Volume 22 Number 1
Comorbidities and clinical features of Martorell hypertensive ischemic leg ulcers: findings from a retrospective cohort study
Juan José Téllez Zaya, Elena Conde-Montero, Lorena Recarte Marín, Laura Pérez Jerónimo, Alicia Peral Vázquez, Alba Casillas Pérez, Pablo de la Cueva Dobao
Keywords epidemiology, Martorell ulcer, hypertensive ischemic leg ulcer, arteriolosclerosis, hypertension
DOI 10.35279/jowm202104.04
Abstract
Background Martorell hypertensive ischemic leg ulcers are commonly misdiagnosed, and their prevalence may be underestimated. There are still some aspects to be defined about the aetiopathogenesis of Martorell ulcers and the risk factors that may be involved with them.
Methods This is a single-centre retrospective case series study on the demographic characteristics and comorbidities in a series of patients with Martorell ulcer treated at a public university hospital in Madrid.
Results Comparing our results to previous studies, which are few and include small samples, the risk factors that we outline are an average age over 70 years and high blood pressure. Only two (5%) participants had poor control of their high blood pressure.
Conclusions and Implications for Clinical Practice Defining the epidemiological features of this type of leg ulcer may be very useful in differential diagnosis with other disorders, such as pyoderma gangrenosum.
INTRODUCTION
The most common causes of lower limb ulcers are venous insufficiency, arterial insufficiency and neuropathy. However, other less common aetiologies do exist and should be considered for differential diagnosis when atypical features arise, or when a wound does not respond to an accurate standard treatment.1
These less frequent wounds are classified as ‘atypical’ wounds. Martorell ulcers are included in this group.
In 1945, Fernando Martorell2 described four cases of supramalleolar ulcers with underlying arteriolitis in obese women with uncontrolled hypertension. From then on, many authors have published various clinical and histological features that characterise these lesions.2,3
The incidence of these ulcers is underestimated because they are an under-diagnosed type. This diagnostic failure is essentially due to a lack of knowledge of the existence of this entity. Consequently, it is essential to carry out studies that provide keys to facilitating its recognition and diagnosis.
The typical clinical presentation is a painful ulcer over the Achilles tendon or dorsolateral leg. Multiple bilateral lesions may be present in half of the cases. Skin infarction typically begins as a livid, painful area that rapidly turns into a necrotic lesion with reddish-purple edges. The development of satellite lesions is common (see Figures 1 and 2).

Figure 1: Typical clinical presentation of HYTILU on the Achilles tendon.
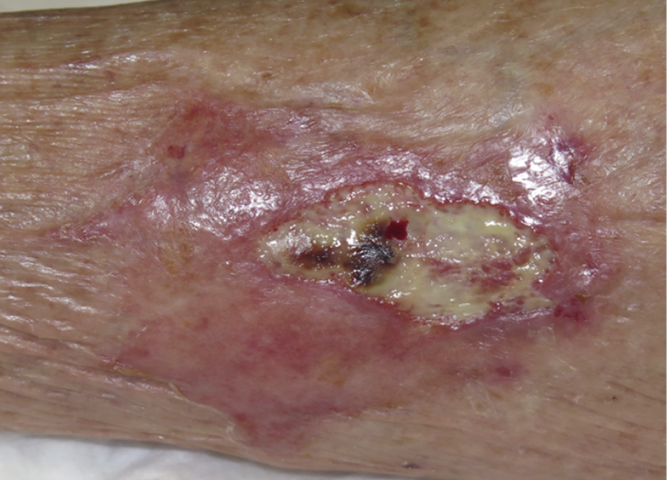
Figure 2: Typical clinical presentation of HYTILU on the lateral aspect of the leg.
Regarding epidemiological features, Martorell ulcers are more frequent in women, and most patients are more than 60 years old. Even though these ulcers have traditionally been associated with uncontrolled high blood pressure, they also commonly present following many years of well-controlled arterial hypertension and type 2 diabetes mellitus. Some patients describe a minor trauma as the trigger, but others report only a spontaneous onset with an initial livid macule.3 By definition, Martorell patients have no end-stage renal disease; otherwise, they would qualify for the distal form of ‘classical’ calciphylaxis. Calciphylaxis is a condition characterised by necrosis of the skin and subcutaneous tissue, which shares clinical and histological features with Martorell ulcers, but this is seen mainly in patients with end-stage kidney disease.
Considering the typical histopathology of the underlying arterioles, which show arteriosclerotic changes with a distinctive wall thickening that results in a narrow lumen, the term hypertensive ischemic leg ulcer (HYTILU) has been coined.4 However, the eponymous term ‘Martorell ulcer’ continues to be used.
As there are still aspects to be defined about the aetiopathogenesis of Martorell ulcer and the risk factors that may be involved, we have conducted a descriptive retrospective study on demographic characteristics and comorbidities in a series of patients with Martorell ulcers.
MATERIALS AND METHODS
Patients with Martorell HYTILUs treated in the outpatient wound practice of a public university hospital in Madrid between October 2015 and January 2020 were included in this single-centre descriptive retrospective study. All patients diagnosed with Martorell HYTILU were assessed with pulse palpation to rule out peripheral artery disease and, in cases of absence or doubt, a toe-brachial index was performed. All patients presented with typical clinical features, and biopsies were only taken to rule out other differential diagnoses. Demographic data from patients, their comorbidities and wound characteristics were registered. Data were obtained from the database of a previous study approved by the ethics committee. For statistical analysis, all qualitative variables are described by percentage, while quantitative variables are described by the mean and range.
RESULTS
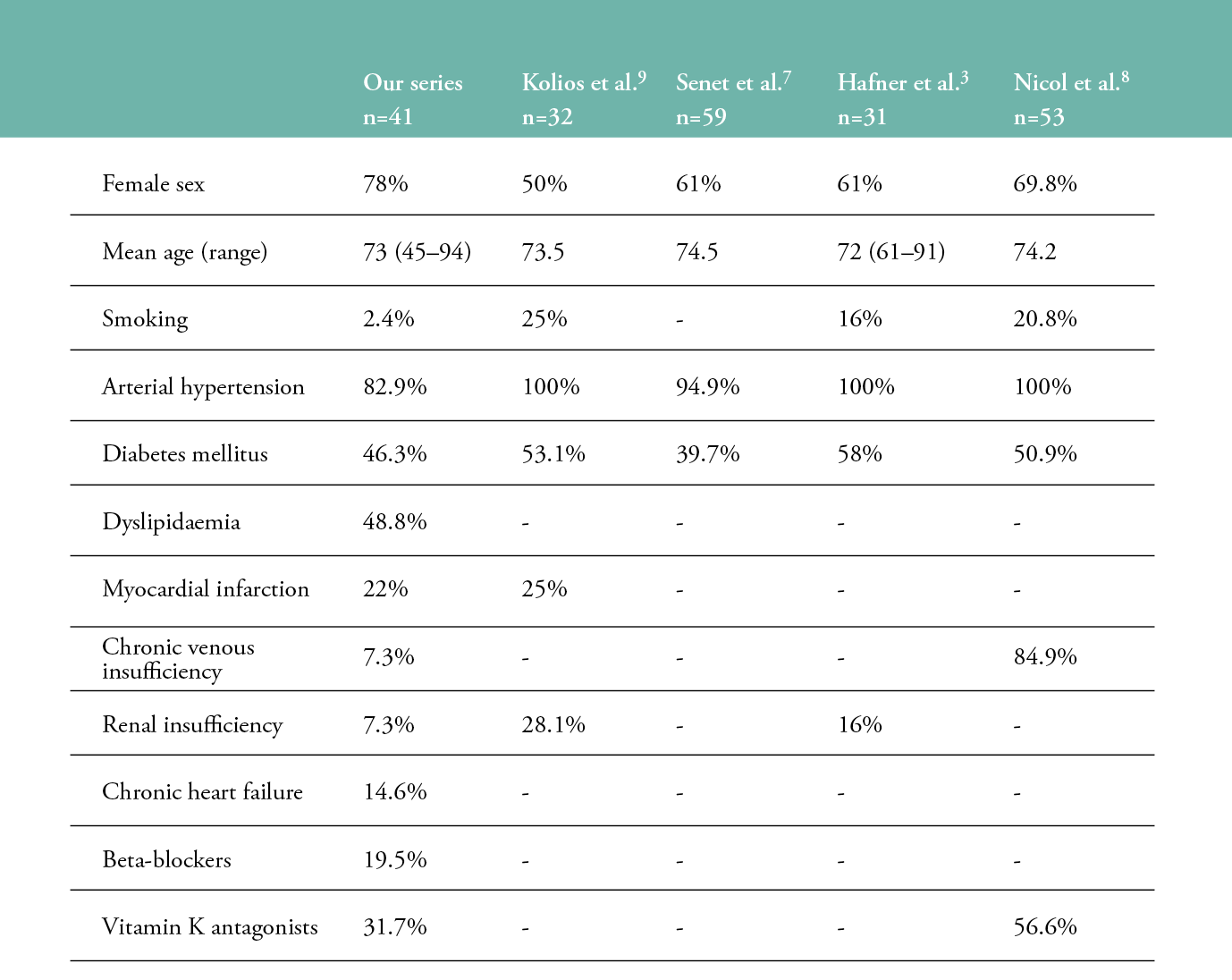
Forty-one patients were included in this case series study, of which 32 (78%) were women and 9 (22%) were men. The mean age was 73 years (range: 45–94 years old). In all, 34 patients (83%) presented with high blood pressure, 19 (46%) with type 2 diabetes mellitus and 20 (49%) with dyslipidaemia. Three patients were active smokers, and one patient was a former smoker. It is also remarkable that nine (22%) presented with ischemic myocardiopathy. It should be noted that only two (5%) had poor control of their high blood pressure. Three patients presented with chronic venous insufficiency (7.3%), and three had non-severe stages of chronic kidney disease (Table 1).
Table 1: Comparison of the epidemiological findings with previously published studies.
(-) Unknown information.
Only 2.44% of the wounds were biopsied to confirm diagnosis, and pyoderma gangrenosum (PG) was the differential diagnosis to rule out in those cases.
Regarding treatment for comorbidities, eight (19.5%) of the patients were taking beta-blockers, and 13 (31.7%) were treated with vitamin K antagonists at the time of the initial consultation. The average time until referral to our specialised clinic was 3 months (range: 2 weeks-–15 months). As for the surface of the wounds, the average was 1 cm2 (range 0.5–400 cm2).
DISCUSSION
Martorell leg ulcers are classically associated with essential hypertension (usually long-standing and well-controlled), type 2 diabetes mellitus and sometimes with vitamin K antagonist medications.3,5,8 It has also been suggested that nonselective beta-blockers are contraindicated for reducing cardiac output, as they worsen skin perfusion pressure.7
Martorell HYTILU and calciphylaxis share common epidemiological, clinical and histological characteristics and may be considered to be on the same spectrum. Common atherosclerosis results from inflammation and the remodelling of the arterial vessel wall. Hypertension, diabetes, dyslipidaemia and smoking are the four major cardiovascular risk factors in both entities.6
Compared with four epidemiological studies from Swiss and French investigators3,7–9, our mean patient age is similar, but the prevalence in women is superior. Mean wound duration is also similar, but the range of wound areas in our series was wider. Even if high blood pressure has been traditionally described as an inherent feature, in a French multi-centre study7 and in our case series, a small percentage of the patients did not present high blood pressure. Regarding diabetes mellitus, the condition was more prevalent in previous studies than in our series, but the range was 40–58%.7 Comparisons with other epidemiological studies are shown in Table 1.3,7–9
Martorell HYTILUs have a high level of vascular resistance due to a decrease in the compensatory dilatation of the arterioles supplying the dermal capillary bed.4 This vascular resistance may exist in hypertensive patients whose blood pressure has been under control for years. Consequently, Martorell ulcers may arise in patients with well-controlled hypertension; it seems that adequate therapeutic control of hypertension may not be sufficient for either preventing the occurrence or stopping the progression of Martorell HYTILUs.3
Regarding treatment at the initial consultation, 31.7% were on vitamin K antagonist medication. A French study of 54 patients evaluated the association between Martorell ulcers and the presence or absence of concomitant vitamin K antagonists. In the present study, we found no obvious differences.8
The need to perform a skin biopsy to confirm subcutaneous arteriolosclerosis as underlying pathology is controversial.7 The French school suggests basing a diagnosis of Martorell HYTILU on clinical patterns alone, provided that the clinical picture is characteristic. They argue that, particularly in small skin ulcers, a biopsy may iatrogenically worsen the condition, and that subcutaneous arteriolosclerosis is a nonspecific histopathologic finding, especially in the elderly population. In fact, arteriosclerosis is not exclusive to Martorell’s ulcer, but is associated with age and can be the trigger for extensive post-traumatic ulcers in older patients. Therefore, one could speak of a spectrum of lesions in the context of arteriosclerosis. As we agree with these French colleagues, we only performed skin biopsies when PG, necrotising vasculitis or further pathologies had to be ruled out.10
It is essential to promote epidemiological studies, in order to better define Martorell HYTILU as part of a spectrum of arteriosclerotic lesions. Moreover, the definition of typical comorbidities will help to differentiate it from the main differential diagnosis, which is PG. In fact, in a study by Hafner et al.3 of 31 patients, 52% of diagnosed Martorell ulcers were referred following a suspected diagnosis of PG. A Swiss study compared 32 HYTILU patients and 34 PG patients in terms of demographic data, laboratory values, localisation and comorbidities.9 Compared to PG, HYTILU appeared less frequently in women; at a later age; more often in smokers; showed lesion localisation only at the lower leg; featured more cardiovascular comorbidities, such as arterial hypertension, diabetes mellitus, peripheral artery occlusive disease and metabolic syndrome; and more microbial superinfections. These risk factors may be helpful for differential diagnosis.
CONCLUSION
A misdiagnosis of a Martorell ulcer not only means that treatment will not be effective, but it can also produce major complications, such as infections secondary to unnecessary immunosuppressive treatments. Defining the clinical features and comorbidities of this type of leg ulcer may be very useful in differential diagnosis.
Key messages
Martorell leg ulcer is a frequently misdiagnosed entity. In addition to histological findings, identification of typical risk factors may help to avoid misdiagnosis with pyoderma gangrenosum.
Author(s)
Juan José Téllez Zaya
Hospital Universitario Infanta Leonor, Madrid
Elena Conde-Montero
PhD. Department of Dermatology, Hospital Universitario Infanta Leonor y Virgen de la Torre, Madrid.
Lorena Recarte Marín
Centro de Especialidades Vicente Soldevilla, Madrid
Laura Pérez Jerónimo
Centro de Especialidades Vicente Soldevilla, Madrid
Alicia Peral Vázquez
Centro de Especialidades Vicente Soldevilla, Madrid
Alba Casillas Pérez
Centro de Especialidades Vicente Soldevilla. Madrid
Pablo de la Cueva Dobao
PhD, Chief of Service. Department of Dermatology, Hospital Universitario Infanta Leonor y Virgen de la Torre, Madrid
Correspondence: elenacondemontero@gmail.com
Conflicts of Interest: None
References
- Shelling ML, Federman DG, Kirsner RS. Clinical approach to atypical wounds with a new model for understanding hypertensive ulcers. Arch Dermatol 2010; 146(9):1026–9.
- Martorell F. Las ulceras supramaleolares por arteriolitis de las grandes hipertensas. Actas (Reun Cientif Cuerpo Facul) Inst Policlinico Barcelona 1945; 1(1):6–9.
- Hafner J, Nobbe S, Partsch H, et al. Martorell hypertensive ischemic leg ulcer: a model of ischemic subcutaneous arteriolosclerosis. Arch Dermatol 2010; 146(9):961–8.
- Hines EA, Farber EM. Ulcer of the leg due to arteriosclerosis and ischemia, occurring in the presence of hypertensive disease (hypertensive-ischemic ulcers). Proc Staff Meet Mayo Clin 1946; 21(18):337–46.
- Alavi A, Mayer D, Hafner J, Sibbald RG. Martorell hypertensive ischemic leg ulcer: an underdiagnosed Entity. Adv Skin Wound Care 2012; 25(12):563–72.
- Isoherranen K, O’Brien JJ, Barker J, et al. Atypical wounds. Best clinical practice and challenges. J Wound Care 2019; 28(Sup6):S1–92. doi:10.12968/jowc.2019.28.Sup6.S1
- Senet P, Beneton N, Debure C, et al. Angiodermites nécrotiques: caractéristiques épidémiologiques et facteurs pronostiques de cicatrisation dans une cohorte prospective [Hypertensive leg ulcers: epidemiological characteristics and prognostic factors for healing in a prospective cohort]. Ann Dermatol Venereol 2012; 139(5):346–9.
- Nicol P, Bernard P, Nguyen P, Durlach A, Perceau G. Étude rétrospective des angiodermites nécrotiques au CHU de Reims: données épidémiologiques, cliniques, évolutives et rôle des antivitamine K [Retrospective study of hypertensive leg ulcers at Reims University Hospital: Epidemiological, clinical, disease progression data, effects of vitamin K antagonists]. Ann Dermatol Venereol 2017 Jan; 144(1):37–44.
- Kolios AGA, Hafner J, Luder C, Guenova E, Kerl K, Kempf W, Nilsson J, French LE, Cozzio A. Comparison of pyoderma gangrenosum and Martorell hypertensive ischaemic leg ulcer in a Swiss cohort. Br J Dermatol 2018 Feb; 178(2):e125–6.
- Monfort JB, Cury K, Moguelet P, Chasset F, Bachmeyer C, Francès C, Barbaud A, Senet P. Cutaneous arteriolosclerosis is not specific to ischemic hypertensive leg ulcers. Dermatology 2018; 234(5-6):194–7.
