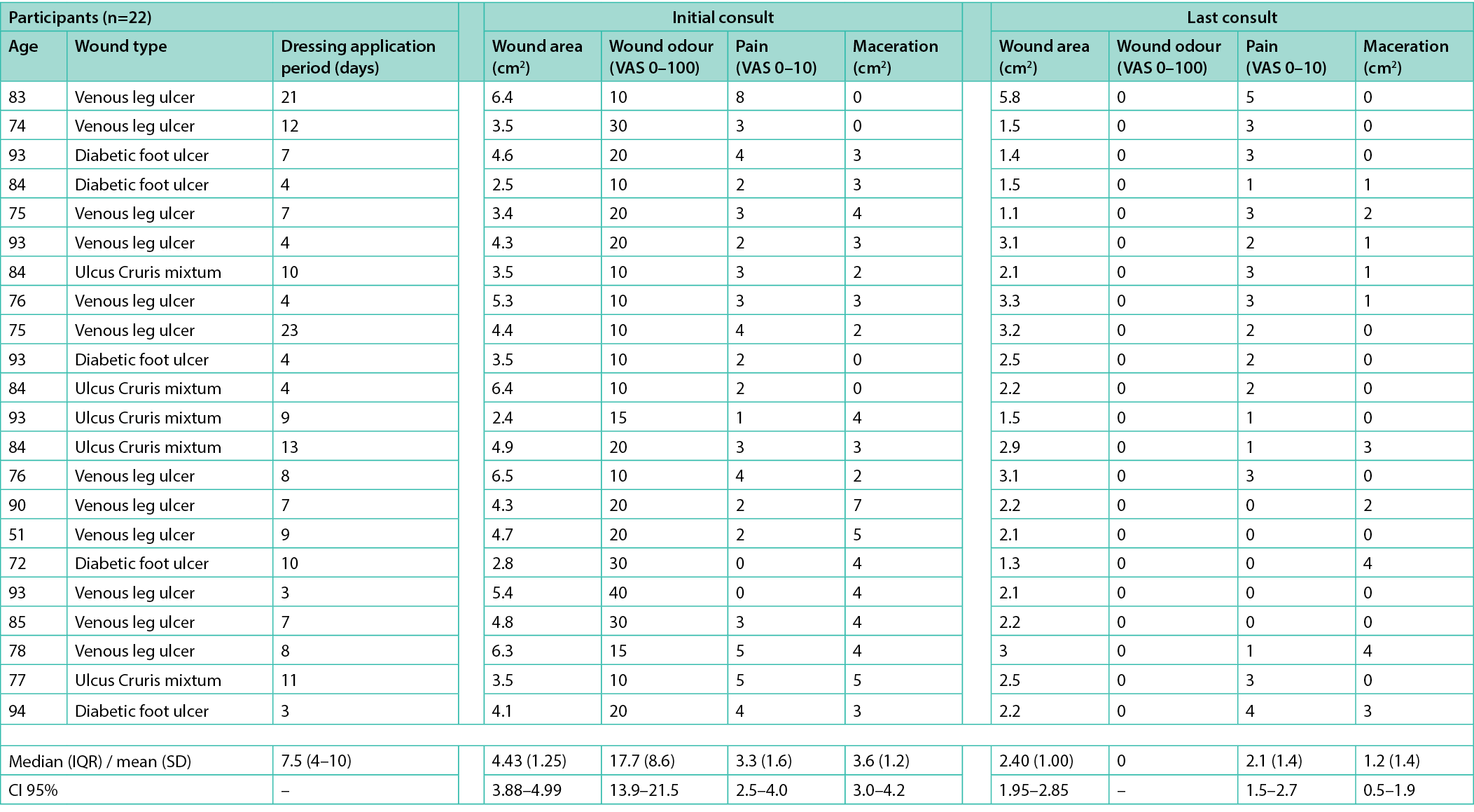
The mean level of odour was 17.7 (SD 8.6; 95% CI [13.9–21.5]; range 10–40) at the start of the study, as perceived by the study nurses. The multi-purpose dressing was used for periods ranging from 3–23 days (median 7.5; IQR 4–10). All participants experienced a complete disappearance of their wound odour (p<0.001) (Table 2).
Table 2. Individual participants’ wound characteristics
Exudate evolution
Among all participants, 81.8% (n=18) presented with exudative wounds accompanied by peri-wound skin maceration at the start of the study. In these exudative wounds, the mean maceration area extended to 3.6cm² (SD 1.2; 95% CI [3.0–4.2]; range 2–7). After the application of the multi-purpose dressing, maceration was reduced to a mean area of 1.2cm² (SD 1.4; 95% CI [0.5–1.9]; range 0–4) (p<0.001). The mean percentage of maceration area reduction was 65.1% (SD 40%; median 69.0%; IQR [50–100%]). Complete reduction of maceration was observed in 44.4% (8/18) of cases.
Pain evolution
At baseline, 90.9% (n=20) of the participants reported having pain, with a mean level of 3.3 (SD 1.6; 95% CI [2.5–4.0]). After the dressing application, the perceived pain decreased to a mean level of 2.1 (SD 1.4; 95% CI [1.5–2.7]) (p=0.001) (Table 2). In 25% of the participants experiencing pain (5/20), pain was reduced by at least two-thirds after a mean dressing application period of 8.8 days (SD 2.5; range 7–13). It reduced completely in 15.0% of participants (3/20), while it remained unchanged in another 45% (9/20).
Wound area evolution
The mean wound area was 4.43cm² (SD 1.25; 95% CI [3.88–4.99]) at the start of the study and 2.40cm² (SD 1.00; 95% CI [1.95–2.85]) at the end of the study (p<0.001). All wounds showed an area reduction between the two visits, with a mean percentage decrease of 45.5% (SD 15.3; range 9.4–69.6%), but none of them completely healed during the study period.
Discussion
This case series study, involving 22 participants, was designed to assess the performance of a multi-purpose dressing in managing odour, exudate, pain and wound area reduction. The examined wound dressing was a superabsorbent dressing with an integrated activated charcoal layer. Our study population was comparable to those of other studies on CWs17,18. The results demonstrate that this dressing had an effect in controlling odour. Evidence underscores the importance of odour control, as it can cause psychological distress and embarrassment for patients and their families9. Healthcare professionals face the challenge of controlling odour and providing appropriate wound care to improve the patients’ quality of life. In addition to managing odour, the assessment of exudate management was carried out. Our results demonstrate that when applying a multi-purpose dressing, the maceration area was reduced by an average of 65.1%. Therefore, managing exudate is crucial in preventing maceration11.
Wound-related pain is multidimensional in nature, encompassing persistent pain between dressing changes and intermittent pain that is often exacerbated during dressing changes19. It is therefore important to prevent pain during dressing changes because traumatic removal can cause pain and re-injury to the wound. This multi-purpose dressing includes a highly permeable non-woven layer helping to decrease pain. All cases showed a wound area reduction which we attribute to the creation of a moisture-balanced environment which limits maceration and promotes healing.
Additionally, odour and exudate containment may reduce dressing changes, resulting in an improved quality of life for patients. In our study, nearly all wounds (92.6%) showed an area reduction between the two visits, with a mean percentage of decrease of 46.5%. This can lead back because providing a moisture-balanced environment, limiting maceration of the wound bed and promotes wound healing. Thus, the use of a multi-purpose dressing in CWs could impinge on a person’s independence. During the entire study period no undesirable effects were observed.
Limitations
This case series had a number of limitations arising principally from including a heterogeneous sample and patients with various wound aetiologies. In addition, the inclusion criteria were large and therefore introduces further limitations in terms of generalisability. The inclusion of patients with non-healing wounds of the same aetiology would have provided opportunities for further comparative analysis.
Conclusion
The use of a case series helps generate valuable information regarding the use of wound dressings for patients with CWs. This case series evaluation supports the versatility of a multi-purpose dressing in achieving treatment goals, including the control of malodour, absorption of excessive exudate, pain reduction, and progress toward healing. Using a multi-purpose dressing may improve the patients’ quality of life due to resolution of malodour and containment of exudate which tend to make them very self-conscious and embarrassed.
Conflict of Interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
Author(s)
Sebastian Probst*1–4 DClinPrac, MNS, RN, Camille Saini1 PhD
1Geneva School of Health Science, HES-SO University of Applied Sciences and Arts, Western Switzerland, Avenue Champel 47, 1206 Geneva, Switzerland
2Care Directorate, University Hospital Geneva, Switzerland
3Faculty of Medicine Nursing and Health Sciences, Monash University, VIC, Australia
4College of Medicine Nursing and Health Sciences, University of Galway, Ireland
*Corresponding author email sebastian.probst@hesge.ch
References
- Martinengo L, Olsson M, Bajpai R, Soljak M, Upton Z, Schmidtchen A, et al. Prevalence of chronic wounds in the general population: systematic review and meta-analysis of observational studies. Ann Epidemiol 2019;29:8–15.
- Kapp S, Miller C, Santamaria N. The quality of life of people who have chronic wounds and who self-treat. J Clin Nurs 2018;27(1–2):182–92.
- Soares Dantas J, Silva CCM, Nogueira WP, de Oliveira ESAC, de Araújo E, da Silva Araújo P, et al. Health-related quality of life predictors in people with chronic wounds. J Tissue Viabil 2022;31(4):741–5.
- Phillips CJ, Humphreys I, Fletcher J, Harding K, Chamberlain G, Macey S. Estimating the costs associated with the management of patients with chronic wounds using linked routine data. Int Wound J 2016;13(6):1193–7.
- Järbrink K, Ni G, Sönnergren H, Schmidtchen A, Pang C, Bajpai R, et al. The humanistic and economic burden of chronic wounds: a protocol for a systematic review. System Rev 2017;6(1):15.
- Frykberg RG, Banks J. Challenges in the treatment of chronic wounds. Adv Wound Care 2015;4(9):560–82.
- Gethin G, Vellinga A, McIntosh C, Sezgin D, Probst S, Murphy L, et al. Systematic review of topical interventions for the management of odour in patients with chronic or malignant fungating wounds. J Tissue Viabil 2023;32(1):151–7.
- Gethin G, Grocott P, Probst S, Clarke E. Current practice in the management of wound odour: an international survey. Int J Nurs Stud 2014;51(6):865–74.
- Probst S, Arber A, Faithfull S. Malignant fungating wounds: the meaning of living in an unbounded body. Eur J Oncol Nurs 2013;17(1):38–45.
- Probst S. Wound care nursing. 3rd ed. London: Elsevier; 2021.
- Zhao R, Liang H, Clarke E, Jackson C, Xue M. Inflammation in chronic wounds. Int J Mol Sci 2016;17(12).
- Chamanga E. Effectively managing wound exudate. Br J Community Nurs 2015;Suppl Wound Care:S8, s10.
- Probst S, Saini C, Rosset C, Skinner MB. Superabsorbent charcoal dressing versus silver foam dressing in wound area reduction: a randomised controlled trial. J Wound Care 2022;31(2):140–6.
- Veličković VM, Szilcz M, Milošević Z, Godfrey T, Siebert U. Cost-effectiveness analysis of superabsorbent wound dressings in patients with moderate-to-highly exuding leg ulcers in Germany. Int Wound J 2022;19(2):447–59.
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007;335(7624):806–8.
- Anghel EL, Kumar A, Bigham TE, Maselli KM, Steinberg JS, Evans KK, et al. The reliability of a novel mobile 3-dimensional wound measurement device. Wounds 2016;28(11):379–86.
- Hindhede A, Meuleneire F. A clinical case-series evaluation of a superabsorbent dressing on exuding wounds. J Wound Care 2012;21(11):574, 6–80.
- Atkin L, Barrett S, Chadwick P, Callaghan R, Rippon MG, Rogers AA, et al. Evaluation of a superabsorbent wound dressing, patient and clinician perspective: a case series. J Wound Care 2020;29(3):174–82.
- Price PE, Fagervik-Morton H, Mudge EJ, Beele H, Ruiz JC, Nystrøm TH, et al. Dressing-related pain in patients with chronic wounds: an international patient perspective. Int Wound J 2008;5(2):159–71.
